Submitted:
26 November 2024
Posted:
27 November 2024
You are already at the latest version
Abstract
Keywords:
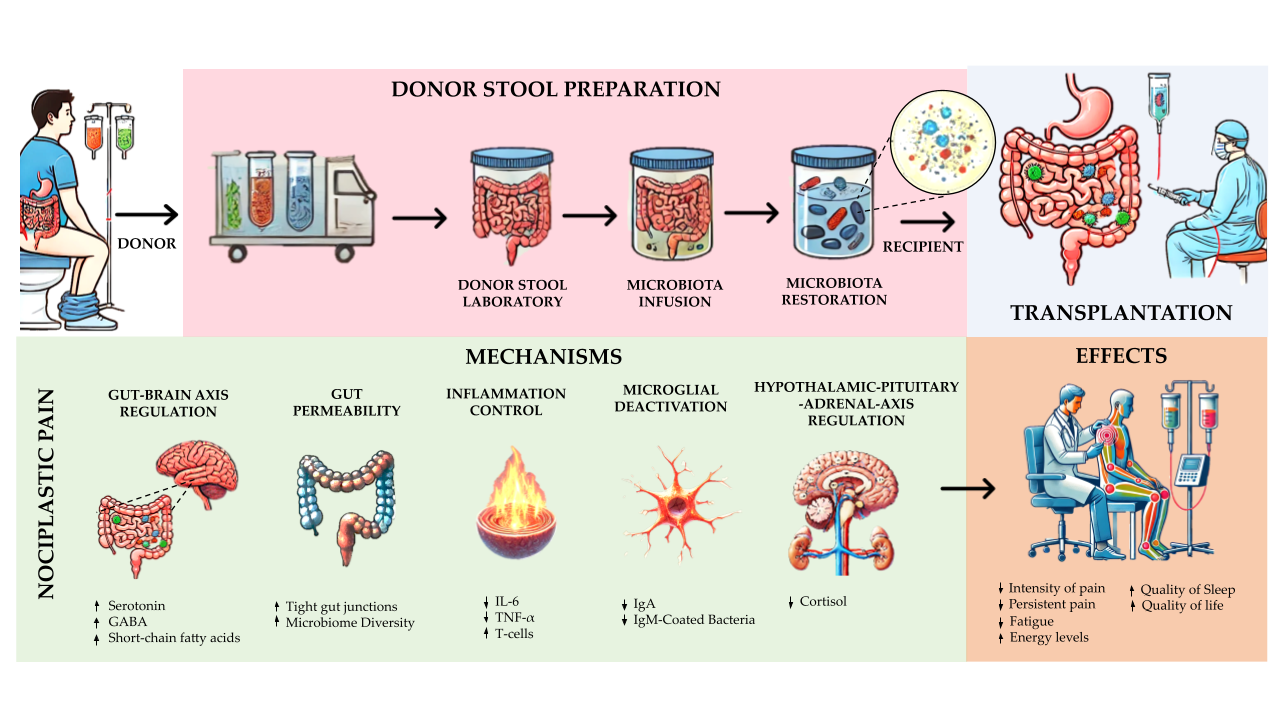
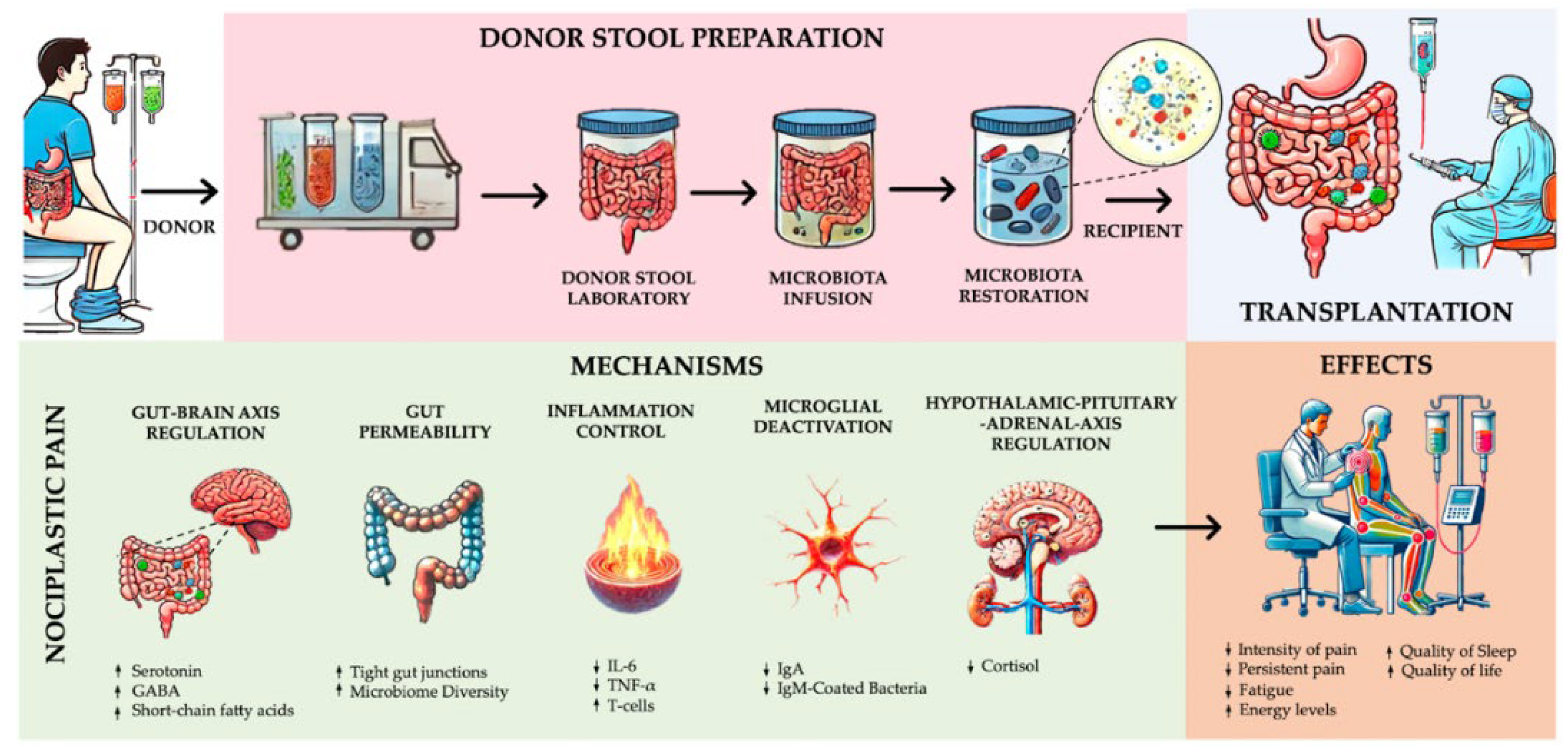
1. Introduction
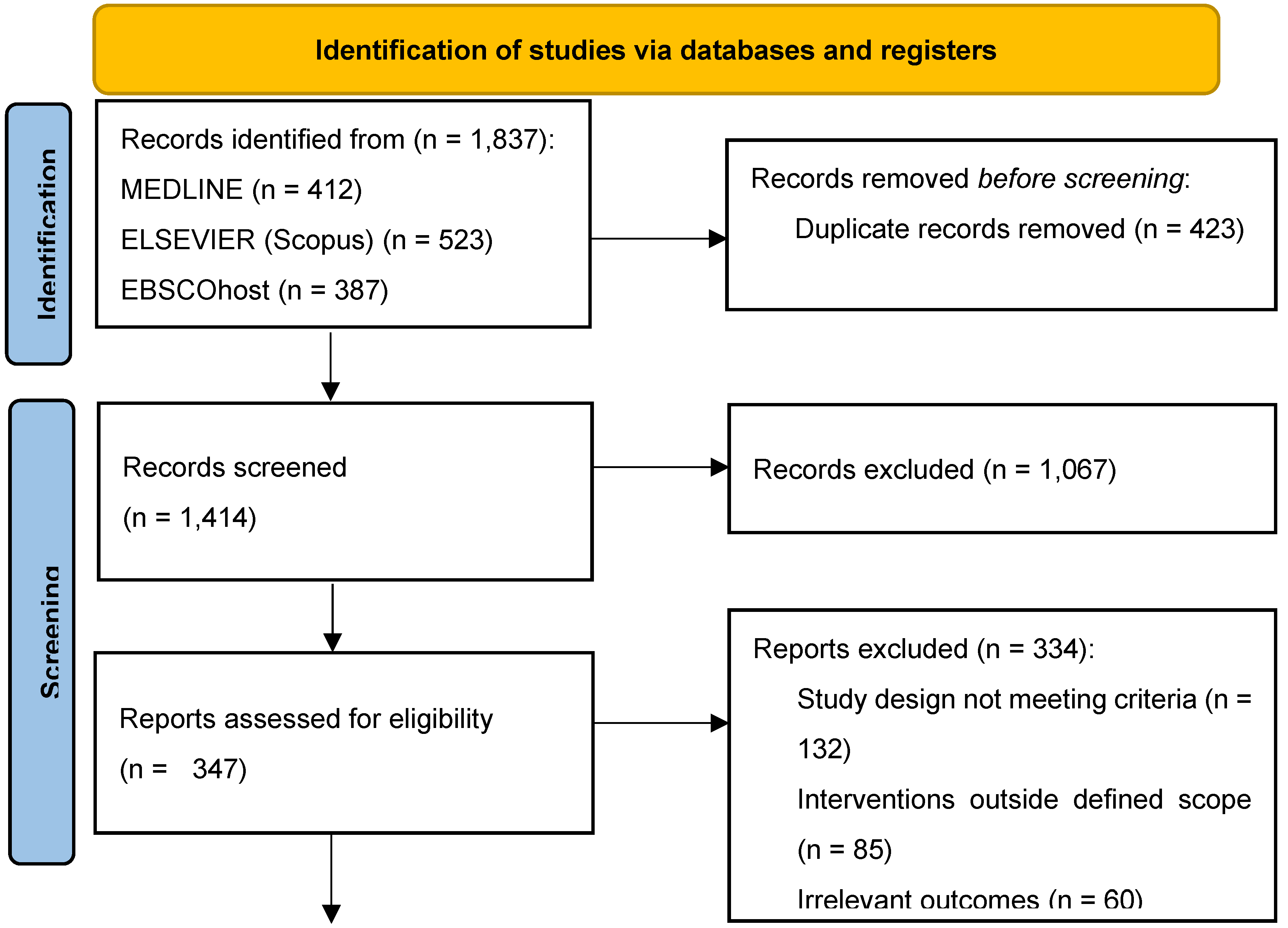
2. Materials and Method
2.1. Data Sources and Search Strategy
| Search date | Database | Search terms | Search string |
|---|---|---|---|
| 30/11/2024 | EBSCOhost | "faecal microbiota transplantation", "nociplastic pain", "FMT", "gut microbiota", "immune response modulation", "FMT intervention strategies", "chronic pain management", "central sensitization" | ((faecal microbiota transplantation OR FMT) AND (nociplastic pain OR FMT)) AND (gut microbiota OR immune response modulation OR FMT intervention strategies OR chronic pain management OR central sensitization) |
| 14/11/2024 | EBSCOhost | "nociplastic pain treatments", "FMT approaches in pain", "gut microbiome modulation", "FMT for nociplastic pathways", "immune modulation in pain disorders", "chronic inflammatory response modulation" | ((nociplastic pain treatments OR FMT approaches in pain OR gut microbiome modulation) AND (FMT for nociplastic pathways OR immune modulation in pain disorders OR chronic inflammatory response modulation)) |
| 30/10/2024 | Scopus | "nociplastic pain", "gut-brain axis", "FMT efficacy for pain", "chronic pain disorders", "gut microbiome modulation", "FMT and nociplastic pain", "inflammatory response in chronic pain" | (TITLE-ABS-KEY("nociplastic pain") OR TITLE-ABS-KEY("gut-brain axis") OR TITLE-ABS-KEY("FMT efficacy for pain")) AND (TITLE-ABS-KEY("chronic pain disorders") OR TITLE-ABS-KEY("gut microbiome modulation") OR TITLE-ABS-KEY("FMT and nociplastic pain") OR TITLE-ABS-KEY("inflammatory response in chronic pain")) |
| 10/10/2024 | MEDLINE (PubMed) | “faecal microbiota transplant", "fecal microbiota transplantation", "nociplastic pain", "chronic pain", "pain sensitization", "central sensitization", "gut-brain axis", "pain modulation" | ("faecal microbiota transplant"[Title/Abstract] OR "fecal microbiota transplantation"[Title/Abstract] OR "fecal transplantation"[Title/Abstract] OR "faecal transplant"[Title/Abstract] OR "gut microbiota"[Title/Abstract]) AND ("nociplastic pain" OR "chronic pain" OR "pain sensitization" OR "central sensitization" OR "gut-brain axis" OR "pain modulation") |
| 05/10/2024 | EBSCOhost | "FMT for pain disorders", "immune modulation in chronic pain", "gut microbiota interventions", "pain sensitization modulation", "nociplastic pain strategies", "chronic pain inflammatory response", "gut-brain modulation" | ((FMT for pain disorders OR gut microbiota interventions) AND (immune modulation in chronic pain OR pain sensitization modulation OR nociplastic pain strategies OR chronic pain inflammatory response OR gut-brain modulation)) |
| 01/10/2024 | Web of Science (WOS) | "gut microbiota interventions", "FMT treatment strategies", "nociplastic pain pathways", "chronic pain treatment", "immune modulation therapies", "gut-brain immune connection", "FMT in pain modulation" | TS=("gut microbiota interventions" OR "FMT treatment strategies" OR "nociplastic pain pathways") AND TS=("chronic pain treatment" OR "immune modulation therapies" OR "gut-brain immune connection" OR "FMT in pain modulation") |
| 20/09/2024 | MEDLINE (PubMed) | “FMT for chronic pain", "faecal microbiota transplantation", "immune modulation in pain", "microbiota interventions", "pain disorders", "gut-brain immune axis", "chronic nociceptive pain", "gut microbiome" | ("FMT for chronic pain"[Title/Abstract] OR "faecal microbiota transplantation"[Title/Abstract] OR "microbiota interventions"[Title/Abstract]) AND ("immune modulation in pain" OR "pain disorders" OR "gut-brain immune axis" OR "chronic nociceptive pain" OR "gut microbiome") |
| 15/09/2024 | Scopus | "chronic pain treatment", "FMT intervention", "gut microbiota therapy", "pain modulation therapies", "central sensitization disorders", "nociplastic pain interventions" | (TITLE-ABS-KEY("FMT intervention") OR TITLE-ABS-KEY("gut microbiota therapy") OR TITLE-ABS-KEY("chronic pain treatment")) AND (TITLE-ABS-KEY("pain modulation therapies") OR TITLE-ABS-KEY("central sensitization disorders") OR TITLE-ABS-KEY("nociplastic pain interventions")) |
| 14/09/2024 | Web of Science (WOS) | "FMT for chronic inflammatory pain", "nociplastic pain interventions", "gut-brain axis modulation", "immune modulation and pain", "FMT for nociplastic mechanisms", "chronic inflammation modulation" | TS=("FMT for chronic inflammatory pain" OR "nociplastic pain interventions") AND TS=("gut-brain axis modulation" OR "immune modulation and pain" OR "FMT for nociplastic mechanisms" OR "chronic inflammation modulation") |
| 12/09/2024 | Scopus | "faecal microbiota transplant", "fecal microbiota transplantation", "gut microbiota modulation", "nociplastic pain mechanisms", "FMT for chronic pain", "chronic inflammatory pain", "pain modulation strategies" | (TITLE-ABS-KEY("faecal microbiota transplant") OR TITLE-ABS-KEY("fecal microbiota transplantation") OR TITLE-ABS-KEY("gut microbiota modulation") OR TITLE-ABS-KEY("FMT for chronic pain")) AND (TITLE-ABS-KEY("nociplastic pain mechanisms") OR TITLE-ABS-KEY("chronic inflammatory pain") OR TITLE-ABS-KEY("pain modulation strategies")) |
| 07/09/2024 | Cochrane Library | "faecal microbiota transplant", "fecal microbiota transplantation", "gut microbiota modulation", "nociplastic pain mechanisms", "FMT for chronic pain", "chronic inflammatory pain", "pain modulation strategies" | ("faecal microbiota transplant" OR "fecal microbiota transplantation" OR "gut microbiota modulation" OR "FMT for chronic pain") AND ("nociplastic pain mechanisms" OR "chronic inflammatory pain" OR "pain modulation strategies") |
| 04/09/2024 | MEDLINE (PubMed) | “gut microbiota modulation", "FMT efficacy", "pain modulation", "nociplastic mechanisms", "microbiota-gut-brain axis", "inflammatory modulation", "central pain sensitization", "gut dysbiosis" | ("gut microbiota modulation"[Title/Abstract] OR "FMT efficacy"[Title/Abstract] OR "faecal microbiota transplant"[Title/Abstract]) AND ("nociplastic mechanisms" OR "microbiota-gut-brain axis" OR "pain modulation" OR "inflammatory modulation" OR "central pain sensitization" OR "gut dysbiosis") |
| 04/09/2024 | Web of Science (WOS) | "faecal microbiota transplantation", "nociplastic pain", "chronic inflammatory disorders", "gut microbiota", "central sensitization", "pain disorders", "immune modulation", "pain treatment", "FMT therapy" | TS=("faecal microbiota transplantation" OR "FMT" OR "faecal transplant") AND TS=("nociplastic pain" OR "chronic inflammatory disorders" OR "central sensitization" OR "pain disorders" OR "gut microbiota" OR "immune modulation" OR "pain treatment") |
| 02/09/2024 | Cochrane Library | "gut microbiota modulation", "FMT efficacy", "pain modulation", "nociplastic mechanisms", "microbiota-gut-brain axis", "inflammatory modulation", "central pain sensitization", "gut dysbiosis" | ("gut microbiota modulation"[Title/Abstract] OR "FMT efficacy"[Title/Abstract] OR "faecal microbiota transplant"[Title/Abstract]) AND ("nociplastic mechanisms" OR "microbiota-gut-brain axis" OR "pain modulation" OR "inflammatory modulation" OR "central pain sensitization" OR "gut dysbiosis") |
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Methodological Quality Assessment
2.4.1. Randomized Controlled Trials
2.4.2. Non-randomized Clinical Trials
2.4.3. Case Reports
2.4.4. Observational Study
3. Results
3.1. Study Selection
3.2. Characteristics of Included Studies
3.3. Methodological Quality Assessment
3.3.1. Randomized Controlled Trials
3.3.2. Open-Label Trials
3.3.4. Case Reports
3.3.5. Retrospective Outcome Study
3.4. Main Results
3.4.1. Severity of Nociplastic Pain Following FMT
3.4.2. Functionality and Quality of Life of Nociplastic Pain Following FMT
3.4.2. Other Effects in Nociplastic Pain Following FMT
4. Discussion
4.1. Severity of Nociplastic Pain Following FMT
4.2. Functionality and Quality of Life in Nociplastic Pain Following FMT
4.3. Other Physiological and Biochemical Effects of FMT on Nociplastic Pain
4.4. Implications for Practice
4.5. Implications for Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fitzcharles, M.A.; Cohen, S.P.; Clauw, D.J.; Littlejohn, G.; Usui, C.; Häuser, W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet 2021, 397, 2098–2110. [Google Scholar] [CrossRef] [PubMed]
- Yoo, Y.M.; Kim, K.H. Current understanding of nociplastic pain. Korean J. Pain 2024, 37, 107–118. [Google Scholar] [CrossRef]
- Hausteiner-Wiehle, C.; Henningsen, P. Nociplastic pain is functional pain. Lancet 2022, 399, 1603–1604. [Google Scholar] [CrossRef]
- Martínez-Lavín, M. Centralized nociplastic pain causing fibromyalgia: an emperor with no clothes? Clin. Rheumatol. 2022, 41, 3915–3917. [Google Scholar] [CrossRef]
- Clauw, D.J. From fibrositis to fibromyalgia to nociplastic pain: how rheumatology helped get us here and where do we go from here? Ann. Rheum. Dis. 2024, 83, 1421–1427. [Google Scholar] [CrossRef] [PubMed]
- Murphy, A.E.; Minhas, D.; Clauw, D.J.; Lee, Y.C. Identifying and Managing Nociplastic Pain in Individuals With Rheumatic Diseases: A Narrative Review. Arthritis Care Res. (Hoboken) 2023, 75, 2215–2222. [Google Scholar] [CrossRef] [PubMed]
- Kosek, E.; Clauw, D.; Nijs, J.; Baron, R.; Gilron, I.; Harris, R.E.; Mico, J.A.; Rice, A.S.C.; Sterling, M. Chronic nociplastic pain affecting the musculoskeletal system: clinical criteria and grading system. Pain 2021, 162, 2629–2634. [Google Scholar] [CrossRef]
- Ablin, J.N. Nociplastic Pain: A Critical Paradigm for Multidisciplinary Recognition and Management. J. Clin. Med. 2024, 13, 5741. [Google Scholar] [CrossRef] [PubMed]
- Alcántara Montero, A.; Pacheco de Vasconcelos, S.R.; Castro Arias, A. Contextualization of the concept of nociplastic pain in irritable bowel syndrome. Rev. Esp. Enferm. Dig. 2024. [CrossRef]
- Midenfjord, I.; Grinsvall, C.; Koj, P.; Carnerup, I.; Törnblom, H.; Simrén, M. Central sensitization and severity of gastrointestinal symptoms in irritable bowel syndrome, chronic pain syndromes, and inflammatory bowel disease. Neurogastroenterol. Motil. 2021, 33, e14156. [Google Scholar] [CrossRef]
- Nijs, J.; Leysen, L.; Vanlauwe, J.; Logghe, T.; Ickmans, K.; Polli, A.; Malfliet, A.; Coppieters, I.; Huysmans, E. Treatment of central sensitization in patients with chronic pain: time for change? Expert Opin. Pharmacother. 2019, 20, 1961–1970. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A.; Ryu, H.J.; Bhatt, R.R. The neurobiology of irritable bowel syndrome. Mol. Psychiatry 2023, 28, 1451–1465. [Google Scholar] [CrossRef]
- Cryan, J.F.; O'Riordan, K.J.; Cowan, C.S.M.; Sandhu, K.V.; Bastiaanssen, T.F.S.; Boehme, M.; Codagnone, M.G.; Cussotto, S.; Fulling, C.; Golubeva, A.V.; Guzzetta, K.E.; Jaggar, M.; Long-Smith, C.M.; Lyte, J.M.; Martin, J.A.; Molinero-Perez, A.; Moloney, G.; Morelli, E.; Morillas, E.; O'Connor, R.; Cruz-Pereira, J.S.; Peterson, V.L.; Rea, K.; Ritz, N.L.; Sherwin, E.; Spichak, S.; Teichman, E.M.; van de Wouw, M.; Ventura-Silva, A.P.; Wallace-Fitzsimons, S.E.; Hyland, N.; Clarke, G.; Dinan, T.G. The Microbiota-Gut-Brain Axis. Physiol. Rev. 2019, 99, 1877–2013. [Google Scholar] [CrossRef] [PubMed]
- Pratt, M.L.; Plumb, A.N.; Manjrekar, A.; Cardona, L.M.; Chan, C.K.; John, J.M.; Sadler, K.E. Microbiome contributions to pain: a review of the preclinical literature. Pain 2024. [CrossRef]
- Lee, J.; Lee, G.; Ko, G.; Joong Lee, S. Nerve injury-induced gut dysbiosis contributes to spinal cord TNF-α expression and nociceptive sensitization. Brain Behav. Immun. 2023, 110, 155–161. [Google Scholar] [CrossRef]
- Garvey, M. The Association between Dysbiosis and Neurological Conditions Often Manifesting with Chronic Pain. Biomedicines 2023, 11, 748. [Google Scholar] [CrossRef]
- Goudman, L.; Demuyser, T.; Pilitsis, J.G.; Billot, M.; Roulaud, M.; Rigoard, P.; Moens, M. Gut dysbiosis in patients with chronic pain: a systematic review and meta-analysis. Front. Immunol. 2024, 15, 1342833. [Google Scholar] [CrossRef] [PubMed]
- Agirman, G.; Yu, K.B.; Hsiao, E.Y. Signaling inflammation across the gut-brain axis. Science 2021, 374, 1087–1092. [Google Scholar] [CrossRef]
- Donoso, F.; Cryan, J.F.; Olavarría-Ramírez, L.; Nolan, Y.M.; Clarke, G. Inflammation, Lifestyle Factors, and the Microbiome-Gut-Brain Axis: Relevance to Depression and Antidepressant Action. Clin. Pharmacol. Ther. 2023, 113, 246–259. [Google Scholar] [CrossRef]
- Borody, T.J.; Khoruts, A. Fecal microbiota transplantation and emerging applications. Nat. Rev. Gastroenterol. Hepatol. 2011, 9, 88–96. [Google Scholar] [CrossRef]
- Gupta, S.; Allen-Vercoe, E.; Petrof, E.O. Fecal microbiota transplantation: in perspective. Therap. Adv. Gastroenterol. 2016, 9, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.W.; Kuo, C.H.; Kuo, F.C.; Wang, Y.K.; Hsu, W.H.; Yu, F.J.; Hu, H.M.; Hsu, P.I.; Wang, J.Y.; Wu, D.C. Fecal microbiota transplantation: Review and update. J. Formos. Med. Assoc. 2019, 118 Suppl 1, S23–S31. [Google Scholar] [CrossRef]
- Hsu, W.H.; Wang, J.Y.; Kuo, C.H. Current applications of fecal microbiota transplantation in intestinal disorders. Kaohsiung J. Med. Sci. 2019, 35, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.M.; Pestana, L.; Pardi, R.; Pardi, D.S.; Khanna, S. Fecal microbiota transplant via colonoscopy may be preferred due to intraprocedure findings. Intest. Res. 2019, 17, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Ramai, D.; Zakhia, K.; Fields, P.J.; Ofosu, A.; Patel, G.; Shahnazarian, V.; Lai, J.K.; Dhaliwal, A.; Reddy, M.; Chang, S. Fecal Microbiota Transplantation (FMT) with Colonoscopy Is Superior to Enema and Nasogastric Tube While Comparable to Capsule for the Treatment of Recurrent Clostridioides difficile Infection: A Systematic Review and Meta-Analysis. Dig. Dis. Sci. 2021, 66, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Luo, Y.; Walsh, S.; Grinspan, A. Oral Fecal Microbiota Transplant Capsules Are Safe and Effective for Recurrent Clostridioides difficile Infection: A Systematic Review and Meta-Analysis. J. Clin. Gastroenterol. 2021, 55, 300–308. [Google Scholar] [CrossRef]
- Lucarini, E.; Di Pilato, V.; Parisio, C.; Micheli, L.; Toti, A.; Pacini, A.; Bartolucci, G.; Baldi, S.; Niccolai, E.; Amedei, A.; Rossolini, G.M.; Nicoletti, C.; Cryan, J.F.; O'Mahony, S.M.; Ghelardini, C.; Di Cesare Mannelli, L. Visceral Sensitivity Modulation by Faecal Microbiota Transplantation: The Active Role of Gut Bacteria in Pain Persistence. Pain 2022, 163, 861–877. [Google Scholar] [CrossRef]
- de Groot, P.F.; Frissen, M.N.; de Clercq, N.C.; Nieuwdorp, M. Fecal Microbiota Transplantation in Metabolic Syndrome: History, Present and Future. Gut Microbes 2017, 8, 253–267. [Google Scholar] [CrossRef]
- Settanni, C.R.; Ianiro, G.; Bibbò, S.; Cammarota, G.; Gasbarrini, A. Gut Microbiota Alteration and Modulation in Psychiatric Disorders: Current Evidence on Fecal Microbiota Transplantation. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110258. [Google Scholar] [CrossRef]
- Tao, R.; Liu, S.; Crawford, J.; Tao, F. Gut-Brain Crosstalk and the Central Mechanisms of Orofacial Pain. Brain Sci. 2023, 13, 1456. [Google Scholar] [CrossRef]
- Guo, R.; Chen, L.H.; Xing, C.; Liu, T. Pain Regulation by Gut Microbiota: Molecular Mechanisms and Therapeutic Potential. Br. J. Anaesth. 2019, 123, 637–654. [Google Scholar] [CrossRef] [PubMed]
- Lin, B.; Wang, Y.; Zhang, P.; Yuan, Y.; Zhang, Y.; Chen, G. Gut Microbiota Regulates Neuropathic Pain: Potential Mechanisms and Therapeutic Strategy. J. Headache Pain 2020, 21, 103. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011); The Cochrane Collaboration: 2011. Available online: https://www.handbook.cochrane.org (accessed on 17 november 2024).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomized Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomized Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D. The CARE Guidelines: Consensus-Based Clinical Case Reporting Guideline Development. J. Clin. Epidemiol. 2014, 67, 46–51. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O'Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-randomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 17 november 2024).
- Fang, H.; Hou, Q.; Zhang, W.; Su, Z.; Zhang, J.; Li, J.; Lin, J.; Wang, Z.; Yu, X.; Yang, Y.; Wang, Q.; Li, X.; Li, Y.; Hu, L.; Li, S.; Wang, X.; Liao, L. Fecal Microbiota Transplantation Improves Clinical Symptoms of Fibromyalgia: An Open-Label, Randomized, Nonplacebo-Controlled Study. J. Pain 2024, 25, 104535. [Google Scholar] [CrossRef]
- Salonen, T.; Jokinen, E.; Satokari, R.; et al. Randomized, Double-Blinded, Placebo-Controlled Pilot Study: Efficacy of Faecal Microbiota Transplantation on Chronic Fatigue Syndrome. J. Transl. Med. 2023, 21, 513. [Google Scholar] [CrossRef]
- Singh, P.; Alm, E.J.; Kelley, J.M.; Cheng, V.; Smith, M.; Kassam, Z.; Nee, J.; Iturrino, J.; Lembo, A. Effect of Antibiotic Pretreatment on Bacterial Engraftment after Fecal Microbiota Transplant (FMT) in IBS-D. Gut Microbes 2022, 14, 2020067. [Google Scholar] [CrossRef]
- Holvoet, T.; Joossens, M.; Vázquez-Castellanos, J.F.; Christiaens, E.; Heyerick, L.; Boelens, J.; Verhasselt, B.; van Vlierberghe, H.; De Vos, M.; Raes, J.; De Looze, D. Fecal Microbiota Transplantation Reduces Symptoms in Some Patients With Irritable Bowel Syndrome With Predominant Abdominal Bloating: Short- and Long-Term Results From a Placebo-Controlled Randomized Trial. Gastroenterology 2021, 160, 145–157e8. [Google Scholar] [CrossRef]
- Kragsnaes, M.S.; Kjeldsen, J.; Horn, H.C.; Munk, H.L.; Pedersen, J.K.; Just, S.A.; Ahlquist, P.; Pedersen, F.M.; de Wit, M.; Möller, S.; Andersen, V.; Kristiansen, K.; Kinggaard Holm, D.; Holt, H.M.; Christensen, R.; Ellingsen, T. Safety and Efficacy of Faecal Microbiota Transplantation for Active Peripheral Psoriatic Arthritis: An Exploratory Randomised Placebo-Controlled Trial. Ann. Rheum. Dis. 2021, 80, 1158–1167. [Google Scholar] [CrossRef]
- Zeng, J.; Peng, L.; Zheng, W.; Huang, F.; Zhang, N.; Wu, D.; Yang, Y. Fecal Microbiota Transplantation for Rheumatoid Arthritis: A Case Report. Clin. Case Rep. 2020, 9, 906–909. [Google Scholar] [CrossRef]
- Fretheim, H.; Chung, B.K.; Didriksen, H.; Bækkevold, E.S.; Midtvedt, Ø.; Brunborg, C.; Holm, K.; Valeur, J.; Tennøe, A.H.; Garen, T.; Midtvedt, T.; Trøseid, M.; Zarè, H.; Lund, M.B.; Hov, J.R.; Lundin, K.E.A.; Molberg, Ø.; Hoffmann-Vold, A.M. Fecal Microbiota Transplantation in Systemic Sclerosis: A Double-Blind, Placebo-Controlled Randomized Pilot Trial. PLoS ONE 2020, 15, e0232739. [Google Scholar] [CrossRef] [PubMed]
- Lahtinen, P.; Jalanka, J.; Hartikainen, A.; Mattila, E.; Hillilä, M.; Punkkinen, J.; Koskenpato, J.; Anttila, V.J.; Tillonen, J.; Satokari, R.; Arkkila, P. Randomised Clinical Trial: Faecal Microbiota Transplantation Versus Autologous Placebo Administered via Colonoscopy in Irritable Bowel Syndrome. Aliment. Pharmacol. Ther. 2020, 51, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Kenyon, J.N.; Coe, S.; Izadi, H. A Retrospective Outcome Study of 42 Patients with Chronic Fatigue Syndrome, 30 of Whom Had Irritable Bowel Syndrome. Half Were Treated with Oral Approaches, and Half Were Treated with Faecal Microbiome Transplantation. Hum. Microbiome J. 2019, 13, 100061. [Google Scholar] [CrossRef]
- Johnsen, P.H.; Hilpüsch, F.; Valle, P.C.; Goll, R. The Effect of Fecal Microbiota Transplantation on IBS-Related Quality of Life and Fatigue in Moderate to Severe Non-Constipated Irritable Bowel: Secondary Endpoints of a Double-Blind, Randomized, Placebo-Controlled Trial. EBioMedicine 2020, 51, 102562. [Google Scholar] [CrossRef]
- El-Salhy, M.; Hatlebakk, J.G.; Gilja, O.H.; Bråthen Kristoffersen, A.; Hausken, T. Efficacy of Faecal Microbiota Transplantation for Patients with Irritable Bowel Syndrome in a Randomised, Double-Blind, Placebo-Controlled Study. Gut 2020, 69, 859–867. [Google Scholar] [CrossRef]
- Cai, T.T.; Ye, X.L.; Yong, H.J.; Song, B.; Zheng, X.L.; Cui, B.T.; Zhang, F.M.; Lu, Y.B.; Miao, H.; Ding, D.F. Fecal Microbiota Transplantation Relieve Painful Diabetic Neuropathy: A Case Report. Medicine (Baltimore) 2018, 97, e13543. [Google Scholar] [CrossRef]
- Thurm, T.; Ablin, J.N.; Buskila, D.; Maharshak, N. Fecal Microbiota Transplantation for Fibromyalgia: A Case Report and Review of the Literature. Open J. Gastroenterol. 2017, 7, 131–139. [Google Scholar] [CrossRef]
- Ustianowska, K.; Ustianowski, Ł.; Machaj, F.; Gorący, A.; Rosik, J.; Szostak, B.; Szostak, J.; Pawlik, A. The Role of the Human Microbiome in the Pathogenesis of Pain. Int. J. Mol. Sci. 2022, 23, 13267. [Google Scholar] [CrossRef]
- Liu, L.; Wu, Q.; Chen, Y.; Ren, H.; Zhang, Q.; Yang, H.; Zhang, W.; Ding, T.; Wang, S.; Zhang, Y.; Liu, Y.; Sun, J. Gut Microbiota in Chronic Pain: Novel Insights into Mechanisms and Promising Therapeutic Strategies. Int. Immunopharmacol. 2023, 115, 109685. [Google Scholar] [CrossRef]
- Santoni, M.; Miccini, F.; Battelli, N. Gut Microbiota, Immunity and Pain. Immunol. Lett. 2021, 229, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.J.; Zhang, X.J.; Zhang, N.N.; Yan, B.; Xu, K.K.; Peng, L.H.; Pan, F. Fecal Microbiota Transplantation for Patients with Irritable Bowel Syndrome: A Meta-Analysis of Randomized Controlled Trials. Front. Nutr. 2022, 9, 890357. [Google Scholar] [CrossRef] [PubMed]
- Matheson, J.T.; Holsinger, R.M.D. The Role of Fecal Microbiota Transplantation in the Treatment of Neurodegenerative Diseases: A Review. Int. J. Mol. Sci. 2023, 24, 1001. [Google Scholar] [CrossRef]
- Vergne-Salle, P.; Bertin, P. Chronic Pain and Neuroinflammation. Joint Bone Spine 2021, 88, 105222. [Google Scholar] [CrossRef]
- Ji, R.R.; Nackley, A.; Huh, Y.; Terrando, N.; Maixner, W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology 2018, 129, 343–366. [Google Scholar] [CrossRef]
- Zhang, W.H.; Jin, Z.Y.; Yang, Z.H.; Zhang, J.Y.; Ma, X.H.; Guan, J.; Sun, B.L.; Chen, X. Fecal Microbiota Transplantation Ameliorates Active Ulcerative Colitis by Downregulating Pro-Inflammatory Cytokines in Mucosa and Serum. Front. Microbiol. 2022, 13, 818111. [Google Scholar] [CrossRef]
- Porcari, S.; Benech, N.; Valles-Colomer, M.; Segata, N.; Gasbarrini, A.; Cammarota, G.; Sokol, H.; Ianiro, G. Key Determinants of Success in Fecal Microbiota Transplantation: From Microbiome to Clinic. Cell Host Microbe 2023, 31, 712–733. [Google Scholar] [CrossRef]
- Strandwitz, P. Neurotransmitter Modulation by the Gut Microbiota. Brain Res. 2018, 1693, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Kaelberer, M.M.; Rupprecht, L.E.; Liu, W.W.; Weng, P.; Bohorquez, D.V. Neuropod Cells: The Emerging Biology of Gut-Brain Sensory Transduction. Annu. Rev. Neurosci. 2020, 43, 337–353. [Google Scholar] [CrossRef]
- Szőke, H.; Kovács, Z.; Bókkon, I.; Vagedes, J.; Szabó, A.E.; Hegyi, G.; Sterner, M.G.; Kiss, Á.; Kapócs, G. Gut Dysbiosis and Serotonin: Intestinal 5-HT as a Ubiquitous Membrane Permeability Regulator in Host Tissues, Organs, and the Brain. Rev. Neurosci. 2020, 31, 415–425. [Google Scholar] [CrossRef]
- Quaranta, G.; Guarnaccia, A.; Fancello, G.; Agrillo, C.; Iannarelli, F.; Sanguinetti, M.; Masucci, L. Fecal Microbiota Transplantation and Other Gut Microbiota Manipulation Strategies. Microorganisms 2022, 10, 2424. [Google Scholar] [CrossRef] [PubMed]
- Hartikainen, A.K.; Jalanka, J.; Lahtinen, P.; Ponsero, A.J.; Mertsalmi, T.; Finnegan, L.; Crispie, F.; Cotter, P.D.; Arkkila, P.; Satokari, R. Fecal Microbiota Transplantation Influences Microbiota without Connection to Symptom Relief in Irritable Bowel Syndrome Patients. NPJ Biofilms Microbiomes 2024, 10, 73. [Google Scholar] [CrossRef] [PubMed]
- Rebeaud, J.; Peter, B.; Pot, C. How Microbiota-Derived Metabolites Link the Gut to the Brain during Neuroinflammation. Int. J. Mol. Sci. 2022, 23, 10128. [Google Scholar] [CrossRef]
- Ahmed, H.; Leyrolle, Q.; Koistinen, V.; Kärkkäinen, O.; Layé, S.; Delzenne, N.; Hanhineva, K. Microbiota-Derived Metabolites as Drivers of Gut-Brain Communication. Gut Microbes 2022, 14, 2102878. [Google Scholar] [CrossRef]
- Albrecht, D.S.; Forsberg, A.; Sandström, A.; Bergan, C.; Kadetoff, D.; Protsenko, E.; Lampa, J.; Lee, Y.C.; Höglund, C.O.; Catana, C.; et al. Brain Glial Activation in Fibromyalgia - A Multi-Site Positron Emission Tomography Investigation. Brain Behav. Immun. 2019, 75, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.; Fang, Y.D.; Jones, C.; McConathy, J.E.; Raman, F.; Lapi, S.E.; Younger, J.W. Evidence of Neuroinflammation in Fibromyalgia Syndrome: A [18F]DPA-714 Positron Emission Tomography Study. Pain 2023, 164, 2285–2295. [Google Scholar] [CrossRef]
- Marcondes Ávila, P.R.; Fiorot, M.; Michels, M.; Dominguini, D.; Abatti, M.; Vieira, A.; de Moura, A.B.; Behenck, J.P.; Borba, L.A.; Botelho, M.E.M.; et al. Effects of Microbiota Transplantation and the Role of the Vagus Nerve in Gut-Brain Axis in Animals Subjected to Chronic Mild Stress. J. Affect. Disord. 2020, 277, 410–416. [Google Scholar] [CrossRef]
- Xu, D.; Ren, L.; Zhang, W.; Wu, S.; Yu, M.; He, X.; Wei, Z. Therapeutic Effects and Mechanisms of Fecal Microbiota Transplantation on EAE Partly through HPA Axis-Mediated Neuroendocrine Regulation. Heliyon 2024, 10, e33214. [Google Scholar] [CrossRef] [PubMed]
- Braga, J.D.; Thongngam, M.; Kumrungsee, T. Gamma-Aminobutyric Acid as a Potential Postbiotic Mediator in the Gut-Brain Axis. NPJ Sci Food 2024, 8, 16. [Google Scholar] [CrossRef]
- Lou, X.; Xue, J.; Shao, R.; Yang, Y.; Ning, D.; Mo, C.; Wang, F.; Chen, G. Fecal Microbiota Transplantation and Short-Chain Fatty Acids Reduce Sepsis Mortality by Remodeling Antibiotic-Induced Gut Microbiota Disturbances. Front. Immunol. 2023, 13, 1063543. [Google Scholar] [CrossRef]
- Silva, Y.P.; Bernardi, A.; Frozza, R.L. The Role of Short-Chain Fatty Acids from Gut Microbiota in Gut-Brain Communication. Front. Endocrinol. (Lausanne) 2020, 11, 25. [Google Scholar] [CrossRef]
- Gupta, S.; Dinesh, S.; Sharma, S. Bridging the Mind and Gut: Uncovering the Intricacies of Neurotransmitters, Neuropeptides, and Their Influence on Neuropsychiatric Disorders. Cent. Nerv. Syst. Agents Med. Chem. 2024, 24, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Dalile, B.; Van Oudenhove, L.; Vervliet, B.; Verbeke, K. The Role of Short-Chain Fatty Acids in Microbiota-Gut-Brain Communication. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 461–478. [Google Scholar] [CrossRef] [PubMed]
- van de Wouw, M.; Boehme, M.; Lyte, J.M.; Wiley, N.; Strain, C.; O'Sullivan, O.; Clarke, G.; Stanton, C.; Dinan, T.G.; Cryan, J.F. Short-Chain Fatty Acids: Microbial Metabolites That Alleviate Stress-Induced Brain-Gut Axis Alterations. J. Physiol. 2018, 596, 4923–4944. [Google Scholar] [CrossRef] [PubMed]
- Marizzoni, M.; Cattaneo, A.; Mirabelli, P.; Festari, C.; Lopizzo, N.; Nicolosi, V.; Mombelli, E.; Mazzelli, M.; Luongo, D.; Naviglio, D.; Coppola, L.; Salvatore, M.; Frisoni, G.B. Short-Chain Fatty Acids and Lipopolysaccharide as Mediators Between Gut Dysbiosis and Amyloid Pathology in Alzheimer's Disease. J. Alzheimers Dis. 2020, 78, 683–697. [Google Scholar] [CrossRef]
- Więdłocha, M.; Marcinowicz, P.; Janoska-Jaździk, M.; Szulc, A. Gut Microbiota, Kynurenine Pathway and Mental Disorders - Review. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 106, 110145. [Google Scholar] [CrossRef]
- Deng, Y.; Zhou, M.; Wang, J.; Yao, J.; Yu, J.; Liu, W.; Wu, L.; Wang, J.; Gao, R. Involvement of the Microbiota-Gut-Brain Axis in Chronic Restraint Stress: Disturbances of the Kynurenine Metabolic Pathway in Both the Gut and Brain. Gut Microbes 2021, 13, 1–16. [Google Scholar] [CrossRef]
- Janzon, A.; Goodrich, J.K.; Koren, O.; TEDDY Study Group; Waters, J. L.; Ley, R.E. Interactions Between the Gut Microbiome and Mucosal Immunoglobulins A, M, and G in the Developing Infant Gut. mSystems 2019, 4, e00612–19. [Google Scholar] [CrossRef]
- DuPont, H.L.; Jiang, Z.D.; Alexander, A.S.; DuPont, A.W.; Brown, E.L. Intestinal IgA-Coated Bacteria in Healthy- and Altered-Microbiomes (Dysbiosis) and Predictive Value in Successful Fecal Microbiota Transplantation. Microorganisms 2022, 11, 93. [Google Scholar] [CrossRef]
| Year, Author | Study design | Participants | Intervention | Comparison | Outcomes | Conclusion |
|---|---|---|---|---|---|---|
| Fang et al. (2024) [38] China |
Open-label, randomized, non-placebo-controlled study | N = 60 (Fibromyalgia Syndrome) | FMT vs. continued standard treatment | Standard treatment |
Fibromyalgia Symptom Reduction: Significant reduction in pain intensity, fatigue, and other symptoms compared to control; no specific numerical values provided for exact reductions. Quality of Life Improvement and Gut Microbiota Changes: Observed improvements without detailed quantification. |
FMT may relieve Fibromyalgia symptoms by modulating gut microbiota. Further research is needed for confirmation. |
| Salonen et al. (2023) [39] Finland |
Randomized, double-blinded, placebo-controlled pilot study | N = 11 (Chronic Fatigue Syndrome patients, 10 female, 1 male, mean age 42.2 years) |
Dose: Universal donor stool. Route: Colonoscopy. Follow-up: 1 and 6 months. |
Placebo (autologous FMT) |
Fatigue & QoL: No statistically significant improvements. Adverse Events: None reported. |
FMT was safe but did not improve QoL for CFS patients |
| Singh et al. (2022) [40] India |
Randomized, placebo-controlled, single-center study | N = 44 (Irritable Bowel Syndrome-D patients) |
Dose: FMT alone or with antibiotic pretreatment. Route: Colonoscopy. Follow-up: 10 weeks. |
Placebo |
Engraftment: Higher (15.5%) in FMT alone vs. 5% (rifaximin pre-FMT) and 2.4% (CM-FMT). Symptom Scores: No significant difference in IBS severity. |
FMT alone may provide better microbiota engraftment for IBS-D |
| Holvoet et al. (2021) [41] Belgium |
Randomized, placebo-controlled trial | N = 62 (Irritable Bowel Syndrome patients with bloating) |
Dose: 50 g donor stool. Route: Nasojejunal tube. Follow-up: 12 weeks (up to 1 year). |
Autologous stool (placebo) |
Symptom Improvement: 56% FMT vs. 26% placebo (p=0.03). Quality of Life: Significant improvement initially, effects diminished over a year. |
FMT effective for IBS, but long-term effects vary |
| Kragsnaes et al. (2021) [42] Denmark |
Randomized, double-blind, placebo-controlled trial | N = 31 (Psoriatic arthritis) |
Dose: Single FMT. Route: Gastroscopy (Duodenum). Follow-up: 26 weeks. |
Sham (Placebo) |
Treatment Failure: Higher in FMT (60%) vs. sham (19%). HAQ-DI Score: Lesser improvement (-0.07 vs. -0.30, p=0.031). ACR20 Response: No significant difference |
FMT appears less effective than placebo for PsA symptoms |
| Zeng et al. (2021) [43] China |
Case report | N = 1 (20-year-old female with rheumatoid arthritis) | Dose: Single FMT. Route: Colonoscopy. Follow-up: 4 months. | No comparison |
Rapid and significant improvement in symptoms: HAQ-DI dropped from 1.4 to 0.05. Reduction in DAS28 from 6.6 to 1.4. Titer of rheumatoid factor decreased significantly. Symptoms maintained for 4 months with reduced need for medication. |
FMT shows potential for RA but requires further research |
| Fretheim et al. (2020) [44] Norway |
Double-blind, placebo-controlled randomized pilot trial | N = 10 (patients with systemic sclerosis) |
Dose: Commercial anaerobic human intestinal microbiota (ACHIM). Route: Gastroduodenoscopy. Follow-up: 16 weeks with two FMT sessions at weeks 0 and 2. |
Placebo |
Reduction in GI Symptoms: 80% (4/5) of patients receiving FMT improved compared to 50% (2/4) in the placebo group. Changes in Gut Microbiota Composition: Quantitative changes in IgA-, IgM-coated bacteria observed (no exact values provided). Procedure-Related Adverse Events: 2 serious events in the placebo group (1 case of laryngospasms, 1 case of duodenal perforation). |
FMT reduced GI symptoms but had procedural risks |
| Lahtinen et al.(2020) [45] Finland |
Randomized clinical trial | N = 49 (Irritable Bowel Syndrome) |
Dose: 30 g donor stool. Route: Colonoscopy. Follow-up: 12 weeks. |
Autologous FMT (placebo) |
IBS Symptoms: Improvement at 12 weeks (p=0.01), but no sustained effects. Microbiota Composition: Resembles donor. |
FMT provided transient symptom relief, but not a sustained improvement over placebo, limiting its clinical use. |
| Kenyon et al. (2019) [46] United Kingdom |
Retrospective outcome study | N = 42 (Chronic Fatigue Syndrome, 30 with Irritable Bowel Syndrome) |
Dose: 10 rectal FMTs from different donors. Route: Rectal catheter. Follow-up: Not specified. |
Standard oral approaches |
Improvement: Greater for sham (median change in HAQ-DI score -0.30 vs. -0.07 FMT). Treatment Failure: Higher for FMT (60%). |
FMT appears less effective for some CFS patients; further trials recommended |
| Johnsen et al. (2019) [47] Norway |
Double-blind, randomized, placebo-controlled trial | N = 90 (non-constipated Irritable Bowel Syndrome patients) |
Dose: 50-80 g donor stool. Route: Colonoscopy. Follow-up: 6 months. |
Placebo (own stool) |
QoL Improvement: OR = 3.801 (p=0.011). Fatigue Reduction: OR = 4.398 (p=0.020). |
QoL and fatigue improved in select IBS patients |
| El-Salhy et al. (2019) [48] Norway |
Randomized, double-blind, placebo-controlled study | N = 165 (Irritable Bowel Syndrome) |
Dose: 30 g or 60 g donor stool. Route: Gastroscope. Follow-up: 12 weeks. |
Placebo (own stool) |
Response Rate: 30 g = 76.9%, 60 g = 89.1%, placebo = 23.6% (p < 0.0001). Fatigue & QoL: Improved. Adverse Events: Mild. |
FMT is effective for IBS, showing a dose-dependent response with emphasis on donor selection. |
| Cai et al. (2018) [49] China |
Clinical case report | N = 1 (female, diabetic neuropathy) |
Dose: Two FMTs over 3 months. Route: Colonoscopy. Follow-up: 3 months. |
No explicit comparison group |
Pain Relief: Significant improvement. Glycemic Control: Noted improvement. Adverse Events: None observed. |
FMT may offer therapeutic benefit for diabetic complications |
| Thurm et al. (2017) [50] Germany |
Case report and literature review | N = 1 (58-year-old male with Fibromyalgia, Irritable Bowel Syndrome with Chronic Fatigue Syndrome) |
Dose: 6 self-administered FMTs. Route: Enema. Follow-up: 9 months. |
No formal comparison |
FMT group showed significantly greater improvement compared to the oral treatment group (Mann-Whitney U = 111.5, p = 0.003). Median improvement in the FMT group was markedly higher than oral treatment. No significant adverse effects except minor intolerance in 2 patients (1 with diarrhea; 1 tolerated half the implants). |
FMT may help complex functional disorders, though randomized trials are needed |
| Study | Design | Methodological Quality Tool | Final Score | Observed Biases |
|---|---|---|---|---|
| Fang et al. (2024) [38] | Open-label, randomized | ROBINS-I | Moderate | Open-label design leading to potential performance and detection biases. |
| Salonen et al. (2023) [39] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | Moderate | Concerns with blinding of outcome assessment and selective reporting. |
| Singh et al. (2022) [40] | Open-label, randomized | ROBINS-I | Moderate | Open-label nature affecting blinding and performance outcomes. |
| Holvoet et al. (2021) [41] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | Low | Appropriate randomization and effective blinding; potential unclear risk from missing data handling and selective reporting. |
| Kragsnaes et al. (2021) [42] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | Moderate | Issues with selective reporting noted. |
| Zeng et al. (2021) [43] | Case report | CARE | Good | Limited by lack of comparative data and generalizability. |
| Fretheim et al. (2020) [44] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | Moderate | Limited by small sample size and short follow-up. |
| Lahtinen et al. (2020) [45] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | Moderate | Potential blinding bias. |
| Kenyon et al. (2019) [46] | Retrospective outcome study | NOS | Moderate | Issues with selection bias and comparability between cohorts. |
| Johnsen et al. (2019) [47] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | High | Minor concerns regarding selective reporting. |
| El-Salhy et al. (2019) [48] | Randomized, double-blind, placebo-controlled | Cochrane RoB 2 | High | Minimal concerns noted. |
| Cai et al. (2018) [49] | Case report | CARE | Good | Inherent limitations due to case report nature |
| Thurm et al. (2017) [50] | Case report and literature review | CARE | Good | Detailed patient outcomes but limited generalizability and need for controlled trials. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





