Submitted:
22 November 2024
Posted:
26 November 2024
You are already at the latest version
Abstract
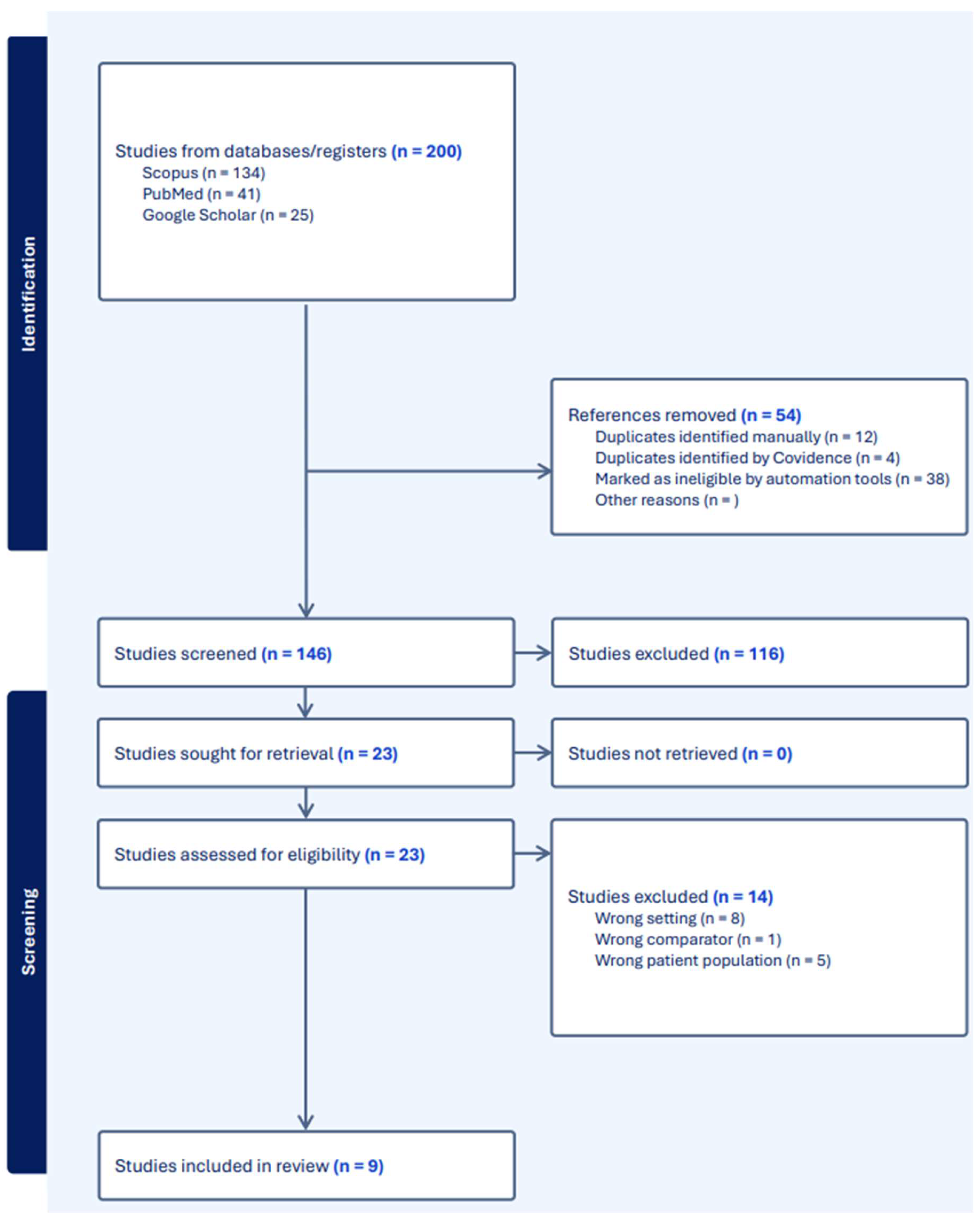
Background and Objectives: Persistent urogenital sinus (PUGS) is a rare congenital anomaly resulting from disruptions in urogenital development during embryogenesis, with an incidence of approximately 6/100,000 females. Characterized by the confluence of the vaginal canal and urethra into a single channel, it poses diagnostic and management challenges, particularly in adult patients. Surgical correction remains the primary treatment at an early age, yet there are no universally accepted guidelines regarding treatment at later stages in life. We explored current evidence on the management of high urogenital sinus (HUGS) in adults, focusing on surgical techniques, outcomes, perioperative care, and follow-up. Materials and Methods: A systematic review was conducted using PubMed, Scopus, and Google Scholar, including studies published up to August 2024. Search terms included "high urogenital sinus," "adult patients," and related conditions. Articles were included if they addressed clinical, diagnostic, or therapeutic data on HUGS in adult populations. Data extraction was performed independently by two reviewers, and a PRISMA flow diagram was used to outline the study selection process. Results: Nine studies met inclusion criteria, with data on surgical techniques, perioperative care, and long-term outcomes extracted for analysis. The included studies highlighted diverse surgical approaches such as feminizing genitoplasty, buccal mucosa vaginoplasty, posterior prone techniques, and robotic-assisted urogenital sinus mobilization. Complications like vaginal stenosis, urethrovaginal fistula, and urinary incontinence were reported. Long-term outcomes were underreported, with limited data on sexual function and patient satisfaction. Hormonal therapies, including glucocorticoids played critical roles in managing cases associated with congenital adrenal hyperplasia (CAH). Conclusions: The management of HUGS requires a multidisciplinary approach integrating advanced surgical techniques and individualized perioperative care. While short-term outcomes are generally favorable, long-term data on sexual function and quality of life remain scarce. Future research should prioritize longitudinal studies to address these gaps, aiming to optimize surgical outcomes, patient satisfaction, and psychosocial well-being.
Keywords:
Introduction
Embryology
Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Data Extraction and Quality Assessment
2.3 PRISMA Flow Diagram
Results
Discussion
Management Strategies and Surgical Techniques
Feminizing Genitoplasty and Buccal Mucosa Vaginoplasty
Feminizing Genital Reconstruction with Long-term Follow-up
Perineal Prone Approach without Division of the Rectum
Partial Urogenital Mobilization and Flap Vaginoplasty
Posterior Prone Approach with Pelvic Muscle Sparing
UGS Mobilization Maneuver for CAH Patients
Robotic Total Urogenital Sinus Mobilization
Staged Vaginal Reconstruction and Long-term Dilation
Peri-operative Care: Hormonal Treatment
Follow-up
Psychological Well-being and Support System
Conclusion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Valentini, A.L.; Giuliani, M.; Gui, B.; et al. Persistent Urogenital Sinus: Diagnostic Imaging for Clinical Management. What Does the Radiologist Need to Know? Am J Perinatol. 2016, 33, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Singh, P.; Singh, R.J. Persistent Urogenital Sinus. J Anat Soc India. 2010, 59, 242–244. [Google Scholar] [CrossRef]
- Shen, J.; Cunha, G.R.; Sinclair, A.; Cao, M.; Isaacson, D.; Baskin, L. Macroscopic whole-mounts of the developing human fetal urogenital-genital tract: Indifferent stage to male and female differentiation. Dev Hum Male Female Urogenit Tracts. 2018, 103, 5–13. [Google Scholar] [CrossRef]
- Schoenwolf GC, Bleyl SB, Brauer PR, Francis-West PH. Larsen’s Human Embryology. Elsevier Health Sciences; 2014.
- Acién, P.; Acién, M.I. The history of female genital tract malformation classifications and proposal of an updated system. Hum Reprod Update. 2011, 17, 693–705. [Google Scholar] [CrossRef]
- Martínez Escoriza, J.C.; Palacios Marqués, A.M.; López Fernández, J.A.; et al. Congenital vesicovaginal fistula with or without menouria: a literature review. Eur J Obstet Gynecol Reprod Biol. 2014, 175, 38–48. [Google Scholar] [CrossRef]
- Fernando, M.A.; Creighton, S.M.; Wood, D. The long-term management and outcomes of cloacal anomalies. Pediatr Nephrol. 2015, 30, 759–765. [Google Scholar] [CrossRef]
- Drews, U.; Sulak, O.; Schenck, P.A. Androgens and the development of the vagina. Biol Reprod. 2002, 67, 1353–1359. [Google Scholar] [CrossRef]
- Drews, U. Helper Function of the Wolffian Ducts and Role of Androgens in the Development of the Vagina. Sex Dev. 2007, 1, 100–110. [Google Scholar] [CrossRef]
- Larkins, C.E.; Enriquez, A.B.; Cohn, M.J. Spatiotemporal dynamics of androgen signaling underlie sexual differentiation and congenital malformations of the urethra and vagina. Proc Natl Acad Sci. 2016, 113, E7510–E7517. [Google Scholar] [CrossRef]
- Yucel, S.; Cavalcanti, A.G.; Wang, Z.; Baskin, L.S. The impact of prenatal androgens on vaginal and urogenital sinus development in the female mouse. J Urol. 2003, 170, 1432–1436. [Google Scholar] [CrossRef]
- Hotchkiss, A.K.; Furr, J.; Makynen, E.A.; Ankley, G.T.; Gray, L.E. In utero exposure to the environmental androgen trenbolone masculinizes female Sprague-Dawley rats. Toxicol Lett. 2007, 174, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, A.K.; Lambright, C.S.; Ostby, J.S.; Parks-Saldutti, L.; Vandenbergh, J.G.; Gray, L.E. Prenatal testosterone exposure permanently masculinizes anogenital distance, nipple development, and reproductive tract morphology in female Sprague-Dawley rats. Toxicol Sci Off J Soc Toxicol. 2007, 96, 335–345. [Google Scholar] [CrossRef]
- Braz, A. Posterior sagittal transanorectal approach in patients with ambiguous genitalia: report of eight cases. Pediatr Surg Int. 1999, 15, 108–110. [Google Scholar] [CrossRef]
- Samuelson, M.L.; Baker, L.A. Autologous buccal mucosa vulvovaginoplasty for high urogenital sinus. J Pediatr Urol. 2006, 2, 486–488. [Google Scholar] [CrossRef] [PubMed]
- Podesta, M.; Urcullo, J. Perineal mobilization of the common urogenital sinus for surgical correction of high urethrovaginal confluence in patients with intersex disorders. J Pediatr Urol. 2008, 4, 352–358. [Google Scholar] [CrossRef]
- Bailez, M.M.; Cuenca, E.S.; Dibenedetto, V. Urinary Continence Following Repair of Intermediate and High Urogenital Sinus (UGS) in CAH. Experience with 55 Cases. Front Pediatr. 2014, 2, 67. [Google Scholar] [CrossRef] [PubMed]
- Sircili, M.H.P.; Bachega, T.S.S.; Madureira, G.; Gomes, L.; Mendonca, B.B.; Dénes, F.T. Surgical Treatment after Failed Primary Correction of Urogenital Sinus in Female Patients with Virilizing Congenital Adrenal Hyperplasia: Are Good Results Possible? Front Pediatr. 2016, 4, 118. [Google Scholar] [CrossRef]
- Wang, Y.; Hu, S.; Wang, H. Multimodal ultrasound imaging of persistent urogenital sinus with uterus didelphys and double vagina malformation: A case report. Medicine (Baltimore) 2021, 100. https://journals.lww.com/md-journal/fulltext/2021/12300/multimodal_ultrasound_imaging_of_persistent.47.aspx. [CrossRef]
- Ulusoy, O.; Sabuncu, S.; Karakuş, O.Z.; et al. Urinary continence after high urogenital sinus repair conducted with posterior prone approach: electromyography-uroflowmetric assessment. Int Urol Nephrol. 2021, 53, 1813–1818. [Google Scholar] [CrossRef]
- Ellerkamp, V.; Rall, K.K.; Schaefer, J.; et al. Surgical Therapy After Failed Feminizing Genitoplasty in Young Adults With Disorders of Sex Development: Retrospective Analysis and Review of the Literature. J Sex Med. 2021, 18, 1797–1806. [Google Scholar] [CrossRef]
- Yang, J.; Syed, H.; Baker, Z.; Vasquez, E. Urogenital Sinus Diagnosed During Workup of Recurrent Urinary Tract Infections: A Case Report. Urology. 2023, 174, 165–167. [Google Scholar] [CrossRef] [PubMed]
- Rink, R.; Pope, J.; Kropp, B.; Smith, E.; Keating, M.; Adams, M. Reconstruction of the high urogenital sinus: early perineal prone approach without division of the rectum. J Urol. 1997, 158, 1293–1297. [Google Scholar] [CrossRef] [PubMed]
- Bailez, M.M.; Gearhart, J.P.; Migeon, C.; Rock, J. Vaginal reconstruction after initial construction of the external genitalia in girls with salt-wasting adrenal hyperplasia. J Urol. 1992, 148, 680-682; discussion 683-684. [Google Scholar] [CrossRef]
- Ghoniem, G.; Samaan, N.M.; Samir, M.; Hammad, M.A.M.; Fahmy, A.G. Successful management of high urogenital sinus in an adult female: Case report. Cont Rep. 2024, 12, 100068. [Google Scholar] [CrossRef]
- Auer, M.K.; Nordenström, A.; Lajic, S.; Reisch, N. Congenital adrenal hyperplasia. Lancet Lond Engl. 2023, 401, 227–244. [Google Scholar] [CrossRef]
- El-Maouche, D.; Arlt, W.; Merke, D.P. Congenital adrenal hyperplasia. Lancet Lond Engl. 2017, 390, 2194–2210. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, S.; Gomez-Lobo, V. Hormonal Contraceptives, Intrauterine Devices, Gonadotropin-releasing Hormone Analogues and Testosterone: Menstrual Suppression in Special Adolescent Populations. J Pediatr Adolesc Gynecol. 2019, 32, S23–S29. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists’ Committee on Clinical Consensus–Gynecology. General Approaches to Medical Management of Menstrual Suppression: ACOG Clinical Consensus No. 3. Obstet Gynecol. 2022, 140, 528–541. [Google Scholar] [CrossRef]
- Options for Prevention and Management of Menstrual Bleeding in Adolescent Patients Undergoing Cancer Treatment: ACOG Committee Opinion, Number 817. Obstet Gynecol. 2021, 137, e7–e15. [CrossRef]
- Almasri, J.; Zaiem, F.; Rodriguez-Gutierrez, R.; et al. Genital Reconstructive Surgery in Females With Congenital Adrenal Hyperplasia: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2018, 103, 4089–4096. [Google Scholar] [CrossRef]
- Nordenström, A.; Frisén, L.; Falhammar, H.; et al. Sexual function and surgical outcome in women with congenital adrenal hyperplasia due to CYP21A2 deficiency: clinical perspective and the patients’ perception. J Clin Endocrinol Metab. 2010, 95, 3633–3640. [Google Scholar] [CrossRef]
- Rapp, M.; Duranteau, L.; van de Grift, T.C.; et al. Self- and proxy-reported outcomes after surgery in people with disorders/differences of sex development (DSD) in Europe (dsd-LIFE). J Pediatr Urol. 2021, 17, 353–365. [Google Scholar] [CrossRef] [PubMed]
- MILLER, R.J.; BREECH, L.L. Surgical Correction of Vaginal Anomalies. Clin Obstet Gynecol 2008, 51. https://journals.lww.com/clinicalobgyn/fulltext/2008/06000/surgical_correction_of_vaginal_anomalies.7.aspx. [CrossRef] [PubMed]
- Burgu, B.; Duffy, P.G.; Cuckow, P.; Ransley, P.; Wilcox, D.T. Long-term outcome of vaginal reconstruction: comparing techniques and timing. J Pediatr Urol. 2007, 3, 316–320. [Google Scholar] [CrossRef]
- Filipas, D.; Black, P.; Hohenfellner, R. The use of isolated caecal bowel segment in complicated vaginal reconstruction. BJU Int. 2000, 85, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Krege, S.; Walz, K.H.; Hauffa, B.P.; Körner, I.; Rübben, H. Long-term follow-up of female patients with congenital adrenal hyperplasia from 21-hydroxylase deficiency, with special emphasis on the results of vaginoplasty. BJU Int. 2000, 86, 253-258; discussion 258-259. [Google Scholar] [CrossRef]
- Callens, N.; De Cuypere, G.; De Sutter, P.; et al. An update on surgical and non-surgical treatments for vaginal hypoplasia. Hum Reprod Update. 2014, 20, 775–801. [Google Scholar] [CrossRef]
- Mukherjee, B.; McCauley, E.; Hanford, R.B.; Aalsma, M.; Anderson, A.M. Psychopathology, psychosocial, gender and cognitive outcomes in patients with cloacal exstrophy. J Urol. 2007, 178, 630–635; discussion 634-635. [Google Scholar] [CrossRef]
- Ebert, A.; Scheuering, S.; Schott, G.; Roesch, W.H. Psychosocial and psychosexual development in childhood and adolescence within the exstrophy-epispadias complex. J Urol. 2005, 174, 1094–1098. [Google Scholar] [CrossRef]
| No. | Author(s) | Year | Diagnosis | Method of Diagnosis | Management | Complications | Number of Cases | Remarks/Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Braz, A | 1999 | Urogenital sinus, high vaginal implantation, normal rectum, sigmoidostomy | Cystoscopic and radiological examinations | Vaginal replacement with sigmoid colon, protective sigmoidostomy | Urethrovaginal fistula (re-operated and cured) | 8 | One patient successfully engaged in sexual intercourse post-vaginal replacement. |
| 2 | Mindy L. Samuelsonet al | 2006 | Mid-to-high urogenital sinus in adrenogenital syndrome | Clinical examination, endoscopic evaluation | Feminizing genitoplasty, buccal mucosa vulvovaginoplasty | None reported | 1 | - |
| 3 | Podesta, M et al | 2008 | Urogenital sinus anomalies in DSD | Clinical history, examination, laboratory tests, karyotyping, ultrasound, radiology, urethroscopy | Feminizing genital reconstruction | Glans atrophy, vaginal stricture, urinary stress incontinence | 12 | Achieved a satisfactory feminine genital appearance; long-term follow-up needed. |
| 4 | Bailez, M.M. et al | 2014 | Congenital adrenal hyperplasia (CAH) with intermediate and high urogenital sinus | Contrast imaging studies | Urogenital sinus mobilization maneuver | None reported | 55 | Does not compromise voiding function or urinary continence. |
| 5 | Sircili, M.H.P. et al | 2016 | Congenital adrenal hyperplasia (CAH) with failed previous surgery | Cystoscopy | Y-V perineal flap with/without partial mobilization of urogenital sinus | One patient required a second reoperation | 20 | Eight adult patients were sexually active without experiencing dyspareunia. |
| 6 | Wang et al | 2021 | Persistent urogenital sinus (PUG) with uterus didelphys and double vagina | Transabdominal ultrasound, transrectal ultrasound, contrast-enhanced ultrasound | Urethral reconstruction, vaginal pull-through, artificial vaginoplasty, bilateral hysterosalpingectomy | None reported | 1 | Urination normal after six months; continuous vaginal dilation used to prevent stenosis. |
| 7 | Oktay Ulusoy et al | 2021 | High urogenital sinus | Clinical and imaging evaluation | Posterior prone approach for repair without rectal division | None reported | 7 | Electromyography and uroflowmetric tests showed normal function; pelvic EMG was also normal in all patients. |
| 8 | Ellerkamp, V et al | 2021 | Secondary vaginal stenosis after reconstructive surgery for urogenital sinus anomalies | Genitoscopy, genitography, MRI | Perineal flap with partial urogenital mobilization | None reported | 13 | Uneventful outcomes post-surgery. |
| 9 | Jessica Yang et al | 2023 | VACTERL syndrome, urinary tract infection, high urogenital sinus, bicornuate uterus | Ultrasound, voiding cystourethrogram (VCUG), MRI | Vaginoplasty, robotic urogenital sinus mobilization, posterior sagittal anorectoplasty | None reported | 1 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





