Submitted:
25 November 2024
Posted:
26 November 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
Background
2. Methods
2.1. Inclusion and Exclusion Criteria
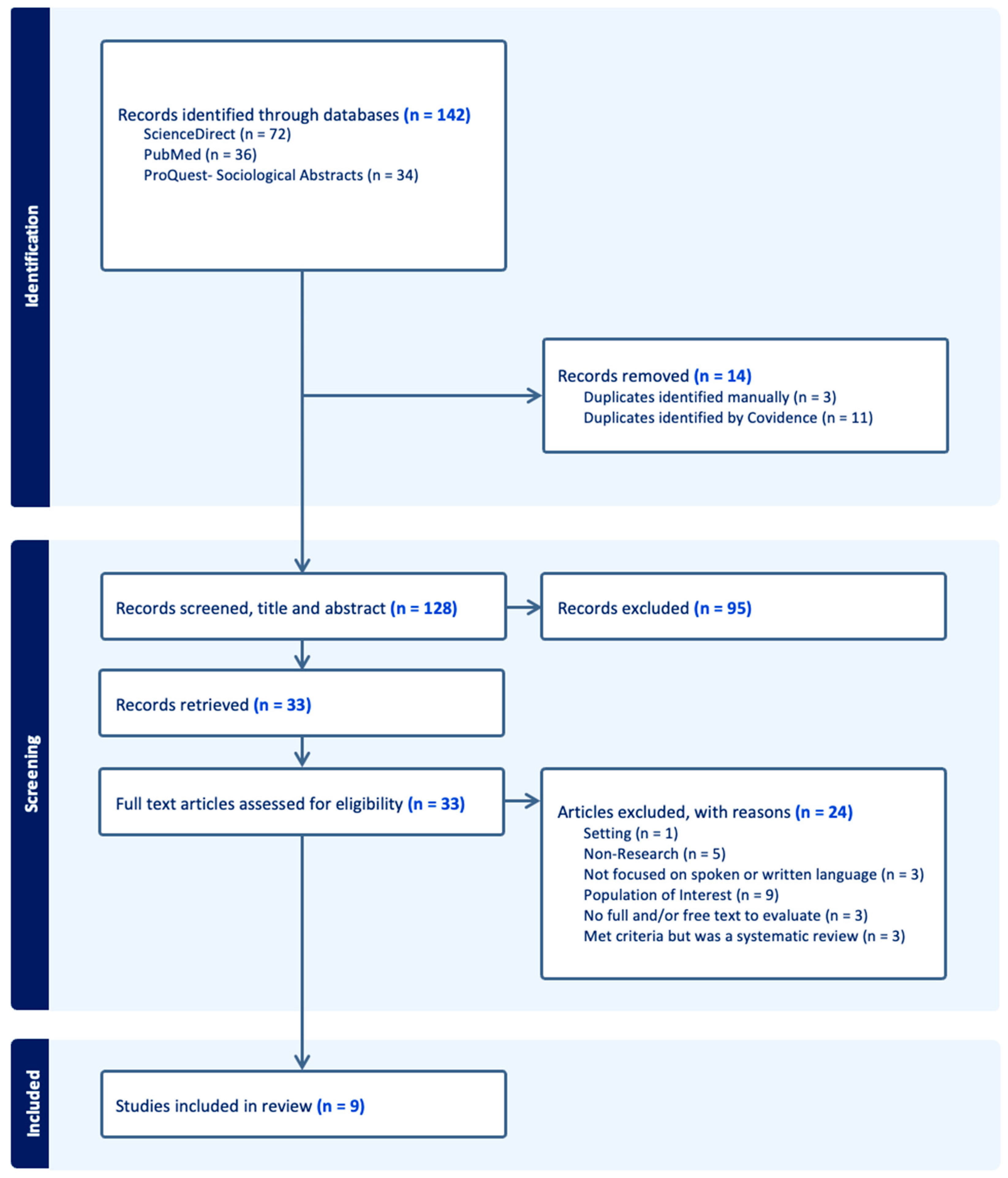
2.2. Literature Search Strategy
2.3. Screening, Extraction, and Review of Identified Literature
2.3.1. Data Screening
2.3.2. Data Extraction
2.3.3. Data Synthesis and Analysis
2.4. Ethical Considerations
3. Results
3.1. Recruitment and Data Collection of Included Studies
3.2. Study Participant Characteristics of Included Studies
3.3. Inclusion and Exclusion Criteria of Included Studies
| Table 2. Participant Characteristics and Inclusion/Exclusion Criteria of Included Studies | ||||
|---|---|---|---|---|
| Lead Author (Year) | Method of Recruitment of Participants | Population Characteristics | Inclusion criteria | Exclusion criteria |
| Zota et al. (2023) | About 64% of the sample was female. Most participants were employed in Greece (21.2%). The majority were physicians (45%), followed by nurses, other allied health professionals (i.e., psychologists, paramedics, health administration staff, nursing assistants, social workers, dentists/dental hygienists, dietitians/nutritionists, health promotion specialists, public health specialists) and students from health-related sectors. | Physicians, nurses, other allied health professionals (i.e., psychologists, paramedics, health administration staff, nursing assistants, social workers, dentists/dental hygienists, dietitians/nutritionists, health | Participants who did not specify health specialty/training or age | |
| Sun et. al (2022) | COVID-19 Data Mart | Almost one-third (29.7 percent) of the patients were White, 60.6 percent were Black, 6.2 percent were Hispanic or Latino, and 3.5 percent were categorized as other. The mean age was 47.4 years (SD23.0; data not shown) | All patients treated in an ED or inpatient setting between April 30, 2020 and October 1, 2020. | Patients with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes for dementia (n = 647), |
| Raney et al. (2021) | Not Specified | The target population is broad, including any provider, trainee, or staff member who works with patients in a clinical environment. | All health professionals caring for patients and documenting in the electronic medical record, including novice learners | Health professionals not documenting in electronic medical records |
| Park et al. (2021) | Random selection | Most patients were identified in the medical record as female (n = 350 [69%]). Most patients were identified as Black/African American (n = 406 [80%]), and 76 (15%) were identified as White | Patient medical records that had been written by physicians (attendings and residents) in 2017 at an ambulatory internal medicine setting at an urban academic medical center | Patient medical records not written in 2017 |
| Himmelstein et al. (2022) | Free-text admission notes of all patients admitted to a large academic medical center in 2018 | the 29,783 patients had a mean (SD) of 46.9 (27.7) years and 17 334 (58.2) were female, 840 (2.8%) were Hispanic patients, 1033 (3.5%) non-Hispanic Asian patients, 2498 (8.4%) were non-Hispanic Black patients, 18 956 (63.6%) were non-Hispanic White patients, and 1394 (4.7%) were another race (including American Indian or Alaskan Native and Hawaiian or Pacific Islander), and 2939 (9.9%) preferred a language other than English | All patients admitted to a large academic medical center in 2018 | Patients admitted to a non-academic medical center or patients not admitted in the year 2018 |
| DeMaria et al. (2023) | Email, Purposive Sampling, Snowball Sampling | Average Age- 25.8 ± 5.3; Race: White/Caucasian- 12 (54.5%); Black/African American - 7 (31.8%) Education: Some College or Undergraduate Degree - 13 (59.1%); Graduate Degree- 5 (22.7%) Employment: Student- 10 (45.5%); Full-Time- 11 (50.0%) |
- Women were eligible to participate in the study if they were 18–45 years of age and had ever sought reproductive healthcare at a community health center or program in Indiana - Non-physician healthcare professionals (i.e., NP, RN, CNM, doula, pharmacist, chiropractor) were eligibale if they were Iliving in Indiana who worked in a community healthcare setting |
Not working in a community healthcare setting |
| Deb Finn et al. (2021) | Purposive Sampling | Of the participants that completed the rating activity (n= 72), 41 participants identified as racialized health care users, 23 participants identified as non-racialized health care users, and 11 participants identified as either a ra- cialized or non-racialized health care provider. Of the 41 racialized health care users, 25 participants identified as female and 22 identified as Canadian-born | Recruited health care users were participants who had had a negative experience in Toronto or the GTA health care system within the past 5 years, age 16 years or older, and were able to write in English Recruited health care providers were front line providers (e.g. nurse, doctor, social worker, and pharmacist) who had at least 1 year of practice experience working in Toronto or the GTA |
Participant eligibility was group specific |
| Ashford et al. (2019) | Research Match- a national health volunteer registry. An email was sent to participants found in the registry | Participants had a mean age of 46.29 years (SD = 15.19), with the majority identifying as female (n = 225 / 75.3%), white (n = 271 / 90.6%), and either married or in a domestic partnership (n = 155 / 51.8%). Many participants had either a post-graduate degree (n = 135 / 45.2%) or a 4-year degree (n = 103 / 34.4%), were employed (n = 210 / 70.2%), and had a last year income over $50,000 (n = 200 / 66.9%). Less than a third of participants were in recovery (n = 87 / 29.1%) | Volunteers that elected to receive more information about the study | Random volunteers who did not respond |
| Goddu et al. (2018) | Of the 413 study participants (54% response rate), 42.8% were female, 43.5% were residents, and 14% were Hispanic/Latino. Most respondents were white (54.7%), 26.9% were Asian, and 10.4% identified as black or African American. | Residents in the medical center’s two internal medicine (IM) programs and one emergency medicine (EM) program | Non-residents | |
3.4. Measures and Outcomes of Studies
3.5. Key Conclusions of Included Studies
4. Discussion
4.1. Increased Training and Research on Inclusive Language
4.2. Racial Bias on Language Usage in US Healthcare Settings
5. Review Limitations
6. Public Health Implications and Recommendations
6. Conclusions
Author Contributions
Data Availability Statement
Acknowledgments
Conflicts of Interest
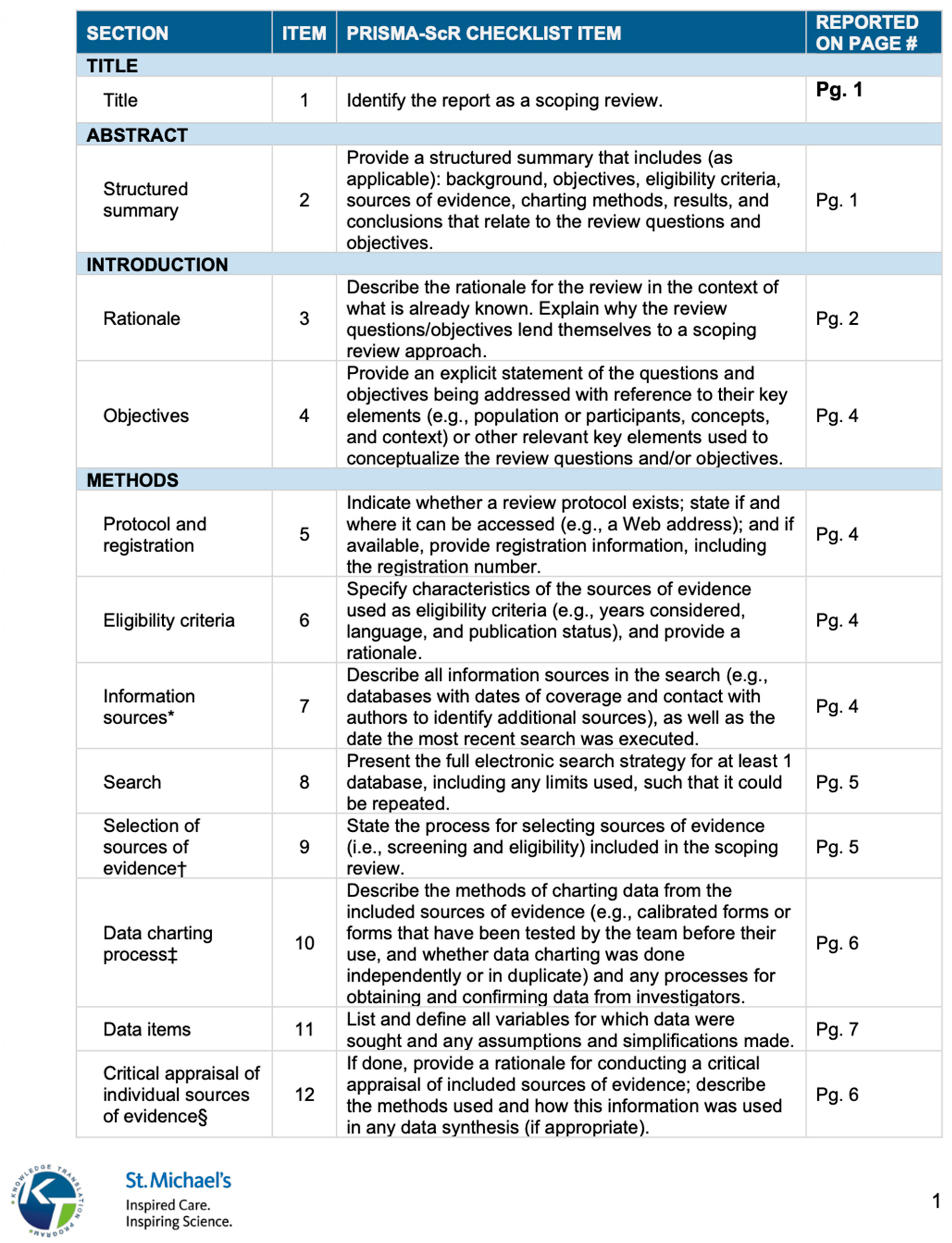
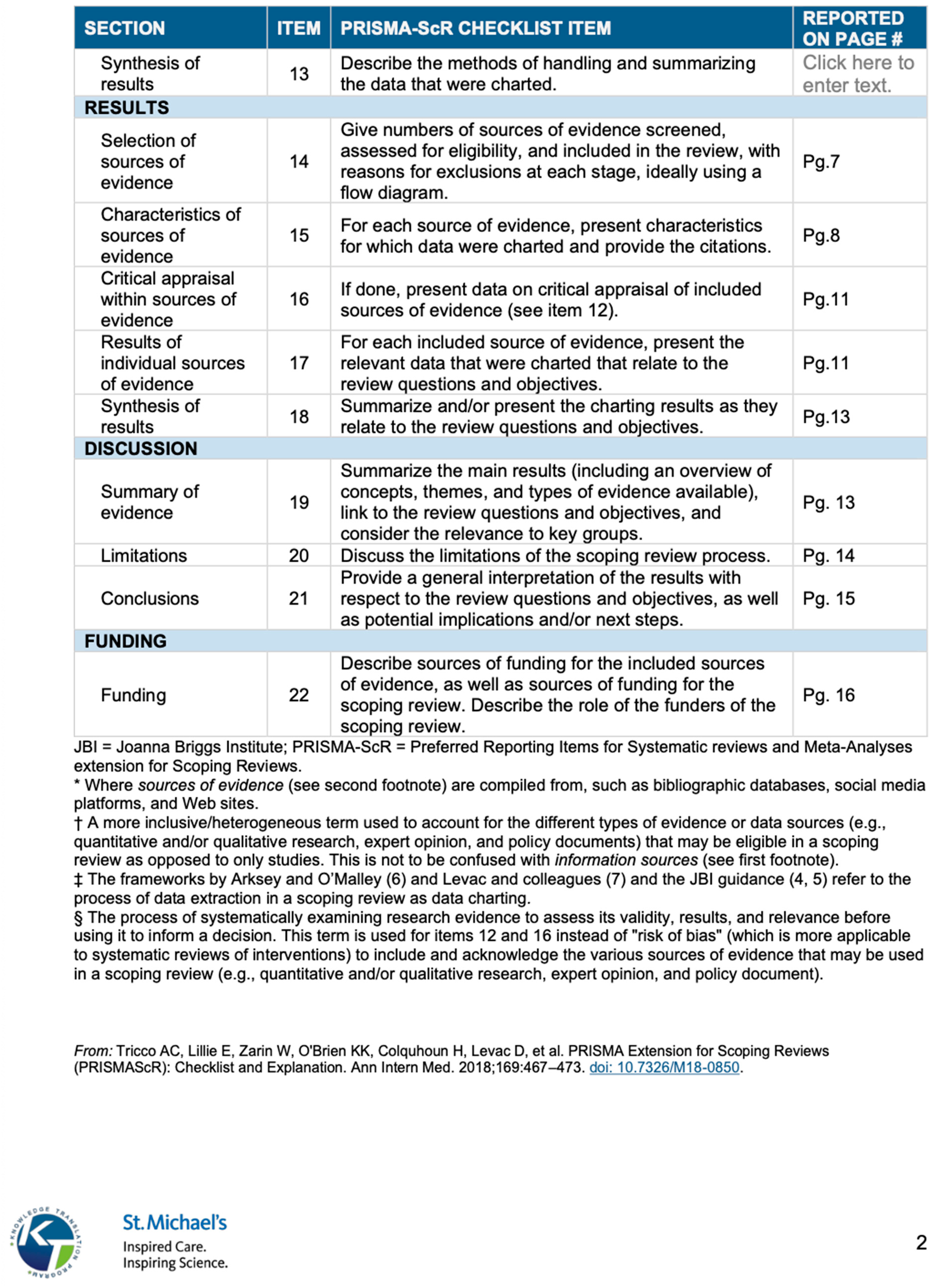
Appendix A. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist
Appendix B. Word Combinations used in Data Search.
| Appendix B. Data Search | |||
| Database: ScienceDirect | |||
| Keyterms: | Number of Original Return | Number of Filtered for Research Articles | Number of Articles Exported |
| Bias language AND Healthcare | 43,754 | 27,657 | 5 |
| Bias language AND Healthcare Workers | 10,830 | 6,732 | 0 |
| Bias language AND Infectious Diseases | 15,734 | 8,645 | 5 |
| Public Health AND bias language | 92,573 | 61,723 | 8 |
| Public Health AND Stigmatizing Language | 11,527 | 7,603 | 13 |
| Healthcare Workers AND Stigmatizing Language | 2,304 | 1,451 | 8 |
| Healthcare Workers AND Stigma | 7,607 | 4,750 | 12 |
| Healthcare AND Stigma AND Sexually Transmitted Diseases | 2,009 | 1,604 | 5 |
| Hospitals AND Stigma AND Sexually Transmitted Diseases | 3,435 | 1,816 | 11 |
| Database: PubMed | |||
| Keyterms: | Number of Original Returns | Number of Filtered for Research Articles | Number of Articles Exported |
| Bias language AND Healthcare | 1,693 | 1,351 | 3 |
| Bias language AND Healthcare Workers | 521 | 373 | 0 |
| Bias language AND Infectious Diseases | 350 | 310 | 0 |
| Public Health AND bias language | 7,150 | 5,494 | 2 |
| Public Health AND Stigmatizing Language | 407 | 253 | 12 |
| Healthcare Workers AND Stigmatizing Language | 126 | 63 | 8 |
| Healthcare Workers AND Stigma | 4,264 | 2,593 | 2 |
| Healthcare AND Stigma AND Sexually Transmitted Diseases | 2,773 | 2,412 | 7 |
| Hospitals AND Stigma AND Sexually Transmitted Diseases | 1,311 | 1,021 | 1 |
| Database: ProQuest Socioligcal Abstract | |||
| Keyterms: | Number of Original Return | Number of Filtered for Research Articles | Number of Articles Exported |
| Bias language AND Healthcare | 5,434 | 3,567 | 7 |
| Bias language AND Healthcare Workers | 3,463 | 3,216 | 1 |
| Bias language AND Infectious Diseases | 1,321 | 852 | 3 |
| Public Health AND bias language | 20,549 | 15,723 | 7 |
| Public Health AND Stigmatizing Language | 2,601 | 549 | 1 |
| Healthcare Workers AND Stigmatizing Language | 680 | 367 | 12 |
| Healthcare Workers AND Stigma | 3,382 | 2,270 | 0 |
| Healthcare AND Stigma AND Sexually Transmitted Diseases | 740 | 509 | 2 |
| Hospitals AND Stigma AND Sexually Transmitted Diseases | 779 | 523 | 0 |
| All Databases and Keyterms searched on December 26, 2023. Present day searches may vary | |||
| Database: CINAHL | |||
| Keyterms: | Number of Original Return | Number of Filtered for Research Articles | Number of Articles Exported |
| Bias language AND Healthcare | 37 | 34 | 3 |
| Bias language AND Healthcare Workers | 3 | 3 | 0 |
| Bias language AND Infectious Diseases | 0 | 0 | 0 |
| Public Health AND bias language | 4 | 4 | 0 |
| Public Health AND Stigmatizing Language | 9 | 9 | 1 |
| Healthcare Workers AND Stigmatizing Language | 3 | 3 | 0 |
| Healthcare Workers AND Stigma | 868 | 832 | 11 |
| Healthcare AND Stigma AND Sexually Transmitted Diseases | 149 | 142 | 0 |
| Hospitals AND Stigma AND Sexually Transmitted Diseases | 13 | 13 | 4 |
| All Databases and Keyterms searched on June 26, 2024. Present day searches may vary | |||
References
- Bible, New International Version. Proverbs 18:21. Biblica 2011.
- Ashford, R.D.; Brown, A.M.; McDaniel, J.; Curtis, B. Biased labels: An experimental study of language and stigma among individuals in recovery and health professionals. Subst Use Misuse 2019, 54(8), 1376–1384. [CrossRef]
- Marjadi, B.; Flavel, J.; Baker, K.; Glenister, K.; Morns, M.; Triantafyllou, M.; Gardiner, P.A. Twelve Tips for Inclusive Practice in Healthcare Settings. Int J Environ Res Public Health 2023, 20(5), 4657. [CrossRef]
- Gerchow, L.; Burka, L.R.; Miner, S.; Squires, A. Language barriers between nurses and patients: A scoping review. Patient Educ Couns 2021, 104(3), 534–553. [CrossRef]
- Hsueh, L.; Hirsh, A.T.; Maupomé, G.; Stewart, J.C. Patient-Provider Language Concordance and Health Outcomes: A Systematic Review, Evidence Map, and Research Agenda. Med Care Res Rev 2021, 78(1), 3-23. [CrossRef]
- Vella, E.; White, V. M.; Livingston, P. Does cultural competence training for health professionals impact culturally and linguistically diverse patient outcomes? A systematic review of the literature. Nurse Education Today 2022, 118, 105500. [CrossRef]
- Robling, K., Cosby, C., Parent, G., Gajjar, S., Chesher, T., Baxter, M., & Hartwell, M. (2023). Person-centered language and pediatric ADHD research: a cross-sectional examination of stigmatizing language within medical literature. Journal of osteopathic medicine, 123(4), 215–222. [CrossRef]
- Griffin, Z.; Long, P.; Peña, A.; Jacobsen, S.; Johnson, A. L.; Ottwell, R.; Torgerson, T.; Walters, C.; Ghebrehiwet, M.; Vassar, M.; Hartwell, M. Obesity, stigma, and person-centered language: A serial cross-sectional analysis of scientific literature.
- Harney, B.L.; Korchinski, M.; Young, P.; Scow, M.; Jack, K.; Linsley, P.; Bartlett, S.R. It is time for us all to embrace person-centred language for people in prison and people who were formerly in prison. Int J Drug Policy 2022, 99, 103455. [CrossRef]
- Goddu, A.P.; O'Conor, K.J.; Lanzkron, S.; Saheed, M.O.; Saha, S.; Peek, M.E.; Haywood, C., Jr; Beach, M.C. Do Words Matter? Stigmatizing Language and the Transmission of Bias in the Medical Record. J Gen Intern Med 2018, 33(5), 685–691. [CrossRef]
- Columbia University. Using Inclusive Language. Columbia University Department of Pediatrics 2022. Available online: https://www.pediatrics.columbia.edu/using-inclusive-language#:~:text=Inclusive%20language%20is%20a%20framework,person%20rather%20than%20their%20characteristics (accessed on 29 May 2024).
- Crocker, A. F., & Smith, S. N. (2019). Person-first language: are we practicing what we preach?. Journal of multidisciplinary healthcare, 12, 125–129. [CrossRef]
- Blum, A. (2022). Remove Race as an Initial Identifier From Clinical Presentations. American Family Physician, 106(2), 120–121.
- Håkansson Eklund, J.; Holmström, I. K.; Kumlin, T.; Kaminsky, E.; Skoglund, K.; Höglander, J.; ... Summer Meranius, M. "Same same or different?" A review of reviews of person-centered and patient-centered care. Patient Educ Couns 2019, 102(1), 3-11. [CrossRef]
- Murphy, K. (2013, February 15). HIV/AIDS movement has lost historic voice in NAPWA. NMAC. https://www.nmac.org/hivaids-movement-has-lost-historic-voice-in-napwa/#:~:text=NAPWA%20was%20founded%20in%201983,discussions%20that%20impacted%20their%20lives.
- U.S. Department of Health and Human Services. (2023, April 12). Writing respectfully: Person-first and identity-first language. National Institutes of Health. https://www.nih.gov/about-nih/what-we-do/science-health-public-trust/perspectives/writing-respectfully-person-first-identity-first-language.
- UNAIDS. (2023, June 26). The Denver principles: 40 Years on. UNAIDS. https://www.unaids.org/en/resources/presscentre/featurestories/2023/june/20230626_denver-principles-40-years-on.
- Kim, S.K.; Park, M. Effectiveness of person-centered care on people with dementia: a systematic review and meta-analysis. Clin Interv Aging 2017, 12, 381-397. [CrossRef]
- Lee, K. H.; Lee, J. Y.; Kim, B. Person-Centered Care in Persons Living With Dementia: A Systematic Review and Meta-analysis. The Gerontologist 2022, 62(4), e253–e264. [CrossRef]
- Wu, Q.; Qian, S.; Deng, C.; Yu, P. Understanding Interactions Between Caregivers and Care Recipients in Person-Centered Dementia Care: A Rapid Review. Clinical interventions in aging 2020, 15, 1637–1647. [CrossRef]
- Auckburally, S.; Davies, E.; Logue, J. The Use of Effective Language and Communication in the Management of Obesity: the Challenge for Healthcare Professionals. Curr Obes Rep 2021, 10(3), 274-281. [CrossRef]
- Ivezaj, V.; Lydecker, J. A.; Grilo, C. M. Language Matters: Patients' Preferred Terms for Discussing Obesity and Disordered Eating with Health Care Providers After Bariatric Surgery. Obesity (Silver Spring, Md.) 2020, 28(8), 1412–1418. https://doi.org/10.1002/oby.22868. Headley, S., Potter, I., Ottwell, R., Rogers, T., Vassar, M., & Hartwell, M. (2022). Adherence rates of person-centered language in amputation research: A cross-sectional analysis. Disabil Health J, 15(1), 101172. [CrossRef]
- Headley, S.; Potter, I.; Ottwell, R.; Rogers, T.; Vassar, M.; Hartwell, M. Adherence rates of person-centered language in amputation research: A cross-sectional analysis. Disabil Health J 2022, 15(1), 101172. [CrossRef]
- Stortenbeker, I. A.; Houwen, J.; Lucassen, P.; Stappers, H. W.; Assendelft, W. J. J.; van Dulmen, S.; ... Das, E. Quantifying positive communication: Doctor's language and patient anxiety in primary care consultations. Patient Educ Couns 2018, 101(9), 1577-1584. [CrossRef]
- Truong, M.; Lazarus, M.; Ochoa, G. G.; Brand, G. Resisting and unlearning dehumanising language in nursing and healthcare practice, education and research: A call to action. Nurse Educ Today 2022, 116, 105458. [CrossRef]
- Peters, Micah & Godfrey, Christina & Mcinerney, Patricia & Munn, Zachary & Trico, Andrea & Khalil, Hanan. (2020). Chapter 11: Scoping Reviews. 10.46658/JBIMES-20-12.
- Sutton, A., Clowes, M., Preston, L., & Booth, A. (2019). Meeting the review family: exploring review types and associated information retrieval requirements. Health information and libraries journal, 36(3), 202–222. [CrossRef]
- Khalil, H., Peters, M. D., Tricco, A. C., Pollock, D., Alexander, L., McInerney, P., Godfrey, C. M., & Munn, Z. (2021). Conducting high quality scoping reviews-challenges and solutions. Journal of clinical epidemiology, 130, 156–160. [CrossRef]
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane 2021. Available from train-ing.cochrane.org/handbook.
- Sarkis-Onofre, Rafael; Catalá-López, Ferrán; Aromataris, Edoardo; Lockwood, Craig. How to properly use the PRISMA Statement. Systematic Reviews 2021, 10. [CrossRef]
- Uman L. S. Systematic reviews and meta-analyses. Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal de l'Academie canadienne de psychiatrie de l'enfant et de l'adolescent 2011, 20(1), 57–59.
- Covidence. (2022). About Us. Retrieved from https://www.covidence.org/about-us-covidence/.
- PRISMA. (2022). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Retrieved from https://www.prisma-statement.org/.
- Park, J.; Saha, S.; Chee, B.; Taylor, J.; Beach, M. C. Physician Use of Stigmatizing Language in Patient Medical Records. JAMA Netw Open 2021, 4(7), e2117052. [CrossRef]
- Himmelstein, G.; Bates, D.; Zhou, L. Examination of Stigmatizing Language in the Electronic Health Record. JAMA Netw Open 2022, 5(1), e2144967. [CrossRef]
- Sun, M.; Oliwa, T.; Peek, M. E.; Tung, E. L. Negative Patient Descriptors: Documenting Racial Bias In The Electronic Health Record. Health Affairs 2022, 41(2), 203-208. [CrossRef]
- Zota, D.; Diamantis, D. V.; Katsas, K.; Karnaki, P.; Tsiampalis, T.; Sakowski, P.; Linos, A. Essential Skills for Health Communication, Barriers, Facilitators and the Need for Training: Perceptions of Healthcare Professionals from Seven European Countries. Healthcare 2023, 11(14), 2058. [CrossRef]
- Raney J, Pal R, Lee T, Saenz SR, Bhushan D, Leahy P, Johnson C, Kapphahn C, Gisondi MA, Hoang K. Words Matter: An Antibias Workshop for Health Care Professionals to Reduce Stigmatizing Language. MedEdPORTAL. 2021;17:11115. [CrossRef]
- Mahdi, D.A.; Fiedler, B.A. Culture, language, and health care professionals. In Three Facets of Public Health and Paths to Improvements; Academic Press 2020, pp. 213-237. [CrossRef]
| Lead Author (Year) | Title | Country in Which the Study Conducted | Study Design | Total Number of Participants | Health Condition |
|---|---|---|---|---|---|
| Zota et al. (2023) |
Essential Skills for Health Communication, Barriers, Facilitators and the Need for Training: Perceptions of Healthcare Professionals from Seven European Countries |
Europe: Cyprus, Germany, Greece, Poland, Spain | Cross Sectional Study | N = 702 Patients | N/A |
| Sun et. al (2022) |
Negative Patient Descriptors: Documenting Racial Bias In The Electronic Health Record |
United States | Cross Sectional Study | N = 18,459 Patients | N/A |
| Raney et al. (2021) | Words Matter: An Antibias Workshop for Health Care Professionals to Reduce Stigmatizing Language | United States | Qualitative Study | N = 66 Participants | N/A |
| Park et al. (2021) |
Physician Use of Stigmatizing Language in Patient Medical Records |
United States | Qualitative Study | N = 138 Clinicians (attendings and residents) | Not Specfied |
| Himmelstein et al. (2022) |
Examination of Stigmatizing Language in the Electronic Health Record |
United States | Cross Sectional Study | N1 = 29,783 Patients N2 = 1,932 Clinicians | Diabetes, Substance Use Disorder, and Chronic Pain |
| DeMaria et al. (2023) | The role of community healthcare professionals in discussing sexual assault experiences during obstetrics and gynecological healthcare appointments | United States | Qualitative Study | N = 22 Women | Sexual Trauma |
| Deb Finn et al. (2021) | Experiences of everyday racism in Toronto's health care system: a concept mapping study | Canada | Semi-Qualitative Study | Size varies based on activity | N/A |
| Ashford et al. (2019) | Biased labels: An experimental study of language and stigma among individuals in recovery and health professionals | United States | Randomised Controlled Trial | N = 299 Participants | Substace Use Disorder (SUD) |
| Goddu et al. (2018) |
Do Words Matter? Stigmatizing Language and the Transmission of Bias in the Medical Record |
United States | Randomized Vignette Study | N = 413 physicians-in-training | Sickle Cell Disease |
| Table 3. Measurements and Outcomes of Included Studies | |||||
|---|---|---|---|---|---|
| Lead Author (year) | Method of Outcome | Outcomes Measured | Primary Outcomes Reported | Secondary Outcomes Reported | Key Conclusions of Authors |
| Zota et al. (2023) | Online questionnaire, comprising 35 close-ended questions | Benefits, barriers and outcomes of effective health communication from the point of view of healthcare professionals | Physicians appear to be less concerned about communication skills, the barriers and facilitators of effective communication and perceived outcomes of successful communication | N/A | - Many healthcare professionals have yet to receive HCT, even though almost everyone identifies the beneficial effect of successful health communication on improved professional–patient relations, professional satisfaction and patient satisfaction, trust and medication adherence |
| Sun et. al (2022) | Natural language processing and machine learning | The occurrence of at least one negative descriptor in a patient’s history and physical note | In total, 8.2 percent of patients had one or more negative descriptors recorded in the history and physical notes in their EHR | Black patients had 2.54 times the odds of being described with one or more negative descriptors in the history and physical notes of their EHRs, even after we adjusted for their sociodemographic and health characteristic | This difference may indicate implicit racial bias not only among individual providers but also among the broader beliefs and attitudes maintained by the health care system |
| Raney et al. (2021) | Course Evaluation | Data familiarization, identifying themes, developing and applying a coding scheme, and organizing codes and themes. | Most believed the workshop met its objectives (4.8 out of 5.0) and strongly agreed that they would apply skills learned (4.8) | N/A | Workshop provided actionable skills for replacing biased language in clinical presentations and electronic health records |
| Park et al. (2021) | Encounter notes | Common linguistic characteristics reflecting an overall positive or negative attitude toward the patient | Five negative language categories: questioning credibility, disapproval, stereotyping, difficult patient, and unilateral decisions Six positive language categories: compliment, approval, self-disclosure, minimizing blame, personalize, and bilateral decision making |
N/A | This qualitative study found that physicians express negative and positive attitudes toward patients when documenting in the medical record Patients who have difficult interactions with a clinician may perceive that they are not receiving high-quality, patient-centered care, and may be at risk of distrusting or disengaging from care |
| Himmelstein et al. (2022) | Admission Notes | Stigmatizing language | Stigmatizing language appeared in 1197 of all 48 651 notes (2.5%); diabetes-specific stigmatizing language appeared in 599 notes for patients with diabetes (6.9%); language stigmatizing substance use appeared in 209 notes for patients with substance use disorder (3.4%); 37 notes for patients with chronic pain included stigmatizing language regarding pain (0.7%) | Across all medical conditions studied, stigmatizing language appeared more frequently in notes written about non-Hispanic Black patients | Although the stigmatizing language we assessed appeared infrequently, it has the potential to unnecessarily alienate patients and influence subsequent clinicians. Findings suggest that stigmatizing language appears in patients’ EHR admission notes, varies by medical condition, and is more often used to describe non-Hispanic Black than non-Hispanic White patients. Therefore, efforts to understand and minimize the use of stigmatizing language might improve patients’ care and their trust in their clinicians |
| DeMaria et al. (2023) | Semi-structured protocol focus groups and key-informant interviews | perspectives, novel experiences, and shared knowledge | There were three resulting themes: (1) healthcare professionals’ approaches to screening for a history of sexual assault varied depending on the providers’ work setting and their field; (2) healthcare experiences can compound traumatic experiences and create professional distrust with survivors; (3) sexual assault impacts patient healthcare experiences through the services they seek, how professionals interact with them, and type of professional they are willing to see. | N/A | One strength of this study was the inclusion of doulas. Doulas may gain additional patient context that a healthcare professional can use, with patient permission, to increase sensitivity to women’s needs in their birth experience Incorporating healthcare professionals’ and patients experiences and preferences for sexual assault-related discussions during routine obstetrical and gynecological care can assist in sexual assault prevention and treatment efforts, improve patient-professional rapport, and yield better health outcomes |
| Deb Finn et al. (2021) | Concept Mapping using Concept System® Global MAXTM software | Understanding complex the experiences of the target population | Racialized health care users reported that access to and quality of medical care are challenges cur- rently experienced in Toronto’s health care system | N/A | - Racialized health care users from Toronto (Canada’s largest city) and the Greater Toronto Area, reported ‘race’/ethnic based discrimination as largely contributory to the challenges experienced when receiving care. - Racialized health care users also prioritized unequal access to medical care for taking action/change |
| Ashford et al. (2019) | Scoring of the GNATs was done using the d-prime (d’) method. The method calculates sensitivity, indexed by d’, by converting the proportion of correct responses for signal items and incorrect responses for noise items into z-scores and then calculating the difference between the z-score value | Recovery status and employment types effects on views of SUD terminology | Descriptive statistics showed that while participants not in recovery had stronger associations than participants in recovery with most linguistic choices (addict + good M = 1.66; SUD + good M = 1.61, SUD + bad M = 2.10), that participants in recovery had stronger associations than participants not in recovery for addict + bad (M = 2.58). | health professional participants had stronger associations than non-health professional participants for all linguistic choices, with mean differences of .511 for substance abuse + good, .431 for substance abuse + bad, .248 for SUD + good, and .145 for SUD + bad. |
- The labels that are often used to identify and describe individuals with a SUD or in recovery can often be stigmatizing. - Terms such as “addict’ and “substance abuser” are also associated with greater levels of bias among individuals in recovery and health professionals. - Health professionals, having greater levels of negative association with stigmatizing terms, should commit to improving their linguistic choices in all manner of communication. |
| Goddu et al. (2018) | Qualtrics survey platform | Attitudes towards the hypothetical patient and pain management decisions (residents only | Exposure to the stigmatizing language note was associated with more negative attitudes towards the patient (20.6 stigmatizing vs. 25.6 neutral, p < 0.001) | reading the stigmatizing language note was associated with less aggressive management of the patient’s pain (5.56 stigmatizing vs. 6.22 neutral, p = 0.003) |
Stigmatizing language used in medical records to describe patients can influence subsequent physicians-in-training in terms of their attitudes towards the patient and their medication prescribing behavior |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





