1. Introduction
Advances in neuroscience and technology have significantly contributed to the development of non-invasive neuromodulation (NM) techniques, which aim to modulate neural activity without invasive procedures [
2]. Non-invasive NM provides an alternative, innovative approach for treating various neuropsychiatric conditions, such as depression, anxiety, ADHD, autism, and cognitive deficits, as well as neurological disorders, chronic pain, and sleep disturbances [
3,
4].
The NM has emerged as a prominent technique, with growing research interest owing to its diverse therapeutic applications. Although neuromodulation may appear to be a relatively new intervention—considering that 52.17% of practitioners in this study reported using it for approximately five years—its study dates back to the mid-1990s and early 2000s. Neuromodulation generally uses electrical, photonic, or another physic stimulation to manage a range of conditions, including neurocognitive disorders and chronic pain [
12,
13]. Neuromodulation techniques can be classified as either invasive or non-invasive. Invasive techniques are more commonly utilized by neurosurgeons, while non-invasive NM is a widely accepted and versatile approach to the surgical option. Non-invasive NM includes methods such as transcranial direct current stimulation (tDCS), transcranial photobiomodulation (tPBM), and transcranial magnetic stimulation (TMS), among others [
14]. Thus, non-invasive NM encompasses a range of techniques that manipulate neural activity through external stimuli. The selection of a specific method depends on the clinical objectives, patient population, and acceptance by both practitioner and patient [
4].
The NM techniques hold promise in enhancing cognitive, behavioral, social, and emotional processes, which are often compromised in neurological and neuropsychological conditions. Evidence suggests that NM supports rehabilitation by modulating neuroplasticity in the brain, thereby promoting recovery and improvement [
4,
5]. Studies indicate that NM can regulate brain activity by influencing neuronal connectivity and plasticity, leading to potential enhancements in social, emotional, and motor functioning [
5,
6].
One of the notable benefits of non-invasive NM is its safety profile, with minimal adverse effects such as mild headaches, tingling, or itching sensations during application, and occasional dizziness or skin irritation [
3]. However, a systematic review with meta-analysis identified substantial variability among studies, highlighting a lack of standardized NM protocols for patient management [
7].
Despite the eminent growth on NM research, the technique faces certain challenges, primarily related to patient safety and the individual variability responses to NM [
2]. Addressing these challenges requires optimization of procedural parameters and thorough practitioner training. Nonetheless, the literature reveals a gap in guidance on practitioner training, as limited resources are available on standardized protocols, practitioner experience, and training adequacy. A comprehensive evaluation of practitioners' experiences, therapy outcome perceptions, and adherence to standardized protocols is critical for enhancing NM efficacy and safety.
The present study aimed to assess the training levels and experiences of healthcare practitioners using NM, examining their perceptions of patient condition severity, observed clinical improvements, and the effectiveness of NM relative to pre-established therapeutic goals. Additionally, this study seeks to identify which health conditions derive the most benefit from NM interventions and to evaluate the competency of NM practitioners.
2. Materials and Methods
2.1. Participants
This observational study aimed to assess the clinical experiences of practitioners from various fields—including physiotherapy, speech therapy, psychology, occupational therapy, pedagogy, and psychopedagogy—who integrate non-invasive neuromodulation (NM) into their therapeutic interventions. The study focused on evaluating the severity of patients’ conditions, the effectiveness of NM treatments, and the overall improvements observed in patients. Recruitment was conducted online through established NM social media groups, targeting practitioners with at least a higher education degree and NM-specific training. Those with fewer than three months of NM experience were excluded. All participants provided informed consent through an online form, and each received a copy of the consent and a protocol of NM best practices by email. This study was approved by the Ethics Committee of the Federal University of Juiz de Fora (CAAE: 76799523.8.0000.5147), in adherence to Resolution 466/12 of the National Ethics Committee. The sample size was determined using G-Power software (version 3.1.9.7), with a two-tailed chi-square test, a variance ratio of 1.85, an alpha level of 5%, and a power of 95%. The minimum sample size was calculated as 70 participants; however, to account for an anticipated 30% sample loss, the target was set at 91 participants.
2.2. Procedures
To establish a baseline, participants initially completed a questionnaire designed to capture their professional profiles, training backgrounds, and NM knowledge (Appendix 1). Following this, an adapted questionnaire based on the Clinical Global Impression (CGI) scale was administered (Appendix 2). The CGI is a widely validated tool that provides a comprehensive overview of patient condition before and after intervention, initially developed for schizophrenia assessment but now broadly applied across various health conditions study, the CGI assessed practitioners’ perceptions of NM outcomes, including changes in motor deficits, psychological symptoms (e.g., depression, anxiety, ADHD), and other related issues. Due to its non-specific nature, the CGI enables a reliable and ecologically valid assessment of treatment progression.
The CGI scale includes three main dimensions:
Clinical Global Impression of Severity (CGI-S): Evaluates the current severity of the patient’s illness.
Clinical Global Impression of Improvement (CGI-I): Measures the degree of improvement since treatment began.
Clinical Global Impression of Efficacy (CGI-E): Assesses the overall effectiveness of the treatment in terms of symptom improvement.
Likert-type multiple-choice questions were used to allow participants to choose responses that best aligned with their perspectives.
2.3. Statistical Analysis
Data were analyzed using descriptive statistics, including measures of central tendency and dispersion. The Shapiro-Wilk test assessed data normality, while the Levene’s test evaluated homogeneity. Results were presented in graphs and tables. Chi-square tests (χ²) were applied to assess associations between variables, and Cramér's V was used to measure effect sizes (ES). The ES was qualitatively categorized based on degrees of freedom (df) as: df = 2: negligible (0 < 0.07); small (0.07 < 0.21); medium (0.21 < 0.35); large (0.35 or more); df = 4: negligible (0 < 0.05); small (0.05<0.15); medium (0.15 < 0.25); large (0.25 or more). All statistical analysis was conducted using
Jamovi software (the
Jamovi project [2022], v. 2.3, retrieved from:
https://www.jamovi.org, accessed on 1 July 2022), with a set significance at p<0.05.
3. Results
A total of 117 NM practitioners participated in the survey, and the findings are summarized below.
3.1. Demographic Overview
The sample consisted predominantly of female practitioners (86.96%), with males comprising 13.04%. Regarding age distribution, 2.6% were aged 20-24 years, 9.6% were 25-34 years, 40.86% were 35-44 years, 33.04% were 45-54 years, and 13.9% were over 55 years. Most participants (88.69%) held a completed specialization; among these, 91.3% reported at least one specialization, while 8.69% had none (table 1).
3.2. Professional Backgrounds and NM Usage
The majority of NM users were psychologists (51.3%), followed by psychopedagogists (12.17%) and physiotherapists/occupational therapists (9.6%). Other fields with smaller representations included nutrition, gerontology, language therapy, administration, physical education, pharmacy, music therapy, and human resources. Among participants, 52.17% reported using NM for 1 to 5 years (table 1).
Table 1.
Participants’ characteristics.
Table 1.
Participants’ characteristics.
| Gender |
Female |
86.96% |
| Male |
13.04% |
| Age |
20-24 |
2.6% |
| 25-34 |
9.6% |
| 35-44 |
40.86% |
| 45-54 |
33.04% |
| 55+ |
13.9% |
| Level of Education |
Complete specialization |
88.69% |
| Incomplete specialization |
7.83% |
| Complete higher education |
3.48% |
| Degree |
Phsycology |
51.3% |
| Psychopedagogy |
12.17% |
| Physiotherapy |
9.6% |
| Speech Therapy |
9.6% |
| Neuropsychopedagogy |
3.48% |
| Occupational Therapy |
1.74% |
| Medicine |
1.74% |
| Nursing |
1.74% |
| Pedagogy |
1.74% |
| Others |
6.96% |
| Specialization |
Yes |
91.3% |
| No |
8.69% |
| Work experience with NM |
Less than 1 year |
41.74% |
| 3 months - 1 year |
2.61% |
| 1-5 years |
52.17% |
| 6-10 years |
3.48% |
| 10 years or more |
0% |
| Workplace |
Hospital |
0% |
| Ambulatory |
93.92% |
| Health Center |
1.76% |
| Home care |
2.58% |
| Specialized service |
0.87% |
| Research |
0.87% |
| Frequency of NM use |
1 to 2 times a week |
40% |
| 3 to 4 times a week |
29.56% |
| 5 to 7 times a week |
30.43% |
3.3. Training Characteristics
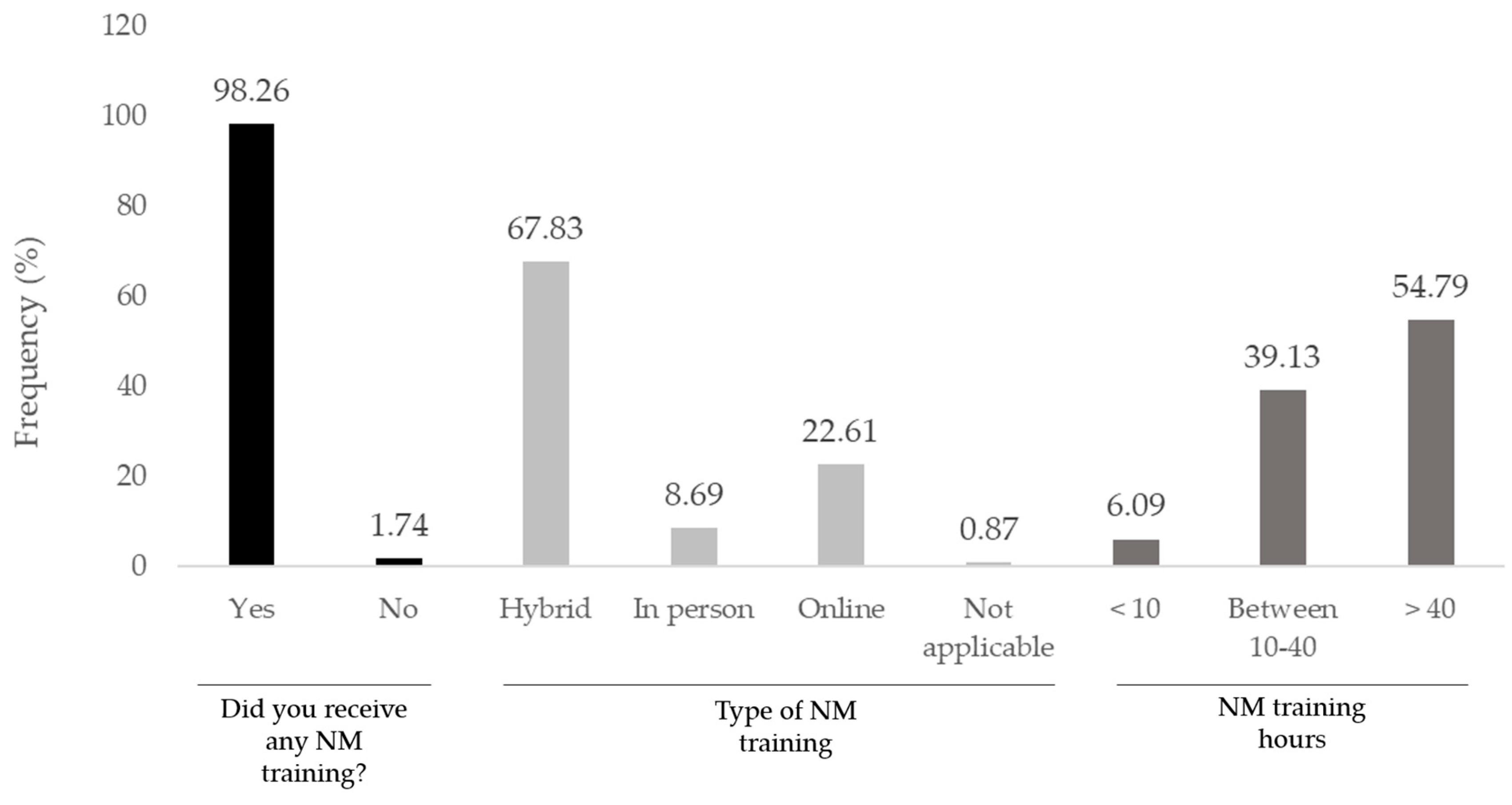
Hybrid training (a combination of online and in-person formats) was the most common (67.83%), followed by online-only (22.61%) and in-person-only (8.69%) training (figure 1). The NM training hours was more than 40 h for 54.79%, followed by 10-40 hours (39.13%), and less than 10 h (6.09%). The majority of practitioners considered their training as sufficient (45.22%) or very sufficient (5.22%), while 22.61% and 23.48% remained neutral or considered the received training as insufficient, respectively. Only 3.48% considered their NM training as very insufficient. Also, the majority of the respondents (85.22%) have recently attended to courses and/or workshops to update their NM training.
Figure 1.
Training characteristics.
Figure 1.
Training characteristics.
3.3. Application and Frequency
The data indicate that most practitioners employ a combination of NM methods, typically administering treatment 1 to 2 times per week (40%). The primary focus of NM treatments was neuropsychiatric disorders, with 76.41% of practitioners reporting such applications. Regarding patient demographics, NM was most frequently applied to adults and elderly patients (39.13%), while 11.3% of practitioners reported treating only children, and 49.56% treated both adults and children. Motor, neuropsychiatric, and speech dysfunctions were the most treated conditions, alone or combined (table 2).
Table 2.
Treated conditions.
Table 2.
Treated conditions.
| Condition |
Frequency |
| Motor Dysfunction |
2.61% |
| Neurological Dysfuncion |
76.41% |
| Sensory Dysfunction |
0.87% |
| Motor, Neurological, and Sensory Dysfunction |
12.18% |
| Motor and Neurological Dysfunction |
1.74% |
| Neurological and Sensory Dysfunction |
3.48% |
| Tinnitus |
0.87% |
| Cognitive performance |
0.87% |
| Addiction |
0.87% |
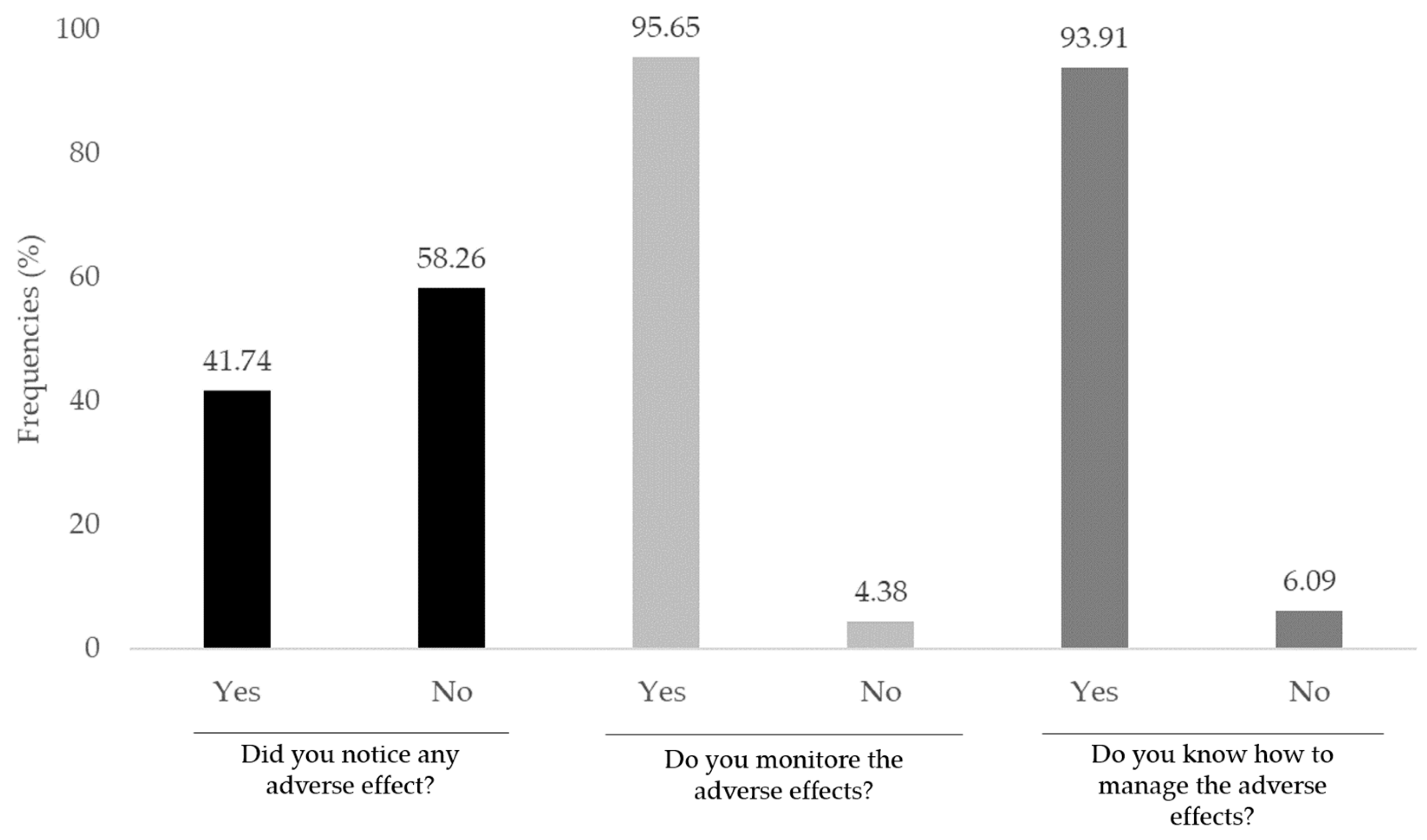
3.4. Adverse Effects
Figure 2 illustrates the participants' responses regarding their experience with adverse effects related to neuromodulation interventions. The chart is divided into three main questions: “Did you notice any adverse effect?" – Here, 41.74% of respondents reported noticing adverse effects, while 58.26% indicated they did not experience any; "Do you monitor the adverse effects?" – A significant majority, 95.65%, reported actively monitoring adverse effects, with only 4.38% indicating they do not; “Do you know how to manage the adverse effects?" – The data shows that 93.91% of respondents felt confident in managing adverse effects, whereas 6.09% reported a lack of knowledge on managing these effects. This data highlights the awareness and preparedness of practitioners regarding adverse effects in neuromodulation applications. The high percentages for monitoring and knowledge on managing adverse effects suggest a strong emphasis on safety and competency in handling potential complications. However, the occurrence of adverse effects (41.74%) underscores the importance of continuing education and adherence to safety protocols.
3.5. Type of NM Techniques
The vast majority of the practitioners combined some techniques to manage their patients with NM (table 3). The neurofeedback with tDCS were the most prevalent techniques combined for neuromodulation purposes (28.7%), while neurofeedback alone was the most frequent single cited technique (22.61%), followed by the tDCS (10.43%).
Table 3.
Range of NM techniques.
Table 3.
Range of NM techniques.
| Technique |
Frequency |
| TMS, tDCS, tPBM, taVNS |
0.87% |
| tDCS, tPBM ,taVNS, NFB |
13.04% |
| tDCS, tPBM, NFB |
0.87% |
| tDCS, taVNS, NFB |
12.17% |
| TMS and tDCS |
0.87% |
| tDCS and tPBM |
0.87% |
| tDCS and taVNS |
4.35% |
| tDCS and NFB |
28.7% |
| tPBM and taVNS |
0.87% |
| taVNS and NFB |
0.87% |
| tDCS |
10.43% |
| tPBM |
0.87% |
| taVNS and NFB |
1.74% |
| NFB |
22.61% |
3.6. Efficacy Perception and CGI Findings:
Nearly all respondents (99.13%) perceived NM as effective in their clinical practice. According to the CGI scale results, 62.61% of practitioners primarily treated patients with moderate-severity conditions. Overall, practitioners reported significant symptom improvements and expressed satisfaction with NM outcomes, as shown in
Table 4.
3.7. Associations Results
The association tests yielded some interesting results. The association between overall perceptions of the efficacy of NM on treating different conditions and different domains of the Clinical Global Impressions scale was tested. Large significant ES were observed considering the NM technique with general perceptions of the improvements in patients' disabilities (χ² = 58.2; p = 0.001; ES = 0.499), the overall quality of life after treatment (χ² = 63.1; p = 0.001; ES = 0.519), the achievement of treatment goals (χ² = 18.3; p = 0.001; ES = 0.395), and the patient or caregiver satisfaction (χ² = 48.03; p = 0.001; ES = 0.454).
All the above-mentioned findings highlight the demographic composition, training backgrounds, and clinical experiences of NM practitioners, underscoring the perceived effectiveness of NM across various conditions and patient populations.
4. Discussion
In the present study, isolated analysis showed that tDCS was the second most used technique among practitioners, following neurofeedback. Both tDCS and neurofeedback are employed to modulate brain activity, aiming to improve cognitive function and treat neuropsychiatric disorders [
15]. However, the neurofeedback demands the patient’s focus in order to achieve the proposed goal. On the other hand, the tDCS is a passive-like intervention, using the low-intensity electric current to achieve the neural results. Notably, neuropsychiatric disorders were the most commonly treated conditions (76.41%), including autism spectrum disorder (ASD), ADHD, anxiety, and depression [
16]. Non-invasive NM offers targeted modulation of specific brain regions, as the probe positioning (laser, LED, electrodes, etc.) is essential to apply the NM techniques. The NM also present fewer systemic side effects and a lower risk of dependence compared to pharmacological interventions. Additionally, NM can produce sustained benefits even after the cessation of treatment [
17,
19].
Other conditions than neuropsychiatric treated by practitioners in this study included motor dysfunctions, speech impairments, cognitive deficits, tinnitus, and cases of substance or alcohol dependence. In particular, the study by Lefebvre-Demers et al. (2021) demonstrated the effectiveness of repetitive TMS (rTMS) in alleviating tinnitus symptoms by modulating activity in the auditory cortex and insula, areas involved in auditory processing. Additionally, the study reported reductions in anxiety and depression levels among patients following rTMS treatment for tinnitus [
19]. This finding supports the perceptions of practitioners in our study, who also selected rTMS as a preferred treatment for tinnitus management. Regarding motor impairments, non-invasive neuromodulation has shown significant promise in reorganizing neural activities associated with motor functions [
1]. The most frequently cited techniques are those used in treating sequelae or symptoms resulting from Stroke, Parkinson's disease, and spinal cord injuries [
25]. In the present study, a small proportion of professionals (2.61%) focus exclusively on managing motor impairments. Nevertheless, the literature demonstrates favorable outcomes related to the use of tDCS, tACS, TMS, and NF in addressing these deficits. These approaches have been shown to enhance neural plasticity, intensify rehabilitation efforts, and even reduce muscle stiffness, thereby facilitating the recovery of movement and improving communication between brain areas involved in motor control [
25].
Similarly, Yamaguchi and Tazaki’s (2016) study on the use of neurofeedback for treating alcohol dependence indicated beneficial effects on neural plasticity, with changes observed in electroencephalographic patterns after a single session, suggesting that prolonged interventions may not be necessary to achieve lasting effects [
21]. Notably, no participants in their study reported any adverse effects, underscoring the safety profile of neurofeedback [
22]. Evidence indicates that tDCS is effective in treating addiction to alcohol and other substances. According to a 2017 guideline, bi-hemispheric stimulation of the dorsolateral prefrontal cortex, with the anode positioned on the right (F4) and the cathode on the left (F3), has demonstrated probable efficacy (Level B evidence) in reducing cravings and impulsivity among individuals with substance dependence [
18] This effect is attributed to the stimulation of the dorsolateral prefrontal cortex, which is linked to the modulation of impulsivity and inhibitory control, resulting in functional changes in the ventromedial prefrontal cortex that contribute to improved abstinence from substances such as alcohol and cocaine [
18]. Moreover, repeated sessions (2 mA, 20 minutes per session, for 5 consecutive days) have shown promise as a non-invasive approach to mitigating impulsivity, leading to a linear reduction in cravings and enhancements in cognitive processing among users of crack and cocaine, without the adverse side effects associated with conventional pharmacological treatments [
18].
Regarding NM usage frequency among practitioners, the results were evenly distributed. Approximately 40% of practitioners reported using NM one to two times per week, 30% used it three to four times per week, and the remainder applied it five to seven times per week. This variation likely reflects NM's adaptability and personalized nature; treatment protocols are tailored based on individual assessments, goals, and therapeutic needs [
22]. Like any intervention, non-invasive NM may have associated risks. Reported adverse effects in the literature are minimal, typically including mild headache, tingling, itching, dizziness, and, rarely, skin irritation [
4]. Consistent with the literature, practitioners in our study reported itching or tingling (33.91%) and headache (14.78%) as the most common adverse effects, with fewer cases of numbness, drowsiness, agitation, skin redness, and anxiety or manic episodes. Given NM's direct stimulation of nerve cells, these mild adverse effects may be expected [
23].
Practitioner perceptions of NM efficacy often align with their years of experience; studies indicate that satisfaction and acceptance of NM techniques tend to increase with experience and specialized training [
24,
26]. The present study, however, did not show significant association between perception of efficacy and experience time (p = 0.827; ES = 0.08). Our findings revealed strong, significant associations between perceived NM efficacy and various outcomes, including improvements in the severity of the treated condition, the patient’s overall quality of life, goal attainment, and patient or family satisfaction with the treatment. These associations are consistent with existing literature, reinforcing NM's clinical value.
The efficacy of NM in alleviating symptoms and reducing the severity of specific conditions, particularly depression, chronic pain, and epilepsy, underscores its viability as a therapeutic option [
24]. Additionally, an essential outcome highlighted in this study is the improvement in quality of life for patients receiving NM. Historically, therapeutic focus has often been limited to symptom management, neglecting the broader biopsychosocial impacts on patients’ daily lives. However, quality of life is a critical outcome that can influence treatment adherence and long-term functionality, demonstrating NM's potential to foster holistic well-being [
27].
Some limitations must be addressed. This was an exploratory study focused on identifying practitioners' perceptions regarding the practice of non-invasive neuromodulation. Despite disseminating the surveys through various electronic channels, the majority of responses came from practitioners’ who were part of social media groups, which may have limited the reach to a broader audience, thereby restricting the generalizability of the findings. Additionally, we did not identify the specific regions of Brazil where these professionals were practicing, which also limits certain interpretations. Further studies are needed to provide a robust foundation for new discussions on the topic. Nevertheless, the present study demonstrated that Brazilian practitioners are engaged and possess adequate training to work with non-invasive neuromodulation. However, such inferences should be cautioned by the present limitations.
Author Contributions
Conceptualization, O.C.,L. and C.B.,A; methodology, O.C.,L.; formal analysis, O.C.,L.; investigation, O.C.,L.; resources, O.C.,L. and C.B.,A; data curation, O.C.,L. and C.B.A; writing—original draft preparation, O.C.L.; writing—review and editing, C.B.A., A.B.M. and L.G.G; visualization, A.B.M. and L.G.G; supervision, C.B.A.; project administration, O.C.L. and C.B.A; All authors have read and agreed to the published version of the manuscript.
Appendix 1
This is a questionnaire to capture the professional profiles, training backgrounds, and NM knowledge:
- 1.
What is your age range?
( ) 20 - 24 years ( ) 25 - 34 years ( ) 35 - 44 years ( ) 45 - 54 years ( ) 55 years or older
- 2.
How do you identify yourself?
( ) Female ( ) Male ( ) Other ( ) Prefer not to answer
- 3.
What is your highest level of education?
( ) Completed higher education ( ) Incomplete postgraduate studies ( ) Completed postgraduate studies
- 4.
What is your professional background?
( ) Physiotherapy ( ) Psychology ( ) Speech Therapy ( ) Occupational Therapy ( ) Medicine ( ) Nursing ( ) Psychopedagogy ( ) Other
- 5.
Do you hold any specialization?
( ) Yes ( ) No
- 6.
How long have you been working with neuromodulation?
( ) Less than 3 months ( ) 3 months - 1 year ( ) 1-5 years ( ) 6-10 years ( ) 10 years or more
- 7.
What is the primary demographic profile of your patients?
( ) Children ( ) Adults/Seniors ( ) Both ( ) Other
- 8.
What are the main conditions you treat using non-invasive neuromodulation (NMNI)?
( ) Motor dysfunctions ( ) Psychological conditions (e.g., anxiety, depression, ADHD) ( ) Speech disorders ( ) Behavioral changes ( ) Autism Spectrum Disorder (ASD) ( ) Other
- 9.
What is your current workplace setting?
( ) Hospital ( ) Outpatient Clinic ( ) Health Center ( ) Other: _________
- 10.
Which non-invasive brain stimulation techniques do you utilize in your clinical practice?
( ) TMS - Transcranial Magnetic Stimulation ( ) tDCS - Transcranial Direct Current Stimulation ( ) tPBM - Transcranial Photobiomodulation (Low Intensity Polarized Light Therapy) ( ) tVNS - Transcutaneous Vagus Nerve Stimulation ( ) Neurofeedback
- 11.
How frequently do you apply these techniques?
( ) 1 to 2 times per week ( ) 3 to 4 times per week ( ) 5 to 7 times per week
- 12.
Have you ever encountered any adverse effects after applying any non-invasive brain stimulation technique?
( ) Yes ( ) No
- 13.
If yes, what is the most common type of adverse effect you observe in your patients?
( ) Headache ( ) Dizziness ( ) Itching or tingling ( ) None ( ) Other
- 14.
Are you aware of the safety measures that should be followed when applying non-invasive brain stimulation techniques?
( ) Yes ( ) No
- 15.
Have you received specific training in non-invasive brain stimulation techniques?
( ) Yes ( ) No
- 16.
If yes, what was the format of your training?
( ) In-person ( ) Online ( ) Hybrid (online + in-person) ( ) Not applicable
- 17.
What was the duration of your training?
( ) Less than 10 hours ( ) Between 10 and 40 hours ( ) More than 40 hours
- 18.
How would you rate the sufficiency of the training workload you completed?
( ) Very insuficiente ( ) Insufficient ( ) Neutral ( ) Sufficient ( ) Very sufficient
- 18.
Have you ever participated in any course, workshop, or training program focused on non-invasive brain stimulation?
( ) Yes ( ) No
- 19.
Do you monitor adverse effects in your patients following the application of non-invasive brain stimulation techniques?
( ) Yes ( ) No
- 20.
Do you have a standard protocol in place for handling adverse events?
( ) Yes ( ) No
- 21.
Do you perceive non-invasive brain stimulation as effective for the treatment of your patients?
( ) Yes ( ) No
Appendix 2
Adapted questionnaire to assess healthcare Practioners' perceptions using the Clinical Global Impression (CGI) scale.
For each question, please select the option that best represents your perception regarding your patients' characteristics in response to treatment with non-invasive neuromodulation:
CGI-S (Severity)
1) How would you rate the severity of your patient's condition prior to the initiation of non-invasive neuromodulation treatment?
( ) Mild severity
( ) Moderate severity
( ) Very severe
( ) Extremely severe
CGI-I (Improvement)
2) If there has been an overall change in the severity of the condition after treatment with non-invasive neuromodulation, how would you describe this change?
( ) Much better
( ) Better
( ) Slightly better
( ) No change
( ) Minimally worse
( ) Worse
( ) Much worse
3) Regarding your patient's behavior after treatment with non-invasive neuromodulation, how would you rate the change?
( ) Much better
( ) Better
( ) Slightly better
( ) No change
( ) Minimally worse
( ) Worse
( ) Much worse
4) Concerning the skills in which your patient had deficits, how would you assess their improvement after non-invasive neuromodulation treatment?
( ) Much better
( ) Better
( ) Slightly better
( ) No change
( ) Minimally worse
( ) Worse
( ) Much worse
5) How would you rate the general quality of life of your patient after treatment with non-invasive neuromodulation?
( ) Much better
( ) Better
( ) Slightly better
( ) No change
( ) Slightly worse
( ) Worse
( ) Much worse
CGI-E (Effectiveness)
6) Regarding the adverse effects of non-invasive neuromodulation treatment, how would you classify them?
( ) None
( ) Very mild
( ) Mild
( ) Moderate
( ) Severe
7) How would you assess the overall effectiveness of non-invasive neuromodulation treatment for your patients?
( ) Very effective
( ) Effective
( ) Slightly effective
( ) No change
( ) Slightly ineffective
( ) Ineffective
( ) Very ineffective
8) Please select the option that best describes the improvement in your patient's overall functionality following non-invasive neuromodulation treatment:
( ) Much better
( ) Better
( ) Slightly better
( ) No change
( ) Worse
( ) Much worse
9) In relation to your treatment objectives, do you consider that non-invasive neuromodulation:
( ) Completely achieved the objectives
( ) Partially achieved the objectives
( ) No changes were observed
( ) Did not achieve the objectives
10) Regarding the satisfaction of your patient and/or their family members with the results of non-invasive neuromodulation treatment, would you say that they are:
( ) Very satisfied
( ) Satisfied
( ) Neutral
( ) Dissatisfied
( ) Very dissatisfied