I. Introduction
Gingival recession (GR) is the process where the marginal gingiva moves from its normal position on the tooth crown to a lower position on the root surface, beneath the cementoenamel junction (CEJ). The main causes of GR are inflammatory periodontal disease and mechanical trauma. Additional risk factors include a thin gingival biotype, inadequate attached gingiva, bone defects like dehiscence, tooth misalignment, and high frenum or muscle attachments. GR can occur in any demographic globally, but it is more common in older adults. Although the occurrence of GR increases with age, it is not caused by aging itself, thus it is age-associated, not age-related [
1].
Identifying the causative factors is essential before treating gingival recession defects. The causes are often not clear-cut, as gingival recession is typically the result of a combination of factors. The main causes include periodontal inflammation due to plaque and mechanical trauma from incorrect tooth brushing techniques. Clinicians must also take into account susceptibility factors and modifiable conditions associated with gingival recession. Important susceptibility factors are thin gingival biotype, limited or absent keratinized tissue, probing depths that exceed the mucogingival junction, and a history of progressive gingival recession or periodontal disease. Modifiable conditions include plaque accumulation, periodontal disease, misplaced frenum, detrimental oral hygiene practices, subgingival restorations, smoking, and systemic issues like diabetes [
2].
Miller's classification, present the most popular classification of gingival recession which focuses on the extension of the recession to a mucogingival junction (MCJ), interdental soft tissue loss and proximal bone loss. It categorizes gingival recession into four distinct levels to forecast root coverage outcomes, is a well-established system. Gingival recessions are categorized into four classes based on the prognosis for root coverage. In Miller Class I and II gingival recessions, there is no loss of interproximal periodontal attachment or bone, allowing for complete root coverage. In Miller Class III, the loss of interdental periodontal support is mild to moderate, making partial root coverage possible. However, in Miller Class IV, the interproximal periodontal attachment loss is so severe that root coverage is not achievable [
3].
Cairo et al. recently introduced a new classification system of gingival recessions using the level of interproximal clinical attachment as an identification criterion; they also explored the predictive value of the resulting classification system on final root coverage outcomes following surgery. Three recession types (RT) were identified: class RT1 included gingival recession with no loss of interproximal attachment; class RT2 comprised recession with loss of interproximal attachment less than or equal to the buccal site; and class RT3 showed interproximal attachment loss higher than the buccal site. this recession type class is a strong predictor of the final recession reduction after different surgical procedures [
4].
The management of gingival recession defects encompasses both non-surgical and surgical approaches. Non-surgical treatments may include optimal plaque control, the removal of overhanging subgingival restorations, behavioral modifications, and the application of desensitizing agents and fluoride as necessary. The maintenance strategy involves monitoring the patient for key periodontal parameters and documenting only significant negative changes in the periodontal maintenance record, in comparison to the most recent comprehensive data from the periodontal examination record [
5]
.
The surgical treatment of the gingival recession, have two objectives: first, coverage of exposed root surfaces with soft tissue. Second, creation of new keratinised and attached gingiva. Attempting soft tissue coverage of the exposed root surface is more technically and biologically demanding than increasing the amount of keratinised tissue (KT). The free gingival graft technique is most utilized technique to increase KT. This method is also recommended for extending the vestibule and removing the frenulum. It involves harvesting epithelial and connective tissues from a donor site and transplanting them to the recipient site, where achieving effective primary stability is crucial [
6].
The coronally advanced flap (CAF) is the preferred surgical technique for treating recession defects when there is adequate keratinized tissue present. The CAF method provides predictable results, such as complete root coverage, seamless color integration, and the reestablishment of the original soft tissue margin contour. To achieve both root coverage and regeneration of the functional attachment apparatus, researchers frequently combine CAF with other regenerative materials, including connective tissue grafts, which are considered the gold standard of treatment. [
7].
Care must be taken in choosing the best soft tissue grafting technique. Subepithelial connective tissue autograft is indicated for patients with aesthetic demands, inadequate KT, deep root abrasion, root prominence and root pigmentation. But it is contraindicated when GR is caused by a high muscle pull, a gingival cleft extending in alveolar mucosa and a shallow vestibule. The advantage of sub-epithelium connective tissue graft enhances the survival of the graft above the avascular surface of roots and improves the aesthetic results [
8,
9].
The rationale for the surgical technique begins with determining the maximum root coverage (MRC). This involves calculating the optimal height of the anatomical interdental papilla. For teeth affected by gingival recession, the ideal height is the apical-coronal dimension of the interdental papilla necessary for complete root coverage. For non-rotated and correctly aligned teeth, this height is measured on the tooth itself. For rotated or misaligned teeth, the measurement is taken from the corresponding contralateral tooth. The process of measuring the anatomical papilla height includes assessing the vertical distance between two teeth and the horizontal line from the cementoenamel junction (CEJ) of the tooth to the tip of the papilla. In a healthy periodontium with a non-rotated tooth, the papilla tip is aligned with the contact point, which helps in predicting the potential for root coverage. The optimal height is the distance from the mesial-distal line angle to the contact point of the tooth. This line angle is identified by elevating the interdental soft tissues to expose the interdental CEJ. After determining the ideal papilla height, it is marked apically from the mesial and distal tips of the papillae of the recessed tooth. Horizontal projections from these marks to the edge of the recession define two points, which are then connected by a scalloped line to establish the 'line of root coverage [
10].
The present study highlights the utilized method in predicting the position of the soft tissue margin before root coverage surgery to the actual root coverage following surgical procedure.
Case 1:
A 41-year-old male presented at the Department of Periodontics, Faculty of Oral & Dental Medicine, with complaints of gum recession and sensitivity in the left first Premolar in upper teeth. Clinical examination revealed a Miller Class II recession defect on the buccal side of tooth 24. Clinical attachment loss was recorded at 4 mm, and recession width at the cementoenamel junction measured 3 mm. A pocket depth of 1 mm was observed above the mucogingival junction, and the depth of keratinized tissue was 1 mm (as measured from 2 mm apical to gingival margin). The patient generally in good health with good oral hygiene with no systemic diseases, medications, allergies, or smoking history.
Outcome measures:
Primary outcome measures: included aesthetic change related to patient’s opinion, recession depth change clinically and absence of postsurgical complication.
Secondary outcome measures: include KTW change, mean root coverage (MRC) clinically.
Method:
A single-stage treatment approach was planned, all selected patients received a comprehensive periodontal examination and oral hygiene instructions, and they were subjected to full-mouth scaling and root planning. After 30 days, reevaluation was performed, which clinical improvement of clinical parameters (
Figure 1). A coronal advancement flap with connective tissue graft was planned and performed to treat the gingival recession to increase the amount of keratinized tissue.
The Presurgical preparation: was thoroughly explained to the patient, and informed consent was obtained. Patient preparation included scaling and root planning, along with oral hygiene instructions. The modified Stillman brushing technique was recommended for the patient.
Evaluated Parameters: The parameters were evaluated using the UNC-15 periodontal probe. Parameter dependent on CEJ. The following metrics were examined clinically at baseline and 1month post-surgery:
Pocket Depth (PD): The measurement from the gingival margin to the bottom of the gingival sulcus.
Clinical Attachment Level (CAL): Measured from the cementoenamel junction to the base of the periodontal pocket [
11].
Gingival recession Defect (GRD) was determined from the (CEJ) to the most apical point of the gingival edge on the mid-buccal face of the tooth (GM).
Digital measurements: all recession areas were photographed before surgery (baseline) and 1 month postsurgical.
The width of keratinized tissue (KT): was measured as the distance between the gingival margin (GM) and the mucogingival junction (MGJ). KT provides fibrotic collar strength and attachment around the tooth that increase the capacity of the periodontium to withstand the occlusal forces. When it becomes inadequate decreased, it impacts the tooth capacity, aesthetic appearance and plaque control maintenance. Hall identified that keratinized attached gingiva with less than 2 mm should be monitored for active recession [
12].
SURGICAL PROCEDURE:
The objective of periodontal plastic surgery is to regenerate and establish uniform, aesthetically appealing gingival margins.
Root planning and conditioning are vital preliminary steps prior to root coverage procedures.
Isolating the surgical area and anesthetizing the operative sites with 2% xylocaine hydrochloride containing adrenaline (1:200,000) is essential. Gracey curettes GR no. 1/2 and 3/4 are utilized to polish the exposed root surface to a glass-like finish, enhancing tissue adhesion.
Subsequently, 24% EDTA is applied to the root for 2 minutes to eliminate the smear layer, detoxify, decontaminate, and demineralize the surface, revealing the collagenous matrix of the dentin and cementum, which is crucial for optimal healing.
De-epithelialization is performed on the peripheral gingival tissues surrounding the recession (anatomical papillae).
A sulcular incision is made around the first premolar, with horizontal incisions which are positioned at a distance from the tip of the anatomical papillae equal to the depth of the recession plus 1 mm. This horizontal incision will extend only 3mm, never extend to adjacent tooth.
Vertical incisions at the ends of the horizontal incision reach into the alveolar mucosa, facilitating deep, superficial partial split dissection needed for graft integration and contraction. A periosteal elevator is employed to elevate a full thickness flap, just apical to recession area, which is then trimmed apically, and root biomodification by EDTA is carried out up to the mucogingival junction to ready an appropriate bed for the graft.
Technique for obtaining the graft from donor site:
The graft, about 2 mm thick, was taken from the area behind the anterior palatine rugae, in line with teeth numbers 14 to 16.
The same anesthetic used at the recipient site was also applied for a greater palatine nerve block.
connective tissue graft by L shape palatal incision technique was used.
Graft placement:
The graft was placed at the recipient site 1mm coronal to CEJ.
first secured with two interrupted 6-0 vicryl sutures at the mesial and distal ends. It was then fully stabilized using a criss-cross suture technique, supplemented by additional interrupted sutures for further reinforcement.
Gentle pressure was applied with saline-moistened gauze for five minutes to achieve hemostasis and promote fibrin clot formation.
The flap is subsequently repositioned as coronally as feasible. Figure [
12]
Post-operative care:
The patient was prescribed Amoxicillin 500 mg to be taken three times a day for 5 days. In addition, they were given Ibuprofen 400 mg three times daily.
The patient was advised to follow standard post-operative oral hygiene practices and to rinse with 0.12% chlorhexidine Di gluconate mouthwash for two weeks.
They were also cautioned against pulling on their lips to prevent disturbing the surgical site. Sutures were removed 14 days after surgery.
A follow-up was conducted over 1 months, with no post-operative complications noted, and healing was considered satisfactory. The patient reported no post-operative morbidity.
Healing after root coverage procedures: A truly new connective tissue attachment is preferable over a long junctional epithelium. The success of sub-epithelial Connective Tissue Grafts (SCTG) hinges on the connective tissue blood supply [
13].
The prognosis of surgical root coverage [
14]: primarily aims to achieve complete root coverage, which is recognized as the best indicator of success. However, the prognosis is influenced by various factors, including:
Patient-related factors such as poor oral hygiene, compromised health, systemic diseases, and smoking, all of which can negatively impact periodontal surgery.
Gingiva-related factors are critical; these include the cause of the recession, the class of recession defect, periodontal biotype, extent of recession, width of KT, tooth location, vestibular depth, interproximal attachment level, and the aesthetic and functional demands.
Technique related factors: This includes flap design, flap reflection, root surface treatment, type of graft, thickness of the graft and position of gingival margin coronal to CEJ.
Periodontist related factors: Experience and knowledge of surgeons are very important to make a proper treatment plan and determine the proper technique for each case as well as the skills to master the case during surgery.
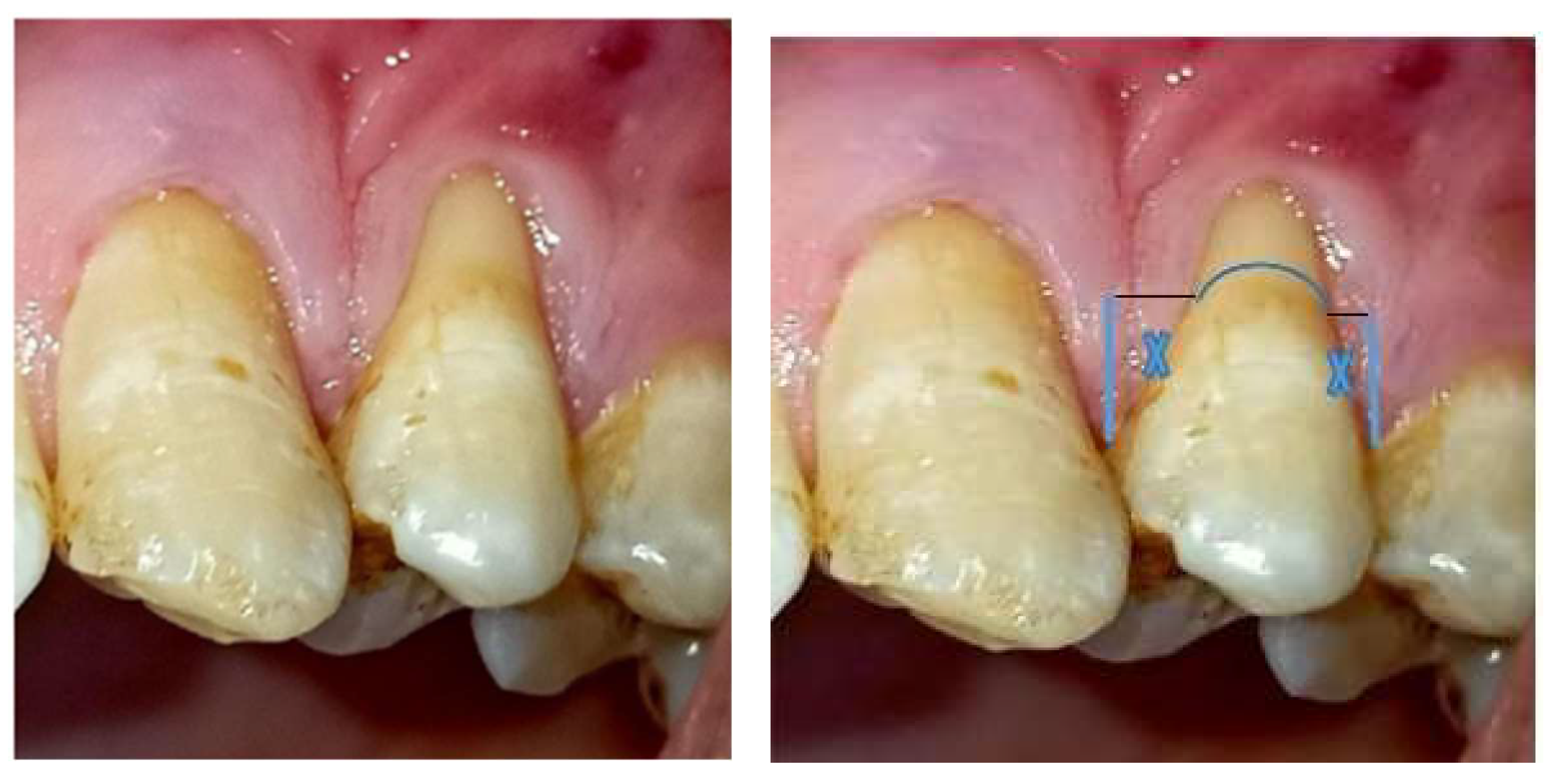
Figure 1.
clinical photograph showing 41years old male patient, has GR miller cl(IIa) at upper left first premolar. In a nonrotated tooth with no interproximal attachment loss and with intact papilla height. the ‘deal papilla height (X) coincides with the anatomical papilla height.
Figure 1.
clinical photograph showing 41years old male patient, has GR miller cl(IIa) at upper left first premolar. In a nonrotated tooth with no interproximal attachment loss and with intact papilla height. the ‘deal papilla height (X) coincides with the anatomical papilla height.
Figure 2.
incision of Coronal Advancement Flap (two horizontal and two vertical incisions, -trapezoid).
Figure 2.
incision of Coronal Advancement Flap (two horizontal and two vertical incisions, -trapezoid).
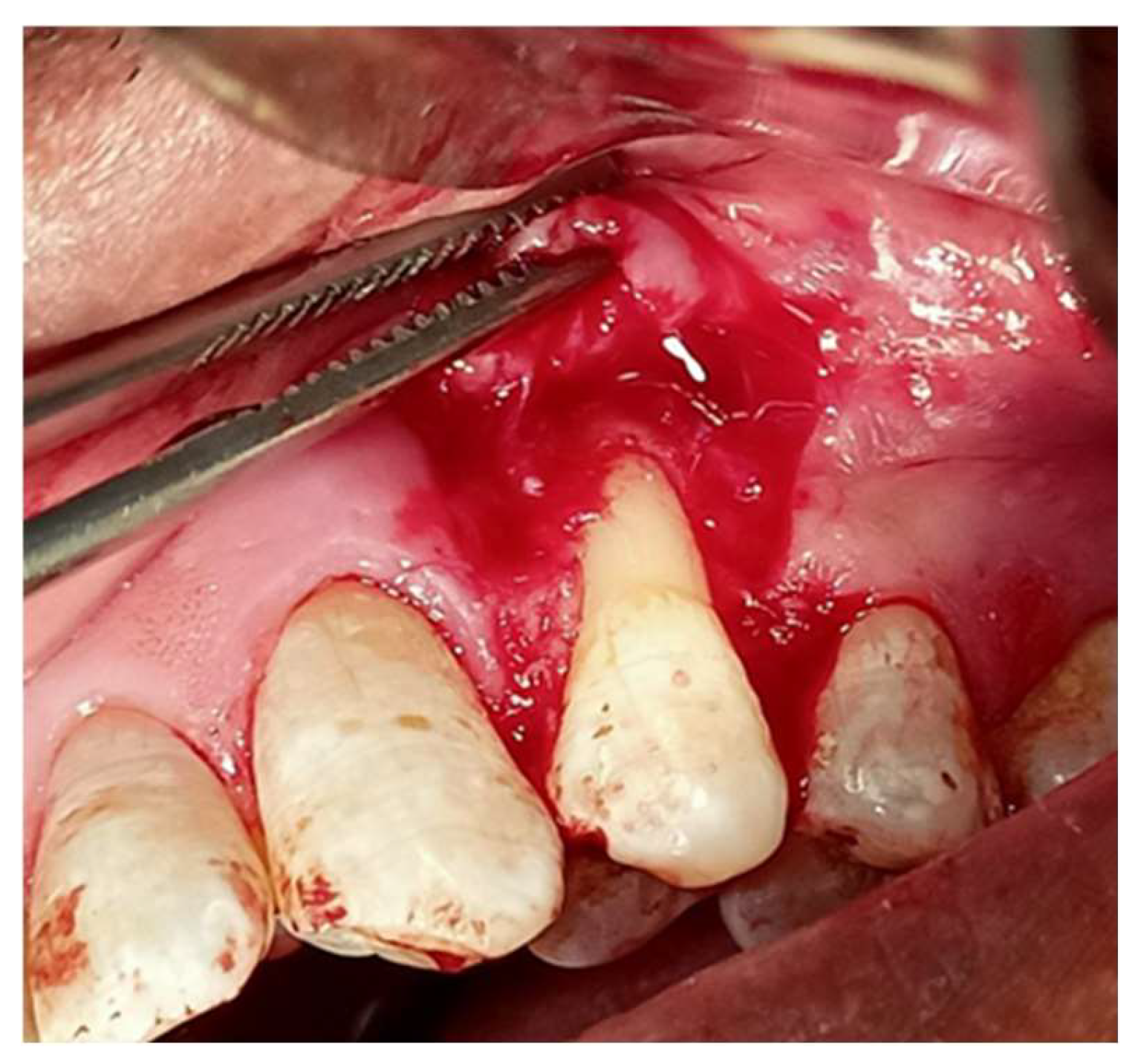
Figure 3.
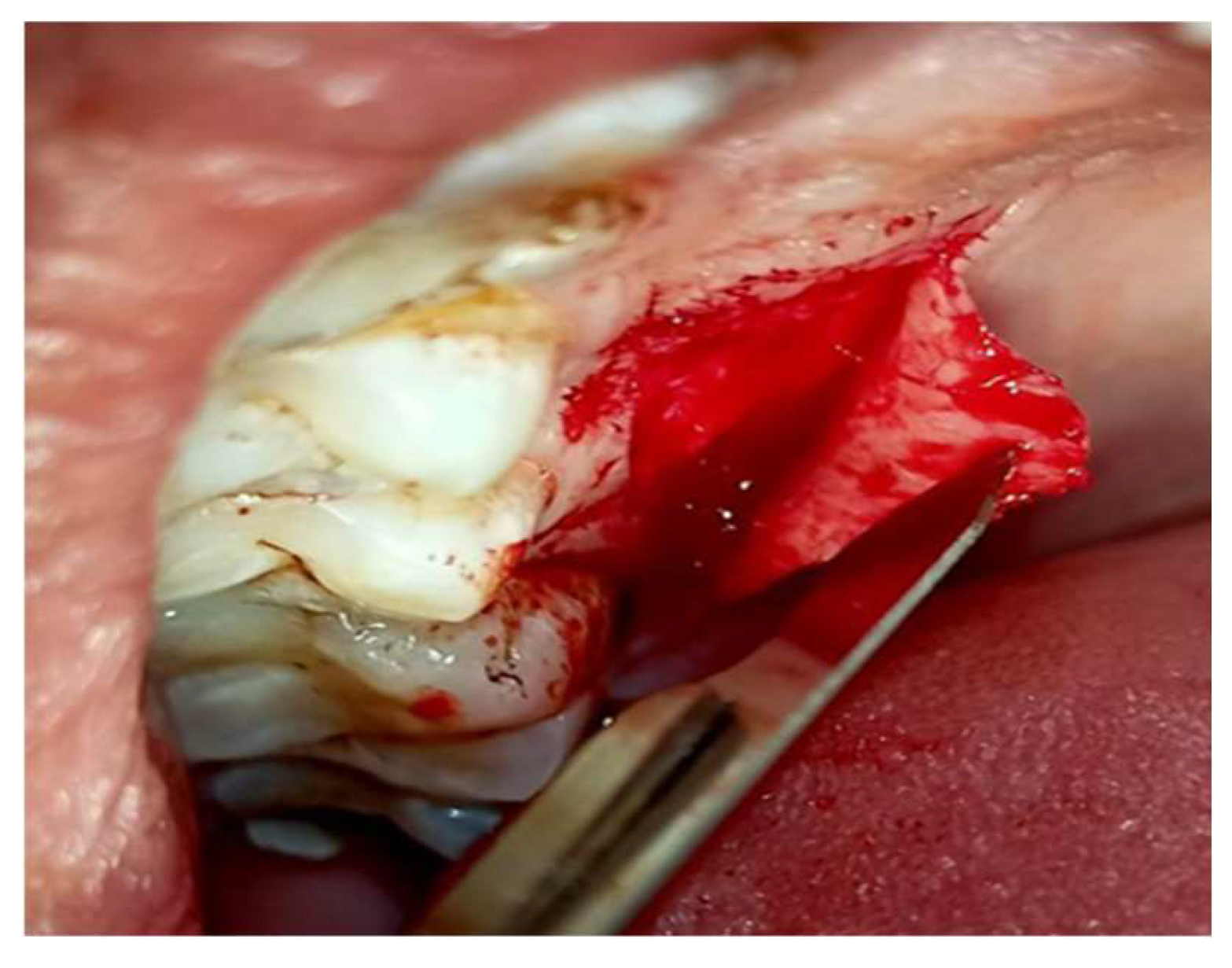
flap elevation.
Figure 3.
flap elevation.
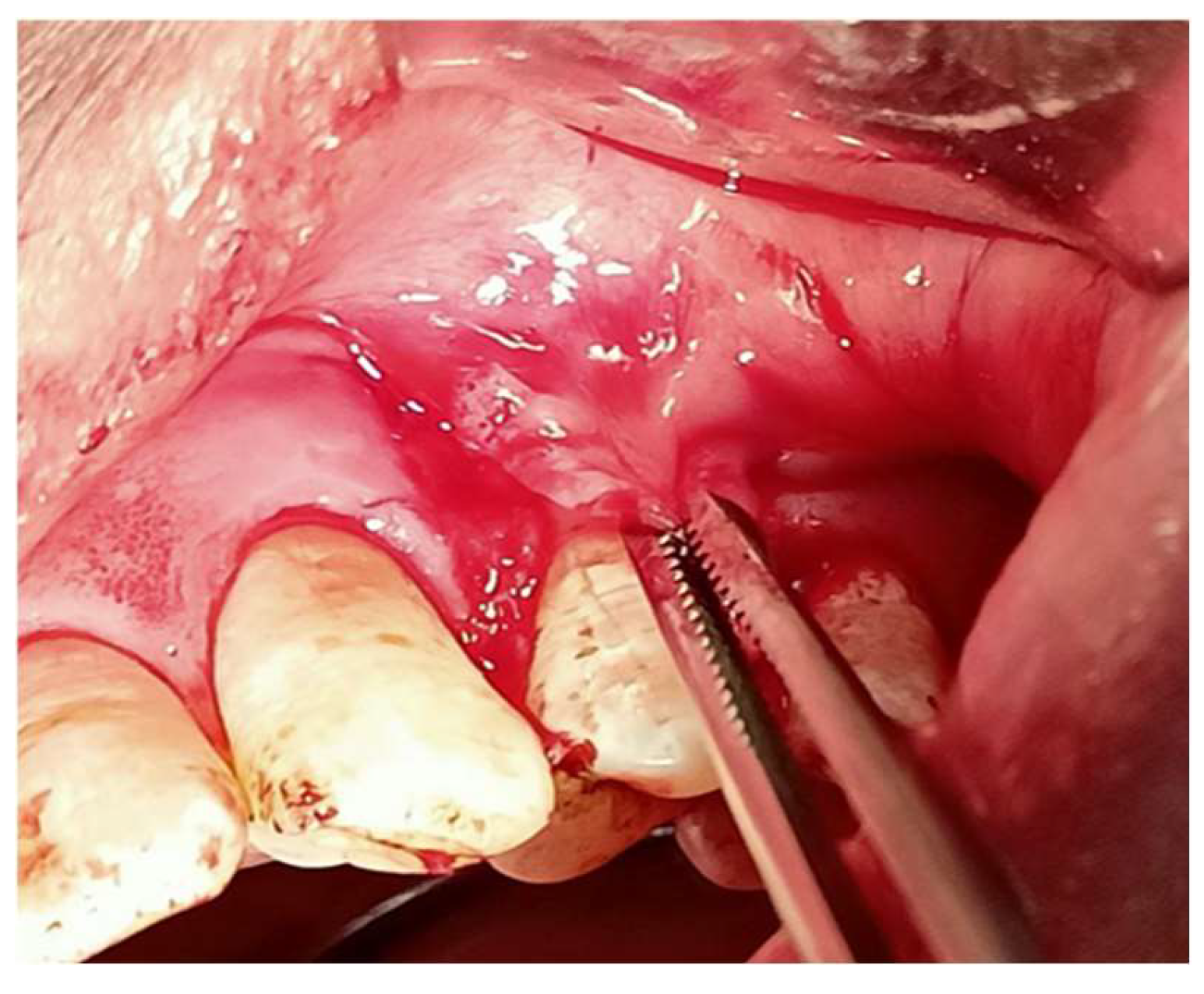
Figure 4.
advancement of flap coronally displacement.
Figure 4.
advancement of flap coronally displacement.
Figure 5.
root conditioning with EDTA gel for 2 min.
Figure 5.
root conditioning with EDTA gel for 2 min.
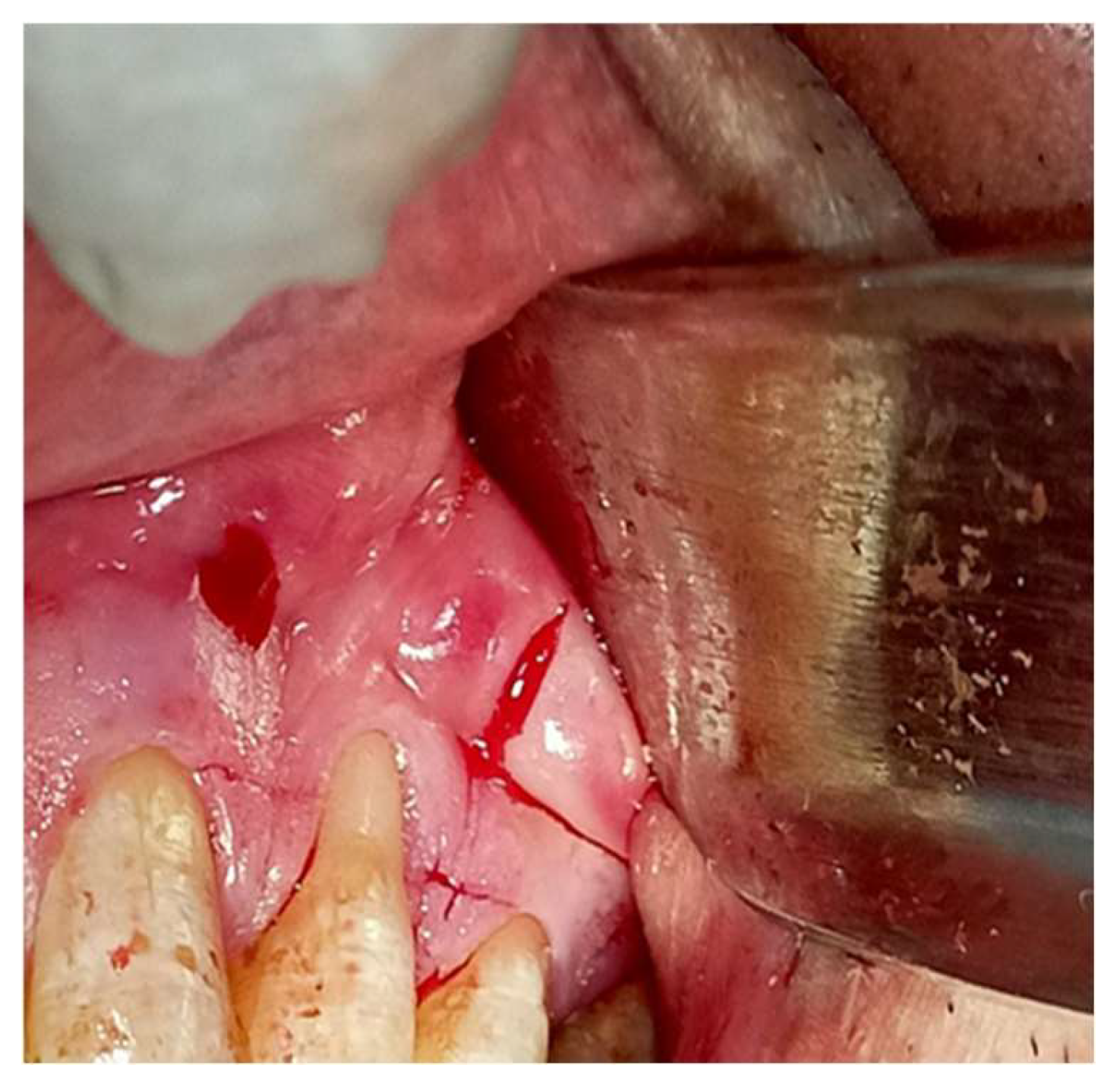
Figure 6.
incision of CTG (L shape technique two incisions one vertical and one horizontal)at hard palate(donor side).
Figure 6.
incision of CTG (L shape technique two incisions one vertical and one horizontal)at hard palate(donor side).
Figure 7.
elevation of epithelium.
Figure 7.
elevation of epithelium.
Figure 9.
position of CTG at cementoenamel junction.
Figure 9.
position of CTG at cementoenamel junction.
Figure 10.
stabilization of CTG with interrupted sutures .
Figure 10.
stabilization of CTG with interrupted sutures .
Figure 11.
stabilization of coronally advanced flap with sling sutures at marginal flap, interrupted sutures at vertical incisions and stress breaking sutures (double horizontal mattress).
Figure 11.
stabilization of coronally advanced flap with sling sutures at marginal flap, interrupted sutures at vertical incisions and stress breaking sutures (double horizontal mattress).
Figure 12.
suturing of donor side (L shape incision) with interrupted sutures.
Figure 12.
suturing of donor side (L shape incision) with interrupted sutures.
Figure 13.
follow up after two weeks.
Figure 13.
follow up after two weeks.
Figure 14.
follow up after one months.
Figure 14.
follow up after one months.
Case 2
45 years old male complain of sensitivity at upper lateral incisor presented at the Department of Periodontics, Faculty of Oral & Dental Medicine, with complaints of gum recession and sensitivity in the right central incisor at upper teeth. Clinical examination revealed a Miller Class III recession defect on the buccal side of tooth 11. Clinical attachment loss was recorded at 4.5 mm, and recession width at the cementoenamel junction measured 3 mm. The patient was in good general health, with no systemic diseases, medications, allergies, or smoking history.
Method:
A single-stage treatment approach was planned, all selected patients received a comprehensive periodontal examination and oral hygiene instructions, and they were subjected to full-mouth scaling and root planning. After 30 days, reevaluation was performed, which clinical improvement of clinical parameters (
Figure 1).
A coronal advancement flap with sub epithelium connective tissue graft was planned and performed to treat the gingival recession Miller class III.
Isolating the surgical area and anesthetizing the operative sites with 2% xylocaine hydrochloride containing adrenaline (1:200,000) is essential. Gracey curettes GR no. 1/2 and 3/4 are utilized to polish the exposed root surface to a glass-like finish, enhancing tissue adhesion.
Subsequently, 24% EDTA is applied to the root for 2 minutes to eliminate the smear layer, detoxify, decontaminate, and demineralize the surface, revealing the collagenous matrix of the dentin and cementum, which is crucial for optimal healing.
Measuring the anatomical papillae height:
When measuring the anatomical papillae height in a rotated tooth or when papillae height is lost, it is expected that the MRC will be coincide distally with the ideal papillae and so MRC will not be parallel to CEJ.
The distance between them should equal the distance between the papillae tip and the contact point, resulting in the most coronal root area remaining uncovered with mucogingival surgery.
The technique involves the same steps as the first case, with the exception of the type of graft being obtained.
Technique for obtaining the graft from donor site:
(using sub-epithelium connective tissue graft)
de-epithelization to obtain connective tissue graft was harvested using a #15 C scalpel via a partial-thickness dissection of this area, and then placed on a moistened damp compress with physiological saline.
For enhanced postoperative comfort and accelerated healing at the palate, a hemostatic sponge was used at the donor site after surgery.
The graft needs to be thick enough to prevent the superficial flap from desquamating due to poor vascularization, to cover any bone dehiscence, and to allow suturing at or above the cementoenamel junction.
To overcome the limitations of harvesting free gingival graft from the palate, collagen matrices (CM) from porcine sources (Mucograft®, Geistlich, Wolhusen, Switzerland) are utilized. These matrices have two functional layers: a dense external collagen layer that maintains structural integrity, provides infection protection, and aids in suturing, and a porous internal layer that promotes early vascularization and cell attraction. They act as scaffolds for fibroblasts and endothelial cells to create new connective tissue and support epithelial cell migration over the matrix from the surrounding tissue. Although they help increase tissue thickness, their effectiveness in expanding the width of keratinized tissue (KT) is limited [
15]
.
The flap is subsequently repositioned as coronally as feasible. Figure[17,18]
Figure 1.
The case represent miller cl (lII).
Figure 1.
The case represent miller cl (lII).
Figure 2.
ideal papilla and anatomical papilla coincide distally.
Figure 2.
ideal papilla and anatomical papilla coincide distally.
Fig3.
Coronal Advancement flap horizontal incision.
Fig3.
Coronal Advancement flap horizontal incision.
Figure 4.
vertical incision.
Figure 4.
vertical incision.
Figure 5.
incisions of CAF (trapezoid flap).
Figure 5.
incisions of CAF (trapezoid flap).
Figure 6.
advancement of flap coronally.
Figure 6.
advancement of flap coronally.
Figure 7.
root planning for pathological dehiscence.
Figure 7.
root planning for pathological dehiscence.
Figures 8,9.
de-epithelization for mesial & distal anatomical papilla.
Figures 8,9.
de-epithelization for mesial & distal anatomical papilla.
Fig 10.
root conditioning with EDTA
Fig 10.
root conditioning with EDTA
Figure 11.
irrigation to remove EDTA.
Figure 11.
irrigation to remove EDTA.
Figure 12.
incision at donor side (hard palate) for free gingival graft.
Figure 12.
incision at donor side (hard palate) for free gingival graft.
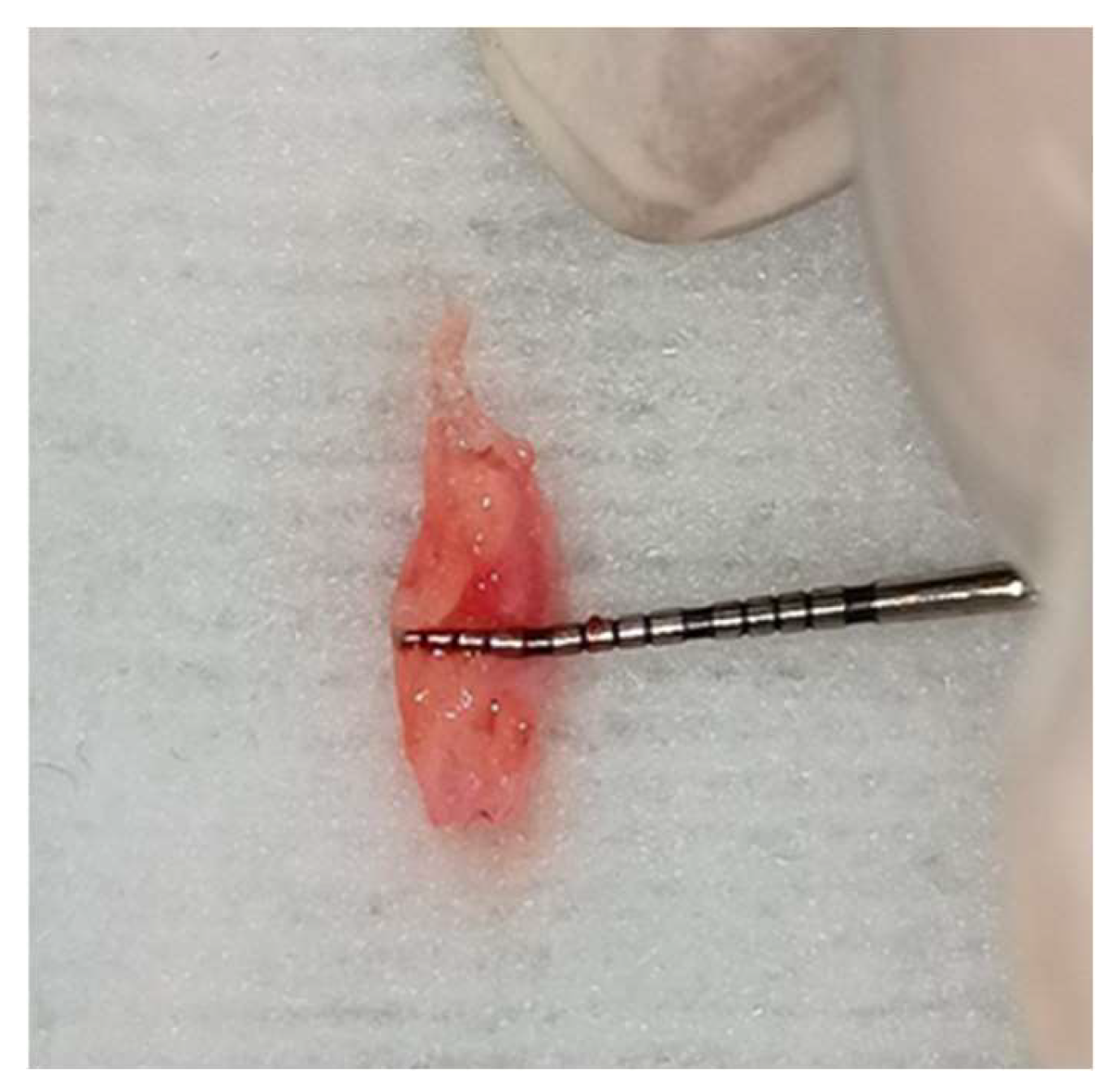
Figure 13.
thickness of CTG.
Figure 13.
thickness of CTG.
Figure 14.
length of CTG.
Figure 14.
length of CTG.
Figure 15.
de-epithelization of free gingival graft to obtain connective tissue graft.
Figure 15.
de-epithelization of free gingival graft to obtain connective tissue graft.
Figure 16.
stabilization of CTG with interrupted and periostium sutures.
Figure 16.
stabilization of CTG with interrupted and periostium sutures.
Fig 17.
stabilization of flap coronally covering CTG.
Fig 17.
stabilization of flap coronally covering CTG.
Figure 18.
occlusal view showing complete coverage of graft.
Figure 18.
occlusal view showing complete coverage of graft.
Figure 19.
follow up after 1 month.
Figure 19.
follow up after 1 month.