1. Introduction
The modern oncological neurosurgery is aimed at sparing pivotal functions, providing a complete neurocognitive assessment [
1]. The visuo-spatial functions (VSf) are essential for everyday life. Unilateral spatial neglect (USN) is an acquired disturb characterised by a difficulty in directing attention to meaningful stimuli presented in the space, contralateral to the brain lesion, not linked to sensory or motor deficits [
2], and can be assessed by administering specific tests developed in neuropsychology. Navigated TMS (nTMS) has been recently proposed in neuro-oncological research to detect brain sites functionally involved in cognitive processes [
3,
4], to preoperatively map cortical areas involved in language [
5], arithmetic calculation [
6], and more recently VSf [
7].
Nowadays, together with Direct Cortical Stimulation (DCS), the gold standard to map cortical functions in awake surgery, repetitive nTMS (rnTMS) is routinely used for preoperative mapping, guiding tumour resection either in asleep or awake surgery [
8,
9,
10,
11]. The joint use of nTMS and DCS can provide useful information on the convergence between these two techniques and reliability on nTMS to map VS attention before and even after surgery. Our research group have recently dedicated attention to Arithmetic calculation nTMS mapping to improve cognitive study and clinical outcome of oncological patients [
6], and this new work is aimed at adding a new component to preoperative planning. As far as we know, in neuro-oncological neurosurgical patients, USN is usually monitored to avoid post-operative impairments, allow a good quality of life after surgery, and possibly return to a normal life. Neuropsychological evaluation, nTMS cortical data, and DTI Tractography can be integrated in the preoperative planning to study multiple functions, guiding surgery, customising the surgical approach, and orienting the postoperative rehabilitation process.
Based on these considerations, we define the main objectives of this work:
-
1)
The primary aim consists of adding the VS perception, reasoning and attention testing within the preoperative mapping with nrTMS to evaluate the pre/post-operative clinical outcome of patients, operated on for brain lesions, including awake or asleep procedures.
-
2)
The secondary aim consists of evaluating the possible subcortical white matter fibre tracts involved in VS network (comparing tractographies derived from anatomical tensor and from nTMS data).
-
3)
The third aim consists of evaluating the correspondence between nTMS and DCS points during awake surgery, to determine nTMS reliability for VS network study and preservation.
2. Materials and Methods
We designed a monocentric, prospective clinical study, collecting data from patients operated on at the University Hospital of Careggi, Florence, Italy, who presented focal lesions in eloquent areas for Language, Arithmetic Calculation, and/or Visuo-spatial functions. Preoperative planning included: neuropsychological/logopaedic evaluation, MRI imaging, nTMS protocol including cognitive functions, such as language (L), calculation (C) and neglect (N). All operations were performed by the same senior Neurosurgeon (A.D.P).
The cognitive evaluation included: MiniMental State Examination (MMSE), Aachener Aphasie Test (AAT), and the Neuropsychological test for aphasia (ENPA), arithmetic items for calculations, VS abilities and presence of USN through the barrage tests (i.e. Broken Hearts test) taken from the translated Italian version of the Oxford Cognitive Screen (OCS), the Bells test, and the Clock drawing test (Shulman correction) [
12].
2.1. Navigated TMS Procedure for VSf
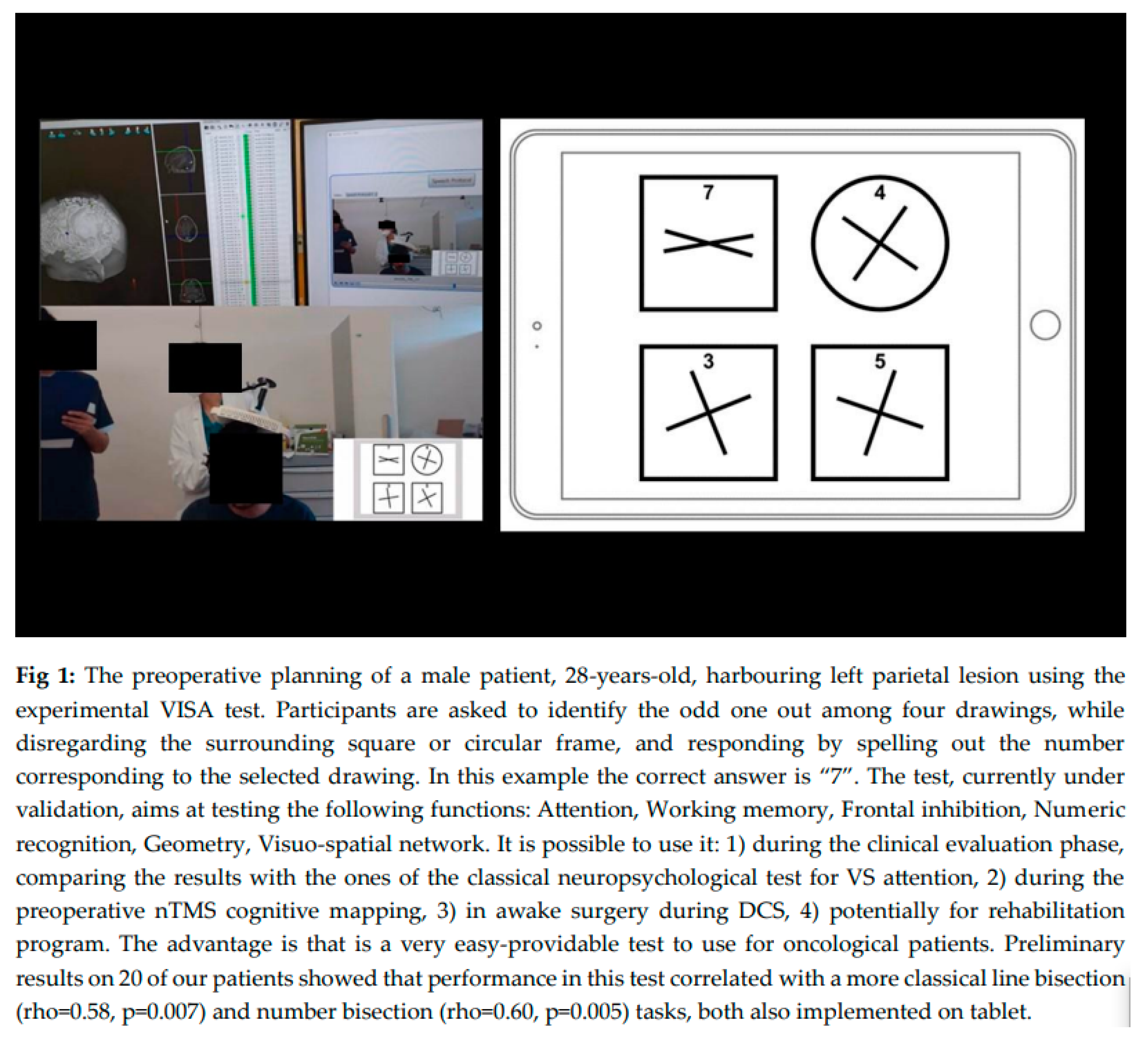
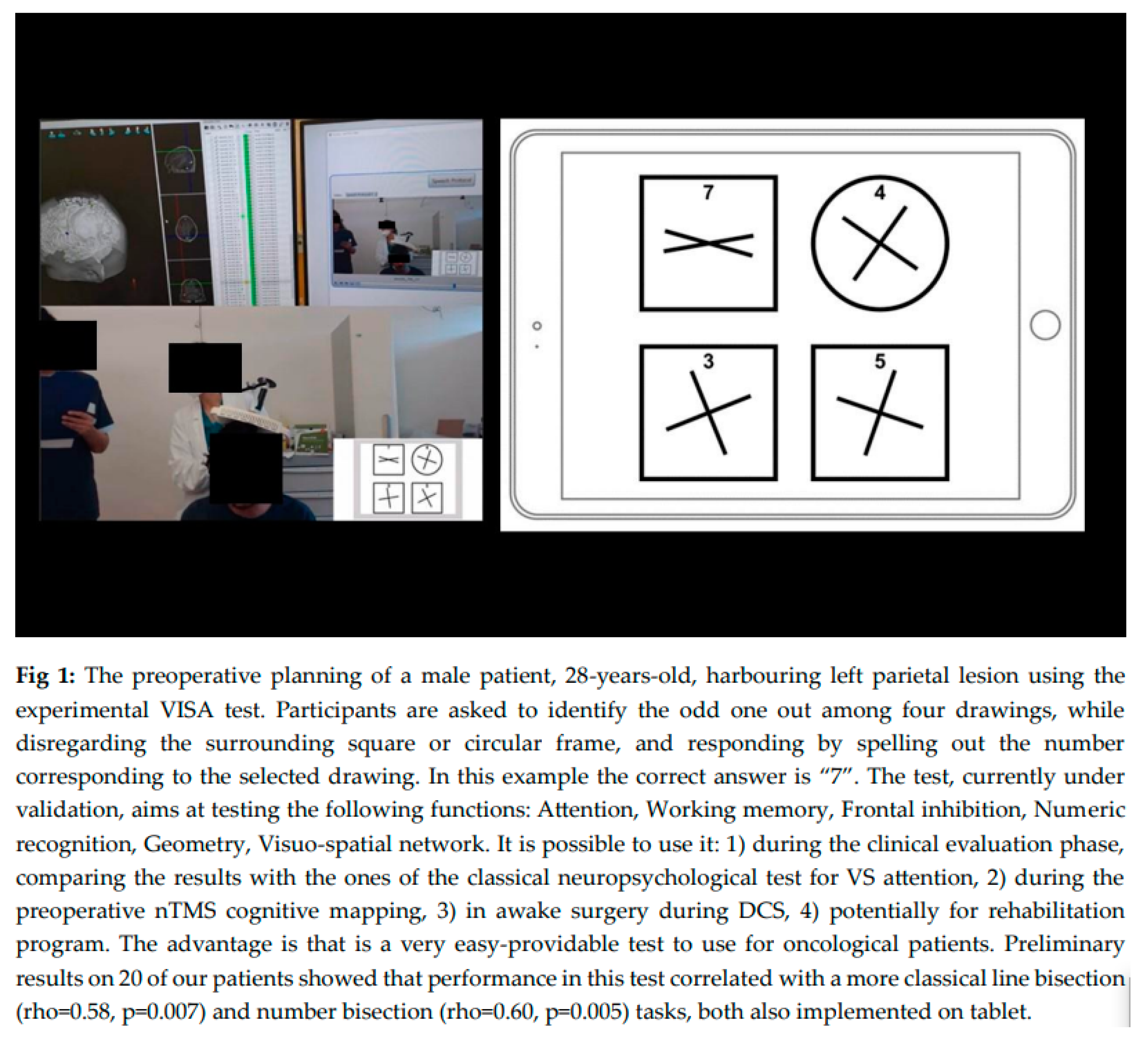
Visuo-Spatial Integrated Assessment (VISA): Experimental test evaluating multiple cognitive functions simultaneously: Dr Castaldi and her colleagues are currently developing a test, inspired from Dehaene et al [
13], to simultaneously evaluate visuo-spatial perception, visuo-spatial attention, non-verbal reasoning, cognitive control, and number reading. This test was proposed to our patients after classical neuropsychological tests for neglect (Classic tests: Line bisection test, OCS, Bells test). (Figure 1).
2.2. Preoperative MRI
A preoperative magnetic resonance imaging (MRI) was performed at our Neuroradiological Department, using a 3T Tesla M.R.I. machine (Ingenia 3T, Philips Medical Systems, Best, The Netherlands). Diffusion Tensor Imaging (DTI) sequences was employed for tractographies. Multiple Regions-of-Interest (ROIs) were identified and used to create subcortical pathways, using IntelliSpace Portal software (Philips). To reproduce the three branches of the Superior Longitudinal Fasciculus (SLF I-II-III), the method previously described [
14] was applied to identify. Our expert Neuroradiologist (A.B.) checked out all the tractographies and verified the correspondent projection of cortical n TMS dots to identify the branches of the SLF principally involved in VS function. The same SLF branches were reconstructed from the nTMS stimulation spots and verified, in comparison to the ones anatomically drawn.
2.3. Preoperative nrTMS Mapping
Preoperative cognitive mapping was performed, including L, C and VSf with rnTMS system (Galileo NetBrain Neuronavigator 9000, EB Neuro Corp., Florence, Italy). The mapping method was previously described [
6]. The experimental integrated VS test, potentially able to detect USN, was adapted for tablet use to facilitate practicality in nTMS dedicated room or in the operating setting. Participants were asked to identify the odd one out among four drawings, while disregarding the surrounding square or circular frame, and responding by spelling out the number corresponding to the selected drawing. [Figure 1]. All tests were displayed on a screen (picture presentation time 4 s; inter-picture interval 1 s) in front of the patient, who answered aloud with 5 pulses-5 Hz nrTMS perturbation. VSf were mapped on 70 spots over parietal, temporal and frontal cortices. A cortical spot was considered positive for any function when nrTMS perturbation induced an error in at least two out of three trials [
15]. MRI DTI scan was used to create an nTMS-based-tractography [
16,
17], to compare with the ‘anatomical’ tractography, based on tensor reconstruction, showing SLF branches.
The Intraoperative monitoring was performed either in awake or asleep procedures, including Motor and Somato-Sensorial Evoked Potentials (MEPs/SSEPs), EEG and Electrocorticography were recorded. In awake surgeries, the Penfield paradigm for DCS applied intensity between 0.5 and 3 mA.
2.4. Anaesthesiologic Parameters for Awake Surgery
Sedation was performed with Propofol 2% in TCI Schnider model, with target effect site concentration (CET) of 1–1.5 µg/ml, and Remifentanil 0.02-0.05 µg/kg/min in spontaneous breathing. Monitoring ECG, invasive blood pressure, oxygen saturation%, respiratory rate, EtC02, and diuresis output were controlled. For scalp nerve block/Mayfield application, Lidocaine 2%, Bupivacaine 0.5% (5mg/ml) with Epinephrine, and Ropivacaine 7.5 mg/ml were administered. During the awake phase and cortical mapping, BIS was maintained over value of 90 [
18]; a continuous EEG pattern was recorded to prevent seizures.
2.5. Identification of n TMS Points for VSf and Neglect
We identified points for VSf and USN in the parietal lobe, either left or right lesions, mainly located on the Supramarginal gyrus (SMG), Angular Gyrus (AG), on the Superior Temporal Gyrus (STG). Using the neuronavigation system integrated in the microscope (Kinevo Zeiss 900), we identified nTMS spots for VS functions and marked them with sterile tags on the brain cortical surface to guide surgical resection, according to functional boundaries in asleep procedures. During awake surgeries, the Penfield bipolar stimulation technique was applied (current intensity between 0.5 and 3 mA) for VSf mapping.
Surgical strategy was modulated based on nTMS preoperative mapping, sparing positive points on the cortical surface whenever possible, considering the areas with negative nTMS points useful for a safe access to brain lesions.
2.6. Statistical Analyses for n TMS/DCS Positive Points Analyses
We used the method previously proposed in our recent work on nTMS for arithmetic calculation monitoring [
6]. We applied statistical evaluation considering the 3D brain location involved with VSf; we based all the analyses on DCS points, collected during awake procedures, and nTMS spatial points coordinates
provided by the neuronavigational system (StealthStation Medtronic, U.S.A) [
6]. All analyses were performed using specific scripts written in
Python and the mathematical statistical method previously elaborated [
6].
Ethics: The study was approved by the Ethics Committee ‘Comitato Etico Area Vasta Centro’ [CEAVC Protocol n 17003], in compliance with the Declaration of Helsinki.
3. Results
Between April 2023 and March 2024, we enrolled 29 patients with diagnosis of primitive intra-axial focal lesions (histologically diagnosed as reported in
Table 1, according to WHO 2021), followed at the Neurosurgical Department of the University Hospital of Florence, to perform n TMS cognitive mapping, including VSf. Patients were enrolled for possible functional involvement of VS network. Thirty-one surgical procedures and preoperative planning were performed since three patients were operated on twice and were tested with n TMS either for the first or second operation. One patient was excluded because of no compliance to neurocognitive testing, and another since he had an extra-axial lesion (histologically diagnosed as meningioma), therefore the final number of patients was 27 and nTMS procedures considered for analyses were 30 [median level of scholarship:12.16± 2 years; mean age:50.77 ± 2 years]. The gender distribution was comparable (M: F=1:1). The histological diagnoses and anatomical locations are summarised in
Table 1. Among 27 patients, 15 were harbouring right lesions, 11 left lesions and one patient had a bilateral G3 glioma, involving the splenium of the corpus callosum. Twelve awake procedures were performed, two of them were aborted for anaesthesiologic issues. The final number was 10.
Seventeen were asleep procedures, where surgical strategy was guided by preoperative nTMS map. (
Table 1). Safety of cognitive n TMS was complete: no patient developed n TMS related epilepsy. The final number of 27 patients was tested for VSf during nTMS mapping. We analysed (I) pre and postoperative clinical outcome, (II) surgical strategy adaptation based on nTMS mapping, and nTMS/DCS correspondence. Finally (III) cortical nTMS and corresponding subcortical circuits were analysed.
Surgical strategy: awake or asleep procedures were chosen based on several characteristics (anaesthesiologic parameters, compliance, no preoperative deficits). At the beginning of the operation, after craniotomy and dura opening, using the neuronavigational system integrated in the microscope, nTMS points were identified and marked with a sterile tag, positioned on the cortical surface, to preserve it in asleep, or to compare it with DCS in awake surgery.
Globally, 55% of nTMS positive points for VS functions were exposed in the craniotomies performed and 75% were spared, when visible, even if at the margins of the craniotomy. We tried to avoid nTMS positive points, considered functionally active, but it was not possible when they were in the pathological cortical surface. Particularly, in two cases they were necessarily removed during surgery and postoperative functional outcome was monitored carefully.
In awake surgery, sterile tags were positioned over the nTMS positive sites and compared to DCS spots, acquiring spatial coordinates of these points.
Our patients were discharged after 5±7 days after surgery, three of them were re-operated for recurrence, one patient had a complication of surgical wound infection, which was treated with surgical toilette and antibiotic therapy. Clinical results were recorded immediately after surgery, at 30±10, and 90±10 days after surgery.
3.1. Clinical Outcome for VS Function
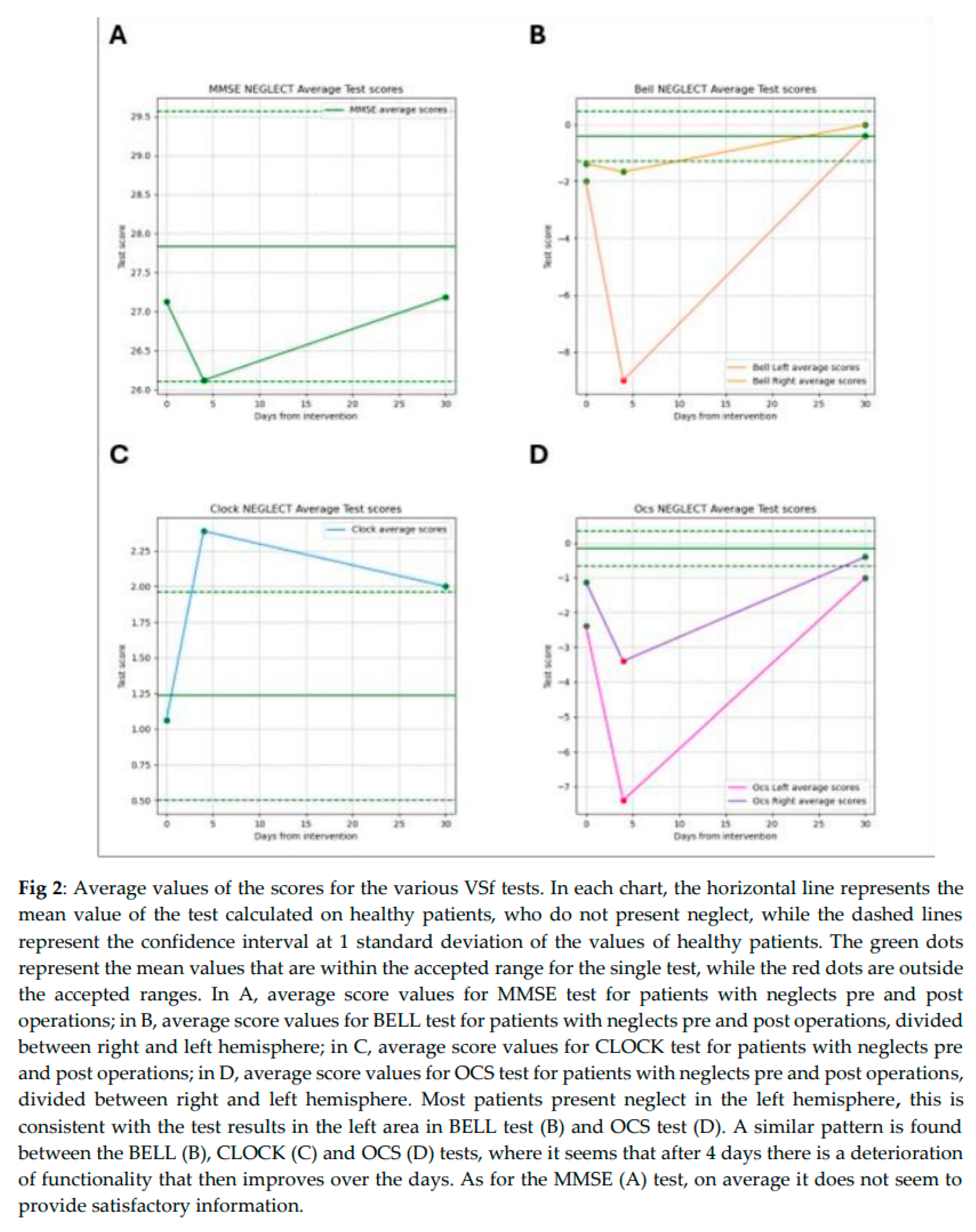
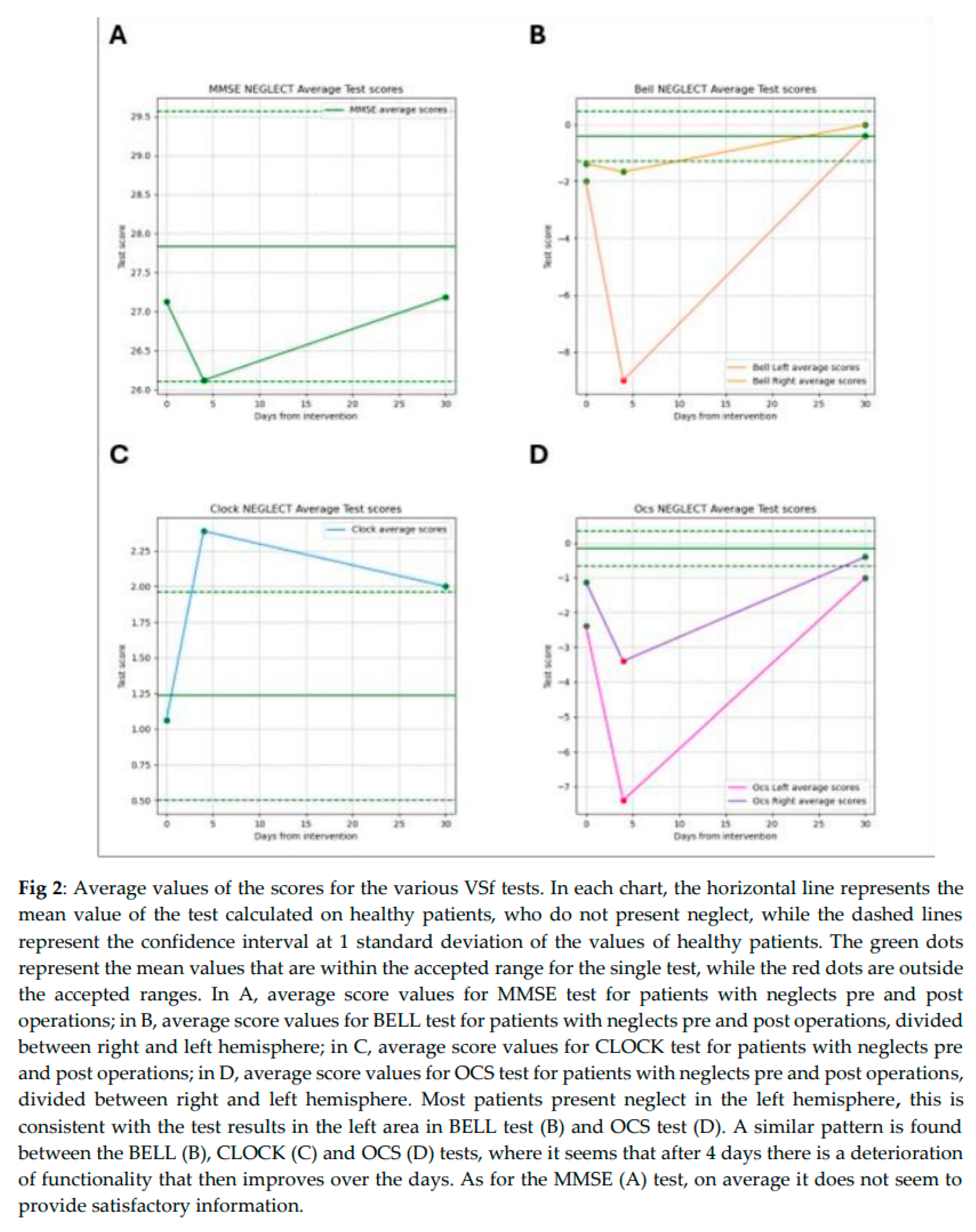
VSf and Neglect were tested preoperatively in 27 patients and 77.78% of procedures were performed on primary lesions. Preoperative deficits were present in 11% (3/27) of patients, whereas the majority did not have any impairment of VSfn (89%, i.e. 24/27). However, in the immediate postoperative period (5±2 days after surgery) we documented deficits in 40,74% of patients (11/27), the 27% (3/11) of them had a preoperative impairment that worsened after surgery. This data was based on cognitive evaluation (including Bell test, OCS and the preoperative cognitive battery). 33% of our patients developed left neglect, i.e. presented neglect in the left hemifield, according to test results in the left area in Bell test and OCS test. A similar pattern was found between the Bell, Clock and OCS tests, where it seems that after 4 days there is a deterioration of functionality that then improves over the days. As for the MMSE test, on average it does not seem to provide satisfactory information (Figure 2A,B). We saw a temporary decrease of MMSE performance in patients with immediate postoperative USN, whose progressive recovery was documented during 3-months-follow-up period, documented by postoperative tests results improving [90.62% in MMSE, 98.86% in Bell Test, 80% in Clock test, 98% in OCS test] (Figure 2,
Table 2). In one case the postoperative evaluation was significantly compromised, including also linguistic-computational deficits. Nevertheless, there was a progressive improvement at 1 month after surgery and an almost complete recovery at distance: we calculated the percentage of functional recovery: 11/27 patients (approximately 40%) experienced transient functional deficits, with a decline in performance across all VS tests, reaching functional decrease to 80-85% for right-sided lesions and 38% for left-sided lesions. Progressive recovery was observed during the follow-up period, with clinical improvement restoring 80-98% of function, based on previous test results.
Experimental VISA—Results
The Visuo-Spatial Integrated Assessment was proposed and corrected by our neuropsychologist and speech therapist. Comparing VISA with the traditional tests for VSf, VISA is advantageous because is very easy-providable to use for oncological patients, with variable level of difficulty, based on the type of images appearing on the screen in front of subjects. The only caution we must adopt is the comprehension of patients, whose capability to understand and consequently perform the test must be checked in advance.Preliminary results on 20 of our patients showed that performance in this test correlated with a more classical line bisection (rho=0.58, p=0.007) and number bisection (rho=0.60, p=0.005) tasks, both also implemented on tablet.
3.2. VS Network: N TMS Based Tractography and n TMS Mapping
Tractographies were reconstructed, based on MRI DTI sequences, using the StealtViz software (Stealthviz; Medtronic, Dublin, Ireland). Multiple ROIs (Region of Interest) at the cortical level were identified, based on the location of specific regions, to reconstruct the three branches of the Superior Longitudinal Fasciculus (SLFI-II-III) [
14,
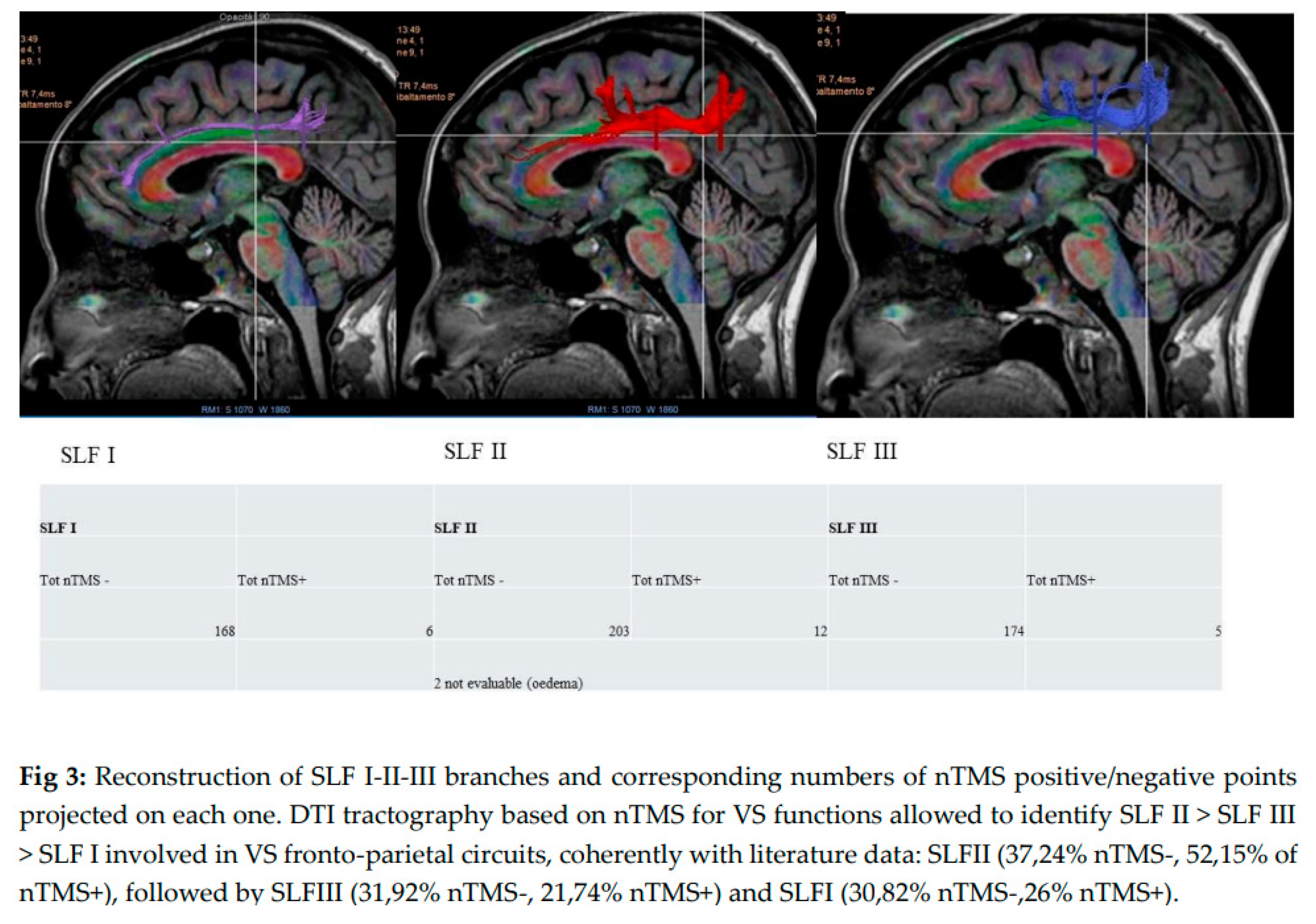
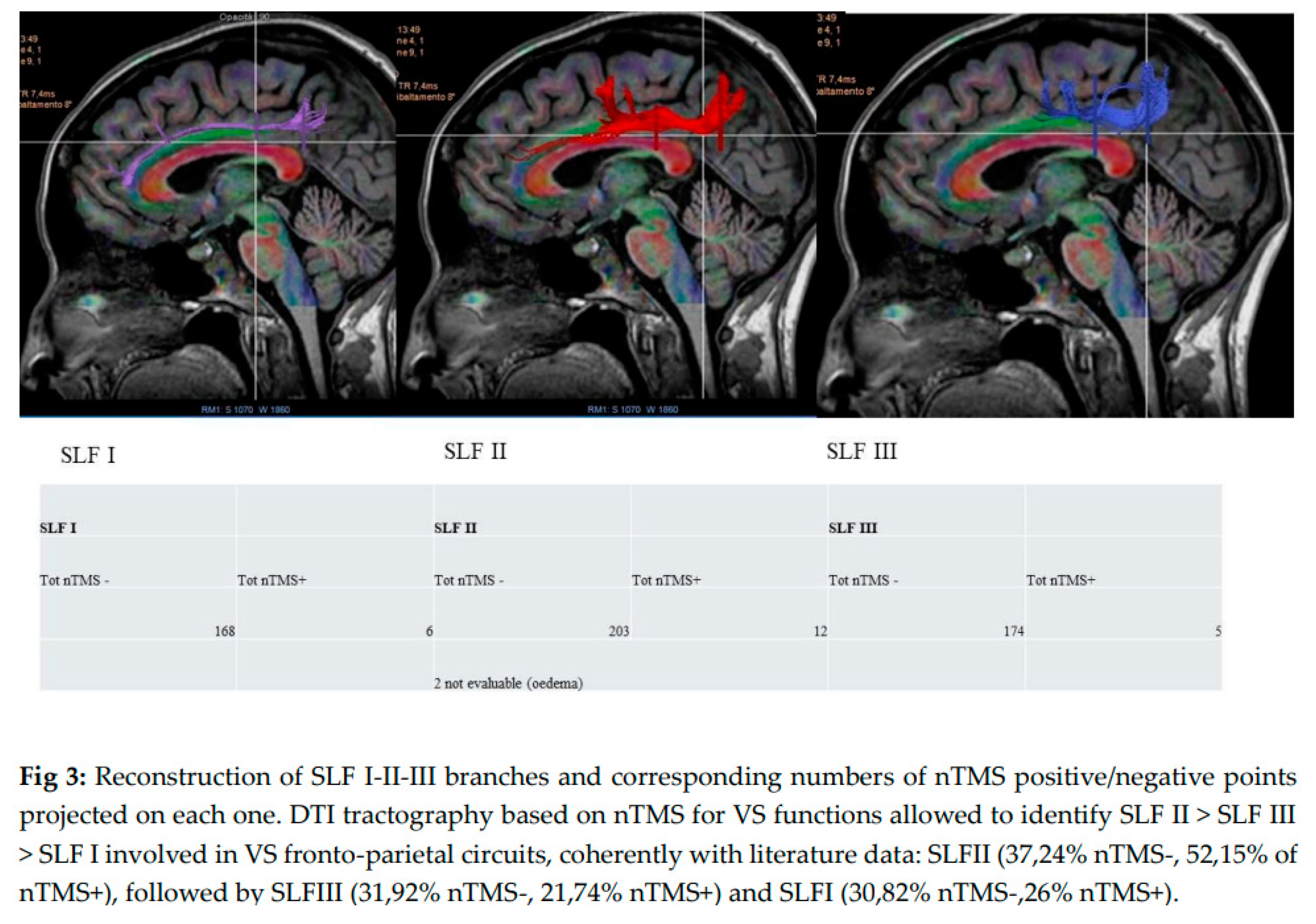
19], and then using multiple ROIs, including also nTMS points for visuospatial functioning. According to our data, projected on SLFI we recorded:168 nTMS - and 6nTMS + points; on SLFII: 203 nTMS- and 12 nTMS+ points; on SLFIII:, 174 nTMS- and 5 nTMS+ points. Therefore, the major represented branch of SLF in VS circuits is SLF II (37,24% nTMS-, 52,15% of nTMS+), followed by SLFIII (31,92% nTMS-, 21,74% nTMS+) and SLFI (30,82% nTMS-,26% nTMS+). according to our preliminary data. [Figure 3]. Further analyses are needed to better understand the role of white matter fibre tracts in elaborating/integrating multiple functions.
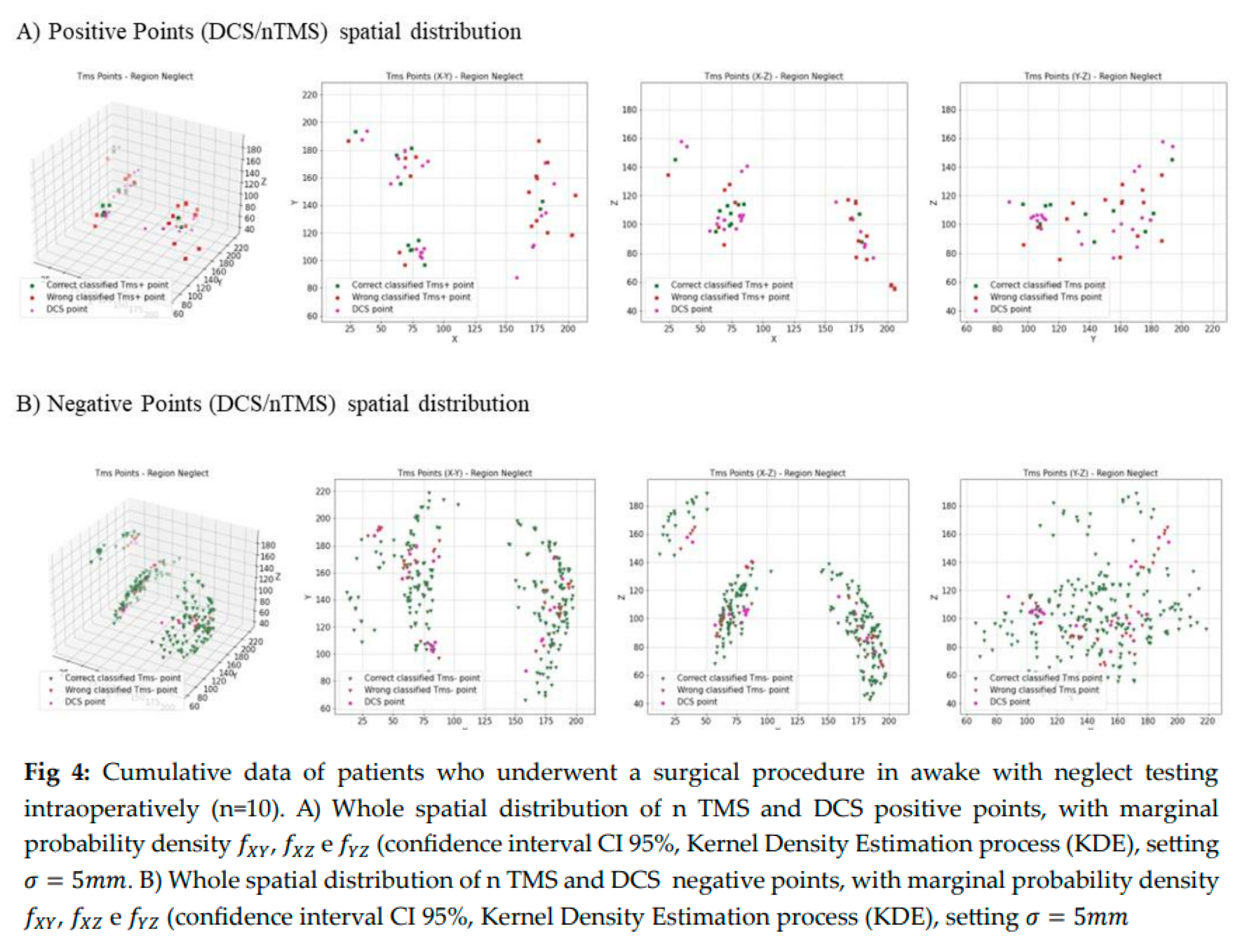
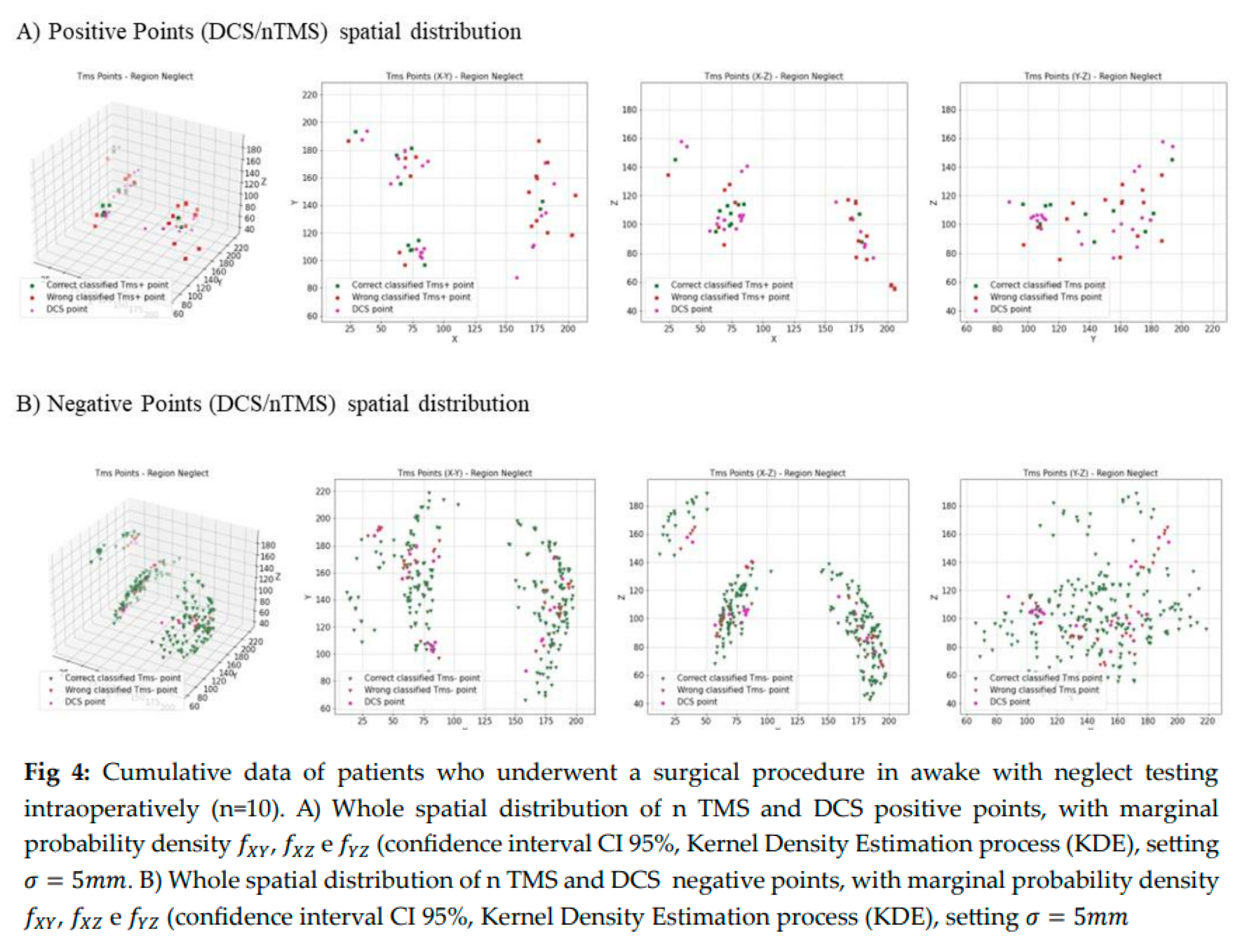
3.3. DCS and n TMS Convergence
For all our patients, to validate n TMS points (n TMS) comparing them with Direct Cortical Stimulation (DCS), we considered 12 awake procedures. Two were aborted for anaesthesiologic problems, so the final number was 10, with standardised protocol of acquiring coordinates (x, y, z) for n TMS and DCS points Comparison between DCS and n TMS positive points may be more objective, reproducible, and reliable. Our analyses documented: Sensitivity (Se)=12%, Specificity (Sp)=91.21%, Positive Predictive Value (PPV)=42%, Negative Predictive Value (NPV)=66%. Accuracy was estimated at 63.7%. Although this is a very small sample of patients, based on these preliminary results, we can optimise our surgical collection of data to validate our method of analysis. [
Table 3 and
Table 4, Figure 4].
4. Discussion
Our work proposed the following main objectives of evaluating:
- 1)
the clinical utility of nTMS preoperative planning for VSf,
- 2)
the white matter fibre tracks underneath VS network, analysing the predominant role of the three branches of the SLF
- 3)
nTMS and DCS during awake procedures to validate n TMS for VS circuits cortical mapping, relating cortical and subcortical data.
4.1. VS Functions
VS functions are fundamental to perform many activities in life. Recent efforts are directed to investigate a wider range of cognitive and perceptual functions in neuro-oncological patients [
20]. USN is a complex neurological disturb, not linked to sensory or motor deficits [
2]. In neuro-psychology, USN impairment is usually assessed by means of: line-bisection tests [
21,
22], line-bisection judgement tasks [
7,
23,
24], and chimeric objects and faces naming tasks [
25]. These tasks were firstly administered to post-stroke patients [
26] and afterwards extended to neuro-oncological patients to control post-operative difficulties [
27,
28]. The line bisection judgment task [
22] and the computerised line bisection task [
28] are among the most used methods to assess the USN in awake surgery routines [
29,
30]. In Neurosurgery, nTMS is gaining a relevant role in pre-operative study of neuro-oncological patients, with validated applications for motor and language functions [
31,
32], and novel ones for arithmetic calculation [
6], and VSf [
7]. Therefore, understanding the convergence between nTMS and DCS is pivotal for and advanced cognitive mapping [
4]. From a structural point of view, the application of cortico-subcortical stimulation in awake surgery led to the identification of brain areas critically involved in VSf and impairment (USN). At the cortical level, the posterior superior parietal lobe and the inferior parietal lobe constitute regions of interest for the USN [
7,
28,
33] while, at the subcortical level, the SLFII has obtained converging evidence for its involvement in visuospatial attention [
21,
34].
4.2. rnTMS and Cognitive Task
To map VS network with rnTMS, a pilot study on 10 healthy right-handed subjects was performed, using Greyscales task [
3], mapping 52 cortical spots in both hemispheres. The task pictures showed pairs of horizontal rectangles shaded continuously from black at one end to white at the other, mirror-reversed [
3,
24], to test Neglect. A case report [
7] of a patient with a right temporal low-grade glioma applied rnTMS with line bisection and Bells Test. Another study [
35] on patients harbouring right parietal lesions exploited Hooper Visual Organization Test (HVOT) to identify cortical areas involved in the VS network. In our experience, the same stimulation parameters (5 pulses/5Hz rnTMS) were used, and experimental VS integrated test was useful either in pre-/intra-/post-operative phases, to prevent USN and analyse clinical outcome. While optimisation and validation of this test is ongoing, it appears to be a promising test to simultaneously measure and preserve visuo-spatial perception, visuo-spatial attention, non-verbal reasoning, cognitive control, and number reading.
4.3. Anatomic Location of VSf and nrTMS Protocol
VS network, thought as capability of directing attention to the spatial stimuli , relies on a fronto-temporal and parietal network [
36] which may be lesioned by the tumours (48% of lesions included in our study involved more than one lobe). Bi-hemispheric mapping protocol is advisable, since reports on ipsilesional neglect are less common than those on classical contralesional neglect [
3,
24]. Rightward errors (or left-sided neglect) occurred significantly more often during stimulation of the right hemisphere, according to a contralesional neglect, than during stimulation of the left hemisphere (ipsilesional neglect). This evidence is coherent with our preliminary results. Furthermore, the rightward errors within the left hemisphere were mainly located to anterior parietal regions. Interestingly, this evidence was confirmed in previous studies [
37]. The stimulation of the left hemisphere elicited primarily leftward errors and then contralesional neglect [
3,
24,
38,
39]. Another study [
35] compared the error rate (per error type) between the right and left hemisphere: VS errors were significantly more frequent in the right hemisphere, while language-based errors in the left hemisphere. These results are coherent with our preliminary data.
Concerning anatomical circuits of VS attention, a study demonstrated that the anatomical areas of brain damage resulting in neglect-like symptoms are highly dependent on the task used to diagnose them [
40]. In our work, only the experimental VISA was used for rnTMS mapping, comparing results with previous cognitive tests performed by the same patients.
4.4. nrTMS Mapping and DTI Tractography
DTI tractography for 20 right parietal lesions was used to compute the subcortical component of the VS network, consisting of the three branches of the superior longitudinal fasciculus (SLF) [
35]. DTI reconstruction was based on multiple region-of-interests (ROI)-based approach, as we did in our study. Tractography studies demonstrated the role of the SLF in the VS network, since SLF-I-II-III connect the posterior parietal cortex to the dorsal and ventral frontal cortex, thus creating a complex fronto-parietal VS network. In our study we tried to correlate the cortical and subcortical data, specifying that SLF II seem to be the most involved branch of the VS circuits, followed by SLFI-III. Respecting the subcortical circuits is essential during surgery to avoid clinical impairment.
4.5. nTMS and DCS for VSf
When comparing nTMS with DCS during awake procedures, we found that nTMS still shows a high negative predictive value (66.07%). This means that negative nTMS points are more reliable for identifying ‘safe entry zones’, which are not functionally active cortical areas, allowing to perform corticectomy and enter the brain parenchyma, creating a safe surgical corridor to the lesion. It is reasonable to suggest that more extensive cognitive nTMS mapping data, including VSf, are needed to make meaningful comparisons with DCS, as VSf has not been thoroughly explored yet, and our study only presents preliminary data.
The parameters of nTMS stimulation were the same used for language and calculation mapping, with an average intensity of 100% of the resting motor threshold (rMT), standard deviation (SD) of 9.0%, and a range of 80-120% of rMT. During awake surgeries, stimulation intensity usually ranges from 0.5 to 3 mA to minimize the risk of seizures.
The previous described value for nTMS mapping for language and calculation6 were higher in terms of sensitivity, specificity, and positive predictive value. We need to implement our data to confirm these results.
4.6. nTMS and Neglect Rehabilitation Program
TMS has been applied for the rehabilitation of USN after a brain lesion, mostly enrolling post stroke patients at different stages of the disease. Following either the hypotheses of the downregulation of the intact hemisphere or the upregulation of the affected hemisphere, different stimulation protocols were proposed with diverging findings. As far as we know, little is known on the potentialities of TMS modulation for the recovery of USN in other populations (e.g., neuro-oncological patients). Our next goal is to implement this point with an early rehabilitation program.
Limitations:
- a)
Limited number of patients and surgical procedures
- b)
Recurrent lesions (possible bias for clinical results)
- c)
VISA is an experimental test, whose value is significant to implement the preoperative study of our patients, however we need more patients to acquire data and compare it with classical neuropsychological evaluations.
5. Conclusions
Our preliminary work shows that nTMS is valuable to explore VS functions and prevent neglect after brain tumour surgery. Our study represents a preliminary but promising experience to implement the use of n TMS in the preoperative mapping of cognitive functions.
Author Contributions
Conceptualization, C.B., E.C, A.D.P..; methodology, E.P., E.C., C.B. R.C.; software, E.P., E.C.; validation, E.C.,E.P., C.B., F.F., A.G..; formal analysis, C.B and E.C..; investigation, C.B.; resources, C.B. A.D.P. A.G..; data curation, C.B., E.P., E.C, .; writing—original draft preparation, C.B and E.C.; writing—review and editing, C.B, E.C., A.D.P., M.G, S.D.P,; visualization, A.D.P .; supervision, A.D.P, E.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
“The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of ‘Comitato Etico Area Vasta Centro’ [CEAVC Protocol n 17003, October 2021].
Acknowledgments
Micheal Frank Angear for revision of the final English version of this work.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Herbet G DH. Contribution of the medial eye field network to the voluntary deployment of visuospatial attention. 2022 Jan 17;Nat Commun: 13(1):328. [CrossRef]
- Swan L. Unilateral spatial neglect. Physical therapy. Sep 2001;81(9):1572-80. [CrossRef]
- Giglhuber K, Maurer S, Zimmer C, Meyer B, Krieg SM. Mapping visuospatial attention: the greyscales task in combination with repetitive navigated transcranial magnetic stimulation. BMC Neuroscience. 2018/07/11 2018;19(1):40. [CrossRef]
- Duffau H. Functional Mapping before and after Low-Grade Glioma Surgery: A New Way to Decipher Various Spatiotemporal Patterns of Individual Neuroplastic Potential in Brain Tumor Patients. Cancers. Sep 13 2020;12(9). [CrossRef]
- Natalizi F, Piras F, Vecchio D, Spalletta G, Piras F. Preoperative Navigated Transcranial Magnetic Stimulation: New Insight for Brain Tumor-Related Language Mapping. Journal of personalized medicine. Sep 27 2022;12(10). [CrossRef]
- Bonaudo C, Pedone A, Capelli F, et al. Brain tumor surgery guided by navigated transcranial magnetic stimulation mapping for arithmetic calculation %J Journal of Neurosurgery. 01 Jun. 2024 2024:1-12. [CrossRef]
- Tamás V, Sebestyén G, Nagy SA, et al. Provocation and prediction of visual peripersonal neglect-like symptoms in preoperative planning and during awake brain surgery. Acta neurochirurgica. Jul 2021;163(7):1941-1947. [CrossRef]
- Krieg SM. Navigated Transcranial Magnetic Stimulation in Neurosurgery, Springer International Publishing AG. 2017 2017;BOOK. [CrossRef]
- Ille S, Schwendner M, Zhang W, Schroeder A, Meyer B, Krieg SM. Tractography for Subcortical Resection of Gliomas Is Highly Accurate for Motor and Language Function: ioMRI-Based Elastic Fusion Disproves the Severity of Brain Shift. Cancers. Apr 9 2021;13(8). [CrossRef]
- Krieg SM, Gerloff C. Updated safety standards for TMS: A must-read in brain stimulation. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. Jan 2021;132(1):214-215. [CrossRef]
- Ille S, Kelm A, Schroeder A, et al. Navigated repetitive transcranial magnetic stimulation improves the outcome of postsurgical paresis in glioma patients - A randomized, double-blinded trial. Brain stimulation. Jul-Aug 2021;14(4):780-787. [CrossRef]
- Shulman KI, Pushkar Gold D, Cohen CA, Zucchero CJIJoGP. Clock-drawing and dementia in the community: A longitudinal study. 1993;8.
- Dehaene S, Izard V, Pica P, Spelke E. Core knowledge of geometry in an Amazonian indigene group. Science (New York, NY). Jan 20 2006;311(5759):381-4. [CrossRef]
- Kamali A, Flanders AE, Brody J, Hunter JV, Hasan KM. Tracing superior longitudinal fasciculus connectivity in the human brain using high resolution diffusion tensor tractography. Brain structure & function. Jan 2014;219(1):269-81. [CrossRef]
- Corina DP, Loudermilk BC, Detwiler L, Martin RF, Brinkley JF, Ojemann G. Analysis of naming errors during cortical stimulation mapping: implications for models of language representation. Brain and language. Nov 2010;115(2):101-12. [CrossRef]
- Sollmann N, Fratini A, Zhang H, Zimmer C, Meyer B, Krieg SM. Associations between clinical outcome and tractography based on navigated transcranial magnetic stimulation in patients with language-eloquent brain lesions. Journal of neurosurgery. Mar 15 2019;132(4):1033-1042. [CrossRef]
- Sollmann N, Zhang H, Schramm S, et al. Function-specific Tractography of Language Pathways Based on nTMS Mapping in Patients with Supratentorial Lesions. Clinical neuroradiology. Mar 2020;30(1):123-135. [CrossRef]
- Nimmo AF, Absalom AR, Bagshaw O, et al. Guidelines for the safe practice of total intravenous anaesthesia (TIVA): Joint Guidelines from the Association of Anaesthetists and the Society for Intravenous Anaesthesia. Anaesthesia. Feb 2019;74(2):211-224. [CrossRef]
- Janelle F, Iorio-Morin C, D'Amour S, Fortin D. Superior Longitudinal Fasciculus: A Review of the Anatomical Descriptions With Functional Correlates. Frontiers in neurology. 2022;13:794618. [CrossRef]
- Castaldi E, Bonaudo C, Maduli G, et al. Neurocognitive Assessment of Mathematics-Related Capacities in Neurosurgical Patients. Brain sciences. Jan 10 2024;14(1). [CrossRef]
- Thiebaut de Schotten M, Urbanski M, Duffau H, et al. Direct evidence for a parietal-frontal pathway subserving spatial awareness in humans. Science (New York, NY). Sep 30 2005;309(5744):2226-8. [CrossRef]
- Herbet G, Yordanova YN, Duffau H. Left Spatial Neglect Evoked by Electrostimulation of the Right Inferior Fronto-occipital Fasciculus. Brain topography. Nov 2017;30(6):747-756. [CrossRef]
- Fierro B, Brighina F, Oliveri M, et al. Contralateral neglect induced by right posterior parietal rTMS in healthy subjects. Neuroreport. May 15 2000;11(7):1519-21.
- Giglhuber K, Maurer S, Zimmer C, Meyer B, Krieg SM. Evoking visual neglect-like deficits in healthy volunteers - an investigation by repetitive navigated transcranial magnetic stimulation. Brain imaging and behavior. Feb 2017;11(1):17-29. [CrossRef]
- Sarri M, Kalra L, Greenwood R, Driver J. Prism adaptation changes perceptual awareness for chimeric visual objects but not for chimeric faces in spatial neglect after right-hemisphere stroke. Neurocase. Jun 2006;12(3):127-35. [CrossRef]
- Moore M, Milosevich E, Beisteiner R, et al. Rapid screening for neglect following stroke: A systematic search and European Academy of Neurology recommendations. European journal of neurology. Sep 2022;29(9):2596-2606. [CrossRef]
- Bartolomeo P, Thiebaut de Schotten M, Duffau H. Mapping of visuospatial functions during brain surgery: a new tool to prevent unilateral spatial neglect. Neurosurgery. Dec 2007;61(6):E1340. [CrossRef]
- Vallar G, Bello L, Bricolo E, et al. Cerebral correlates of visuospatial neglect: a direct cerebral stimulation study. Human brain mapping. Apr 2014;35(4):1334-50. [CrossRef]
- de Zwart B, Ruis C. An update on tests used for intraoperative monitoring of cognition during awake craniotomy. Acta neurochirurgica. May 7 2024;166(1):204. [CrossRef]
- Ruis C. Monitoring cognition during awake brain surgery in adults: A systematic review. Journal of clinical and experimental neuropsychology. Dec 2018;40(10):1081-1104. [CrossRef]
- Tarapore PE, Picht T, Bulubas L, et al. Safety and tolerability of navigated TMS for preoperative mapping in neurosurgical patients. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology. Mar 2016;127(3):1895-900. [CrossRef]
- Ille S, Zhang H, Sogerer L, et al. Preoperative function-specific connectome analysis predicts surgery-related aphasia after glioma resection. Human brain mapping. Dec 15 2022;43(18):5408-5420. [CrossRef]
- Zigiotto L, Amorosino G, Saviola F, et al. Spontaneous unilateral spatial neglect recovery after brain tumour resection: A multimodal diffusion and rs-fMRI case report. Journal of neuropsychology. Mar 2024;18 Suppl 1:91-114. [CrossRef]
- Landers MJF, Sitskoorn MM, Rutten GM, Mandonnet E, De Baene W. A systematic review of the use of subcortical intraoperative electrical stimulation mapping for monitoring of executive deficits and neglect: what is the evidence so far? Acta neurochirurgica. Jan 2022;164(1):177-191. [CrossRef]
- Raffa G, Quattropani MC, Marzano G, et al. Mapping and Preserving the Visuospatial Network by repetitive nTMS and DTI Tractography in Patients With Right Parietal Lobe Tumors. Frontiers in oncology. 2021;11:677172. [CrossRef]
- Arsalidou M, Taylor MJ. Is 2+2=4? Meta-analyses of brain areas needed for numbers and calculations. NeuroImage. Feb 1 2011;54(3):2382-93. [CrossRef]
- Salatino A, Poncini M, George MS, Ricci R. Hunting for right and left parietal hot spots using single-pulse TMS: modulation of visuospatial perception during line bisection judgment in the healthy brain. Frontiers in psychology. 2014;5:1238. [CrossRef]
- Corbetta M, Shulman GL. Spatial neglect and attention networks. Annual review of neuroscience. 2011;34:569-99. [CrossRef]
- Corbetta M, Shulman GL. Control of goal-directed and stimulus-driven attention in the brain. Nature reviews Neuroscience. Mar 2002;3(3):201-15. [CrossRef]
- Ellison A, Schindler I, Pattison LL, Milner AD. An exploration of the role of the superior temporal gyrus in visual search and spatial perception using TMS. Brain : a journal of neurology. Oct 2004;127(Pt 10):2307-15. [CrossRef]
Table 1.
Patients’ Characteristics_Cognitive Mapping with nTMS.
Table 1.
Patients’ Characteristics_Cognitive Mapping with nTMS.
| Patients |
Sex |
Age |
Lesion† |
Scholarship |
Awake |
nTMS§ |
| P1 |
F |
60 |
GBM_Right Temporo-Occipital |
13 |
+ |
L/C/N |
| P1 |
F |
62 |
GBM_Right Temporo-Occipital (R) |
13 |
+ |
|
| P2 |
M |
58 |
Metastasis (Lung Adenok)_Left Parietal |
13 |
+ |
L/N |
| P3 |
F |
44 |
GBM_Right Parieto-Occipital |
15 |
+ |
L/C/N |
| P4 |
M |
66 |
GBM_Right Temporal |
8 |
- |
L/C/N |
| P5 |
F |
60 |
Cavernoma_Right Frontal |
8 |
failed |
L/C/N |
| P6 |
F |
50 |
Right Fronto-Temporo-Insular |
13 |
- |
L/C/N |
| P7 |
M |
68 |
GBM_Left Temporo-Occipital |
8 |
- |
L/C/N |
| P8 |
M |
73 |
GBM_Right Fronto-Temporo-Insular |
8 |
- |
L/C/N |
| P9 |
M |
21 |
GBM_Right Fronto-Parietal |
13 |
+ |
L/C/N |
| P10 |
M |
29 |
G2_Right Frontal |
16 |
- |
L/C/N |
| P11 |
M |
29 |
G2 Right Parietal |
18 |
- |
L/C/N |
| P12 |
M |
54 |
GBM_Right Fronto-Insular |
8 |
- |
L/C/N |
| P13 |
F |
61 |
G2_Right Frontal |
13 |
+ |
L/C/N |
| P14 |
F |
54 |
G2_Left Frontal |
13 |
+ |
L/C/N |
| P15 |
M |
52 |
Cavernoma_Right Temporal |
16 |
+ |
L/C/N |
| P16 EXCLUDED |
F |
50 |
Meningioma_Left Parieto-Occipital |
15 |
- |
L/C/N |
| P17 |
M |
23 |
Focal Cortical Dysplasia_Left Temporal |
13 |
- |
L/C/N |
| P18 |
F |
43 |
G3 _Left Parietal |
16 |
+ |
L/C/N |
| P19 |
M |
57 |
GBM_Right Temporo-Insular |
13 |
- |
L/C/N |
| P20 |
M |
33 |
G3_Left Parietal |
8 |
+ |
L/C/N |
| P21 |
F |
49 |
GBM_Right Temporo-Parieto-Occipital |
8 |
- |
L/C/N |
| P22 |
M |
47 |
GBM_Splenium Corpus Callosum |
13 |
- |
L/C/N |
| P22 |
M |
48 |
GBM_Splenium Corpus Callosum |
13 |
- |
|
| P23 |
F |
43 |
G2_Left Temporo-Insular |
8 |
failed |
L/C/N |
| P24 |
F |
44 |
*G3_Left Frontal |
16 |
+ |
L/C/N |
| P25 |
M |
44 |
*G2_Left Frontal |
16 |
+ |
L/C/N |
| P26 |
M |
67 |
GBM_Left Parietal |
13 |
+ |
|
| P26 |
M |
68 |
GBM_Left Parietal |
13 |
- |
L/C/N |
| P27 |
F |
71 |
*GBM_Right Parietal |
8 |
- |
L/C/N |
| P28 EXCLUDED |
M |
73 |
G3_Right parietal |
8 |
|
L/C/N |
| P29 |
F |
42 |
G3 Left parietal |
13 |
|
L/C/N |
Table 2.
Average values and average percentage of functionality values obtained from tests on patients with neglect. For the BELL and OCS tests, the mean values are reported divided by right and left hemisphere.
Table 2.
Average values and average percentage of functionality values obtained from tests on patients with neglect. For the BELL and OCS tests, the mean values are reported divided by right and left hemisphere.
| |
|
Average Score |
STD Score |
Averange functionality [%] |
| MMSE Pre op |
|
27.13 |
2.72 |
90.42 |
| MMSE Post op 4 D |
|
26.12 |
3.52 |
87.07 |
| MMSE Post op 30 D |
|
27.19 |
1.46 |
90.62 |
| Bell Pre op |
Left |
-2 |
2.60 |
94.29 |
| Right |
-1.375 |
1.41 |
96.07 |
| Bell Post op 4 D |
Left |
-9 |
9.97 |
74.29 |
| Right |
-1.67 |
1.89 |
95.24 |
| Bell Post op 30 D |
Left |
-0.4 |
0.49 |
98.86 |
| Right |
0 |
0 |
100 |
| Clock Pre op |
|
1.06 |
0.17 |
98.75 |
| Clock Post op 4 D |
|
2.39 |
1.54 |
72.22 |
| Clock Post op 30 D |
|
2 |
0.95 |
80 |
| Ocs Pre op |
Left |
-2.38 |
2.34 |
95.25 |
| Right |
-1.13 |
1.69 |
97.75 |
| Ocs Post op 4 D |
Left |
-7.4 |
11.96 |
85.2 |
| Right |
-3.4 |
3.95 |
93.2 |
| Ocs Post op 30 D |
Left |
-1 |
1.55 |
98 |
| Right |
-0.4 |
0.8 |
99.2 |
Table 3.
Results comparing DCS and nTMS points for Neglect.
Table 3.
Results comparing DCS and nTMS points for Neglect.
| |
DCS positive |
DCS negative |
TOTAL |
| nTMS positive |
22(TP) |
38(FP) |
60 |
| nTMS negative |
58(FN) |
476(TN) |
534 |
| TOTAL |
80 |
514 |
|
Table 4.
Statistical Results comparing nTMS and DCS Neglect points.
Table 4.
Statistical Results comparing nTMS and DCS Neglect points.
| Sensitivity (Se) |
11.93% |
| Specificity (Sp) |
91.21% |
| Positive Predictive Value (PPV) |
41.43% |
| Negative Predictive Value (NPV) |
66.07% |
| False Negative Rate (FNR) |
88.07% |
| False Positive Rate (FPR) |
08.78% |
| Accuracy |
63.69% |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).