1. Introduction
Influenza vaccination (IV) has become a challenge for different reasons: yearly vaccine program implementation, identification of the most suitable time for implementation, definition of high-risk groups, availability of vaccines at the appropriate time, and access to the correct type of vaccine, among others. Accessibility to and introduction of new vaccines or vaccines with higher immunogenicity using preexisting or new platforms that could provide better protection also represents a challenge for national immunization programs.
Data gathering for influenza vaccination before and during the COVID-19 pandemic has been complex, and in some cases, unavailable. Estimation of vaccine coverage among different groups is also a challenge, especially when the target population is not well known. For example, some countries do not have certain data of the number of patients with underlying conditions to estimate adequate coverage in these population. In pediatrics, this analysis could be less complex since most countries have accurate estimate data of different age cohorts. The challenge may be related to lack of registry of administered vaccine doses in older children and in those that receive primary vaccination at an older age [
1].
The COVID-19 pandemic had an important impact in vaccination programs, including seasonal influenza vaccine. In countries of South America (Argentina, Chile, and Uruguay), an increase in influenza vaccine administered doses was observed as a result of several factors: lack of COVID-19 vaccine at the beginning of the pandemic, a potential cross protection to SARS-CoV-2 infection with influenza vaccine, prevention of co-infections between viruses, especially in high-risk populations, and avoidance of influenza cases that could lead to hospitalizations or need of medical care.
In 2021, health authorities prioritized COVID-19 vaccine among high-risk groups over other vaccines. In that year, restrictive measures, and lack of knowledge about safety of concomitant vaccination, caused a decrease in influenza vaccine coverage in Argentina and Uruguay. Also, seasonality of influenza virus changed worldwide. In Argentina in 2022, an increase of influenza A (H3N2) circulation was observed during summer in January, with a reduction during winter, and increased cases of influenza B throughout the year. These variations in epidemiology with early viral circulation have possibly generated a reduction in the impact of the vaccine in South America and around the world.
Before the COVID-19 pandemic, there was better documentation of vaccination coverage in South America, so the impact that carried SARS-CoV-2 infection on influenza immunization is not accurate. Nevertheless, it is known that a decrease of coverage was observed in 2020 and 2021, with a recovery in Argentina and Uruguay during 2022. Changes in the number of influenza cases could also be affected by other external factors, such as: isolation of infected people and contacts, reduced collective activities, restriction of group activities, and migratory controls among others. Data regarding circulation of influenza before and during the pandemic was observed yearly and during the pandemic was closely followed and we see that as a good practice to be continued [
2].
Changes of influenza virus circulation reflected in the burden of disease, with reported lower rates of hospitalizations and mortality. An interaction between influenza virus, influenza vaccine, and COVID-19 has been reported, with an apparent association between lower risk of severe COVID-19 and influenza vaccination. A 10% increase in influenza vaccine coverage was associated with a 28% decrease in mortality associated with COVID-19 in the elderly. A study in 92,664 COVID-19 patients documented 8% reduction in Intensive Care Units admission, 18% reduction in ventilatory assistance, and 17% reduction in mortality in dose vaccinated against influenza. [
3] A potential immune modulation role is suspected.
Influenza vaccine introduction in South America and around the world had demonstrated to be effective reducing morbidity and mortality in high-risk groups. Vaccination has changed in time, with a progressive increase before 2020, a considerable decrease in coverage by 2021, and an apparent recovery by 2022 and 2023. Nevertheless, data in the region is scarce.
There are several limitations faced in the region to accomplish adequate vaccine coverage. Different health policies could become barriers for universal vaccination. Health care personnel and patient perception of disease can impact vaccine acceptance and campaigns success. Improvements in vaccine access and availability, incorporation of influenza vaccine to regular immunization programs, availability of better registration, and inclusion of new risk groups among immunization strategies, are among the goals to achieve better coverage.
There are several differences among influenza vaccination in South America. Although defined high-risk groups for IV are similar among countries, they may differ. Also, given the specific policies that every country has, there are several differences in implementation strategies and coverage rates.
2. Materials and Methods
In this paper, we sought to analyze the impact of the COVID-19 pandemic on influenza vaccination coverage in Latin America, specifically in Argentina, Chile, and Uruguay.
The information analyzed corresponded to administrative coverage of influenza vaccination in the countries included in the study, during the years 2018 to 2023. Coverage rates are expressed as a percentage of the corresponding population. Estimates of influenza vaccination coverage are for annual vaccination programs.
These sources used corresponded to those officially reported by PAHO/WHO and the Ministries of Health of the countries that are part of the research.
3. Results
3.1. Chile
In Chile, each year since 1982, the immunization department of the Ministry of Health organized an IV campaign with regional governments, health services, and health providers. It starts on March and accomplishes coverage close to 85% on high-risk groups by the end of the year [
4].
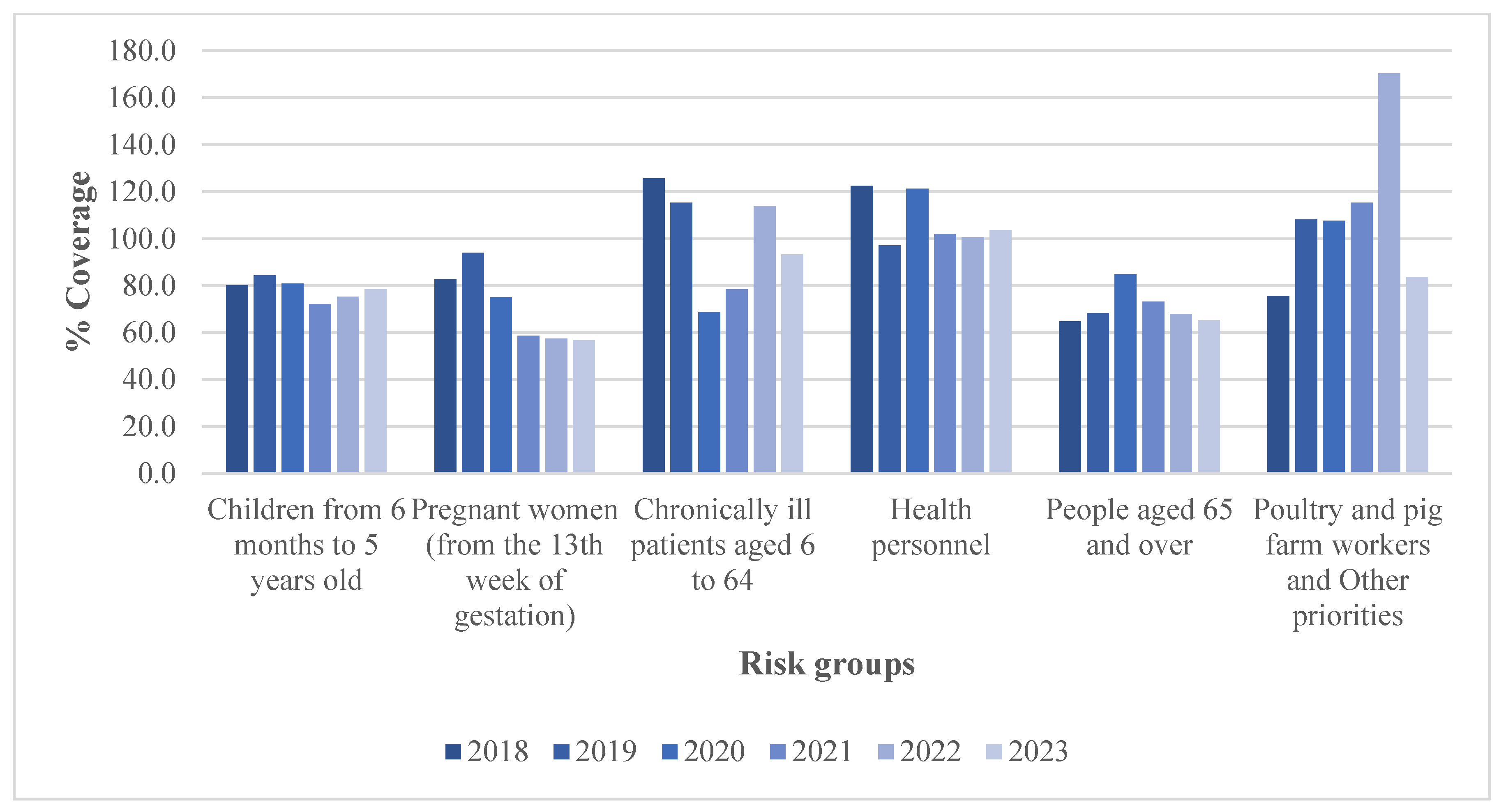
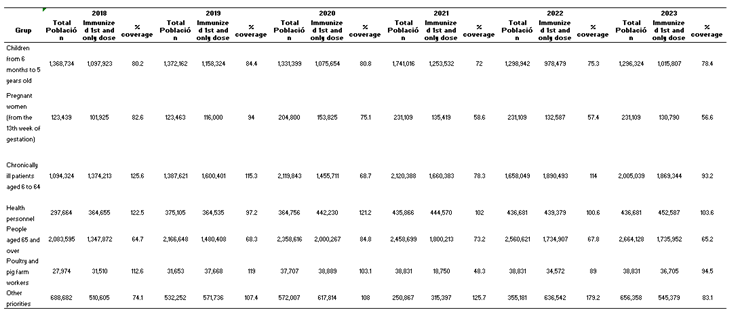
Due to demographic and epidemiological changes, and scientific advances on safety and immunogenicity of IV, the number of doses in the country are modified annually. High-risk population and vaccination objectives are dynamic, and coverage may be impacted, as shown in
Figure 1 [
4,
5].
For 2023, vaccine campaign against influenza in Chile is offered and directed to health care workers, pregnant women, children from six months to ten years of age, teachers, adults 65 years of age or older, pig and poultry farmers, preterm born infant families, families of immunocompromised children younger than six months of age, long-term facilities workers, and children and adults with underlying conditions (diabetes, chronic lung diseases, cardiopathies, neuromuscular disorders, hypertension, obesity, and kidney or hepatic disease) [
6].
Table 1 [
5]
Influenza vaccine coverage has changed before and during the pandemic. By 2014, coverage for children between six and 23 months of age was 72·2%, 75% for adults, 97% for pregnant women, and 100% for people with underlying conditions and health care workers [
1,
7]. In 2020, 98% of the targeted populations received vaccination, with more than 7 million doses administered among children, elderly, and pregnant women [
8]. Vaccination coverages for 2018-2023 are summarized in
Table 2 for the three countries [
9].
3.2. Uruguay
In Uruguay, influenza vaccination program has been developed in different stages to cover all groups of interest. For 2023, risk-groups in Uruguay have been determined as: adults older than 65 years of age, residents and workers of long-term care facilities, pregnant women, and mothers to infants younger than six months of age, inmates, refugees, health-care workers, and poultry farmers. For a second stage of vaccination, children younger than five years old, adolescents, and adults with comorbidities are included. In the final stage of vaccination, the general population is allowed to be vaccinated, even if they do not belong to the vaccination priority groups [
10]. For this period, a trivalent vaccine is used with the formulation recommended by the WHO.
Vaccine coverage in Uruguay has changed trough time. [
11] Vaccination rates between 2018-2023 are shown in
Table 2. In 2014, national report of vaccine coverage in children younger than 2 years was 47%, 82% in those between two and five years of age, 30% for adults, and 46% for health-care providers. [
1,
7,
12] Data for patients with underlying conditions is not available during that period of time.
3.3. Argentina
Vaccination against influenza started in Argentina in 1993 and was consolidated by 2010 after the H1N1 influenza pandemic trough the National Vaccination Campaign, using mono- and trivalent formulations. By 2011, IV was added to the national vaccination program, with the objective to decrease hospitalizations, complications, sequelae, and mortality.
The targeted population for 2023 is: health care workers, pregnant women, and those in the first ten days after pregnancy, infants between six and 24 months of age, adults with underlying conditions (chronic lung diseases, cardiac disease, immunodeficiencies, oncologic and hematologic diseases, obesity, diabetes, chronic renal disease, neuromuscular diseases, severe congenital malformations, and people living with high-risk patients), and elderly. Argentina uses a trivalent formulation, as recommended by the WHO.
Vaccine coverage in Argentina has also changed over time, and pre and post pandemic coverages has evolved. In 2010, coverages over 85% were reported in all risk groups, reaching 99% in health personnel and children and adults with comorbidities. An increased tendency is observed in coverage reports between 2011-23 in most risk groups according to data provided by the Ministry of Health. In 2014, 50% coverage was reported in children younger than two years of age, in contrast with 75% by 2019. By 2014, 90% coverage was reported in elderly, 84% in health-care workers, 35% in patients with comorbidities, and 96% in women during pregnancy [
1,
12].
Variation of vaccination coverage is evident. In Argentina a documented false perception in influenza burden of disease has spread trough years and increasing vaccine coverage in different risk groups has become a challenge (
Table 2) [
13].
Comparatively, vaccination coverage according to risk groups between Argentina, Chile, and Uruguay for the years 2018 to 2023 shows a decreasing trend without achieving optimal vaccination coverage. In Argentina, in 2018, coverage for children under five years of age decreased from 70% to 39% in 2022 and 63% in 2023. for the same years in children under five years of age, vaccination coverage in Chile decreased from 71% to 69% in 2022 and 70% in 2023; and in Uruguay from 24% to 2% in 2022 and 20% in 2023. For older persons, Argentina reported 103% in 2018, 76% in 2022 and 12% in 2023, Chile showed appropriate coverage in this group for 2020 with 85% and 70% for 2022 and 65% in 2023. Uruguay showed a low performance in coverage for this group in 2018 with 32% and 33% for 2022 and 2023. It is to be note an increase in vaccination rates in 2020 for all age groups and risk groups with the exemption of Uruguay in the under five Children group that reported 7%. For the pregnant women group, Argentina reported greater coverage in 2020 with 77%. Chile 90% in 2018 and Uruguay 55% in 2020. In the health care workers group the three countries reached their highest coverage in 2020 with over 100% coverage reported, and they reported a decrease by 2022, with the sharpest decrease in Uruguay that went from 136% in 2020, to 22% in 2022 and 19% in 2023 (
Table 2) High vaccination coverage is evident in health workers. It is important to strengthen actions to achieve an increase in coverage, especially in the at-risk population.
4. Discussion
Argentina, Chile and Uruguay report that they have a current influenza vaccination policy in their countries, which includes risk groups [
14].
Constant efforts to improve influenza vaccination coverage in Southern cone countries are performed. Chile, Uruguay, and Argentina efforts to improve vaccination seeking an increment of vaccine coverage as an objective.
Access to vaccines, availability for high-risk groups, broader campaigns, and more precise registry is necessary to accomplish this goal.
Chile, in its quest to strengthen actions to protect the population and due to the increase in influenza cases so far in 2024, as well as viral circulation in unusual times, expanded vaccine coverage to the entire population starting August 1, 2024 [
15].
The possibility of continuing using or introducing vaccines with higher immunogenicity is important in vulnerable population. For this purpose, cost-effective studies and logistics for implementation should be considered.
Being a demanded stationary vaccine, it is hard to predict the number of doses to be used. Demand varies depending on many circumstances, and planning starts one year before. Hence, the reports show those doses that were applied, and hence we can see the variability in the different target groups each country has defined.
Educational campaigns, building a stronger participation of certain group of medical specialists to reach targeted populations, i.e. obstetricians, cardiologist, pneumologists, geriatricians, for instance, might contribute to better coverage.
Starting in 2022, six countries in the region, including Chile and Uruguay, are collecting and analyzing surveillance and immunization data on Severe Acute Respiratory Infection (SARI) to generate the effectiveness of influenza and COVID-19 vaccines against hospitalizations [
14].
The 2030 immunization agenda, which was adopted by all countries, calls it "a global strategy to leave no one behind." Among its objectives, the agenda has to increase equitable access to new and existing vaccines and their use, as well as the contribution to universal coverage and sustainable development. Therefore, governments must unite efforts of continuous work and "friendly" vaccination campaigns adapted to the community to meet the goals in vaccination coverage [
16].
5. Conclusions
The influenza vaccine is the most effective way to prevent the disease and developing complications, especially in high-risk groups.
Although the countries studied have incorporated the flu vaccine into their vaccination schedules and worked to continue vaccination services during the COVID-19 pandemic, including Argentina and Chile, which have incorporated longer “winter campaigns” lasting more than 3 months in order to strengthen actions [
14], suboptimal vaccination coverage is evident, so a review of actions is suggested in order to improve said vaccination coverage.
Constant monitoring of vaccination coverage and the identification of factors related to non-vaccination or reluctance allow efforts to be directed towards promoting specific actions and ensuring that the population is vaccinated, helping to reduce morbidity and mortality caused by this disease.
The risk groups established, given the probability of developing the disease in a serious manner or death, such as pregnant women, older adults, children under 5 years of age, and patients with chronic diseases, had fluctuating coverage in all countries, below optimal coverage. Uruguay especially has this coverage for all groups in very low percentages.
According to the comprehensive analysis on morbidity and mortality associated with influenza and COVID-19 in the Region of the Americas (2010 to 2023), carried out by PAHO, it preliminarily showed that 70% of the region's population estimates almost 350,000 influenza-related hospitalizations annually [
17], indicating approximately 55 million cases of mild influenza illness per year in the Americas [
17], urging governments to improve vaccination coverage and reduce the burden of this disease in the countries of the region.
The influenza vaccine is a biological that is necessary throughout the life cycle. Immunizing the mother during pregnancy provides transplacental protection up to 6 months; from 6 months onwards, the baby can receive the vaccine through its regular schedule; after 5 years and in adulthood, although it is recommended for risk groups, it is a biological that can be applied at all ages, offering immunity through annual reapplication.
Since 2020, COVID-19 surveillance has been gradually integrated into ongoing surveillance of severe acute respiratory infections (SARI) and influenza-like illnesses (ILI), allowing for comprehensive analysis and monitoring of the behavior of influenza and influenza-like viruses.
According to the regional update report, Influenza and other respiratory viruses. Epidemiological Week (EW) 37 (September 20, 2024) [
18], in the Americas region, the activity of Influenza-like Illness (ILI) and Severe Acute Respiratory Infection (SARI) has shown a general downward trend in the last EW. Influenza activity has remained below the epidemic threshold in all countries. During this period according to the report, the predominant influenza viruses have been type A(H3N2), followed by A(H1N1)pdm09 and B/Victoria. Influenza activity in the countries of the study has shown that Argentina is at epidemic levels, showing a slight increase in the last two epidemiological weeks. In Chile, influenza remains below the epidemic threshold, however it has shown a slight increase in recent years and in Uruguay, influenza and SARS-CoV-2 activity has remained at low levels.
It is important to work together towards the development of electronic vaccination records and digital certificates, which would facilitate population monitoring and the strengthening of joint actions towards improving vaccination coverage.
Estimation of updated population denominators to adequately assess coverage by the Ministries of Health of the countries.
Author Contributions
C.E.T and F.B.P, conceptualized the revision and made substantial contributions and edits. P.B and F.B.P, wrote the original first draft. R.T.V and H.B.C, provided comments on the manuscript and adjusted the final manuscript. All authors participated in the draft revisions and in approving the final draft for submission. The authors accept responsibility for the decision to submit the article for publication.
Funding
This research was developed by the Global Health Consortium, Department of Global Health, Robert Stempel College of Public Health & Social Work Florida International University (Project ID 800017326).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained in the article.
Acknowledgments
Special gratitude to Dr. Fernando Bazzino for providing influenza vaccine coverage data from Uruguay.
Conflicts of Interest
The authors declare no conflicts of interest.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of their workplaces.
References
- Ropero-Alvarez AM, El Omeiri N, Kurtis HJ, Danovaro-Holliday MC, Ruiz-Matus C. Influenza vaccination in the Americas: Progress and challenges after the 2009 A(H1N1) influenza pandemic. Human Vaccines & Immunotherapeutics 2016; 12(8): 2206-14. [CrossRef]
- Pan American Health Organization PAHO. Regional Update, Influenza. Epidemiological Week 44. 2022. https://iris.paho.org/handle/10665.2/56730.
- Fink G, Orlova-Fink N, Schindler T, Grisi S, Ferrer AP, Daubenberger C, et al. Inactivated trivalent influenza vaccination is associated with lower mortality among patients with COVID-19 in Brazil. BMJ Evid Based Med 2020. [CrossRef]
- Bastias M, Avendano M, Munoz F, Brstilo I, Alvarez A, Burgos P, et al. Seasonal influenza campaign 2020 in the context of SARS-CoV-2 pandemic: an unprecedented public health experience in Chile. Rev Chilena Infectol 2021; 38(2): 178-184. 10.4067/S0716-10182021000200178.
- Campana de vacunacion de influenza - Dashboard 2018 - 2023. Departamento de Estadísticas e Información de Salud. Ministerio de Salud, gobierno de Chile. https://deis.minsal.cl/#tableros.
- Vacunacion contra la influenza. 2024. Ministerio de Salud de Chile. https://saludresponde.minsal.cl/vacunacion-contra-la-influenza-2024/.
- Gonzalez-Block MA, Diaz Portillo SP, Arroyo Laguna J, Comes Y, Crocco P, Fachel-Leal A, et al. Barriers and facilitators to influenza vaccination observed by officers of national immunization programs in South America countries with contrasting coverage rates. Cad Saude Publica 2022; 38(3): e00045721. [CrossRef]
- Gobierno destaca cobertura de vacunación contra la Influenza. 2020. Ministerio de Salud de Chile. https://www.minsal.cl/gobierno-destaca-cobertura-de-vacunacion-contra-la-influenza/.
- Cuevas A, Carmona Quiroz L, Thiers Shibar F, Mora Retamal E, Tapia Anazco V. Comparación de coberturas de Campaña Influenza entre los años 2018 y 2020 en Chile: Vacunación en tiempos de COVID-19. Revista de Estudiantes de Medicina del Sur 2021; 9(1). https://dialnet.unirioja.es/servlet/articulo?codigo=8538428.
- Comienza la campaña de vacunación antigripal 2023. Ministerio de Salud Publica de Uruguay. https://www.gub.uy/ministerio-salud-publica/comunicacion/noticias/comienza-campana-vacunacion-antigripal-2023.
- Quian J, Dibarboure H.; Álvarez R, Gutiérrez S, Aguirre M, Abad L, et al. Cobertura de vacunación antigripal en niños de Montevideo en el año 2010. Arch Pediatr Urug 2011; 82(4): 223-7. http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-12492011000400003.
- Vicari AS, Olson D, Vilajeliu A, Andrus JK, Ropero AM, Morens DM, et al. Seasonal Influenza Prevention and Control Progress in Latin America and the Caribbean in the Context of the Global Influenza Strategy and the COVID-19 Pandemic. Am J Trop Med Hyg 2021; 105(1): 93-101. [CrossRef]
- Gentile A, Paget J, Bellei N, Torres JP, Vazquez C, Laguna-Torres A, et al. et al. Influenza in Latin America: A report from the Global Influenza Initiative (GII). Vaccine 2019; 37(20): 2670-8. [CrossRef]
- Nogareda F, Gharpure R, Contreras M, Velandia M, et al. Seasonal influenza vaccination in the Americas: Progress and challenges during the COVID-19 pandemic. Vaccine 2023; 41(31): 4554-4560. [CrossRef]
- Gobierno de Chile. Ampliamos cobertura de vacuna contra la influenza para toda la población. Agosto 2, 2024. https://www.gob.cl/noticias/aumento-cobertura-vacuna-influenza-toda-poblacion-circulacion-virus-respiratorios/.
- World Health Organization. Immunization Agenda 2030: A Global Strategy To Leave No One Behind. https://www.who.int/publications/m/item/immunization-agenda-2030-a-global-strategy-to-leave-no-one-behind.
- World Health Organization. PAHO drives evidence-generation on the burden of influenza through strategic research initiatives. 30 March 2024. https://www.who.int/news/item/30-03-2024-paho-drives-evidence-generation-on-the-burden-of-influenza-through-strategic-research-initiatives.
- Pan American Health Organization PAHO – Institutional Repository for Information Sharing IRIS. Regional Update, Influenza and Other Respiratory Viruses. Epidemiological Week 37 (20 September 2024). https://iris.paho.org/handle/10665.2/61690?locale-attribute=es.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).