1. Introduction
The integrity of the plantar plate (PP) along with the support of the plantar fascia and the plantar flexor tendons is the key to maintaining the stability of the lesser metarso-phalangeal joints (MTPJ), especially during the propulsive phase of gait. Three main scenarios of PP rupture have been identified: acute traumatic rupture, chronic attritional rupture, and rheumatoid PP pathology [
1,
2]. In the early stages of the disease, conservative treatment to reduce and stabilize MTPJ may promote stabilization /scarring of the PP and reduce the risk of progression of deformity. However, patients do not usually present with early-stage disease, which often limits the role of conservative management. For severe cases that do not respond to conservative treatment, surgical treatment may be necessary.
The PP of the lesser MTPJs has been the subject of numerous investigations in the scientific literature; however, nowadays there is still controversy about the best surgical approach to treat the pathology, especially in the second MTPJ.
The common clinical presentation of the instability of the second MTPJ is characterized by chronic pain with positive drawer sing and different degrees of deformity in the second toe mainly. A very positive drawer test with increased vertical displacement and pain indicates a compromise in PP integrity [
3]. For decades, flexor tendon transfer has been considered the mainstay of treatment to stabilize the second subluxed MTPJ. However, in the past 10 years, primary PP repair has been advocated as an alternative approach to pathology. Here, we present two cases of chronic PP instability involving the second MTP joint resolved by flexor digitorum longus (FDL) transfers, metatarsal osteotomy, and interphalangeal arthrodesis. The results of the cases reported here, together with the available evidence, suggest that, in chronic PP tears, indirect repair with transfer of the flexor digitorum longus tendon (FDL) associated or not with metatarsal osteotomy, and proximal interphalangeal arthrodesis seems to be effective with clinical benefit and improved patient satisfaction [
4].
2. Case Reports
Case 1
A 64-year-old male presented with progressive metatarsalgia refractory to plantar orthosis after three years of treatment in the left foot. Physical examination of the second MTPJ showed little swelling, no second toe purchase, very positive drawer test, and fixed clawtoe without plantar hyperkeratosis. The weight-bearing anteroposterior radiographic examination shows a subluxed second MTPJ, dorsiflexion of the proximal phalanx, and degenerative proximal interphalangeal joint (
Figure 1). In the longitudinal ultrasound image, the extensive tear visible through dynamic dorsiflexion manoeuvres of the affected toe could be visualized as a focal hypoechoic distal defect. The surgical procedure proposed was flexor- to- extensor tendon transference associated with metatarsal osteotomy and interphalangeal arthrodesis. Using the dorsal approach, a curved S-shaped incision was made that extended the MTPJ to the proximal interphalangeal joint (PIPJ). The PIPJ was identified and the extensor tendon was transected and reflected proximally all the way to the MTPJ capsule. The collateral ligaments were then released, and the articular surfaces were minimally removed. Subsequently, the extensor tendon was removed from the Hood apparatus and the MTPJ capsule was incised and released using a McGlamry elevator to reduce contracture. Using a sagittal saw, a second metatarsal Weil osteotomy was performed to decompress MTPJ and to recompose the metatarsal parabola. The osteotomy was fixed in the desired position with one small snap-off self- tapping screw. With ankle plantarflexion to relieve tension and using a curved hemostat, FDL was identified and freed from the attachment of soft tissues and clamped and cut as distal as possible. The FDL was split longitudinally, and the tails passed in the medial and lateral aspects of the base of the proximal phalanx. With the toe placed in 20 degrees of plantar flexion of the MTPJ, the tails of the FDL were dorsally crossed and sutured with the appropriate tension and the desired rest position slightly distal to the base of the proximal phalanx. Subsequently, end-to-end proximal arthrodesis of the proximal interphalangeal joint was performed using an absorbable pin of polylactic acid. The extensor tendon was conveniently sutured and routine wound closure was performed. The postoperative compression dressing was applied and the patient was discharged home on the postoperative day. After a five-month follow-up period, the patient returned to normal function and has markedly improved the stability of the affected MTPJ in the absence of pain.
Case 2
A 54-year-old male presented with progressive pain in the second MTPJ of the left foot refractory to conservative treatments (orthosis, physical therapy, and infiltration with steroids). The patient had undergone surgery a year earlier for metatarsalgia and hallux valgus consisting of chevron and Akin osteotomy in the first ray, and Weil osteotomy and proximal interphalangeal arthrodesis in the second MTPJ. The physical examination of the second MTPJ showed little swelling and a very positive drawer test. Dorsoplantar radiological examination showed subluxed MTPJ, and magnetic resonance imaging (MRI) reported postoperative changes in the MTPJ joints of the hallux and second toe with residual hallux valgus. The second MTPJ MRI showed thinning/elongation with signal changes in the T2-weighted sequences, with evidence of partial tearing displaced laterally. No abnormalities were observed in the supporting structures of the joint or other related forefoot pathologies. The longitudinal US image showed a full-thickness PP tear visualized as a focal hypoechoic defect that extends through the substance of the distal plantar plate from the articular to the plantar surface of the plate (Figure 3). Surgical procedure consisting in flexor- to- extensor transference as described by Parrish was proposed [
5]. With a longitudinal incision on the plantar aspect of the second toe, the flexor tendon was released from its insertion at the inferior border of the distal phalanx. The tendon was split longitudinally and then, through a dorsal incision centered on the proximal phalanx, the FDL tails were passed medially and laterally and sutured dorsally at the base of the proximal phalanx. With the toe placed at 20 degrees of plantar flexion of the MTPJ, the flexor tendons were sutured together and attached to the Hood apparatus under light tension. After routine wound closure, a postoperative compression dressing was applied. After a follow-up period of three months, the patient returned to normal function and has markedly improved the stability of the affected MTPJ in the absence of pain.
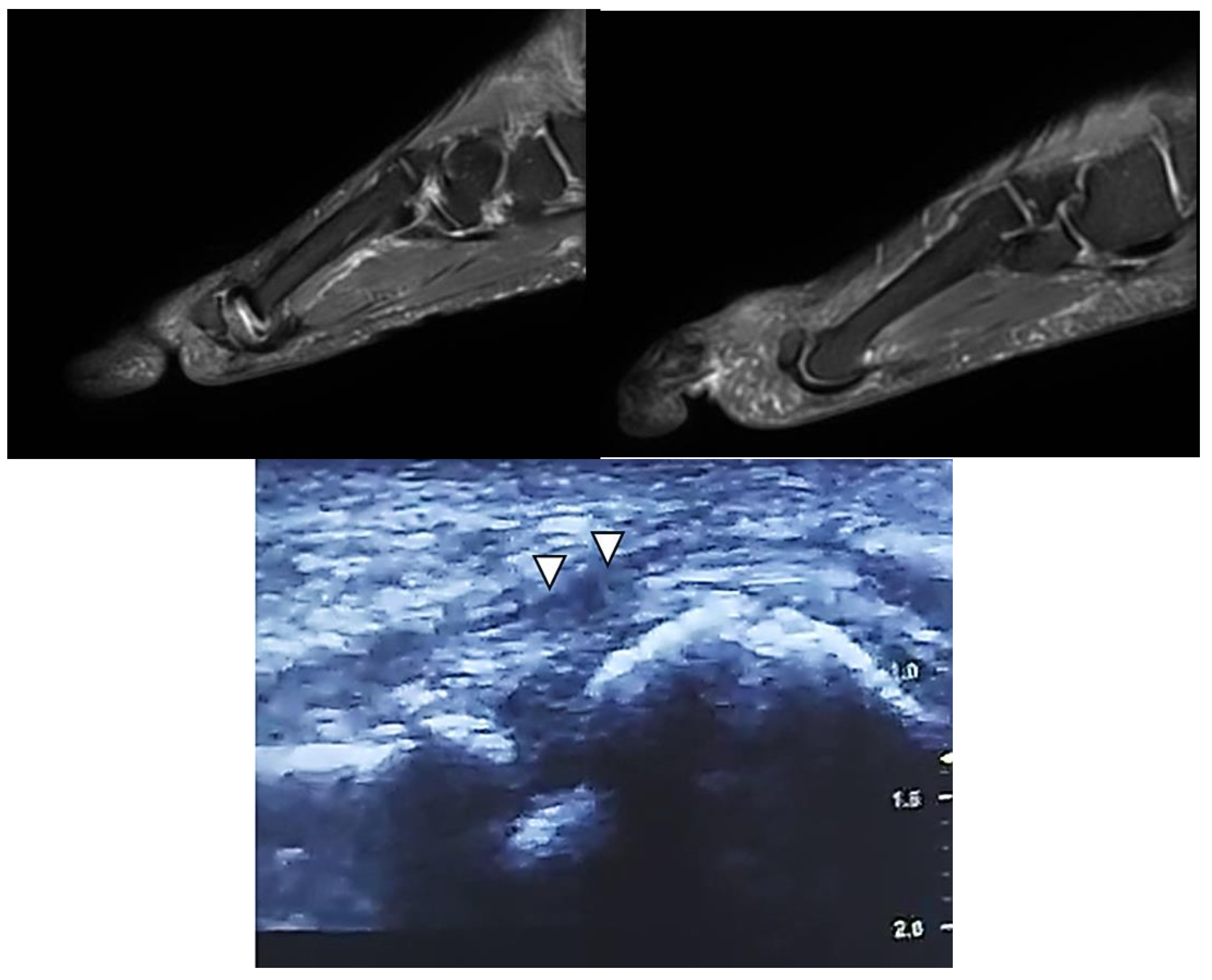
Figure 2.
Diagnostic images corresponding to Case 2. (Left) Second T2-weighted MTPJ MRI sequence, with evidence of partial tearing. (Right) Normal MRI image corresponding to the healthy third MTPJ of the same foot. (Bottom) Longitudinal ultrasound image showing the full-thickness PP tear (arrows) visualized as a focal hypoechoic defect that extends through the substance of the distal PP.
Figure 2.
Diagnostic images corresponding to Case 2. (Left) Second T2-weighted MTPJ MRI sequence, with evidence of partial tearing. (Right) Normal MRI image corresponding to the healthy third MTPJ of the same foot. (Bottom) Longitudinal ultrasound image showing the full-thickness PP tear (arrows) visualized as a focal hypoechoic defect that extends through the substance of the distal PP.
Figure 2.
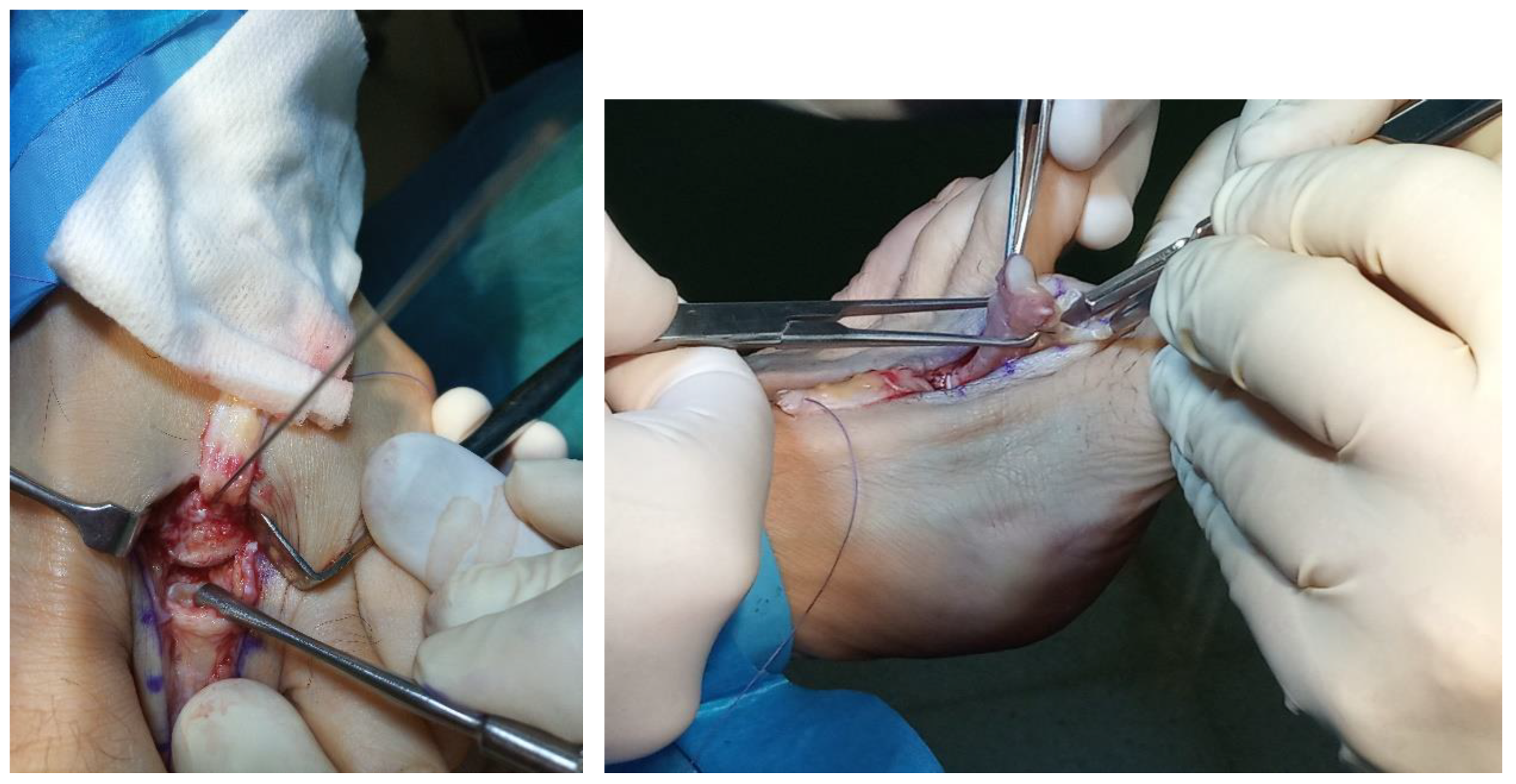
Sequence of surgical procedure and postoperative image after five days corresponding to Case 2.
Figure 2.
Sequence of surgical procedure and postoperative image after five days corresponding to Case 2.
3. Discussion
When the PP is injured, the plantar flexion mechanism is altered with a consequent instability of the MTPJ and a decrease in the plantar flexion strength. This causes a relative imbalance in which the dorsiflexors gain mechanical advantage, accentuating any already existing dorsiflexion toe deformity. In acute PP tears direct repair may be indicated; however, as in the presented cases, chronic PP tears can usually require balancing around the affected lesser MTPJ associated with the treatment of pathological conditions such as hallux valgus in an effort to reduce forefoot overload and pressure under affected lesser MTPJ. In subluxed MTPJ associated with PP tears, a shortening metatarsal osteotomy can be indicated. Some studies suggest that an increase in the second metatarsal protrusion distance together with an increase in the intermetatarsal angle measured on radiographs may correlate with PP injuries [
6,
7]. However, the surgical approach to the pathology must also ensure biomechanical restoration of the unstable MPJ and must address the underlying etiology and dysfunction of the MTPJ that produce the condition. In case 2, although the patient had undergone hallux valgus and hammer toe surgery with Weil osteotomy and interphalangeal toe arthrodesis, it is very likely that the results of the procedure were insufficient to achieve spontaneous healing of a chronic PP tear.
Currently, questions and debate remain about the healing capacity of PP. Cadaver studies in PP have demonstrated the presence of a vasculature network that extends from the surrounding soft tissues to the proximal and distal attachments. In the presence of torn PP, there is increased vascular density suggesting that PP is a structure that may attempt to heal [
8]. In the same way, chronic PP tears are characterized by attenuation and the presence of degenerative fibrous tissue inside their central portion that can make healing difficult [
9]. Clinical experience shows that when chronic PP tears occur, conservative treatment can eliminate symptoms and prevent progression of the deformity, but cannot achieve joint instability and realignment of the deformity of the toe without surgical intervention.
Different classifications have been proposed to define the instability of the second MTPJ describing the clinical progression of the deformity. The signs and symptoms characterized in the initial stage by MTPJ pain and swelling to a variable toe deformity that range from subluxed to dislocated joint [
10]. The positive drawer test or “positive Lachman” is the first objective sign of instability of the MTPJ [
11]. It is a reproducible test based on 5 grades (0= negative test to 4 = dislocated joint). As in both cases presented, the rigid grades III and IV are associated with important PP tears, the test being very positive [
12]. In both cases presented, the patients presented with incapacitating clinical symptoms characteristic of chronic disease. However, often in severe grade IV, PP tears are usually associated with minimal symptoms with several fixed MTPJ deformities (dislocated MTPJ).
Coughlin
et al. proposed a grading system of metatarsophalangeal PP tears that combined clinical findings and anatomical aspects of the associated PP tear. This classification correlates the location, shape, and size of the PP tear observed in cadaveric specimens with the clinical sing and symptoms observed in patients with PP tears [
3]. Other cadaver studies have allowed classification of the types and extent of plantar plate tears associated with increased deformity of the second toe [
13].
Although these classifications are the obvious academic interest, they may not always be precise or easy to establish clinically without the support of imaging probes. Physical examination is initially performed for diagnosis, but imaging can confirm clinical suspicion and play a key role in the management of pathology. High-resolution MRI or ultrasound (US) can confirm the presence of PP degeneration and tear and exclude other pathologies. The available evidence shows that MRI is the best option to provide additional information on the supporting structures of the joint; however dynamic US in the sagittal plane is more sensitive, suggesting that negative US virtually rule out a PP injury [
12]. In case 2, the second MTPJ MRI showed thinning/elongation with signal changes in the T2-weighted sequences, with evidence of important partial tearing, being laterally displaced. In both presented cases, the US examination showed a characteristic appearance compatible with a partial tear of the PP characterized by a focal anechoic defect with loss of echogenic granular texture in the lateral portion of the PP suggesting a partial thickness tear [
15,
16].
Currently, the surgical approach for the PP tear of the second MTPJ includes a variety of direct or indirect repair techniques with or without industry-driven devices. In the last decade, many surgical techniques have been described to manage MTPJ deformities by means of PP repair, but only some of them have been applied, relating treatment with the severity of PP injuries. Clinical experience and prospective clinical studies show that in patters of PP injured grade 0 (attenuation) and grade 1 (little transverse distal tear), conservative treatments or soft tissue releases and joint decompression with or without shortening metatarsal osteotomies are effective with improved clinical results and can encourage spontaneous of PP [
17]. Although direct repair could be justified for an isolated acute event or in cases of grade II tears, in grade III and IV cases (chronic PP tears) such as those presented here, with evident instability in the MTPJ and the presence of degenerative fibrous tissue within the middle or distal portion of the PP, or grade IV with extensive damage, direct repair is not viable.
To date, the most consistently successful salvage procedure is considered an indirect technique to reestablishing MTPJ instability with flexor to extensor tendon transfer with or without Weil osteotomy [
18]. While surgical treatment should be individualized, available evidence shows that overall patient satisfaction levels remain high when performed with the proper indications and concomitantly with other procedures [
19]. The transfer of the FDL to extensor tendon is considered an appropriate procedure for grade III and IV tears.
Taylor is the first author to be credited with performing a long and short flexor transfer into the extensor Hood for correction of claw toes that Girdleston previously had described for flexible toe deformities associated with neuromuscular disorders [
20]. Later, Parrish reported a modification of the original technique, transferring only the FDL and splitting it, passing each half of the tendon through each side of the proximal phalanx [
5]. Most recently, other authors have modified this technique, and now there are various approaches with a single dorsal incision, two or three incisions, and FDL tenodesis to the proximal phalanx [
20,
21]. The approaches for specific tendon transfer, depending on other procedures being concomitantly performed, previous procedures or severity and complexity of the deformity. In one of the cases presented, the technique was performed with a single dorsal incision that allowed metatarsal osteotomy, tendon transposition, and arthrodesis to be performed simultaneously. However, in the second case where only the tendon transposition was performed, the two-incision technique was considered adequate. The main complication reported in the literature with the technique is the risk of postoperative stiffness of the MTPJ [
12]. To avoid this, the tendon should be transferred under physiological tension and after performing the procedure, the position of the MTPJ should be evaluated and, where appropriate, a lengthening or extensor tenotomy should be performed.