Submitted:
25 September 2024
Posted:
26 September 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Research Problem
- ▶
- Operational effectiveness: it has not been systematically evaluated whether the current structure and composition of CEAs in Chile are optimal for addressing emerging ethical dilemmas in modern clinical practice (Beca, 2011).
- ▶
- Impact on clinical decision-making: there is a lack of evidence on how the recommendations of CEAs influence medical decisions and patient health outcomes (Agich, 2009).
- ▶
- Educational and policy role: The role of CEAs in ethics education of healthcare personnel and institutional policy development has not been explored in depth (Doran et al., 2016).
- ▶
- Adaptability to new challenges: The capacity of Chilean CEAs to address emerging ethical issues related to new medical technologies and global health challenges is unknown (Jonsen, 2015).
- ▶
- Perception and utilization: There is a lack of information on how healthcare personnel and patients perceive and use CEA services (Gaudine et al., 2011).
Objectives
- To analyze the current structure and functioning of the CEA in Chile.
- To evaluate the effectiveness of the CEA in the resolution of ethical dilemmas in clinical practice.
- To propose recommendations to improve public health care management through the CEA.
Materials and Methods
Study Design
Study Site
Inclusion criteria:
- ▶
- Documents and records of the CEA of the Clinical Hospital of the University of Chile since its implementation until 2021.
- ▶
- Annual reports and statistics of the CEA.
- ▶
- Ethical cases analyzed by the committee.
Exclusion criteria:
- ▶
- Incomplete or illegible documents.
- ▶
- Ethical cases that were not formally presented to the CEA.
- ▶
- CEA members who participated for less than one year in the committee.
Data collection tools:
- ▶
- Documentary review: annual reports, meeting minutes, and CEA case records were analyzed.
- ▶
- Semi-structured interviews: Interviews were conducted with current and past members of the CEA to obtain information on its functioning and challenges.
- ▶
- Non-participant observation: CEA meetings were attended (with proper consent) to observe its working dynamics.
Study variables:
- ▶
- Composition of the CEA (number of members, disciplines represented).
- ▶
- Functions performed by the CEA.
- ▶
- Number and type of cases analyzed annually.
- ▶
- Methodology of the committee's work.
- ▶
- Challenges and constraints identified by members.
- ▶
- Perceived impact of CEA recommendations on clinical practice.
Data analysis:
Results
-
Composition and Structure:
- ▶
- CEAs in Chile are composed of an average of 9 members, representing diverse disciplines including medicine, nursing, social work, law, and community representatives.
- ▶
- Members' terms of office have a standard duration of three years, with the possibility of renewal.
-
Functions and Activities:
- ▶
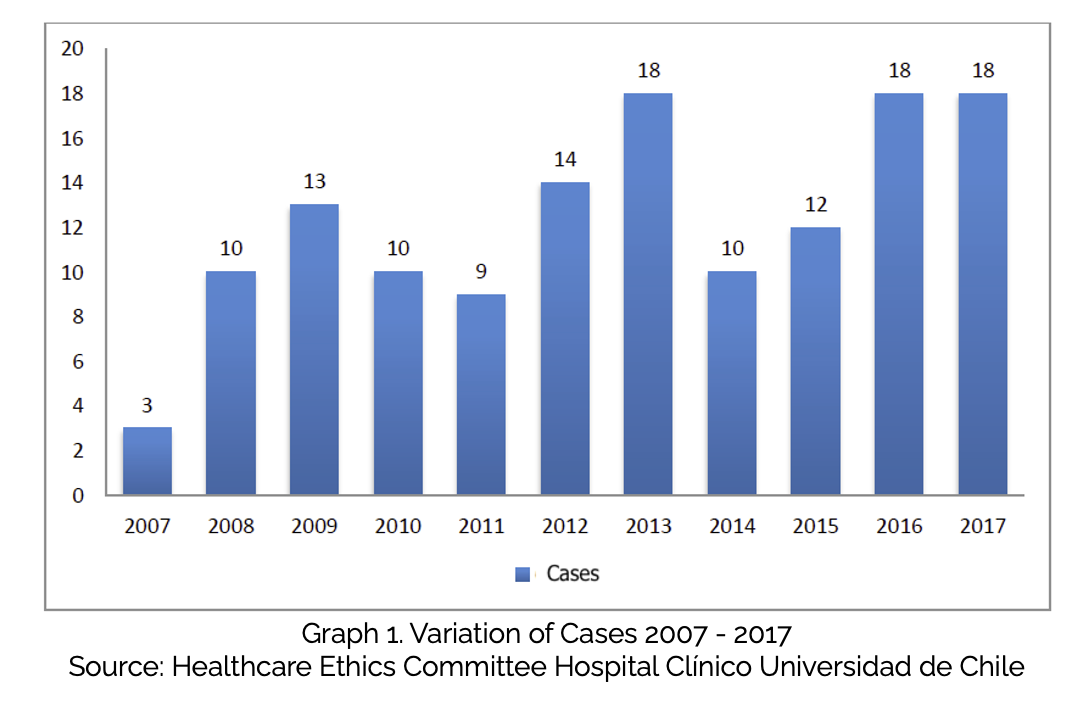
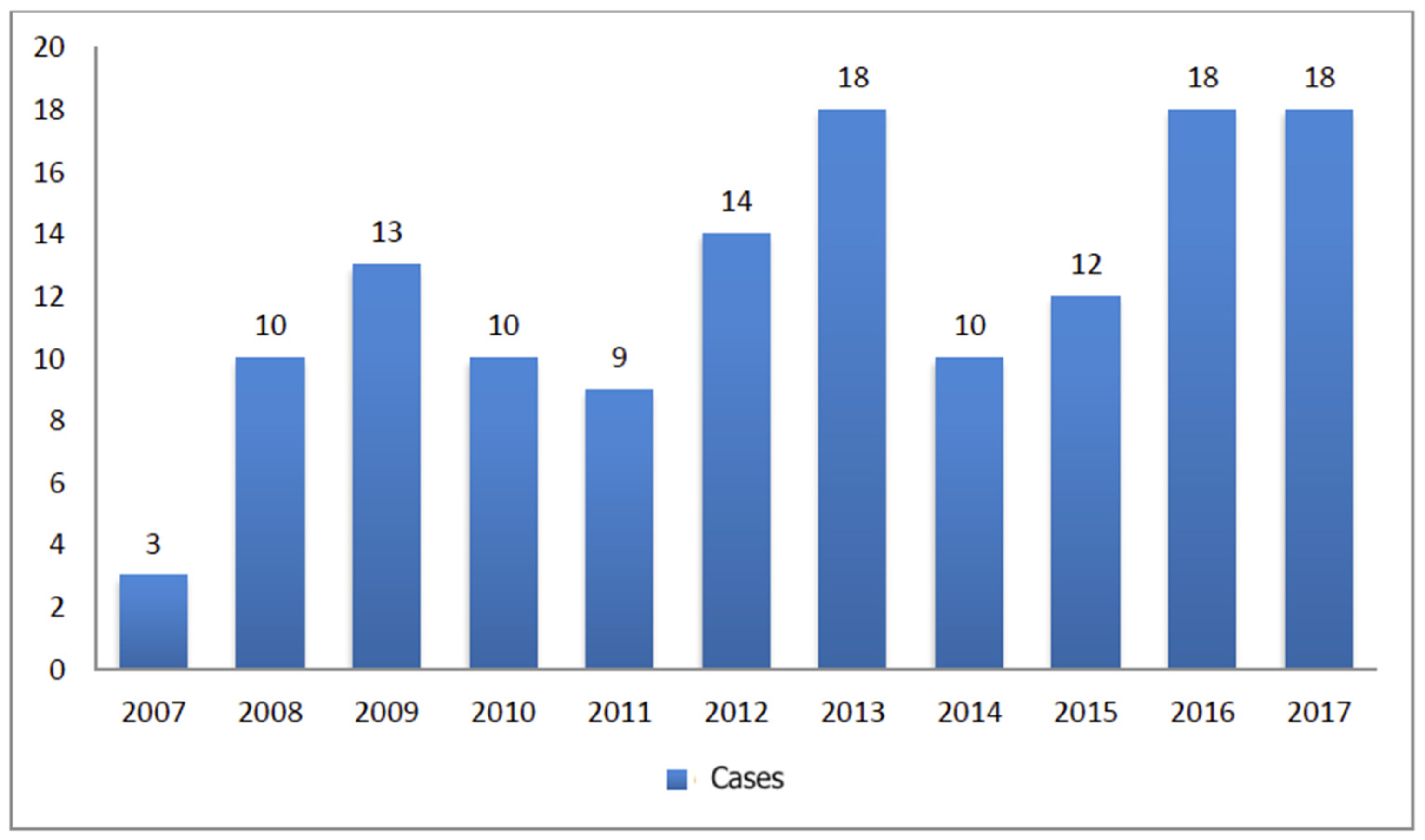
- The advisory function is the most developed, with a steady increase in the number of cases handled annually. In the case of the Hospital Clínico de la Universidad de Chile, an increase from 3 cases in 2007 to 18 cases in 2017 was observed
- ▶
- As can be seen in Graph 1, the cases consulted have been growing in number and complexity in a sustained manner (among other reasons due to the strict application of the regulatory framework on the rights of patients, the new technologies available to the Hospital, etc.). To date, there has been a change in the consultation modality, in which approximately one-third of them must be resolved in extraordinary meetings, that is, immediately and in the patient's room.
- ▶
- The most recurrent topics in the consultations include a) Analysis of therapeutic proportionality b) Limitation and/or adequacy of therapeutic effort c) Conflicts in medical decision-making d) Issues related to transplants and retransplants e) Maternity and perinatal ethics cases.
-
Working Methodology:
- ▶
- A deliberative approach to case analysis has been adopted, involving detailed fact-finding, identification of conflicting values, and proposal of concrete courses of action.
- ▶
- There was a growing trend towards urgent inquiries, which require responses within 24 hours.
-
Normative and Educational Functions:
- ▶
- Although less developed than the consultative function, significant activities were identified in these areas, including the development of internal regulations and participation in training programs for healthcare personnel.
-
Challenges Identified:
- ▶
- A need was noted to improve the visibility and accessibility of CEAs within healthcare institutions.
- ▶
- Ongoing bioethics training for committee members was identified as a crucial factor in maintaining the quality of deliberations and recommendations.
Discussion
Conclusions
- ▶
- Strengthening continuing education: Implement structured continuing education programs in bioethics for CAA members, ensuring that they are updated on the latest trends and debates in the field.
- ▶
- Improving visibility and accessibility: Develop effective communication strategies to increase the visibility of CAAs within healthcare institutions and facilitate access to their services by healthcare personnel and patients.
- ▶
- Expansion of regulatory and educational roles: Encourage a more active role for CAAs in institutional policy development and ethics education of healthcare personnel, drawing on their accumulated experience in resolving complex cases.
- ▶
- Adapting to emerging challenges: Develop the capacity of CAAs to address emerging ethical issues related to new medical technologies, climate change, and other global health challenges.
- ▶
- Systematic impact assessment: Implement monitoring and evaluation mechanisms to measure the actual impact of CEA recommendations on clinical practice and patient health outcomes.
- ▶
- Inter-institutional collaboration: Encourage the creation of collaborative networks between CEAs from different institutions to share experiences and best practices.
- ▶
- Inclusion of the patient perspective: Develop mechanisms to more effectively incorporate the voice and experiences of patients in the deliberations and recommendations of CEAs.
Limitations of the Study
- Limited generalizability: Being a single case study focused on the Hospital Clínico de la Universidad de Chile, the results may not be fully generalizable to other hospitals or contexts within the Chilean health system.
- Temporal bias: The study is based on historical data up to 2017, which may not reflect recent changes in the structure or functioning of the CEA.
- Lack of quantitative measurement of impact: The study did not include quantitative measurements of the direct impact of CEA recommendations on clinical outcomes.
- Absence of patient perspective: The study did not directly include the views or experiences of patients who have been affected by CEA decisions.
Significance Statement
- It contributes to filling a gap in the literature on the practical functioning of CEAs in the Chilean context.
- It offers valuable insights into the challenges and opportunities for improving the effectiveness of CEAs in public health care management.
- Provides evidence-based recommendations to strengthen the role of CAAs in promoting an ethical culture in the health system.
- Emphasizes the importance of continuing education in bioethics and the need to adapt CEAs to emerging challenges in public health.
- It lays the groundwork for future research on the impact of CEA on clinical practice and patient health outcomes.
Author Contributions
References
- Agich, G. J. (2009). The issue of expertise in clinical ethics. Diameters, 22, 3-20. [CrossRef]
- Barra Novoa, R. (2021). Nueva Economía en tiempos de crisis: Una aproximación teórica a la transformación tecnológica y social. Journal of Management & Business Studies, 3(1), 1-13. [CrossRef]
- Beca, J. P. (2011). Clinical ethics consultants: reasons, advantages and limitations. Revista médica de Chile, 139(6), 815-819. [CrossRef]
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. [CrossRef]
- Charmaz, K. (2014). Constructing grounded theory. Sage. [CrossRef]
- Creswell, J. W., & Creswell, J. D. (2017). Research design: Qualitative, quantitative, and mixed methods approaches. Sage publications.
- Doran, E., Fleming, J., Jordens, C., Stewart, C. L., Letts, J., & Kerridge, I. H. (2016). Managing ethical issues in patient care and the need for clinical ethics support. Australian Health Review, 40(3), 286-290 . [CrossRef]
- Gaudine, A., Thorne, L., LeFort, S. M., & Lamb, M. (2011). Evolution of hospital clinical ethics committees in Canada. Journal of Medical Ethics, 37(12), 730-735. [CrossRef]
- Jonsen, A. R. (2015). Bioethics beyond the headlines: Who lives? Who dies? Who decides? Rowman & Littlefield.
- Novoa, RB (2021). Estado del arte y futuras aplicaciones de la salud digital en Chile. Revista Internacional de Salud y Ciencias Médicas , 4 (3), 355-361. [CrossRef]
- Petersen, A. (2013). From bioethics to a sociology of bio-knowledge. Social Science & Medicine, 98, 264-270 . [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




