Submitted:
07 August 2024
Posted:
09 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Material and Methods
2.1. Research Question
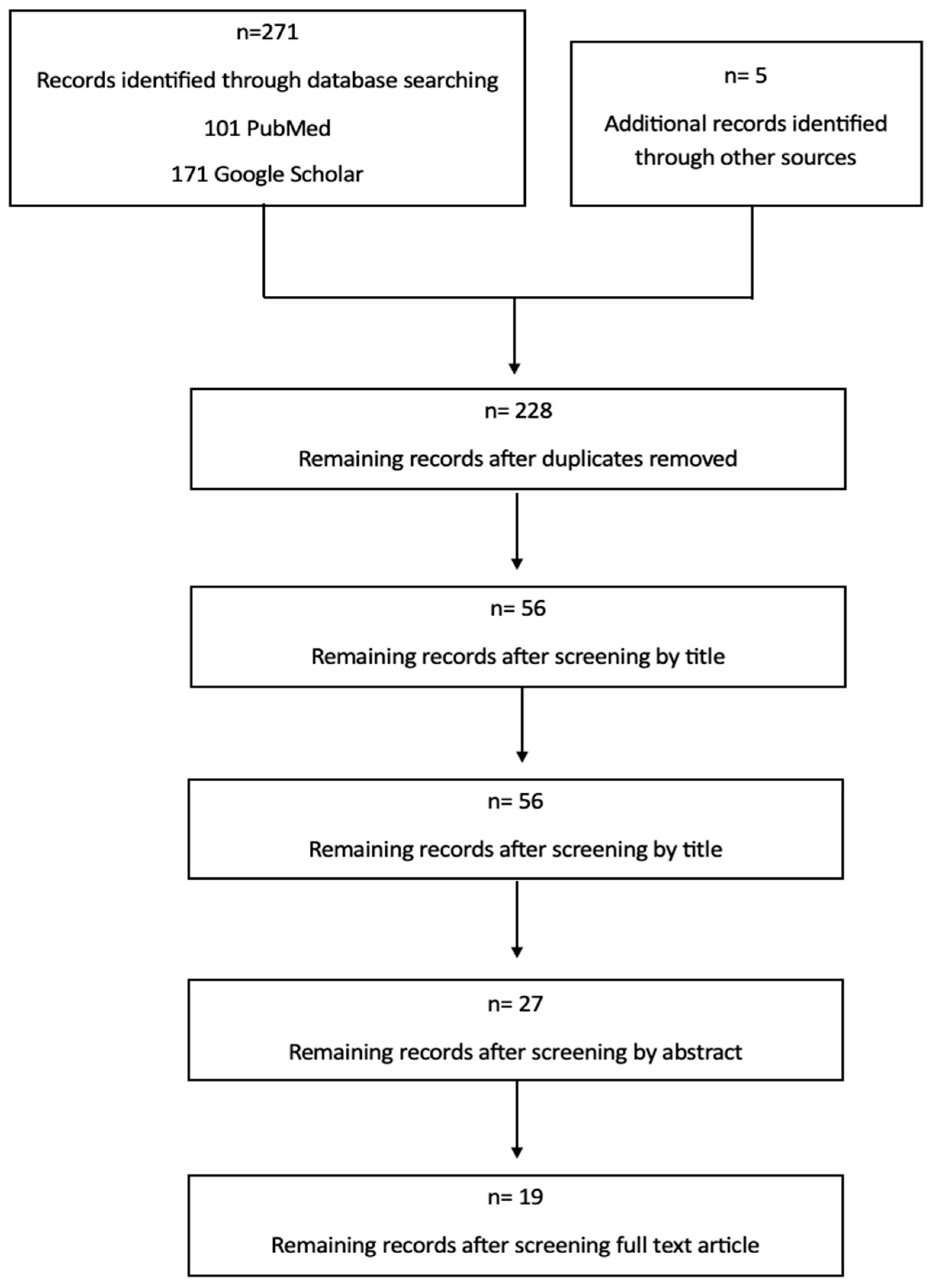
2.2. Search Strategy
2.3. Selection Criteria and Information Analysis
3. Results
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- ERA-Registry-Annual-Report-2021_231206.pdf.
- nited States Renal Data System. 2023 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2023.
- Registro Español de Enfermos Renales. Informe de Diálisis y Trasplante 2023. Sociedad Española de Nefrología [INTERNET]. Available from: https://www.senefro.org/contents/webstructure/SEN_2023_REER_V2_1_.pdf.
- Domenick Sridharan N, Fish L, Yu L, Weisbord S, Jhamb M, Makaroun MS, et al. The associations of hemodialysis access type and access satisfaction with health-related quality of life. J Vasc Surg. 2018 Jan;67(1):229–35.
- de Arriba G, Gutiérrez Avila G, Torres Guinea M, Moreno Alia I, Herruzo JA, Rincón Ruiz B, et al. La mortalidad de los pacientes en hemodiálisis está asociada con su situación clínica al comienzo del tratamiento. Nefrología. 2021 Jul 1;41(4):461–6.
- Ibeas J, Roca-Tey R, Vallespín J, Moreno T, Moñux G, Martí-Monrós A, et al. Spanish Clinical Guidelines on Vascular Access for Haemodialysis. Nefrologia. 2017 Nov;37 Suppl 1:1–191.
- Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020 Apr;75(4 Suppl 2):S1–164. [CrossRef]
- Poinen K, Quinn RR, Clarke A, Ravani P, Hiremath S, Miller LM, et al. Complications From Tunneled Hemodialysis Catheters: A Canadian Observational Cohort Study. Am J Kidney Dis. 2019 Apr;73(4):467–75. [CrossRef]
- Ravani P, Palmer SC, Oliver MJ, Quinn RR, MacRae JM, Tai DJ, et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol. 2013 Feb;24(3):465–73.
- Murea M, Gardezi AI, Goldman MP, Hicks CW, Lee T, Middleton JP, et al. Study protocol of a randomized controlled trial of fistula vs. graft arteriovenous vascular access in older adults with end-stage kidney disease on hemodialysis: the AV access trial. BMC Nephrol. 2023 Feb 24;24(1):43. [CrossRef]
- Nassar GM, Ayus JC. Infectious complications of the hemodialysis access. Kidney Int. 2001 Jul;60(1):1–13. [CrossRef]
- Ng Y-Y, Hung Y-N, Wu S-C, Ko P-J. Characteristics and 3-year mortality and infection rates among incident hemodialysis patients with a permanent catheter undergoing a first vascular access conversion. Clin Exp Nephrol. 2014 Apr;18(2):329–38. [CrossRef]
- Pisoni RL, Zepel L, Port FK, Robinson BM. Trends in US Vascular Access Use, Patient Preferences, and Related Practices: An Update From the US DOPPS Practice Monitor With International Comparisons. Am J Kidney Dis. 2015 Jun 1;65(6):905–15. [CrossRef]
- Shah S, Leonard AC, Meganathan K, Christianson AL, Thakar CV. Gender and Racial Disparities in Initial Hemodialysis Access and Outcomes in Incident End-Stage Renal Disease Patients. Am J Nephrol. 2018 Jul 10;48(1):4–14. [CrossRef]
- MacRae JM, Clarke A, Ahmed SB, Elliott M, Quinn RR, James M, et al. Sex differences in the vascular access of hemodialysis patients: a cohort study. Clin Kidney J. 2021 May;14(5):1412–8. [CrossRef]
- Beaumier M, Ficheux M, Couchoud C, Lassalle M, Launay L, Courivaud C, et al. Is there sex disparity in vascular access at dialysis initiation in France? A mediation analysis using data from the Renal Epidemiology and Information Network registry. Clin Kidney J. 2022 Nov;15(11):2144–53. [CrossRef]
- Lok CE, Rajan DK, Clement J, Kiaii M, Sidhu R, Thomson K, et al. Endovascular Proximal Forearm Arteriovenous Fistula for Hemodialysis Access: Results of the Prospective, Multicenter Novel Endovascular Access Trial (NEAT). Am J Kidney Dis. 2017 Oct 1;70(4):486–97. [CrossRef]
- Hull JE, Jennings WC, Cooper RI, Waheed U, Schaefer ME, Narayan R. The Pivotal Multicenter Trial of Ultrasound-Guided Percutaneous Arteriovenous Fistula Creation for Hemodialysis Access. J Vasc Interv Radiol. 2018 Feb;29(2):149-158.e5. [CrossRef]
- Kitrou PM, Balta L, Papachristou E, Papasotiriou M, Katsanos K, Theofanis M, Papadoulas S, Anagnostopoulos F, Georgopoulou GA, Goumenos D, Karnabatidis D. Percutaneous Arteriovenous Fistula Creation with the WavelinQ 4-French EndoAVF System: A Single-Center Retrospective Analysis of 30 Patients. J Vasc Interv Radiol [Internet]. Available from: http://dx.doi.org/10.1016/j.jvir.2021.09.021. [CrossRef]
- Shahverdyan R, Beathard G, Mushtaq N, Litchfield TF, Nelson PR, Jennings WC. Comparison of Outcomes of Percutaneous Arteriovenous Fistulae Creation by Ellipsys and WavelinQ Devices. J Vasc Interv Radiol. 2020 Sep;31(9):1365–72. [CrossRef]
- Zemela MS, Minami HR, Alvarez AC, Smeds MR. Real-World Usage of the WavelinQ EndoAVF System. Ann Vasc Surg. 2021 Jan;70:116–22. [CrossRef]
- Berland TL, Clement J, Griffin J, Westin GG, Ebner A. Endovascular Creation of Arteriovenous Fistulae for Hemodialysis Access with a 4 Fr Device: Clinical Experience from the EASE Study. Ann Vasc Surg. 2019 Oct;60:182–92. [CrossRef]
- Inston N, Khawaja A, Tullett K, Jones R. WavelinQ created arteriovenous fistulas versus surgical radiocephalic arteriovenous fistulas? A single-centre observational study. J Vasc Access. 2020 Sep;21(5):646–51. [CrossRef]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71.
- Hecking M, Bieber BA, Ethier J, Kautzky-Willer A, Sunder-Plassmann G, Säemann MD, et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the Dialysis Outcomes and Practice Patterns Study (DOPPS). PLoS Med. 2014 Oct;11(10):e1001750. [CrossRef]
- Caplin N, Sedlacek M, Teodorescu V, Falk A, Uribarri J. Venous access: women are equal. Am J Kidney Dis. 2003 Feb;41(2):429–32. [CrossRef]
- Silpe J, Koleilat I, Yu J, Kim YH, Taubenfeld E, Talathi S, et al. Sex disparities in hemodialysis access outcomes: A systematic review. Semin Vasc Surg. 2023 Dec;36(4):560–70. [CrossRef]
- Hoffstaetter T, Silpe J, Delijani D, Landis GS, Etkin Y. Sex Disparities in Arteriovenous Fistula Maturation Outcomes. Ann Vasc Surg. 2023 Sep;95:197–202. [CrossRef]
- Miller CD, Robbin ML, Allon M. Gender differences in outcomes of arteriovenous fistulas in hemodialysis patients. Kidney Int. 2003 Jan;63(1):346–52. [CrossRef]
- Angelici L, Marino C, Umbro I, Bossola M, Calandrini E, Tazza L, et al. Gender Disparities in Vascular Access and One-Year Mortality among Incident Hemodialysis Patients: An Epidemiological Study in Lazio Region, Italy. J Clin Med Res [Internet]. 2021 Oct 30;10(21). Available from: http://dx.doi.org/10.3390/jcm10215116. [CrossRef]
- Arhuidese IJ, Faateh M, Meshkin RS, Calero A, Shames M, Malas MB. Gender-Based Utilization and Outcomes of Autogenous Fistulas and Prosthetic Grafts for Hemodialysis Access. Ann Vasc Surg. 2020 May;65:196–205. [CrossRef]
- Lauvao LS, Ihnat DM, Goshima KR, Chavez L, Gruessner AC, Mills JL Sr. Vein diameter is the major predictor of fistula maturation. J Vasc Surg. 2009 Jun;49(6):1499–504. [CrossRef]
- Marcus RJ, Marcus DA, Sureshkumar KK, Hussain SM, McGill RL. Gender differences in vascular access in hemodialysis patients in the United States: developing strategies for improving access outcome. Gend Med. 2007 Sep;4(3):193–204. [CrossRef]
- McGill RL, Lacson E. Sex, race, and hemodialysis vascular access processes. J Vasc Access. 2017 Mar 21;18(2):132–8. [CrossRef]
- Allon M, Lockhart ME, Lilly RZ, Gallichio MH, Young CJ, Barker J, et al. Effect of preoperative sonographic mapping on vascular access outcomes in hemodialysis patients. Kidney Int. 2001 Nov;60(5):2013–20. [CrossRef]
- Lee T, Barker J, Allon M. Associations with predialysis vascular access management. Am J Kidney Dis. 2004 Jun;43(6):1008–13. [CrossRef]
- Peterson WJ, Barker J, Allon M. Disparities in fistula maturation persist despite preoperative vascular mapping. Clin J Am Soc Nephrol. 2008 Mar;3(2):437–41. [CrossRef]
- Kim J-K, Jeong JH, Song YR, Kim HJ, Lee WY, Kim KI, et al. Obesity-related decrease in intraoperative blood flow is associated with maturation failure of radiocephalic arteriovenous fistula. J Vasc Surg. 2015 Oct;62(4):1010-1017.e1. [CrossRef]
- Kats M, Hawxby AM, Barker J, Allon M. Impact of obesity on arteriovenous fistula outcomes in dialysis patients. Kidney Int. 2007 Jan;71(1):39–43. [CrossRef]
- Raulli SJ, Sather K, Dicken QG, Farber A, Kalish JA, Eslami MH, et al. Higher body mass index is associated with reinterventions and lower maturation rates after upper extremity arteriovenous access creation. J Vasc Surg. 2021 Mar;73(3):1007–15. [CrossRef]
- Delgado Ramírez A, Latorre López LI, Ruiz García E, Crespo Montero R. Factores que influyen en la supervivencia de la fístula arteriovenosa interna y su relación con la técnica de punción. Enferm Nefrol. 2016 Sep 15;19(3):215–30.
- Chan SM, Weininger G, Langford J, Jane-Wit D, Dardik A. Sex Differences in Inflammation During Venous Remodeling of Arteriovenous Fistulae. Front Cardiovasc Med. 2021 Jul 21;8:715114. [CrossRef]
- Dember LM, Imrey PB, Duess M-A, Hamburg NM, Larive B, Radeva M, et al. Vascular Function at Baseline in the Hemodialysis Fistula Maturation Study. J Am Heart Assoc [Internet]. 2016 Jul 22;5(7). Available from: http://dx.doi.org/10.1161/JAHA.116.003227. [CrossRef]
- Valdivielso JM, Jacobs-Cachá C, Soler MJ. Sex hormones and their influence on chronic kidney disease. Curr Opin Nephrol Hypertens. 2019 Jan;28(1):1–9. [CrossRef]
- Satam K, Ohashi Y, Thaxton C, Gonzalez L, Setia O, Bai H, et al. Sex hormones impact early maturation and immune response in the arteriovenous fistula mouse model. AMERICAN JOURNAL OF PHYSIOLOGY HEART AND CIRCULATORY PHYSIOLOGY [ISSN: 0363-6135] [ISSN: 1522-1539] [Internet]. 2023; Available from: http://dx.doi.org/10.1152/ajpheart.00049.2023. [CrossRef]
- Mallios A, Bourquelot P, Franco G, Hebibi H, Fonkoua H, Allouache M, et al. Midterm results of percutaneous arteriovenous fistula creation with the Ellipsys Vascular Access System, technical recommendations, and an algorithm for maintenance. J Vasc Surg. 2020 Dec;72(6):2097–106. [CrossRef]
- Beathard GA, Litchfield T, Jennings WC. Two-year cumulative patency of endovascular arteriovenous fistula. J Vasc Access. 2020 May;21(3):350–6. [CrossRef]
- Morton RL, Turner RM, Howard K, Snelling P, Webster AC. Patients who plan for conservative care rather than dialysis: a national observational study in Australia. Am J Kidney Dis. 2012 Mar;59(3):419–27. [CrossRef]
- Yong DSP, Kwok AOL, Wong DML, Suen MHP, Chen WT, Tse DMW. Symptom burden and quality of life in end-stage renal disease: a study of 179 patients on dialysis and palliative care. Palliat Med. 2009 Mar;23(2):111–9. [CrossRef]
- García GG, Iyengar A, Kaze F, Kierans C, Padilla-Altamira C, Luyckx VA. Sex and gender differences in chronic kidney disease and access to care around the globe. Semin Nephrol. 2022 Mar;42(2):101–13. [CrossRef]
- Gasparini A, Evans M, Coresh J, Grams ME, Norin O, Qureshi AR, et al. Prevalence and recognition of chronic kidney disease in Stockholm healthcare. Nephrol Dial Transplant. 2016 Dec;31(12):2086–94. [CrossRef]
- Kausz AT, Obrador GT, Arora P, Ruthazer R, Levey AS, Pereira BJG. Late initiation of dialysis among women and ethnic minorities in the United States. J Am Soc Nephrol. 2000 Dec;11(12):2351-2357. [CrossRef] [PubMed]
- Berland T, Clement J, Inston N, Kreienberg P, Ouriel K, WavelinQ 4 French Investigators. Percutaneous arteriovenous fistula creation with the 4F WavelinQ EndoAVF System. J Vasc Surg. 2022 Mar;75(3):1038-1046.e3. [CrossRef]
- Harika G, Mallios A, Allouache M, Costanzo A, de Blic R, Boura B, et al. Comparison of surgical versus percutaneously created arteriovenous hemodialysis fistulas. J Vasc Surg. 2021 Jul;74(1):209–16. [CrossRef]
- Habib SG, Jano A, Ali AA, Phillips A, Pinter J, Yuo TH. Early clinical experience and comparison between percutaneous and surgical arteriovenous fistula. J Vasc Surg. 2023 Sep;78(3):766–73. [CrossRef]
- Hebibi H, Achiche J, Franco G, Rottembourg J. Clinical hemodialysis experience with percutaneous arteriovenous fistulas created using the Ellipsys® vascular access system. Hemodial Int. 2019 Apr;23(2):167–72. [CrossRef]
- Hull JE, Elizondo-Riojas G, Bishop W, Voneida-Reyna YL. Thermal Resistance Anastomosis Device for the Percutaneous Creation of Arteriovenous Fistulae for Hemodialysis. J Vasc Interv Radiol. 2017 Mar;28(3):380–7. [CrossRef]
- Mordhorst A, Clement J, Kiaii M, Faulds J, Hsiang Y, Misskey J. A comparison of outcomes between open and endovascular arteriovenous access creation for hemodialysis. J Vasc Surg. 2022 Jan;75(1):238-247.e1. [CrossRef]
- Osofsky R, Byrd D, Reagor J, Das Gupta J, Clark R, Argyropoulos C, et al. Initial Outcomes Following Introduction of Percutaneous Arteriovenous Fistula Program with Comparison to Historical Surgically Created Fistulas. Ann Vasc Surg. 2021 Jul;74:271–80. [CrossRef]
- Radosa CG, Radosa JC, Weiss N, Schmidt C, Werth S, Hofmockel T, et al. Endovascular Creation of an Arteriovenous Fistula (endoAVF) for Hemodialysis Access: First Results. Cardiovasc Intervent Radiol. 2017 Oct;40(10):1545–51. [CrossRef]
- Rajan DK, Ebner A, Desai SB, Rios JM, Cohn WE. Percutaneous creation of an arteriovenous fistula for hemodialysis access. J Vasc Interv Radiol. 2015 Apr;26(4):484–90. [CrossRef]
- Shahverdyan R, Beathard G, Mushtaq N, Litchfield TF, Vartanian S, Konner K, et al. Comparison of Ellipsys Percutaneous and Proximal Forearm Gracz-Type Surgical Arteriovenous Fistulas. Am J Kidney Dis. 2021 Oct;78(4):520-529.e1. [CrossRef]
- Sultan S, Langsfeld M, Chavez L, Fabre A, Osofsky R, Argyropoulos C, et al. Initial 6-month quality review of a percutaneous endovascular arteriovenous fistula program. J Vasc Access. 2021 Jul;22(4):540–6. [CrossRef]

| Autor/year | Study Type | Number of participants | Mean Age | Gender N (%) |
Device |
|---|---|---|---|---|---|
| Beathard et al [47], 2020 | Retrospective Cohort Study | 105 | 56,2 | Male: 77 (73,3) Female: 28 (26,3) |
Ellipsys Vascular Access System |
| Berland et al [53], 2022 | Retrospective Cohort Study | 120 | 55,6±15,9 | Male: 97 (80,8) Female: 23 (19,2) |
Wavelin Q EndoAVF System |
| Harika et al [54] | Retrospective comparative study | 107 | 63,6±15,41 | Male: 66 (61,7) Female: 41 (38,3) |
Ellipsys Vascular Access System/ Surgical AVF |
| Habib et al [55], 2023 | Retrospective comparative study | 51 | 58 ± 13,5 | Male 40 (78) Female: 11 (22) |
Ellipsys Vascular Access System/ Wavelin Q EndoAVF System / Surgical AVF |
| Hebibi et al [56], 2019 | Retrospective Cohort Study | 34 | 62 | Male: 20 (58) Female: 34 (42) |
Ellipsys Vascular Access System |
| Hull, et al [57], 2017 | Prospective Cohort Study | 26 | 45,5±13,6 | Male: 10 (38,46) Female: 16 (61,54) |
Ellipsys Vascular Access System |
| Hull et al [18], 2018 | Prospective Cohort Study | 107 | 56,7±12 | Male: 78 (72,9) Female: 29 (27,1) |
Ellipsys Vascular Access System |
| Inston et al[23], 2019 | Prospective comparative study | 30 | 57±15 | Male: 25 (75) Female: 5 (30) |
Wavelin Q EndoAVF System/Surgical AVF |
| Kitrou et al [19], 2022 | Retrospective Cohort Study | 30 | 55,3±13,6 | Male: 30 (100) Female: 0 (0). |
Wavelin Q EndoAVF System |
| Lok et al [17], 2017 | Prospective Cohort Study | 60 | 59 ±13,6 | Male: 39 (65) Female: 21 (35) |
Everlin Q EndoAVF System |
| Mallios et al[46] , 2020 | Retrospective Cohort Study | 234 | 64 | Male: 148 (63,24) Female: 86 (36,76) |
Ellipsys Vascular Access System |
| Mordhorst et al[58], 2022 | Retrospective comparative study | 61 | 64 | Male: 46 (75,4) Female: 15 (24,6) |
Everlin Q EndoAVF/Surgical AVF |
| Osofsky et al[59], 2021 | Retrospective comparative study | 24 | 56,7±22,6 | Male: 12 (50) Female: 12 (50) |
Ellipsys Vascular Access System/ Surgical AVF |
| Radosa et al [60], 2017 | Retrospective Cohort Study | 8 | 57 | Male: 6 (75) Female: 2 (25) |
Everlin Q EndoAVF System |
| Rajan et al [61], 2015 | Prospective Cohort Study | 33 | 51±11,4 | Male: 20 (61) Female: 13 (39) |
Everlin Q EndoAVF System |
| Shahverdyan et al [20], 2020 | Retrospective comparative study | 100 | 64,18 ± 14,18 | Male: 69 (69) Female: 31 (31) |
Ellipsys Vascular Acces System/ Wavelin Q EndoAVF System |
| Shahverdyan et al [62], 2021 | Restrospective comparative study | 89 | 67,9 | Male: 58 (65,2) Female: 31 (34,8) |
Ellipsys Vascular Access System/ Surgical AVF |
| Sultan et al [63] | Retrospective Cohort Study | 18 | 63,8 | Male: 10 (55,6) Female: 8 (44,4) |
Everlin Q EndoAVF System |
| Zemela et al [21], 2021 | Retrospective Cohort Study | 32 | 60,2 | Male: 23 (71,9) Female: 8 (28,1) |
Wavelin Q EndoAVF System |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





