Submitted:
08 August 2024
Posted:
09 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion Criteria and Validated Questionnaire
2.3. Treatment Administration
2.4. Effectiveness Evaluation Procedures
2.5. Statistical Analyses
3. Results
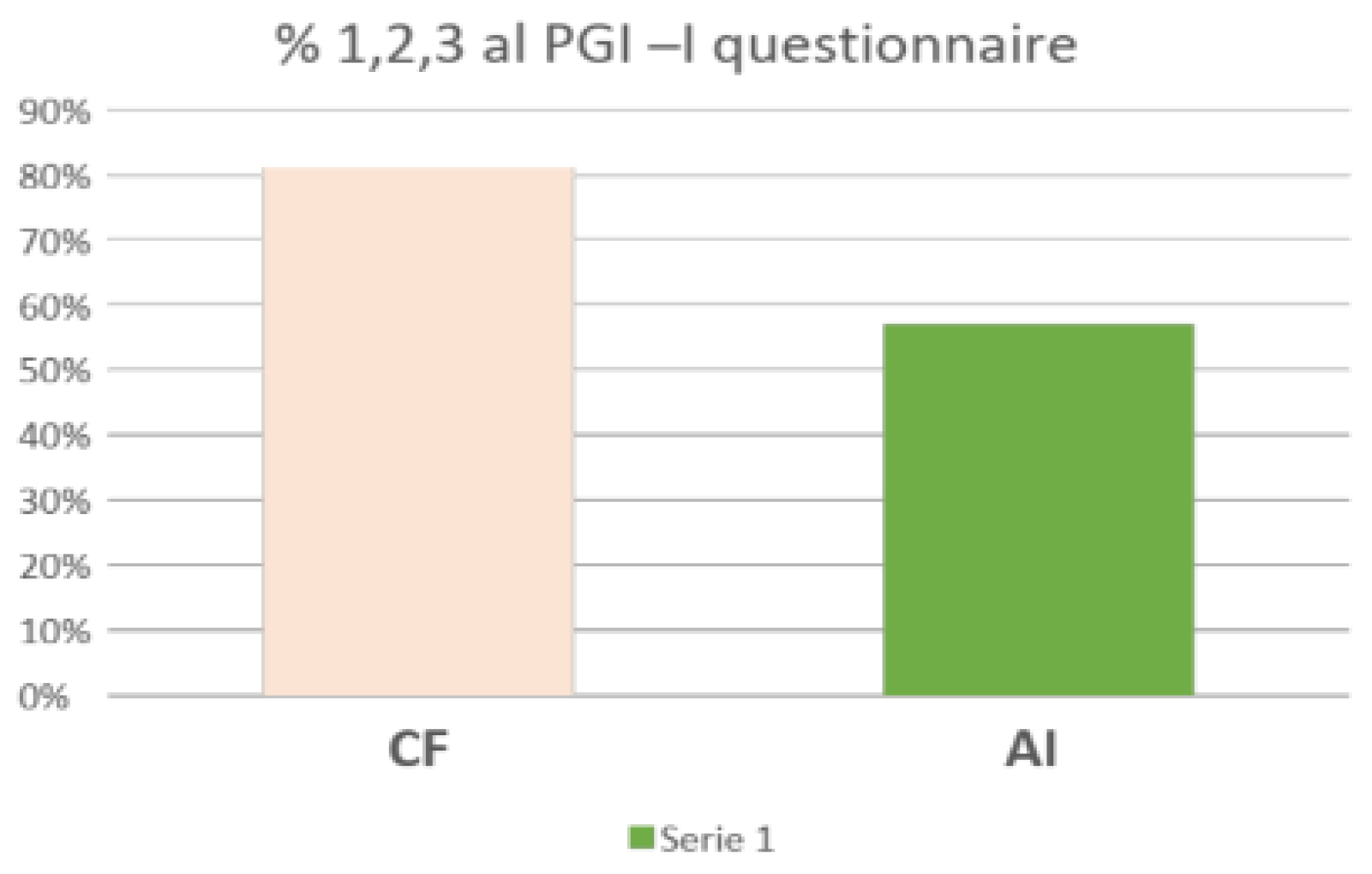
3.1. Primary Endpoint: PGI-I Questionnaire at 10 Weeks after Treatment
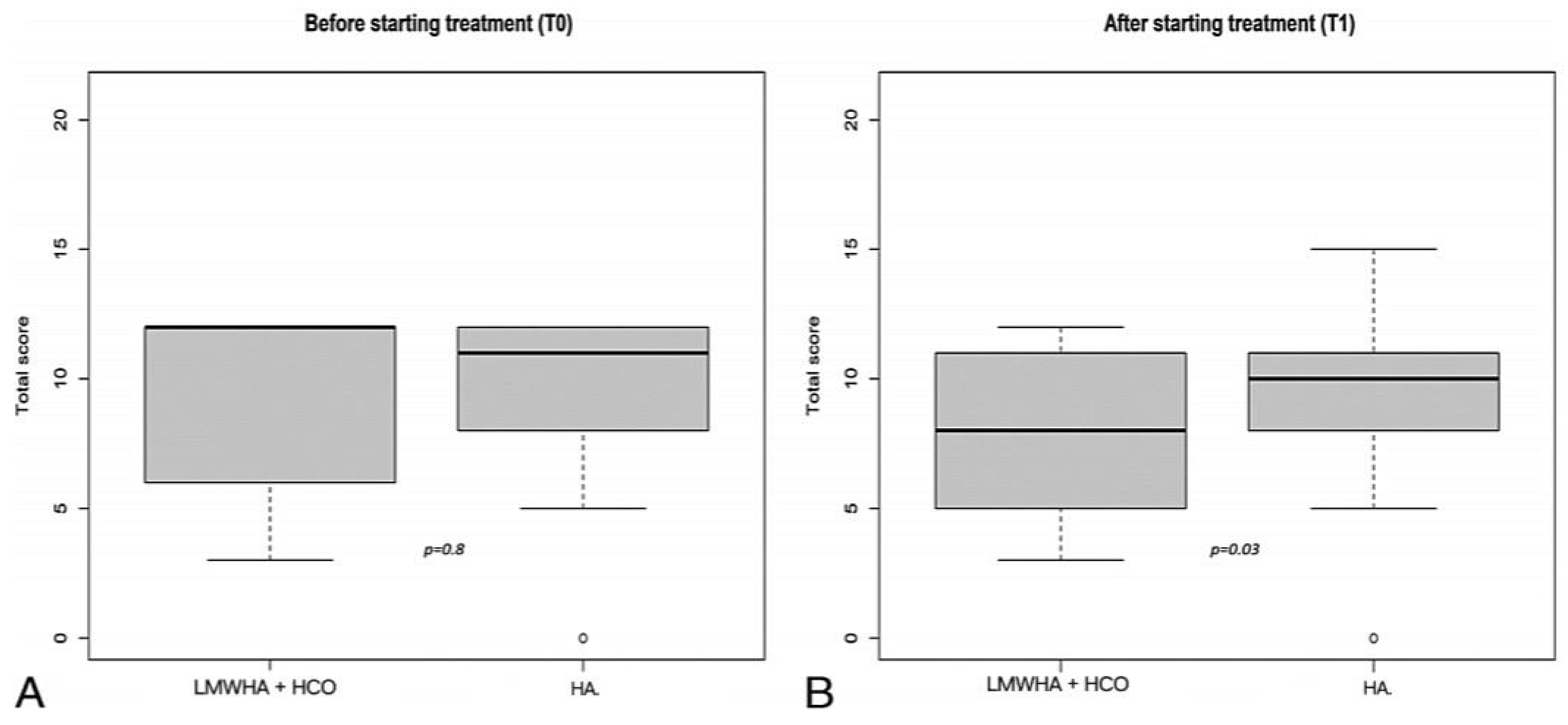
3.2. Secondary Endpoint I: ICIQ-SF Questionnaire
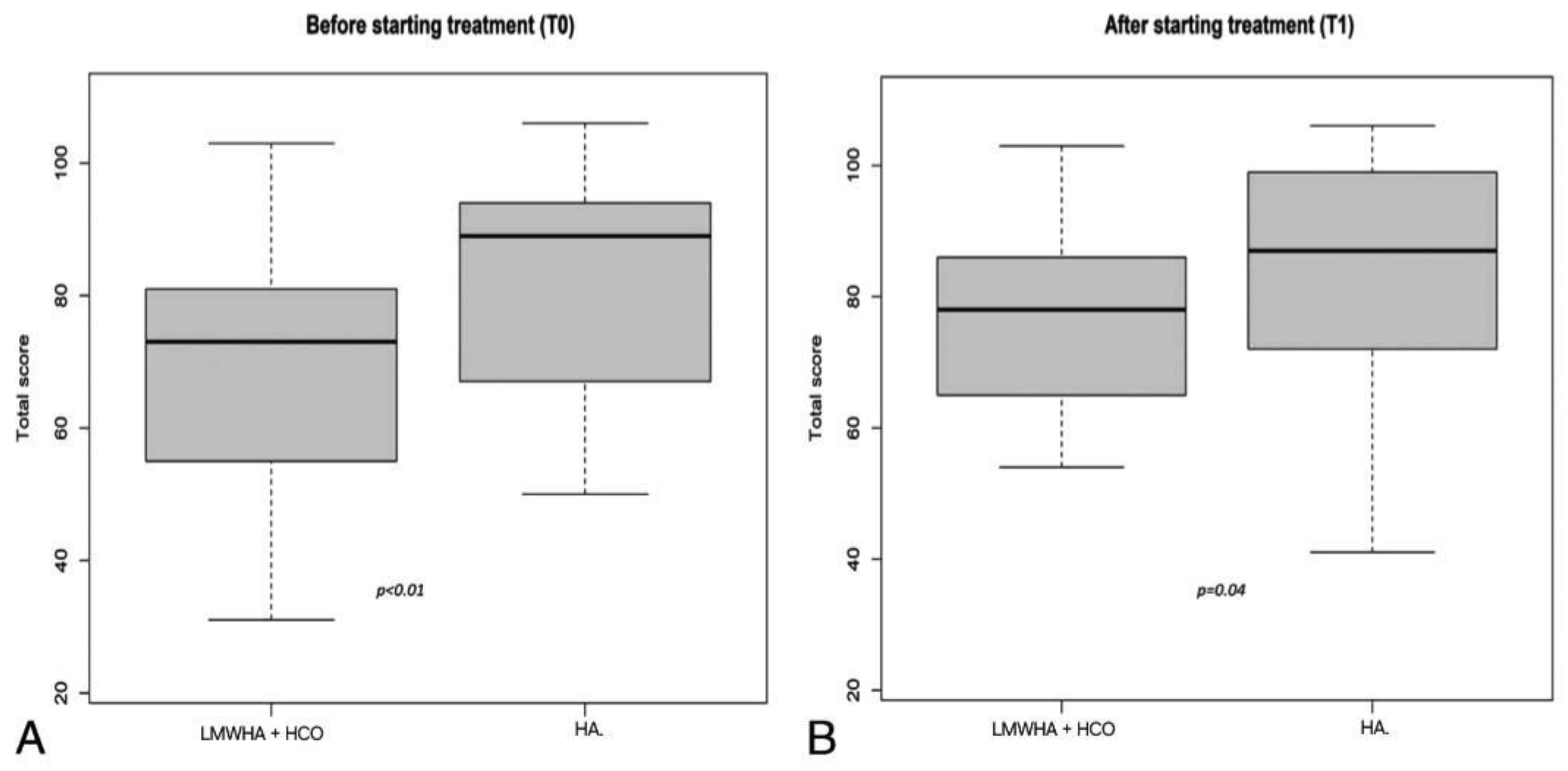
3.3. Secondary Endpoint II: IQoL Questionnaire
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, Athanasiou S. The Genitourinary Syndrome of Menopause: An Overview of the Recent Data. Cureus. 2020 Apr 8;12(4):e7586. [CrossRef]
- Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary Incontinence in Women: A Review JAMA. 2017 Oct 24;318(16):1592-1604. [CrossRef]
- Palma F, Volpe A, Villa P, Cagnacci A; Writing group of AGATA study. Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: The AGATA study. Maturitas. 2016 Jan;83:40-44. [CrossRef]
- Mitchell CM, Waetjen LE. Genitourinary Changes with Aging. Obstet Gynecol Clin North Am. 2018 Dec;45(4):737-750. [CrossRef]
- Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, Khan SA. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am J Obstet Gynecol. 2016 Dec;215(6):704-711. [CrossRef]
- Sturdee DW, Panay N; International Menopause Society Writing Group. Recommendations for the management of postmenopausal vaginal atrophy. Climacteric. 2010 Dec;13(6):509-22. [CrossRef]
- Traish AM, Vignozzi L, Simon JA, Goldstein I, Kim NN. Role of Androgens in Female Genitourinary Tissue Structure and Function: Implications in the Genitourinary Syndrome of Menopause. Sex Med Rev. 2018 Oct;6(4):558-571. [CrossRef]
- Nappi RE, Particco M, Biglia N, Cagnacci A, Di Carlo C, Luisi S, Paoletti AM. Attitudes and perceptions towards vulvar and vaginal atrophy in Italian post-menopausal women: Evidence from the European REVIVE survey. Maturitas. 2016 Sep;91:74-80. [CrossRef]
- Claudia Collà Ruvolo, MD,1 Olimpia Gabrielli, MD,1 Carmen Formisano, MD,1 Gianluigi Califano, MD,1 Paolo Manna, MD,2 Roberta Venturella, MD,2 and Costantino Di Carlo, MD1 Prasterone in the treatment of mild to moderate urge incontinence: an observational study , The Journal of The North American Menopause Society 2022. [CrossRef]
- Piovella et al. Effects of high concentration oxygen in combination with sodium hyaluronate, in the meibomites secondary to chronic blepharitis and palpebral tonicity. Euvision 2017; 2/17 p. 5.
- Condemi L. et al. Vaginal Natural Oxygenation Device (VNOD): concomitant administration of hyaluronic acid and topical hyperbaric oxygen to treat vulvo-vaginal atrophy. European Review for Medical and Pharmacological Sciences 2018. Accepted publication.
- Patel et al. Oxygen: from the benefits of inducing VEGF expression to managing the risk of hyperbaric stress. Antioxid Redox Signal. 2005 Sep-Oct;7(9- 10):1377-87. [CrossRef]
- Jokar A, Davari T, Asadi N, Ahmadi F, Foruhari S. Comparison of the Hyaluronic Acid Vaginal Cream and Conjugated Estrogen Used in Treatment of Vaginal Atrophy of Menopause Women: A Randomized Controlled Clinical Trial. Int J Community Based Nurs Midwifery. 2016 Jan;4(1):69-78.
- Tubaro A, Zattoni F, Prezioso D, Scarpa RM, Pesce F, Rizzi CA, Santini AM, Simoni L, Artibani W; Flow Study Group. Italian validation of the International Consultation on Incontinence Questionnaires. BJU Int. 2006 Jan;97(1):101-8. [CrossRef]
- McKown S, Abraham L, Coyne K, Gawlicki M, Piault E, Vats V. Linguistic validation of the NQOL (ICIQ), OAB-q (ICIQ), PPBC, OAB-S and ICIQ-MLUTSsex questionnaires in 16 languages. Int J Clin Pract. 2010 Nov;64(12):1643-52. [CrossRef]
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev 2016; 2016: CD001500. [CrossRef]
- Sinha A, Ewies AA. Non-hormonal topical treatment of vulvovaginal atrophy: an up-to-date overview. Climacteric 2013; 16: 305-31. [CrossRef]
- Teodoro, M.C., Scibilia, G., Lomeo, E., ...Scollo, P., Pecorino, B. Carbon dioxide laser as a new valid treatment of lichen sclerosus. Clinical and Experimental Obstetrics and Gynecology, 2019, 46(2), pp. 206–210. [CrossRef]
| HCO + LMWH Combined | HA Topically Alone | |
|---|---|---|
| Age | 59,7 | 58,5 |
| BMI | 24,7 | 25,0 |
| Parity | 2,1 | 1,8 |
| LMP (y) | 50,2 | 51,2 |
| Distance from LMP (y) | 5,5 | 6,0 |
| IQoL score pre-treatment | 73 | 89 |
| OAB score pre treatment | 27 | 26 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





