1. Introduction
Larsen et al. (OMIM:150250) described multiple congenital large joint dislocations associated with distinctive facial phenotypic characterization in six unrelated patients [
1]. The most striking findings were a typical flattened “dish-like” facies, bilateral dislocations of multiple joints, and equinovarus deformities of the feet. Larsen syndrome is characterised by distinctive facies (flat face, hypertelorism, depressed nasal bridge, prominent forehead, cleft palate, and cleft uvula. Ligamentous hyperlaxity of the joints associated with dislocated elbows, hips, and knees (genu recurvatum) [
1,
2,
3]. The phenotype of the hands is characteristic cylindrical fingers, spatulate –like thumbs, short and broad fingertips and in some cases multiple wrist ossification centres can be encountered. The foot is characterized by a resistant type of clubfoot deformity, though the radiological phenotype can be diagnostic via the presence of a juxta –calcaneal accessory bone or bifid calcaneus [
3,
4,
5,
6]. Remarkable number of children with Larsen syndrome are presented with sensorineural or mixed hearing loss associated with abnormal ear anatomy. Other forms of dislocations have been encountered such as dislocation of the malleus and incus [
6,
7]. Abnormalities of the central nervous system were part of the syndrome in some patients (neurological impairment in connection with cord compression, hydrocephalus, intellectual disability, subependymal glial proliferation of the lateral ventricle can mimiks tuberous sclerosis) [
8]. The joint deformities associated with ligamentous hyperlaxity include dislocations of the hip, anterior dislocations of the knee, dislocations of the radial head, dislocation of the patella as well as the wrist, shoulder and the carpometacarpal joint of thumb and even of the superior tibio-fibular joint [
9,
10]. Congenital talipes equinovarus is not of uncommon occurrence in children with Larsen syndrome [
11]. Life threatening congenital heart defects of aortic dilatation and valvular insufficiency and aneurysm of the ductus arteriosus have been described [
12,
13]. Spine abnormalities include dyssegmentation and craniocervical instability [
14,
15]. The progressive spine deformities may lead to progressive kyphosis and lordosis, and eventually in some cases death [
17]. At the lumbo-sacral junction the neural arches may show maldevelopment associated with narrow interpedicular distances. Scoliosis develops in early childhood and can be progressive (fusion is preferably performed by the age of 10 years). The gene has been located - it is filamin B, children showed heterozygosity for de novo mutations in FLNB gene (OMIM 603381) [
18]. Though, the same mutated gene has been diagnosed in children with atelosteogenesis types I and III, and in spondylocarpotarsal syndromes. Mutations seem to cluster in about 5 of the 46 exons [
19]. Autosomal recessive type of Larsen syndrome has been diagnosed in children with CHST3 gene mutation [
20].
2. Materials and Methods
The study protocol was approved by the Ethics Committee of the (Ilizarov Scientific Research Institute, No. 4(50)/13.12.2016, Kurgan, Russia). Informed consents were obtained from the patient’s Guardians. Six children (four boys and two girls, age range of a few months -7 years) have been referred to our departments) have been referred to our departments for diagnosis and treatment. In Larsen syndrome, the paediatricians as well as orthopaedic surgeons may be confronted with one of the most confusing and challenging constellations of musculo-skeletal deformities. The first and the foremost clinical confusion is the initiation of the false diagnosis of arthrogryposis multiplex congenita (AMC). AMC when seen in children with generalized ligamentous hyperlaxity associated with alterations in muscle tone can easily be misunderstood as hypotonia. This sort of mis-conception drove the medical group to direct their clinical potential towards listing these children within the category of floppy child syndrome and other syndromes with ligamentous hyperlaxity. Vigorous investigations to confirm or rule out neuromuscular disorders such as chromosomal aberrations such as trisomy 21, and endocrinopathies, specifically hypothyroidism, were time consuming with fruitless results for the children and were of remarkable turmoil for the families. Structured questionnaire and history taking is the fundamental element for diagnosis. In particular the maternal gestational history of miscarriages, bleeding in the first trimester, feeble in utero movement, stillbirths, eclampsia, hydro/oligo-hydraminious and history of difficulties with conceiving such as history of primary or secondary sterility. Unusual events in gestational histories such infections (toxoplasmosis, cytomegalovirus, AIDS virus and so forth). Full details regarding the labour circumstances (history of breech delivery, foetal distress and cyanosis. Measurements of Baby’s growth parameters. The past family history of medical pathologies, operations, interventions, skeletal dysplasia, metabolic bone disorders, and syndromic association complexes. Careful clinical inspection of craniofacial abnormalities, general physique and build, upper limbs, lower limbs, contractures, and the spine in conjunction with comprehensive radiological phenotypic characterization to detect additional pathologic features.
3. Results
3.1. The Classical Clinical and Radiological Phenotype in Children with Larsen Syndrome
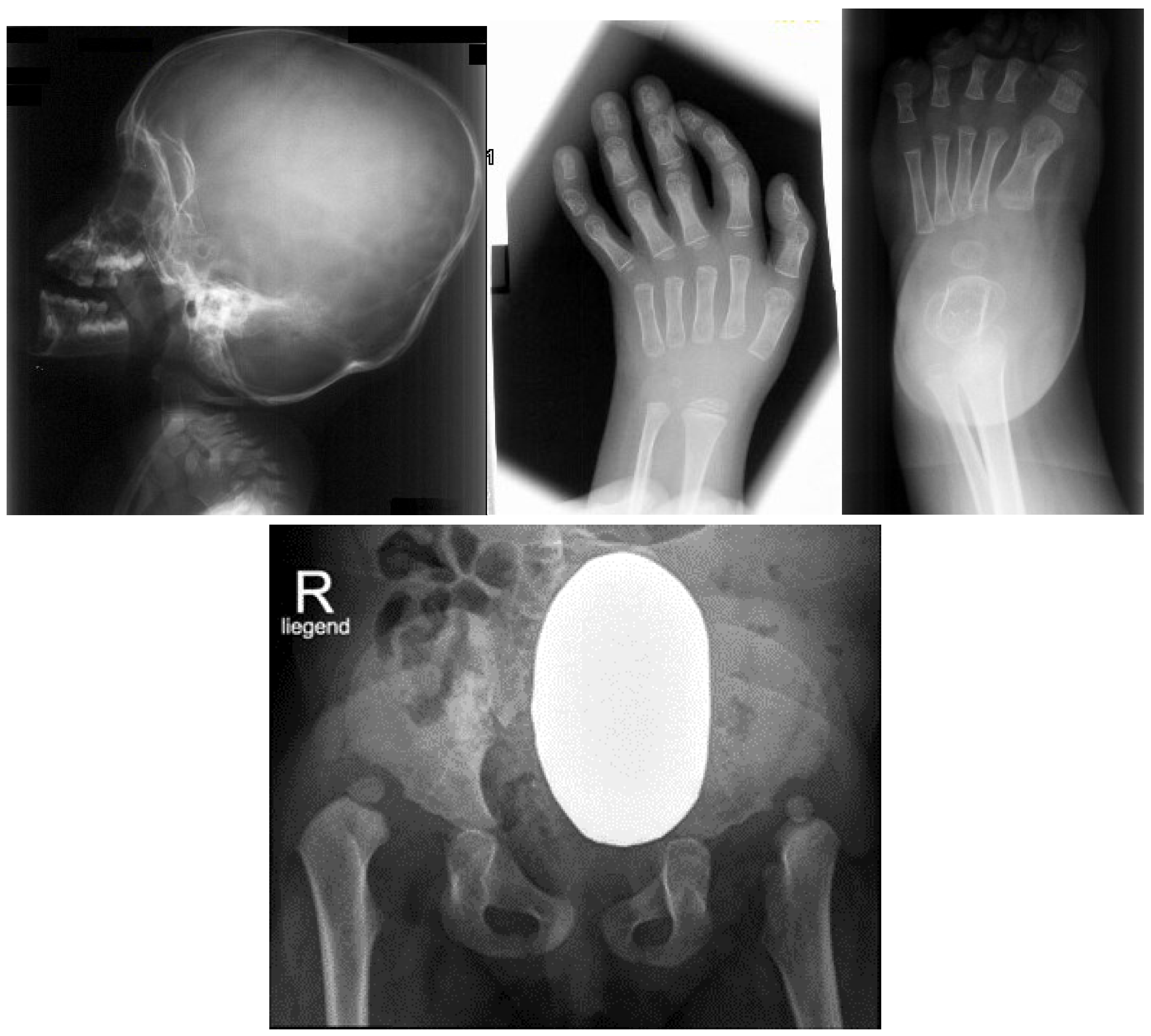
In these children, the dysmorphic facial features were evident, which encompassed distinctive facial features, frontal bossing and a flattened nasal bridge giving the facial phenotype of a dish-like facies. Our orthopedic strategy is based upon, detailed clinical and radiological phenotypic characterization. Radiological phenotypic interpretations have been organized for all children with referring to 3D CT scan. Lateral skull radiograph of a -7-months-old-boy with Larsen syndrome. Note brachycephaly, frontal bossing and marked disproportionate small facial bones in comparison with large cranium and dysplastic cervical spine, osteopenia of the lambdoid bones causing downward bulging and prominence of the occipital bone associated with progressive thinning protuberance of the squamous part. Hyperostosis of the skull base and a J-shaped sella turcica. AP hand radiograph of a -3-year-old-boy with Larsen syndrome showed retarded bone age, expansion of the distal ends of the shortened metacarpals, the thumb is proximally placed and the presence of accessory bone adjacent to the distal third metacarpal-phalangeal bone. Delta phalanx of the middle metacarpophalangeal bone of the fifth finger (b). AP foot radiograph of a 1-year-old-boy-with Larsen syndrome showed talipes equinovarus and undertubulation of the distal phalanges and to a certain extent undertubulation of the metatarsals. Note two ossification centers of the calcaneus are present (
Figure 1c). AP pelvis radiograph of an 18-month-old-girl with Larsen syndrome showed bilateral hip dislocation with maldevelopment of pseudo-dysplastic-acetabulum and dysplastic capital femoral epiphysis (
Figure 1d).
3.2. Congenital Tetraplegia in A Child with Larsen Syndrome
Congenital tetraplegia has been never described in children with Larsen syndrome. The overall clinical criteria of the lethal type of Larsen syndrome which is characterized by immediate death after birth is not consistent with our current child. Though, no CT scan studies for the craniocervical junctions have been descibed in the lethal type of Larsen syndrome.
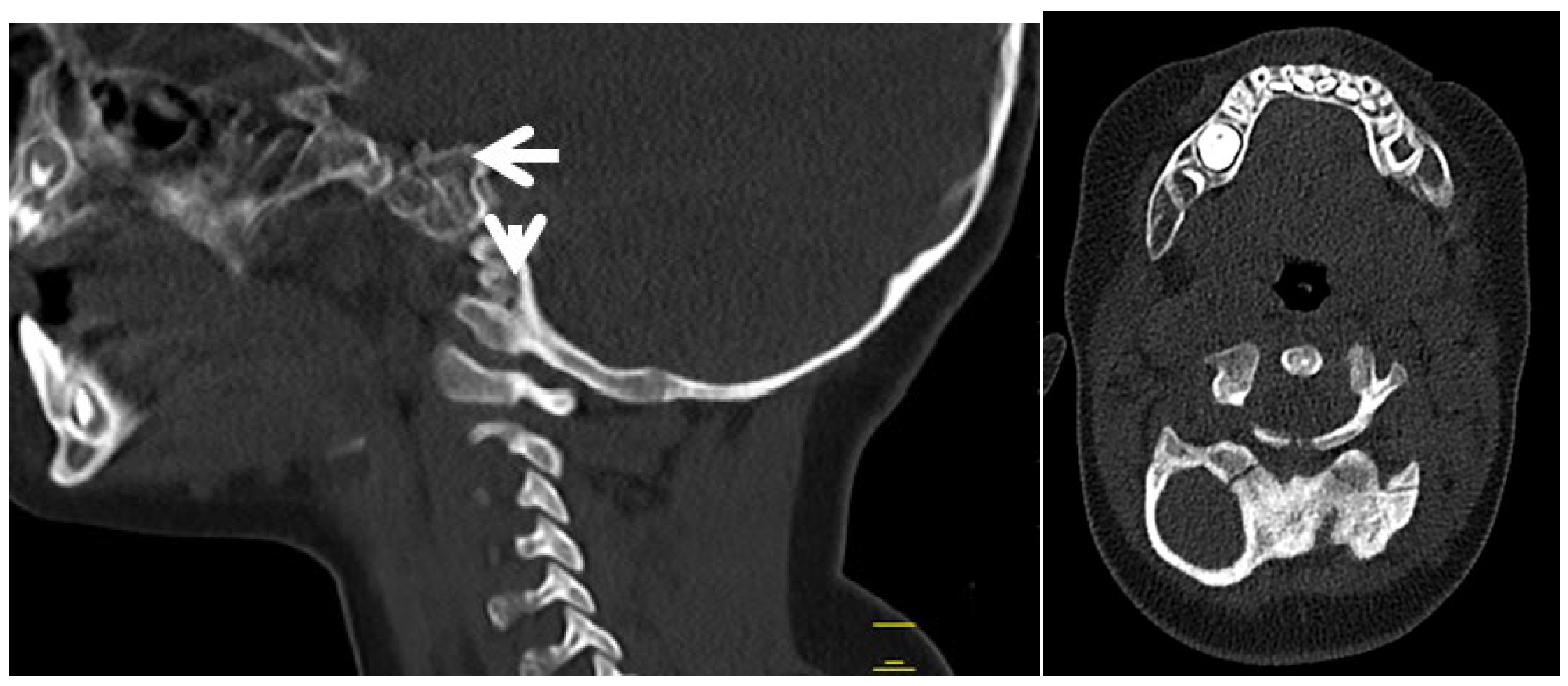
3D reformatted sagittal CT scan of the cranium in a-six month-old-child who was born with congenital tetraplagia). Maldevelopment of the anterior ring of the atlas C1 which has been displaced along the superior surface of the clivus. Also the (odontoid process is hypoplastic and dislocated and get located between the maldeveloped anterior rings)-arrow head. Fusion of the fragmented anterior and posterior rings of C1 and fusion of these fragments effectively the development of a bifurcation like structure (a).Axial 3D reformatted CT scan showed congenital maldevelopment of the anterior arch of the atlas and fusion of the remnants of anterior ring with the lateral mass of C1 (forming a bifurcated bone like) (arrow head).The posterior ring of C1 is hypoplastic (arrow). (
Figure 2b).
3.3. Acute Angled Kyphosis in A Child with Larsen Syndrome
Kyphosis presenting at birth or later on is almost always due to a congenital vertebral malformation. In this child the deformity is purely kyphotic. Conservative treatment alone is of limited value in the management of congenital kyphosis. Though some restrictions have to be considered to perform surgical interventions, especially when there is cardiopulmonary dysfunction, associated kidney anomalies and neurological pathologies such as Arnold-Chiari lesion, a filum terminale syndrome or diastematomyelia.
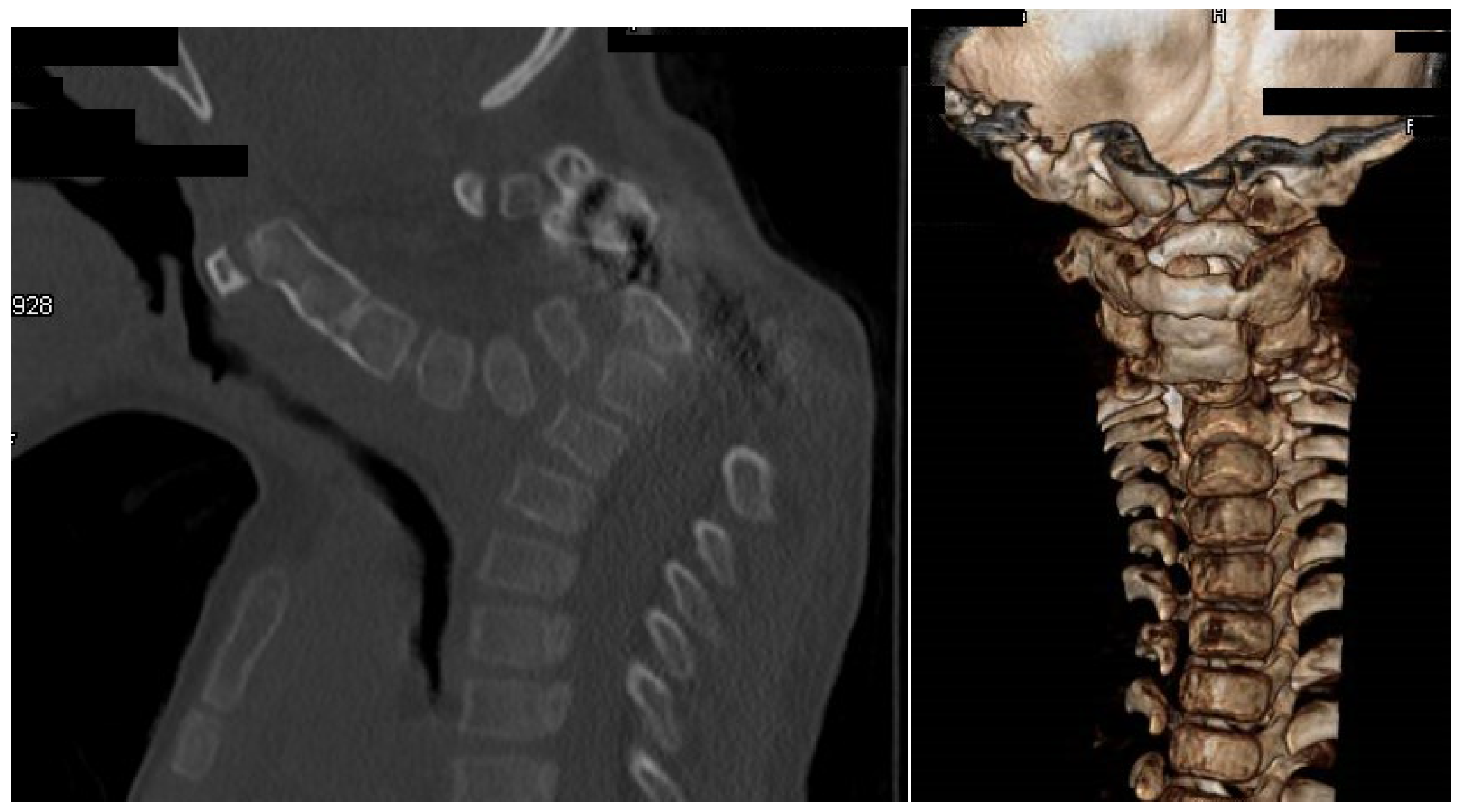
A Sagittal 3D reformatted CT scan of a -7-year-old-boy with Larsen syndrome showed cervico-thoracic kyphosis (Cobb’s angle of 90°). Hypoplastic anterior and posterior arch of the atlas.Note fusion of C2-3 and hypoplasia and fragmentation of the 7th cervical spine (arrow) (
Figure 3a). A 3D reconstruction CT scan of the same child showed fusion of C2-3 associated with hypoplastic vertebral bodies causing the development of acute cervico-thoracic kyphosis (
Figure 3b).
3.4. Surgical Interventions to Correct Hip/Knee Dislocations and Talipes Equinovarus
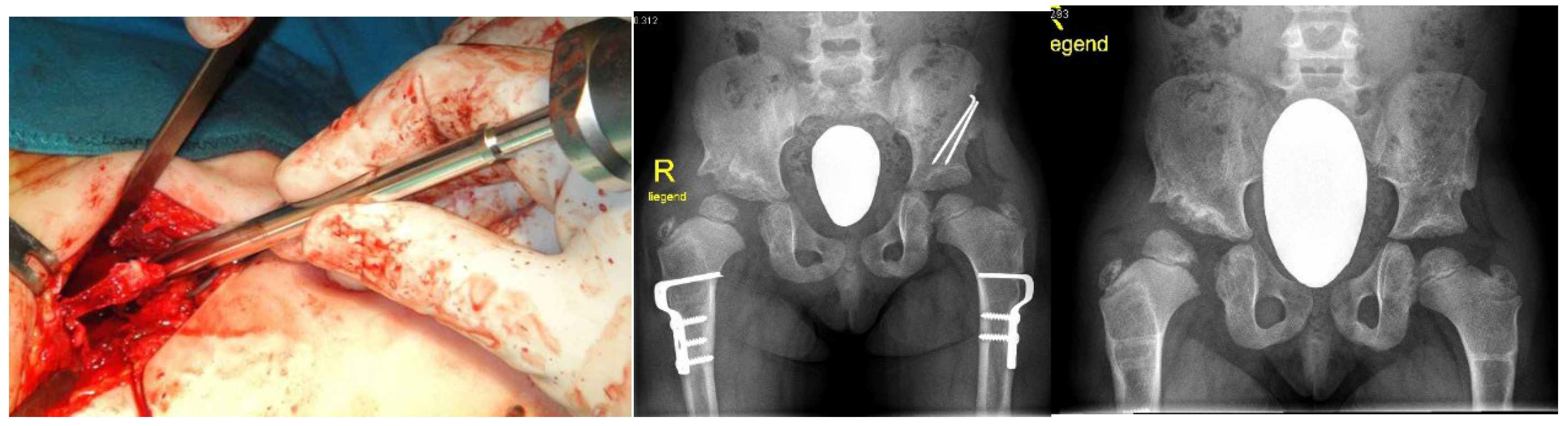
Congenital multiple dislocations often proves an uneasy task for the paediatric orthopaedic surgeons. The liability of skeletal deformities in Larsen syndrome can recur. The dislocated hip joints must be treated as early as possible. Since at the same time there is often hyperlaxity of the knee joints with anterior dislocation of the tibia, conservative treatment with physiotherapy and a Pavlik harness must primarily be carried out. While it is usually possible to reduce the knee joints through slow repression, the hip joints have to be openly reduced, which is technically difficult because they are due to the Larsen Syndrome extremely unstable joints. In order to achieve sufficient joint stability, the open reduction must be combined with a bony procedure in which the dysplastic acetabulum is corrected. The surgical method according to Pemberton/Dega has proven successful in our hands, in which a slightly curved chisel is inserted cranial to the edge of the acetabulum, the ileum is severed to just above the Y joint, and a triangular bone graft, inserted into the osteotomy gap is fixed with a K wire. Depending on the existing anatomical conditions, an intertrochanteric osteotomy may also be indicated - for example in the case of increased ante torsion of the femoral neck - in order to achieve optimal centering and stability of the femoral head in the joint socket. Because of the bony procedures the surgery should not be indicated before the age of 12 months. We performed simultaneous combined proximal femoral varus osteotomy and shelf acetabuloplasty has been performed in a-14-months old girl with Larsen syndrome. The aim of these surgical procedures is to assure good containment of the bilateral hip dislocation. A double incision was used for this type of surgery (
Figure 4a). Proximal femoral osteotomy for varization and derotation was performed at the intertrochanteric level (
Figure 4b). Postoperative, neck-shaft angles were never reduced to less than 110°, and the derotation angle was less than 20° (
Figure 4c).
Knee dislocations: Primarily we started gentle manipulation soon after birth with traction and flexion of the knees. A long leg cast fixation has been applied to restore knee flexion at 90°, in concomitant with application of Pavlik harness. The severe shortening of the quadriceps warranted operative corrections. The incision was made extending from lateral parapatellar proximal to the crossing of the midline distally to the patella ending at the medial tibial tuberosity. arthrotomy through mobilization of the quadriceps and hamstrings was applied. VY plasty and shortening osteotomy of the femur with plate fixation (preservation of extensor mechanism) was applied by a reverse Mc-Intosh soft tissue plasty for joint stabilization associated with posterior capsulorrhaphy and cruciate plasty (the aim was shortening of the elongated anterior cruciate ligament). Postoperatively, we applied plaster cast in 30-45 ° flexion. The first change of plaster was on the second day after surgery, this was followed by plaster fixation for 4-6 weeks and finally splints and physiotherapy and orthotic management have been achieved successfully.
Talipes equinovarus of the foot was corrected via soft tissue release (when the child is older than 1 year of age). The deformity in some children was very resistant, even to aggressive release. Postoperative bracing with ankle-foot orthoses was applied in an attempt to delay recurrence. Though recurrent deformity required repeated surgeries. In some children we were able to achieve and maintain a plantigrade foot. Talectomy and talar decancellation were attempted in some children. AP knees radiograph of a -5 months –old-boy with Larsen syndrome showed bilatral dislocations associated with undertubulation of the tibae and fibulae. Note the fragmented/deformed epiphyses and the right tibia is medially subluxated. Note bilateral talipes equinivarus associated with double ossifications of the calcaneus(
Figure 5a). Postoperative photo showed corrections of the hip, knee and talipes equinivarus (
Figure 5b).
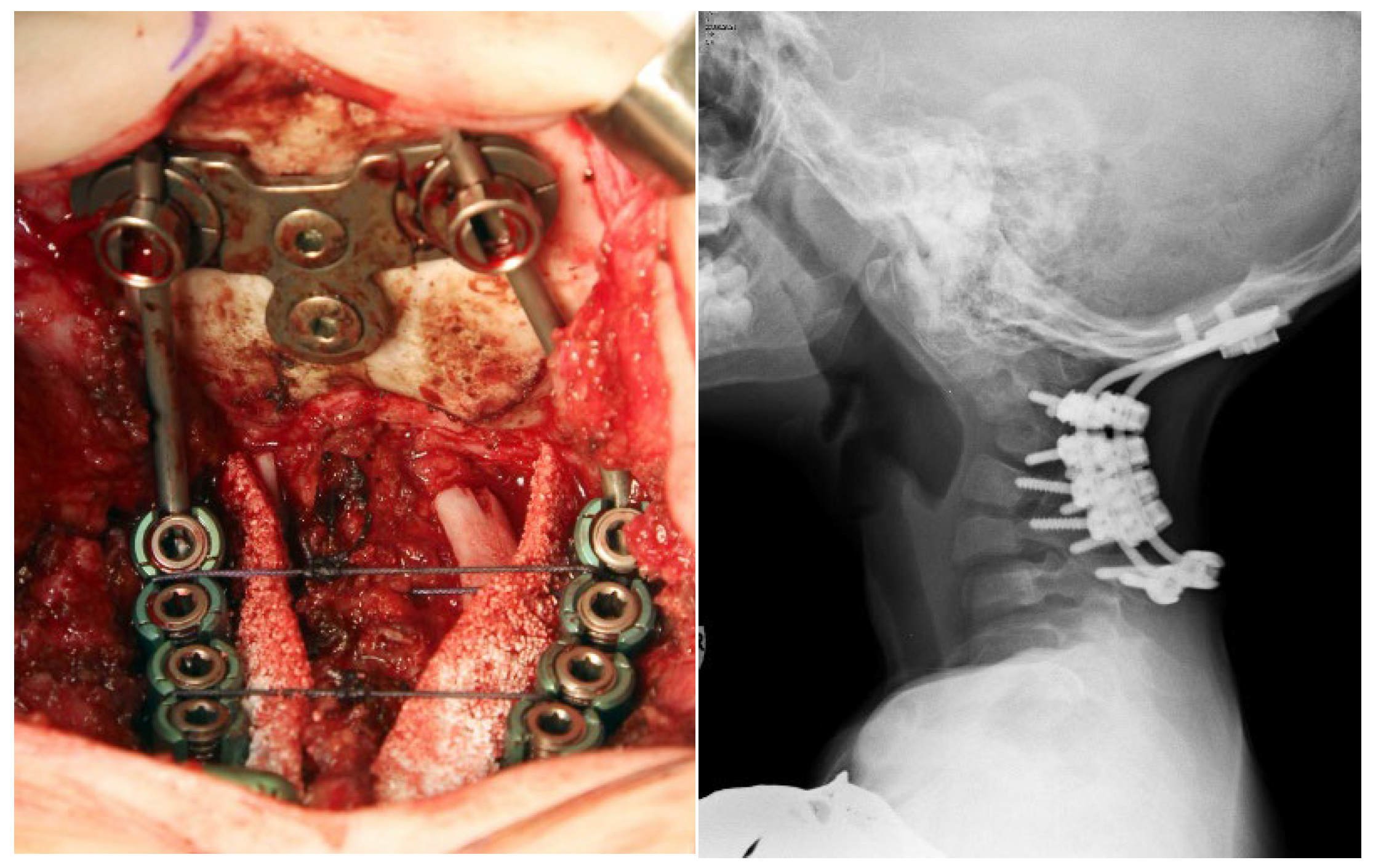
3.5. Surgical Intervention to Correct Traumatic Tertaplagia
A-2- year old boy with Larsen syndrome became tetraplegic after minor trauma (jumping down from the sofa). Halo traction with 1 kg was used in the local emergency trauma center and then after 1 week he was transferred to Ilizarov Center with minor neurological improvement. The lateral skull and spine radiograph showed hypoplastic and maldevelopment of the cervical spine associated with C1-2 instability and apparent kyphotic deformity with C4 body hypoplasia. The size of the cervical spinal canal is normal. So SCIWORA (spinal cord injury without radiographic – like) was a bit confusing due to laxity. But nevertheless, the kyphotic deformity was so evident and therefore the mechanism of cord trauma was expected (
Figure 6a). Axial reformatted CT scan confirmed the hypoplasia of the vertebral body of C4 (
Figure 6b).
Photo (intraoperative) At the end of the surgery 10,3,5 mm screws were inserted in the lateral masses of C3-6 and intralaminar in C7 as well as standard two screws occipital plate was applied(
Figure 7a). The surgery was followed by breath problems due to chest softness. Thereby, we were obliged to stop the operation every 30 minutes in order to give the child better oxygenation through lifting the child in our hands. Good neurological recovery in 2 weeks after surgery was noticeable. Lateral cervical spine radiograph, ten years after surgery showed good bone fusion and the hardware is still stable (
Figure 7b).
4. Discussion
Larsen Syndrome is characterized by multiple joint dislocations. The most frequent Assoziation (45%) is with developmental dysplasia of the hips, which can be diagnosed clinically at birth. The ossification of the femoral head occurs earlier than normal [
21]
Children with Larsen syndrome may require many operations to fulfil some sort of corrections. These corrections are needed to approach sufficient success to ameliorate the locomotor system. The knees are particularly difficult to stabilize and, in spite of prolonged splintage, instability can occur. In some patients bilateral knee disarticulation in some instances can be problematic [
22]. The hips are usually irreducible except by operative release but, if this is the only solution, it is better done during the first years of life. The dislocated elbows cause effectively total disruption for both the radio –capittelar and humero-ulnar joints because of the dysplasia of the distal humerus qnd condylar underdevelopment [
23]. Talipes equinovarus or equinovalgus, or hindfoot valgus with forefoot adduction. These deformities warrant surgical corrections. A constellation of foot deformities have been described such as adducus, valgus, cavus, and equinovarus. Cervical spine deformities in Larsen syndrome have been described in the literature as being the most serious life-threatening manifestation. A constellation of cervical spine defects can cause morbid impingement on the spinal cord, which can include vertebral body hypoplasia, posterior element dysraphism, and craniocervical/ cervical spine dyssegmentations [
26]. All the aforementioned vertebral anomalies can result in C1-2 instability and or leads to the development of acute angled cervical kyphosis. Acute angle cervical spine kyphosis can expose the spinal cord to suffer from severe damage, especially when progressive traumatic injury at the apex of the acute kyphosis occurs. Larsen syndrome with congenital tetraplegia (quadriplegia) was diagnosed in one child, in addition he manifested more severe skeletal and extraskeletal manifestations, which were to certain extent consistent with the diagnosis of the lethal type of Larsen syndrome which is characterized by death of the child soon after birth.. In our patient neither brain dysplasia nor pulmonary pathologies have been encountered [
27,
28]. Family history in this tetraplegic child showed first cousin marriages, compatible with autosomal recessive pattern of inheritance [
29]. Lethal variant of Larsen syndrome was described in the literature. Apart from neonatal death due to pulmonary hypoplasia and laryngotracheomalacia the main distinguishing features appear to be serious congenital respiratory pathology [
30,
31,
32]. The differential diagnosis of Larsen syndrome is mandatory, other disorders with multiple dislocations have to be considered. Hall et al., described three unrelated patients with an unusual form of spondyloepimetaphyseal dysplasia with multiple joint dislocations. Skeletal survey revealed small flattened and irregular and fragmented epiphyses with wide and irregular metaphyses. There is streaky sclerosis of the metaphyses [
33]. Idaho syndrome is another disorder characterized by multiple joint dislocations and craniosynostosis. The limb abnormalities are diagnostically important, in that there is a complete anterior dislocation of the tibia and fibula, and the patellae are absent. The thumbs are proximally implanted and there is camptodactyly at the interphalangeal joints [
34,
35].
5. Conclusions
Orthopaedic strategy for patients with Larsen syndrome should be based upon early and precise diagnosis. Congenital multiple dislocations often proves an uneasy task for the paedictric orthopaeid surgeons. The liability of skeletal deformities in Larsen syndrome can to recur. Children with Larsen syndrome may require many operations to fulfil some sort of corrections. These corrections are needed to approach sufficient success to ameliorate the locomotor system. Cervical spine deformities were the most serious and life-threatening manifestations in our patients with Larsen syndrome because of the impingement on the spinal cord at the apex of the kyphosis. If spinal cord compression occurs before myelination, the presence of hyperactive deep tendon reflexes or spasiticity as a sign of upper motor neuron dysfunction will not be present. Therefore, the necessity of establishing orthopedic strategy for children not only with Larsen syndrome, but all forms of congenital malformation complex is imperative. The early recognition of the nature of deformities can facilitate the diagnostic process. The precise clinical assessment and analysis of these children can lead to a much better management. We continue to express our clinical expertise as a multidisciplinary team with different orthopedic specialties towards the best possible outcome, which is almost always based on our clinical merit.
Author Contributions
AAK conceptualization and methodology; validation, AAK., FG, AG, VD.; formal analysis, AKK, AG, SR, HAK, SGK.; investigation, SK; data curation, HAK, SR, FG; writing— original draft preparation, AKK.; writing—review and editing, FG.; visualization, AAK.; supervision, FG, AAK. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol was approved by Ethics Committee of the (Ilizarov Scientific Research Institute, No. 4(50)/13.12.2016, Kurgan, Russia). Informed consents were obtained from the patient’s Guardians. Informed Consent Statement: A signed consent form was obtained from the patient’s Guardians.
Acknowledgments
We wish to thank and aknowledge the collaboration of the families and the guardians of the patients.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Larsen, L.J.; Schottstaedt, E.R.; Bost, F.C. Multiple congenital dislocations associated with characteristics facial abnormality. J. Pediatr. 1950, 37, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Klenn, P.J.; Iozzo, R.V. Larsen's syndrome with novel congenital anomalies. Hum. Pathol. 1991, 22, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Latta, R.J.; Graham, C.B.; Aase, J.; Scham, S.M.; Smith, D.W. Larsen's syndrome: A skeletal dysplasia with multiple joint dislocations and unusual facies. J. Pediatr. 1971, 78, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Kozlowski, K.; Robertson, F.; Middleton, R. Radiographic Findings In Larsen's Syndrome. Australas. Radiol. 1974, 18, 336–344. [Google Scholar] [CrossRef]
- De Smet, L.; Legius, E.; Fabry, G.; Fryns, J.P. The Larsen syndrome. The diagnostic contribution of the analysis of the metacarpophalangeal pattern profile. Genet. Couns. 1993, 4, 157–64. [Google Scholar]
- Maack, R.W.; Muntz, H.R. Ossicular abnormality in Larsen's syndrome: A case report. Am. J. Otolaryngol. 1991, 12, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Kaga, K; et al. Temporal bone pathology of two infants with Larsen´s syndrome. Int J Pediatr Otorhinolaryngol 1991, 22, 257. [Google Scholar] [CrossRef]
- Henriksson, P; et al. Larsen syndrome and glial profileration in the brain. Acta Paediatr Scand. 1977, 66, 653. [Google Scholar] [CrossRef]
- Goldberg MJ. The Dysmorphic child. An Orthopedic Perspective. Raven Press ;1986; New York.
- Steel, H.H.; Kohl, E.J. Multiple congenital dislocations associated with other skeletal anomalies (Larsen's syndrome) in three siblings. J Bone Joint Surg 1972, 54, 75–82. [Google Scholar] [CrossRef]
- Silverman, F.N. Larsen’s syndrome: congenital dislocation of the knees and other joints, distinctive facies, and frequently, cleft palate. Ann Radiol. 1972, 15, 297–328. [Google Scholar]
- Strisciuglio, P.; Sebastio, G.; Andria, G.; Maione, S.; Raia, V. Severe cardiac anomalies in sibs with Larsen syndrome. J. Med Genet. 1983, 20, 422–424. [Google Scholar] [CrossRef]
- Eletta, R.; Pandey, A.; Dharmasaputra, T.; Moreno, M.; Oparaugo, Y.; Kumar, T.S.; Beker, S. Severe Aortic Root Dilatation in a Patient With Larsen Syndrome. World J. Pediatr. Congenit. Hear. Surg. 2023, 14, 532–535. [Google Scholar] [CrossRef] [PubMed]
- Micheli, L.J.; E Hall, J.; Watts, H.G. Spinal instability in Larsen's syndrome: report of three cases. J Bone Joint Surg 1976, 58, 562–5. [Google Scholar] [CrossRef] [PubMed]
- Weisenbach, J.; Melegh, B. Vertebral anomalies in Larsen's syndrome. Pediatr. Radiol. 1996, 26, 682–683. [Google Scholar] [CrossRef]
- Lutter, L.D. Larsen syndrome: clinical features and treatment--a report of two cases. J Pediatr Orthop. 1990, 10, 270–4. [Google Scholar]
- Johnston, C.E.; Birch, J.G.; Daniels, J.L. Cervical Kyphosis in Patients Who Have Larsen Syndrome*. J. Bone Jt. Surg. 1996, 78, 538–45. [Google Scholar] [CrossRef]
- Krakow, D.; Robertson, S.P.; King, L.M.; Morgan, T.; Sebald, E.T.; Bertolotto, C.; Wachsmann-Hogiu, S.; Acuna, D.; Shapiro, S.S.; Takafuta, T.; et al. Mutations in the gene encoding filamin B disrupt vertebral segmentation, joint formation and skeletogenesis. Nat. Genet. 2004, 36, 405–410. [Google Scholar] [CrossRef]
- Zhang, D.; Herring, J.A.; Swaney, S.S.; et al. Mutations responsible for Larsen syndrome cluster in the FLNB protein. J Med Genet 2006, 43, e24. [Google Scholar] [CrossRef] [PubMed]
- Hermanns, P.; Unger, S.; Rossi, A.; Perez-Aytes, A.; Cortina, H.; Bonafé, L.; Boccone, L.; Setzu, V.; Dutoit, M.; Sangiorgi, L.; et al. Congenital Joint Dislocations Caused by Carbohydrate Sulfotransferase 3 Deficiency in Recessive Larsen Syndrome and Humero-Spinal Dysostosis. Am. J. Hum. Genet. 2008, 82, 1368–1374. [Google Scholar] [CrossRef]
- De La Rocha, A.; Birch, J.G.; Schiller, J.R. Precocious appearance of the capital femoral nucleus in Larsen Syndrome. J Bone Joint Surg Am 2012, 94, pe55. [Google Scholar] [CrossRef]
- Curtis, B.H.; Fisher, R.L. Congenital hyperextension with anterior subluxation of the knee. Surgical treatment and long-term observations. J Bone Joint Surg Am. 1969, 51, 255–1969. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, A.; Asenjo, B.; Dominguez, R.; Lemaire, R. [Larsen syndrome: multicenter study of 12 new cases. Diagnosis, planning and results of treatment]. Acta Orthop Belg 1994, 60, 259–73. [Google Scholar] [PubMed]
- Morcuende, J.A.; Dolan, L.A.; Dietz, F.R.; Ponseti, I.V. Radical Reduction in the Rate of Extensive Corrective Surgery for Clubfoot Using the Ponseti Method. Pediatrics 2004, 113, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Gerlach, D.J.; A Gurnett, C.; Limpaphayom, N.; Alaee, F.; Zhang, Z.; Porter, K.; Kirchhofer, M.; Smyth, M.D.; Dobbs, M.B. Early Results of the Ponseti Method for the Treatment of Clubfoot Associated with Myelomeningocele. J. Bone Jt. Surg. 2009, 91, 1350–1359. [Google Scholar] [CrossRef] [PubMed]
- Merrill RK, Ishmael TG, Samdani AF, Hwang SW, Pahys JM. Severe Cervical Kyphosis and Spondyloptosis with Myelopathy in Larsen Syndrome: 2021. A Report of 2 Cases. JBJS Case Connect. 4;11(3).
- McKay, S.D.; Al-Omari, A.; Tomlinson, L.A.; Dormans, J.P. Review of Cervical Spine Anomalies in Genetic Syndromes. Spine 2012, 37, E269–E277. [Google Scholar] [CrossRef] [PubMed]
- Armouti, M.; Hirbawi, H.; Jadaan, M.; Hashem, H.; Muhsen, B.A. Surgical management of cervical kyphosis in larsen syndrome. Case report and review of literature. Ann. Med. Surg. 2022, 75, 103372. [Google Scholar] [CrossRef] [PubMed]
- Unger, S.; Lausch, E.; Rossi, A.; Mégarbané, A.; Sillence, D.; Alcausin, M.; Aytes, A.; Mendoza-Londono, R.; Nampoothiri, S.; Afroze, B.; et al. Phenotypic features of carbohydrate sulfotransferase 3 (CHST3) deficiency in 24 patients: Congenital dislocations and vertebral changes as principal diagnostic features. Am. J. Med Genet. Part A 2010, 152A, 2543–2549. [Google Scholar] [CrossRef]
- Chen, H.; Chang, C.-H.; Perrin, E.; et al. A lethal, Larsen-like multiple joint dislocation syndrome. Am J Med Genet 1982, 13, 149–161. [Google Scholar] [CrossRef]
- Clayton-Smith, J.; Donnai, D. A further patient with the lethal type of Larsen syndrome. J. Med Genet. 1988, 25, 499–500. [Google Scholar] [CrossRef]
- Caksen, H.; Kurtoğlu, S. Larsen syndrome associated with severe congenital hydrocephalus. Genet. Couns. 2001, 12, 369–72. [Google Scholar]
- Hall, C.M.; Elcioglu, N.H.; MacDermot, K.D.; Offiah, A.C.; Winter, R.M. Spondyloepimetaphyseal dysplasia with multiple dislocations (Hall type): three further cases and evidence of autosomal dominant inheritance. J. Med Genet. 2002, 39, 666–670. [Google Scholar] [CrossRef]
- Cohen MM Jr. Craniosynostosis: Diagnosis, Evaluation, and Management. 1986. New York, Raven Press.
- Escobar, L.F.; Bixler, D.; Weaver, D.D.; et al. Larsen syndrome and craniosynostosis: Idaho syndrome? Dysmorph Clin Genet 1989, 3, 24–27. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).