Submitted:
23 July 2024
Posted:
24 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Post-COVID Syndrome
1.2. Mental Health Impairments in PASC
1.3. Research Objectives
2. Material and Methods
2.1. Participants and Data Collection
2.2. Measures/Variables
2.2.1. Sociodemographic and Health Related Data
2.2.2. PASC Symptoms
2.2.3. Mental Health Symptoms
Generalized Anxiety Disorder (GAD-7)
Patient Health Questionnaire (PHQ-9)
Patient Health Questionnaire (PHQ-15)
The Fatigue Severity Scale (FSS)
DePaul Post-Exertional-Malaise Screening
Psychotherapeutic Treatment
Cardiological Data
Other Data
2.3. Data Analysis
2.4. Missings
3. Results
3.1. Sociodemographic and Health Related Data
3.2. Post-COVID Related and Cardiac Variables
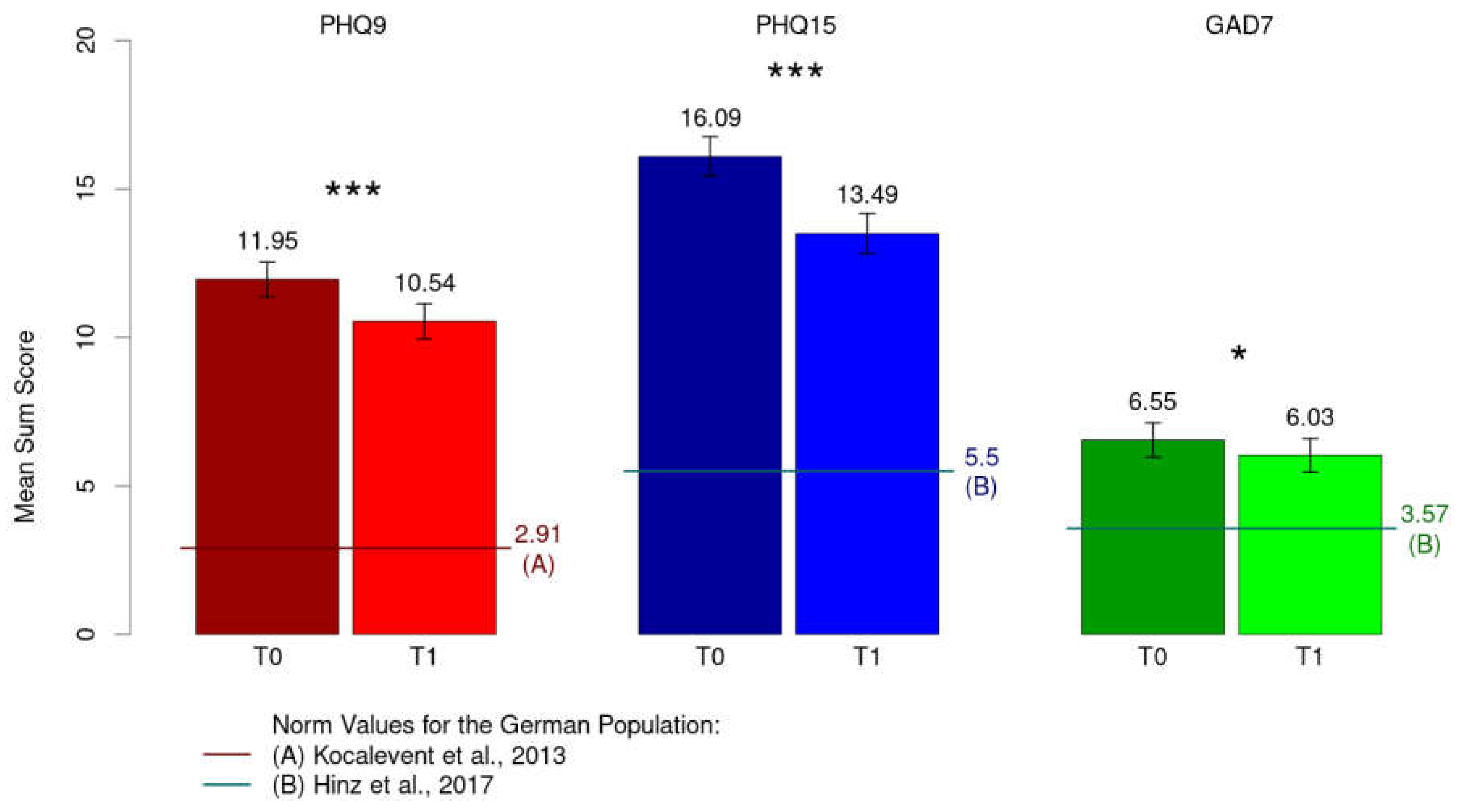
3.3. Mental Health
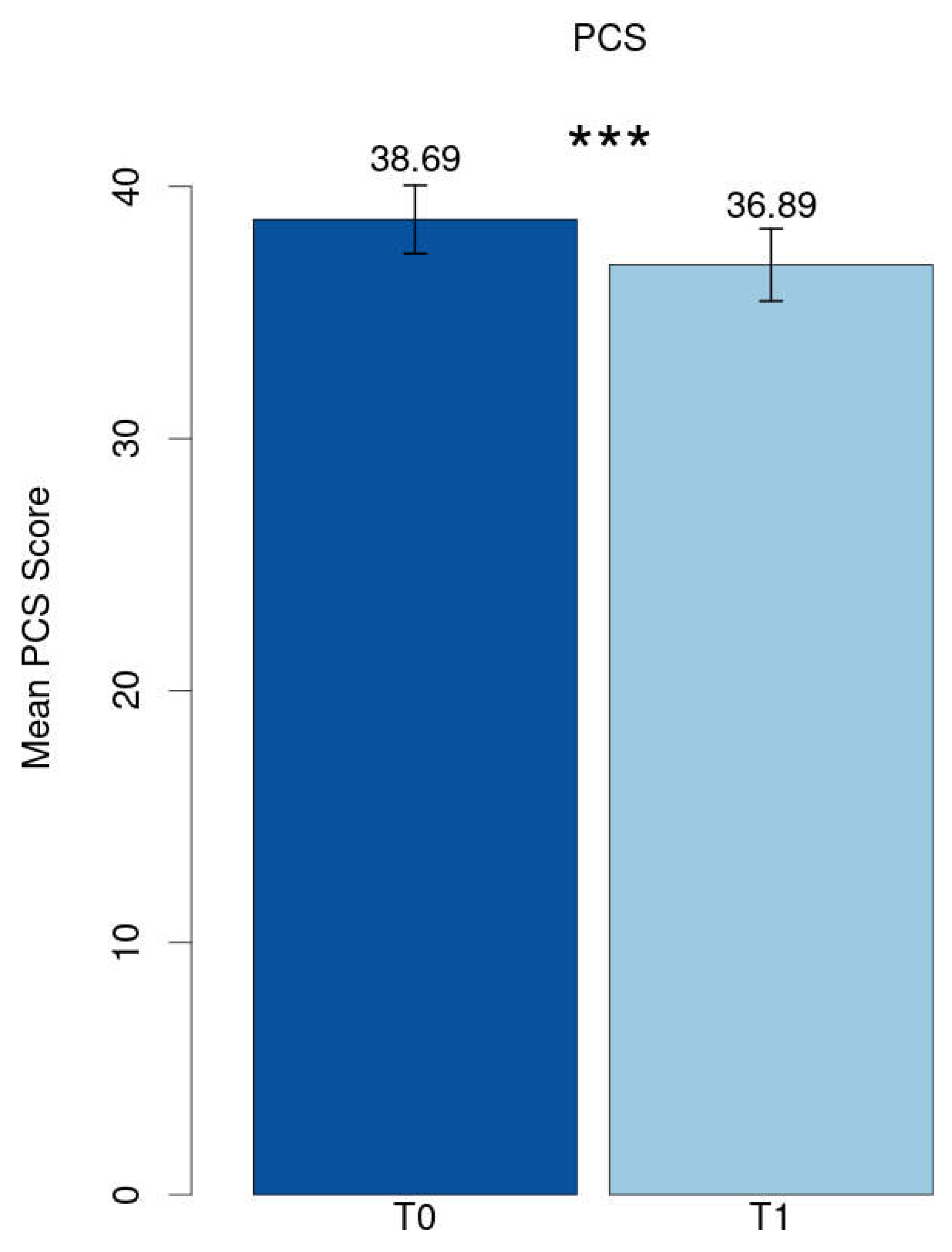
Severity of Symptoms and Development at Follow-Up
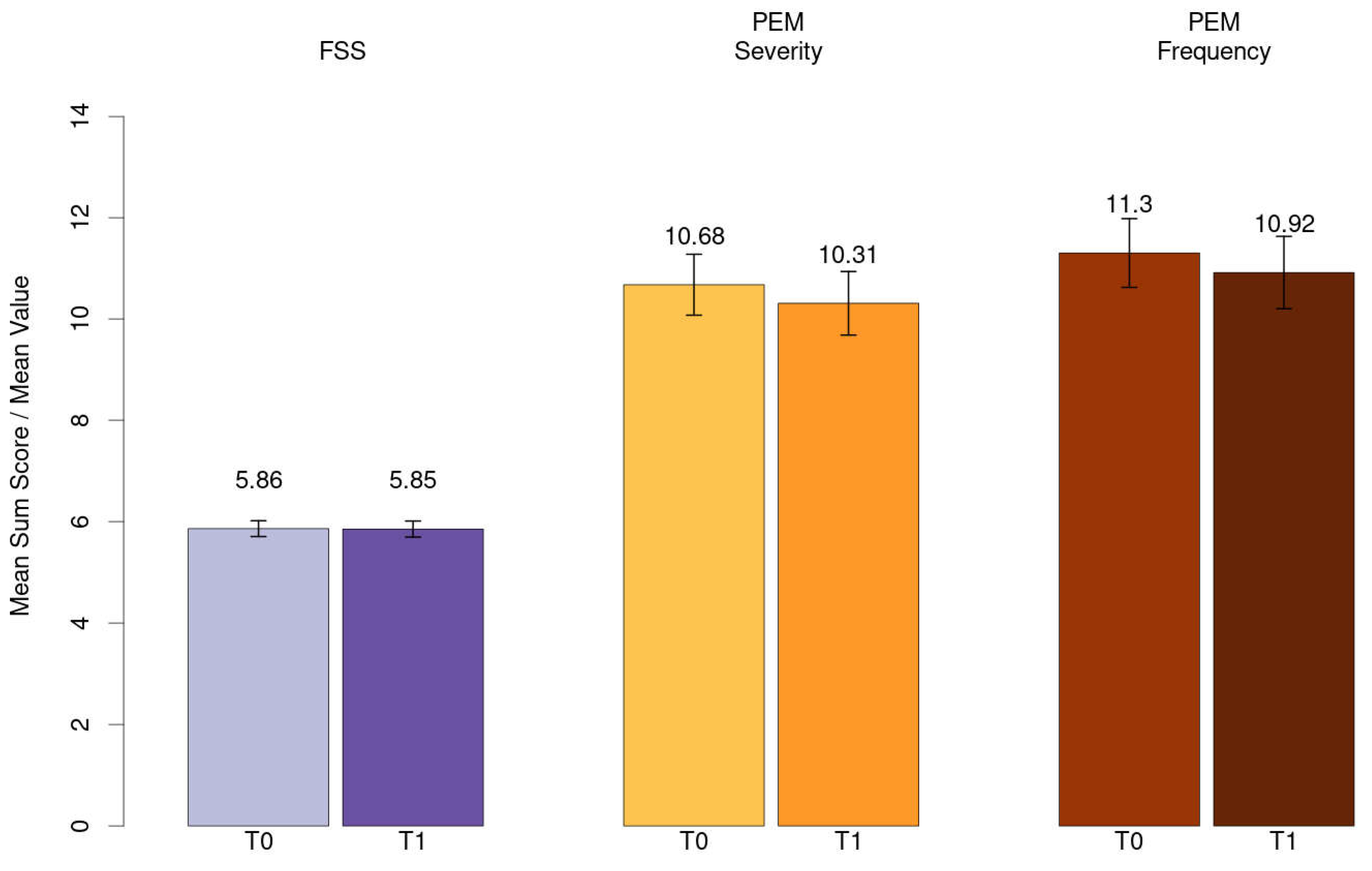
Frequency of Symptoms
3.4. Utilization of Psychotherapeutic Treatment
3.5. Mixed Model Analysis
4. Discussion
4.1. Sociodemographic and Health-Related Variables
4.2. Post-COVID Related Variables and Post-COVID Syndrome Score
4.3. Mental Health
4.3.1. Depression, Anxiety, Persisting Somatic Symptoms
4.3.2. Fatigue and Post-Exertional Malaise
4.3.3. Persistence of Symptoms
4.4. Risk and Protective Factors
4.4.1. Sociodemographic Data and Time
4.4.2. Psychotherapeutic Utilization before PASC
4.5. Strengths and Limitations
5. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgements
Conflicts of Interest
References
- WHO. Coronavirus disease (COVID-19). 2023; Available from: https://www.who.int/news-room/fact-sheets/detail/coronavirus-disease-%28covid-19%29. Last accessed on: 07.05.2024.
- guideline, N. COVID-19 rapid guideline: managing the long-term effects of COVID-19. 2020; Available from: https://www.nice.org.uk/guidance/ng188. Last accessed on: 07.05.2024.
- German Guidelines for “Long/Post COVID syndrome” 2021; Available from: https://register.awmf.org/assets/guidelines/020-027p_S1_Post_COVID_Long_COVID_2023-02.pdf. Last accessed on: 07.05.2024.
- Yong, S.J. , Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond), 2021. 53(10): p. 737-754.
- Luo, D.; Mei, B.; Wang, P.; Li, X.; Chen, X.; Wei, G.; Kuang, F.; Li, B.; Su, S. Prevalence and risk factors for persistent symptoms after COVID-19: a systematic review and meta-analysis. Clin. Microbiol. Infect. 2024, 30, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Premraj, L.; Kannapadi, N.V.; Briggs, J.; Seal, S.M.; Battaglini, D.; Fanning, J.; Suen, J.; Robba, C.; Fraser, J.; Cho, S.-M. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J. Neurol. Sci. 2022, 434, 120162–120162. [Google Scholar] [CrossRef] [PubMed]
- Morawa, E.; Krehbiel, J.; Borho, A.; Herold, R.; Lieb, M.; Schug, C.; Erim, Y. Cognitive impairments and mental health of patients with post-COVID-19: A cross-sectional study. J. Psychosom. Res. 2023, 173, 111441. [Google Scholar] [CrossRef]
- Taquet, M.; Geddes, J.R.; Husain, M.; Luciano, S.; Harrison, P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 2021, 8, 416–427. [Google Scholar] [CrossRef] [PubMed]
- Alkodaymi, M.S.; Omrani, O.A.; Fawzy, N.A.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin. Microbiol. Infect. 2022, 28, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Peghin, M.; Palese, A.; Venturini, M.; De Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Raman, B. , et al., Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine, 2021. 31: p. 100683.
- Tsampasian, V. , et al., Risk Factors Associated With Post-COVID-19 Condition: A Systematic Review and Meta-analysis. JAMA Intern Med, 2023. 183(6): p. 566-580.
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, K.M.; Vasarmidi, E.; Russell, A.-M.; Andrejak, C.; Crestani, B.; Delcroix, M.; Dinh-Xuan, A.T.; Poletti, V.; Sverzellati, N.; Vitacca, M.; et al. European Respiratory Society statement on long COVID follow-up. Eur. Respir. J. 2022, 60, 2102174. [Google Scholar] [CrossRef] [PubMed]
- Malik, P. , et al., Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis. J Med Virol, 2022. 94(1): p. 253-262.
- Zeng, N.; Zhao, Y.-M.; Yan, W.; Li, C.; Lu, Q.-D.; Liu, L.; Ni, S.-Y.; Mei, H.; Yuan, K.; Shi, L.; et al. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol. Psychiatry 2022, 28, 423–433. [Google Scholar] [CrossRef]
- Shanbehzadeh, S.; Tavahomi, M.; Zanjari, N.; Ebrahimi-Takamjani, I.; Amiri-Arimi, S. Physical and mental health complications post-COVID-19: Scoping review. J. Psychosom. Res. 2021, 147, 110525–110525. [Google Scholar] [CrossRef]
- Marchi, M.; Grenzi, P.; Serafini, V.; Capoccia, F.; Rossi, F.; Marrino, P.; Pingani, L.; Galeazzi, G.M.; Ferrari, S. Psychiatric symptoms in Long-COVID patients: a systematic review. Front. Psychiatry 2023, 14, 1138389. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re'Em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Yan, M.Z.; Li, X.; Lau, E.H.Y. Sequelae of COVID-19 among previously hospitalized patients up to 1 year after discharge: a systematic review and meta-analysis. Infection 2022, 50, 1067–1109. [Google Scholar] [CrossRef] [PubMed]
- Tracy, M.F.; Hagstrom, S.; Mathiason, M.; Wente, S.; Lindquist, R. Emotional, mental health and physical symptom experience of patients hospitalized with COVID-19 up to 3 months post-hospitalization: A longitudinal study. J. Clin. Nurs. 2023, 33, 591–605. [Google Scholar] [CrossRef] [PubMed]
- Rass, V.; Beer, R.; Schiefecker, A.J.; Lindner, A.; Kofler, M.; Ianosi, B.A.; Mahlknecht, P.; Heim, B.; Peball, M.; Carbone, F.; et al. Neurological outcomes 1 year after COVID-19 diagnosis: A prospective longitudinal cohort study. Eur. J. Neurol. 2022, 29, 1685–1696. [Google Scholar] [CrossRef] [PubMed]
- Houben-Wilke, S.; Goërtz, Y.M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.; van Herck, M.; Burtin, C.; Posthuma, R.; Franssen, F.M.; et al. The Impact of Long COVID-19 on Mental Health: Observational 6-Month Follow-Up Study. JMIR Ment. Heal. 2022, 9, e33704. [Google Scholar] [CrossRef] [PubMed]
- Kyzar, E.J.; Purpura, L.J.; Shah, J.; Cantos, A.; Nordvig, A.S.; Yin, M.T. Anxiety, depression, insomnia, and trauma-related symptoms following COVID-19 infection at long-term follow-up. Brain, Behav. Immun. - Heal. 2021, 16, 100315. [Google Scholar] [CrossRef] [PubMed]
- Guillen-Burgos, H.F.; Galvez-Florez, J.F.; Moreno-Lopez, S.; Gonzalez, I.; Guillen, M.; Anaya, J.-M. Factors associated with mental health outcomes after COVID-19: A 24-month follow-up longitudinal study. Gen. Hosp. Psychiatry 2023, 84, 241–249. [Google Scholar] [CrossRef] [PubMed]
- van der Feltz-Cornelis, C. , et al., Prevalence of mental health conditions and brain fog in people with long COVID: A systematic review and meta-analysis. Gen Hosp Psychiatry, 2024. 88: p. 10-22.
- Natarajan, A.; Shetty, A.; Delanerolle, G.; Zeng, Y.; Zhang, Y.; Raymont, V.; Rathod, S.; Halabi, S.; Elliot, K.; Shi, J.Q.; et al. A systematic review and meta-analysis of long COVID symptoms. Syst. Rev. 2023, 12, 1–19. [Google Scholar] [CrossRef]
- Peter, R.S.; Nieters, A.; Kräusslich, H.-G.; O Brockmann, S.; Göpel, S.; Kindle, G.; Merle, U.; Steinacker, J.M.; Rothenbacher, D.; Kern, W.V. Post-acute sequelae of covid-19 six to 12 months after infection: population based study. BMJ 2022, 379, e071050. [Google Scholar] [CrossRef]
- Legler, F. , et al., Long-term symptom severity and clinical biomarkers in post-COVID-19/chronic fatigue syndrome: results from a prospective observational cohort. EClinicalMedicine, 2023. 63: p. 102146.
- Mazza, M.G.; Palladini, M.; De Lorenzo, R.; Magnaghi, C.; Poletti, S.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; Benedetti, F. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: Effect of inflammatory biomarkers at three-month follow-up. Brain, Behav. Immun. 2021, 94, 138–147. [Google Scholar] [CrossRef]
- Choutka, J.; Jansari, V.; Hornig, M.; Iwasaki, A. Unexplained post-acute infection syndromes. Nat. Med. 2022, 28, 911–923. [Google Scholar] [CrossRef]
- Bahmer, T.; Borzikowsky, C.; Lieb, W.; Horn, A.; Krist, L.; Fricke, J.; Scheibenbogen, C.; Rabe, K.F.; Maetzler, W.; Maetzler, C.; et al. Severity, predictors and clinical correlates of Post-COVID syndrome (PCS) in Germany: A prospective, multi-centre, population-based cohort study. eClinicalMedicine 2022, 51, 101549. [Google Scholar] [CrossRef]
- Spitzer, R.L. , et al., A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med, 2006. 166(10): p. 1092-7.
- Kroenke, K., R. L. Spitzer, and J.B. Williams, The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 2001. 16(9): p. 606-13.
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-15: Validity of a New Measure for Evaluating the Severity of Somatic Symptoms. Psychosom. Med. 2002, 64, 258–266. [Google Scholar] [CrossRef]
- Valko, P.O. , et al., Validation of the fatigue severity scale in a Swiss cohort. Sleep, 2008. 31(11): p. 1601-7.
- Jason, L. and L. Froehlich, DePaul Symptom Questionnaire - Short Form & Post Exertional Malaise (DSQ-SF & DSQ-PEM) German Translation. 2022.
- Kocalevent, R.-D.; Hinz, A.; Brähler, E. Standardization of the depression screener Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2013, 35, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Hinz, A.; Ernst, J.; Glaesmer, H.; Brähler, E.; Rauscher, F.G.; Petrowski, K.; Kocalevent, R.-D. Frequency of somatic symptoms in the general population: Normative values for the Patient Health Questionnaire-15 (PHQ-15). J. Psychosom. Res. 2017, 96, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Hinz, A.; Klein, A.M.; Brähler, E.; Glaesmer, H.; Luck, T.; Riedel-Heller, S.G.; Wirkner, K.; Hilbert, A. Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J. Affect. Disord. 2017, 210, 338–344. [Google Scholar] [CrossRef]
- Walker, S.; Goodfellow, H.; Pookarnjanamorakot, P.; Murray, E.; Bindman, J.; Blandford, A.; Bradbury, K.; Cooper, B.; Hamilton, F.L.; Hurst, J.R.; et al. Impact of fatigue as the primary determinant of functional limitations among patients with post-COVID-19 syndrome: a cross-sectional observational study. BMJ Open 2023, 13, e069217. [Google Scholar] [CrossRef] [PubMed]
- Wahlgren, C.; Forsberg, G.; Divanoglou, A.; Balkhed, ..; Niward, K.; Berg, S.; Levi, R. Two-year follow-up of patients with post-COVID-19 condition in Sweden: a prospective cohort study. Lancet Reg. Heal. - Eur. 2023, 28, 100595. [Google Scholar] [CrossRef]
- Kim, Y.; Bae, S.; Chang, H.-H.; Kim, S.-W. Characteristics of long COVID and the impact of COVID-19 vaccination on long COVID 2 years following COVID-19 infection: prospective cohort study. Sci. Rep. 2024, 14, 1–12. [Google Scholar] [CrossRef]
- Lemhöfer, C.; Bahmer, T.; Baumbach, P.; Besteher, B.; Boekel, A.; Finke, K.; Katzer, K.; Lehmann-Pohl, K.; Lewejohann, J.-C.; Loudovici-Krug, D.; et al. Variations and Predictors of Post-COVID Syndrome Severity in Patients Attending a Post-COVID Outpatient Clinic. J. Clin. Med. 2023, 12, 4013. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.K.; Khedr, E.M.; Hamad, D.A.; Meshref, T.S.; Hashem, M.M.; Aly, M.M. Long term impact of Covid-19 infection on sleep and mental health: A cross-sectional study. Psychiatry Res. 2021, 305, 114243–114243. [Google Scholar] [CrossRef] [PubMed]
- Seighali, N.; Abdollahi, A.; Shafiee, A.; Amini, M.J.; Athar, M.M.T.; Safari, O.; Faghfouri, P.; Eskandari, A.; Rostaii, O.; Salehi, A.H.; et al. The global prevalence of depression, anxiety, and sleep disorder among patients coping with Post COVID-19 syndrome (long COVID): a systematic review and meta-analysis. BMC Psychiatry 2024, 24, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Schou, T.M.; Joca, S.; Wegener, G.; Bay-Richter, C. Psychiatric and neuropsychiatric sequelae of COVID-19 – A systematic review. Brain, Behav. Immun. 2021, 97, 328–348. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; Palladini, M.; Villa, G.; De Lorenzo, R.; Querini, P.R.; Benedetti, F. Prevalence, trajectory over time, and risk factor of post-COVID-19 fatigue. J. Psychiatr. Res. 2022, 155, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Scott, E.S.; Lubetkin, E.I.; Janssen, M.F.; Yfantopolous, J.; Bonsel, G.J.; Haagsma, J.A. Cross-sectional and longitudinal comparison of health-related quality of life and mental well-being between persons with and without post COVID-19 condition. Front. Epidemiology 2023, 3, 1144162. [Google Scholar] [CrossRef] [PubMed]
- Bota, A.V.; Bogdan, I.; Razvan, D.V.; Ilie, A.C.; Tudor, R.; Indries, M.F.; Csep, A.N.; Marincu, I. A Three-Year Cross-Sectional Analysis of Depression, Anxiety, and Quality of Life in Patients with Post-COVID-19 Syndrome. Int. J. Gen. Med. 2024, ume 17, 751–762. [Google Scholar] [CrossRef]
- Lier, J.; Stoll, K.; Obrig, H.; Baum, P.; Deterding, L.; Bernsdorff, N.; Hermsdorf, F.; Kunis, I.; Bräsecke, A.; Herzig, S.; et al. Neuropsychiatric phenotype of post COVID-19 syndrome in non-hospitalized patients. Front. Neurol. 2022, 13, 988359. [Google Scholar] [CrossRef] [PubMed]
- Poole-Wright, K.; Guennouni, I.; Sterry, O.; A Evans, R.; Gaughran, F.; Chalder, T. Fatigue outcomes following COVID-19: a systematic review and meta-analysis. BMJ Open 2023, 13, e063969. [Google Scholar] [CrossRef] [PubMed]
- Diem, L.; Fregolente-Gomes, L.; Warncke, J.D.; Hammer, H.; Friedli, C.; Kamber, N.; Jung, S.; Bigi, S.; Funke-Chambour, M.; Chan, A.; et al. Fatigue in Post-COVID-19 Syndrome: Clinical Phenomenology, Comorbidities and Association With Initial Course of COVID-19. J. Central Nerv. Syst. Dis. 2022, 14. [Google Scholar] [CrossRef]
- Jason, L.A.; Dorri, J.A. ME/CFS and Post-Exertional Malaise among Patients with Long COVID. Neurol. Int. 2022, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nehme, M.; Chappuis, F.; Kaiser, L.; Assal, F.; Guessous, I. The Prevalence, Severity, and Impact of Post-COVID Persistent Fatigue, Post-Exertional Malaise, and Chronic Fatigue Syndrome. J. Gen. Intern. Med. 2022, 38, 835–839. [Google Scholar] [CrossRef] [PubMed]
- Koczulla, A.R. , et al., [S1 Guideline Post-COVID/Long-COVID]. Pneumologie, 2021. 75(11): p. 869-900.
- Holtzman, C.S.; Bhatia, S.; Cotler, J.; Jason, L.A. Assessment of Post-Exertional Malaise (PEM) in Patients with Myalgic Encephalomyelitis (ME) and Chronic Fatigue Syndrome (CFS): A Patient-Driven Survey. Diagnostics 2019, 9, 26. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal Coagulation Parameters Are Associated with Poor Prognosis in Patients with Novel Coronavirus Pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef] [PubMed]
- Hazumi, M.; Usuda, K.; Okazaki, E.; Kataoka, M.; Nishi, D. Differences in the Course of Depression and Anxiety after COVID-19 Infection between Recovered Patients with and without a Psychiatric History: A Cross-Sectional Study. Int. J. Environ. Res. Public Heal. 2022, 19, 11316. [Google Scholar] [CrossRef] [PubMed]
- Sauer, M.C.; Barlow, P.B.; Comellas, A.P.; Garg, A. Anxiety and depression symptoms among patients with long COVID: a retrospective cohort study. Eur. Arch. Psychiatry Clin. Neurosci. 2024, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, R.; Cerda, I.H.; Ibrahim, A.; Chen, J.A.; Stevens, C.; Liu, C.H. Long COVID and psychological distress in young adults: Potential protective effect of a prior mental health diagnosis. J. Affect. Disord. 2023, 340, 639–648. [Google Scholar] [CrossRef]
| Variables | Sample at baseline (n = 265) |
|---|---|
|
Gender, n (%) Women Men Missing |
187 (70.6) 75 (28.3) 3 (1.1) |
|
Age, years M (SD) Range |
45, 5 (12.1) 19 - 79 |
|
Marital status, n (%) Single without partnership Single with partnership Married In separation Widowed Divorced Missing |
46 (17.4) 43 (16.2) 157 (59.2) 2 (0.8) 2 (0.8) 12 (4.5) 3 (1.1) |
|
Children, n (%) Yes No Missing |
161 (60.8) 101 (38.1) 3 (1.1) |
|
Education level, n (%) Without certificate Lower secondary school certificate Secondary school certificate High school certificate Other Missing |
1 (0.4) 44 (16.6) 86 (32.5) 128 (48.3) 3 (1.2) 3 (1.1) |
|
Professional qualification, n (%) None Master school Apprenticeship certificate University degree Missing |
13 (4.9) 54 (20.4) 97 (36.6) 97 (36.6) 4 (1.5) |
|
Employment status, n (%) Full-time employed Part-time employed Unemployed Retired / pensioned Sick leave / incapacitated for work Other Missing |
88 (33.2) 74 (27.9) 14 (5.3) 18 (6.8) 40 (15.0) 27 (10.3) 4 (1.5) |
|
Smoking, n (%) Yes No Missing |
19 (7.2) 238 (89.8) 8 (3.0) |
|
BMI, kg/m2 M (SD) Range < 18,5 (n, %) 18,5 – 24,9 (n, %) ≥ 25 – 29,9 (n, %) > 30 – 39,9 (n, %) > 40 (n, %) Missing |
26.2 (5.4) 16.6 – 49.6 9 (3.4) 116 (43.8) 80 (30.2) 53 (20.0) 4 (1.5) 3 (1.1) |
|
Self-reported pre-existing disease, n (%) 1 Yes No Hormonal or metabolic Psychiatric diseases Nervous system Cardiovascular system Respiratory system Muskolosceletal and connective tissue Digestive system Dermatological Other |
112 (42.3) 153 (57.7) 37 (14) 25 (9.4) 7 (2.6) 18 (6.8) 28 (10.6) 24 (9.1) 20 (7.5) 16 (6.0) 32 (12.1) |
| Variables | Sample at follow-up (n = 265) |
|---|---|
|
Time since the SARS-CoV-22 infection and baseline, months M (SD) Range |
17.1 (8.7) 3-42 |
|
Time since the SARS-CoV-22 infection and follow-up, months M (SD) Range |
22.5 (8.2) 10-47 |
|
Time since baseline and follow-up, months M (SD) Range |
5.0 (2.4) 3-11 |
|
Course of the acute SARS-CoV-2 infection, n (%) Asymptomatic Symptomatic, therapy at home or outpatient Symptomatic, inpatient therapy without intensive care admission Symptomatic, inpatient therapy with intensive care admission |
14 (5.3) 224 (84.5) 21 (7.9) 6 (2.3) |
|
PCR, n (%) Carried out Not carried out |
236 (89.1) 29 (10.9) |
|
Vaccine, n (%) None 1x 2x 3x 4x 5x |
14 (5.3) 11 (4.2) 58 (21.9) 154 (58.1) 24 (9.1) 4 (1.5) |
|
Cardiac pathology, n (%) 1 Yes (Scores 1-3) No (Score 0) Missing Ejection fraction Pulmonic artery pressure elevation Left ventricle dilatation Pericardial effusion present Atrial fibrillation |
28 (10.6) 197 (74.3) 40 (15.1) 3 (1.1) 5 (1.9) 9 (3.4) 13 (4.9) 0 (0.0) |
| Variables | Sample at baseline (n = 265) 1 | Sample at follow-up (n = 265) |
|---|---|---|
| Post-COVID Symptom Score (PCS-S), cut-off >26.25 n (%) | 224 (84.5) | 214 (80.8) |
| Fatigue-Severity Scale (FSS), cut-off ≥4 n (%) | 237 (89.4) | 237 (89.4) |
| Patient Health Questionnaire 9 (PHQ-9), cut-off ≥10 n (%) | 181 (68.3) | 148 (55.8) |
| Generalized Anxiety Disorder 7 (GAD-7), cut-off ≥10 n (%) | 64 (24.2) | 50 (18.9) |
| Patient Health Questionnaire 15 (PHQ-15), cut-off >10 n (%) | 230 (86.8) | 192 (72.5) |
| Variable | ||||
|---|---|---|---|---|
| Outcome Measure (Coefficient, [95% Confidence Interval], p-value) | PHQ-91 | PHQ-152 | GAD-73 | FSS4 |
| Intercept | 7.830, [4.104; 11.556], <0.001* | 17.206, [12.929; 21.483], <0.001 | 4.748, [1.274; 8.222], 0.008 | 5.102, [4.12; 6.084], <0.001 |
| Sex (Male) | 0.120, [-1.20; 1.441], 0.858 | -1.321, [-2.847; 0.205], 0.091 | 0.318, [-0.911; 1.547], 0.612 | 0.001, [-0.346; 0.349], 0.995 |
| Age | 0.064, [0.011; 0.117], 0.018 | -0.003, [-0.063; 0.058], 0.927 | 0.027, [-0.022; 0.076], 0.284 | 0.009, [-0.005; 0.023], 0.216 |
| BMI ≥25 | 0.371, [-0.777; 1.519], 0.527 | -0.532, [-1.758; 0.694], 0.396 | 0.096, [-0.001; 1.184], 0.862 | -0.173, [-0.481; 0.134], 0.27 |
| Smoker | -0.889, [-2.567; 0.789], 0.3 | -1.425, [-3.2; 0.35], 0.116 | -0.767, [-2.316; 0.827], 0.346 | -0.093, [-0.543; 0.357], 0.685 |
| Pathologic echocardiography | -0.409, [-2.22;1.404], 0.659 | 0.219, [-1.88; 2.317], 0.839 | 0.545, [-1.14; 2.23], 0.527 | -0.274, [-0.751; 0.203], 0.261 |
| Working | -0.806, [-1.924; 0.312], 0.659 | -0.453, [-1.537; 0.631], 0.413 | -0.430, [-1.518; 0.658], 0.439 | -0.234, [-0.539; 0.071], 0.133 |
| Not working | -0.630, [-1.848; 0.588], 0.311 | 0.102, [-1.077; 1.281], 0.866 | -0.382, [-1.569; 0.804], 0.528 | -0.077, [-0.412; 0.258], 0.651 |
| Prior psychiatric illness without prior psychotherapy | -3.641, [-8.752; 1.471], 0.164 | -2.604, [-8.523; 3.314], 0.389 | -0.386, [-5.139; 4.366], 0.874 | 0.047, [-1.299; 1.393], 0.945 |
| Prior psychiatric illness with prior psychotherapy | 2.370, [0.186; 4.554], 0.035 | 3.566, [1.039; 6.039], 0.006 | 2.159, [0.128; 4.191], 0.038 | 0.424, [-0.151; 1], 0.15 |
| Partnership (Yes) | 0.710, [-0.513; 1.933], 0.256 | 0.995, [-0.301; 2.291], 0.133 | 0.284, [-0.877; 1.444], 0.632 | -0.155, [-0.483; 0.174], 0.357 |
| Time between the acute infection and T0 | 0.000, [-0.75; 0.076], 1 | 0.024, [-0.063; 0.112], 0.586 | -0.011, [-0.081; 0.06], 0.765 | 0.013, [-0.007; 0.033], 0.207 |
| Highschool certificate | -0.603, [-1.841; 0.635], 0.341 | -1.178, [-2.604; 0.249], 0.107 | -0.543, [-1.696; 0.609], 0.357 | 0.035, [-0.291; 0.36], 0.834 |
| Acute infection with inpatient treatment | 0.080, [-1.899; 2.059], 0.937 | 0.898, [-1.396; 3.192], 0.444 | 1.278, [-0.561; 3.118], 0.175 | -0.213, [-0.734; 0.308], 0.424 |
| Number of vaccinations | 0.364, [-0.287; 1.016], 0.275 | -0.287, [-1.042; 0.468], 0.457 | 0.165, [-0.441; 0.771], 0.595 | 0.141, [-0.031; 0.312], 0-109 |
| Time to T1 | -1.613, [-2.158; -1.069], <0.001 | -2.716, [-3.209; -2.223], <0.001 | -0.621, [-1.164; -0.078], 0.026 | -0.045, [-0.198; 0.108], 0.565 |
| Outcome Measure (Coefficient, 95% Confidence Interval, p-value) | PCS-S5 | PEM Frequency6 | PEM Severity7 | |
| Intercept | 34.203, [25.427; 42.978], <0.001 | 8.719, [4.25; 13.189], <0.001 | 9.262, [5.369; 13.154], <0.001 | |
| Sex (Male) | -2.762, [-5.883; 0.359], 0.084 | 0.408, [-1.187; 2.004], 0.616 | 0.227, [-1.163; 1.617], 0.749 | |
| Age | 0.095, [-0.03; 0.219], 0.138 | -0.004, [-0.068; 0.061], 0.91 | -0.013, [-0.069; 0.044], 0.661 | |
| BMI ≥25 | -0.915, [3.565; 1.734], 0.499 | -0.451, [-1.817; 0.916], 0.518 | 0.045, [-1.137; 1.228], 0.94 | |
| Smoker | -0.530, [-4.388; 3.328], 0.788 | -0.439, [-2.54; 1.662], 0.682 | -0.160, [-1.98; 1.659], 0.863 | |
| Pathologic echocardiography | -1.554, [-5.843; 2.734], 0.478 | -1.327, [-3.522; 0.867], 0.237 | -0.707, [-2.619; 1.206], 0.47 | |
| Working | -1.847, [-4.318; 0.623], 0.144 | -0.516, [-1.763; 0.731], 0.418 | -0.549, [-1.617; 0.518], 0.314 | |
| Not working | 1.103, [-1.612; 3.818], 0.427 | 0.235, [-1.141; 1.611], 0.738 | 0.462, [-0.717; 1.641], 0.443 | |
| Prior psychiatric illness without prior psychotherapy | -3.446, [-15.541; 8.648], 0.577 | 2.068, [-4.099; 8.236], 0.512 | 1.747, [-3.629; 7.123], 0.525 | |
| Prior psychiatric illness with prior psychotherapy | 5.509, [0.342; 10.676], 0.038 | 1.462, [-1.167; 4.092], 0.277 | 1.421, [-0.871; 3.713], 0.226 | |
| Partnership (Yes) | -0.227, [-3.046; 2.592], 0.875 | -0.066, [-1.497; 1.365], 0.928 | -0.240, [-1.477; 0.997], 0.704 | |
| Time between the acute infection and T0 | 0.131, [-0.047; 0.309], 0.151 | 0.112, [0.021; 0.203], 0.017 | 0.085, [0.005; 0.164], 0.038 | |
| Highschool certificate | -0.522, [-3.441; 2.397], 0.726 | -0.499, [-1.993; 0.995], 0.513 | -0.740, [-2.042; 0.561], 0.266 | |
| Acute infection with inpatient treatment | -2.500, [-7.184; 2.183], 0.297 | -1.559, [-3.943; 0.826], 0.202 | -1.267, [-3.345; 0.812], 0.234 | |
| Number of vaccinations | 0.014, [-1.527; 1.554], 0.986 | 0.378, [-0.407; 1.162], 0.347 | 0.298, [-0.386; 0.982], 0.394 | |
| Time to T1 | -2.233, [-3.413; -1.054], <0.001 | -0.422, [-1.017; 0.174], 0.167 | -0.425, [-0.959; 0.055], 0.082 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




