1. Introduction
Plantar fasciitis is one of the most common causes of heel pain; the pain is more acute in the morning, tends to decrease during the day with movement, and flares up after sitting for a long time [
1]. It presents as inflammation and simultaneous degeneration of the insertion of the fascia that covers the muscles present at the sole of the foot, with progressive evolution with calcification of the insertion. The incidence is between 9 and 20% of the population, with a higher incidence in middle-aged obese women and young male runners [
2]. The diagnosis is based on radiography, to verify any district deformities or the presence of the spur under the heel, and ultrasound, to verify the integrity of the fascia and its thickening. Magnetic resonance imaging (MRI) images are useful for evaluating the calcaneus and plantar fascia, particularly for distinguishing various causes of calcaneal pain, including stress fractures, tarsal tunnel syndrome, and Achilles tendinopathy [
3]. Signal alteration with bone edema is found in association with plantar fasciitis. This nonspecific sign could be the result of avulsive trauma, stress fractures, intrabony fractures, or a combination of these situations. These findings are similar to those described in the elbow in some patients suffering from epicondylitis, in which repeated overuse could be the cause of increased bone edema [
4].
Previous studies have highlighted the presence of bone edema at the calcaneal level on MRI in 35% of patients suffering from plantar fasciitis [
5,
6]. In shock wave treatment, the presence of bone edema of the calcaneus could be a highly predictive factor for a better response [
7]. Therefore, while the presence of fascia thickening and soft tissue signal changes would not correlate with the clinical response, the presence of bone edema could be highly predictive for a response to biostimulation.
Standard treatments for plantar fasciitis include stretching exercises of the posterior muscle chain and plantar fascia, taking anti-inflammatories, cortisone infiltration or biostimulation with physical therapies (laser therapy, shock waves, ultrasound therapy, etc). In forms that do not respond to conservative treatments, surgical treatment is opted for.
Laser therapy is a physical therapy that uses a form of electromagnetic radiation emission, characterized by monochromaticity, collimation, coherence and high brightness of the light [
9]. These characteristics guarantee biological effects in cells: increased ATP production, increased activity of membrane enzymes, increased DNA and RNA synthesis, acceleration of electrolyte exchange between the cell and the extra-cellular space [
9]. Furthermore, at the tissue level, vasodilation, reduction of intra-capillary pressure, increased excitability of nerve fibers and stimulation of the immune response occurs [
10]. Recently, the application of high intensity laser therapy is finding space in the treatment of tendinopathies supported by the proliferative, analgesic and inflammation-modulating effects on the musculoskeletal system [
11,
12,
13].
The aim of this study was to investigate the relationship between bone edema and outcomes of temperature controlled high energy adjustable multi-mode emission laser and/or exercises in patients with plantar fasciitis.
2. Materials and Methods
We conducted a prospective randomized clinical trial. Patients who came to our clinic with a diagnosis of a plantar fasciitis with or without bone edema were included in our study and gave written informed consent to participate.
The inclusion criteria are as follows: history of heel pain for at least 3 months before enrollment; pain on palpation of the medial calcaneal tubercle or proximal plantar fascia; plantar fascia thickness of 4.0 mm or greater.
The exclusion criteria are as follows: age under 18 years, history of systemic diseases; pregnancy; previous lower limb surgery; a diagnosis of fibromyalgia, neurologic disease, Achilles tendinopathy, metatarsalgia, acute ankle sprain, tarsal tunnel syndrome, or heel spur syndrome; body mass index (BMI) greater than 35 kg/m2; wounds, infections in the treatment area; altered sensation in the area to be treated; changes in skin pigmentation in the area to be treated (tattooing, birthmarks); metal implants in the treatment area; treatment with oral or injected corticosteroids within the last six weeks; diagnosis of neurological heel pain (radiculopathy); diagnosis of systemic inflammatory arthritis (rheumatoid arthritis, etc.); other acute pathologies (fever, cold, etc.) requiring treatment; other painful conditions that require painkillers (toothache, back pain, etc.); tumor, cardiac pacemaker or other device.
For each patient, the epidemiological and anthropometric variables (age, gender, weight, height, BMI, smoking habit) and the clinical characteristics (site of the pathology, heel spur, duration, previous therapies and clinical outcomes). Each patient was evaluated at the beginning of treatment (T0) and after two (T1) and six months (T2). The Visual Analogue Scale (VAS) quantified pain (score of increasing pain intensity from 0 to 10). The Foot Functional Index (FFI) (this score ranges from 0% to 100% of disability). At T1 and T2 Roles and Maudsley (RM) score was used to quantify perception of improvement by the patient (from 1 for excellent to 4 for poor). On enrolment, an echography of the plantar fascia and MRI of foot were evaluated.
At two and six months the patients were re-evaluated with an ultrasound to monitor the thickness and appearance of the plantar fascia. In the case of the first finding of bone edema, the MRI was also repeated at the two subsequent follow-ups, to monitor the bone edema. Any adverse effects were recorded: increased pain, petechiae, ecchymosis, vagal crisis.
Patients were randomized to one of two groups:
- control group: treatment with stretching exercises.
- laser group: THEAL treatment (Temperature controlled High Energy Adjustable multi-mode emission Laser) and stretching exercises.
Control Group
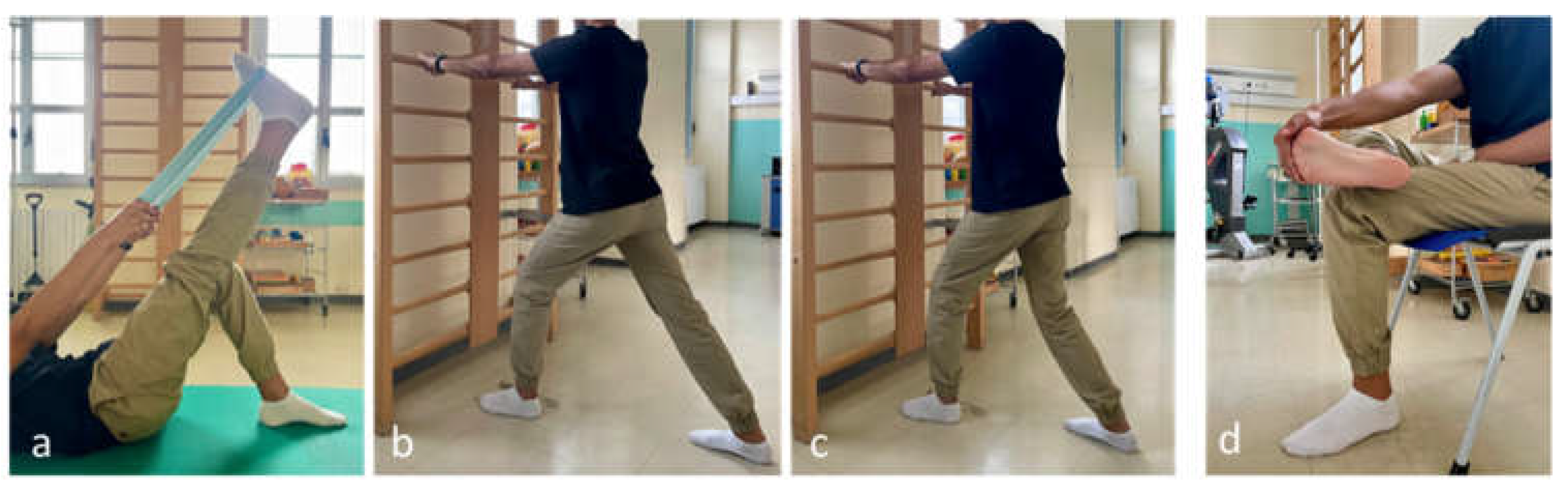
Patients were instructed to perform four daily stretching exercises (three sets of 30 seconds) for 6 weeks.
1. Stretch the hamstrings and ankle plantar flexors (supine straight leg raise).
2. Self-stretching of the calf muscles: the patient bent forward in a standing position with the affected foot furthest from the wall, keeping the heel on the floor.
3. The soleus muscle is stressed with the knee flexed and the gastrocnemius muscle with the knee extended.
4. Self-stretching of the plantar fascia: in a sitting position, the patient crosses the affected foot over the contralateral thigh and performs passive extension of the metatarsophalangeal joints (
Figure 1).
An expert physiotherapist conducted the first stretching treatment session in order to demonstrate the exercises program.
Laser Group
The Temperature controlled High Energy Adjustable multi-mode emission Laser (THEAL) was delivered with an Ixyon XP device (Mectronic, Bergamo, Italy) which allows the delivery of 4 wavelengths (650 nm, 810 nm, 980 nm and 1064 nm), with continuous and pulsed mode, average power up to 30 W, administering 10 sessions every other day. Each single session was divided into three phases, the energy parameters of which are described in
Table 1.
In the first phase, the activation of the inguinal, popliteal and malleolar lymphatic stations was envisaged for 1 minute 40 sec for each station, accompanying it with very light manual mechanical pressure (1800 J). The applicator used was small IR (Infra red), 600 J were delivered, with thermal control ranging from 40 °C – 43 °.
The second phase involved the treatment of the plantar fascia, with anti-inflammatory and biostimulant action, identifying the treatment area by approximating the surface to a 5 cm x 5 cm square and inserting the data into the device software in order to determine the time of the therapy (4 minutes 18 sec) (1750 J). The applicator was large IR, delivering the dose of 70 J/cm² with variable thermal control of 38 °C – 42 °C.
The third phase aimed to treat the latent trigger points (TP) of the tibialis and triceps surae muscles, with analgesic and decontracting action (120 J). The applicator used was IR collimated (20 sec), delivering 60 J x TP, thermal control stop at 42 °C.
The patients performed the stretching exercises at the same time, as expected in the control group.
Statistical Analysis
The primary end point was pain reduction, assessed with the VAS scale. The secondary end point was clinical improvement, assessed with FFI and Roles and Maudsley score. The tertiary end point was the instrumental improvement, with the evaluation of the reduction in the thickness of the plantar fascia (assessed by ultrasound) and the reduction of bone edema (assessed by MRI), when present at T0.
The data were collected on paper forms and then computerized into an Excel database. To estimate the sample size, a VAS value at enrollment (T0) of 6.5 was assumed for both groups [
14,
15], with a mean reduction at the primary endpoint (T2) of 4.1 in the control group [
14] and 2.6 in the laser group, with a standard deviation for both groups of 1.7. Sample estimation was performed using the t test, and a significance level (alpha) of 0.05 and a test power of 80% were set. A sample size of 44 subjects was estimated; assuming a 10% loss to follow-up, the number of subjects to be recruited is 48 (24 per group). This effect was selected as the smallest effect that would be important to detect, meaning that any smaller effect would have no clinical or substantive significance.
The assignment to the groups was carried out by randomization, with the two groups being homogeneous for the covariates, sex and diagnosis of bone edema (in relation to the hypothesis that the presence of bone edema could be a prognostic factor influencing the response).
Categorical variables were described as percentages and proportions. Quantitative variables were described as mean (± standard deviation). The changes of the VAS and FFI values and the echography-measured thickness of the plantar fascia between the study and control group over 6 months were studied via the t-student test, to verify whether the use of laser therapy improved the outcome of treatment or not. The Roles and Maudsley score at T1 and T2 were also confronted between the two groups via the t-student test for repeated measures; however, the T2 scores were confronted via the Mann-Whitney test due to non-normality of the variable’s distribution. The presence of RMI improvement between T0 and T2 was studied via Chi-squared test.
Multivariable regression was employed for all considered endpoints. The outcomes were represented by the change over time of the VAS and FFI, by the echography improvement and by the RM score at T2. The main determinants that were studied were the use of laser therapy and the presence of bone oedema, while sex, age, smoking habit, body mass index (BMI), laterality, months since diagnosis, cardiovascular comorbidities, metabolic comorbidities, previous non-steroid anti-inflammatory therapy, previous therapy and presence of spur were taken into consideration as confounders. The association was expressed as adjusted odds ratio (aOR) and 95% confidence interval (95% CI).
A p-value <0.05 was chosen as indicator of statistical significance. The database was built via Microsoft Excel®. All calculations, including the sample numerosity assessment, were performed via StataMP17®, which was also used for randomization.
3. Results
Population Characteristics
The study enrolled 48 subjects equally distributed between the laser group and the control group. A patient from the former asked to drop out of the study due to significant pain making it impossible to continue the current therapy (final distribution: 23 subjects in the laser group, 24 in the control group). The population’s characteristics are resumed in
Table 2. The mean age was 58.04 years (±9.13 years), while the mean BMI was 26.16 kg/m2 (±3.07 kg/m2). The mean time since diagnosis was 13.14 months (±13.42 months).
Endpoints
A significant reduction of the mean VAS from T0 to T1 was observed in both the laser group (t: 8.25; p-value <0.001) and the control group (t: 9.01; p-value <0.001). The mean reduction was -3.28 (±1.88). This significance was confirmed at T2 for both groups (laser group: t: 9.81; p-value <0.001; control group: t: 8.90; p-value <0.001), and the mean variation from T0 to T2 was -4.34 (±2.24).
A significant reduction from T0 to T1 was also observed for the FFI of both the laser group (t: 5.98; p-value <0.001) and the control group (t: 5.80; p-value <0.001). The mean reduction was -22.21 (±18.11). This significant reduction was confirmed from T0 to T2 in both the laser group (t: 7.73; p-value <0.001) and the control group (t: 7.34; p-value <0.001), with a mean reduction of -30.05 (±19.15).
The mean RM score at T1 was 1.96 (±0.88), while it dropped to 1.68 (±0.89) at T2. When measured via echography, the fascia plantaris of enrolled subjects had a mean thickness reduction of -0.57mm (±0.74mm) between T0 and T2; this reduction was significant for both the laser group (t: 4.67; p-value <0.001) and the control group (t: 2.85; p-value: 0.005) (
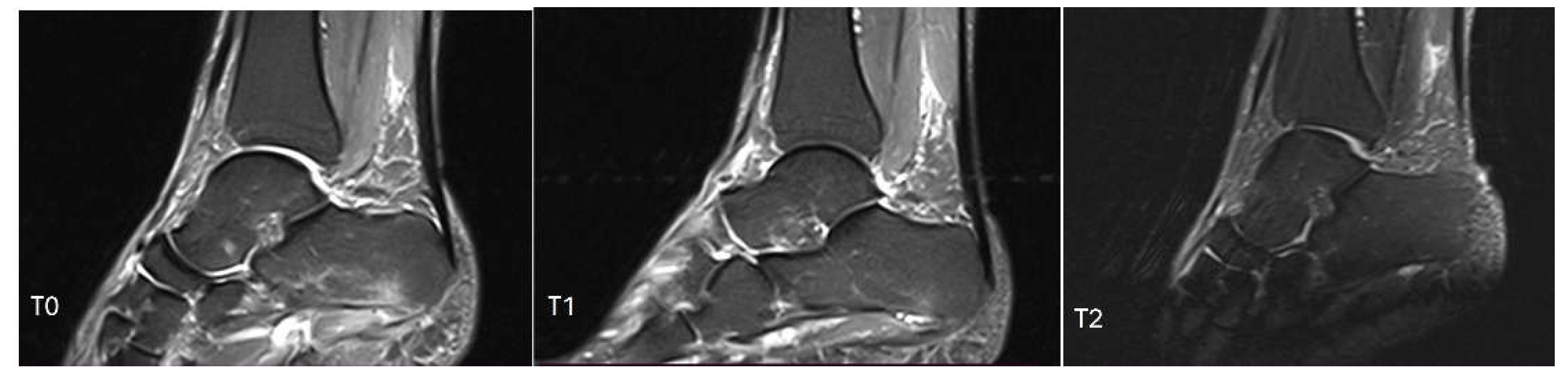
Figure 2). Finally, 12.77% of patients (6/47) showed MRI bone edema remission over time (
Figure 3). No adverse effects were recorded in the two groups. The VAS, FFI and RM score changes over time are described in
Table 3.
Inferential Statistics
Laser group showed no significant improvement in terms of both MRI (Chi2: 0.86; p-value: 0.352) and echography evaluation (t: 1.47; p-value: 0.149). The VAS modification over time was also not significantly different between the laser and control group (t: 0.67; p-value: 0.506). The FFI change over time was not significantly different, either (t: 0.07; p-value: 0.942).
The two groups did not show a significantly different RM score at T1 (t: 0.99; p-value: 0.324). However, a significant improvement was observed in the RM score at T2 (z: 2.21; 0.027) [Mann-Whitney test due to non-normal distribution].
Regression Analysis
The VAS variation over time showed to be significantly impacted by the presence of bone edema; in particular, subjects with edema showed a significantly lower reduction (aOR: 1.60; 95% CI: 0.03-3.18; p-value: 0.047). Similarly, the FFI reduction was significantly lower in case of bone edema (aOR: 14.43; 95% CI: 0.81-28.05; p-value: 0.039). All other tested independent variables were not significant in determining the changes of VAS and FFI over time (p-value >0.05).
Echography improvement, on the contrary, were significantly influenced by laser therapy, with exposed subjects having a greater reduction of the thickness of the fascia plantaris (aOR: -0.45; 95% CI: -0.89 - -0.01; p-value: 0.047). Previous physiotherapy also showed a significant influence, with reduced improvements over time (aOR: 0.62; 95% CI: 0.58-1.17; p-value: 0.032).
Finally, the RM score at T2 was significantly lower in males (aOR: -0.81; 95% CI: -1.39 - -0.23; p-value: 0.008) and in younger subjects (aOR: 0.36; 95% CI: 0.01-0.07; p-value: 0.022).
4. Discussion
In this randomized study, we compared two different conservative therapy methods in plantar fasciitis treatment. To the best of our knowledge, this is the first study that evaluates the high intensity laser therapy in fasciitis plantar also in contextual presence of calcanear bone edema.
We found that the two protocols (temperature controlled high energy adjustable multi-mode emission laser and exercises or exercises only) resulted in a significant improvement in pain, functional recovery and the perception of remission at T1 and T2. The improvements were also found in the presence of bone edema, although to a lesser extent than the VAS and FFI. The combined treatment of temperature controlled high energy adjustable multi-mode emission laser and exercises had a more important impact on the reduction in thickness of the plantar fascia and on the perception of improvement at T2. The improvement in Roles and Maudsley score was more significant in men and younger subjects.
These results are in agreement with previous studies that had investigated high intensity laser treatment (with a wavelength of 1064 nm) in plantar fasciitis. Ordahan et al. [
16] had demonstrated the effectiveness of high intensity laser therapy vs low intensity laser therapy, in association with stretching and the use of an insole. Yesil et al. [
17] have verified that high intensity laser therapy, in association with therapeutic exercise, has determined improvements in dynamic baropodometric measurements compared to placebo. On the other hand, other authors, such as Tkocz and colleagues [
18] and Naruseviciute and Kubilius [
15] had not found significant differences in favor of high intensity laser in the treatment of plantar fasciitis.
In plantar fasciitis, histological analysis has demonstrated degenerative changes at the level of the enthesis with a deterioration of collagen fibers, increased secretion of connective proteins, focal area of fibroblast proliferation and increased vascularization [
19,
20]. In the literature it is reported that calcaneal bone edema is found in 35% to 79% of patients suffering from plantar fasciitis, clinically characterized by nocturnal pain [
7,
20,
21,
22]. Therefore, some authors suggest modifying the definition of this pathology with the term “plantar fasciosis” [
20].
Various etiopathogenetic hypotheses have been put forward: one is that the inflammatory process affecting the plantar fascia is responsible for local vascular ectasia, with consequent increase in water in the skeletal compartment and subsequent increase in intraosseous pressure [
20]. Another hypothesis is that it is associated with a fatigue or stress injury to the bone, as a consequence of the pain and dysfunction of the heel [
23].
Patients in both groups in this study performed fascia and hamstring stretching exercises. A systemic review confirms the effectiveness of stretching in reducing symptoms in plantar fasciitis [
24]. The plantar fascia is made up of type 1 collagen fibers [
25], the synthesis of which is stimulated by stretching [
19,
20,
26], resulting in clinical and functional improvement.
In the laser group, a high intensity laser cycle was administered, with the simultaneous emission of 4 different wavelengths: 650 nm, which determines proliferative effects of mesenchymal cells, collagen and fibronectin [
27,
28,
29]; 810 nm, which accelerates ATP production and promotes tendon regeneration [
30]; 980 nm, which stimulates thermal and mechanical receptors and induces analgesic effects through gate control [
31]; 1064 nm, which induces anti-inflammatory effects on connective tissue ([
31]. The benefits found in reducing the thickness of the plantar fascia in these patients can be traced back to these tissue remodeling stimuli.
The clinical and functional improvement was also found in the presence of bone edema, although to a lesser extent than in patients in whom bone edema was absent. In clinical practice, laser therapy currently has no indications in the treatment of bone tissue pathologies, despite encouraging results from experimental studies, in which laser therapy stimulated the proliferation of osteoblasts [
32], induced neo-angiogenesis [
33,
34] and determined an anti-edema effect on bone tissue [
35]. On the other hand, the biological stimulus of the high intensity laser has proven to be able to significantly reduce the thickness of the fascia, confirming the biostimulating effects on the connective tissue [
36]. Limitation of the present study include the lack of a control group receiving no treatment.
Furthermore, due to the lack of longer-term follow-ups, it was not possible to verify the persistence of the benefits beyond 6 months. On the other hand, the study made it possible to monitor the effects of high intensity laser therapy even in the presence of bone edema, confirming how this may be responsible for a lower response to conservative treatment. Subsequent studies could investigate the effects of other therapies, such as extracorporeal shock waves therapy or pulsed electromagnetic fields in this pathological model.
5. Conclusions
In conclusion, the two investigated treatments of temperature controlled high energy adjustable multi-mode emission laser and exercises or exercises alone were effective in the treatment of plantar fasciitis, even in the presence of bone edema. On the other hand, when calcaneal edema was present, the clinical and functional response was lower. The high intensity laser treatment resulted in a significant reduction in the thickness of the plantar fascia, in accordance with the biostimulation effects of the connective tissue, and a better perception of clinical improvement at the end of the study.
Author Contributions
Conceptualization, NA., C.I. and M.B.; methodology, N.A. and C.I.; formal analysis, D.L.A.; investigation, C.I.; writing—original draft preparation, N.A; writing—review and editing, N.A., D.G.S., and S.G.; supervision, S.G. and M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Territorial Ethics Committee of the University Hospital Consortium of the Polyclinic of Bari (protocol code 7741, 17 May 2023). The study is registered at ClinicalTrials.gov (NCT05925777).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request due to privacy.
Acknowledgments
We gratefully acknowledge the colleagues and patients who enabled us to write this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Klein, S.E.; Dale, A.M.; Hayes, M.H.; Johnson, J.E.; McCormick, J.J.; Racette, B.A. Clinical Presentation and Self-Reported Patterns of Pain and Function in Patients with Plantar Heel Pain. Foot Ankle Int. 2012, 33, 693–698. [CrossRef]
- Hill, C.L.; Gill, T.K.; Menz, H.B.; Taylor, A.W. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. J. Foot Ankle Res. 2008, 1, 2. [CrossRef]
- Grasel, R.P.; E Schweitzer, M.; Kovalovich, A.M.; Karasick, D.; Wapner, K.; Hecht, P.J.; Wander, D.; Grasel, M.E.S.R.P.; Theodorou, D.J.; Theodorou, S.J.; et al. MR imaging of plantar fasciitis: edema, tears, and occult marrow abnormalities correlated with outcome. Am. J. Roentgenol. 1999, 173, 699–701. [CrossRef]
- Herber, S.; Kalden, P.; Kreitner, K.F.; Riedel, C.; Rompe, J.D.; Thelen, M. MRI in chronic epicondylitis humeri radialis using 1.0 T equipment--contrast medium administration necessary? Rofo 2001,173(5), 454-459.
- Berkowitz, J.F.; Kier, R.; Rudicel, S. Plantar fasciitis: MR imaging. Radiology 1991, 179, 665–667. [CrossRef]
- Sutera, R.; Iovane, A.; Sorrentino, F.; Candela, F.; Mularo, V.; La Tona, G.; Midiri, M. Plantar fascia evaluation with a dedicated magnetic resonance scanner in weight-bearing position: our experience in patients with plantar fasciitis and in healthy volunteers. La Radiol. medica 2010, 115, 246–260. [CrossRef]
- Maier, M.; Steinborn, M.; Schmitz, C.; Stäbler, A.; Köhler, S.; Pfahler, M.; Dürr, H.R.; Refior, H.J. Extracorporeal shock wave application for chronic plantar fasciitis associated with heel spurs: prediction of outcome by magnetic resonance imaging. J. Rheumatol. 2000, 27, 2455–62.
- Rhim, H.C.; Kwon, J.; Park, J.; Borg-Stein, J.; Tenforde, A.S. A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life (Basel) 2021, 11(12), 1287.
- Tafur, J.; Mills, P.J. Low-Intensity Light Therapy: Exploring the Role of Redox Mechanisms. Photomed. Laser Surg. 2008, 26, 323–328. [CrossRef]
- Prindeze, N.J.; Moffatt, L.T.; Shupp, J.W. Mechanisms of action for light therapy: A review of molecular interactions. Exp. Biol. Med. 2012, 237, 1241–1248. [CrossRef]
- Notarnicola, A.; Covelli, I.; DE Giorgi, S.; Moretti, B. High intensity laser therapy in the treatment of tendinopathy: a brief narrative review and update of current literature. Minerva Orthop. 2024, 75, 32–42. [CrossRef]
- Notarnicola, A.; Maccagnano, G.; Rifino, F.; Pesce, V.; Gallone, M.F.; Covelli, I.; Moretti, B. Short-term effect of shockwave therapy, temperature controlled high energy adjustable multi-mode emission laser or stretching in Dupuytren’s disease: A prospective randomized clinical trial. J. Biol. Regul. Homeost. Agents 2017, 31, 775–784.
- Notarnicola, A.; Maccagnano, G.; Tafuri, S.; Forcignanò, M.I.; Panella, A.; Moretti, B. CHELT therapy in the treatment of chronic insertional Achilles tendinopathy. Lasers Med Sci. 2013, 29, 1217–1225. [CrossRef]
- Kamonseki, D.H.; Gonçalves, G.A.; Yi, L.C.; Júnior, I.L. Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: A randomized controlled single-blind clinical trial. Man. Ther. 2016, 23, 76–82. [CrossRef]
- Naruseviciute, D.; Kubilius, R. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: randomized participant blind controlled trial. Clin. Rehabilitation 2020, 34, 1072–1082. [CrossRef]
- Ordahan, B.; Karahan, A.Y.; Kaydok, E. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: a randomized clinical trial. Lasers Med Sci. 2018, 33, 1363–1369. [CrossRef]
- Yesil, H.; Dundar, U.; Toktas, H.; Eyvaz, N.; Yeşil, M. The effect of high intensity laser therapy in the management of painful calcaneal spur: a double blind, placebo-controlled study. Lasers Med Sci. 2020, 35, 841–852. [CrossRef]
- Tkocz, P.; Matusz, T.; Kosowski, .; Walewicz, K.; Argier, .; Kuszewski, M.; Hagner-Derengowska, M.; Ptaszkowski, K.; Dymarek, R.; Taradaj, J. A Randomised-Controlled Clinical Study Examining the Effect of High-Intensity Laser Therapy (HILT) on the Management of Painful Calcaneal Spur with Plantar Fasciitis. J. Clin. Med. 2021, 10, 4891. [CrossRef]
- Jarde, O.; Diebold, P.; Havet, E.; Boulu, G.; Vernois, J. Degenerative lesions of the plantar fascia: surgical treatment by fasciectomy and excision of the heel spur. A report on 38 cases. 2003, 69, 267–74.
- Lemont, H.; Ammirati, K.M.; Usen, N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc 2003, 93, 234–237.
- McMillan, A.M.; Landorf, K.B.; Gregg, J.M.; De Luca, J.; Cotchett, M.P.; Menz, H.B. Hyperemia in Plantar Fasciitis Determined by Power Doppler Ultrasound. J. Orthop. Sports Phys. Ther. 2013, 43, 875–880. [CrossRef]
- Drake, C.; Whittaker, G.A.; Kaminski, M.R.; Chen, J.; Keenan, A.M.; Rathleff, M.S.; Robinson, P.; Landorf, Karl, B. Medical imaging for plantar heel pain: a systematic review and meta-analysis J Foot Ankle Res 2022, 15(1), 4.
- Cetin, A.; Sivri, A.; Dincer, F.; Kiratli, P.; Ceylan, E. Evaluation of Chronic Plantar Fasciitis by Scintigraphy and Relation to Clinical Parameters. J. Musculoskelet. Pain 2001, 9, 55–61. [CrossRef]
- Sweeting, D.; Parish, B.; Hooper, L.; Chester, R. The effectiveness of manual stretching in the treatment of plantar heel pain: a systematic review. J. Foot Ankle Res. 2011, 4, 19–13. [CrossRef]
- Stecco, C.; Corradin, M.; Macchi, V.; Morra, A.; Porzionato, A.; Biz, C.; De Caro, R. Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. J. Anat. 2013, 223, 665–676. [CrossRef]
- Langberg, H.; Ellingsgaard, H.; Madsen, T.; Jansson, J.; Magnusson, S.P.; Aagaard, P.; Kjær, M. Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand. J. Med. Sci. Sports 2006, 17, 61–66. [CrossRef]
- Notarnicola, A.; Maccagnano, G.; Tafuri, S.; Gallone, M.F.; Moretti, L.; Moretti, B. High level laser therapy for the treatment of lower back pain: Clinical efficacy and comparison of different wavelengths. J. Biol. Regul. Homeost. Agents 2017, 30, 1157–1164.
- Hamilton, H.K.; Dover, J.S.; Arndt, K.A. Successful Treatment of Disfiguring Hemosiderin-Containing Hyperpigmentation With the Q-Switched 650-nm Wavelength Laser. JAMA Dermatol. 2014, 150, 1221–1222. [CrossRef]
- Lopes-Martins, R.A.B.; Albertini, R.; Lopes, P.S.L.; Bjordal, J.M.; Neto, H.C.C.F. Spontaneous Effects of Low-Level Laser Therapy (650 nm) in Acute Inflammatory Mouse Pleurisy Induced by Carrageenan. Photomed. Laser Surg. 2005, 23, 377–381. [CrossRef]
- Byrnes, K.R.; Waynant, R.W.; Ilev, I.K.; Wu, X.; Barna, L.; Smith, K.; Heckert, R.; Gerst, H.; Anders, J.J. Light promotes regeneration and functional recovery and alters the immune response after spinal cord injury. Lasers Surg. Med. 2005, 36, 171–185. [CrossRef]
- Anderson, P.R. Cutaneous Laser Surgery. St. Louis, Missouri: Mosby Inc; Laser-Tissue Interactions. 1999; pp. 13–18.
- Coombe, A.R.; Ho, C.T.; Darendeliler, M.A.; Hunter, N.; Philips, J.R.; Chapple, C.C.; Yum, L.W. The effects of low level laser irradiation on osteoblastic cells. Clin. Orthod. Res. 2001, 4, 3–14. [CrossRef]
- Ribeiro, D.A.; Matsumoto, M.A. Low-level laser therapy improves bone repair in rats treated with anti-inflammatory drugs. J. Oral Rehabil. 2008, 35, 925–933. [CrossRef]
- Shibata, M.; Kodani, I.; Osaki, M.; Araki, K.; Adachi, H.; Ryoke, K.; Ito, H. Cyclo-oxygenase-1 and -2 expression in human oral mucosa, dysplasias and squamous cell carcinomas and their pathological significance. Oral Oncol. 2005, 41, 304–312. [CrossRef]
- Baek, W.Y.; Byun, I.H.; Yun, I.S.; Kim, J.Y.; Roh, T.S.; Lew, D.H; Kim, Y.S. The effect of light-emitting diode (590/830 nm)-based low-level laser therapy on posttraumatic edema of facial bone fracture patients. J Craniomaxillofac Surg 2017, 45(11), 1875-1877.
- Notarnicola, A.; Covelli, I.; Macchiarola, D.; Bianchi, F.P.; Cassano, G.D.; Moretti, B. The Efficacy of Temperature-Controlled High-Energy Polymodal Laser Therapy in Tendinopathy of the Shoulder J Clin Med 2023, 12(7), 2583.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).