1. Introduction
Erectile dysfunction (ED) is the inability to attain or maintain an erection sufficient for performing sexual intercourse [
1]. The prevalence worldwide is variable between the different geographic regions, but is high and growing all over the world, reaching 42% in the US and 42.6–48.6% in Europe [
1]. A previous work estimated that the world population affected by ED may reach 322 million people by 2025, meaning an increase of 115% since 1995 [
2]. Up to 50% of patients do not seek treatment, resulting in the infradiagnosis of the disease [
3]. Apart from the medical aspect, this disease has an economic impact, with a loss of productivity estimated to be
$7270 per worker per year in the US [
4].
Several diseases have been related to ED, with COVID-19 being one of the most recent. Since its description [
5], COVID-19 has been known to be an infectious disease that has led to a great variety of complications [
6,
7,
8] in affected individuals, with a strong socioeconomic impact [
9]. Some of them will last for a long time, which has led to the description of a condition known as long COVID [
10]. SARS-CoV-2 vaccination strategies have been implemented to try to change the natural history of the disease, but a number of serious adverse effects have been described [
11]. Since Sansone et al. described a relationship between COVID-19 and ED for the first time [
12], other investigations [
13,
14] reported similar findings. Although evidence about long-term erectile function impairment after COVID-19 recovery is scarce, erectile dysfunction seems to last for at least one year after recovery [
15].
COVID-19 is a disease with a complex pathogenesis [
5] that has shown an unequal recovery of health-related quality of life after the acute phase [
16]. In this sense, it is important to recognise those patients who are at risk of having long-term ED after COVID-19 recovery in order to avoid the associated complications. Machine learning is a subfield of artificial intelligence involved in the analysis and processing of large datasets [
17]. In urology, it has mainly been used in oncology [
18]. However, its data processing properties might facilitate the development of a prediction model for a multifactorial disease like ED [
19]. Erectile function is, apart from its sexual aspect, a marker of cardiovascular [
12] and general health [
20]. Predicting long-term ED after COVID-19 recovery would lead to an early ED diagnosis, an early treatment strategy and the prevention of adverse effects over general health.
Therefore, our work aimed to develop a machine learning-based model for the identification of features involved in the prediction of long-term ED after COVID-19 recovery.
2. Materials and Methods
2.1. Study Design
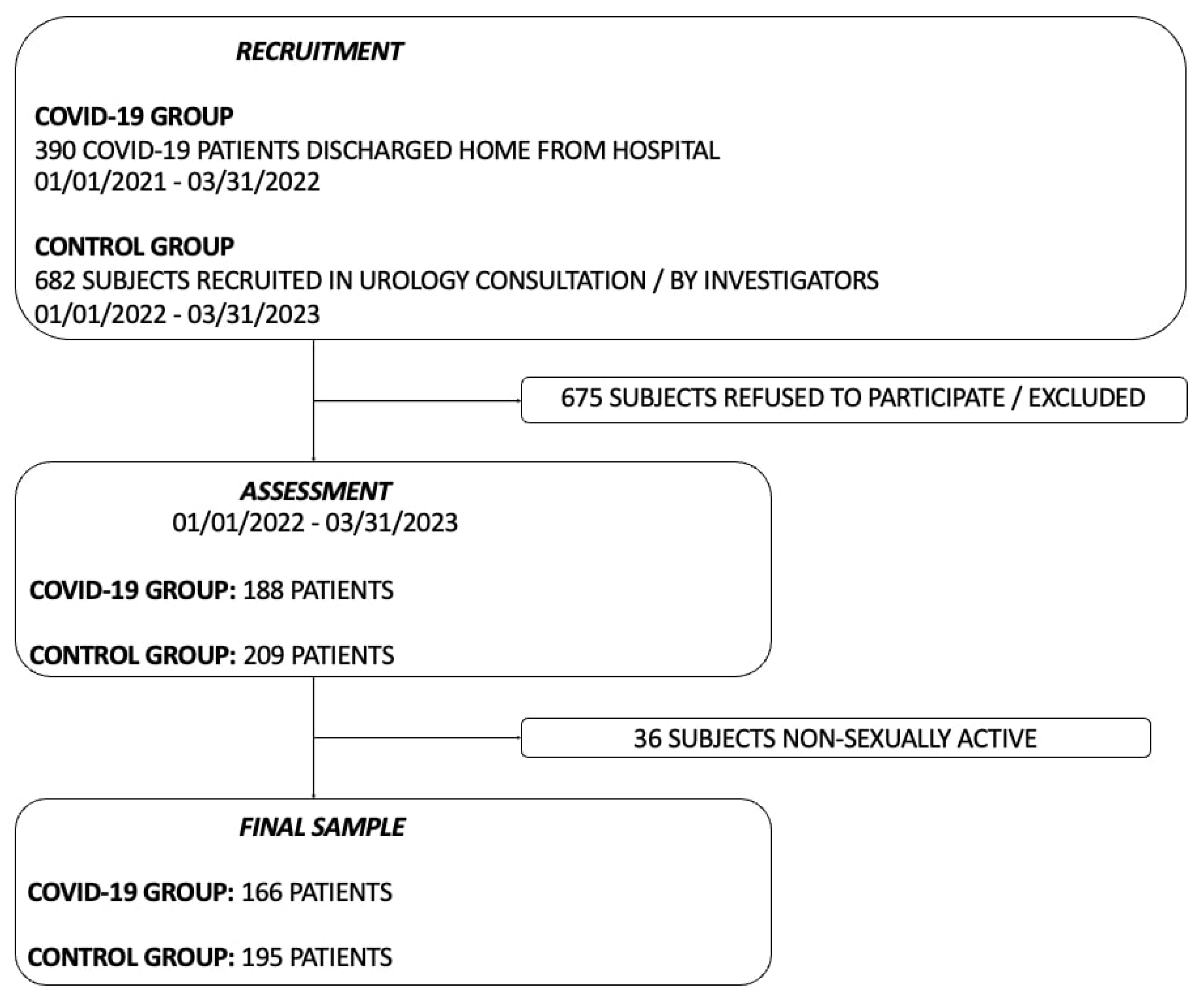
We carried out a prospective observational multicentre investigation in the following institutions: Clinic University Hospital of Valladolid, the Río Hortega University Hospital and the Santa Barbara Hospital. This study was approved by the ethics committees of all three institutions: CEIC Área de Salud Valladolid Este (cod: PI-GR-21-2405), CEIC Área de Salud Valladolid Oeste (cod: 21-PI211) and CEIC Área de Salud Burgos y Soria (cod: 2873). We performed the study in accordance with the ethical standards of the Declaration of Helsinki. Patients signed written informed consent prior to being enrolled in the study. Patients were divided in 2 groups according to their history of COVID-19: I) the COVID-19 group: men aged 40–70 years hospitalised for COVID-19 (fever resistant to medical treatment; pneumonia diagnosed by X-ray or CT; not suitable for outpatient treatment) and discharged from hospital between 1 January 2021 and 31 March 2022 and II) the Control group: men aged 40–70 years with neither a past history of microbiologic diagnosis of COVID-19 nor a past history of hospital admission in the last 12 months who were recruited in a Urology outpatient consultation between 1 January 2022 and 31 March 2023. A convenience sampling was used due to the limited availability of cases of interest. Exclusion criteria were a past history of rectal, urethral, prostate or penile prosthesis surgery and a past history of ED. We declared those individuals who had not experienced sexual intercourse in the month before the assessment as non-sexually active, who were also excluded.
2.2. Outcomes
We assessed both groups ED using the 5-item International Index of Erectile Function (IIEF-5)[
21], which is a self-report instrument for the evaluation of male sexual function using five questions focused on erectile function. According to the standardised use of the instrument, ED is defined as a score of 21 or lower. We collected data concerning epidemiological variables (age, BMI, highest level of education, occupation, physical activity, civil status, living arrangements, SARS-CoV-2 vaccination), habits (smoking, alcohol, coffee, cannabis), comorbidities (ischemic heart disease, high blood pressure [hypertension], atrial fibrillation, heart failure, stroke, peripheral arterial disease [PAD], diabetes, obstructive sleep apnoea syndrome [OSAS], chronic obstructive pulmonary disease [COPD], asthma, hypothyroidism, chronic kidney failure, chronic active hepatitis, Parkinson disease, cancer, anxiety/depression, lower urinary tract symptoms [LUTS], autoimmune disease) and active treatments (beta blockers, statins, non-thiazide diuretics, spironolactone, corticosteroids, antiplatelet therapy, anticoagulation therapy [acenocumarol or new oral anticoagulants], low-molecular-weight heparin [LMWH], benzodiazepines, antidepressants, antipsychotics, anticholinergics, alpha-1 receptor antagonists or 5-alpha reductase inhibitors). Intensive Care Unit (ICU) admission during hospitalisation was collected for the COVID-19 group.
2.3. Data Collection
We designed a questionnaire with questions regarding the outcomes described previously. Patients completed the questionnaire through a telephone interview or filled in it using Google Forms between 1 January 2022 and 31 March 2023.
2.4. Data Analysis
First, we performed a descriptive analysis of the previously described variables. Results were reported as medians (interquartile range) for continuous variables and as frequencies and percentages for categorical variables. Empty records or those filled with null data were eliminated. We then carried out a machine learning-based model for the automatic selection of the variables involved in the prediction of erectile dysfunction in our sample. We used three algorithms that have different characteristics, as detailed below:
It is possible to identify the main characteristics used in the classification by observing the magnitude of the coefficients.
The algorithms RF, LR and SVM reported the variables involved in the prediction of ED (target event) in their outputs. We decided to select the common variables at the output of our three algorithms model applied, in order to detect and mitigate the implicit algorithm bias. The previously described algorithms analyse variables, but do not evaluate each of the values that a variable can take. We executed a variant of SVM, the algorithm Recursive Feature Elimination (RFE) with non-linear Kernel metrics [
22], which allows the evaluation of specific values of the variables. We determined that, among the variables included in the final selection of our model, the values with a positive Kernel vector output were involved in the prediction of the target event ED, according to the algorithm principles [
22]. Finally, two of the authors with experience in ED diagnosis and management assessed the performance of the proposed model.
We used the programming language Python (from Python Software Foundation) version 3.8 to perform the descriptive analysis and implement the algorithms used for machine learning.
3. Results
We identified 1072 eligible patients. Following the application of exclusion criteria and the exclusion of non-sexually active individuals, we obtained the final sample for our study (
Figure 1).
COVID-19 group individuals completed the questionnaire a median of 374 days (interquartile range 20) after discharge from hospital. The median age was 55 years in both groups. The descriptive analysis of the most relevant variables is shown in
Table 1. The detailed descriptive analysis of all the variables investigated is shown in
Figure S1.
The output of the machine learning-based model applied included the following variables: group, SARS-CoV-2 vaccination, hypertension, diabetes, beta blockers, antiplatelet therapy and coffee intake (
Table 2).
The application of the algorithm SVM-RFE found that Group COVID-19 (past history of COVID-19) and SARS-CoV-2 vaccination obtained a positive Kernel vector value that determined their involvement in ED prediction, as shown in
Table 3.
4. Discussion
To the best of our knowledge, this is the first time a machine learning-based model was developed for the prediction of long-term ED following COVID-19 recovery. Our multicentre study showed that a past history of COVID-19 and SARS-CoV-2 vaccination were both predictors of long-term ED in our model.
We found an ED prevalence of 55.9% in the COVID-19 group in our work, which was higher than the described Spanish ED prevalence rates (43.5%) [
1] and is similar to those found in the Control group (44.1%). Given that ED can persist following COVID-19 recovery in some patients, one question seemed crucial: Can we predict which of them will develop long-term ED after COVID-19 recovery? Machine learning is an advanced statistical method that provides an in-depth analysis of large datasets, creating sequences and automating processes [
17,
23]. Learning through these datasets facilitates the study of large populations, even if they are unequal. This makes it a valuable tool in medicine and particularly in the study of complex diseases such as ED. We created a machine learning-based model, a simple clinical tool, which is able to predict long-term ED in recovered COVID-19 patients. Among the seven features that our model selected, a past history of COVID-19 was one of them, revealing the long-lasting impact of the disease on general health. SARS-CoV-2 vaccination was also one of the features selected. The prediction of ED could be explained in this case by the addition of a highly thrombotic virus like COVID-19 and the complications which SARS-CoV-2 vaccination has shown [
11].
A relationship between COVID-19 and ED was described for the first time in 2020 [
12] and later in other works [
13,
14]. Moreover, Gök et al. reported an impairment of erectile function outcomes even 12 months after COVID-19 recovery [
15]. Our predictive model and the features that integrate it support these findings and underline the impact of COVID-19 on general health. There is social concern about the adverse effects of SARS-CoV-2 vaccination, mainly caused by the description of thrombotic events following vaccination [
11] and the link between SARS-CoV-2 vaccination and Long COVID [
24]. Even one of the vaccines available has recently stopped its distribution. Our results show the involvement of the SARS-CoV-2 vaccination in the prediction of long-term ED, which has not been described before to the best of our knowledge. Other variables selected by our model (hypertension, diabetes, beta blockers) are previously established erectile dysfunction risk factors [
19]. As such, our findings would take COVID-19 and SARS-CoV-2 vaccination to the level of other well-known determinants of ED.
Erectile function is a marker of general health [
12,
20], while ED is considered a strong predictor of cardiovascular events [
25]. Up to 3 October 2023, there have been more than 600,000,000 known COVID-19 cases worldwide [
26]. Given the high global COVID-19 incidence and the unlikely eradication of the disease in the future [
27,
28], more complications and sequels are expected in the coming months and years. Our machine learning-based model could be decisive in the prediction of long-term ED following COVID-19 in community settings. The application of our predictive tool in recovered COVID-19 patients, in a screening program, would result in the early detection of the patients at risk of developing long-term ED, the prevention of adverse consequences and the avoidance of its unfavourable economic effect.
Some limitations must be described: Data of interest were collected through a survey, trusting the facts described by participants. Our machine learning-based model should be externally validated in other populations. Future investigations should include sharing datasets about ED in recovered COVID-19 patients. This would allow the creation of great multicentric databases which lead to the application of predictive tools involved in ED screening. A reduction in the utilisation of health resources and the socioeconomic impact of the disease could then be seen.
In conclusion, we developed a machine learning-based model for the prediction of long-term ED following COVID-19 recovery. We showed that a past history of COVID-19 and SARS-CoV-2 vaccination were both predictors of long-term ED in our model. The application of our predictive tool in recovered COVID-19 patients in a community setting could avoid ED adverse effects and its unfavourable economic impact.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Table S1: Descriptive analysis of the characteristics of the patients.
Author Contributions
Conceptualization, FN, MC and ET; methodology, FN , ET, AB and MJ; software, MJ; validation, ET and FN; formal analysis, AB and MJ; investigation, FN, NS, AG and CM; resources, AB, ET and MJ; data curation, FN, AB and MJ; writing-original draft preparation, FN and MJ; writing-review and editing, AB and ET; visualization, MC, NS, AG and CM; supervision, ET; project administration, ET, FN; funding acquisition, ET. The submitted version of the manuscript was approved by all the authors.
Funding
This work was funded by Instituto de Salud Carlos III (grant number PI21/00917, PI18/01238, CIBERINFEC CB21/13/00051), Junta de Castilla y León (grant number GRS 2546/A/22, GRS 2425/A/21, GRS 1922/A/19, GRS 2057/A/19), Consejería de Educación de Castilla y León (grant number VA256P20) and Fundación Ramón Areces (grant number CIVP19A5953).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committees of all three institutions: CEIC Área de Salud Valladolid Este (cod: PI-GR-21-2405), CEIC Área de Salud Valladolid Oeste (cod: 21-PI211) and CEIC Área de Salud Burgos y Soria (cod: 2873).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and/or analyzed during the current investigation are available from the corresponding author upon reasonable request.
Acknowledgments
We appreciate the collaboration of the Research Unit of the Clinic University Hospital of Valladolid, Spain.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Goldstein I, Goren A, Li VW, Tang WY, Hassan TA. Epidemiology update of erectile dysfunction in eight countries with high burden. Sex Med Rev. 2020 Jan;8(1):48-58. [CrossRef]
- Aytac IA, Mckinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU International (1999), 84, 50-56. [CrossRef]
- Lin H, Zhao L, Wu H, Cao M, Jiang H. Sexual life and medication taking behaviours in young men: an online survey of 92620 respondents in China. Int J Clin Pract. 2020 Jan;74(1):e13417. [CrossRef]
- Rojanasarot S, Bhattacharyya SK, Burnett AL. Cost of lost productivity due to erectile dysfunction and impact of employer benefit exclusion of penile prosthesis implantation treatment. J Occup Environ Med. 2022 May 1;64(5):403-408. [CrossRef]
- Lamers MM, Haagmans BL. SARS-CoV-2 pathogenesis. Nat Rev Microbiol. 2022 May;20(5):270-284. [CrossRef]
- Qu G, Zhen Q, Wang W, Fan S, Wu Q, Zhang C et al. Health-related quality of life of COVID-19 patients after discharge: A multicentre follow-up study. J Clin Nurs. 2021;30(11-12):1742-1750. [CrossRef]
- Tamayo-Velasco Á, Bombín-Canal C, Cebeira MJ, Sánchez-De Prada L, Miramontes-González JP, Martin-Fernández M et al. Full characterisation of thrombotic events in all hospitalised COVID-19 patients in a Spanish tertiary hospital during the first 18 months of the pandemic. J Clin Med. 2022;11(12):3443. [CrossRef]
- Tamayo-Velasco Á, Martínez-Paz P, Peñarrubia-Ponce MJ, de la Fuente I, Pérez-Gonzalez S, Fernandez I et al. HGF, IL-1α, and IL-27 are robust biomarkers in early severity stratification of COVID-19 patients. J Clin Med. 2021;10(9):2017. [CrossRef]
- Stylianou T, Ntelas K. Impact of COVID-19 pandemic on mental health and socioeconomic aspects in Greece. Int J Environ Res Public Health. 2023 Jan 19;20(3):1843. [CrossRef]
- Yong SJ. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect Dis (Lond). 2021;53(10):737-754. [CrossRef]
- Iba T, Levy JH. Thrombosis and thrombocytopenia in COVID-19 and after COVID-19 vaccination. Trends Cardiovasc Med. 2022 Jul;32(5):249-256. [CrossRef]
- Sansone A, Mollaioli D, Ciocca G, Colonnello E, Limoncin E, Balercia G et al. “Mask up to keep it up”: Preliminary evidence of the association between erectile dysfunction and COVID-19. Andrology. 2021;9(4):1053-1059. [CrossRef]
- Hebert KJ, Matta R, Horns JJ, Paudel N, Das R, McCormick BJ et al. Prior COVID-19 infection associated with increased risk of newly diagnosed erectile dysfunction. Int J Impot Res. 2023 Mar 15:1-5. [CrossRef]
- Zhang J, Shi W, Zou M, Zeng Q, Feng Y, Luo Z et al. Prevalence and risk factors of erectile dysfunction in COVID-19 patients: A systematic review and meta-analysis. J Endocrinol Invest. 2023;46:795-804. [CrossRef]
- Gök A, Altan M, Dogan AE, Eraslan A, Uysal FS, Öztürk U et al. Does post-COVID-19 erectile dysfunction improve over time? J Clin Med. 2023;12(3):1241. [CrossRef]
- Maestre-Muñiz MM, Arias A, Mata-Vázquez E, Martin-Toledano M, Lopez-Larramona G, Ruiz-Chicote AM, et al. Long-term outcomes of patients with Coronavirus Disease 2019 at one year after hospital discharge. J Clin Med. 2021;10(13):2945. [CrossRef]
- Suarez-Ibarrola R, Hein S, Reis G, Gratzke C, Miernik A. Current and future applications of machine and deep learning in urology: a review of the literature on urolithiasis, renal cell carcinoma, and bladder and prostate cancer. World J Urol. 2020 Oct;38(10):2329-2347. [CrossRef]
- Hasannejadasl H, Roumen C, van der Poel H, Vanneste B, van Roermund J, Aben K et al. Development and external validation of multivariate prediction models for erectile dysfunction in men with localised prostate cancer. PLoS One. 2023 Mar 3;18(3):e0276815. [CrossRef]
- McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD et al. Risk factors for sexual dysfunction among women and men: A consensus statement form the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13(2):153-167. J Sex Med. 2016 Feb;13(2):153-67. [CrossRef]
- Jannini EA. SM = SM: The interface of systems medicine and sexual medicine for facing non-communicable diseases in a gender-dependent manner. Sex Med Rev. 2017 Jul;5(3):349-364. [CrossRef]
- Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999; 11(6):319-326. [CrossRef]
- Sanz H, Valim C, Vegas E, Oller JM, Reverter F. SVM-RFE: selection and visualization of the most relevant features through non-linear kernels. BMC Bioinformatics. 2018 Nov 19;19(1):432. [CrossRef]
- Xiong Y, Zhang Y, Zhang F, Wu C, Qin F, Yuan J. Applications of artificial intelligence in the diagnosis and prediction of erectile dysfunction: a narrative review. Int J Impot Res. 2023 Mar;35(2):95-102. [CrossRef]
- Romero-Rodríguez E, Pérula-de Torres LÁ, Castro-Jiménez R, Gonzalez-Lama J, Jimenez-Garcia C, Gonzalez-Bernal JJ et al. Hospital admission and vaccination as predictive factors of long COVID-19 symptoms. Front Med (Lausanne). 2022 Nov 11:9:1016013. [CrossRef]
- Yannas D, Frizza F, Vignozzi L, Corona G, Maggi M, Rastrelli G. Erectile dysfunction is a hallmark of cardiovascular disease: Unavoidable matter of fact or opportunity to improve men's health? J Clin Med. 2021;10(10):2221. [CrossRef]
- COVID-19 Map - Johns Hopkins Coronavirus Resource Centre [Internet]. Available online: https://coronavirus.jhu.edu/map.html (accessed on 21 May 2024).
- Ghasemiyeh P, Mohammadi-Samani S. Lessons we learned during the past four challenging years in the COVID-19 era: pharmacotherapy, long COVID complications, and vaccine development. Virol J. 2024 Apr 26;21(1):98. [CrossRef]
- Hu X, Hu Z, Xu T, Zhang K, Lu HH, Zhao J et al. Equilibrium points and their stability of COVID-19 in US. Sci Rep. 2024; 14:1628. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).