1. Introduction
Ureteral calculi are common urological diseases, often presenting with pain and hematuria, but some ureteral calculi may be asymptomatic and easily overlooked. If the ureter is completely obstructed and not promptly relieved, it can lead to hydronephrosis and ultimately loss of kidney function. This case report describes a case of nephrectomy due to asymptomatic ureteral calculus causing a non-functional kidney. The patient was first diagnosed with left hydronephrosis and left ureteral obstruction. After one month of nephrostomy treatment without improvement in kidney function, nephrectomy was performed upon admission. This report aims to emphasize the importance of early diagnosis and treatment of obstructive stones and the management of kidney function loss, providing diagnostic and therapeutic experience for similar cases.
2. Case Information
2.1. Patient Information and Medical History
Patient: male, 34 years old, Admission Date: July 8, 2024. Chief Complaint: Hydronephrosis for more than one month, one month after percutaneous nephrostomy. Present Illness: One month before admission, the patient was found to have left hydronephrosis during an ultrasound examination. There was no urinary frequency, urgency, dysuria, or abdominal and back pain. No difficulty in urination, abnormal urine color, or volume. No hematuria or pyuria. No gastrointestinal symptoms such as nausea, vomiting, or loss of appetite. The patient underwent ultrasound-guided percutaneous left nephrostomy and drainage at a local hospital. Follow-up urinary system CT in our outpatient clinic on July 7, 2024, showed left kidney percutaneous nephrostomy state; calculus at the origin of the left ureter, proximal left collecting system dilation and hydronephrosis, and thinning of the left renal cortex. The patient was admitted for further treatment.
Past Medical History: Healthy, denies family and genetic history, no epidemiological history.
2.2. Physical Examination
Temperature: 36.8°C, Heart Rate: 68 beats/min, Respiration: 18 breaths/min, Blood Pressure: 126/86 mmHg. Abdominal examination: No abnormal masses in the abdomen and waist, nephrostomy tube visible on the left axillary line. No tenderness in the ureteral path, no tenderness in the bilateral costovertebral angle and bladder area, and no palpable kidneys. No percussion pain in the kidneys. No vascular murmur heard in the kidneys. Rectal examination: Smooth finger entry, normal anal sphincter tone, grade I prostate, firm, smooth surface without nodules, central groove present, no tenderness, no blood on the glove.
2.3. Auxiliary Examinations
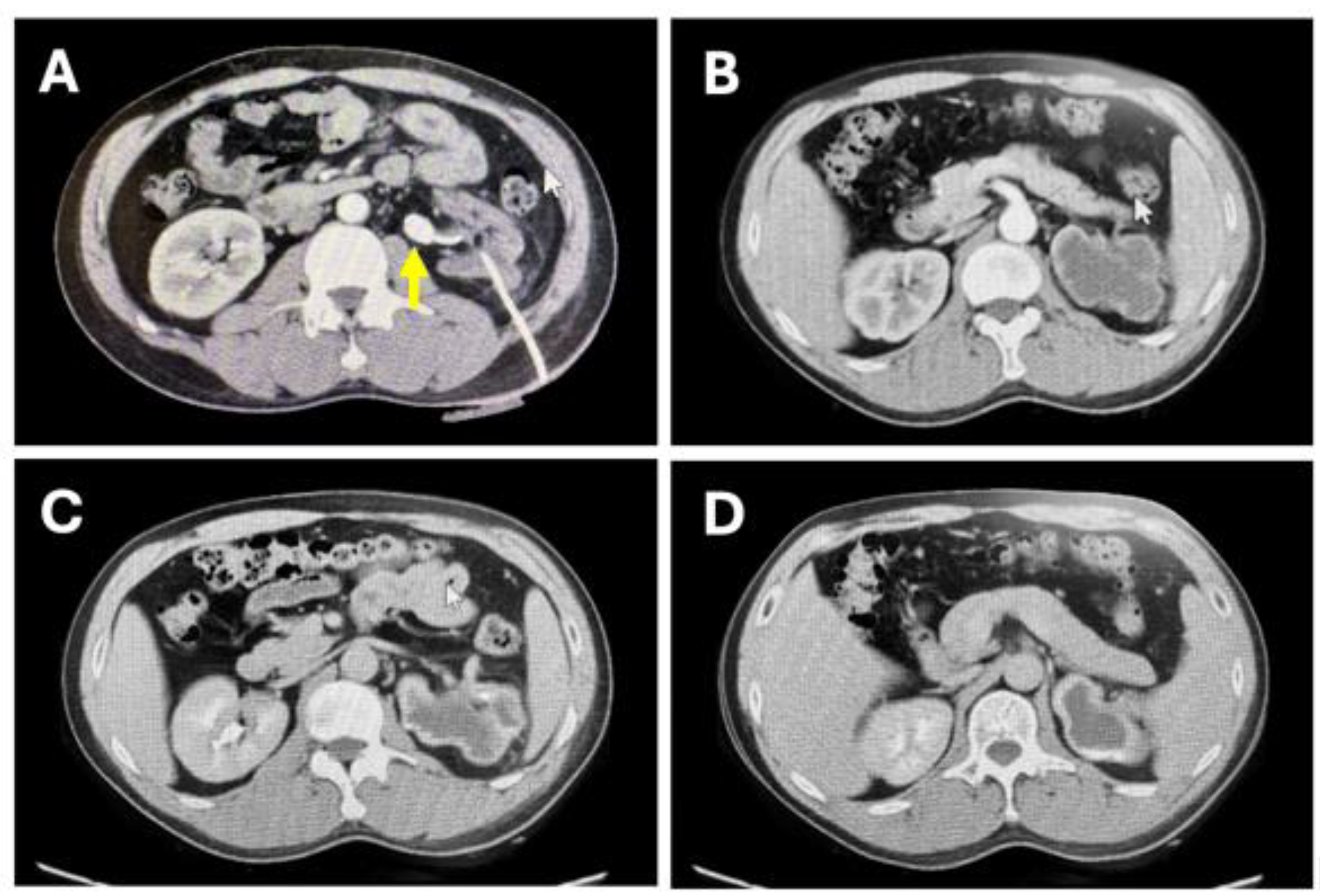
(1) Blood routine: White blood cells: 6.76*10^9/L (normal), neutrophils: 65.4% (normal), hemoglobin: 151 g/L (normal), platelets: 317*10^9/L (normal)(2) Blood biochemistry: Albumin: 46.4 g/L (normal), creatinine: 113 μmol/L (mildly elevated), blood urea nitrogen: 6.00 mmol/L (mildly elevated), uric acid: 477 μmol/L (mildly elevated), potassium: 4.0 mmol/L (normal)(3) Enhanced CT of the urinary system: Abnormal left kidney morphology, thinning of the parenchyma, percutaneous nephrostomy state; poor enhancement in the arterial phase of the left kidney, no significant enhancement in the renal pelvis during the excretory phase; calculus at the origin of the left ureter, size 1.8*1.3 cm, proximal left collecting system dilation and hydronephrosis, atrophy of the left renal parenchyma; multiple calculi in both renal calyces, the largest in the lower calyx of the left kidney, about 0.9*0.7 cm.
Figure 1.
CT enhanced scan of the urinary system before surgery. (A) shows the left ureteral calculus and the position of the nephrostomy tube. (B) shows the thinning of the left renal cortex with poor enhancement in the arterial phase. (C) shows slight enhancement of the left renal cortex in the excretory phase, without contrast agent excretion in the renal pelvis. (D) shows a small amount of contrast agent excretion in the left renal pelvis in the excretory phase.
Figure 1.
CT enhanced scan of the urinary system before surgery. (A) shows the left ureteral calculus and the position of the nephrostomy tube. (B) shows the thinning of the left renal cortex with poor enhancement in the arterial phase. (C) shows slight enhancement of the left renal cortex in the excretory phase, without contrast agent excretion in the renal pelvis. (D) shows a small amount of contrast agent excretion in the left renal pelvis in the excretory phase.
2.4. Diagnosis and Differential Diagnosis Current Diagnosis: Left Ureteral Calculus, Left Hydronephrosis, Left Non-Functional Kidney, Renal Insufficiency, Multiple Renal Calculi in Both Kidneys
Diagnostic basis: Young male patient, previously healthy. Ultrasound during a health check-up one month ago revealed left hydronephrosis and ureteral calculus. Diagnosed with hydronephrosis and ureteral calculus at a local hospital, and underwent percutaneous nephrostomy. After one month, CT enhanced scan in our hospital confirmed left hydronephrosis and left ureteral calculus at the origin. After one month of nephrostomy, there was no improvement in left renal cortex thickness or hydronephrosis, and poor enhancement in the arterial phase and no significant enhancement in the renal pelvis during the excretory phase. Blood biochemistry showed creatinine 113 μmol/L (mildly elevated), blood urea nitrogen 6.00 mmol/L (mildly elevated), indicating renal insufficiency and confirming the diagnosis of a non-functional left kidney. This diagnosis was supported by the patient's history, laboratory tests, and imaging findings. Differential diagnosis: (1) Renal tumor: CT showed no occupying lesions in the left kidney and ureter, no abnormal enhancement, excluded. (2) Congenital renal abnormalities: Patient's history and imaging did not suggest congenital ureteral stenosis or renal abnormalities, excluded. (3) Pyelonephritis: No infection symptoms, normal blood routine, no elevated white blood cells, normal neutrophil ratio, excluded.
2.5. Treatment Intervention
After admission, the patient completed preoperative examinations. After one month of nephrostomy without significant improvement in kidney function, confirming the diagnosis of a non-functional kidney. To avoid secondary infection and malignancy, and meeting surgical indications without clear contraindications, robotic-assisted left nephrectomy was performed.
2.6. Treatment Outcome, Follow-Up, and Prognosis
The patient recovered well postoperatively. Biochemical renal function showed creatinine 108.9 μmol/L and blood urea nitrogen 5.90 mmol/L, slightly decreased compared to preoperative levels. The patient was discharged three days postoperatively, in good condition with the drainage tube removed. The patient was advised to follow up in the outpatient clinic two weeks post-discharge to review biochemical tests and incision recovery. CT was scheduled one month post-discharge to assess the contralateral kidney, followed by semi-annual biochemical and urinary ultrasound reviews to monitor contralateral kidney function and stone changes, preventing contralateral kidney stone obstruction.
3. Discussion
Ureteral calculi are common urological diseases that can cause severe complications such as hydronephrosis and kidney function loss . This case describes a patient with asymptomatic ureteral calculus leading to a non-functional kidney, diagnosed through detailed examination as left ureteral calculus, left hydronephrosis, left non-functional kidney, and multiple renal calculi, ultimately undergoing robotic-assisted left nephrectomy. According to the American Urological Association (AUA) guidelines, surgical intervention is recommended for ureteral calculi larger than 10 mm, especially in cases causing hydronephrosis and impaired kidney function . This patient's left ureteral calculus was 1.8 cm in diameter, causing severe hydronephrosis and renal insufficiency, meeting surgical indications. Compared to similar cases, this case was asymptomatic and only discovered after hydronephrosis and function loss occurred . Some literature reports early detection and intervention of asymptomatic stones can effectively prevent kidney function deterioration. This case emphasizes the importance of regular physical examinations and urinary system checks for asymptomatic patients. This report provides diagnostic and therapeutic experience for managing hydronephrosis and non-functional kidneys caused by asymptomatic ureteral calculi, especially when severe complications have already occurred. It also highlights the importance of early screening and regular urinary system checks for asymptomatic patients for early detection and intervention. In this case, despite adequate nephrostomy to relieve obstruction, left kidney function did not significantly improve, confirming a non-functional kidney, leading to nephrectomy. The robotic-assisted left nephrectomy was chosen to minimize surgical trauma and enhance postoperative recovery. Future research should focus on early screening strategies for stones, new treatment methods, and long-term follow-up plans to more effectively diagnose and treat urinary calculi and prevent kidney function damage.
References
- Turk C, Petrik A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol 2016; 69(3): 475-82. [CrossRef]
- Assimos D, Krambeck A, Miller N L, et al. Surgical Management of Stones: American Urological Association/Endourological Society Guideline PART I. J Urol 2016; 196(4): 1153-60. [CrossRef]
- Antonelli J A, Maalouf N M, Pearle M S, et al. Use of the National Health and Nutrition Examination Survey to calculate the impact of obesity and diabetes on cost and prevalence of urolithiasis in 2030. Eur Urol 2014; 66(4): 724-9. [CrossRef]
- Scales C D Jr, Smith A C, Hanley J M, et al. Prevalence of kidney stones in the United States. Eur Urol 2012; 62(1): 160-5. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).