Submitted:
09 July 2024
Posted:
10 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
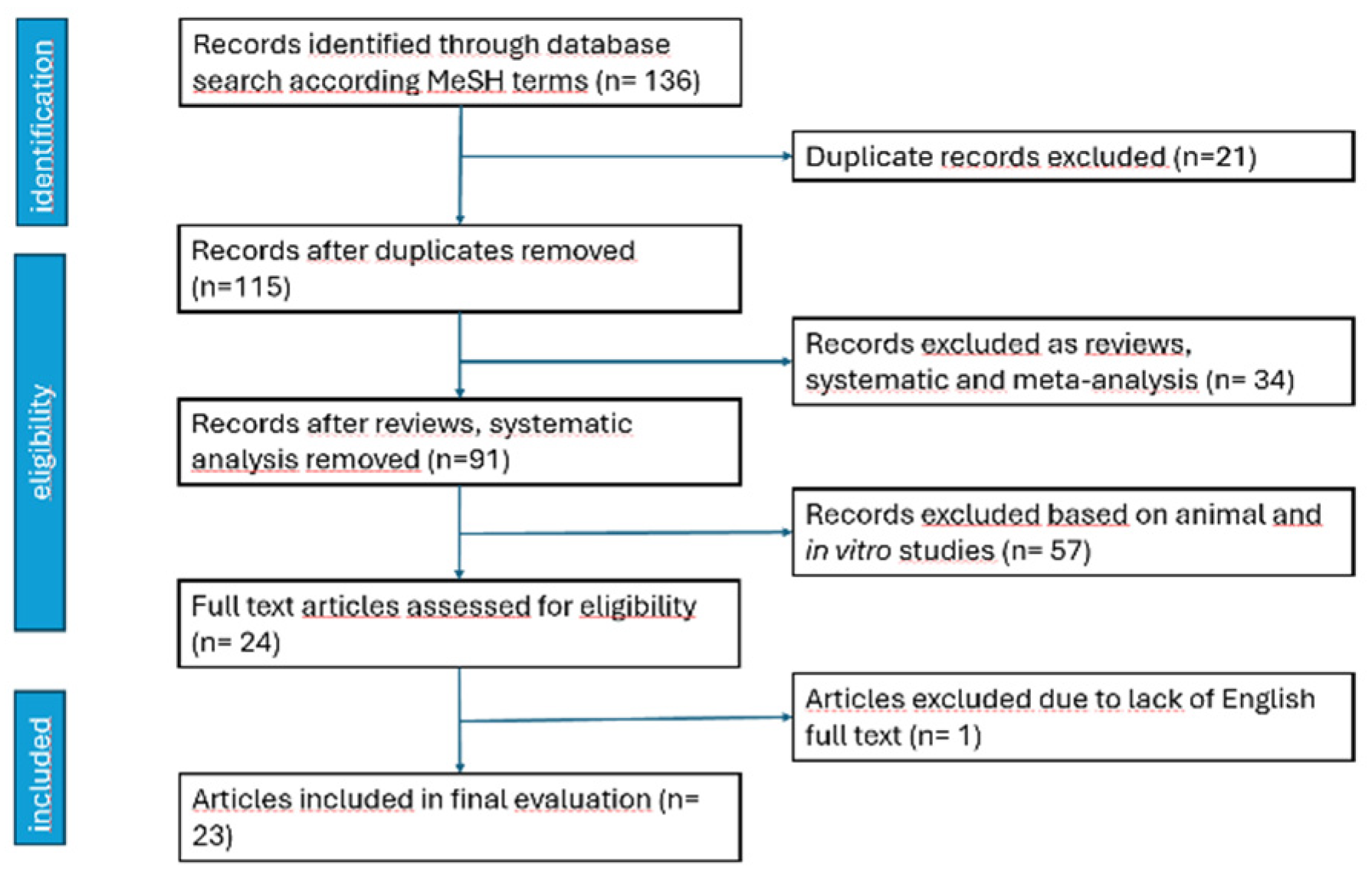
2. Materials and Methods
3. Results
4. Discussion
4.1. HILT versus Sham/Placebo
4.2. HILT versus LLLT
4.3. HILT versus Other Therapeutic Modalities
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Turkiewicz. A.; Petersson. I.F.; Bjork. J.; et al. Current and future impact of osteoarthritis on health care: A population-based study with projections to year 2032. Osteoarthritis Cartilage. 2014; 22(11): 1826-32. [CrossRef]
- Nasui. B.A.; Talaba. P.; Nasui. G.A.; et al. The Influence of Diet and Physical Activity on Oxidative Stress in Romanian Females with Osteoarthritis. Nutrients. 2022 Oct 7;14(19):4159. [CrossRef] [PubMed] [PubMed Central]
- Arroyo-Fernández. R.; Aceituno-Gómez. J.; Serrano-Muñoz. D.; et al. High-Intensity Laser Therapy for Musculoskeletal Disorders: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Journal of Clinical Medicine. 2023; 12(4):1479. [CrossRef]
- Dundar. U.; Turkmen. U.; Toktas. H; et al. Effect of high-intensity laser therapy in the management of myofascial pain syndrome of the trapezius: a double-blind, placebo-controlled study. Lasers Med Sci. 2015 Jan;30(1):325-32. Epub 2014 Oct 2. [CrossRef] [PubMed]
- Ahmed. H.; Abu Taleb. E.; Ameen. F. High intensity laser therapy on pain in patients with myofascial trigger points. Egyptian Journal of Physical Therapy.2020;3(1), 1-8. [CrossRef]
- de la Barra Ortiz. H.; Liebano. R.E.; Vera. MA.; et al. Effectiveness of high-intensity laser therapy added to a physical therapy program for the treatment of myofascial pain syndrome - a systematic review and meta-analysis. Advances in Rehabilitation. 2022, 36(3), 35-48. [CrossRef]
- Alayat. M.S.M.; Mohamed. A.A.; Helal. O.F. et al. Efficacy of high-intensity laser therapy in the treatment of chronic neck pain: a randomized double-blind placebo-control trial. Lasers Med Sci. 2016, 31, 687–694 (2016). [CrossRef]
- Yılmaz. M.; Eroglu. S.; Dundar. U.; et al. The effectiveness of high-intensity laser therapy on pain, range of motion, functional capacity, quality of life, and muscle strength in subacromial impingement syndrome: a 3-month follow-up, double-blinded, randomized, placebo-controlled trial. Lasers Med Sci. 2022, 37, 241–250 (2022). [CrossRef]
- Gocevska. M.; Nikolikj-Dimitrova. E.; Gjerakaroska-Savevska. C. Effects of High - Intensity Laser in Treatment of Patients with Chronic Low Back Pain. Open access Macedonian journal of medical sciences, 2019, 7(6), 949–954. [CrossRef]
- Ordahan. B.; Karahan. A.Y.; Kaydok. E. The Effect of High-Intensity versus Low-Level Laser Therapy in the Management of Plantar Fasciitis: A Randomized Clinical Trial. Lasers Med. Sci. 2018, 33, 1363–1369.
- Tkocz. P.; Matusz. T.; Kosowski. Ł. et al. A Randomised-Controlled Clinical Study Examining the Effect of High-Intensity Laser Therapy (HILT) on the Management of Painful Calcaneal Spur with Plantar Fasciitis. J. Clin. Med. 2021, 10, 4891. [CrossRef]
- Naruseviciute. D.; Kubilius. R. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: randomized participant blind controlled trial. Clinical Rehabilitation. 2020;34(8):1072-1082. [CrossRef]
- Yesil. H.; Dundar. U.; Toktas. H. et al. The effect of high intensity laser therapy in the management of painful calcaneal spur: a double blind, placebo-controlled study. Lasers Med Sci. 2020, 35, 841–852 (2020). [CrossRef]
- Ezzati. K.; Laakso. E. L.; Salari. A. et al. The Beneficial Effects of High-Intensity Laser Therapy and Co-Interventions on Musculoskeletal Pain Management: A Systematic Review. Journal of lasers in medical sciences, 2020,11(1), 81–90. [CrossRef]
- Štiglić-Rogoznica. N.; Stamenković. D.; Frlan-Vrgoč. L.; et al. Analgesic effect of high intensity laser therapy in knee osteoarthritis. Collegium antropologicum, 2011, 35 Suppl 2, 183-5. PMID: 22220431.
- White. P.F.; Cao. X.; Elvir-Lazo. L.; et al. Effect of High-Intensity Laser Treatments on chronic pain related to osteoarthritis in former professional athletes: A case series. J Mol Biomark Diagn 2017; 8: 343. [CrossRef]
- Viliani. T.; Carabba. C.; Mangone. G.; Pasquetti. P. High intensity pulsed Nd: YAG laser in painful knee osteoarthritis: the biostimulating protocol. Energy for Health. 2012;9:18–22.
- Viliani. T.; Ricci. E.; Mangone. G.; Graziani. C.; Pasquetti P. Effects of Hilterapia vs.Visco supplementation in knee osteoarthritis patients a randomized controlled clinical trial. Energy for Health. 2009;3:14–17.
- Sabbahi. S. I. Clinical experience using HilterapiaⓇ in ‘knee arthrosis’ Energy for Health. 2009;4, article 24.
- Kheshie. A.R.; Alayat. M.S.; Ali. M.M. High-intensity versus low-level laser therapy in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci. 2014 Jul;29(4):1371-6. Epub 2014 Feb 1. [CrossRef] [PubMed]
- Kim. G.J.; Choi. J.; Lee. S.; Jeon. C.; Lee. K. The effects of high intensity laser therapy on pain and function in patients with knee osteoarthritis. J Phys Ther Sci. 2016 Nov;28(11):3197-3199. Epub 2016 Nov 29. [CrossRef] [PubMed] [PubMed Central]
- Angelova. A.;, Ilieva. E.M. Effectiveness of High Intensity Laser Therapy for Reduction of Pain in Knee Osteoarthritis, Pain Research and Management, 2016, Article ID 9163618, 11 pages, 2016. [CrossRef]
- Alayat. M.S.M.; Aly. T.H.A.; Elsayed. A.E.M. et al. Efficacy of pulsed Nd:YAG laser in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci 2017, 32, 503–511. [CrossRef]
- Nazari. A.; Moezy. A.; Nejati. P.; Mazaherinezhad. A. Efficacy of high-intensity laser therapy in comparison with conventional physiotherapy and exercise therapy on pain and function of patients with knee osteoarthritis: a randomized controlled trial with 12-week follow up. Lasers Med Sci. 2019 Apr;34(3):505-516. Epub 2018 Sep 3. [CrossRef] [PubMed]
- Ciplak. E.; Akturk. S.; Buyukavci. R.; Ersoy. Y. Efficiency of high intensity laser therapy in patients with knee osteoarthritis. Medicine Science| International Medical Journal. 2018;7:724–727. [CrossRef]
- Akaltun. M.S.; Altindag. O.; Turan. N.; et al. Efficacy of high intensity laser therapy in knee osteoarthritis: a double-blind controlled randomized study. Clin Rheumatol 2021;40, 1989–1995. [CrossRef]
- Koevska. V.; Nikolic-Dimitrova. E.; Mitrevska. B.; et al. Application of high-intensity laser in pain treatment of patients with knee osteoarthritis. Arch Pub Health. 2021 Nov. 20;13(2):78-90. Available from: https://www.id-press.eu/aph/article/view/6008. [CrossRef]
- Siriratna. P.; Ratanasutiranont. C.; Manissorn. T.; et al. Short-Term Efficacy of High-Intensity Laser Therapy in Alleviating Pain in Patients with Knee Osteoarthritis: A Single-Blind Randomised Controlled Trial. Pain Res Manag. 2022 Oct 21;2022:1319165. [CrossRef] [PubMed] [PubMed Central]
- Samaan. S.S.R.R.; Sedhom. M.G.; Grace. M.O. A randomized comparative study between high-intensity laser vs low-intensity pulsed ultrasound both combined with exercises for the treatment of knee osteoarthritis. Int J Rheum Dis. 2022; 25(8):877–886. [CrossRef]
- Mostafa. M.S.E.M.; Hamada. H.A.; Kadry. A.M.; Zahran. S.S.; Helmy. N.A. Effect of High-Power Laser Therapy Versus Shock Wave Therapy on Pain and Function in Knee Osteoarthritis Patients: A Randomized Controlled Trial. Photobiomodul Photomed Laser Surg. 2022 Mar;40(3):198-204. Epub 2022 Jan 5. [CrossRef] [PubMed]
- Ekici. B.; Ordahan. B. Evaluation of the effect of high-intensity laser therapy (HILT) on function, muscle strength, range of motion, pain level, and femoral cartilage thickness in knee osteoarthritis: randomized controlled study. Lasers Med Sci. 2023 Sep 25;38(1):218. [CrossRef] [PubMed]
- Taheri. P.; Maghroori. R.; Aghaei. M. Effectiveness of High-intensity Laser Therapy for Pain and Function in Knee Osteoarthritis: A Randomized Controlled Trial. Middle East J Rehabil Health Stud. 2024;11(1):e134330. [CrossRef]
- Katana. B.; Macak. A.; Kaljić. E.; Mujezinovic. A.; et al. Comparative analysis of different physical therapy programs in the treatment of people with knee osteoarthritis. Journal of Health Sciences. 2023. [CrossRef]
- Ahmad. M.A.; Moganan. M.A.; Hamid. M.S.; et al. Comparison between Low-Level and High-Intensity Laser Therapy as an Adjunctive Treatment for Knee Osteoarthritis: A Randomized, Double-Blind Clinical Trial. Life. 2023; 13(7):1519. [CrossRef]
- Astri. S.W.; Murdhana. N.; Nusdwinuringtyas. N.; et al. The Comparison Of The Low-Level Laser Therapy And High Intensity Laser Therapy On Pain And Functional Ability In Knee Osteoarthritis. Journal Of The Indonesian Medical Association. 2023; 72(6), 275 - 283. [CrossRef]
- Roheym. M.I.; Morsy. M.E.; Saber. M.; et al. Impact of high-power laser therapy on bilateral knee osteoarthritis: A randomized trial. Fizjoterapia Polska. 2023 23(5); 162-168. [CrossRef]
- Wibisono. K.; Handoyo. R.; Setiawati. E. Comparison Of The Effectiveness Of High Intensity Laser Therapy (HILT) And Low-Level Laser Therapy (LLLT) On Improving Balance In Knee Osteoarthritis. Medica Hospitalia: Journal of Clinical Medicine. 2024; 11. 33-37. [CrossRef]
- Brosseau. L.; Taki. J.; Desjardins. B.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Clin Rehabil. (2017) 31:582–624. [CrossRef]
- Poenaru. D.; Sandulescu. M.I.; Cinteza. D. Pain Modulation in Chronic Musculoskeletal Disorders: Botulinum Toxin, a Descriptive Analysis. Biomedicines. 2023 Jul 3;11(7):1888. [CrossRef] [PubMed] [PubMed Central]
- Poenaru. D.; Sandulescu. M.I.; Cinteza. D. Biological effects of extracorporeal shockwave therapy in tendons: A systematic review. Biomed Rep. 2022 Dec 29;18(2):15. [CrossRef] [PubMed] [PubMed Central]
- Karaca. B. Effectiveness of high-intensity laser therapy in subacromial impingement syndrome. Photomed Laser Surg 2016;34:223–228. [CrossRef]
- Kim. S.H.; Kim. Y.H.; Lee. H.R.; Choi. Y.E. Short-term effects of high-intensity laser therapy on frozen shoulder: a prospective randomized control study. Man Ther 2015;20:751–757. [CrossRef]
- Choi. H.W.; Lee. J.; Lee. S.; et al. Effects of high intensity laser therapy on pain and function of patients with chronic back pain. J Phys Ther Sci 2017;29:1079–1081. [CrossRef]
| Author, year of the trial | Trial type, no of patients | Intervention | Outcome | Moments of the study | Results |
| Viliani, 2009 [18] | Prospective, randomized, 41 pts | Group A: HA intraarticular (4 weekly infiltrations). Group B: HILT, 10 sessions on alternate day. |
Function (WOMAC, Lequesne scale) | Baseline. End of the treatment. 4 months. |
Intragroup: significant improvement at the end of the treatment, maintaining the values at 4 months |
| Sabbahi, 2009 [19] | Prospective, randomized, 30 pts | HILT + ET. LLLT + ET. US + ET. 2 sessions / week, 3 weeks |
Pain (VAS), Walking distance without pain (in meters), Squatting with/without pain. |
Baseline. End of the treatment. |
Intragroup: improvement for all US and LLLT equally efficient Significant better results for HILT |
| Stiglig-Rogoznica, 2011 [15] | Prospective, clinical, pre- and after treatment, 96 pts | HILT, 10 consecutive days | Pain (VAS) | Baseline. End of the treatment. |
Pain significantly decreased |
| Viliani, 2012 [17] | Prospective, open label, before-after, clinical trial, 34 pts (41 knees) | Group A: HILT (ten sessions, 3000 J/session, on alternate days) Group B: control |
Function (WOMAC) | Baseline. End of the treatment. 4 months. |
Group A improved significantly after treatment and at 4 months (with a slight regression). Group B showed worsening of the parameter. |
| Kheshie, 2014 [20] | Prospective, single-blinded randomized controlled trial, 53 pts | Exercise + HILT Exercise + LLLT Exercise + sham 2 sessions / week, x 6 weeks |
Pain (VAS) Function (WOMAC) |
Baseline. End of the treatment. |
Both LLLT and HILT were better than sham. HILT improved significantly than LLLT. |
| Kim, 2016 [21] | Prospective, randomized, 20 pts | Group CPT (conservative physical therapy), Group HILT (CPT + HILT) 3 times/week, 4 weeks, 1500 J/cm2 |
Pain (VAS) Function (WOMAC) |
Baseline. End of the treatment. |
Intra-group: both groups improved statistically. Inter group: HILT had better scores. |
| Angelova, 2016 [22] | Prospective, pilot trial, randomized, clinical, single-blinded, placebo controlled, 72 patients | HILT (300J/session analgesic, 3000 J/session biostimulatory) versus sham, 7 daily sessions |
Pain Pedobarometric gait analysis (static and dynamic) |
Baseline. End of the treatment. 1 and 3 months. |
HILT group improved significantly after treatment and results were maintained at follow-up |
| Alayat, 2017 [23] | Prospective, single-blinded randomized controlled trial, 67 pts | Group 1: HILT, GCS, ET. Group 2: GCS + ET. Group 3: placebo + ET. 2 sessions/ week, 6 weeks |
Pain (VAS) Function (WOMAC) US (synovial thickness, femoral condylar cartilage) |
Baseline. End of the treatment. 3 months. |
Intragroup: all have significant improvement at 6 weeks, persistent at 3 months, except US cartilage thickness Between groups: HILT improved better, no difference between groups 2 and 3 |
| White, 2017 [16] | Prospective, case series, before- and after treatment, 39 pts | 1 – 3 daily sessions HILT | Pain (VAS) Function (ROM) Clinical issues (swelling, numbness) |
Baseline. End of treatment. 1 – 3 weeks. |
Improvement of all items at all moments |
| Nazari, 2018 [24] | Prospective, assessor-blind, randomized controlled trial, 93 pts | HILT + ET, TENS + US + ET, ET alone, 12 sessions, 3 sessions/week |
Pain (VAS) Function (flexion ROM, timed up and go test TUG, 6-min walk test 6MWT, WOMAC) |
Baseline. End of the treatment. 12 weeks. |
Intragroup: improvements at all moments, all parameters Between groups: HILT had better results on all parameters |
| Ciplak, 2018 [25] | Prospective, randomized, single blinded, 48 pts |
Hotpack + US + TENS + ET Hotpack + HILT + ET 10 sessions /2 weeks |
Pain (VAS) Function (WOMAC) |
Baseline. End of the treatment. 6 weeks. |
HILT was better significantly at all moments |
| Akaltun, 2021 [26] | Prospective, double-blind randomized placebo-controlled, 40 pts | HILT + ET (300J/session analgesia, 3000J/session biostimulation) Placebo + ET 5 sessions /week, 2 weeks |
Pain (VAS) Functional (WOMAC, flexion ROM) US: cartilage thickness |
Baseline. End of the treatment. 6 weeks. |
Both groups: 2 and 6 weeks: VAS, WOMAC-pain, WOMAC-function, WOMAC-stiffness, and WOMAC-total, cartilage thickness and FROM increased, 6 weeks: HILT+ET significant better values for all parameters versus PL+ET |
| Koevska, 2021 [27] | Prospective, one-sided blind randomized comparative study, 72 pts | HILT versus LLLT 10 sessions |
Pain (VAS) |
Baseline. End of the treatment. 30 days. |
Both goups improved significantly. After treatment, pain on VAS had lower scores for HILT groups that LLLT. |
| Siriratna, 2022 [28] | Prospective, randomized, single-blind, parallel group study, 42 pts | Conservative treatment + HILT (562.5 J/session) Conservative treatment + sham 2 – 3 sessions /week, a total of 10 sessions |
Pain (VAS) Function (WOMAC) |
Baseline. End of the treatment. |
Intra-group: both groups improved significantly all items. Inter-group: HILT had lower pain scores, significant. No difference for WOMAC. |
| Samaan, 2022 [29] | Prospective, single blinded, randomized, controlled trial 60 pts |
HILT + ET, LIPUS + ET,ET alone, 5 sessions /week, 2 weeks |
Pain (VAS) Function (ROM, WOMAC) Proprioception accuracy |
Baseline. End of the treatment. |
HILT better results in all parameters |
| Mostafa, 2022 [30] | Prospective, randomized controlled trial, 40 pts | ESWT, one session / week, 4 weeks. HILT, 3 sessions/ week, 4 weeks |
Pain (VAS) Function (6MWT, WOMAC) |
Baseline. End of the treatment. |
Intragroup: both improved Between groups: HILT better results |
| Ekici, 2023 [31] | Prospective, double-blinded, placebo-controlled, randomized, 60 pts | Group 1 (HILT + hotpack + TENS + ET) 300J/session followed by 3000J/session Group 2 (sham laser + hotpack + TENS + ET) 9 sessions / 3 weeks |
Pain (VAS) Functional (flexion ROM, isokinetic muscle strength, WOMAC) US: cartilage thickness |
Baseline. End of the treatment. 3 months |
Both groups improved all items at the end of treatment and at 3 months There was no difference between groups at any moment. |
| Taheri, 2023 [32] | Prospective, randomized, controlled, 56 pts | ET + NSAID + topic ointment. ET + NSAID + topic ointment + HILT (3 session / week, 2 weeks) |
Pain (VAS) Function (WOMAC) |
Baseline. End of treatment. 3 months. |
All parameters were better in HILT group at the end of the treatment and after 3 months |
| Katana, 2023 [33] | Prospective, descriptive, experimental, randomized trial, 60 pts | Group I, standard protocol + HIMS. Group II, standard protocol + HILT One session/week, 8 weeks |
Pain (Likert scale) Functional (ROM) Disability (KOOS) |
Baseline. Middle (4 weeks). End of the treatment (8 weeks). |
Intra-group analysis, both improved all parameters at all moments Intergroup analysis, group II had significant grester improvement at all moments |
| Ahmad, 2023 [34] | Prospective, randomized, double-blinded, parallel-group clinical trial, 34 pts | HILT + ET LLLT + ET Once a week, 12 weeks |
Pain Disability (KOOS) Function (active flexion ROM, Timed Up-and-Go test, TUG) |
Baseline. End of the treatment. |
Intragroup: all parameters improved HILT has significant greater improvement. |
| Astri, 2023 [35] | Prospective, double-blind randomized controlled clinical trial, 61 pts | LLLT + ET HILT + ET 3 sessions / week, 2 weeks |
Pain Function (50-feet walk test) |
Baseline. Pain (after every session). End of the treatment. |
Pain improved in both groups, with better evolution at every moment for HILT Function improved better for HILT |
| Roheym, 2023 [36] | Prospective, randomized, double-blinded, pre-, posttest trial, 30 pts with bilateral KO | ET ET + HILT (300J/session, followed by 3000 J /session) 3 sessions /week, 4 weeks |
US: suprapatellar fluid detection Function (WOMAC) |
Baseline. End of the treatment. |
Intragroup: significant improvements. Better results in HILT. |
| Wibisono, 2024 [37] | Prospective, randomized, pre-test and post-test-controlled, 27 pts | HILT versus LLLT 2 sessions /week, 4 weeks |
Berg Balance Scale | Baseline. End of the treatment. |
Intragroup: both groups improved significantly. HILT improved better. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





