Submitted:
25 June 2024
Posted:
27 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Cross-Sectional
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thacker, S.B.; Birkhead, G. Surveillance. In Gregg, M.B. Field Epidemiology. Second edition. Oxford University Press New York 2020, pp. 26–50.
- Waldman, R. Epidemiological surveillance: information is for action. Public Health Action 2020;10, 86.
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science 2020, 368, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Lau, H.; Khosrawipour, T.; Kocbach, P.; Ichii, H.; Bania, J.; Khosrawipour, V. Evaluating the massive underreporting and undertesting of COVID-19 cases in multiple global epicenters. Pulmonology 2021, 27, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Russell, T.W.; Golding, N.; Hellewell, J.; Abbott, S.; Wright, L.; Pearson, C.A.B.; van Zandvoort, K.; Jarvis, C.I.; Gibbs, H.; Liu, Y.; et al. Reconstructing the early global dynamics of under-ascertained COVID-19 cases and infections. BMC Med 2020, 18, 332. [Google Scholar] [CrossRef] [PubMed]
- Byambasuren, O.; Dobler, C.C.; Bell, K.; Rojas, D.P.; Clark, J.; McLaws, M.L.; Glasziou, P. Comparison of seroprevalence of SARS-CoV-2 infections with cumulative and imputed COVID-19 cases: Systematic review. PLoS One 2021, 16, e0248946. [Google Scholar] [CrossRef] [PubMed]
- Jayara,j V. J.; Ng, C.W.; Bulgiba, A., Appannan, M.R.; Rampal, S. Estimating the infection burden of COVID-19 in Malaysia. PLoS Negl Trop Dis 2022, 16, e0010887. [Google Scholar]
- Gibbons, C.L.; Mangen, M.J.; Plass, D.; Havelaar, A.H.; Brooke, R.J.; Kramarz, P.; Peterson, K.L.; Stuurman, A.L.; Cassini, A.; Fèvre, E.M.; et al. Measuring underreporting and under-ascertainment in infectious disease datasets: a comparison of methods. BMC Public Health 2014, 14, 147. [Google Scholar] [CrossRef] [PubMed]
- Ricoca-Peixoto, V.; Nunes, C.; Abrantes, A. Epidemic Surveillance of Covid-19: Considering Uncertainty and Under-Ascertainment. Port J Public Health 2020, 38, 1–7. [Google Scholar] [CrossRef]
- Ibrahim, N.K. Epidemiologic surveillance for controlling Covid-19 pandemic: types, challenges and implications. J Infect Public Health 2020, 13, 1630–1638. [Google Scholar] [CrossRef]
- Meadows, AJ, Oppenheim, B. ; Guerrero, J.; Ash, B.; Badker, R.; Lam, C.K.; Pardee, C.; Ngoon, C.; Savage, P.T.; Sridharan, V.; et al. Infectious disease underreporting is predicted by country-level preparedness, politics, and pathogen severity. Health Secur 2022, 20, 331–338.
- Albani, V.; Loria, J.; Massad, E.; Zubelli, J. COVID-19 underreporting and its impact on vaccination strategies. BMC Infect Dis 2021, 21, 1111. [Google Scholar] [CrossRef]
- You, C.; Gai, X.; Zhang, Y.; Zhou, X. Determining the Covertness of COVID-19 - Wuhan, China, China CDC Wkly 2021, 3, 170–173. 3.
- Havers, F.P.; Reed, C.; Lim, T.; Montgomery, J.M.; Klena, J.D.; Hall, A.J.; Fry, A.M.; Cannon, D.L.; Chiang, C.F.; Gibbons, A.; et al. Seroprevalence of antibodies to SARS-CoV-2 in 10 sites in the United States, -May 12, JAMA Intern Med 2020, 180, 1576–1586. 180, 23 March.
- Alves, T.H.E.; de Souza, T.A.; Silva, S.A.; Ramos, N.A.; de Oliveira, S.V. Underreporting of death by COVID-19 in Brazil's second most populous state. Front Public Health 2020, 8, 578645. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Agundez, A.; Ojo, O.; Hernández-Roig, H.A.; Baquero, C.; Frey, D.; Georgiou, C.; Goessens, M.; Lillo, R.E.; Menezes, R.; Nicolaou, N.; et al. Estimating the COVID-19 prevalence in Spain with indirect reporting via open surveys. Front Public Health 2021, 9, 658544. [Google Scholar] [CrossRef]
- Desta, B.N.; Ota, S.; Gournis, E.; Pires, S.M.; Greer, A.L.; Dodd, W.; Majowicz, S.E. Estimating the under-ascertainment of COVID-19 cases in Toronto, Ontario, March to May J Public Health Res 2023, 12, 22799036231174133.
- Milanesi, S.; De Nicolao, G. Correction of Italian under-reporting in the first COVID-19 wave via age-specific deconvolution of hospital admissions. PLoS One 2023, 18, e0295079. [Google Scholar] [CrossRef]
- Pullano, G.; Di Domenico, L.; Sabbatini, C.E.; Valdano, E.; Turbelin, C.; Debin, M.; Guerrisi, C.; Kengne-Kuetche, C.; Souty, C.; Hanslik, T.; et al. Underdetection of cases of COVID-19 in France threatens epidemic control. Nature 2021, 590, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Angulo, F.J.; Finelli, L.; Swerdlow, D.L. Estimation of US SARS-CoV-2 infections, symptomatic infections, hospitalizations, and deaths using seroprevalence surveys. JAMA Netw Open 2021, 4, e2033706. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Wisniak, A.; Piumatti, G.; Azman, A.S.; Lauer, S.A.; Baysson, H.; De Ridder, D.; Petrovic, D; Schrempft, S. ; Marcus K.; et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet 2020, 396, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernán, M.A.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; Fernández de Larrea, N.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Li, Z.; Guan, X.; Mao, N.; Luo, H.; Qin, Y.; He, N.; Zhu, Z.; Yu, J.; Li, Y.; Liu, J.; et al. Antibody seroprevalence in the epicenter Wuhan, Hubei, and six selected provinces after containment of the first epidemic wave of COVID-19 in China. Lancet Reg Health West Pac 2021, 8, 100094. [Google Scholar] [CrossRef] [PubMed]
- Domènech-Montoliu, S.; Pac-Sa, M.R.; Vidal-Utrillas, P.; Latorre-Poveda, M.; Del Rio-González, A.; Ferrando-Rubert, S.; Ferrer-Abad, G.; Sánchez-Urbano, M.; Aparisi-Esteve, L.; Badenes-Marques, G.; et al. "Mass gathering events and COVID-19 transmission in Borriana (Spain): A retrospective cohort study". PLoS One 2021, 16, e0256747. [Google Scholar] [CrossRef]
- Egger, M.; Bundschuh, C.; Wiesinger, K.; Gabriel, C.; Clodi, M.; Mueller, T.; Dieplinger, B. Comparison of the Elecsys® Anti-SARS-CoV-2 immunoassay with the EDI™ enzyme linked immunosorbent assays for the detection of SARS-CoV-2 antibodies in human plasma. Clin Chim Acta 2020, 509, 18–21. [Google Scholar] [CrossRef]
- Boletín Oficial del Estado (BOE) Orden SND/404/2020, de 11 de mayo, de medidas de vigilancia epidemiológica de la infección por SARS-CoV-2 durante la fase de transición hacia una nueva normalidad (State offical newsletter (BOE) Order SND/404/2020 of May 11, on epidemiological surveillance measures for SARS-CoV-2 infection during the transition pahe to a new normality) . https://www.boe.es/eli/es/o/2020/05/11/snd404 (accessed on 28 February 2023).
- Working group for the surveillance and control of COVID-19 in Spain. The first wave of the COVID-19 pandemic in Spain: characterisation of cases and risk factors for severe outcomes, as at 27 April Euro Surveill 2020, 25, 2001431.
- Barry, A.M; Yuill, C. Understanding the sociology of health: An introduction. Second edition. Sage Publications Ltd London 2008; pp. 91–118.
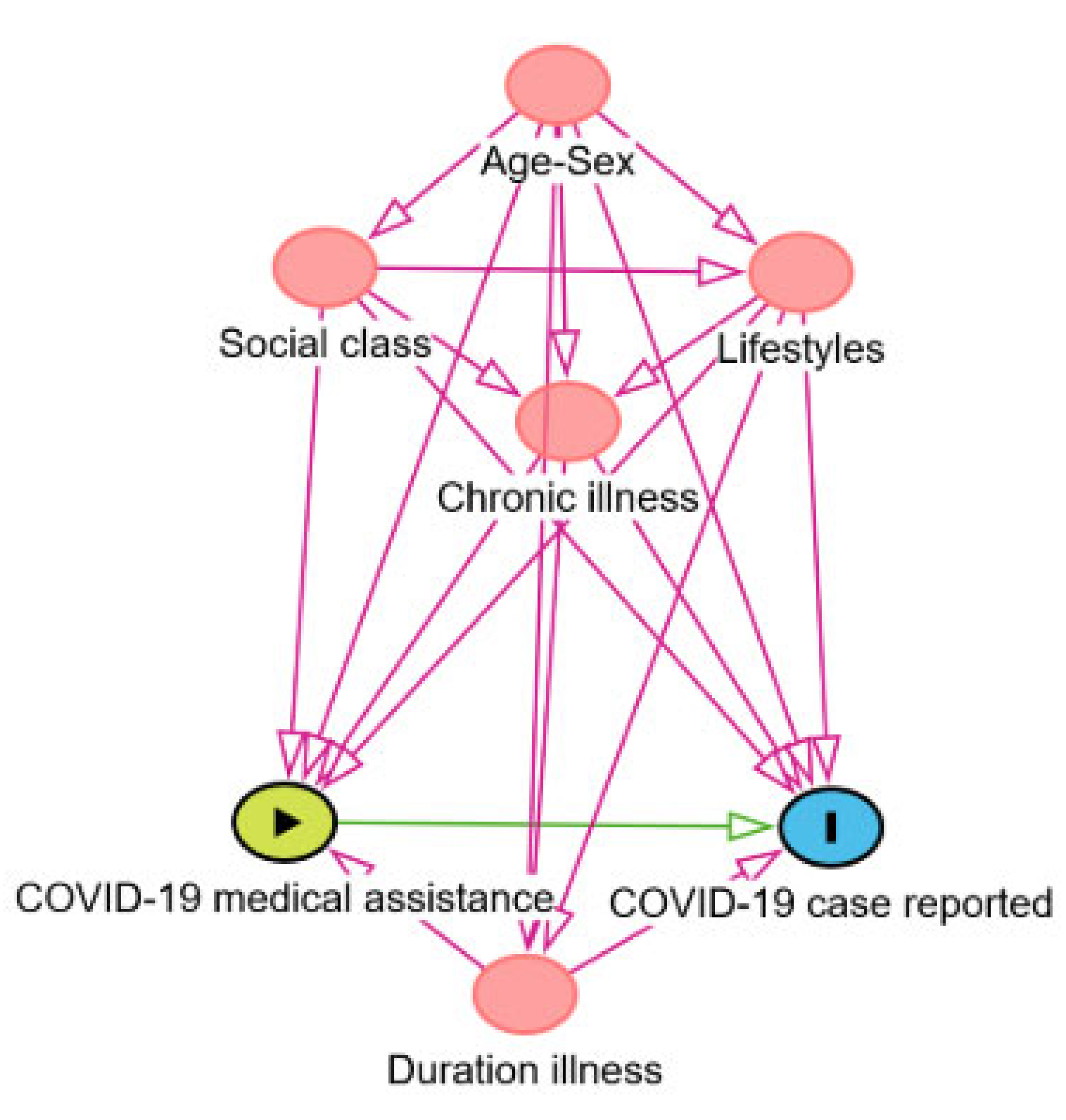
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liskiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: the R package 'dagitty'. Int J Epidemiol 2016, 45, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- González-Val, R.; Marcén, M. Mass gathering events and the spread of infectious diseases: Evidence from the early growth phase of COVID-Econ Hum Biol 2022, 46, 101140. 46.
- Brandl, M.; Selb, R.; Seidl-Pillmeier, S.; Marosevic, D.; Buchholz, U.; Rehmet, S. Mass gathering events and undetected transmission of SARS-CoV-2 in vulnerable populations leading to an outbreak with high case fatality ratio in the district of Tirschenreuth, Germany. Epidemiol Infect 2020, 148, e252. [Google Scholar] [CrossRef] [PubMed]
- Herng, L.C.; Singh, S.; Sundram, B.M.; Zamri, A.S.S.M.; Vei, T.C.; Aris, T.; Ibrahim, H.; Abdullah, N.H.; Dass, S.C.; Gill, B.S. The effects of super spreading events and movement control measures on the COVID-19 pandemic in Malaysia. Sci Rep 2022, 12, 2197. [Google Scholar] [CrossRef] [PubMed]
- Rocha, I.C.N.; Pelayo, M.G.A.; Rackimuthu, S. Kumbh Mela religious gathering as a massive superspreading event: Potential culprit for the exponential surge of COVID-19 cases in India. Am J Trop Med Hyg 2021, 105, :868–871. [Google Scholar] [CrossRef] [PubMed]
- Stange, M.; Mari, A.; Roloff, T.; Seth-Smith, H.M.; Schweitzer, M.; Brunner, M.; Leuzinger, K.; Søgaard, K.K.; Gensch, A.; Tschudin-Sutter, S, et al. SARS-CoV-2 outbreak in a tri-national urban area is dominated by a B.1 lineage variant linked to a mass gathering event. PLoS Pathog 2021, 17, e1009374. [Google Scholar] [CrossRef] [PubMed]
- Phalippou, L.; Zhang, D. The cost of mass gatherings during a pandemic. SSM Popul Health 2023, 23, 101460. [Google Scholar] [CrossRef] [PubMed]
- Millimet, D.L.; Parmeter, C.F. COVID-19 severity: A new approach to quantifying global cases and deaths. J R Stat Soc Ser A Stat Soc 2022, 185, 1178–1215. [Google Scholar] [CrossRef] [PubMed]
- Krantz, S.G.; Rao, A.S.R.S. Level of underreporting including underdiagnosis before the first peak of COVID-19 in various countries: Preliminary retrospective results based on wavelets and deterministic modeling. Infect Control Hosp Epidemiol 2020, 41, 857–859. [Google Scholar] [CrossRef] [PubMed]
- Shang, W.; Wang, Y.; Yuan, J.; Guo, Z.; Liu, J.; Liu, M. Global excess mortality during COVID-19 pandemic: A systematic review and meta-analysis. Vaccines (Basel) 2022, 10, 1702. [Google Scholar] [CrossRef]
- Vandoros, S. Excess mortality during the Covid-19 pandemic: Early evidence from England and Wales. Soc Sci Med. 2020, 258, 113101. [Google Scholar] [CrossRef] [PubMed]
- Royo-Cebrecos, C.; Vilanova, D.; López, J.; Arroyo, V.; Pons, M.; Francisco, G.; Carrasco, M.G.; Piqué, J.M.; Sanz, S.; Dobaño, C.; et al. Mass SARS-CoV-2 serological screening, a population-based study in the Principality of Andorra. Lancet Reg Health Eur 2021, 5, 100119. [Google Scholar] [CrossRef]
- Vial, P.A.; González, C.; Apablaza, M.; Vial, C.; Lavín, M.E.; Araos, R.; Rubilar, P.; Icaza, G.; Florea, A.; Pérez, C.; et al. First wave of SARS-CoV-2 in Santiago Chile: Seroprevalence, asymptomatic infection and infection fatality rate. Epidemics 2022, 40, 100606. [Google Scholar] [CrossRef] [PubMed]
- Pritsch, M.; Radon, K.; Bakuli, A.; Le Gleut, R.; Olbrich, L.; Guggenbüehl-Noller, J.M.; Saathoff, E.; Castelletti, N.; Garí, M.; et al. Prevalence and risk factors of infection in the representative COVID-19 cohort Munich. Int J Environ Res Public Health 2021, 18, 3572. [Google Scholar] [CrossRef] [PubMed]
- Abdella, S.; Riou, S.; Tessema, M.; Assefa, A.; Seifu, A.; Blachman, A.; Abera, A.; Moreno, N.; Irarrazaval, F.; Tollera, G.; et al. Prevalence of SARS-CoV-2 in urban and rural Ethiopia: Randomized household serosurveys reveal level of spread during the first wave of the pandemic. EClinicalMedicine. 2021, 35, 100880. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, T.A.; Auranen, K.; Kulathinal, S.; Härkänen, T.; Melin, M.; Palmu, A.A.; Jokinen, J. Underreporting of SARS-CoV-2 infections during the first wave of the 2020 COVID-19 epidemic in Finland-Bayesian inference based on a series of serological surveys. PLoS One 2023, 18, e0282094. [Google Scholar] [CrossRef] [PubMed]
- Mutevedzi, P.C.; Lokotfwako, V.; Kwatra, G. , Maphalala, G.; Baillie, V.; Dlamini, L., Dlamini, S.; Mhlanga, F.; Dlamini, T.; Nhlabatsi, N.; et al. Prevalence and levels of anti-SARS-CoV-2 antibodies in the Eswatini population and subsequent severity of the fourth COVID-19 epidemic wave. COVID 2024, 4, 317–333. [Google Scholar] [CrossRef]
- Sierra-Moros, M.J.; Martínez-Sánchez, E.V.; Monge-Corella, S.; García-San Miguel, L.; Suárez-Rodríguez, B.; Simón-Soria, F. Lecciones de la vigilancia de la COVID-Necesidad urgente de una nueva vigilancia en salud pública. Informe SESPAS 2022. Gac Sanit 2022, 36 (Suppl 1), S68–S75. [Google Scholar] [CrossRef] [PubMed]
- Guillen, M.; Bardes Robles, I.; Bordera-Cabrera, E.; Acebes-Roldán, X.; Bolancé, C.; Jorba, D.; Moriña, D. Acute respiratory infection rates in primary care anticipate ICU bed occupancy during COVID-19 waves. PLoS One 2022, 17, e0267428. [Google Scholar] [CrossRef]
- Álvarez, I.C.; Orea, L.; Wall, A. Estimating the propagation of both reported and undocumented COVID-19 cases in Spain: a panel data frontier approximation of epidemiological models. J Product Anal 2023, 59, 259–279. [Google Scholar] [CrossRef]
- Hervada-Vidal, X; Pérez-Romero, C.; Rodríguez-Artalejo, F.; Urbanos-Garrido, R. Evaluación del desempeño del Sistema Nacional de Salud Español frente a la pandemia del COVID Lecciones de y para una pandemia. Ministerio de Sanidad Madrid 2023. https://www.sanidad.gob.es/areas/alertasEmergenciasSanitarias/alertasActuales/nCov/documentos/EVALUACION_DEL_DESEMPENO_DEL_SNS_ESPANOL_FRENTE_A_LA_PANDEMIA_DE_COVID-19.pdf (accessed on 6 May 2024).
- Omori, R.; Mizumoto, K.; Nishiura, H. Ascertainment rate of novel coronavirus disease (COVID-19) in Japan. Int J Infect Dis 2020, 96, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Samant, Y.; Støver, M.; Haarberg, I.S.; Lohmann-Lafrenz, S.; Strømholm, T. Underreporting of work-related COVID-19 cases in Norway. New Solut 2023, 33, 149–153. [Google Scholar] [CrossRef]
- Wang, G.; Foney, D.M.; DiBari. J.; Hong, X.; Showell, N.; Kim, K.S.; Ji, H.; Pearson, C.; Mirolli, G.; Rusk, S.; Sharfstein, J.; et al. A prospective cohort study on the intersectionality of obesity, chronic disease, social factors, and incident risk of COVID-19 in US low-income minority middle-age mothers. Int J Obes (Lond) 2021, 45, 2577–2584. [Google Scholar] [PubMed]
- Alene, M.; Yismaw, L.; Assemie, M.A.; Ketema, D.B.; Mengist, B.; Kassie, B.; Birhan, T.Y. Magnitude of asymptomatic COVID-19 cases throughout the course of infection: A systematic review and meta-analysis. PLoS One 2021, 16, e0249090. [Google Scholar] [CrossRef] [PubMed]
- Domènech-Montoliu, S.; Puig-Barberà, J.; Pac-Sa, M.R.; Vidal-Utrillas, P.; Latorre-Poveda, M.; Del Rio-González, A.; Ferrando-Rubert, S.; Ferrer-Abad, G.; Sánchez-Urbano, M.; Aparisi-Esteve, L.; et al. Persistence of anti-SARS-CoV-2 antibodies six months after infection in an outbreak with five hundred COVID-19 cases in Borriana (Spain): A prospective cohort study. COVID 2021, 1, 71–82. [Google Scholar] [CrossRef]
- Kamalrathne, T.; Amaratunga, D.; Haigh, R.; Kodituwakku, L. Need for effective detection and early warnings for epidemic and pandemic preparedness planning in the context of multi-hazards: Lessons from the COVID-19 pandemic. Int J Disaster Risk Reduct 2023, 92, 103724. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, J.B. The United States' SARS-CoV-2 testing challenges underscore the need to improve surveillance ahead of the next health security crisis. Clin Chem 2021, 68, 30–32. [Google Scholar] [CrossRef]
- Han, Q.; Bragazzi, N.; Asgary, A.; Orbinski, J.; Wu, J.; Kong, J.D. Estimation of epidemiological parameters and ascertainment rate from early transmission of COVID-19 across Africa. R Soc Open Sci 2023, 10, 230316. [Google Scholar] [CrossRef]
- Farsalinos, K.; Poulas, K.; Kouretas, D.; Vantarakis, A.; Leotsinidis, M.; Kouvelas, D.; Docea, A.O.; Kostoff, R.; Gerotziafas, G.T.; Antoniou, M.N.; et al. Improved strategies to counter the COVID-19 pandemic: Lockdowns vs. primary and community healthcare. Toxicol Rep 2021, 8, 1–9. [Google Scholar] [CrossRef]
- Brainard, J.; Lake, I.R.; Morbey, R.A.; Jones, N.R.; Elliot, A.J.; Hunter, P.R. Comparison of surveillance systems for monitoring COVID-19 in England: a retrospective observational study. Lancet Public Health 2023, 8, e850–e858. [Google Scholar] [CrossRef]
- Ageron, F.X.; Hugli, O.; Dami, F.; Caillet-Bois, D.; Pittet, V.; Eckert, P.; Beysard, N.; Carron, P.N. Lessons from COVID-19 syndromic surveillance through emergency department activity: a prospective time series study from western Switzerland. BMJ Open 2022, 12, e054504. [Google Scholar] [CrossRef] [PubMed]
- Arnedo-Pena, A.; Guillen-Grima, F. Incidence and risk factors of the COVID-19 pandemic: An epidemiological approach. Epidemiologia 2023, 4, 134–136. [Google Scholar] [CrossRef] [PubMed]
- Clark, E.C.; Neumann, S.; Hopkins, S.; Kostopoulos, A.; Hagerman, L.; Dobbins, M. Changes to public health surveillance methods due to the COVID-19 pandemic: scoping review. JMIR Public Health Surveill 2024, 10, e49185. [Google Scholar] [CrossRef] [PubMed]
- Oliver, N.; Barber, X.; Roomp, K.; Roomp, K. Assessing the impact of the COVID-19 pandemic in Spain: Large-scale, online, self-reported population survey. J Med Internet Res 2020, 22, e21319. [Google Scholar] [CrossRef] [PubMed]
- Splinter, B.; Saadah, N.H.; Chavannes, N.H.; Kiefte-de Jong, J.C.; Aardoom, J.J. Optimizing the acceptability, adherence, and inclusiveness of the COVID radar surveillance app: Qualitative study using focus groups, thematic content analysis, and usability testing. JMIR Form Res 2022, 6, e36003. [Google Scholar] [CrossRef] [PubMed]
- Kondylakis, H.; Katehakis, D.G.; Kouroubali, A.; Logothetidis, F.; Triantafyllidis, A.; Kalamaras, I.; Votis, K.; Tzovaras, D. COVID-19 mobile apps: A systematic review of the literature. J Med Internet Res 2020, 22, e23170. [Google Scholar] [CrossRef]
- Anglemyer, A. , Moore, T.H.; Parker, L.; Chambers, T.; Grady, A.; Chiu, K.; Parry, M.; Wilczynska, M.; Flemyng, E.; Bero, L. Digital contact tracing technologies in epidemics: a rapid review. Cochrane Database Syst Rev 2020, 8, CD013699. [Google Scholar] [PubMed]
- Mavragani, A. Infodemiology and Infoveillance: Scoping Review. J Med Internet Res 2020, 22, e16206. [Google Scholar] [CrossRef] [PubMed]
- Mehraeen, E.; Pashaei, Z.; Akhtaran, F.K.; Dashti, M.; Afzalian, A.; Ghasemzadeh, A.; Asili, P.; Kahrizi, M.S.; Mirahmad, M.; Rahimi, E.; et al. Estimating Methods of the Undetected Infections in the COVID-19 Outbreak: A Systematic Review. Infect Disord Drug Targets. 2023, 23, e240123213106. [Google Scholar] [CrossRef]
- Chang, Z.; Zhan, Z.; Zhao, Z.; You, Z.; Liu, Y.; Yan, Z.; Fu, Y. , Liang, W.; Zhao, L. Application of artificial intelligence in COVID-19 medical area: a systematic review. J Thorac Dis. 2021, 13, 7034–7053. [Google Scholar] [CrossRef]
- Cildoz, M.; Gaston, M.; Frias, L.; Garcia-Vicuña, D.; Azcarate, C.; Mallor, F. Early detection of new pandemic waves. Control chart and a new surveillance index. PLoS One 2024, 19, e0295242. [Google Scholar] [CrossRef]
- Brizzi, A.; O'Driscoll, M.; Dorigatti, I. Refining reproduction number estimates to account for unobserved generations of infection in emerging epidemics. Clin Infect Dis 2022, 75, e114–e121. [Google Scholar] [CrossRef]
- Amereh, F.; Negahban-Azar, M.; Isazadeh, S.; Dabiri, H.; Masihi, N.; Jahangiri-Rad, M.; Rafiee, M. Sewage systems surveillance for SARS-CoV-2: Identification of knowledge gaps, emerging threats, and future research needs. Pathogens 2021, 10, 946. [Google Scholar] [CrossRef]
- Gogoi, G.; Singh, S.D.; Kalyan, E.; Koch, D.; Gogoi, P.; Kshattry, S.; Mahanta, H.J.; Imran, M.; Pandey, R.; Bharali, P. An interpretative review of the wastewater-based surveillance of the SARS-CoV-2: where do we stand on its presence and concern? Front Microbiol 2024, 15, 1338100. [Google Scholar] [CrossRef]
- Robishaw, J.D.; Alter, S.M.; Solano, J.J.; Shih, R.D.; DeMets, D.L.; Maki, D.G.; Hennekens, C.H. Genomic surveillance to combat COVID-19: challenges and opportunities. Lancet Microbe 2021, 2, e481–e484. [Google Scholar] [CrossRef]
- Bendall, E.E.; Paz-Bailey, G.; Santiago, G.A.; Porucznik, C.A.; Stanford, J.B.; Stockwell, M.S.; Duque, J.; Jeddy, Z.; Veguilla, V.; Major, C.; et al. SARS-CoV-2 genomic diversity in households highlights the challenges of sequence-based transmission inference. mSphere 2022, 7, e0040022. [Google Scholar] [CrossRef]
- Choi, Y.; Ladoy, A.; De Ridder, D.; Jacot, D.; Vuilleumier, S.; Bertelli, C.; Guessous, I.; Pillonel, T.; Joost, S.; Greub, G. Detection of SARS-CoV-2 infection clusters: The useful combination of spatiotemporal clustering and genomic analyses. Front Public Health 2022, 10, 1016169. [Google Scholar] [CrossRef]
- Bilal, M.Y.; Klutts, J.S. Molecular epidemiological investigations of localized SARS-CoV-2 outbreaks-utility of public algorithms. Epidemiologia 2022, 3, 402–411. [Google Scholar] [CrossRef]
- López, M.G.; Chiner-Oms, Á.; García de Viedma, D.; Ruiz-Rodriguez, P.; Bracho, M.A.; Cancino-Muñoz, I.; D'Auria, G.; de Marco, G.; García-González, N.; Goig, G.A.; et al. The first wave of the COVID-19 epidemic in Spain was associated with early introductions and fast spread of a dominating genetic variant. Nat Genet 2021, 53, 1405–1414. [Google Scholar] [CrossRef]
- Sharmin, M.; Manivannan, M.; Woo, D.; Sorel, O.; Auclair, J.R.; Gandhi, M.; Mujawar, I. Cross-sectional Ct distributions from qPCR tests can provide an early warning signal for the spread of COVID-19 in communities. Front Public Health 2023, 11, 1185720. [Google Scholar] [CrossRef]
- Ley 14/1986, de 25 de Abril, General de Sanidad (Law General of Health). Available online: https://www.boe.es/eli/es/l/1986/04/25/14/con (accessed on 2 May 2024). (In Spanish)..
- Ley 16/2003, de 28 de Mayo, de Cohesión y Calidad del Sistema Nacional de Salud. (Law of Cohesion and Quality of the National System of Health). Available online: https://www.boe.es/eli/es/l/2003/05/28/16 (accessed on 2 May 2024). (In Spanish)..
- Ley 33/2011, de 4 de Octubre, General de Salud Pública (Law General of Public Health). Available online: https://www.boe.es/eli/es/l/2011/10/04/33/con (accessed on 2 May 2024). (In Spanish)..
| Variables | Reported cases N=36 (%) |
Unreported cases N=432 (%) |
p-value |
|---|---|---|---|
| Age (years)±SD1 | 45.7±16.4 | 37.2±16.5 | 0.001 |
| Male | 14 (38.8) | 162 (37.5) | 0.860 |
| No received medical assistance for COVID-19 disease | 2 (5.6) | 236 (54.6) | 0.000 |
| Duration illness (days)±SD1,2 | 24.2±21.9 | 10.5±14.9 | 0.000 |
| No chronic illness4 | 14 (38.8) | 295 (68.3) | 0.001 |
| Middle and lower social classes5,6 | 25 (69.4) | 375 (87.4) | 0.009 |
| Body mass index (kg/m2)±SD1,7 | 26.4±5.8 | 25.0±5.0 | 0.183 |
| Obesity ≥30 kg/m2±SD1,8 | 10 (27.8) | 69 (16.1) | 0.102 |
| Current smoker9 | 3 (8.3) | 64 (15.3) | 0.333 |
| Alcohol intake yes10 | 11 (30.6) | 100 (23.8) | 0.417 |
| Habitual physical exercise yes | 17 (47.2) | 256 (59.3) | 0.164 |
| Nutritional diet yes11 | 10 (27.8) | 75 (17.4) | 0.121 |
| Variable | OR | 95% CI | aOR | 95% CI | p-value |
|---|---|---|---|---|---|
| Age (years)1 | 0.97 | 0.95-0.99 | 0.97 | 0.94-0.99 | 0.003 |
| Male2 | 0.94 | 0.47-1.89 | 1.16 | 0.94-2.35 | 0.690 |
| No medical assistance for COVID-19 disease3 | 17.6 | 4.86-86.30 | 10.83 | 2.49-47.11 | 0.001 |
| Duration illness (days)4 | 0.98 | 0.96-0.99 | 0.98 | 0.97-0.99 | 0.037 |
| No chronic illness5 | 3.34 | 1.66-6.72 | 2.81 | 1.28-6.17 | 0.010 |
| Middle and lower social classes,6 | 3.06 | 1.42-6.56 | 3.12 | 1.42-6.85 | 0.005 |
| Body mass index (kg/m2)7 | 0.94 | 0.88-1.01 | 0.98 | 0.91-1.06 | 0.651 |
| Obesity ≥30 kg/m2 7 | 0.50 | 0.33-1.08 | 0.64 | 0.28-1.47 | 0.294 |
| Current smoker8 | 1.98 | 0.59-6.67 | 2.14 | 0.62-7.41 | 0.228 |
| Alcohol intake yes9 | 0.70 | 0.34-1.49 | 0.59 | 0.26-1.33 | 0.203 |
| Habitual physical exercise10 yes | 1.63 | 0.2-3.21 | 1.91 | 0.91-4.00 | 0.085 |
| Nutritional diet yes11 | 0.55 | 0.25-1.18 | 0.65 | 0.29-1.48 | 0.307 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





