1. Introduction
Adolescent idiopathic scoliosis (AIS) is a complex three-dimensional misalignment of the spine consisting of a coronal curve of more than 10°, vertebral rotation [
1] and altered sagittal curvature [
2,
3,
4], with no congenital or neuromuscular abnormal findings [
5]. AIS can progress over the years if untreated, especially during growth, and can cause significant musculoskeletal problems, pain in adulthood, pulmonary impairment and psychological problems [
6,
7,
8,
9]. Measuring the Cobb angle on a standing posteroanterior full-length spine X-ray is the gold standard for diagnosing AIS, assessing its severity, monitoring its changes and making decisions about its treatment [
10,
11,
12,
13,
14]. The selection of the vertebrae defining the boundaries of the scoliotic curves plays a pivotal role in determining the Cobb angle and accurately describing the curve’s length, which is crucial for devising appropriate treatment strategies. For instance, if a scoliotic curve exceeds 50°, the most appropriate treatment is posterior spinal fusion, which irreversibly alters the biomechanical function of the spine [
15,
16,
17]. In this surgical procedure, selecting the appropriate vertebral boundaries determines the curve length to be fused, affecting the biomechanical stability achieved and reducing the incidence of post-surgical complications [
18,
19]. Conversely, there is a consensus in the literature that selecting the boundary vertebrae in the Cobb angle measurement method in AIS X-ray is a significant source of intrinsic error [
20,
21,
22,
23] or the primary source of intrinsic error [
24,
25,
26,
27]. The literature on the accuracy and precision of the Cobb method in AIS X-ray indicates that potential sources of intrinsic error in traditional manual measurement include erroneous choice of vertebral endplates, inaccurate drawing of lines along the vertebral endplates, imprecise drawing of perpendicular lines, and inaccurate angle measurement itself [
22,
25,
26,
27,
28,
29].
This study aims to evaluate the error in selecting cranial and caudal boundary vertebrae on AIS X-ray images by experienced and novice observers. Additionally, it aims to explore the correlation between the error in selecting boundary vertebrae and the error in measuring the Cobb angle and between the error in selecting boundary vertebrae and the error in quantifying the length of scoliotic curves.
2. Materials and Methods
2.1. Measurement Tool
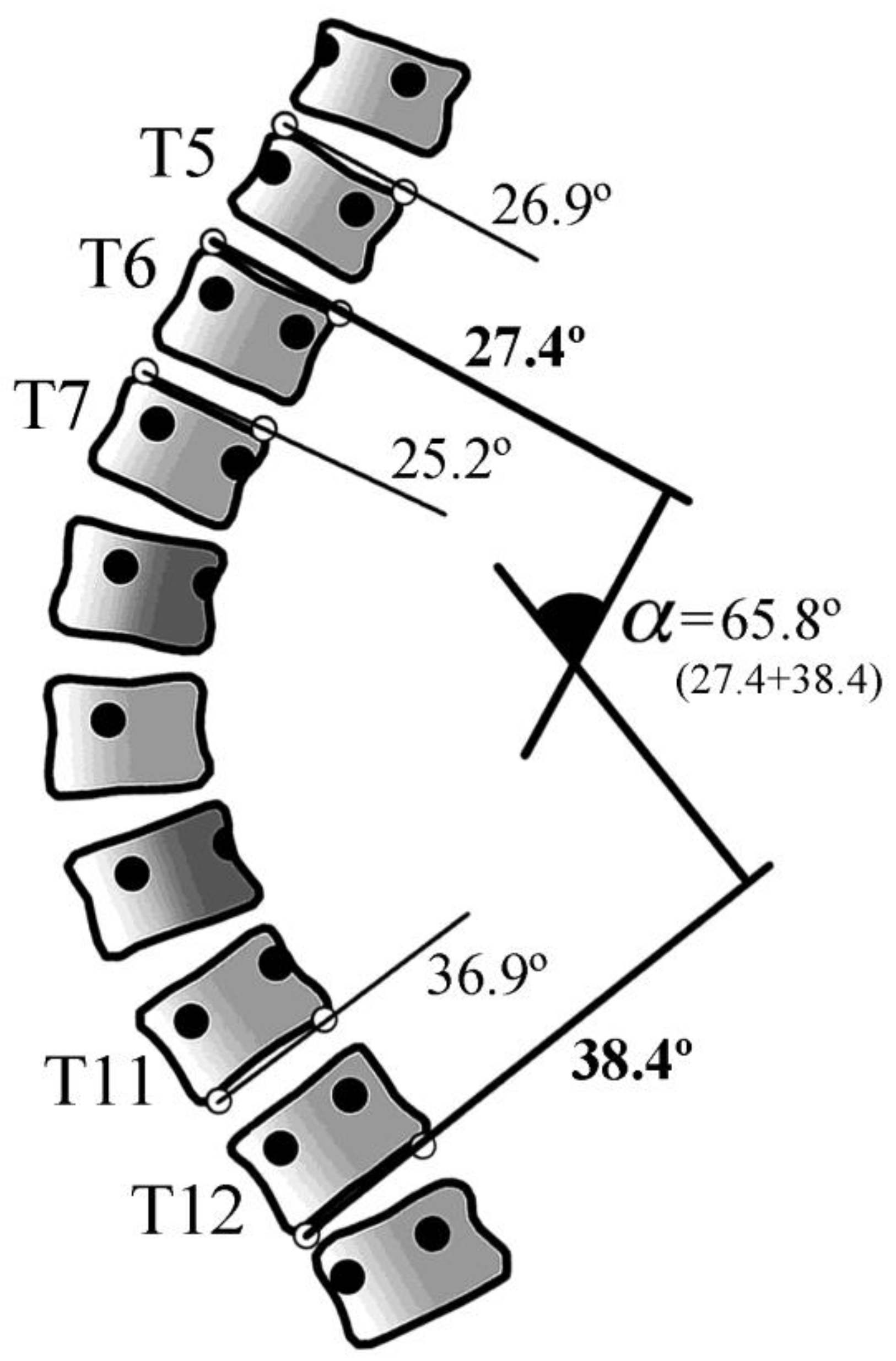
The software Traumameter v.873 [Hurtado-Avilés and Santonja-Medina, registration number 08/2021/374, Murcia, Spain] was employed to identify the limit vertebrae, measure the Cobb angle, and quantify the length of the scoliotic curves. This software replicates the manual Cobb angle measurement method observed in AIS X-rays, enabling measurements with high intra- and inter-observer accuracy and precision (MBE=1.8°, SD=0.65°, CI95% 1.58°-2.02° and MBE=1.82°, SD=0.59°, CI95% 1.62°-2.02°, respectively) [
30]. The software eliminates the intrinsic error due to inaccurate drawing of perpendicular lines and inaccurate angle measurement. On the other hand, it reduces the error due to the wrong choice of boundary vertebrae and inaccurate line drawing along the vertebral endplates through tools such as the ability to zoom in on the regions of interest and to vary the contrast (fractional difference in the optical density of brightness between two regions of an image) of the digital X-ray image. The software allows the observer to draw lines along the vertebral endplates of various cranial and caudal vertebrae and selects the steepest ones, returning the Cobb angle result in degrees (
Figure 1).
2.2. Study Design and Measurement Protocol
A prospective and observational study was conducted on 68 scoliotic curves in 42 standing frontal full-length spine X-rays of patients with AIS. The X-ray images were selected retrospectively from an image repository during routine medical care of patients with AIS. Our study adhered to the World Medical Association Declaration of Helsinki’s ethical standards, as revised in 2013. The study was exempted from the requirement for ethical approval since the complete and irreversible anonymisation of the images did not involve data processing. The X-ray sample is homogeneous, has equivalent image quality, and is without defects. The X-ray images were obtained natively in digital format (in DICOM, with a resolution of 283.46 pixels/mm).
According to the angular classification proposed by the International Society on Scoliosis Orthopaedic and Rehabilitation Treatment [
31], the selected X-rays showed asymmetry in 2 cases (curves between 0° and 10°), low scoliosis in 17 cases (curves between 11° to 20°), moderate scoliosis in 25 cases (curves between 21° and 35°), moderate to severe scoliosis in 9 cases (curves between 36° and 40°), severe scoliosis in 11 cases (curves between 41° and 50°), severe to very severe scoliosis in 1 cases (curves between 51° and 55°), and very severe scoliosis in 3 cases (curves with 56° or more). Of the cranial vertebrae, 66 (97.1%) were thoracic and 2 (2.9%) were lumbar. Of the caudal vertebrae, 35 (51.5%) were thoracic and 33 (48.5%) were lumbar.
The Hopkins absolute reliability criteria [
32,
33] were employed to assess validity and reliability. These criteria stipulate that a minimum of 30 cases must be included, at least six blinded observers must act as assessors, and at least three tests must be conducted per observer, with a minimum of two-week intervals between tests. A specialist in Orthopaedics and Traumatology and a specialist in Physical Medicine and Rehabilitation, with over 35 years of professional experience each in the field of the spine, were engaged in a joint and simultaneous measurement of all scoliotic curves on the same computer to establish a gold standard for the Cobb angles, the boundary vertebrae, and the length of each curve.
The research was conducted with eight independent evaluators with varying experience levels in measuring Cobb angles. Four observers, designated as “Experienced”, were one Orthopaedic specialist and three Physical Therapy and Rehabilitation specialists with more than 20 years of experience in the routine measurement of radiographs of scoliotic patients in their daily practice, but who had not determined their intra-observer error. Despite their theoretical knowledge of X-ray measurement techniques for the spine, the four “Novice” observers from various health sciences disciplines (without being orthopaedic surgeons) had never applied Cobb’s method in practice. Prior to the commencement of the measurements, a five-hour briefing was held, during which comprehensive information was provided on the study and training in the use of the Traumameter v.873 software. In each X-ray, each observer identified the curves, measured Cobb’s angle on them with the software, and recorded the resulting measurement and the uppermost and lowest vertebrae of each scoliotic curve in an Excel table. The observers conducted the measurements on three occasions, with a one-month interval between each measurement. A total of 1632 curves were evaluated for this study (204 curves by each observer). The study coordinator randomly assigned the sequence in which the radiographic images were presented in each test to avoid bias, keeping the randomisation key confidential.
2.3. Statistics
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 25 for Windows (SPSS, Inc., Chicago, Illinois, USA). The values of the variable “Cobb angle error” (eCobb) were obtained in degrees with one decimal place due to the scale of the software measuring tool. The values of the variables “error in the choice of the cranial vertebra” (eCr), “error in the choice of the caudal vertebra” (eCa) and “error in the quantification of the length of the scoliotic curve” (eLC), were obtained in the unit “number of vertebrae per curve” with one decimal place. The eCobb, eCr, eCa and eLC values for each scoliotic curve were obtained from the distribution of the 24 scoliotic curve measurements (8 observers in the three tests). In the measurement distributions of each curve, values lower than Q1-(1.5xIQR) and higher than Q3+(1.5xIQR) (where IQR is the interquartile range) were identified. These values were considered outliers and eliminated from each distribution (1.96% of eCobb; 0.12% of eCr; 0.06% of eCa; 0% of eLC). The percentage error of each observer in the choice of caudal and cranial vertebrae was used to obtain four distributions, namely “percentage of cranial and caudal vertebrae wrongly chosen by experienced and novices, respectively”. These distributions did not contain any outliers. The Shapiro-Wilk test was employed to ascertain that the p-values of the data from these distributions were above the significance level of 0.05, with the null hypothesis that the data fit a normal distribution being accepted. In all cases, p≥0.34. All variables were reported as Mean Bias Error (MBE), Standard Deviation (SD), Standard Error of the Mean (SEM) and Confidence Interval of 95%. A Student’s t-test was employed to ascertain whether the differences in MBE values between each pair of measurements were statistically significant. Two-sided p values and the CI95% were reported, and significance was accepted at p<0.05. Pearson correlation was obtained between the distributions eCr+Ca (sum of the distributions eCr and eCa) and eCobb and between the distributions eCr+Ca and eLC.
3. Results
Table 1a and 1b (supplementary material) show the gold standard and observer-recorded data for the Cobb angle and boundary vertebrae, respectively. Table 2 (supplementary material) shows the outliers removed.
Table 3 shows the data for the error selection of the boundary vertebrae, the measurement of the Cobb angle, and the quantification of the length of the scoliotic curves for the total set of measurements.
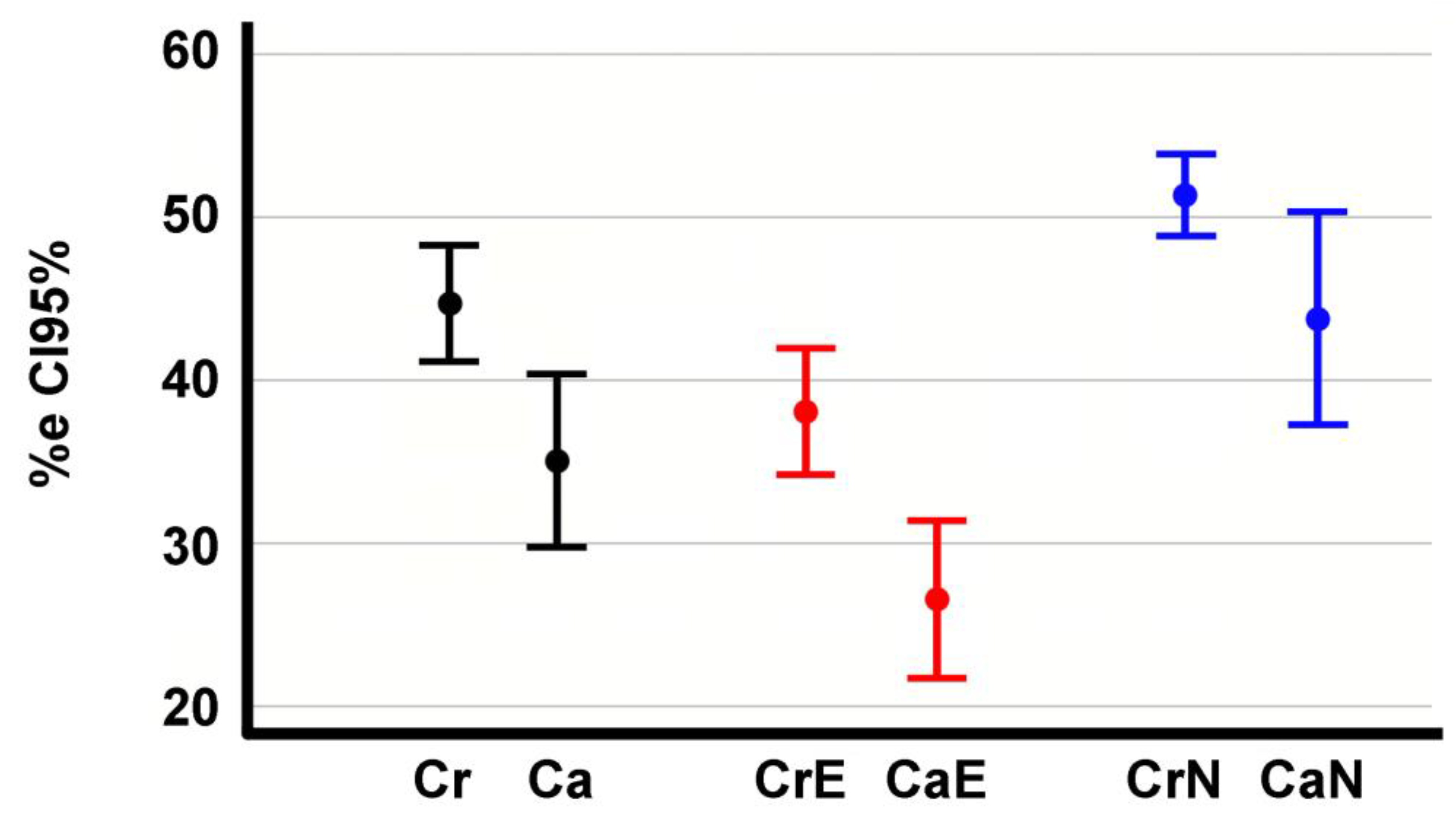
The error rate in the choice of cranial vertebrae is higher than for caudal vertebrae (44.7%, CI95% 41.05-48.3 compared to 35%, CI95% 29.7-40.4). This difference is statistically significant (p=0.008) (
Figure 2). The error percentage in the choice of boundary vertebrae is lower in the experienced than in the novices, with a statistically significant difference (p=0.009 between cranial vertebrae, p=0.000 between caudal vertebrae) (
Figure 2). The percentage of erroneous choices made by experienced was 37.99% (CI95% 33.96-42), while that of novices was 51.35% (CI95% 48.77-53.97). Experienced incorrectly identified the caudal vertebra in 26.35% (CI95% 21.45-31.25) of the measurements, while novices incorrectly identified it in 43.75% (CI95% 37.06-50.44).
Experienced evaluators incorrectly identified one boundary vertebra in 36.6% (274) of the scoliotic curves, while in 15.4% (126) of the cases, they incorrectly identified two boundary vertebrae. In contrast, novices incorrectly identified one boundary vertebra in 34.7% (278) of the scoliotic curves, while in 30.39% (248) of the cases, they incorrectly identified two boundary vertebrae.
Table 4 (supplementary material) presents the number of incorrectly selected boundary vertebrae and the error in the Cobb angle for each measurement. It demonstrates that the error in the Cobb angle measurements for each scoliotic curve is randomly distributed and unrelated to the number of incorrectly selected boundary vertebrae.
Further analysis was performed on the distribution of Cobb angle measurements for each scoliotic curve to identify the 50% of measurements closest to the gold standard value. This analysis showed that 44.6% (365) of these measurements were carried out with the two boundary vertebrae correctly identified. In contrast, 33.9% (278) were obtained with one of the boundary vertebrae incorrectly identified, and 21.5% (176) were obtained with both boundary vertebrae incorrectly identified.
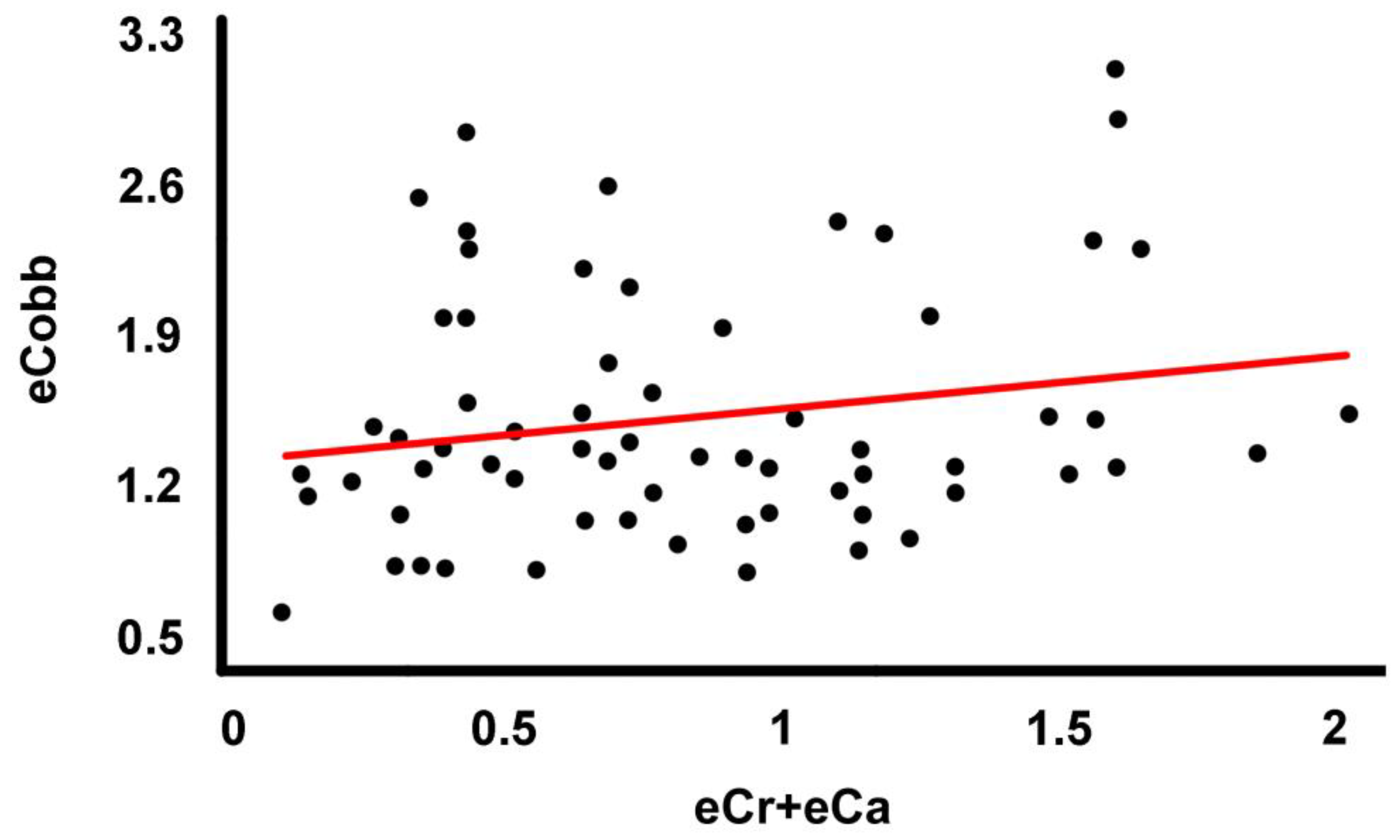
The correlation between the error in the choice of boundary vertebrae and the error in the Cobb angle measurements is not statistically significant (r= 0.198, r^2=0.039, p=0.111) (
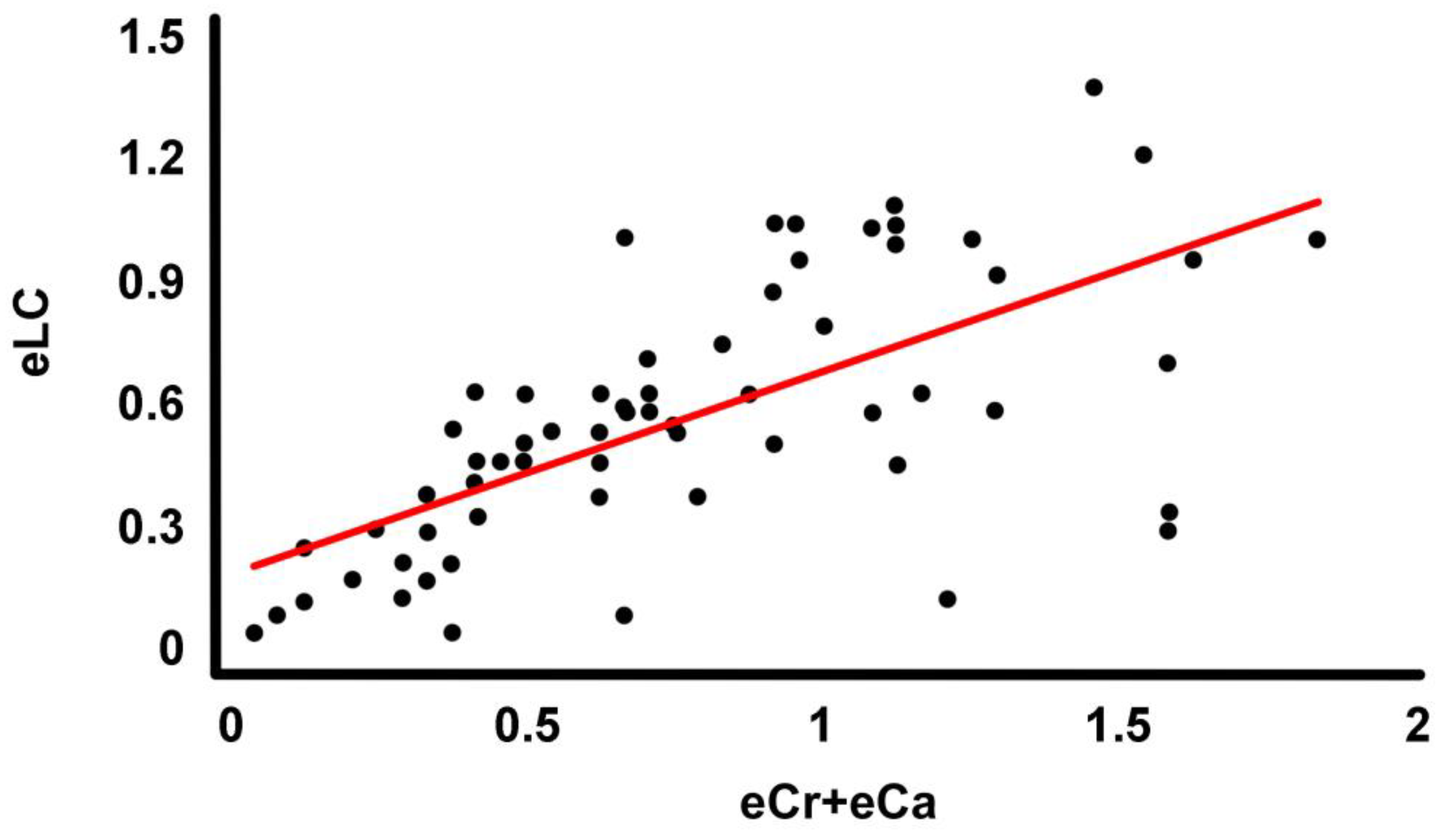
Figure 3). The correlation between the error in the choice of the limit vertebrae and the error in the determination of the length of the scoliotic curves is statistically significant (r=0.673, r^2= 0.453, p=0.000) and positive (
Figure 4). The linear equation forced to the origin of coordinates describing the correlation is eCr+eCa=1.243·eLC (r= 0.610).
4. Discussion
The most important finding of the present study was that errors in selecting boundary vertebrae are common among both experienced and novice observers, with a greater frequency of error in the cranial vertebrae. Likewise, the lack of dependence between the boundary vertebrae error and the Cobb angle error is also relevant.
In AIS, the error in selecting the uppermost and the lowest vertebrae when measuring the Cobb angle can be relevant to the correct decision on treatment (observation, physiotherapy, orthosis, surgery) and its characteristics [
10,
11,
13,
34]. For example, if the applicable treatment for a scoliotic curve is instrumented arthrodesis, longer than necessary fusion means sacrificing too many segments of motion and therefore function [
34,
35,
36,
37], increased risk of neurological complications and infection, and increased cost. There is consensus that the incorrect selection of the boundary vertebrae is a significant source of intrinsic error in measuring the Cobb angle on AIS X-rays [
22,
23,
27]. However, in studies of Cobb angle inaccuracy where the error is measured using preselected boundary vertebrae, the erratum is not significantly improved, with intra-observer MBE error in such studies ranging from 3° to 9.04° [
25,
26,
28,
29,
38].
Our study’s absolute error in the Cobb angle mean was MBE=1.53°, CI95% 1.42°-1.63°. With this accuracy and precision, we found that the error in the Cobb angle measurements was not related to the correct choice of the boundary vertebrae (p=0.111). Of the 50% of Cobb angle measurements closest to the actual value, 55.4% (454) were obtained by incorrectly selecting at least one boundary vertebrae. In summary, the erroneous choice of the boundary vertebrae is not a source of intrinsic error in the Cobb method but a consequence of the inaccurate drawing of the lines along the vertebral endplates.
The error in selecting the boundary vertebrae and the error in measuring the Cobb angle have the exact cause when using the Traumameter v.873 software. When using the manual Cobb method, the sources of error are many, but with our software, they are reduced to one; the inaccuracy in drawing the straight line parallel to the upper and lower surface of the boundary vertebrae is greater than the difference in inclination of the vertebrae adjacent to the boundary vertebrae and the boundary vertebrae. Due to the high accuracy and precision of the TraumaMeter v.873 software, the error in the choice of boundary vertebrae results in a minimal error in determining the Cobb angle, as the difference in inclination between the correct and incorrectly chosen boundary vertebrae is tiniest. Our study found that the error rate in the choice of boundary vertebrae is higher in cranial vertebrae (44.7%) than in caudal vertebrae (35%), which is statistically significant. The fact that cranial vertebrae tend to appear in the thoracic region, with the overlapping of different organs and structures on X-ray, or the better visibility of the lower region of the endplate architecture [
39] could justify the more significant error in their choice.
The error rate in choosing boundary vertebrae was statistically significantly higher in novice observers than in experienced. Experienced wrongly chose at least one of the boundary vertebrae in 52% of the measurements (400) and novices in 65.1% (526). This aspect can be explained by the lower Cobb angle measurement error shown by experienced measurers [
30] when measuring with the TraumaMeter v.873 software and manually traditionally. Our results show a significant positive correlation between the error in choosing boundary vertebrae and the error in determining the length of the scoliotic curves. From the regression line obtained from the correlation, we can predict an increase in the error in scoliotic curve length determination of 0.805 vertebrae for each incorrectly chosen boundary vertebra.
This study is not without its limitations. Firstly, we did not consider the computer equipment of each observer (e.g. visible image size, display resolution, luminance, contrast ratio or the characteristics of the mouse or touchpad), which may have influenced the accuracy of the measurements. Secondly, the outliers removed from the distribution used in the study could be due not only to imperfect measurement but also to errors in recording the value of the measurements in the database provided by each observer. Despite these limitations, the authors believe that the study results are valuable. One of the strengths of our study is that its design meets the Hopkins criteria (minimum of 30 cases, at least six blinded observers and at least three tests per observer, separated by at least two weeks) [
32,
33]. Also, we established training sessions for the observers to avoid measurement bias.
5. Conclusions
Errors in selecting boundary vertebrae are common among experienced and novice observers, with a greater frequency of error in the cranial vertebrae. There is no correlation between the error in selecting the boundary vertebrae and the Cobb angle error. Inappropriate choice of boundary vertebrae leads to an estimated error in determining the length of the scoliotic curves of 0.805 vertebrae for each boundary vertebra chosen incorrectly.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, José Hurtado-Avilés and Fernando Santonja-Medina; Data curation, José Hurtado-Avilés; Formal analysis, José Hurtado-Avilés and Vicente J. León-Muñoz; Investigation, Fernando Santonja-Medina; Methodology, José Hurtado-Avilés and Fernando Santonja-Medina; Project administration, José Hurtado-Avilés and Fernando Santonja-Medina; Software, José Hurtado-Avilés and Fernando Santonja-Medina; Supervision, José Hurtado-Avilés, Vicente J. León-Muñoz, Fernando Santonja-Medina, Paolo Raimondi and Francisco Martínez-Martínez; Validation, José Hurtado-Avilés, Vicente J. León-Muñoz, Fernando Santonja-Medina, Paolo Raimondi and Francisco Martínez-Martínez; Visualization, José Hurtado-Avilés and Vicente J. León-Muñoz; Writing – original draft, José Hurtado-Avilés and Vicente J. León-Muñoz; Writing – review & editing, José Hurtado-Avilés and Vicente J. León-Muñoz.
Funding
This research received no external funding.
Institutional Review Board Statement
Our study was exempted from the requirement for ethical approval and adhered to the World Medical Association Declaration of Helsinki’s ethical standards, as revised in 2013.
Informed Consent Statement
Patient consent was waived due to the complete and irreversible anonymisation of the images (the study was exempted from the requirement for ethical approval).
Acknowledgments
We thank Dr. Rafael Leal Adán (Instituto Radiológico del Sureste, Murcia, Spain) for providing the copies of the X-rays used for this research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Perdriolle, R.; Vidal, J. Morphology of scoliosis: three-dimensional evolution. Orthopedics 1987, 10, 909–915. [CrossRef]
- Chung, N.; Cheng, Y.-H.; Po, H.-L.; Ng, W.-K.; Cheung, K.-C.; Yung, H.-Y.; Lai, Y.-M. Spinal phantom comparability study of Cobb angle measurement of scoliosis using digital radiographic imaging. J. Orthop. Transl. 2018, 15, 81–90. [CrossRef]
- Ma, Q.; Lin, H.; Wang, L.; Zhao, L.; Chen, M.; Wang, S.; Rao, Z.; Luo, Y. Correlation between spinal coronal balance and static baropodometry in children with adolescent idiopathic scoliosis. Gait Posture 2020, 75, 93–97. [CrossRef]
- Nelson, S.; Sanders, J.O. Available online: https://educationresources.srs.org/adolescent-idiopathic-scoliosis/idiopathic-scoliosis.
- Kuznia, A.L.; Hernandez, A.K.; Lee, L.U. Adolescent Idiopathic Scoliosis: Common Questions and Answers. Am. Fam. Physician 2020, 101, 19–23.
- Théroux, J.; Stomski, N.; Hodgetts, C.J.; Ballard, A.; Khadra, C.; Le May, S.; Labelle, H. Prevalence of low back pain in adolescents with idiopathic scoliosis: a systematic review. Chiropr. Man. Therap. 2017, 25, 10. [CrossRef]
- Yaszay, B.; Bastrom, T.P.; Bartley, C.E.; Parent, S.; Newton, P.O. The effects of the three-dimensional deformity of adolescent idiopathic scoliosis on pulmonary function. Eur. spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2017, 26, 1658–1664. [CrossRef]
- Wong, A.Y.L.; Samartzis, D.; Cheung, P.W.H.; Cheung, J.P.Y. How Common Is Back Pain and What Biopsychosocial Factors Are Associated With Back Pain in Patients With Adolescent Idiopathic Scoliosis? Clin. Orthop. Relat. Res. 2019, 477, 676–686. [CrossRef]
- Teles, A.R.; St-Georges, M.; Abduljabbar, F.; Simões, L.; Jiang, F.; Saran, N.; Ouellet, J.A.; Ferland, C.E. Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. Eur. spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2020, 29, 1959–1971. [CrossRef]
- Kuklo, T.R.; Potter, B.K.; Lenke, L.G. Vertebral rotation and thoracic torsion in adolescent idiopathic scoliosis: what is the best radiographic correlate? J. Spinal Disord. Tech. 2005, 18, 139–147. [CrossRef]
- Carlson, B.B.; Burton, D.C.; Asher, M.A. Comparison of trunk and spine deformity in adolescent idiopathic scoliosis. Scoliosis 2013, 8, 2. [CrossRef]
- Amzallag-Bellenger, E.; Uyttenhove, F.; Nectoux, E.; Moraux, A.; Bigot, J.; Herbaux, B.; Boutry, N. Idiopathic scoliosis in children and adolescents: assessment with a biplanar X-ray device. Insights Imaging 2014, 5, 571–583. [CrossRef]
- Mohanty, S.P.; Pai Kanhangad, M.; Gullia, A. Curve severity and apical vertebral rotation and their association with curve flexibility in adolescent idiopathic scoliosis. Musculoskelet. Surg. 2021, 105, 303–308. [CrossRef]
- San Román Gaitero, A.; Shoykhet, A.; Spyrou, I.; Stoorvogel, M.; Vermeer, L.; Schlösser, T.P.C. Imaging Methods to Quantify the Chest and Trunk Deformation in Adolescent Idiopathic Scoliosis: A Literature Review. Healthc. (Basel, Switzerland) 2023, 11. [CrossRef]
- Lenke, L.G.; Edwards, C.C. 2nd; Bridwell, K.H. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila. Pa. 1976). 2003, 28, S199-207. [CrossRef]
- Pesenti, S.; Clément, J.-L.; Ilharreborde, B.; Morin, C.; Charles, Y.P.; Parent, H.F.; Violas, P.; Szadkowski, M.; Boissière, L.; Jouve, J.-L.; et al. Comparison of four correction techniques for posterior spinal fusion in adolescent idiopathic scoliosis. Eur. spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2022, 31, 1028–1035. [CrossRef]
- Vatkar, A.; Najjar, E.; Patel, M.; Quraishi, N.A. Vertebral body tethering in adolescent idiopathic scoliosis with more than 2 years of follow-up- systematic review and meta-analysis. Eur. spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2023, 32, 3047–3057. [CrossRef]
- Smith, J.S.; Lafage, V.; Shaffrey, C.I.; Schwab, F.; Lafage, R.; Hostin, R.; OʼBrien, M.; Boachie-Adjei, O.; Akbarnia, B.A.; Mundis, G.M.; et al. Outcomes of Operative and Nonoperative Treatment for Adult Spinal Deformity: A Prospective, Multicenter, Propensity-Matched Cohort Assessment With Minimum 2-Year Follow-up. Neurosurgery 2016, 78, 851–861. [CrossRef]
- Quarto, E.; Zanirato, A.; Ursino, C.; Traverso, G.; Russo, A.; Formica, M. Adult spinal deformity surgery: posterior three-column osteotomies vs anterior lordotic cages with posterior fusion. Complications, clinical and radiological results. A systematic review of the literature. Eur. spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2021, 30, 3150–3161. [CrossRef]
- Ylikoski, M.; Tallroth, K. Measurement variations in scoliotic angle, vertebral rotation, vertebral body height, and intervertebral disc space height. J. Spinal Disord. 1990, 3, 387–391.
- Dang, N.R.; Moreau, M.J.; Hill, D.L.; Mahood, J.K.; Raso, J. Intra-observer reproducibility and interobserver reliability of the radiographic parameters in the Spinal Deformity Study Group’s AIS Radiographic Measurement Manual. Spine (Phila. Pa. 1976). 2005, 30, 1064–1069. [CrossRef]
- Srinivasalu, S.; Modi, H.N.; SMehta, S.; Suh, S.-W.; Chen, T.; Murun, T. Cobb Angle Measurement of Scoliosis Using Computer Measurement of Digitally Acquired Radiographs-Intraobserver and Interobserver Variability. Asian Spine J. 2008, 2, 90. [CrossRef]
- Thalengala, A.; Bhat, S.N.; Anitha, H. Computerized image understanding system for reliable estimation of spinal curvature in idiopathic scoliosis. Sci. Rep. 2021, 11, 7144. [CrossRef]
- Oda, M.; Rauh, S.; Gregory, P.B.; Silverman, F.N.; Bleck, E.E. The significance of roentgenographic measurement in scoliosis. J. Pediatr. Orthop. 1982, 2, 378–382. [CrossRef]
- Morrissy, R.T.; Goldsmith, G.S.; Hall, E.C.; Kehl, D.; Cowie, G.H. Measurement of the Cobb angle on radiographs of patients who have scoliosis. Evaluation of intrinsic error. J. Bone Joint Surg. Am. 1990, 72, 320–327.
- Gstoettner, M.; Sekyra, K.; Walochnik, N.; Winter, P.; Wachter, R.; Bach, C.M. Inter- and intraobserver reliability assessment of the Cobb angle: manual versus digital measurement tools. Eur. Spine J. 2007, 16, 1587–1592. [CrossRef]
- Wills, B.P.D.; Auerbach, J.D.; Zhu, X.; Caird, M.S.; Horn, B.D.; Flynn, J.M.; Drummond, D.S.; Dormans, J.P.; Ecker, M.L. Comparison of Cobb angle measurement of scoliosis radiographs with preselected end vertebrae: traditional versus digital acquisition. Spine (Phila. Pa. 1976). 2007, 32, 98–105. [CrossRef]
- Carman, D.L.; Browne, R.H.; Birch, J.G. Measurement of scoliosis and kyphosis radiographs. Intraobserver and interobserver variation. J. Bone Joint Surg. Am. 1990, 72, 328–333.
- Shea, K.G.; Stevens, P.M.; Nelson, M.; Smith, J.T.; Masters, K.S.; Yandow, S. A comparison of manual versus computer-assisted radiographic measurement. Intraobserver measurement variability for Cobb angles. Spine (Phila. Pa. 1976). 1998, 23, 551–555. [CrossRef]
- Hurtado-Avilés, J.; Santonja-Medina, F.; León-Muñoz, V.J.; Sainz de Baranda, P.; Collazo-Diéguez, M.; Cabañero-Castillo, M.; Ponce-Garrido, A.B.; Fuentes-Santos, V.E.; Santonja-Renedo, F.; González-Ballester, M.; et al. Validity and Absolute Reliability of the Cobb Angle in Idiopathic Scoliosis with TraumaMeter Software. Int. J. Environ. Res. Public Health 2022, 19. [CrossRef]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [CrossRef]
- Hopkins, W.G. Measures of Reliability in Sports Medicine and Science. Sport. Med. 2000, 30, 1–15. [CrossRef]
- Atkinson, G.; Nevill, A.M. Selected issues in the design and analysis of sport performance research. J. Sports Sci. 2001, 19, 811–827. [CrossRef]
- Marks, M.C.; Bastrom, T.P.; Petcharaporn, M.; Shah, S.A.; Betz, R.R.; Samdani, A.; Lonner, B.; Miyanji, F.; Newton, P.O. The Effect of Time and Fusion Length on Motion of the Unfused Lumbar Segments in Adolescent Idiopathic Scoliosis. Spine Deform. 2015, 3, 549–553. [CrossRef]
- Parsch, D.; Gaertner, V.; Brocai, D.R.; Carstens, C. The effect of spinal fusion on the long-term outcome of idiopathic scoliosis. A case-control study. J. Bone Joint Surg. Br. 2001, 83, 1133–1136. [CrossRef]
- Helenius, L.; Diarbakerli, E.; Grauers, A.; Lastikka, M.; Oksanen, H.; Pajulo, O.; Löyttyniemi, E.; Manner, T.; Gerdhem, P.; Helenius, I. Back Pain and Quality of Life After Surgical Treatment for Adolescent Idiopathic Scoliosis at 5-Year Follow-up: Comparison with Healthy Controls and Patients with Untreated Idiopathic Scoliosis. J. Bone Joint Surg. Am. 2019, 101, 1460–1466. [CrossRef]
- Baghdadi, S.; Baldwin, K. Selection of Fusion Levels in Adolescent Idiopathic Scoliosis. Curr. Rev. Musculoskelet. Med. 2024, 17, 23–36. [CrossRef]
- Pruijs, J.E.; Hageman, M.A.; Keessen, W.; van der Meer, R.; van Wieringen, J.C. Variation in Cobb angle measurements in scoliosis. Skeletal Radiol. 1994, 23, 517–520. [CrossRef]
- Cheung, J.; Wever, D.J.; Veldhuizen, A.G.; Klein, J.P.; Verdonck, B.; Nijlunsing, R.; Cool, J.C.; Van Horn, J.R. The reliability of quantitative analysis on digital images of the scoliotic spine. Eur. Spine J. 2002, 11, 535–542. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).