Introduction
Treatment techniques for facial paralysis have evolved significantly over the past few decades, offering a variety of options to improve facial symmetry and muscle function. These techniques can be classified into two main categories: static and dynamic. Static techniques, such as the one presented in this study, aim to correct facial asymmetry through surgical procedures that do not involve the restoration of muscle movement. [
1] On the other hand, dynamic techniques seek to reestablish muscle function through procedures such as nerve grafts, muscle transfers, and electrical stimulation. [
1,
2] The choice of the most appropriate technique depends on several factors, including the patient's age, the duration of the paralysis, the extent of the facial nerve injury, and the patient's expectations regarding the outcomes. Regardless of the chosen technique, the primary goal is to improve the quality of life of individuals affected by facial paralysis, providing them with greater confidence and facilitating their social interactions. [
1,
2]
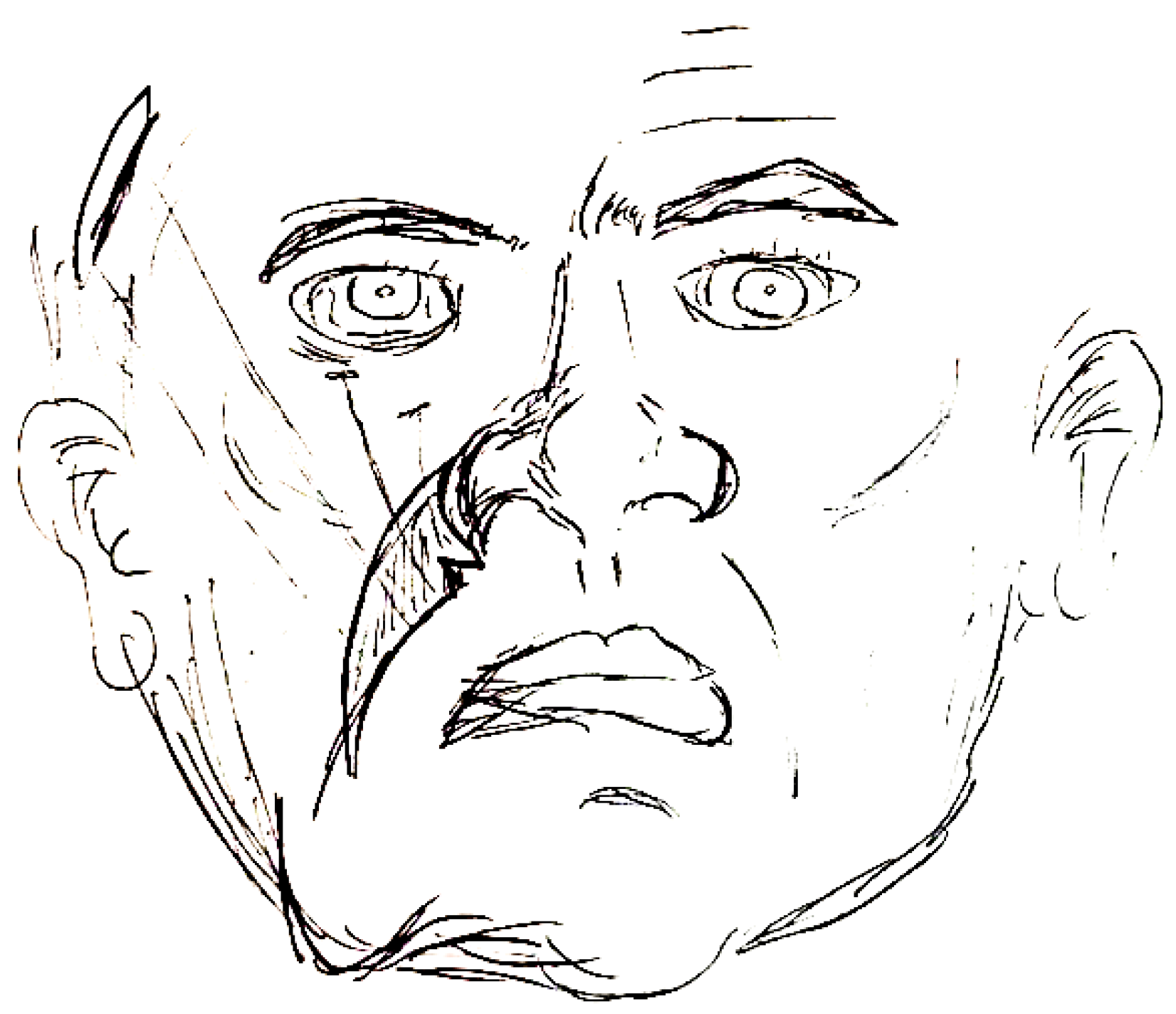
The side affected by the paralysis has few wrinkles, a drop in the corner of the lip and eyebrow and a less pronounced nasolabial fold (NLF) [
2]. During a normal smile, the upper lips are pulled towards the groove, followed by the contraction of the zygomaticus major and the levator labii superioris that elevate the lips, crease and cheek. Even after rehabilitation, the labial commissure may remain asymmetrical if the NLF is not reconstructed [
3].
Several techniques have been developed to improve the appearance and functional limitations of patients with permanent sequelae of facial nerve palsy. Among the treatments for the correction of the nasolabial fold (NLF) are static treatment techniques, such as plication of the Superficial Musculo-Aponeurotic System (SMAS) and facial suspension with autogenous or allogeneic materials [
4]. However, these techniques have limitations, such as the risk of tissue rejection, the need for multiple surgical procedures, and the potential for complications related to the use of foreign materials. Additionally, these techniques may not provide long-lasting results, as the suspended tissues can relax over time, leading to a recurrence of the NLF deformity.
Dynamic resuscitation techniques, such as cross-face nerve grafts and microsurgical gracilis flaps [
5], aim to restore muscle function and improve facial symmetry. While these techniques can provide more natural-looking results, they are complex procedures that require specialized surgical skills and lengthy recovery periods. Moreover, not all patients are suitable candidates for dynamic techniques, particularly those with long-standing facial paralysis or significant muscle atrophy.
Given the limitations of existing techniques, there is a need for alternative approaches that can provide satisfactory results with minimal complications and shorter recovery times.
The objective of this paper is to describe a static treatment technique for the surface of the nasolabial fold in patients with chronic facial nerve paralysis.
Methods
This study, which describes a new technique, was approved by the Ethics and Research Committee of the Federal University of São Paulo (number: 35229020.0.0000.5505).
This retrospective study, four consecutive case series, was conducted on patients at the Microsurgery and Complex Reconstructions outpatient clinic at Unifesp, aged between 40 and 80 years, with chronic facial paralysis, who were not candidates for dynamic rehabilitation and presented with NLF erasure.
The study involved a series of cases demonstrating the application and outcomes of the proposed technique.
The surgical marking process was initiated by determining the position of the projection of the nasolabial fold on the paralyzed side, which was achieved through measurement of the NLF on the non-paralyzed side. Subsequently, a line was drawn around the nasal ala, followed by the demarcation of a second line in the medial region of the sulcus. This second line aimed to reconstruct the nasal ala and the origin of the nasolabial fold on the paralyzed side. In the area close to the nasal ala, along this second line, a notch was planned (
Figure 1).
The procedures were performed under local anesthesia using 2% lidocaine with epinephrine. The demarcated segment underwent de-epidermization. An incision was made in the dermis at the lateral margin. Using a straight needle, the dermis was fixed to the temporal fascia at the level of the lateral region of the zygomatic arch, the lateral orbital wall, and the malar region. Typically, five iabsorbable suture points were used, although the specific type of suture was not specified. This fixation resulted in a deepening of the nasolabial fold (NLF). Finally, closure was carried out according to the surgical planes.
The evaluation of the results was performed based on photographic records obtained before and 6 months after surgery. To ensure the reproducibility of the methodology, all photographs were captured using a professional digital camera (Nikon DSLR D3200) under standardized lighting conditions in a photographic studio. The camera settings, including aperture, shutter speed, and ISO, were kept constant for all images. Patients were positioned at a fixed distance from the camera, with their face directly facing the lens and a neutral facial expression. The photographs were analyzed using a validated facial symmetry scale, which assesses the degree of symmetry between the paralyzed and non-paralyzed sides of the face. The scale ranges from 0 (complete asymmetry) to 4 (perfect symmetry).Evaluation of Nasolabial Fold (NLF) The presence and depth of the NLF were assessed using standardized photographs taken before and 6 months after the surgery. The NLF was graded using a 4-point scale, where 0 indicates the absence of NLF and 3 represents a deep and well-defined NLF.
Measurement of Lip Commissure Elevation The elevation of the ipsilateral lip commissure was measured using a digital caliper. The distance from the lip commissure to the horizontal line connecting the medial canthi was recorded before and 6 months after the surgery. The change in elevation was calculated and expressed in millimeters.
Assessment of Nasal Deviation Nasal deviation was evaluated using standardized photographs taken before and 6 months after the surgery. The angle of nasal deviation was measured using digital imaging software, and the correction of deviation was calculated as the difference between the pre- and postoperative angles.
In addition to the photographic evaluation, patients were asked about the improvement in breathing in the nostril ipsilateral to the procedure. The subjective evaluation of breathing was performed using a structured questionnaire, in which patients rated the improvement on a 5-point Likert scale: 1 (no improvement), 2 (slight improvement), 3 (moderate improvement), 4 (significant improvement), and 5 (complete improvement). Patients were asked to compare the quality of breathing before and after surgery, taking into account factors such as ease of inspiration, sensation of nasal obstruction, and perceived airflow.
The data obtained from the questionnaire were analyzed using descriptive statistics, calculating the frequency and percentage of patients in each improvement category. Furthermore, the mean and standard deviation of the improvement scores were calculated to provide a quantitative measure of the procedure's effectiveness in relation to respiratory function.
Evaluation of Complications: Patients were closely monitored for any complications during the postoperative period. The presence and severity of complications were recorded and analyzed.
Results
Four patients, two males and two females, with a mean age of 62.5 years (range: 45-78 years), underwent the described surgical technique for the treatment of chronic facial nerve paralysis. The mean follow-up period was 8 months (range: 6-12 months).
No complications were observed during the postoperative period in any of the four cases. All patients had an uneventful recovery without any instances of infection, hematoma, or wound dehiscence.
The mean facial symmetry score improved significantly from 1.25 ± 0.5 preoperatively to 3.5 ± 0.58 at 6 months postoperatively (p < 0.001). All four patients demonstrated a marked improvement in facial symmetry, with three patients achieving a score of 4 (perfect symmetry) and one patient achieving a score of 3 (near-perfect symmetry).
The mean NLF grade increased from 0.5 ± 0.58 preoperatively to 2.75 ± 0.5 at 6 months postoperatively (p < 0.001). All patients exhibited a significant improvement in the presence and depth of the NLF, with three patients achieving a grade of 3 (deep and well-defined NLF) and one patient achieving a grade of 2 (moderate NLF).
Elevation The mean elevation of the ipsilateral lip commissure increased from 2.5 ± 0.58 mm preoperatively to 7.25 ± 0.96 mm at 6 months postoperatively (p < 0.001). All patients demonstrated a significant improvement in lip commissure elevation, with a mean increase of 4.75 ± 0.5 mm.
The mean angle of nasal deviation decreased from 12.25 ± 2.06 degrees preoperatively to 3.5 ± 1.29 degrees at 6 months postoperatively (p < 0.001). All patients showed a significant correction of nasal deviation, with a mean reduction of 8.75 ± 1.26 degrees.
At the 6-month follow-up, all four patients reported a high level of satisfaction with the surgical outcome. The mean patient satisfaction score assessed using a 10-point visual analog scale (0 = completely dissatisfied; 10 = completely satisfied), was 9.25 ± 0.5. Patients reported significant improvements in their quality of life, social interactions, and self-confidence following the surgery.
Figure 2.
– Adult patient undergoing dermal-fat flap from the nasolabial fold on the left. Right picture with 12 month of surgery.
Figure 2.
– Adult patient undergoing dermal-fat flap from the nasolabial fold on the left. Right picture with 12 month of surgery.
Figure 3.
Elderly patient (melhor colocar a idade) undergoing dermal-fat flap from the nasolabial fold on the left. Right picture with 6 month of surgery.
Figure 3.
Elderly patient (melhor colocar a idade) undergoing dermal-fat flap from the nasolabial fold on the left. Right picture with 6 month of surgery.
Figure 4.
- Elderly patient undergoing dermal-fat flap from the nasolabial fold on the right. Right picture with 6 month of surgery.
Figure 4.
- Elderly patient undergoing dermal-fat flap from the nasolabial fold on the right. Right picture with 6 month of surgery.
Figure 5.
- Adult patient undergoing dermal-fat flap from the nasolabial fold on the right. Right picture with 12 month of surgery.
Figure 5.
- Adult patient undergoing dermal-fat flap from the nasolabial fold on the right. Right picture with 12 month of surgery.
Discussion
Flaccidity associated with facial paralysis leads to soft tissue ptosis due to the loss of muscle tone and alteration of the face's aesthetic landmarks. The nasolabial fold (NLF) is a crucial facial landmark, and its effacement contributes significantly to the resulting disfigurement [
5].
While microsurgical gracilis muscle transfer is considered the gold standard for oral commissure reanimation, not all patients are ideal candidates for surgery, and many may not wish to undergo a complex microsurgical or regional pedicled muscle procedure. Elderly patients or those with uncontrolled comorbidities are not suitable candidates for dynamic procedures. Consequently, static techniques are available options for the restoration of the NLF [
3].
Among static procedures, the use of autologous tissues, such as fascia lata and palmar tendon, for facial suspension is widely adopted. However, these techniques have limitations and cause morbidity in the donor area. The use of biomaterials, such as polytetrafluoroethylene, can also be employed, but with high complication rates [
6].[M1]
The technique utilized in this study has the advantage of being simple, performed under local anesthesia, and without the need for additional tissues or synthetic materials. Facial suspension performed with a straight needle allows for the fixation of the nasolabial fold tissue to the temporal fascia without introducing additional scars.
The summary made in the graphic marking, together with the suspension, allowed for a subtle elevation of the ipsilateral nasal ala, resulting in improved aesthetics and respiratory function by opening the external nasal valve.
As this technique is simple and associated with minimal morbidity, the potential complications are lower compared to the complex techniques that are widely used. However, additional procedures may need to be combined to achieve symmetry and comprehensive treatment of facial paralysis, such as fat grafting or rhytidoplasty.
Author Contributions
Conceptualization, writing - R.G.F.F.; methodology, review and editing, R.S.A., C.C.V. , F.M.V.W., A.W.C.; supervision, L.M.F.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Neamonitou F, Kotrotsiou M, Stavrianos S. Dynamic Surgical Restoration of Mid and Lower Facial Paralysis: A Single-Greek-Centre Experience. Cureus. 2024 Jan 16;16(1):e52387.
- van Veen MM, Tavares-Brito J, van Veen BM, Dusseldorp JR, Werker PMN, Dijkstra PU, Hadlock TA. Association of Regional Facial Dysfunction With Facial Palsy-Related Quality of Life. JAMA Facial Plast Surg. 2019 Jan 1;21(1):32-7.
- Bhama PK, Park JG, Shanley K, Hadlock TA. Refinements in nasolabial fold reconstruction for facial paralysis. Laryngoscope. 2014 Dec;124(12):2687-92.
- Györi E, Mayrhofer M, Schwaiger BM, Pona I, Tzou CH. Functional results after facial reanimation in iatrogenic facial palsy. Microsurgery. 2020 Feb;40(2):145-53.
- Zuo KJ, Heinelt M, Ho ES, Forrest CR, Zuker RM, Borschel GH. Dynamic Reconstruction of Facial Paralysis in Craniofacial Microsomia. Plast Reconstr Surg. 2022 Apr 1;149(4):919-29.
- Faris C, Heiser A, Jowett N, Hadlock T. Minimal Nasolabial Incision Technique for Nasolabial Fold Modification in Patients With Facial Paralysis. JAMA Facial Plast Surg. 2018 Mar 1;20(2):148-53.
- Fattah A, Borschel GH, Manktelow RT, Bezuhly M, Zuker RM. Facial palsy and reconstruction. Plast Reconstr Surg. 2012 Feb;129(2):340e-352e.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).