Submitted:
22 April 2024
Posted:
23 April 2024
You are already at the latest version
Abstract
Keywords:
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
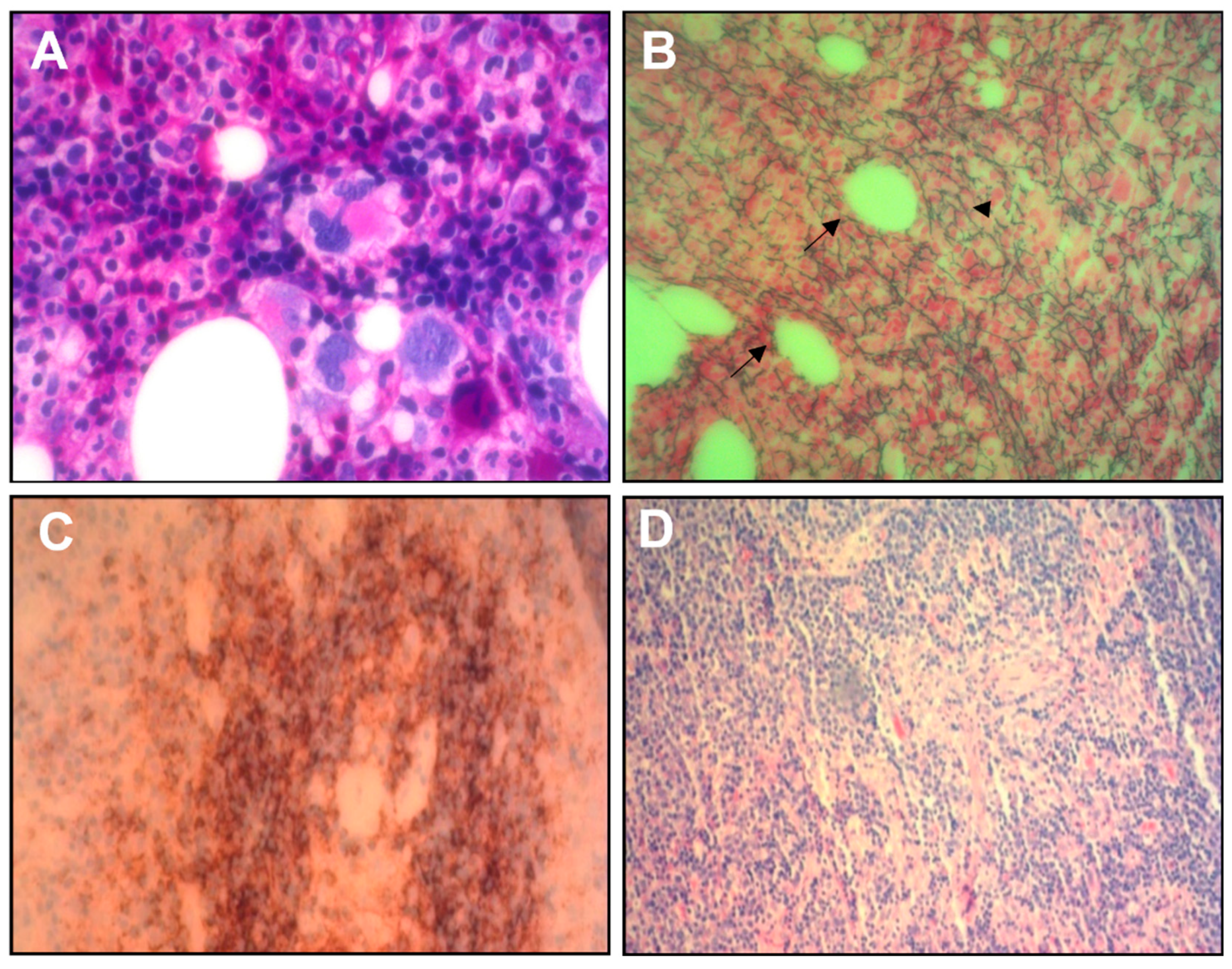
- Takai K, Nikkuni K, Shibuya H, Hashidate H. Thrombocytopenia with mild bone marrow fibrosis accompanied by fever, pleural effusion, ascites and hepatosplenomegaly. [Article in Japanese]. Rinsho Ketsueki 2010;51(5):320-5.
- Masaki Y, Kawabata H, Takai K, et al. Proposed diagnostic criteria, disease severity classification, and treatment strategy for TAFRO syndrome, 2015 version. Int J Hematol. 2016; 103:686–692. [CrossRef]
- Iwaki N, Fajgenbaum DC, Nabel CS, et al. Clinicopathologic analysis of TAFRO syndrome demonstrates a distinct subtype of HHV-8-negative multicentric Castleman disease. Am J Hematol. 2016;91(2):220–6. [CrossRef]
- Awano N, Inomata M, Sonoda Y, et al. A case of multicentric Castleman’s disease of mixed-type, which showed a constellation of symptoms, i.e., thrombocytopenia, anasarca, anemia, fever, myelofibrosis, and lymphadenopathy. J Clin Exp Hematol. 2013; 53:101–105.
- Coutier F, Meaux Ruault N, Crepin T, Bouiller K, Gil H, Humbert S, Bedgedjian I, Magy-Bertrand N. A comparison of TAFRO syndrome between Japanese and non-Japanese cases: a case report and literature review. Ann Hematol. 2018 Mar;97(3):401-407. [CrossRef]
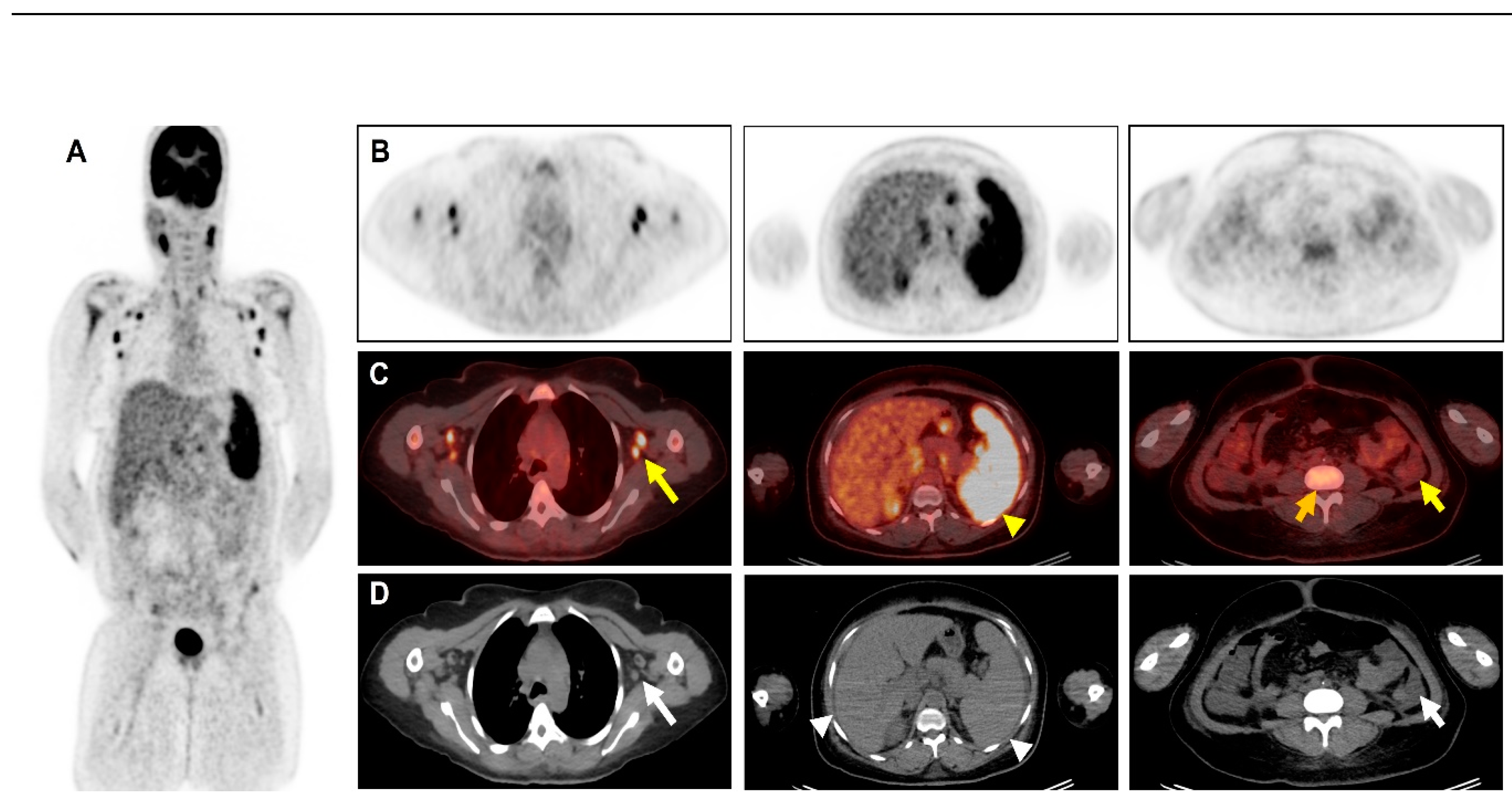
- Kiguchi T, Sato C, Takai K, et al. CT findings in 11 patients with TAFRO syndrome: a variant of multicentric Castleman’s disease. Clin Radiol. 2017; 72:905. e1–905.e5. [CrossRef]
- Burrell SC, Fischman AJ. Myelofibrosis on F-18 FDG PET Imaging. Clin Nucl Med. 2005; 30:674. [CrossRef]
- Derlin T, Alchalby H, Bannas P, et al. Serial 18F-FDG PET for monitoring treatment response after allogeneic stem cell transplantation for myelofibrosis. J Nucl Med. 2016; 57:1556–1559. [CrossRef]
- Han N, Sun X, Qin C, Hassan Bakari K, Wu Z, Zhang Y, Lan X. Value of 18F-FDG PET/CT Combined With Tumor Markers in the Evaluation of Ascites. AJR Am J Roentgenol. 2018 May;210(5):1155-1163. [CrossRef]
- Zhang M, Jiang X, Zhang M, Xu H, Zhai G, Li B. The role of 18F-FDG PET/CT in the evaluation of ascites of undetermined origin. J Nucl Med 2009; 50:506–512. [CrossRef]
- Han N, Sun X, Qin C, Hassan Bakari K, Wu Z, Zhang Y, et al. Value of 18F-FDG PET/CT combined with tumor markers in the evaluation of Ascites. American Journal of Roentgenology. 2018;210(5):1155–63. doi:10.2214/ajr.17.18733. [CrossRef]
- Fajgenbaum, David C. Novel insights and therapeutic approaches in idiopathic multicentric Castleman disease. Blood, (), blood-2018-05-848671).
- Behnia F, Elojeimy S, Matesan M, Fajgenbaum DC. Potential value of FDG pet-CT in diagnosis and follow-up of TAFRO syndrome - annals of hematology [Internet]. Springer Berlin Heidelberg; 2016.
- Hotta M, Minamimoto R, Yashima A, Nakano M, Yamashita H. FDG PET/CT findings in TAFRO syndrome. Clinical Nuclear Medicine. 2018. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




