Surgical Treatment
After the successful development of medical treatment of tuberculosis (Tb) in the 1950s, the use of surgery has decreased in many countries. Priority of the former Soviet Union (SU) in this field was claimed (Ots et al. 2009; Perelman 1998). The surgery of Tb has been performed not only in specialized centres but also in peripheral hospitals (Kucherov 1975; Bogush and Kalinichev 1979). This development was associated with the name of Mikhail Perelman, who criticized the Directly Observed Treatment, Short Course (DOTS) Program by the World Health Organization and endorsed the surgical treatment (Lichterman 2013).
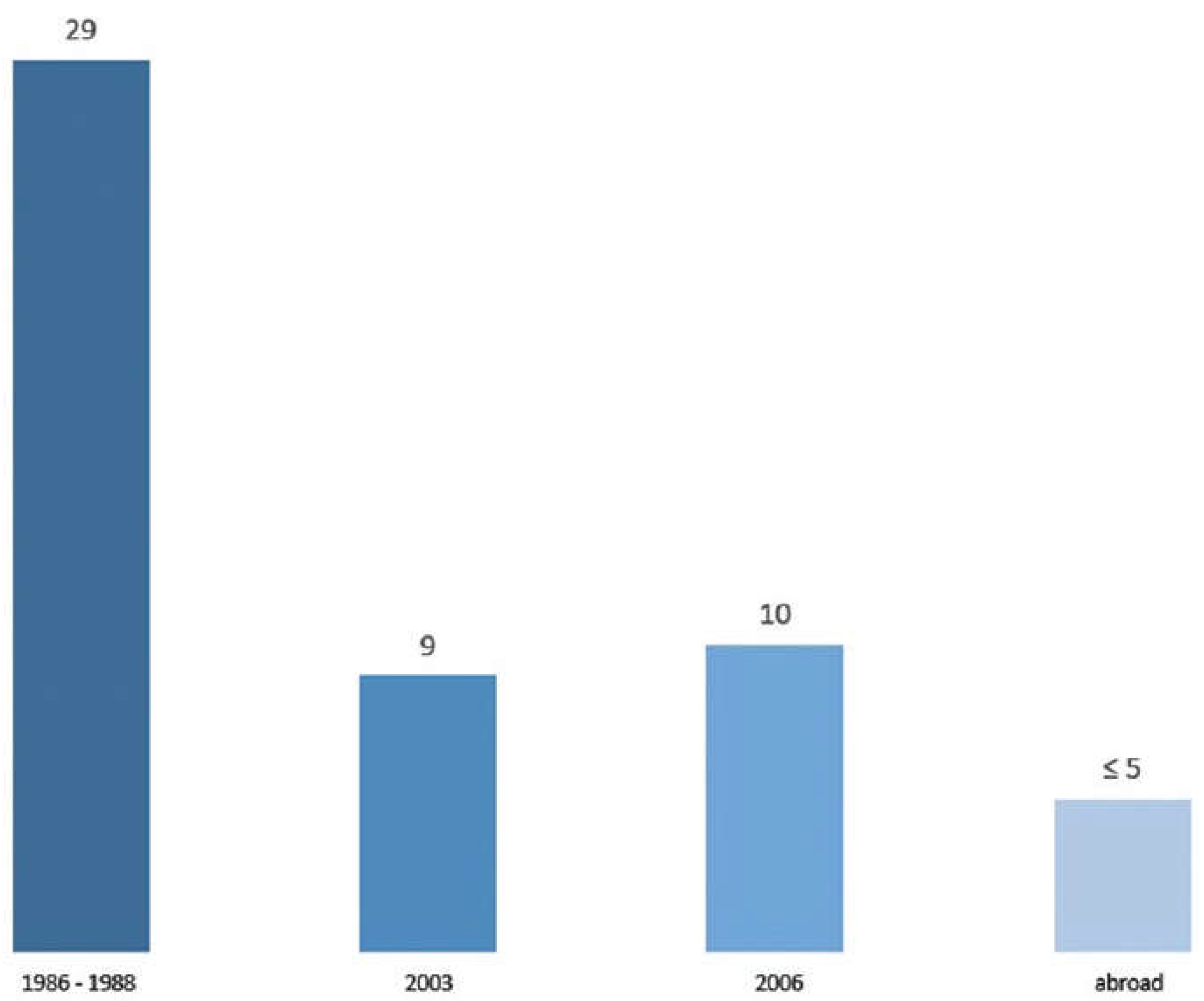
In the period 1973-1987, 285,000 patients with pulmonary Tb had been operated in the former SU, in 1987 - 26,000, while 85% of the surgeries were lung resections. In 1986-1988, ~17,500 operations for lung Tb were performed annually in the Russian Federation (RF) only in specialized institutions (Perelman 1998; Perelman et al. 1989). The incidence of Tb in 1986 and 1988 was, respectively, 43.8 and 40.8 per 100,000 (Nechaeva 2018). More than 29% of newly diagnosed Tb cases were operated at that time. By 2003, the quantity of surgeries decreased down to 10,479 (~9% of newly diagnosed cases), regarded to be insufficient (Shilova et al. 2005). In the foreign literature, corresponding figures are usually below 5% (Ahuja et al. 2012; Dewan and Pezzella 2016; Olcmen et al. 2006). The incidence of Tb in Russia increased from 34.0 in 1991 to 90.4 per 100,000 in the year 2000 (Nechaeva 2018). Similarly to other diseases (Leon et al. 1997; Jargin 2015), this drastic increase could have been partly explained by an underestimation during the Soviet period. In the year 2006, 12,286 operations were performed in RF for pulmonary Tb (
Figure 1), including 9300 (75.7%) resections and 399 (3.2%) pneumonectomies (Ots et al. 2009). According to another report, the forms of Tb most frequently treated by resections and pneumonectomies were cavitary Tb (52.2%) and tuberculoma (43.9%) (Kibrik and Bukharin 1976). For example, a series of 578 operations in 502 patients, including those with fibro-cavernous Tb (196 cases) and tuberculomas (161 cases), was reported, whereas the most frequent procedures were resection (280 cases) and pneumonectomy (80). The authors concluded that “indications for surgical management of pulmonary Tb should be generally expanded” (Perelman and Strelzov 1997). Tuberculoma was the form of Tb most often operated by Giller et al. (2013): 81 from 179 cases in one series. The video-assisted thoracoscopic surgery (VATS) is used increasingly these days (Smerdin et al. 2022).
Resections were recommended also for patients with inactive post-Tb fibrosis including oligosymptomatic cases (Kiseleva 1976). On the other hand, surgeries were performed in florid disseminated Tb (Meladze 1975). In some provinces of the Urals, Siberia and Volga regions, 25-40% of patients with destructive Tb were operated on (Priimak 1989). At the time of initial Tb diagnosis, surgery is currently considered to be indicated in 15-20% of patients (Borodulina et al. 2022; Kalechenkov and Elkin 2016; Perelman 1998). According to another paper, indications for surgery were found in 20-30% of patients at the time of diagnosis and/or in those with active Tb (Perelman et al. 2002). In Ekaterinburg and surrounding province (years 2006-2008), indications for surgery were found in 1784 from 4402 (40.5%) patients with pulmonary Tb, while 1079 (24.5%) were operated. Among reasons of the supposedly low surgery rate were the patients’ non-compliance and unavailability (Motus et al. 2009). According to the recent handbook, ~6.4% of Tb patients are operated in RF; but “in some provinces, which cooperated with the Perelman’s Institute… the percentage has been much higher” (Giller and Mishin 2020). Despite the lack of clinical trial data on efficacy of adjunctive surgical therapy of Tb, some countries of the former SU have continued performing many lung surgeries, predominantly resections (Benito et al. 2020; Giller et al. 2013; Kempker et al. 2012).
The recommendation to remove tuberculomas stems from Lev Bogush (Editorial 1975). Tuberculoma larger than 2 cm has been generally regarded as an indication for surgery, in adults as well as in children and adolescents (Giller et al. 2016; Giller and Mishin 2020). Tuberculomas >1 cm were often operated on (Gur’ianov et al. 2000; Pilipchuk et al. 1974; Uspenskii et al. 1986), which is contradicting to the international practice. It is widely agreed that potential instability of tuberculoma does not justify thoracic surgery and that asymptomatic patients with stable solid lesions do not require therapy. Nevertheless, tuberculoma was the most frequent indication for lung surgery in Tb patients (44.2%; in children - 40.7%) at the leading institution: Sechenov Medical University in Moscow (Ots et al. 2009; Martel 2016); while at some hospitals this percentage reached 50-80% (Valiev et al. 2014). Now as before, tuberculoma is among Tb forms that are most frequently operated on (Borodulina et al. 2022). The surgical treatment of tuberculoma was recommended also for cases with extensive lesions in remaining pulmonary tissues (Health Ministry 1983). Bilateral resections were performed for various forms of Tb including tuberculomas on both sides (Andrenko et al. 2000; Porkhanov et al. 1998; Repin 1990). A research from the Sechenov University reported 771 lung operations, including 168 pneumonectomies, 181 lobectomies, 180 other resections, performed in 700 Tb patients, up to 4 operations in one patient. Postoperative complications were recorded in 100 (12.9%) and lethal outcomes in 12 (1.5%) patients (Ots 2012). Another example from the same institution: among 60 operated Tb patients the complication rate was 37%, mortality - 5%; 18.3% of the patients were dehospitalized with persisting complications (Kulbak et al. 2004).
Out of 1,311 Tb cases operated at the Phthisiopulmonology Institute in St. Petersburg, 241 had Tb recurrences and 203 underwent repeated interventions (El’kin et al. 2004). Postoperative recurrences were regarded as indications for repeated surgeries up to concluding pneumonectomy (Repin 1990) and resections of the remaining sole lung (Korneevskii 1975). For example, repeated resections on both sides with a concluding pneumonectomy along with 52 bronchoscopies were performed in one case (Kravchenko et al. 2003). Bilateral lobectomies or pneumonectomy plus contralateral “sparing” resection were regarded to be indicated for patients with a Tb lesion on one side and non-specific inflammatory or fibrotic lesions in the contralateral lung (Niiazov 1976). Bilateral resections and bilobectomies were performed in different forms of Tb including tuberculomas (Andrenko et al. 2000; Korneevskii 1975; Niiazov 1976; Ots 1991; Porkhanov et al. 1998; Repin 1990). According to a recent monograph, among 420 patients operated for tuberculoma, bilateral operations were performed in 130 (31%) (Polyansky et al. 2021). Resections were regarded to be applicable also in cases with severe respiratory insufficiency (Bogush and Kalinichev 1979; Bogush et al. 1983; Korneevskii 1975; Naumov and Karaeva 1993).
Resections for Tb were performed by some experts without preceding attempt of medical treatment or within one month after the diagnosis, when medical therapy could have been efficient (Gur’ianov 2000; Zyskin 1991). One of the arguments in favour of the early surgery was non-compliance increasing with time (Gur’ianov et al. 2000) as the patients collected knowledge and advice. The frequency of adverse effects has probably been underestimated due to the limited follow-up. Lung operations were performed and recommended also for aged patients with comorbidities (Gorovenko et al. 1975; Polianskii 1999; Sokolov 1975, 1978). Sokolov (1975) found indications for surgery in 210 from 289 (72.6%) Tb patients 50-73 years old and operated 180 (62.2%) of them, 144 operations being lung resections. Among the latter 144 patients, 93 (66.4%) had cavitating disease and 43 (30.8%) tuberculoma. A post-surgery reactivation of Tb was recorded in 8.6% of the cases, fistula - in 27.2%, atelectasis - 20%, pneumonia - 5.7%, pleural empyema - 3.6%, other complications - 12.9%; 8 (5.7%) patients died after the operations. In the monograph based on 233 lung resections in Tb patients older than 50 years (mortality - 5.4%), Gorovenko et al. (1975) reasonably concluded: “It is important that a surgery doesn’t provoke an unfavourable outcome.” According to another report, tuberculoma was the most common indication, and lobectomy - the most frequent operation in elderly Tb patients, whereas potential contagiosity was among arguments in favour of the surgical treatment (Sokolov 1978). Statements of this kind can be found also in recent papers e.g.: “Surgery in patients with tuberculomas is recommended to reduce their infectiousness” (Yablonskii et al. 2019). According to Giller et al. (2013), a reduction of Tb incidence and mortality can be achieved only by means of a “radical sanitation” of contagious patients also without destructive pulmonary lesions. Note that tuberculoma is usually not contagious. It seems to be evident that potential contagiosity does not justify a thoracic surgery. One more citation: “Active surgical sanitation of infectiously dangerous patients with pulmonary Tb contributes to the rapid improvement of epidemiological indicators” (Pekhtusov 2022). No mentions of informed consent have been found in this connection.
Pulmonary resections and pneumonectomies for Tb were performed also in the former GDR. Indications for surgery were more limited than discussed above, being evaluated after chemotherapy and stabilisation of the disease. Contralateral foci of the disease were considered to be contraindications. Mainly small case series were reported (Künstler and Koss 1961; Schwarz and Endres 1961; Simon 1961). Of note, amongst 502 surgical cases (81 pneumonectomies, 266 lobectomies, 155 segmental resections), there were only 3 tuberculomas (Müller 1965). In 1965, results of a study were published reporting a decline in the vital capacity of the lungs after resections (Anstett 1965). A tendency of a decrease in the frequency of resections for Tb was noticed (Müller 1965; Anstett 1968; Teschner 1998). Today, surgeries for pulmonary tuberculosis are highly selective (Pfannschmidt and Schönfeld 2017).
Bronchoscopy (Bs)
Bs has been applied in all forms of Tb in many institutions and research cohorts (Belenkii and Balon 1977; Bubochkin et al. 1989; Chernushenko et al. 1986; Kvasnitskii and Voloshchuk 1984; Lebedev et al. 1989; Spitsyna et al. 1984) also when Tb was suspected (Nikolaev et al. 1982); among others, in a diagnostic algorithm for suspected Tb with the sputum negative for Mycobacteria (Palamarchuk et al. 2015). Primary Tb was regarded as an indication for Bs in children (Isaeva 1994), although it is reportedly no more sensitive for the culture than gastric aspiration (Feinsilver and Fein 1995; McIntosh et al. 2004). Bs was used as a screening method for Tb in patients with general malaise, having both negative and “hyperergic” (high degree of hypersensitivity) tuberculin tests (Belenki 1962; Chelidze et al. 1982), or as a second step of screening for Tb in children (Aksenova et al. 2005). Endoscopic monitoring was applied in pulmonary Tb with non-specific bronchial lesions (Berzner et al. 1988; Filippov and Chernichenko 2014). In the recent handbook of paediatric pulmonology, “suspected Tb” is listed among indications for Bs (Blokhin 2021). Therapeutic Bs and bronchoscopic monitoring has been applied in Tb also with non-specific bronchial lesions (Berzner et al. 1988; Filippov and Chernichenko 2014; Chernekhovskaia et al. 2011). In destructive Tb, therapeutic Bs (1-2 weekly during 2-4 months) was recommended by the Health Ministry (1982). An example: 22,469 Bs were performed in 5195 patients from 1994 through 2013 (1123 Bs yearly on average), including 1766 (34%) patients older than 65 years, at a phthisiological hospital in Moscow (705-1225 beds at different times; 368 surgeries performed in 2013) (Svistunov and Svistunova 2015; Sobkin 2014). Of note, viruses can be transmitted at endoscopy (Saludes et al. 2013). Not surprisingly, the incidence of hepatitis B was found to be five times higher in Tb patients than in the general population of Russia (Kulakova et al. 2004). The enhanced frequency of viral hepatitis or of its markers in Tb patients including children was reported (Asratian et al. 1989). Indications for Bs are beyond the scope of this preprint. Outside the former SU, Bs has not been routinely performed in all Tb patients; references are in (Jargin 2021).
Surfactant Therapy
The surfactant (Sf) therapy of pulmonary diseases including Tb, acute respiratory distress syndrome (ARDS), pneumonia and other conditions (excluding newborn respiratory distress syndrome - NRDS), and Bs as the delivery method, have been discussed by Jargin (2021). Sf-BL from bovine lungs has been developed and registered in Russia. The manufacturing method is described in the patent by Rozenberg and Seiliev (2019), where it is stated that Sf-BL contains ~2% of protein. Endobronchial instillations of xenogeneic proteins may cause immune reactions. A more pronounced immune response can be expected in adults and children than in premature infants with NRDS. Apparently, exogenous Sf is useless if alveoli are filled with exudation, distorted by inflammation and/or fibrosis; the instillations would just add protein-containing substance to the bronchial contents. Reportedly, endobronchial instillations of porcine Sf enhanced eosinophilic inflammation in asthmatics (Erpenbeck et al. 2004). Nonetheless, St-BL was used in asthma, bronchitis, pneumonia, chronic obstructive pulmonary diseases and Tb; more details are in the review by Rozenberg (2019) and the patent by Rozenberg and Seiliev (2019). St-BL was also used in patients with COVID-19 (Bautin et al. 2020), where immune and inflammatory reactions might contribute to the “cytokine storm”. Bs was used as the delivery method of Sf preparations (Bautin et al. 2003, 2006, 2020; Granov et al. 2001; Rozenberg 2019; Tsybul'kin et al. 1999; Kozlov and Poptsov 2005a,b; Pochepen et al. 2011); with bronchial biopsies in the study by Lepekha (1995). Either inhalations or bronchoscopic instillations of Sf were used in Tb (Lepekha 1995; Lovacheva et al. 2006). Sf-BL was recommended by the Health Ministry (2009) for viral pneumonia referring to the manufacturer's Instruction, where the following is stated (shortened translation): Sf-BL can be used preventively in threatening ARDS in patients with chronic (including obstructive) lung disease ... The optimal method of the Sf delivery is instillation into individual segmental bronchi (
Figure 2 top) (Biosurf 2021). The following information is provided in regard to Tb: in patients without favourable effect from chemotherapy during 2-6 months, an additional 2-month course of Sf-BL inhalations resulted in disappearance of mycobacteria from sputum in 80% of cases, reduction or disappearance of infiltrative and focal lesions in 100% and closure of caverns in 70% of patients (
Figure 1 bottom) (Biosurf 2021). Physiologically this effect is hardly understandable.
Until recently, Oleg Rosenberg had been director of the manufacturing firm Biosurf. No conflicts of interest have been declared in his publications. Misquoting was found in his papers. Here follow several examples: “A number of studies have shown an improvement in oxygenation, a decrease in the time spent on mechanical ventilation and an increase in survival” (Rozenberg 2019). In the cited publications, the conclusions are different, for example: “This pilot study presents preliminary evidence that Sf might have therapeutic benefit for patients with ARDS” (Gregory et al. 1997). Furthermore: “… Sf-BL reduces mortality in adults with ARDS 3-4-fold” (Rozenberg 2019). There are no such statements in the cited source (Lachmann 1992). “Deficiency of pulmonary Sf or changes in its composition have been described not only in NRDS, but also in … pulmonary Tb and other diseases” (Rozenberg 2019). A Russian-language handbook by Erokhin et al. (2000) is cited, where tuberculosis is not mentioned on the indicated pages 167-181. Misquoting was found also in the patent by Rozenberg and Seiliev (2019): “… these data can serve as the basis for multicenter randomized clinical studies of the efficacy of CHF5633 for the treatment of ARDS.” In the cited publication by Sweet et al. (2017) ARDS is not mentioned. We checked some references in other articles by the same author: “Results of the phase II multicenter randomized clinical trials and pilot studies of the efficacy of natural Sf preparations in the treatment of ARDS showed a significant improvement in oxygenation, decreased mechanical ventilation time and decreased mortality” (Rozenberg 2014). One of the cited studies reported that the treatment of asthmatics with a porcine Sf preparation resulted in an enhancement of the eosinophilic inflammation after allergen challenge. The authors concluded that the treatment is not suitable to decrease the allergic response in bronchial asthma (Erpenbeck et al. 2004). In another cited publication, the effectiveness of St-therapy in asthmatic children was not confirmed (Oetomo et al. 1996). The references related to Tb in the article by Rozenberg (2014) are self-citations (Lovacheva et al. 2006; Zhemkov et al. 2013). The following quote is from the article by the Rozenberg (2014): “It is believed that disturbances in the pulmonary Sf system can be the cause of bronchial obstruction, mucosal edema and increased fluid secretion into the bronchial lumen.” The cited publication was not found; an article with a similar title contains no such statements but the following: “Although there is no direct proof that surfactant dysfunction in human asthma causes airway obstruction, the above-mentioned and published data from the literature support the concept that poor functioning surfactant contributes to the pathophysiological scenario in asthma” (Hohlfeld 2002). There are also other incorrect citations. As mentioned above, some papers from Russia have reported that inhalations of Sf improve the effectiveness of the anti-Tb therapy, significantly accelerating healing, dissolution of specific Tb infiltrations and closing of caverns, while Mycobacterium tuberculosis disappeared from sputum (Erokhin et al. 2002, 2013; Lovacheva et al. 2006; Zhemkov et al. 2013). No similar reports have been found in the international literature.
Compulsory Hospitalisation and Treatment
According to the governmental Regulation No. 378 of June 16, 2006, patients with contagious Tb are not permitted to reside in one flat with other people. The outpatient treatment of Tb, usual in other countries, is supposed to be hardly applicable in RF (Bogadel’nikova et al. 2000). As per the Federal Law No. 77 “Prevention of the Tb spread” of June 18, 2001 (amended 2013), “patients with contagious Tb, repeatedly violating the anti-epidemic regime, and those evading examinations for Tb or (emphasis added) the therapy, are hospitalized for obligatory examination and treatment.” It is specified by the same Law that the principle of informed consent is not applicable under these circumstances, and that Tb patients must undergo prescribed examination and therapy. The non-observance of this law may lead to a criminal persecution. A survey found more than 6000 legal proceedings in the period 2004-2008 whereas 3163 Tb patients were compulsorily hospitalized (Bogorodskaia et al. 2009). In one series, 463 judicial cases resulted in 421 court decisions to hospitalize Tb patients (Lomova et al. 2009). All claims of that kind from medical authorities are currently satisfied by courts in the Moscow region. The police are obliged to help at hospitalizations and to search evading individuals. The implementation of compulsory examinations and treatments of Tb patients is increasingly efficient these days. Reportedly, 100% of bacillus excretors in the Moscow region had been hospitalized since 2019 (Smerdin et al. 2022). Compulsory treatments are generally at variance with the international practice and regulations. According to The World Medical Association, neither the statutory exceptions to the principle of informed consent nor the conditions of required care allow legally binding measures against patients refusing a treatment or hospitalization (Bouvet and Le Gueut 2013). The consent for invasive procedures and chemotherapy is of particular importance in conditions where an overtreatment may occur. The author agrees to the viewpoint that informed consent is grounded in the principle of bodily integrity, thus being not obligatory for non-invasive procedures such as sputum samples collected through expectoration (Coleman et al. 2012). Excessively rigorous interpretations of the informed consent are potentially harmful as they put non-invasive tests into one ethical category with invasive manipulations potentially resulting in less responsible attitude to both.
The Comorbidity of Tuberculosis and Alcoholism
A particular ethical problem has been the overuse of surgery in Tb patients concomitantly diagnosed with an alcohol use disorder. According to official instructions, indications for surgery were broader in alcohol-dependent than in other Tb patients (Health Ministry 1987). In case of alcoholism, surgeries were recommended to be performed earlier, after a shorter period of medical therapy (Pilipchuk et al. 1974). Perelman et al. (1983) insisted on early surgery in Tb patients with alcohol dependence, and operated them also in the absence of demonstrable Tb infection (e.g. a series of 49 patients with tuberculoma plus 41 with cavernous Tb, whereas micobacteria were demonstrated in 55 cases). At the same time, it was noticed that alcoholics have more frequent post-surgery complications (Perelman et al. 1983). Bronchoscopy was applied in cases with bronchitis (Entin 1990), the latter being frequent among alcoholics in Russia due to smoking and the risk to sleep down at a cold place. Along with other complications, vocal cord injuries were observed after repeated bronchoscopies sometimes performed in conditions of insufficient procedural quality. It was noticed that vomiting triggered by apomorphine as aversive therapy of alcohol dependence provoked hemoptysis in patients with Tb (Entin 1990).
Rudoi et al. (1994) reported that ~60% patients of a “phthisio-narcological” institution for compulsory treatment broke out; over 50% of them were returned by the police. The duration of stay in such institutions was a year or longer (Entin 1990). The compulsory treatment has been endorsed by laws and regulations (Entin 1990; Grishko 1991). In 1974, chronic alcoholism was officially declared to be a ground for enforced treatments; the regulations were made stricter in 1985, making compulsory hospitalization and therapy of chronic alcoholics independent on their anti-social behaviour. This practice was found in the 1990s to be contradictory to human rights. Nonetheless, some writers recommended restoration and further expansion of the compulsory treatment system (Bogorodskaia et al. 2009). According to a survey, 62.6% of specialists in addiction medicine supported compulsory treatment of alcoholism (Mendelevich 2016). Enforced therapy of socially dangerous alcoholics is stipulated by Articles 97 and 98 of the Criminal Code of RF; besides, there is a legal mechanism enabling compulsory treatment of persons with alcohol use disorder in prisons (Maslennikova 2023).
Invasive procedures have been applied to alcoholics more often than to other patients. Intravenous infusions were recommended for patients with alcoholism including moderately severe withdrawal syndrome: 7-10 infusions daily, sometimes combined with intramuscular injections (Entin 1990; Gavrilenko 1989; Ivanets and Vinnikova 2011; Galankin et al. 2003; Health Ministry 1998; Krut’ko 1990; Makhov et al. 1996; Shabanov 2015; Nikitin 1990). The intravenous detoxification was regarded to be “indicated to nearly all alcohol-depended patients, especially to those with prolonged withdrawal syndrome” (Entin 1990), also in the absence of (severe) intoxication (Livanov et al. 2000). Recommendations of intravenous infusion therapy of alcohol intoxication and withdrawal syndrome with both crystalloid and colloid solutions can be found also in recent instructive publications (Abdullaev and Utkin 2018; Gromova and Torshin 2018; Vinnikova et al. 2018). Besides, various intramuscular injections were recommended: magnesium sulphate, sodium bromide and thiosulphate, subcutaneous infusions of saline and insufflations of oxygen (300-500 ml); Unithiol, Dimercaprol, cranio-cerebral hypothermia (1-1.5 hours); extracorporeal ultraviolet irradiation of blood, sorbent hemo- and lymphoperfusion etc. (Gavrilenko 1989; Health Ministry 1987; Livanov et al. 2000; Nikitin 1990; Garbusenko et al. 2013; Styagov and Timoshok 1991; Syropiatov et al. 2000). Among patients with alcoholism, biopsies were taken with questionable indications (also for research) from kidneys, pancreas, liver, lung, salivary glands, stomach and skin, repeatedly in some cases (Lebedev et al. 1984; Serov and Lebedev 1988; Tarasova and Beloborodova 2003). Celiacography, endoscopic cholangiopancreatography and other invasive procedures were applied in alcoholics without clear indications by Makhov et al. (1996).
Discussion and Conclusion
The mentioning of informed consent started in papers from Russia not long ago, for example, in a bronchoscopic study of paediatric asthma, where consent of parents was sufficient (Fedorov et al. 2005). Of note, the principle of informed consent or assent is applicable to some extent also to adolescents and children. It has been recommended in the recent monograph titled “Pulmonary tuberculoma” to “explain to the patients in popular form that surgery is necessary” (Polyansky et al. 2021) instead of objective depiction of pros and cons. Justifications of surgical hyper-radicalism could be heard in private conversations among medics, for example: “The hopelessly ill are dangerous” i.e. may commit reckless acts undesirable by the state. For example, glioblastoma patients were routinely operated on, while it was believed by some staff that the treatment was generally useless, just forcing many patients to spend the rest of their lives in bed (Jargin 2024). The training of medical personnel under the imperative of readiness for war has been another motive. Some surgical and other invasive methods with questionable indications were advocated by first generation military surgeons. The Soviet period brought about an expansion of admission numbers to universities and medical educational institutions, sometimes with little regard for the quality of the academic preparation (Isakov 1980; Jargin 2013). At the same time, medical faculties were separated from universities; and medical science was partly separated from the mainstream scientific thought (Burger et al. 2004). Furthermore, among factors contributing to the use of invasive procedures with questionable indications has been the partial isolation from international scientific community, insufficient consideration of the principles of professional autonomy and scientific polemics, as well as paternalistic attitude to patients. Ethical and legal basis of medical practice and research has not been sufficiently known and observed in Russia. The term “deontology” is often used for medical ethics in this country. Textbooks and monographs on deontology explained the matter somewhat vaguely, with truisms and generalities but not much practical guidance. Insufficient coordination of medical studies and partial isolation from the international community can result in parallelism in research, unnecessary experimentation, and application of invasive procedures without sufficient indications (Jargin 2020). All said, the role of surgery in Tb remains controversial. The message of this preprint is that patients should not undergo operations to comply with doctrines. Evidence-based clinical indications must be determined individually, the patients being objectively informed on potential benefits and risks.
References
- Abdullaev TYu, Utkin SI. Different approaches to infusion therapy in alcohol addicted patients. Voprosy Narkologii - Journal of Addiction Problems 2018; 8(168): 54-75.
- Ahuja SD, Ashkin D, Avendano M, Banerjee R, Bauer M, Bayona JN, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: An individual patient data metaanalysis of 9,153 patients. PLOS Med 2012; 9: e1001300.
- Aksenova VA, Rozinova NN, Mokhnachevskaia AI, Kravchenko AF. Detection of Tuberculosis in Children and Adolescents with Non-specific Pulmonary Pathology in Public Health Institutions. Moscow: I.M. Sechenov Medical Academy, 2005. (in Russian).
- Andrenko AA, Krasnov VA, Grishchenko NG. Surgical treatment of patients with advanced bilateral destructive pulmonary tuberculosis. Probl Tuberk 2000; (3): 32-35.
- Anstett F. Function tests before and after pulmonary surgery for tuberculosis Z Tuberk Erkr Thoraxorg 1965; 123: 5-11. [PubMed]
- Anstett F. Surgery of the lung and pleura Z Tuberk Erkr Thoraxorg 1968; 129: 53-93. [PubMed]
- Asratian AA, Danilina GA, Kozhevnikova LK, Marina-Fedorova RF, Zotova IO. Serologic markers of hepatitis B in patients at a tuberculosis hospital. Probl Tuberk 1989; (4): 36-38.
- Bautin AE, Khubulava GG, Fadeev AA, Rozenberg OA. The first experience with using a preparation of lung surfactant for prevention and treatment of the acute lung injury syndrome after operations on the heart and aorta. Vestn Khir Im I I Grek 2003; 162(2): 79-83. [PubMed]
- Bautin A, Khubulava G, Kozlov I, Poptzov V, Osovskikh V, Seiliev A, et al. Surfactant therapy for patients with ARDS after cardiac surgery J Liposome Res 2006; 16: 265-272.
- Bautin AE, Avdeev SN, Seyliev AA, Shvechkova MV, Merzhoeva ZM, Trushenko NV, et al. Inhalation surfactant therapy in the integrated treatment of severe COVID-19 pneumonia Tuberk Bolezn Legk 2020; 98(9): 6-12.
- Belen’ki MS (1962) Diagnosis of chronic tuberculosis intoxication on adults. Dissertation. Kharkov Medical Institute (in Russian).
- Belenkii MS, Balon NB. Diagnostic and therapeutic bronchoscopy under conditions of a district antituberculosis dispensary Probl Tuberk 1977; (4): 45-48.
- Benito P, Vashakidze S, Gogishvili S, Nikolaishvili K, Despuig A, Tukvadze N, et al. Impact of adjuvant therapeutic surgery on the health-related quality of life of pulmonary tuberculosis patients. ERJ Open Res 2020; 6: 1-11.
- Berzner AN, German AK, Kovalenbko BA, Kostrub LA, Li BP. Treatment effectiveness in intrathoracic tuberculosis in children and adolescents and the characteristics of the residual posttuberculosis changes Probl Tuberk 1988; (1): 32-34.
- Biosurf. Instruction for Medical Use of the preparation Surfactant-BL. Registration No. 003383/01-230710. Amendment PN003983/01-030221 of 03 February 2021 (the date hardly readable). Available from: https://biosurf.ru/doctor/.
- Blokhin BM. Childhood Pulmonology: National Manual. Moscow: Geotar-Media, 2021. (in Russian).
- Bogadel’nikova IV, Sagalovich VIa, Perelman MI. The efficacy of the ambulatory treatment of patients with newly detected pulmonary tuberculosis. Probl Tuberk 2000; (5): 23-28.
- Bogorodskaia EM, Ol’khovatskii EM, Borisov SE. Legal aspects of compulsory hospitalization of incompliant patients with tuberculosis. Probl Tuberk Bolezn Legk 2009; (4): 8-14.
- Bogush LK, Kalinichev GA. Korrigiruiushhie operacii pri rezekcii legkih (Corrective operations at lung resections). Tbilisi: Sabchota Sakartvelo, 1979.
- Bogush LK, Kariev TM, Eshankhanov M. Hirurgia tiazhelyh form tuberkuleza legkih (Surgery of Severe forms of Pulmonary Tuberculosis). Tashkent: Meditsina, 1983.
- Borodulina EA, Kolsanov AV, Rogozhkin PV. Hirurgicheskie vmeshatelstva v kompleksnom lechenii tuberkuleza legkih. Predoperacionnoe planirovanie s 3D-modelirovaniem (Surgical interventions in the complex treatment of pulmonary tuberculosis. Preoperative planning with 3D modeling). Moscow: INFRA-M, 2022.
- Bouvet R, Le Gueut M. Tuberculose et refus de soins: recours à la législation sur les menaces sanitaires graves. Rev Mal Respir 2013; 30: 451-457. [CrossRef] [PubMed]
- Bubochkin BP, Sobolev GS, Radchenko TN. The endoscopic bronchial picture of patients with pulmonary tuberculosis of various age groups Probl Tuberk 1989; (9): 19-22.
- Burger EJ, Ziganshina L, Ziganshin AU. Academic medicine in Russia. Croat Med J 2004; 45(6): 674-676. [PubMed]
- Chelidze AV, Chernousova TIa, Karpukhina NV, Khorosheva MN, Moiseenko LM. Bronchial status in children, adolescents and young people with elevated tuberculin sensitivity Probl Tuberk 1982; 9: 27-30.
- Chernekhovskaia NE, Andreev VG, Povaliaev AV. Therapeutic Bronchoscopy in the Complex Therapy of Respiratory Organs. Moscow: Medpress-Inform, 2011. (in Russian).
- Chernushenko EF, Shatrov VA, Belianovskaia TI, Kuznetsova LV, Shpak OI. The function of phagocytosing cells in pulmonary tuberculosis patients Probl Tuberk 1986; 1: 59-63.
- Coleman CH, Selgelid MJ, Reis A, Reichman LB, Jaramillo E. The role of informed consent in tuberculosis testing and screening. Eur Respir J 2012; 39: 1057-1059. [CrossRef] [PubMed]
- Dewan RK, Pezzella AT. Surgical aspects of pulmonary tuberculosis: An update. Asian Cardiovasc Thorac Ann 2016; 24: 835-846.
- Editorial. Lev Konstantinovich Bogush (on his 70th birthday). Khirurgiia (Mosk) 1975; (3): 143-144.
- El’kin AV, Repin IM, Levashev IN. Surgical treatment for postoperative recurrent pulmonary tuberculosis. Probl Tuberk Bolezn Legk 2004; (2): 28-32.
- Entin GM. Lechenie alkogolizma (Treatment of alcoholism). Moscow: Meditsina, 1990.
- Erokhin VV, Romanova LK, Erokhin VV, Romanova LK. Pulmonary surfactant system Pulmonary Cell Biology in the Norm and Pathology. Moscow: Meditsina, 2000; pp. 167-181 (in Russian).
- Erokhin VV, Lovacheva OV, Lepekha LN, Rozenberg OA, Seiliev AA, Volchkov VA. Pulmonary tuberculosis treatment method. Patent RU2195313C1 (2002).
- Erokhin VV, Lepekha LN, Erokhina MV, Lovacheva OV. The Surfactant System in Pulmonary Tuberculosis. 2013 Moscow: Central Tuberculosis Research Institute, 2013.
- Erpenbeck VJ, Hagenberg A, Dulkys Y, Elsner J, Bälder R, Krentel H, et al. Natural porcine surfactant augments airway inflammation after allergen challenge in patients with asthma Am J Respir Crit Care Med 2004; 169: 578-586.
- Fedorov IA, Wilson SJ, Davies DE, Holgate ST. Epithelial stress and structural remodelling in childhood asthma. Thorax 2005; 60: 389-394. [CrossRef]
- Feinsilver SH, Fein A. Textbook of Bronchoscopy. Baltimore: Williams & Wilkins, 1995.
- Filippov VP, Chernichenko NV. Bronchoscopy in Pulmonary Diseases Moscow: Binom, 2014.
- Galankin LN, Livanov GA, Guzikov BM, Volkov NIu. Method fordetermining treatment tactics in the cases of alcohol abstinence syndrome. Patent RU2202946C2 (2003).
- Garbusenko ON, Babashev BB, Salahanov RA. Ultraviolet irradiation of bloodin therapy of acute alcohol abstinence syndrome. Efferent Therapy 2013; 19(1): 98-99.
- Gavrilenko VS. Kompleksnoe lechenie bolnyh tuberkulezom legkih, stradaiushhih alkogolizmom (Combined treatment of patients with pulmonary tuberculosis suffering of alcoholism). Methodical Recommendations Moscow: Health Ministry of RSFSR, 1989.
- Giller DB, Mishin VI. Ftiziatriia (Phthisiology). Moscow: Geotar-Media, 2020.
- Giller DB, Bizhanov AB, Khasanshin GS, Trishina LV, Klestova AA. Treatment of the newly diagnosed destructive lung tuberculosis with elimination of bacilli. Khirurgiia (Mosk) 2013; (6): 83-87.
- Giller DB, Martel II, Baryshnikova LA. Hirurgia tuberkuleza u detei (Surgery of Tuberculosis in Children). Moscow: Aldi-Print, 2016.
- Gorovenko GG, Sokolov SB, Slepukha IM. Hirurgicheskoe lechenie zabolevanii legkih u bolnyh pozhilogo vozrasta (Surgical Treatment of Lung Diseases in Elderly Patients). Kiev: Zdorov’ia, 1975.
- Granov AM, Rozenberg OA, Tsybul'kin EK, Erokhin VV, Khubulava GG, Likhvantsev VV, et al. Critical state medicine. Surfactant therapy of adult respiratory distress syndrome (results of multicenter studies) Vestn Ross Akad Med Nauk 2001; (5): 34-38.
- Gregory TJ, Steinberg KP, Spragg R, Gadek JE, Hyers TM, Longmore WJ, et al. Bovine surfactant therapy for patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 1997; 155(4): 1309-1315. [CrossRef] [PubMed]
- Grishko AIa. Pravovye i kriminologicheskie problemy socialnoi reabilitacii hronicheskih alkogolikov i narkomanov (The institute of compulsory treatment and occupational re-education of chronic alcoholics and drug addicts, its social purpose). Moscow: Academy of the Ministry of Internal Affairs, 1991.
- Gromova OA, Torshin IYu. Magnii i "bolezni civilizacii" (Magnesium and diseases of civilization). Moscow: Geotar-Media; 2018.
- Gur’ianov VN, Strel’tsov VP, Al’ba MN. Early surgical treatment of new restrictive forms of pulmonary tuberculosis. Probl Tuberk 2000; (6): 48-51.
- Health Ministry of RSFSR. Methodical Recommendations Endobronchial Methods of Tuberculosis Treatment. Moscow, 1982.
- Health Ministry of Uzbek SSR. Ekonomnye i kombinirovannye rezekcii legkih pri rasprostranennyh formah tuberkuleza (Sparing and Combined Lung Resections in Extended Forms of Tuberculosis). Methodical Recommendations. Tashkent, 1983.
- Health Ministry of Ukrainian SSR. Osobennosti vyшavlenija, diagnostiki, klinicheskogo techenia, lechenia i profilaktiki tuberkuleza u bolnyh hronicheskim alkogolizmom (Special features of detection, diagnosis, clinical course, treatment and prevention of tuberculosis in patients with chronic alcoholism). Methodical Recommendations. Kiev, 1987.
- Health Ministry of Russian Federation. Standarty (modeli protokolov) diagnostiki i lechenia narkologicheskih bolnyh [Standards (models protocol) for diagnostics and treatment of substance addicts]. Annex to the Order No. 140; updated 1998 April 28. Available from: http://docs.cntd.ru/document/1200119087.
- Health Ministry of Russian Federation. Gripp A/H1N1 i vyzvannaia im pnevmonia u beremennyh. Etiotropnaia i respiratornaia terapia [A/H1N1 influenza and pneumonia in pregnant women induced by it]. Etiotropic and respiratory therapy. Signed by V.I. Skvortsova. Information Letter 24-5/10/2-9533 of November 28, 2009.
- Hohlfeld JM. The role of surfactant in asthma. Respir Res 2002; 3(1): 4. [CrossRef] [PubMed]
- Isaeva LA. Pediatrics. Moscow: Meditsina, 1994.
- Isakov IuF. Medical Institutes. In: Large Medical Encyclopedia. Moscow: Soviet Encyclopedia, 1980; 14: 421-427.
- Ivanets NN, Vinnikova MA. Alkogolizm (Alcoholism). Moscow: MIA, 2011.
- Jargin SV. Some aspects of medical education in Russia. Am J Med Stud 2013; 1(2): 4-7.
- Jargin SV. Cardiovascular mortality trends in Russia: Possible mechanisms. Nat Rev Cardiol 2015; 12: 740. [CrossRef] [PubMed]
- Jargin SV. Misconduct in medical research and practice. Series: Ethical Issues inthe 21st Century. New York: Nova Science Publishers, 2020.
- Jargin SV. Surgical and endoscopic treatment of pulmonary tuberculosis: A Report from Russia. Hamdan Medical Journal 2021; 14(4): 154-162. [CrossRef]
- Jargin SV. The treatment of glioblastoma: Letter from Russia. J Cancer Sci 2024; 9(1): 1.
- Kalechenkov MK, Elkin AV. Ekonomnye operacii pri tuberkuleze legkih (Sparing surgeries for pulmonary tuberculosis). St. Petersburg: Mechnikov North-Western Medical University, 2016.
- Kempker RR, Vashakidze S, Solomonia N, Dzidzikashvili N, Blumberg HM. Surgical treatment of drug-resistant tuberculosis. Lancet Infect Dis 2012; 12: 157-166. [CrossRef] [PubMed]
- Kibrik BS, Bukharin PA. Rehabilitation of patients following pulmonary resections for tuberculosis. Probl Tuberk 1976; (12): 43-47.
- Kiseleva IA. Clinical aspects and results of surgical treatment of metatuberculous changes of the lungs. Probl Tuberk 1976; (12): 31-35.
- Korneevskii MD. Dvustoronnie rezekcii legkih u bolnyh tuberkulezom (Bilateral lung resections in tuberculosis patients). In: Problemy legochnoi hirurgii. K 70-letiu prof. L.K. Bogush’a (Problems of the lung surgery (to the 70th anniversary of Prof. L.K. Bogush). Moscow: Central Institute of Tuberculosis, 1975; pp. 376-384.
- Kozlov IA, Poptsov VN. Combined therapy with nitric oxide and Surfactant-BL for acute respiratory distress syndrome after operations using extracorporeal circulation. Obshtshaia Reanimatologiia 2005a; (1): 15-19.
- Kozlov IA, Poptsov VN. Surfactant-BL and inhaled nitric oxide in acute respiratory distress syndrome in cardiac surgical patients Anesteziol Reanimatol 2005b; (6): 38-41.
- Kravchenko AF, Vinokurov II, Ivanov IuS, O-zhi-kho EA. A case of multiple operations in pulmonary tuberculosis. Probl Tuberk Bolezn Legk 2003; (5): 48-49.
- Krut’ko VS. Pneumonia in patients with pulmonary tuberculosis and alcoholism. Probl Tuberk 1990; (1): 64-66.
- Kucherov AL. Osnovnye etapy razvitia ftiziohirurgii v RSFSR (Main developmental steps of the phthisiatric surgery in the RSFSR). In: Problemy legochnoi hirurgii. K 70-letiu prof. L.K. Bogush’a (Problems of the lung surgery. To the 70th anniversary of Prof. L.K. Bogush). Moscow: Central Institute of Tuberculosis, 1975; pp. 93-99.
- Kulakova AV, Kokina NI, Kogan EA, Ablitsov YM, Pavlov CS, Zeliger LR, et al. Abstract 46. Peculiarities of therapy in patients with tuberculosis associated to viral hepatitis In: Abrosimov VN (ed). Abstract book. 3rd Congress of European region. International Union against Tuberculosis and Lung diseases (IUATLD). 14th National Congress of Lung diseases; 22-26 June 2004. Moscow, 2004; p. 16.
- Kulbak VA, Lakomkin MM, Martirosjan NL. Abstract 196. The peculiarities of the surgical treatment of drug resistant pulmonary tuberculosis. In: Abrosimov VN (ed). Abstract book. 3rd Congress of European region. International Union against Tuberculosis and Lung diseases (IUATLD). 14th National Congress of Lung diseases; 22-26 June 2004. Moscow, 2004; p. 55.
- Künstler S, Koss FH. Indication for resection in pulmonary tuberculosis in childhood and adolescence. Z Tuberk Erkr Thoraxorg 1961; 117: 71-92.
- Kvasnitskii BI, Voloshchuk EO. Frequency and nature of bronchial changes based on data from a provincial tuberculosis dispensary. Vrach Delo 1984; (4): 56-58.
- Lachmann B. Open up the lung and keep the lung open. Intensive Care Med 1992; 18: 319-321. [CrossRef] [PubMed]
- Lebedev KM, Filippov VP, Vasil'ev VIu, Bolotov PA. Use of carbon dioxide laser in the treatment of tuberculosis of the bronchi and trachea in children and adolescents Probl Tuberk 1989; (3): 30-33.
- Lebedev SP, Vinogradova LG, Sukhova GK. Alcoholic hyaline and interstitial filaments as markers of alcoholic damage of internal organs. Arkh Patol 1984; 46(11): 52-58. [PubMed]
- Leon DA, Chenet L, Shkolnikov VM, Zakharov S, Shapiro J, Rakhmanova G, et al. Huge variation in Russian mortality rates 1984-94: Artefact, alcohol, or what? Lancet 1997; 350: 383-388. [CrossRef] [PubMed]
- Lepekha LN. Pulmonary surfactant system in experimental tuberculous inflammation and evaluation of its morpho-functional condition in humans. Doctoral Dissertation. Moscow: Research Institute of Human Morphology, 1995.
- Lichterman B. Mikhail Izrailevich Perelman. BMJ 2013; 346: f3042. [CrossRef]
- Lomova LA, Kopylova IF, Smerdin SV, Chernov MT, Baeva LB, Saranchina SV. Compulsory hospitalization of non-compliant patients with tuberculosis. Tuberk Biolezni Legkih 2009; (7): 9-13.
- Lovacheva OV, Erokhin VV, Chernichenko NV, Evgushchenko GV, Lepekha LN, Rozenberg OA. Results of use of surfactant in complex therapy of patients with destructive pulmonary tuberculosis Probl Tuberk Bolezn Legk 2006; (10): 12-17.
- Makhov VM, Abdullin RG, Gitel' EL, Zavodnov VIa, Podzolkov VI, Sozinova TIu, et al. Visceral lesions in alcoholism. Ter Arkh 1996; 68(8): 53-56.
- Martel AI. Hirurgicheskoe lechenie tuberkuleza organov dyhania u detei i podrostkov (Surgical treatment of respiratory tuberculosis in children and adolescents). Doctoral thesis. Moscow: Sechenov Medical University, 2016.
- Maslennikova EA. Osobennost ispolneniia lisheniia svobody osuzhdennymi, bolnymi alkogolizmom (Peculiarities of execution of imprisonment by convicts with alcoholism). Ryazan: IP Konyakhin, 2023.
- McIntosh N, Helms PJ, Smyth RL. Forfar & Arneil’s Textbook of Pediatrics: 6th Edition. J R Soc Med 2004; 97: 96.
- Meladze GD. K voprosu rezekcii legkih pri rasprostranennom tuberkuleze (On the lung resection in extended tuberculosis). In: Problemy legochnoi hirurgii. K 70-letiu prof. L.K. Bogush’a (Problems of the lung surgery (to the 70th anniversary of Prof. L.K. Bogush). Moscow: Central Institute of Tuberculosis, 1975; pp. 406-410.
- Mendelevich VD. Etika sovremennoi narkologii (Ethics of modern narcology). Moscow: Gorodets, 2016.
- Motus IY, Skorniakov SN, Golubev DN, Karskanova SS, Malceva AS. Surgical treatment of pulmonary tuberculosis. Vestnik Ural'skoi Meditsinskoi Akademicheskoi Nauki (Journal of Ural Medical Academic Science) 2009; (3): 103-106. https://www.elibrary.ru/item.asp?id=12877524.
- Müller RW. On our past and present therapeutic methods in the treatment of tuberculosis Z Tuberk Erkr Thoraxorg 1965; 123: 64-67.
- Naumov VN, Karaeva GB. Surgical treatment of patients with disseminated and progressing pulmonary tuberculosis. Probl Tuberk 1993; (5): 23-26.
- Nechaeva OB. Tuberculosis situation in Russia. Tuberk Biolezni Legkih 2018; (8): 15-24. [CrossRef]
- Niiazov IB. Bilateral resection in patients with tuberculosis associated with nonspecific lung diseases. Probl Tuberk 1976; (12): 29-31.
- Nikitin IuP. Profilaktika i lechenie alkogolizma (Prevention and treatment of alcoholism). Kiev: Zdorov’ia, 1990.
- Nikolaev IS, Mishanov RF, Patsenker II. Early detection of tuberculosis and nontuberculous lung diseases Probl Tuberk 1982; (4): 31-34.
- Oetomo SB, Dorrepaal C, Bos H, Gerritsen J, van der Mark TW, Koëter GH, et al. Surfactant nebulization does not alter airflow obstruction and bronchial responsiveness to histamine in asthmatic children Am J Respir Crit Care Med 1996; 153: 1148-1152.
- Olcmen A, Gunluoglu MZ, Demir A, Akin H, Kara HV, Dincer SI. Role and outcome of surgery for pulmonary tuberculosis. Asian Cardiovasc Thorac Ann 2006; 14: 363-366. [CrossRef] [PubMed]
- Ots ON. Bilateral lung resections. Grud Serdechnososudistaia Khir 1991; (11): 35-38.
- Ots ON. The surgical treatment of pulmonary tuberculosis with the resistance of mycobacteria to drugs. Sechenov Medical Journal 2012; (2): 15-23. https://www.elibrary.ru/item.asp?id=21947449.
- Ots ON, Sinitsyn MV, Semenov GI, Latyshev AN, Agkatsev TV, Kessel' MM. Surgery for respiratory tuberculosis at the Research Institute of Phthisiopulmonology, I. M. Sechenov Moscow Medical Academy: History and current trends. Tuberk Biolezni Legkih 2009; (12): 11-21.
- Palamarchuk GF, Akopov AL, Arseniev AI, Derevianko AV, Nagornaya OA. Bronhoskopia v diagnostike i lechenii zabolevanii organov dyhania (Bronchoscopy in the diagnosis and treatment of respiratory diseases). St. Petersburg: Foliant, 2019.
- Pekhtusov VA. Vozmozhnosti hirurgicheskogo metoda v umenshenii rezervuara tuberkuleznoi infekcii v Tambovskoi oblasti (Possibilities of the surgical method in reducing the reservoir of tuberculosis infection in the Tambov province). Candidate thesis. Moscow: Central Research Institute of Tuberculosis, 2022.
- Perelman MI. Surgery of pulmonary tuberculosis. Probl Tuberk 1998; (3): 27-32. [CrossRef] [PubMed]
- Perelman MI, Strelzov VP. Surgery for pulmonary tuberculosis. World J Surg 1997; 21(5): 457-467. [CrossRef] [PubMed]
- Perelman MI, Safarov RN, Epshtein TV, Gorelik ES, Palei ME. Hirurgicheskoe lechenie bolnyh tuberkulezom legkih i hronicheskim alkogolizmom (Surgical treatment of patients with pulmonary tuberculosis and chronic alcoholism). In: Sovremennye metody hirurgicheskogo lechenia tuberkuleza legkih (Modern methods of surgical treatment of pulmonary tuberculosis). Collected works. Moscow: Institute of Tuberculosis; 1983; pp. 65-67.
- Perelman MI, Streltsov VP, Naumov VN. Klinicheskie i socialnye aspekty organoshhadiashhih operacii na legkih pri tuberkuleze (Clinical and social aspects of organ-preserving lung surgery in tuberculosis). In: Perelman MI (ed.) Organoshhadjashhie operativnye vmeshatelstva vo ftiziopulmonologii (Organ-Preserving Operations in Phthisio-pulmonology). Moscow: Scientific Centre for Phthisio-Pulmonology, 1989; pp. 4-6.
- Perelman MI, Naumov VN, Dobkin VG, Strel’tsov VP, Dubrovskii AV. Indication for the surgery in patients with pulmonary tuberculosis. Probl Tuberk 2002; (2): 51-55.
- Pfannschmidt J, Schönfeld N. Interdisciplinary Treatment of Patients with Pulmonary Tuberculosis Zentralbl Chir 2017; 142: S53-65. [PubMed]
- Pilipchuk NS, Kharchenko EF, Ivaniuta OM. Tuberkulemy legkih, plevry i sredostenia (Tuberculoma of the lungs, pleura and mediastinum). Kiev: Zdorov’ia, 1974.
- Pochepen ON, Zolotuhina LV, Zemec EA, Markevich MN, Troyanovskiy ES. The use of Surfactant-BL in treatment of inhalation injury after severe burns. Skoraia Meditsinskaia Pomoshtsh 2011; (12): 44-47. https://biosurf.ru/upload/iblock/6c4/6c4a77f6bcae8c66bc33fb7caeae4cfd.pdf.
- Polianskii VK. The surgical treatment of pulmonary tuberculosis. Voen Med Zh 1999; 320(10): 42-45. [PubMed]
- Polyansky VK, Beznosik RV, Savitsky GG. Tuberkulema legkih: monografiya (Pulmonary tuberculoma: monography). Pushkino: Kantsler, 2021.
- Porkhanov VA, Mova VS, Poliakov IS, Grebennikov SV, Marchenko LG. Surgical treatment of bilateral pulmonary tuberculosis. Probl Tuberk 1998; (1): 36-39.
- Priimak AA. Znachenie hirurgicheskih metodov v kompleksnoi terapii tuberkuleza (Significance of surgical methods in the combined therapy of tuberculosis). In: Perelman MI (ed.) Organoshhadjashhie operativnye vmeshatelstva vo ftiziopulmonologii (Organ-Preserving Operations in Phthisio-pulmonology). Moscow: Scientific Centre for Phthisio-Pulmonology, 1989; pp. 7-8.
- Repin IM. Repeated pneumonectomy in recurrence of pulmonary tuberculosis. Probl Tuberk 1990; (1): 35-39.
- Rozenberg ОА. Pulmonary surfactants for acute and chronic lung diseases (Part II). Obshhaia reanimatologia - General Reanimatology 2014; (10): 69-86.
- Rozenberg OA. Pulmonary surfactant preparations and surfactant therapy for ARDS in surgical intensive care (a literature review). Creat Surg Oncol 2019; 9: 50-65. [CrossRef]
- Rozenberg OA, Seiliev AA. Method for obtaining surfactant from bovine lungs. Patent RU2691648C1 (2019).
- Saludes V, Esteve M, Casas I, Ausina V, Martró E. Hepatitis C virus transmission during colonoscopy evidenced by phylogenetic analysis. J Clin Virol 2013; 57(3): 263-266. [CrossRef] [PubMed]
- Serov VV, Lebedev SP. Clinical morphology of visceral alcoholism. Vestn Akad Med Nauk SSSR 1988; (3): 48-53.
- Shilova MV, Khruleva TS, Tsybikova EB. Surgical aid to patients with respiratory tuberculosis. Probl Tuberk Bolezn Legk 2005; (5): 31-36.
- Schwarz E, Endres G. On relations between resection therapy in pulmonary tuberculosis and pregnancy Z Tuberk Erkr Thoraxorg 1961; 117: 28-36.
- Shabanov PD. Narkologia (Narcology). 2nd edition. Moscow: Geotar-Media, 2015.
- Simon K. Special features of thoracic surgery for tuberculosis in children and adolescents Z Tuberk Erkr Thoraxorg 1961; 117: 100-105.
- Smerdin SV, Untanova LS, Plekhanova MA. Organizacia protivotuberkuleznoi pomoshhi v Moskovskoi oblasti: 2018-2022 gg. Analiticheskii obzor (Organization of anti-tuberculosis care in the Moscow region: 2018-2022. Analytical review). Moscow: Regional public organization of disabled Zdorovie Cheloveka - Human Health, 2022.
- Sobkin AL. To the 100 anniversary of the state institution of Moscow healthcare “Prof. G.A. Zakhar' in Tuberculosis clinical hospital.” Tuberk Bolezn Legk 2014; (9): 97-99.
- Sokolov SB. Hirurgicheskoe lechenie bolnyh tuberkulezom legkih pozhilogo vozrasta (Surgical treatment of aged tuberculosis patients). In: Problemy legochnoi hirurgii. K 70-letiu prof. L.K. Bogush’a (Problems of the lung surgery (to the 70th anniversary of Prof. L.K. Bogush). Moscow: Central Institute of Tuberculosis, 1975; pp. 103-110.
- Sokolov EA. Surgical treatment of pulmonary tuberculosis patients over 60. Probl Tuberk 1978; (7): 23-27.
- Spitsyna TA, Gerasin VA, Molodtsova VP, Odintsov AI. Bronchial changes in children with primary tuberculosis Probl Tuberk 1984; (4): 26-30.
- Styagov GI, Timoshok AI. Medikamentoznye i nemedikamentoznye metody lechenia bolnyh alkogolizmom v LTP (Medical and non-medical treatment methods of alcoholic patients in LTP (labor-and-treatment prophylactoriums). In: Aktual'nye voprosy i polozhitel'nyi opyt organizacii psihiatricheskoi i narkologicheskoj pomoshhi v ITU i LTP (Current issues and positive experience in organizing psychiatric and drug addiction care in correctional institutions and LTPs) Selected articles. Domodedovo: Ministry of Internal Affairs of the Russian Federation, 1991; pp. 54-62.
- Svistunov BD, Svistunova AS. Endoscopic technologies in phthisiology. Tuberkulez i socialno znachimye zabolevania - Tuberculosis and Socially Significant Diseases 2015; (3): 25-28. Available from: http://in-tub.ru/storage/app/media/online-magazine/3-2015.pdf.
- Sweet DG, Turner MA, Straňák Z, Plavka R, Clarke P, Stenson BJ, et al. A first-in-human clinical study of a new SP-B and SP-C enriched synthetic surfactant (CHF5633) in preterm babies with respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed 2017; 102(6): F497-F503. [CrossRef] [PubMed]
- Syropiatov OG, Dzeruzhynskaia NA. Patogenez i biologicheskoe lechenie alkogolizma (Pathogenesis and biological therapy of alcoholism). Kiev: Military Medical Academy, 2000.
- Tarasova NS, Beloborodova EI. Hormonal and immunological aspects of renal lesions in patients with chronic alcoholism. Ter Arkh 2003; 75(11): 73-76.
- Teschner M. Current indications for resection of tuberculoid lung changes - relics of the pre-chemotherapy era? Pneumologie 1998; 52: 80-84. [PubMed]
- Tsybul'kin EK, Rozenberg OA, Seiliev AA, Volchkov VA, Zaitseva NV, Kuz'menko IG, et al. Our experience in the use of a Russian preparation of pulmonary surfactant in the treatment of acute respiratory distress syndrome and severe pneumonia in children. Anesteziol Reanimatol 1999; (2): 61-65.
- Uspenskii LV, Romanychev IuA, Kodolova IM, Chistov LV, Ablitsov IuA. Diagnosis and treatment of pulmonary tuberculomas. Khirurgiia (Mosk) 1986; (5): 11-15.
- Valiev RS, Valiev NR, Iksanov IY, Filatova MS. Epidemical importance of lung tuberculoma, the efficiency of their surgical and non-surgical treatment based on data from the Republic of Tatarstan. Probl Tuberk Bolezn Legk 2014; (4): 18-21.
- Vinnikova MA, Krenkel NT, Tikov MS, Tsareva IS. Sovremennye podhody k lecheniiu tiazhelogo alkogolnogo abstinentnogo sindroma. Metodicheskie rekomendacii (Modern approaches to the treatment of severe alcohol withdrawal syndrome (guidelines)). Moscow: Research and Practical Centre for Narcology, 2018.
- Yablonskii PK, Kudriashov GG, Avetisyan AO. Surgical resection in the treatment of pulmonary tuberculosis. Thorac Surg Clin 2019; 29: 37-46. [CrossRef] [PubMed]
- Zhemkov VF, Ivanovsky VB, Zhemkova MV, Seiliev AA, Volchkov VA, Rozenberg OA. Use of natural lung surfactant in the combination treatment of pulmonary tuberculosis Probl Tuberk Bolezn Legk 2013; 2: 18-22.
- Zyskin LI, Kozello NA, Grishin MN, Bereza RA. Early operations in pulmonary tuberculosis. Probl Tuberk 1991; (3): 36-38.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).