1. Introduction
First described in 1974 [
1], burnout was defined in 2019 by the World Health Organization as an occupation-dependent syndrome resulting from chronic workplace stress managed unsuccessfully and characterized by energy depletion or exhaustion as well as an increased work-related mental distance, negativism or cynicism, reducing professional efficacy [
2]. It represents a significant cause of healthcare professional turnover [
3], leading to increased on-the-job errors and reduced patient care [
4]. Ended as a global health emergency on 5 May 2023 [
5], COVID-19 has continued as a factor in escalating healthcare professional burnout since the beginning of the pandemic [
6] on 11 March 2020 [
7]. Regarding emergency room healthcare professionals, the impact of COVID-19 on their burnout has been substantial and studied extensively [
8,
9,
10,
11], particularly concerning emergency medicine physicians [
12,
13]. Burnout consideration is lacking regarding the effect of COVID-19 on medical professionals who were unaccustomed to emergency care pre-pandemic–-those previously focused on arranged appointments rather than emergency responses dictated by public health considerations. This study, a first, is intended to provide this examination and, based on the results, suggest positive coping interventions for these medical professionals that have been found effective for reducing burnout regarding emergency care related to COVID-19. The aim is to offer appropriate means for burnout reduction in appointment-centered medical specialists that can assist them in successfully coping during redeployment in pandemic emergencies to emergency care guided by public health considerations while at the same time maintaining the viability of the medical specialty and excellence in patient care.
Fourteen medical specialties were selected to investigate their burnout, representing physicians redirected from their usual practices to provide emergency care during the pandemic. They are those specialties whose members regularly see their patients by prearranged appointments. As such, excluded from the assessment are specialties whose members changed their practices because of COVID-19 considerations but were unassigned to emergency care. Oncologists are an example of specialists who were excluded for this reason [
14]. Those included are as follows: cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, internists, nephrologists, neurologists, obstetricians, orthopedic surgeons, pediatricians, plastic surgeons, psychiatrists, and radiologists. For each, pre-COVID-19, they had a significant degree of control over when, for how long, and under what conditions they would meet with patients. Although there may have been aspects of their patient care that were unpredictable and additionally stressful, they had been trained for these [
15]. Physicians specializing in emergency care are notable for lacking control over when, for how long, and in what circumstances they meet with patients in contrast [
16]. Because of this substantial difference in appointment-centered and emergency care, investigating the effect of COVID-19 burnout on those physicians representing medical specialties unaccustomed to treating patients regarding public health medical emergencies is valuable. Specialties greatly affected by burnout when redeployed to emergency care could represent a risk factor for the detrimental development of a pandemic team during the team’s operation—an additional reason for concern [
17].
The hypothesis is that medical specialists accustomed to planning for unpredictable situations in their practice demonstrate the least burnout regarding COVID-19-related emergencies. To be determined in considering coping as a process resulting from COVID-19 is the accuracy of this hypothesis by comparing and ranking the similarities and differences in the coping strategies of emergency responses across the various normally patient-centered medical specialties. In doing so, the concerns are whether the coping strategies employed by the medical specialties were such that the medical specialty's viability was maintained, as was excellence in patient care. The results support the presented hypothesis. Based on the research presented in the search of articles returned for each specialty, interventions originated by these medical specialties are then suggested that may be effective in reducing burnout while at the same time ensuring medical specialty viability and excellent patient care. The aim is burnout reduction in these appointment-centered medical specialists during pandemic emergencies when they are redeployed and expected to be guided by public health considerations.
2. Materials and Methods
A Google Scholar search over the two days from 30-31 March 2024 gathered the materials for this study. The statement “burnout resulting from COVID-19 emergencies treated by [medical specialty]” was individually searched for each of the fourteen medical specialties. Searched on 30 March were the following medical specialties: cardiology, endocrinology, internal medicine, nephrology, neurology, obstetrics, orthopedics, pediatrics, plastic surgery, psychiatrists, and radiology. Searched on 31 March were the remainder: dermatology, family medicine, and gastroenterology. Selected were the particular medical specialties that see their patients based on prearranged appointments dependent on the physician’s schedule. Although certain specialties, such as obstetrics, may encounter emergencies as part of their practice, the range of emergencies is anticipated and represents one for which the physicians receive training as part of their specialty. Public health considerations regarding a previously unknown, highly contagious, life-threatening virus for which they are untrained previously do not direct these emergencies [
18].
The purpose of the search was to retrieve a sample of the four most cited relevant articles for each specialty to determine three things: the type of emergency with which they were involved regarding COVID-19, the response of the medical specialist to the emergency, and the outcome of this response concerning patient care. Google Scholar was selected as the search engine because it is crawler-based and, therefore, it lists the returns in order of highest number of citations to lowest [
19]. Included with the number of returns is the number of citations each document has received. The four articles selected from the Google Scholar search of the day were the most relevant and had the highest number of citations. When this search was done matters, as, unlike other search engines, Google Scholar returns are inconsistent over different searches—why Google Scholar is neither recommended for a scoping, nor systematic, review [
19].
The methodology used for this analysis is a form of qualitative research. Few studies define qualitative research [
20]. A recent article [
21] indicates that qualitative research discusses how things come to be and their outcome. Discussion for this study regards the approach to emergencies and the outcome. Compositely, a definition provided of qualitative research is “an iterative process in which improved understanding to the scientific community is achieved by making new significant distinctions resulting from getting closer to the phenomenon studied” [
20]. This definition offers the aim of the current investigation as a form of qualitative research [
21]. The case study method is similar to the analysis undertaken here. For COVID-19-related emergencies, both types of analysis focus on a comprehensive exploration of the burnout experienced in the medical specialties examined regarding the viability of the medical specialty and the outcomes of patient care. What differs from the case study is that this research does not include an author-investigated on-site collection method, relying entirely on well-cited, recently published, peer-reviewed articles as materials [
21].
3. Results
Table 1 presents a summary of the results of this investigation. These results are additionally explicated in the alphabetically arranged subsections regarding the four well-cited articles returned for each of the separate medical specialties searched with Google Scholar on 30 or 31 March 2024.
3.1. Cardiology
According to a 2023 summary of COVID-19-related consequences concerning this specialty [
22], cardiologists perhaps saw the most change to their practice. Whereas cardiovascular treatment pre-COVID-19 included processes that were rigorous and extensive, the need for COVID-19-related hospital beds and fear by patients (and healthcare providers) regarding virus contagion meant that there was a vast reduction in the number of patients admitted for acute cardiovascular experiences and, of those served, there was a significant reduction in their stay. This result of COVID-19, two authors note, was entirely unanticipated by cardiologists [
22,
23]. It caused a radical change in the culture of cardiology, leading to such burnout in these specialists that the result was mass resignations to the extent that the reduction in cardiologists has been called a staffing crisis [
24]. The direct impact on patient care was that, with fewer cardiologists conducting a reduced regime of tests, cardiology patient wait times increased while testing services previously considered imperative now were reduced. This outcome was evident even in the beginning days of the pandemic, including those cardiologists in cardio-oncology, with over 85% of cardiologists adopting telemedicine during the early stages of the pandemic [
25], a solution advised based on research undertaken as the pandemic began [
23].
3.2. Dermatology
A survey of Indian dermatologists conducted early in the pandemic noted that burnout among dermatologists was extensive as their practice evolved to become exclusively frontline and involved witnessing “large volumes of infections and deaths” [
26]. A lack of personal protection equipment meant that the evaluation of self-infection risk was the second most common risk factor for stress-resulting burnout. In research on how graduate medical education for dermatologists changed generally during the pandemic [
27], most residents were required to suspend their educational activities and switch to patient care. In doing so, learning hours were limited. In this regard, virtual learning became the alternative, with some residents required to switch to non-dermatologic care. In the United States [
28], burnout of dermatologists rose to 36% in 2020, with uncertainty about the future, fear of exposing loved ones to COVID-19, and a reduction in compensation being the instigators of this burnout–-especially for women [
29]. The consequences for patients have been that with the roles of dermatologists shifted to the frontline, patient care for dermatology switched to telemedicine. Dermatologists saw this practical change as deficient because their practice is “very visual” [
29]. As such, telemedicine cannot provide the level of care to patients thought necessary by these practitioners.
3.3. Endocrinology
Well-cited research publication on the effect of COVID-19-related burnout on endocrinologists began early in the pandemic and continues into 2024. The earliest research [
30] in managing pediatric diabetes during the pandemic noted that pediatric patients were no more likely to be affected by COVID-19 than other patients, and most were either asymptomatic or had mild symptoms. However, delayed hospital admissions were the result of the pandemic for diabetics and other endocrine diseases. This result presented a need for emergency care of these patients because maintaining consistent contact with the endocrinologist is necessary for an endocrine disease. Since this level of in-person contact was impossible during the pandemic, it was a factor in burnout for endocrinologists. The transition to telemedicine solved this problem partially. Women and younger doctors were the Italian endocrinologists most affected by burnout during this period [
31]. Increasing throughout the last four years, by 2024, burnout is experienced frequently by United Kingdom endocrinologists [
32]. The COVID-19 pandemic disrupted endocrine operations in the United States. Burnout was a result. Compared with pre-pandemic levels, thyroid and parathyroid operations remain at a decreased level [
33].
3.4. Family Medicine
Italian family physicians were found in the initial stages of the pandemic to go from resilience to burnout as emergencies related to COVID-19 had a significant impact on their work management brought on by intense emotions producing emotional exhaustion as they became frontline medical providers and had to modify their practice through using telephone calls [
34]. Austrian physicians who were younger or those in junior career stages demonstrated poorer psychological outcomes, leading to burnout, speculated to result from fewer patients in their practice, leading to a fear of lost income; however, patient violence was also recognized as a predictor of burnout [
35]. Of the family physicians surveyed in the United States, 50.4% had manifestations of burnout. Physician shortages depended on how many COVID-19 patients were treated [
36]. Women and those early in their careers burned out most often in Turkey. The result was an increase in mistakes made in treatment [
37].
3.5. Gastroenterology
For gastroenterologists, trainees taking care of patients with COVID-19 were especially likely to report burnout. The residents assigned to COVID-19 isolation wards had no physical contact with their colleagues or families and worked beyond their specialty-related competencies [
38]. The field itself had to adapt to minimize the possibility of spreading the virus, including reducing outpatient visits and procedures while shifting to telemedicine–-even with these changes, burnout was rampant from long shifts, hospitals surpassing capacity, and gastroenterologists being particularly susceptible to the virus [
39]. Burnout in this field from COVID-19 has resulted in physician turnover and reduced clinical hours as doctors are abandoning the profession [
40]. Overall, those gastroenterologists who were most affected by burnout were women and younger members of the profession as a result of the stressors from both the change in work from the virus and its effect on home life and financial uncertainty. Both family and patients were seen for shorter periods, and care for patients was more complicated, involving increased administration that concomitantly expanded the litigiousness of the environment [
41].
3.6. Internal Medicine
In a study for which 42% were physicians specializing in internal medicine experienced burnout from COVID-19 as well as civil war in Libya, the components of burnout were irregular compensation, high levels of verbal abuse, the displacement of physicians from their homes, shortage of supplies, and fear of their own and their family’s infection by COVID-19 [
42]–-demonstrating how much worse the situation with COVID-19 is when accompanied by the effects of a war. Yet, even in a country such as Turkey, which was not at war, verbal abuse was part of the reason for burnout in this specialty. Additionally concerning was the extreme worry over malpractice resulting from COVID-19, with these doctors stating that they lacked sufficient medicolegal training [
43]. In Spain, 40% of internists suffer from burnout because of overwork without compensation and the fear that they would be contagious to their families, as 90% of these doctors were charged with working on the front line [
44]. In contrast with other specialties, burnout did not result in mass resignation. An additional study of Spanish internists found that none took sick leave because of a strong collective spirit and a sense of solidarity with colleagues enhanced by institutional effectiveness in restructuring work shifts and a focus on teamwork–-seen as a sign of support at the institutional level by the doctors [
45].
3.7. Nephrology
Although most learning was remote, surprisingly, of those resident nephrologists studied regarding their burnout experienced concerning COVID-19, only 15% reported burnout. Furthermore, they had additional reasons for burnout, including problems maintaining their knowledge base, poor work-life balance, and exhausting relationships with friends [
46]. A study of nephrologists further in their careers reported 25% burnout—a percentage less than other specialties noted in this study. There was no difference between male and female nephrologists in the level of burnout they experienced, also in contrast to other specialties. What may be unique regarding nephrologists is something related by one of the participants in the study, “My patients are sick, even when they’re ‘well.’ The tools I have to test them with are often as toxic as the diseases, with flimsy evidence to support them” [
47]. In other words, these doctors work under normal conditions comparable to conditions encountered when treating emergency COVID-19 patients. For those nephrologists who did suffer burnout, there was a direct relationship between it and poor institutional support–-including insufficient remuneration for hours worked. All nephrologists in this study noted the need for widespread systems change in response to COVID-19. This call for organizational support, improved training, and additional equipment were the conclusions of a subsequent study of burnout in nephrologists during the pandemic [
48]. Fear of contagion increased when appropriate personal protective equipment was insufficient. Coping strategies included strict infection control based on the training of patients and their close contacts. Nevertheless, even with these safeguards, nephrologists were susceptible to COVID-19 and were among those physicians suffering from long COVID-19 and increasing reported burnout–-especially in institutions known for their poor support. Although these factors pose a risk of increased attrition rates, they have not materialized in this specialty [
49].
3.8. Neurology
During the pandemic, there was a reduced ability to admit and transfer critically ill neurologic patients due to hospital overflow and the risk to patients of COVID-19 exposure. Furthermore, neurologists were among the specialties redeployed to general medicine to assist colleagues in managing the surge of medical patients [
50]. Minimized self-care was noted from this practice change to produce burnout in neurologists, resulting in feeling disempowered, previously described as relevant in contributing to burnout in neurologists in the United States [
51]. The percentage of those neurologists continuing to see neurological patients reporting an experience of burnout was relatively low at 17%, with no statistically significant difference between male and female physicians [
52]. This lack of difference between male and female neurologists regarding rates of burnout was confirmed in another study of neurologists conducted in Norway [
53]. This report highlighted that most neurologists experienced changes in their practices when the focus shifted to COVID-19. Fewer means of access to resources were available, including insufficient personal protection equipment, increasing the danger of contagion to the physician and family members. Yet, interestingly, the concern with becoming infected was not noted as a contributor to burnout. The norm for appointments and consultations became the telephone, and there was a reduction in options for rehabilitation.
3.9. Obstetrics
When COVID-19 resulted in the emergency related to vaginal births shifting from delivery focus to infection avoidance, obstetricians found their coping strategies insufficient to avert burnout. Masking and social distancing resulted in poor communication with the patient during labor, made worse by the required absence of the partner during the birth [
54]. Without pandemic guidelines for adapting their practice, and the often non-compliance of family members with the COVID-19 restrictions, there was a “parallel pandemic” of obstetrician burnout resulting from workplace stress as many obstetricians refused to be present for vaginal births, with planned caesarian sections taking their place [
55]. The healthcare system and the country determined how this drastic effect varied—with the rate of burnout of obstetricians in those countries where the pandemic was most prevalent the greatest—leading to retired staff assisting in deliveries [
56]. The level of preparedness a specialist had devised for emergencies over their years of practice determined the level of burnout in obstetricians. As a result, younger members of the profession with less experience planning their means of coping with emergencies were more greatly affected by burnout, especially when personal protective equipment was limited [
57].
3.10. Orthopedics
For those orthopedic residents reassigned to frontline activity during the pandemic, fatigue caused by sleep deprivation from the long hours worked and enforced self-quarantine produced burnout. COVID-19 resulted in a significant alteration in the concept of urgency and indications for elective treatments. An increased use of telemedicine for outpatient visits was caused [
58]. One study found that orthopedic surgeons were unlikely to experience burnout from COVID-19 because they developed effective coping strategies that improved resilience and produced a general feeling of well-being. These strategies included a willingness to acknowledge challenges, having control over their time, taking mental breaks, providing mentorship, and having support [
59]. Another study mirrored these results in finding that trauma care provided by orthopedic surgeons motivated them to develop strategies that promote well-being in their practice during COVID-19. When burnout did result, fear of contamination of self and family, financial liabilities, poor planning by their institutions, work overload, and shortages of equipment were the causes—things outside the control of the orthopedic surgeon. Maintaining control included developing significant wait lists for orthopedic surgeries [
60]. Preserving a feeling of control over their work was acknowledged in another study as necessary to avoid burnout; otherwise, orthopedic surgeons felt overwhelmed, inadequate, and uncertain. [
61].
3.11. Pediatrics
Regarding pediatric emergencies during COVID-19, pediatrician burnout was often unrelated to either moral dilemmas or the type of injury. Helpful responses to burnout were those devised in Toronto during the 2003 SARS epidemic and included emotional and material support, resources for caregivers, multidisciplinary collaboration, identification of different ways of expressing burnout, and effective hospital leadership that communicated clearly [
62]. However, because of the low incidence of severe COVID-19 among children, the burnout that 37.4% of residents suffered in one 2021 study was not associated with the COVID-19 outbreak, as only a third of pediatricians saw patients who had contracted the virus [
63]. However, by 2023, research had identified that those pediatricians who did attend to COVID-19 emergencies were affected by higher rates of burnout, resulting in chronic exhaustion and sleep disorders, having a strong to severe impact on their lives [
64]. For patients, COVID-19 resulted in pediatricians managing more complex patients, requiring a high level of skill and knowledge for treatment—something that younger pediatricians might feel they lacked, contributing to their burnout [
65].
3.12. Plastic Surgery
As the pandemic began, the advice to plastic surgeons was to postpone all elective operations. Reduced operating room time and minimized hospital stays accompanied non-postponable operations, leaving only those plastic surgeons scheduled surgeries for most cancers continued [
66]. This significant decrease in elective surgeries and redeployment to emergency care represented a factor in residents' burnout who experienced high levels of isolation with their decreased surgical responsibilities during the pandemic, resulting in increased medical errors [
67]. In 2022, New York and New Jersey plastic surgeon residents were significantly affected by burnout. Furthermore, limited by continuing clinical restrictions and social distancing policies, they would have to perform an extra 24 operations and make 783 clinic visits per month over six months to address the surgical backlog brought on by the pandemic. As such, the anticipation was that this would lead to additional residents experiencing burnout [
68]. For cosmetic surgeons working entirely in private facilities during the pandemic, the shift to emergency surgery in hospitals increased performed surgeries and the hours they worked to the extent that one-third of aesthetic surgeons reported the emotional distress found with burnout [
69].
3.13. Psychiatry
In emergency departments at the beginning of the pandemic, psychiatric physicians provided care using a telephone, video camera, or in person with personal protective equipment, with patients considered for psychiatric admission undergoing rapid testing to determine COVID-19 status and then assigned COVID-19 positive and COVID-19 negative inpatient units established under controversy. During this period, symptoms of burnout were prevalent among psychiatrists, and the need for psychiatric treatment for these psychiatrists increased significantly [
70]. Regarding psychiatric residents of Saudi Arabia, in a 2021 study, burnout was found in 27.3%. Those residents in the first two years of training with a history of mental health treatment during their period in residency were found to be at higher risk [
71]. In another 2021 study of both adult and child Turkish psychiatrists, high levels of both work (60.8%) and patient-related burnout (49.8%) were reported, with over half indicating they had insufficient resources during the emergency conditions brought on by COVID-19. Working outside their expertise provided an additional reason for the identified burnout. The study also noted that psychiatrists are known to be more vulnerable to burnout than other physicians and surgeons [
72]. Certain countries had reduced burnout rates in psychiatrists than others because of the introduction of telehealth early in the pandemic, with telepsychiatry considered a technological revolution in psychiatry, improving psychiatrists’ well-being. Within this specialty, telemedicine was not just a valuable aid during COVID-19. It became essential in treating patients, especially regarding the accompanying “mental health pandemic” that was seen to arise with COVID-19 exacerbated by social distancing and was predicted to increase following the pandemic, with many patients preferring being treated online rather than in person [
73].
3.14. Radiology
At the start of the pandemic, 40% of US radiologists reported that their institution did not have a mass casualty imaging plan in place to meet the emergency needs of COVID-19 and, complementarily, 60% reported that there had been an increase in the utilization of portable imaging—chest X-rays were the most common diagnostic approach related to COVID-19. Nearly all radiologists had a decrease in their normal workload as a result of cancelations of non-emergency procedures during the pandemic, resulting in a deployment to emergency departments that might include handing out personal protective equipment, resulting in 61% of respondents noting anxiety levels of 7 or more out of 10, symptomatic of burnout [
74]. In resisting burnout, Italian radiologists sustained frequent shift rotations for the entire radiology staff, encouraged teamwork, employed psychological support, and had sufficient remuneration [
75]. Singapore radiologists reduced burnout based on frequent shift rotations [
76]. Spanish radiologists did not enact these measures, and burnout increased significantly during the pandemic—affecting nearly half of participants [
77].
4. Discussion
This discussion will include three parts. The first represents the various coping strategies available to medical specialties in considering the understanding of Lazarus regarding coping as a process. Based on this investigation of coping strategies, the next section will rank the coping strategies for maintaining the viability of the specialty, resisting burnout, and ensuring excellent patient care used by the fourteen different medical specialties concerning their positive coping and then analyze the ranking provided. The final section is a presentation of the study's limitations.
4.1. Coping Strategies
In defining coping as cognitive and behavioral efforts to manage stress, Lazarus [
78] considered two general approaches to coping—a style and a process. Coping as a style is dependent on preconceived views regarding the health or pathology of the person under stress [
79,
80,
81], confounding the issue in the view of Lazarus. His work, beginning in the 1960s and later standardized with Folkman in the 1980s [
82,
83], instead saw coping as a process based on research findings that, to determine if a strategy is adaptive or maladaptive, coping thoughts and actions must be measured separately from their outcomes under stress [
78]. In other words, coping strategies that may be maladaptive regarding one type of stress may be adaptive to another stress encountered. Furthermore, even with the same stress, over time, strategies can evolve from one adaptation to the other. This version of process theory [
84] then was refined in [
78]. It is the method through which the coping of the various medical specialists to the stress of being redeployed from appointment-centered patient care to the public health emergencies brought on by COVID-19 will be examined.
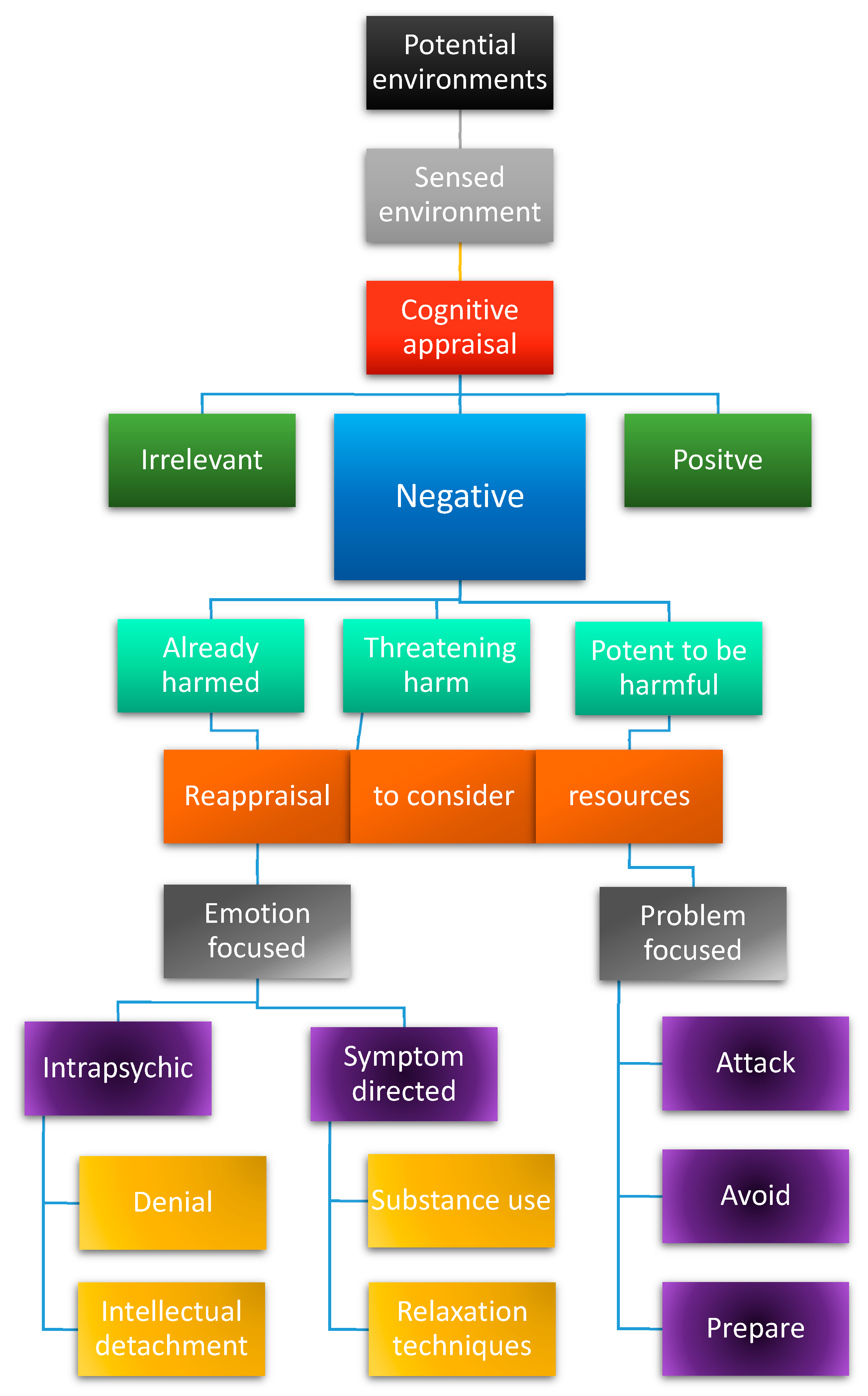
Figure 1 represents a visualization of the hierarchy in process-related coping theory [
78,
82]. Coping theory begins with the understanding that coping is a relationship between the available objective environment and the focus of an individual in that environment. The point of view of the person entirely determines the individual's focus. In this coping theory, from the point of view adopted, the individual makes a cognitive appraisal of the sensed environment. In this regard, there are three possible appraisals. The first is that it is irrelevant to the interests of the individual. Another cognitive appraisal is that it is a positive to the interests of the individual. Although positive appraisals can produce stress, leading to the need for coping behavior [
85], for this analysis related to COVID-19, the focus of this research is the third option—it is a negative to the interests of the individual. Once the medical specialists appraised COVID-19 as a negative, three ways can evaluate its harm. The first is that it had already harmed the individual, the second is that there would be future harm to the individual, and the third is that there was potential for harm, but not necessarily so. Then, medical specialists considered the resources available, reappraising what was sensed based on these resources, regardless of the selection of the three cognitive appraisals.
What is interesting in this theory is that there is no one route that individuals must take in their reappraisal dependent on their initial cognitive appraisal. As such, the interpretation of harm could result in a reappraisal that is either emotion-focused or problem-focused. Furthermore, these foci are not exclusive. In coping, the individual may have opted for both an emotion-focused and a problem-focused solution. In concentrating on emotion-focused strategies, there were two routes. One is intrapsychic, concerned with altering mental perception and divided into stress denial or mentally detaching oneself from the situation. The other is symptom-related, where the hurt that the harm has caused will cause or is likely to cause is reduced by ingesting substances or assisted relaxation techniques. If problem-focused, the specialist had three options to solve the problem—attack, avoid, or prepare. In any case, the focus was making changes to the sensed external environment rather than making internal changes to assist in coping.
Regarding this configuration of
Figure 1 produced by the author, the most well-cited research on coping theory is the collaboration between Lazarus and Folkman in 1984 [
83]. Yet, Folkman interpreted an aspect of the theory with a subtle difference from that of Lazarus. Lazarus viewed a challenge as one type of negative cognitive appraisal [
78]. Folkman defined challenge as an appraisal "characterized by pleasurable emotions, such as excitement and eagerness” [
86]. This definition neglects the negative cognitive appraisal of a challenge essential to coping theory. The possible confusion regarding the term challenge is why the author has substituted “potential to be harmful” for “challenge” in
Figure 1. Moreover, by making this substitution, the divisions of negative cognitive appraisal each now relate to harm. With challenge as the third division in the original theory, it was unclear just what its relationship was to harm.
Lazarus emphasized [
78,
82,
84] that no one coping response is always effective or ineffective. Instead, coping strategies depend entirely on the situation as perceived, the resources available, the time that has passed since the first perception of the threat, and the amount that the individual wants to invest in the stress. Thus, the responses of these medical specialists were adaptive or maladaptive for burnout regarding the contribution of these aspects together and were modifiable throughout the pandemic in conjunction with changes to resources obtainable and the particular experience of burnout. With more than one coping strategy available for use at any time with different levels of success, ranking the adaptations made when the medical specialists were redeployed from appointment-driven patient care to emergency public health-directed care during COVID-19 will go beyond these variables. The various medical specialties will be ranked by how well their coping strategies ensured the viability of the specialty, burnout resistance in the practitioners, and excellent patient care. The author has assigned the rank to these medical specialties based on the four articles analyzed for each medical specialty, combining these variables (see
Table 2).
Based on the results of
Table 2,
Table 3 indicates the effectiveness of the coping strategies for each specialty in the four publications. As such, reordering the medical specialties based on the rank assigned in
Table 2,
Table 3 illustrates the effectiveness of the coping strategies for ensuring the viability of the specialty, burnout resistance in the practitioners, and excellence of patient care.
4.2. Ranking of Medical Specialties Regarding Positive Coping
Lazarus contended that there is no coping strategy that is adaptive or maladaptive in itself [
78]. Furthermore, some strategies normally maladaptive may, at times, be the best coping strategy to alleviate stress and reduce burnout [
84]. Nevertheless, it is interesting that by their actions, none of the specialties approached the stress of being deployed to emergency care by being emotion-focused. That said, the extreme response of the cardiologists with mass resignation partially could be based on a type of intellectual detachment from the problem or the need to be more comfortable with the situation and, therefore, be emotion-focused concerning coping theory. On the other hand, this response could be considered a problem-based solution equaling avoidance. In either case, cardiologists may have reduced their burnout, but at the cost of vastly depleting the number of cardiologists and, in doing so, greatly extending the wait time for patients to see a cardiologist—the reason cardiologists were ranked last.
Regarding the organization of the rankings, the author considered that although the coping strategy adopted was to resist burnout, it is of greater importance that the medical specialty remains viable and that patients continue to receive excellent care. Therefore, specialty viability and excellence in patient care are considered more relevant in the organization of the rankings regarding the coping strategies to resist burnout. With
Table 3, the organization of the rankings should be evident in reading the table from top to bottom and that, for example, a “Yes” is always better than a “Somewhat” reply. However, this is not always the case. Neurology comes before plastic surgery in the ranking because, although plastic surgeons resisted burnout with their chosen coping strategies more than neurologists, the effect on patient care was additionally detrimental to those seeking the care of plastic surgeons as this care increasingly moved to private clinics—reducing access to these services for those unable to afford such care.
Except for this stated anomaly regarding the organization of ranking for
Table 3, in other respects, reading from top to bottom, the table depicts why the rank of the medical specialties is in the order that resulted. Nephrology ranked first because, with the previous measures they devised for attending to their patients in their appointment-centered practice, they had prepared for the public health considerations of COVID-19. Because of this preparedness, they were of the mindset to adapt to any additional changes required. In this way, when employing the coping strategy used by this specialty, there was no real change to any of these variables for this specialty, placing it first in rank. There are two cases where more than one specialty received the same reply for each of the three columns. The case of psychiatry and internal medicine represents one—with the replies of Yes for the two most important categories and Somewhat for burnout reduction. The other is endocrinology and family medicine, each with a Yes, Somewhat, and a No. Given that each medical specialty received the same reply, it is relevant to explain these replies further.
For psychiatry, COVID-19 produced an overwhelming case increase. Yet, rather than burning out, the coping strategy of psychiatrists was to reformulate the specialty with telemedicine. The result was that 2021 research found psychiatrists felt better served by telemedicine, and patients stated they preferred or were equally well-served by telemedicine compared with face-to-face meetings [
87]. The view of patients that telemedicine served them equally well is further enhanced by psychiatrists believing that all of their patients potentially can be served by telemedicine [
88]. Psychiatrists ranked after nephrologists because the “mental health pandemic” provided additional stress. Internal medicine is ranked third because although these specialists very competently adjusted to emergency care with the coping strategies they adopted, the increased abuse faced by these specialists and their concern regarding malpractice were both detrimental. Accompanied by insufficient remuneration for their work, this would lead to burnout. Comparing endocrinology with family medicine—the other specialties with the same replies in
Table 3—family medicine was considered at a lower ranking because these doctors admitted to making errors from the redeployment. This problem was judged more regarding patient care than the longer waits to see endocrinologists.
4.3. Limitations
Although the strength of this study is that it is the first to compare the responses of various medical specialties to their deployment to emergency care based on public health considerations regarding COVID-19, there are limitations. The first—comparison is limited to only fourteen specialties. Consideration was given to only those specialties redeployed. Oncologists were the example provided of a specialty not considered in this regard. However, in lacking four articles returned to the end of the March 2024 Google Scholar search on this matter, ophthalmologists also were excluded. An additional limitation is that the four articles returned with the most citations regarding each specialty presented the situation of the specialty at a specific time during the pandemic and under certain conditions. As Lazarus noted, coping strategies change regularly depending on several considerations. Therefore, these four articles selected to represent each medical specialty may have resulted in a distorted picture of what was the overall response of these specialties regarding COVID-19 because of the timing of the study and the particular conditions the medical specialty was then facing—both regarding the initial cognitive appraisal and the reappraisal concerning the coping theory process. Therefore, the rankings and the results' limitations of the studies were highly dependent. Coping theory was not the focus of the four articles analyzed for each specialty—another limitation. This author interpreted whether the coping strategies were emotion or problem-focused and, if emotion-focused, whether intrapsychic or symptom-directed. In contrast, if problem-directed, whether the coping strategy adopted was an attack, an avoidance, or preparedness.
5. Conclusions
All medical specialists experienced burnout when redeployed from appointment-centered patient care to emergency care based on public health considerations during the COVID-19 pandemic; certain medical specialists resisted burnout more effectively while maintaining the viability of their specialty and providing excellent patient care—others were less effective by these measures. Prepared procedures developed as part of the specialty during the non-pandemic situation, working together as a team, institutional support, and successful use of telemedicine were the coping strategies that were effective as interventions. Regarding telemedicine, although its use became ubiquitous, not all medical specialties took on the challenge of using telemedicine to the advantage of both the specialty and patients, as did psychiatry. Some specialists (such as dermatologists) used telemedicine reluctantly, serving patients less well. In maintaining the viability of the profession and for patient care, the intervention least effective was mass resignation in the face of redeployment—cardiologists' coping strategy.
Future research in this area would be to determine how appropriate the rankings have been for these medical specialists as the effect of the pandemic recedes. Based on the results of this study and their employed coping strategies—nephrology and psychiatry would have become even more effective as medical specialties—shortages of cardiologists would soon become critical. Malpractice concerns would have escalated for internal medicine and gastroenterology. Plastic surgery increasingly would have become attainable only through private clinics. Moreover, wait times for booking patient appointments would have increased with fewer physicians. Almost all resident training was significantly affected by COVID-19. However, it is unclear what the effect will be on future doctors. Although the pandemic altered aspects of resident training [
89], residents had the opportunity to learn skills and achieve training unattainable otherwise by being deployed to emergency care during the pandemic.
The study found the initial hypothesis true—medical specialists accustomed to planning for emergency possibilities in their practice would demonstrate the least burnout regarding COVID-19-related emergencies. However, the result that the coping strategies adopted by the various medical specialists to reduce burnout affected both the viability of their specialty and the excellence of patient care provided was of greater importance. What is positive to note regarding COVID-19 is that, concerning the process of coping theory, cognitive reappraisal can take place at any time and, as such, might increasingly result in coping strategies that improve both specialty viability and excellence in patient care.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The author declares no conflicts of interest.
References
- Freudenberger, H.J. Staff Burn-Out. Journal of Social Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- World Health Organization Burn-out an “Occupational Phenomenon”: International Classification of Diseases 2019.
- Tabur, A.; Elkefi, S.; Emhan, A.; Mengenci, C.; Bez, Y.; Asan, O. Anxiety, Burnout and Depression, Psychological Well-Being as Predictor of Healthcare Professionals’ Turnover during the COVID-19 Pandemic: Study in a Pandemic Hospital. Healthcare 2022, 10, 525. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, M.; Asadi-Pooya, A.A.; Mousavi-Roknabadi, R.S. Burnout among Healthcare Providers of COVID-19; a Systematic Review of Epidemiology and Recommendations : Burnout in Healthcare Providers. Archives of Academic Emergency Medicine 2020, 9, e7. [Google Scholar] [CrossRef] [PubMed]
- Rigby, J.; Satija, B. WHO Declares End to COVID Global Health Emergency. Reuters 2023.
- Morgantini, L.A.; Naha, U.; Wang, H.; Francavilla, S.; Acar, Ö.; Flores, J.M.; Crivellaro, S.; Moreira, D.; Abern, M.; Eklund, M.; et al. Factors Contributing to Healthcare Professional Burnout during the COVID-19 Pandemic: A Rapid Turnaround Global Survey. PLoS ONE 2020, 15, e0238217. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio Medica Atenei Parmensis 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Alanazy, A.R.M.; Alruwaili, A. The Global Prevalence and Associated Factors of Burnout among Emergency Department Healthcare Workers and the Impact of the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Healthcare 2023, 11, 2220. [Google Scholar] [CrossRef]
- Chor, W.P.D.; Ng, W.M.; Cheng, L.; Situ, W.; Chong, J.W.; Ng, L.Y.A.; Mok, P.L.; Yau, Y.W.; Lin, Z. Burnout amongst Emergency Healthcare Workers during the COVID-19 Pandemic: A Multi-Center Study. The American Journal of Emergency Medicine 2021, 46, 700–702. [Google Scholar] [CrossRef]
- Rodriguez, R.M.; Montoy, J.C.C.; Hoth, K.F.; Talan, D.A.; Harland, K.K.; Eyck, P.T.; Mower, W.; Krishnadasan, A.; Santibanez, S.; Mohr, N.; et al. Symptoms of Anxiety, Burnout, and PTSD and the Mitigation Effect of Serologic Testing in Emergency Department Personnel During the COVID-19 Pandemic. Annals of Emergency Medicine 2021, 78, 35–43. [Google Scholar] [CrossRef]
- Schablon, A.; Kersten, J.F.; Nienhaus, A.; Kottkamp, H.W.; Schnieder, W.; Ullrich, G.; Schäfer, K.; Ritzenhöfer, L.; Peters, C.; Wirth, T. Risk of Burnout among Emergency Department Staff as a Result of Violence and Aggression from Patients and Their Relatives. IJERPH 2022, 19, 4945. [Google Scholar] [CrossRef]
- Verougstraete, D.; Hachimi Idrissi, S. The Impact of Burn-out on Emergency Physicians and Emergency Medicine Residents: A Systematic Review. Acta Clinica Belgica 2020, 75, 57–79. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Mu, M.; He, Y.; Cai, Z.; Li, Z. Burnout in Emergency Medicine Physicians: A Meta-Analysis and Systematic Review. Medicine 2020, 99, e21462. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.H.J.; Murali, K.; Kamposioras, K.; Punie, K.; Oing, C.; O’Connor, M.; Thorne, E.; Amaral, T.; Garrido, P.; Lambertini, M.; et al. The Concerns of Oncology Professionals during the COVID-19 Pandemic: Results from the ESMO Resilience Task Force Survey II. ESMO Open 2021, 6, 100199. [Google Scholar] [CrossRef]
- Veronese, C.; Williams, M.; Dickson, J.; Bush, M.; Shenvi, C. Determining the Educational Value of an Emergency Medicine Rotation for Non-Emergency Medicine Residents. Cureus 2023. [Google Scholar] [CrossRef] [PubMed]
- Elizabeth M Schoenfeld; Sarah L Goff; Tala R Elia; Errel R Khordipour; Kye E Poronsky; Kelly A Nault; Peter K Lindenauer; Kathleen M Mazor Physician-Identified Barriers to and Facilitators of Shared Decision-Making in the Emergency Department: An Exploratory Analysis. Emerg Med J 2019, 36, 346. [CrossRef]
- Dionisi, T.; Sestito, L.; Tarli, C.; Antonelli, M.; Tosoni, A.; D’Addio, S.; Mirijello, A.; Vassallo, G.A.; Leggio, L.; Gasbarrini, A.; et al. Risk of Burnout and Stress in Physicians Working in a COVID Team: A Longitudinal Survey. Int J Clin Pract 2021, 75. [Google Scholar] [CrossRef] [PubMed]
- Sinsky, C.; Linzer, M. Practice And Policy Reset Post-COVID-19: Reversion, Transition, Or Transformation?: Commentary Examines Possible Policy and Practice Changes for Health Professionals, Regulators, and Payers after the COVID-19 Pandemic. Health Affairs 2020, 39, 1405–1411. [Google Scholar] [CrossRef] [PubMed]
- Gusenbauer, M.; Haddaway, N.R. Which Academic Search Systems Are Suitable for Systematic Reviews or Meta-analyses? Evaluating Retrieval Qualities of Google Scholar, PubMed, and 26 Other Resources. Research Synthesis Methods 2020, 11, 181–217. [Google Scholar] [CrossRef] [PubMed]
- Aspers, P.; Corte, U. What Is Qualitative in Qualitative Research. Qual Sociol 2019, 42, 139–160. [Google Scholar] [CrossRef]
- Taherdoost, H. What Are Different Research Approaches? Comprehensive Review of Qualitative, Quantitative, and Mixed Method Research, Their Applications, Types, and Limitations. j. of manag. sci. & eng. res. 2022, 5, 53–63. [Google Scholar] [CrossRef]
- Josephson, R.A.; Gillombardo, C.B. Cardiovascular Services in Covid-19 - Impact of the Pandemic and Lessons Learned. Progress in Cardiovascular Diseases 2023, 76, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, P.; Mahadevappa, M.; Alluri, S. COVID-19 Pandemic and the Impact on the Cardiovascular Disease Patient Care. CCR 2020, 16, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.F.; Alasnag, M.; Batchelor, W.B.; Sharma, A.; Luse, E.; Drewes, M.; Welt, F.G.; Itchhaporia, D.; Henry, T.D. The Ongoing National Medical Staffing Crisis: Impacts on Care Delivery for Interventional Cardiologists. Journal of the Society for Cardiovascular Angiography & Interventions 2022, 1, 100307. [Google Scholar] [CrossRef]
- Sadler, D.; DeCara, J.M.; Herrmann, J.; Arnold, A.; Ghosh, A.K.; Abdel-Qadir, H.; Yang, E.H.; Szmit, S.; Akhter, N.; Leja, M.; et al. Perspectives on the COVID-19 Pandemic Impact on Cardio-Oncology: Results from the COVID-19 International Collaborative Network Survey. Cardio-Oncology 2020, 6, 28. [Google Scholar] [CrossRef]
- Bhargava, S.; Sarkar, R.; Kroumpouzos, G. Mental Distress in Dermatologists during COVID-19 Pandemic: Assessment and Risk Factors in a Global, Cross-sectional Study. Dermatologic Therapy 2020, 33. [Google Scholar] [CrossRef] [PubMed]
- Samimi, S.; Choi, J.; Rosman, I.S.; Rosenbach, M. Impact of COVID-19 on Dermatology Residency. Dermatologic Clinics 2021, 39, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.; Dorrell, D.N.; Feldman, S.R.; Huang, W.W. The Impact of the Coronavirus Disease 2019 Pandemic on Dermatologist Burnout: A Survey Study. DOJ 2021, 27. [Google Scholar] [CrossRef] [PubMed]
- Helm, M.F.; Kimball, A.B.; Butt, M.; Stuckey, H.; Costigan, H.; Shinkai, K.; Nagler, A.R. Challenges for Dermatologists during the COVID-19 Pandemic: A Qualitative Study. International Journal of Women’s Dermatology 2022, 8, e013. [Google Scholar] [CrossRef] [PubMed]
- Elbarbary, N.S.; Dos Santos, T.J.; De Beaufort, C.; Wiltshire, E.; Pulungan, A.; Scaramuzza, A.E. The Challenges of Managing Pediatric Diabetes and Other Endocrine Disorders During the COVID-19 Pandemic: Results From an International Cross-Sectional Electronic Survey. Front. Endocrinol. 2021, 12, 735554. [Google Scholar] [CrossRef]
- Loscalzo, Y.; Marucci, S.; Garofalo, P.; Attanasio, R.; Lisco, G.; De Geronimo, V.; Guastamacchia, E.; Giannini, M.; Triggiani, V. Assessment of Burnout Levels Before and During COVID-19 Pandemic: AWeb-Based Survey by the (Italian) Association of Medical Endocrinologists(AME). EMIDDT 2021, 21, 2238–2252. [Google Scholar] [CrossRef]
- Agha, A.; Basu, A.; Anwar, E.; Hanif, W. Burnout among Diabetes Specialist Registrars across the United Kingdom in the Post-Pandemic Era. Front. Med. 2024, 11, 1367103. [Google Scholar] [CrossRef] [PubMed]
- Manzella, A.; Kravchenko, T.; Kheng, M.; Chao, J.; Laird, A.M.; Pitt, H.A.; Beninato, T. Effects of the COVID-19 Pandemic on Endocrine Operations in the United States. The American Journal of Surgery 2024, 228, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Di Monte, C.; Monaco, S.; Mariani, R.; Di Trani, M. From Resilience to Burnout: Psychological Features of Italian General Practitioners During COVID-19 Emergency. Front. Psychol. 2020, 11, 567201. [Google Scholar] [CrossRef] [PubMed]
- Kurzthaler, I.; Kemmler, G.; Holzner, B.; Hofer, A. Physician’s Burnout and the COVID-19 Pandemic—A Nationwide Cross-Sectional Study in Austria. Front. Psychiatry 2021, 12, 784131. [Google Scholar] [CrossRef] [PubMed]
- Ofei-Dodoo, S.; Loo-Gross, C.; Kellerman, R. Burnout, Depression, Anxiety, and Stress Among Family Physicians in Kansas Responding to the COVID-19 Pandemic. J Am Board Fam Med 2021, 34, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Kiliç, O.H.T.; Anil, M.; Varol, U.; Sofuoğlu, Z.; Çoban, İ.; Gülmez, H.; Güvendi̇, G.; Di̇Ri̇M Mete, B. Factors Affecting Burnout in Physicians during COVID-19 Pandemic. Ege Tıp Dergisi 2021, 60, 136–144. [Google Scholar] [CrossRef]
- Ekmektzoglou, K.; Tziatzios, G.; Siau, K.; Pawlak, K.M.; Rokkas, T.; Triantafyllou, K.; Arvanitakis, M.; Gkolfakis, P. Covid-19: Exploring the “New Normal” in Gastroenterology Training. AGEB 2021, 84, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.-J. Psychosocio-Economic Impacts of COVID-19 on Gastroenterology and Endoscopy Practice. Gastroenterology Report 2021, 9, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Marlicz, W.; Koulaouzidis, A.; Charisopoulou, D.; Jankowski, J.; Marlicz, M.; Skonieczna-Zydecka, K.; Krynicka, P.; Loniewski, I.; Samochowiec, J.; Rydzewska, G.; et al. Burnout in Healthcare – the Emperor’s New Clothes. pg 2023, 18, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Lacy, B.E.; Cangemi, D.J.; Burke, C.A. Burnout in Gastrointestinal Providers. Am J Gastroenterol 2024. [Google Scholar] [CrossRef]
- Elhadi, M.; Msherghi, A.; Elgzairi, M.; Alhashimi, A.; Bouhuwaish, A.; Biala, M.; Abuelmeda, S.; Khel, S.; Khaled, A.; Alsoufi, A.; et al. Burnout Syndrome Among Hospital Healthcare Workers During the COVID-19 Pandemic and Civil War: A Cross-Sectional Study. Front. Psychiatry 2020, 11, 579563. [Google Scholar] [CrossRef] [PubMed]
- Buran, F.; Altın, Z. Burnout among Physicians Working in a Pandemic Hospital during the COVID-19 Pandemic. Legal Medicine 2021, 51, 101881. [Google Scholar] [CrossRef] [PubMed]
- Macía-Rodríguez, C.; Alejandre De Oña, Á.; Martín-Iglesias, D.; Barrera-López, L.; Pérez-Sanz, M.T.; Moreno-Diaz, J.; González-Munera, A. Burn-out Syndrome in Spanish Internists during the COVID-19 Outbreak and Associated Factors: A Cross-Sectional Survey. BMJ Open 2021, 11, e042966. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Madrid, M.N.; Pastor-Moreno, G.; Albert-Lopez, E.; Pastor-Valero, M. “You Knew You Had to Be There, It Had to Be Done”: Experiences of Health Professionals Who Faced the COVID-19 Pandemic in One Public Hospital in Spain. Front. Public Health 2023, 11, 1089565. [Google Scholar] [CrossRef] [PubMed]
- Pivert, K.A.; Boyle, S.M.; Halbach, S.M.; Chan, L.; Shah, H.H.; Waitzman, J.S.; Mehdi, A.; Norouzi, S.; Sozio, S.M. Impact of the COVID-19 Pandemic on Nephrology Fellow Training and Well-Being in the United States: A National Survey. JASN 2021, 32, 1236–1248. [Google Scholar] [CrossRef] [PubMed]
- Nair, D.; Brereton, L.; Hoge, C.; Plantinga, L.C.; Agrawal, V.; Soman, S.S.; Choi, M.J.; Jaar, B.G.; Soman, S.; Jaar, B.; et al. Burnout Among Nephrologists in the United States: A Survey Study. Kidney Medicine 2022, 4, 100407. [Google Scholar] [CrossRef] [PubMed]
- Pawłowicz-Szlarska, E.; Forycka, J.; Harendarz, K.; Stanisławska, M.; Makówka, A.; Nowicki, M. Organizational Support, Training and Equipment Are Key Determinants of Burnout among Dialysis Healthcare Professionals during the COVID-19 Pandemic. J Nephrol 2022, 35, 2077–2086. [Google Scholar] [CrossRef] [PubMed]
- Selvaskandan, H.; Nimmo, A.; Savino, M.; Afuwape, S.; Brand, S.; Graham-Brown, M.; Medcalf, J.; Cockwell, P.; Beckwith, H. Burnout and Long COVID among the UK Nephrology Workforce: Results from a National Survey Investigating the Impact of COVID-19 on Working Lives. Clinical Kidney Journal 2022, 15, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Majersik, J.J.; Reddy, V.K. Acute Neurology during the COVID-19 Pandemic: Supporting the Front Line. Neurology 2020, 94, 1055–1057. [Google Scholar] [CrossRef]
- Ayele, R.; Macchi, Z.A.; Dini, M.; Bock, M.; Katz, M.; Pantilat, S.Z.; Jones, J.; Kluger, B.M. Experience of Community Neurologists Providing Care for Patients With Neurodegenerative Illness During the COVID-19 Pandemic. Neurology 2021, 97. [Google Scholar] [CrossRef]
- Goyal, T.; Probasco, J.C.; Gold, C.A.; Klein, J.P.; Weathered, N.R.; Thakur, K.T. Neurohospitalist Practice and Well-Being During the COVID-19 Pandemic. The Neurohospitalist 2021, 11, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, E.S.; Winsvold, B.S.; Sandset, E.C.; Storstein, A.M.; Faiz, K.W. Experiences, Distress and Burden among Neurologists in Norway during the COVID-19 Pandemic. PLoS ONE 2021, 16, e0246567. [Google Scholar] [CrossRef] [PubMed]
- Del Piccolo, L.; Donisi, V.; Raffaelli, R.; Garzon, S.; Perlini, C.; Rimondini, M.; Uccella, S.; Cromi, A.; Ghezzi, F.; Ginami, M.; et al. The Psychological Impact of COVID-19 on Healthcare Providers in Obstetrics: A Cross-Sectional Survey Study. Front. Psychol. 2021, 12, 632999. [Google Scholar] [CrossRef] [PubMed]
- Riggan, K.A.; Reckhow, J.; Allyse, M.A.; Long, M.; Torbenson, V.; Rivera-Chiauzzi, E.Y. Impact of the COVID-19 Pandemic on Obstetricians/Gynecologists. Mayo Clinic Proceedings: Innovations, Quality & Outcomes 2021, 5, 1128–1137. [Google Scholar] [CrossRef]
- Schmitt, N.; Mattern, E.; Cignacco, E.; Seliger, G.; König-Bachmann, M.; Striebich, S.; Ayerle, G.M. Effects of the Covid-19 Pandemic on Maternity Staff in 2020 – a Scoping Review. BMC Health Serv Res 2021, 21, 1364. [Google Scholar] [CrossRef] [PubMed]
- Bogaert, K.C.; Lieb, W.E.; Glazer, K.B.; Wang, E.; Stone, J.L.; Howell, E.A. Stress and the Psychological Impact of the COVID-19 Pandemic on Frontline Obstetrics and Gynecology Providers. Am J Perinatol 2022, 29, 1596–1604. [Google Scholar] [CrossRef] [PubMed]
- Al-Humadi, S.M.; Cáceda, R.; Bronson, B.; Paulus, M.; Hong, H.; Muhlrad, S. Orthopaedic Surgeon Mental Health During the COVID-19 Pandemic. Geriatr Orthop Surg Rehabil 2021, 12, 215145932110352. [Google Scholar] [CrossRef] [PubMed]
- Lazarides, A.L.; Belay, E.S.; Anastasio, A.T.; Cook, C.E.; Anakwenze, O.A. Physician Burnout and Professional Satisfaction in Orthopedic Surgeons during the COVID-19 Pandemic. WOR 2021, 69, 15–22. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Scarlat, M.M. Stress, Anxiety, and Burnout of Orthopaedic Surgeons in COVID-19 Pandemic. International Orthopaedics (SICOT) 2022, 46, 931–935. [Google Scholar] [CrossRef]
- Ambrosio, L.; Vadalà, G.; Russo, F.; Papalia, R.; Denaro, V. The Role of the Orthopaedic Surgeon in the COVID-19 Era: Cautions and Perspectives. J EXP ORTOP 2020, 7, 35. [Google Scholar] [CrossRef]
- Laventhal, N.T.; Basak, R.B.; Dell, M.L.; Elster, N.; Geis, G.; Macauley, R.C.; Mercurio, M.R.; Opel, D.J.; Shalowitz, D.I.; Statter, M.B.; et al. Professional Obligations of Clinicians and Institutions in Pediatric Care Settings during a Public Health Crisis: A Review. The Journal of Pediatrics 2020, 224, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Treluyer, L.; Tourneux, P. Burnout among Paediatric Residents during the COVID-19 Outbreak in France. Eur J Pediatr 2021, 180, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Nigri, L.; Carrasco-Sanz, A.; Pop, T.L.; Giardino, I.; Vural, M.; Ferrara, P.; Indrio, F.; Pettoello-Mantovani, M. Burnout in Primary Care Pediatrics and the Additional Burden from the COVID-19 Pandemic. The Journal of Pediatrics 2023, 260, 113447. [Google Scholar] [CrossRef] [PubMed]
- Rivas-García, A.; Míguez-Navarro, M.C.; Ferrero-García-Loygorri, C.; Marañón, R.; Vázquez-López, P. Burnout Syndrome in Paediatricians Working in Paediatric Emergency Care Settings. Prevalence and Associated Factors: A Multilevel Analysis. Anales de Pediatría (English Edition) 2023, 98, 119–128. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, E.L.; Poore, S.O. Slowing the Spread and Minimizing the Impact of COVID-19: Lessons from the Past and Recommendations for the Plastic Surgeon. Plastic & Reconstructive Surgery 2020, 146, 681–689. [Google Scholar] [CrossRef]
- Crowe, C.S.; Lopez, J.; Morrison, S.D.; Drolet, B.C.; Janis, J.E. ; On behalf of the Resident Council Wellness and Education Study Group The Effects of the COVID-19 Pandemic on Resident Education and Wellness: A National Survey of Plastic Surgery Residents. Plastic & Reconstructive Surgery 2021, 148, 462e–474e. [Google Scholar] [CrossRef]
- Shah, J.; Zhao, R.; Yi, J.; Otterburn, D.; Patel, A.; Szpalski, C.; Tanna, N.; Taub, P.J.; Weichman, K.E.; Ricci, J.A. Frontline Reporting from the Epicenter of a Global Pandemic: A Survey of the Impact of COVID-19 on Plastic Surgery Training in New York and New Jersey. Plastic & Reconstructive Surgery 2022, 149, 130e–138e. [Google Scholar] [CrossRef]
- Gologram, M.; Lomiguen, C.; Chin, J.; Terrell, M. Mental Health and Quality of Life Considerations: Plastic and Cosmetic Surgery During the COVID-19 Pandemic. Am J Cosmet Surg 2023, 40, 162–169. [Google Scholar] [CrossRef]
- Bojdani, E.; Rajagopalan, A.; Chen, A.; Gearin, P.; Olcott, W.; Shankar, V.; Cloutier, A.; Solomon, H.; Naqvi, N.Z.; Batty, N.; et al. COVID-19 Pandemic: Impact on Psychiatric Care in the United States. Psychiatry Research 2020, 289, 113069. [Google Scholar] [CrossRef]
- Alkhamees, A.A.; Assiri, H.; Alharbi, H.Y.; Nasser, A.; Alkhamees, M.A. Burnout and Depression among Psychiatry Residents during COVID-19 Pandemic. Hum Resour Health 2021, 19, 46. [Google Scholar] [CrossRef]
- Child and Adolescent Psychiatry Department, Ankara City Hospital, Ankara, Turkey; Ogutlu, H. ; McNicholas, F.; Child and Adolescent Psychiatry Department, University College of Dublin, Dublin, Ireland; Children Hospital Ireland, Crumlin, Dublin, Ireland; Lucena Rathgar, SJOG CAMHS, Dublin, Ireland; Turkcapar, H.; Psychology Department, Faculty of Social Sciences and Humanities, Social Sciences University of Ankara, Ankara, Turkey STRESS AND BURNOUT IN PSYCHIATRISTS IN TURKEY DURING COVID-19 PANDEMIC. Psychiat Danub 2021, 33, 225–230. [Google Scholar] [CrossRef]
- Yellowlees, P. Impact of COVID-19 on Mental Health Care Practitioners. Psychiatric Clinics of North America 2022, 45, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Demirjian, N.L.; Fields, B.K.K.; Song, C.; Reddy, S.; Desai, B.; Cen, S.Y.; Salehi, S.; Gholamrezanezhad, A. Impacts of the Coronavirus Disease 2019 (COVID-19) Pandemic on Healthcare Workers: A Nationwide Survey of United States Radiologists. Clinical Imaging 2020, 68, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Coppola, F.; Faggioni, L.; Neri, E.; Grassi, R.; Miele, V. Impact of the COVID-19 Outbreak on the Profession and Psychological Wellbeing of Radiologists: A Nationwide Online Survey. Insights Imaging 2021, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.L.; Chen, R.C.; Teo, I.; Chaudhry, I.; Heng, A.L.; Zhuang, K.D.; Tan, H.K.; Tan, B.S. A Survey of Anxiety and Burnout in the Radiology Workforce of a Tertiary Hospital during the COVID-19 Pandemic. J Med Imag Rad Onc 2021, 65, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Oprisan, A.; Baettig-Arriagada, E.; Baeza-Delgado, C.; Martí-Bonmatí, L. Prevalence of Burnout Syndrome during the COVID-19 Pandemic and Associated Factors. Radiología (English Edition) 2022, 64, 119–127. [Google Scholar] [CrossRef]
- Lazarus, R.S. Coping Theory and Research: Past, Present, and Future. Psychosomatic Medicine 1993, 55, 234–247. [Google Scholar] [CrossRef] [PubMed]
- Haan, N. A TRIPARTITE MODEL OF EGO FUNCTIONING VALUES AND CLINICAL AND RESEARCH APPLICATIONS: The Journal of Nervous and Mental Disease 1969, 148, 14–30. [CrossRef]
- Menninger, K. Regulatory Devices of the Ego under Major Stress. The International Journal of Psycho-Analysis 1954, 35, 412–420. [Google Scholar]
- Vaillant, G.E. Adaptation to Life; 1st Harvard University Press pbk. ed.; Harvard University Press: Cambridge, Mass, 1995; ISBN 978-0-674-00414-6. [Google Scholar]
- Lazarus, R.S. Fifty Years of the Research and Theory of R.S. Lazarus: An Analysis of Historical and Perennial Issues; LEA Lawrence Erlbaum Associates: Mahwah (N.J.) London, 1998; ISBN 978-0-8058-2657-9. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, 1984; ISBN 978-0-8261-4191-0. [Google Scholar]
- Lazarus, R.S. The Psychology of Stress and Coping. Issues in Mental Health Nursing 1985, 7, 399–418. [Google Scholar] [CrossRef]
- Folkman, S.; Moskowitz, J.T. Positive Affect and the Other Side of Coping. American Psychologist 2000, 55, 647–654. [Google Scholar] [CrossRef]
- Folkman, S. Personal Control and Stress and Coping Processes: A Theoretical Analysis. Journal of Personality and Social Psychology 1984, 46, 839–852. [Google Scholar] [CrossRef] [PubMed]
- Hunsinger, N.; Hammarlund, R.; Crapanzano, K. Mental Health Appointments in the Era of COVID-19: Experiences of Patients and Providers. TOJ 2021, 21, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Uscher-Pines, L.; Parks, A.M.; Sousa, J.; Raja, P.; Mehrotra, A.; Huskamp, H.A.; Busch, A.B. Appropriateness of Telemedicine Versus In-Person Care: A Qualitative Exploration of Psychiatrists’ Decision Making. PS 2022, 73, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Daniel, M.; Gordon, M.; Patricio, M.; Hider, A.; Pawlik, C.; Bhagdev, R.; Ahmad, S.; Alston, S.; Park, S.; Pawlikowska, T.; et al. An Update on Developments in Medical Education in Response to the COVID-19 Pandemic: A BEME Scoping Review: BEME Guide No. 64. Medical Teacher 2021, 43, 253–271. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).