Keywords colorectal neoplasm; robotic surgery; single-port
Introduction
Minimally invasive surgery (MIS) has been at the center of surgical field since the 1980s. Over the past four decades, surgical innovations have taken an enormous stride into the robotic platform. Among these advancements, DaVinci
® Single-Port Robotic Surgery (SPRS, Intuitive Surgical, Sunnyvale, CA) is at its utmost cutting edge system designed to enhance the performance of complex surgeries with minimal invasiveness. In addition to the benefits of ergonomics provided by the robotic system, SPRS provides additional benefits of cosmesis, reduced postoperative pain requiring analgesics, and reduced costs. [
1,
2,
3] With its clinical debut in 2018, the SPRS platform has been mainly used in urology, gynecology, and general surgery, such as cholecystectomy and adrenalectomy.[
4] However, its application in colorectal surgery was stagnant.
With its first report in 2020 by Marks
et al, SPRS for colectomy has gained momentum in many colorectal surgeons.[
5] Comparative studies between SPRS and single-incision laparoscopic surgery (SILS) have reported similar operation time, complication rates, and pathological outcomes confirming its safe and feasible use.[
6,
7] The hesitant application of SPRS in colorectal surgery pertain to rectal surgery due to the absence of stapling device and angulation. As the SPRS is currently approved for clinical use in United States, South Korea, and Japan, the authors appreciate the importance of sharing our experience and shedding light on ways to overcome some of the difficulties surrounding the SPRS.
Materials and Methods
Patient Selection
Data from patients, who underwent colorectal surgery using the DaVinci Single-Port (SP) robotic platform between May 2023 and December 2023 at the Gangnam Severance Hospital, Yonsei University College of Medicine (Seoul, Korea), were reviewed. A total number of 10 patients were analyzed.
Surgical Procedures
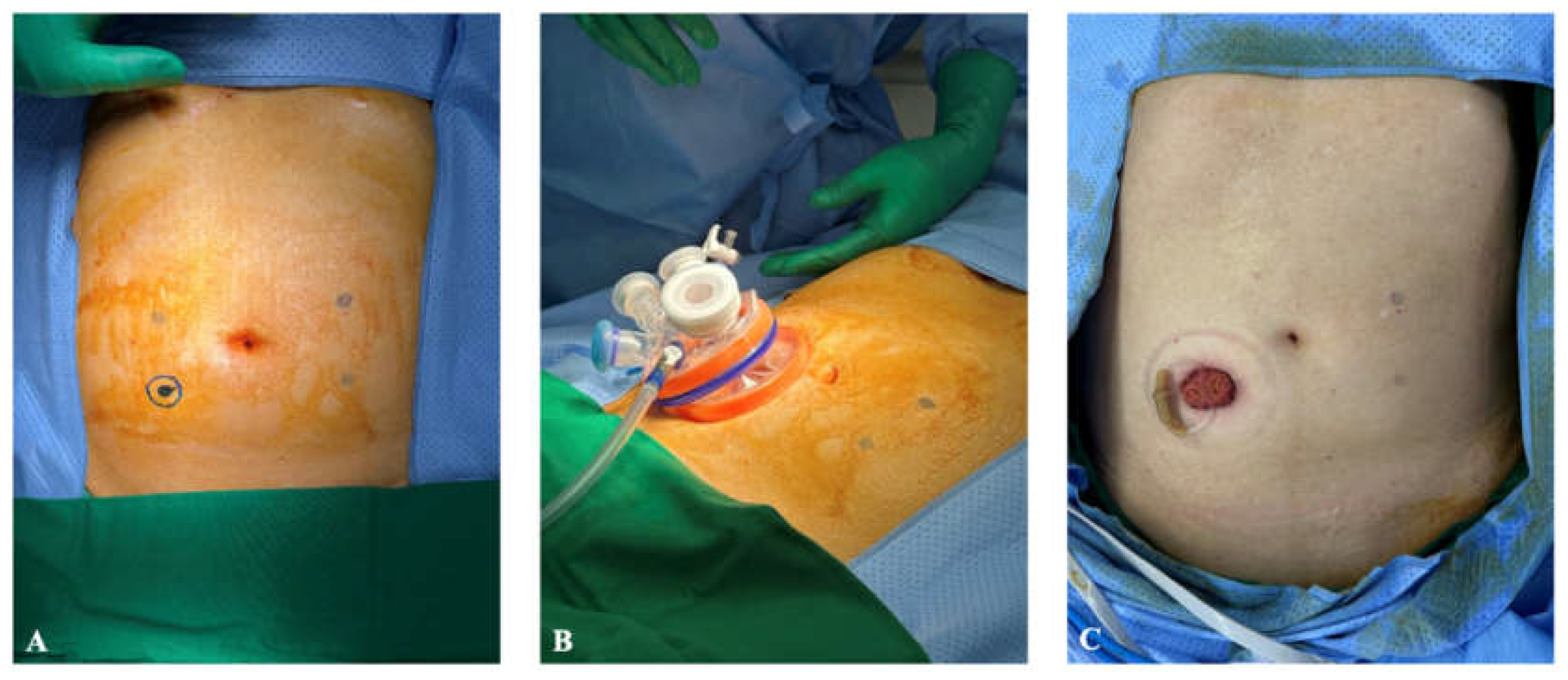
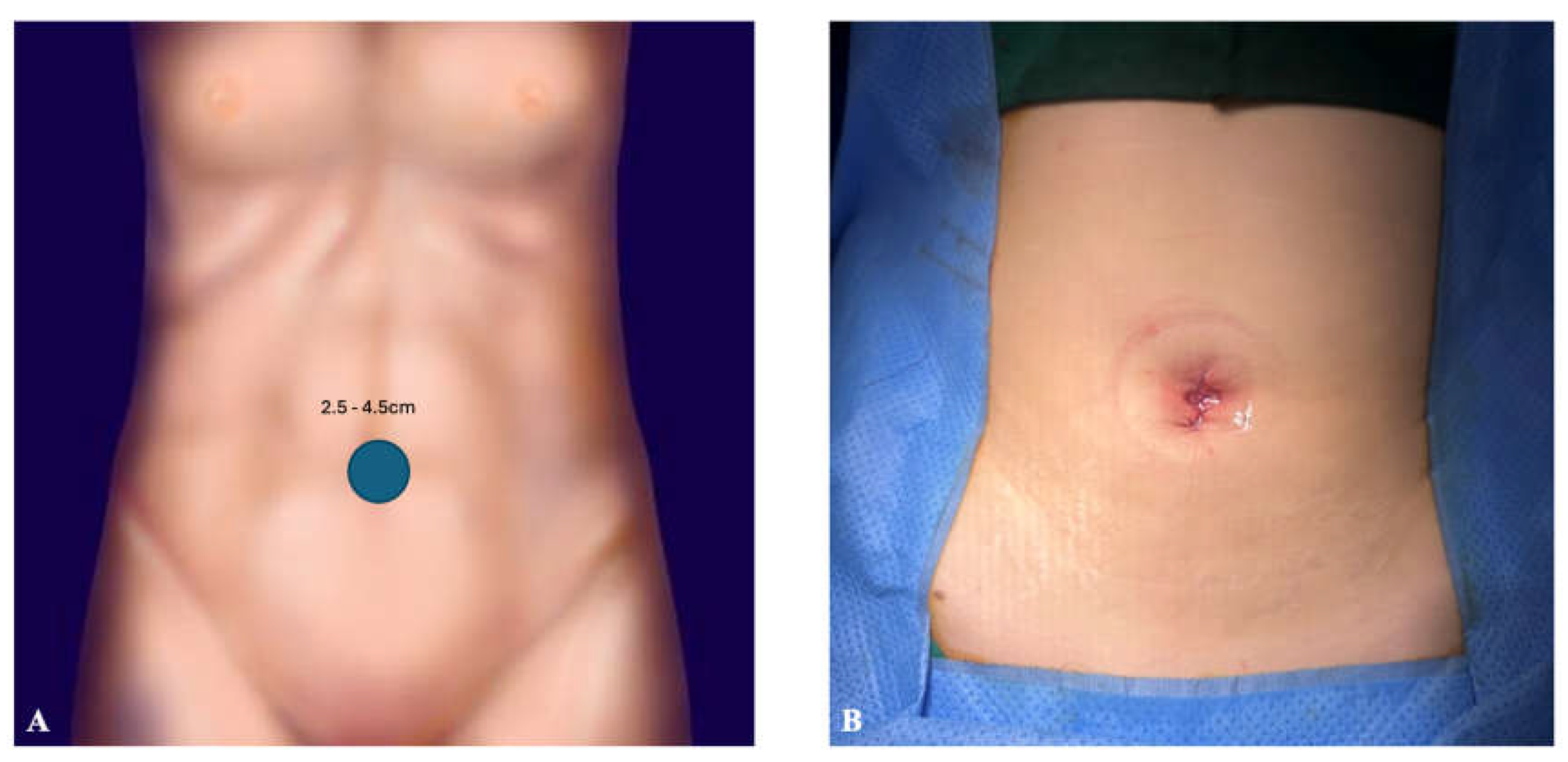
For right-sided colectomy, patient lied in a supine position. Transumbilical incision was made through which a 4-chamber SP glove port (MEDITECH INFRAMED, Seoul, Korea) was inserted. For left-sided colectomy, patient lied in a lithotomy position. Likewise, transumbilical incision was made for the glove port; however, for two ultra-low anterior resections, circular incision was made at right lower quadrant at the position of ileostomy maturation. Incisions can be visualized in
Figure 1 and
Figure 2. The SP robotic arms were positioned and docked from the ipsilateral side of the lesion.
There was one case of additional port inserted at right lower quadrant for low anterior resection. Laparoscopic stapler (SigniaTM, Medtronic, Minneapolis. USA) was inserted for distal margin resection and drain insertion. The other 9 cases were performed with a single incision.
For fascia closure, barbed suture (StratafixTM, Ethicon Inc., USA) was used with an absorbable, synthetic, barbed suture (3-0 vicryl*, Ethicon Inc., USA) and skin adhesive (Liquiband®, Advanced Medical Solutions Ltd., USA).
Measurement of Clinical Variables
Demographics of the patients including age, sex, American Society of Anesthesiologists (ASA) classification, and body mass index (BMI) were collected. Clinical data included the diagnosis of the patient for which surgery was performed, operation date, and discharge date were reviewed. Length of hospital stay (days) was defined as day of surgery to discharge date. Intraoperative results, such as operation time (min), wound size (cm), blood loss (mL), transfusion status, ileostomy status, wound location, as well as drain insertion status were analyzed. Patients graded the pain level using a numeric pain rating scale (NPRS, 1-10) daily and NPRS on postoperative day 1 and 3 were reviewed. The length of intravenous (IV) pain medication was also collected. After discharge, pathologic data was reviewed at outpatient clinic including tumor size, TNM stage, lymphovascular (LVI) and perineural invasion (PNI) status, and adjuvant chemotherapy status. Postoperative complication graded according to Clavien-Dindo classification was assessed. Median follow-up was 6.6months (range 2.6-9.4months).
Statistical Analysis
All analyses were performed using R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria,
https://www.r-project.org/). Data including perioperative parameters and postoperative outcomes were analyzed. Continuous variables were analyzed using t-test and are presented as means, medians, and standard deviations with a range. Categorical variables were analyzed using chi-square test or Fisher’s exact test presented as frequencies.
Results
Data from 10 patients (4 male [40%], 6 female [60%]; mean [± SD] age, 62.9 ± 9.6 years) were analyzed. Mean BMI was 22.87 ± 2.5, and ASA status varied (ASA 1, 1 (10%); ASA 2, 4 (40%); ASA 3, 5 (50%)). The diagnosis of the patients was divided into 9 (90%) colorectal cancer and 1 (10%) rectal gastrointestinal tumor. Surgical procedure was carried out according to the location of the lesion, arranging from two right hemicolectomies, five anterior resections, one low anterior resection, and two ultra-low anterior resections. One patient had double primary cancers at descending and sigmoid colon for which anterior resection was performed, and one patient underwent cholecystectomy in addition to anterior resection for primary sigmoid colon cancer. The baseline demographics of the patients are shown in
Table 1.
Mean operation time was 222.4 ± 66.1min (range 142-316min) with a mean blood loss of 148 ± 126.2ml (range 50-400ml). Two patients for whom ultra-low anterior resection were performed, single port incision was made at the right lower quadrant. Ileostomy was maturated for both patients at the end of the surgery through the single port site. (
Figure 1C) Transumbilical incision was made for the rest of the 8 patients, and the mean wound size was measured at 3.25 ± 0.6cm (range 2.5-4.5cm). (
Figure 2) No intraoperative blood transfusion was given. The average tumor size was 3.15 ± 1.9cm (range 1.2-6.9). Four patients underwent adjuvant chemotherapy, and the pathologic stage of the patients are shown in
Table 2.
Median NPRS on postoperative day 1 and 3 were 3 (range 2-3) on both days. No patients required IV pain medication after 2 days. Mean hospital stay was 6 ± 1.2days (range 4-8days), and no readmission within 30 days was noted. One patient had grade II complication for which blood transfusion was required for low hemoglobin level (6.9g/dL). The patient was discharged on postoperative day 5 without any sequelae. The results abovementioned are shown in
Table 3.
Discussion
Our exploration into the application of the SPRS system for colorectal procedures has illuminated several critical insights. The system's integration into colorectal surgery represents a significant advancement in MIS, echoing the broader shift towards robotics in the surgical field. The utilization of SPRS in colorectal surgery, while initially hesitant, has seen a burgeoning interest following reports of its successful application in colectomy.
The ergonomics of the robotic platform is an undisputable advantage compared to the laparoscopic platform.[
8] Through this benefit, Eisenberg
et al reported a significantly shorter suturing time in the robot system than the standard laparo-endoscopic single-site surgery (
P<0.0001).[
9] The risk of bypassing drain insertion, especially for low anterior resection may hold some risk. However, intracorporeal reinforce suture of the anastomosis using the robotic system can reduce the possible occurrence of anastomosis leakage. A recent systematic review and meta-analysis by Wang
et al demonstrated a lower incidence of anastomosis leakage (RR 0.41, 95% CI 0.25-0.66) in patients with reinforcing sutures with a leakage rate of 4.4% compared to the 11.9% for whom no reinforce suture was performed.[
10]
Our data align with the existing literature that compares SPRS with single-incision laparoscopic surgery (SILS), showing comparable operation times [
6,
7]. Our mean operation time of 222.4min is longer than that reported by Change
et al (185min) but shorter than the comparative analysis performed by Keller
et al (296min). We reported one case of grade II Clavien-Dindo complication of postoperative anemia (Hg 6.9g/dL) requiring transfusion. However, the initial hemoglobin level of the patient was low (8.5g/dL) with hematocrit of 28.1% (normal range 37-47%). The patient was discharged without any sequelae on postoperative day 5. There were no readmissions within 30 days.
The mean wound size of 3.25cm was comparable to all other studies regarding SPRS colectomy. Lim et al reported a transumbilical incision length of 4-6 cm, and Bae
et al reported 5.0cm.[
11,
12] Initial experience by Marks
et al reported an incision length of 4.0 and 4.5cm in SPRS.[
5] Our transumbilical wound incision length of 3.25cm is one of the shortest incision length yet to report, emphasizing the cosmetic benefit of SPRS.
The comparative analysis of length of hospital stays, postoperative pain levels, and the limited need for IV pain medication post-surgery attests to the SP system's advantage in enhancing patient recovery experiences. Mean length of hospital stay was 6 days comparable to the 2-9 days reported by a recent systemic review of SPRS for colonic disease.[
13] Forty percent (4/10) patients did not require any IV analgesic after the day of operation. Two patients required IV pain control up to postoperative day 1, and the rest (40%) up to postoperative day 2. These findings coincide with the overarching goals of MIS to reduce hospitalization duration and expedite patient recovery, pivotal in the current healthcare landscape focused on patient-centered outcomes and cost-efficiency. The median follow-up of 6.6 months, although limited, provides an initial glance at the postoperative trajectory, with outcomes suggesting a positive recovery profile.
The SP system has some drawbacks. Due to the absence of SP-synced stapler, additional trocar is often inserted for such use. The resection of the distal margin in upper to middle rectal cancer using the laparoscopic stapling device using the same single port trocar site may be difficult due to the angle of the device and the narrow space of the pelvic cavity. Many of the studies reporting single-incision robotic colectomies often use an additional port for such reason.[
11,
14,
15] In our study, two patients had drain insertions. First patient was our first colectomy using the SP robotic platform, and the drain was inserted through the umbilical incision site. The second patient was diagnosed with rectal cancer for whom low anterior resection was performed. An additional port was inserted at right lower quadrant through which the assistant used laparoscopic stapler for distal margin resection, and drain was inserted through the additional port at the end of the surgery. Although the recent rise in the use of Enhanced Recovery After Surgery (ERAS) protocol strongly recommends no drainage of the peritoneal cavity and pelvis after colorectal surgery, the role of early detection of anastomosis leakage hinders many surgeons from relinquishing the procedure.[
16] In order to compensate for such burden, for patients with upper to middle rectal cancer for whom low anterior resection is required, a drain may be inserted through the additional port. Based on our experience, we suggest that optimal indications for a true SPRS may include early-stage colorectal cancers located from the cecum to the rectosigmoid junction. This range facilitates the use of a stapler for resection through the single-port site. Furthermore, for cases of low rectal cancer where a diverting ileostomy is necessary, an incision in the right lower quadrant may represent an additional appropriate indication for SPRS.
The most remarkable benefit of SPRS is the ability to perform multi-quadrant operation with a single incision. To our knowledge, other than a case report shared by Juo
et al, no other attempts have been reported on performing subtotal or total colectomy using a single incision.[
17] Patients with inflammatory bowel disease (IBD), such as ulcerative colitis requiring total proctocolectomy may benefit from a single incision, and the advancement of IBD surgery is open for advancement with the SPRS once doors open with FDA approval in the US as well as adoption of SPRS in Europe this year.[
18]
Despite these promising results, our study had several limitations, the first of which was the inherent constraints of its retrospective design. The relatively small sample size may also constrain the generalizability of the findings. Up to date, all reported findings regarding colectomy using SPRS are from case studies. Future research should aim to expand on these preliminary insights through multicenter trials and larger patient cohorts, exploring long-term outcomes and further delineating the criteria for patient selection to optimize benefits.
Conclusions
Overall, our experience with single-port robotic colorectal surgery has been promising. With only one patient with additional port for drain insertion, all nine patients underwent SP-robotic surgery with single incision for colon as well as rectal surgeries. Compared to an average postoperative length of stay of 6.5-8 days in laparoscopic colorectal surgeries reported in literature, SP-robotic surgery showed faster recovery of 6 days highlighting its benefits in patient recovery and satisfaction.
Author Contributions
Hye Jung Cho (HJC) and Woo Ram Kim (WRK) have contributed to the design, data collection, methodology, analysis, as well as writing and reviewing of the manuscript. All authors (HJC and WRK) have read and approved the manuscript.
Funding
The authors have no funding to declare.
Institutional Review Board Statement
This study was approved by the Institutional Review Board and Ethics Committees of Yonsei Severance Hospital (IRB No. 3-2023-0449) and was conducted according to the principles of the Declaration of Helsinki. A written informed consent was not required for this retrospective study.
Conflict of Interest
The authors declare no actual or potential conflicts of interest.
References
- Kudsi, O.Y.; Castellanos, A.; Kaza, S.; McCarty, J.; Dickens, E.; Martin, D.; Gonzalez, A.; et al. Cosmesis, patient satisfaction, and quality of life after da Vinci Single-Site cholecystectomy and multiport laparoscopic cholecystectomy: short-term results from a prospective, multicenter, randomized, controlled trial. Surg Endosc. 2017, 31, 3242–3250. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, A.; Pugliese, L.; Vinci, A.; Peri, A.; Tinozzi, F.P.; Cavazzi, E.; Klersy, C.; et al. Short-term outcomes of single-site robotic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective, randomized, double-blind trial. Surg Endosc. 2016, 30, 3089–3097. [Google Scholar] [CrossRef] [PubMed]
- Su, W.L.; Huang, J.W.; Wang, S.N.; Lee, K.T. Comparison study of clinical outcomes between single-site robotic cholecystectomy and single incision laparoscopic cholecystectomy. Asian J Surg. 2017, 40, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Cianci, S.; Rosati, A.; Rumolo, V.; Gueli Alletti, S.; Gallotta, V.; Turco, L.C.; Uccella, S.; et al. Robotic Single-Port Platform in General, Urologic, and Gynecologic Surgeries: A Systematic Review of the Literature and Meta-analysis. World J Surg. 2019, 43, 2401–2419. [Google Scholar] [CrossRef]
- Marks, J.H.; Salem, J.F.; Anderson, B.K.; Josse, J.M.; Schoonyoung, H.P. Single-port robotic left colectomy: first clinical experience using the SP robot (rSILS). Tech Coloproctol. 2020, 24, 57–63. [Google Scholar] [CrossRef]
- Chang, T.C.; Lin, E.K.; Lu, Y.J.; Huang, M.T.; Chen, C.H. Single-incision robotic colectomy versus single-incision laparoscopic colectomy: A matched case control study. Asian J Surg. 2021, 44, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Keller, D.S.; Reif de Paula, T.; Ikner, T.P.; Saidi, H.; Schoonyoung, H.J.H.M. Perioperative outcomes for single-port robotic versus single-incision laparoscopic surgery: a comparative analysis in colorectal cancer surgery. Surg Endosc. 2024, 38, 1568–1575. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.I.; Lee, M.R.; Green, I.; Allaf, M.; Marohn, M.R. Surgeons’ physical discomfort and symptoms during robotic surgery: a comprehensive ergonomic survey study. Surgical Endoscopy. 2017, 31, 1697–1706. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Vidovszky, T.J.; Lau, J.; Guiroy, B.; Rivas, H. Comparison of robotic and laparoendoscopic single-site surgery systems in a suturing and knot tying task. Surg Endosc. 2013, 27, 3182–3186. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, Y.; Tao, S.; Liu, Y.; Shi, Y.; Guan, J.; Liu, M. Efficacy of reinforcing sutures for prevention of anastomotic leakage after low anterior resection for rectal cancer: A systematic review and meta-analysis. Cancer Rep (Hoboken). 2024, 7, e1941. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.U.; Jegon, W.K.; Baek, S.K. Single plus one-port robotic surgery using the da Vinci Single-Site Platform versus conventional multi-port laparoscopic surgery for left-sided colon cancer. Wideochir Inne Tech Maloinwazyjne. 2022, 17, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Yun, S.H.; Lee, W.Y.; Kim, H.C.; Cho, Y.B.; Huh, J.W.; Shin, J.K.; et al. Single-port laparoscopic versus single-port robotic right hemicolectomy: Postoperative short-term outcomes. Int J Med Robot. 2023, 19, e2509. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.U.; Jeong, W.K.; Baek, S.K. Current status of robotic single-port colonic surgery. Int J Med Robot. 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Wei, P.L.; Huang, Y.J.; Wang, W.; Huang, Y.M. Comparison of robotic reduced-port and laparoscopic approaches for left-sided colorectal cancer surgery. Asian J Surg. 2023, 46, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Hu, Y.; Chen, X.; He, S.; Zhou, X. The application of a robotic single-incision plus one-port laparoscopic total colectomy with fascia space priority for slow-transit constipation - A video vignette. Colorectal Dis. 2023, 25, 824–825. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, U.O.; Scott, M.J.; Hubner, M.; Nygren, J.; Demartines, N.; Francis, N.; Ljungqvist, O.; et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS®) Society Recommendations: 2018. World Journal of Surgery. 2019, 43, 659–695. [Google Scholar] [CrossRef] [PubMed]
- Juo, Y.Y.; Obias, V. Robot-assisted single-incision total colectomy: a case report. Int J Med Robot. 2015, 11, 104–108. [Google Scholar] [CrossRef]
- Ditonno, F.; Licari, L.C.; Franco, A.; Bologna, E.; Manfredi, C.; Soputro, N.A.; Autorino, R.; et al. Current Expectations and Opinions on Single-port Robotic Surgery: A Survey Among European Experts by the SPARC Collaborative Group. Eur Urol Open Sci. 2024, 60, 54–57. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).