Submitted:
27 March 2024
Posted:
28 March 2024
You are already at the latest version
Abstract
Keywords:
Background
Noncommunicable Disease (NCD) Risk Factors
Incidence and Cost of Noncommunicable Diseases (NCDs)
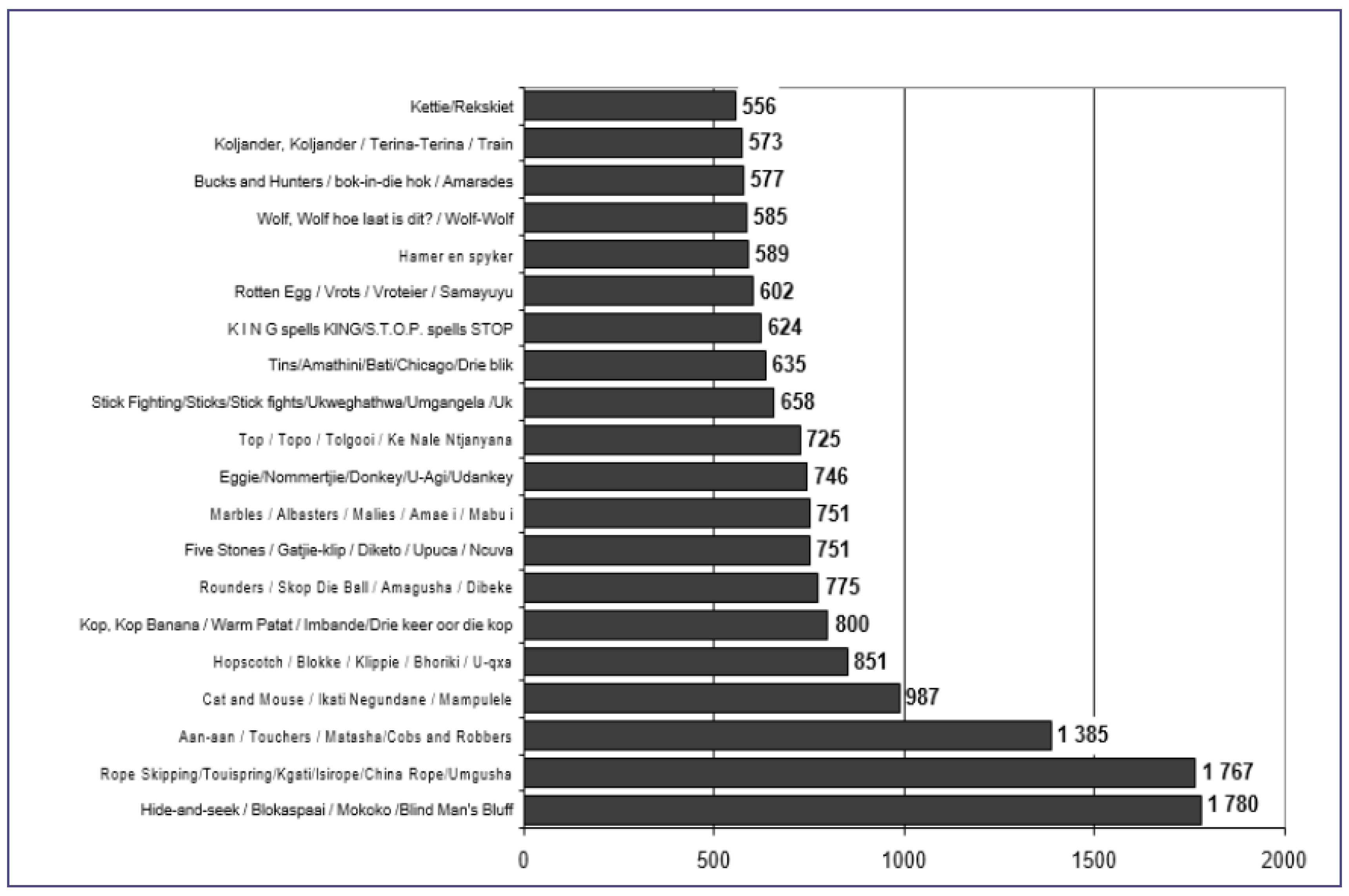
Indigenous Knowledge and Practices: Taxonomy of Indigenous Games
Indigenous Games and Non-Communicable Diseases
Importance of Indigenous Games as an Exercise Intervention for Non-Communicable Diseases (NCDs)
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, et al. (2020) Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors 8. [CrossRef]
- Bolarinwa O, Olagunju OS, Budu E, Seidu AA, Odetokun IA, et al. (2020) Prevalence of Non-Communicable Diseases and Associated Factors in South Africa: Evidence from National Income Dynamics Survey, 20082017. Research Square.
- Wong EB, Olivier S, Gunda R, Koole O, SurujdeenA, et al. (2021) Convergence of Infectious and NonCommunicable Disease Epidemics in Rural South Africa: A Cross-sectional, Population-based Multimorbidity Study. The Lancet Global Health 9: 967-976.
- Godward S (2023) Adult Public Health and Non-Communicable Diseases. Essential Public Health: Theory and Practice 231.
- Hunter DJ, Reddy KS (2013) Noncommunicable Diseases. New England Journal of Medicine 369: 1336-1343.
- Countdown NCD (2022) NCD Countdown 2030: Efficient Pathways and Strategic Investments to Accelerate Progress towards the Sustainable Development Goal Target 3.4 in Low-Income and Middle-Income Countries. Lancet (London, England) 399: 1266.
- Gumede M (2022) Development of a Policy Framework for the Establishment of Physical Exercise Programmes in Reducing Non-Communicable Diseases in the Province of KwazuluNatal, South Africa (Doctoral Dissertation).
- Famogun BU (2023) Lived Experiences of African American Men with Type 2 Diabetes Living in Rural Areas (Doctoral dissertation, Walden University).
- Shandu NM, Mathunjwa ML, Shaw BS (2023) Effects of High-Intensity Interval Training and Continuous Aerobic Training on Health-Fitness, Health Related Quality of Life, and Psychological Measures in College-Aged Smokers. International Journal of Environmental Research and Public Health 20: 653.
- O’Brien N, Li E, Chaibva CN, Gomez Bravo R, Kovacevic L, et al. (2023) Strengths, Weaknesses, Opportunities, and Threats Analysis of the Use of Digital Health Technologies in Primary Health Care in the Sub-Saharan African Region: Qualitative Study. J of Med Int Res 25: 45224. [CrossRef]
- Rakers MM, van Os HJ, Recourt K, Mosis G, Chavannes NH, et al. (2023) Perceived Barriers and Facilitators of Structural Reimbursement for Remote Patient Monitoring, A Exploratory Qualitative Study. Health Policy and Technology 12: 100718.
- Diab P, Flack P (2013) Benefits of Community-Based Education to the Community in South African Health Science Facilities. The African Journal of Primary Health Care & Family Medicine 5: 474.
- Rocha RO, Takahashi ARW, Segatto AP (2023) How does Social Innovation Generate Social Impact?: Contributions from a Meta-synthesis. Revista de Empreendedorismo e Gestão de Pequenas Empresas 12: 3.
- Aparicio-Rodríguez YD, Alonso-Morillejo E, García-Torrecillas JM (2023) Epidemiological Situation of High-Prevalence Non-Communicable Diseases in Spain: A Systematic Review. Journal of Clinical Medicine 12: 7109.
- Reynales-Shigematsu LM, Barnoya J, Cavalcante T, Aburto TC, Romieu I, et al. (2023) Latin America and the Caribbean Code Against Cancer 1st edition: Tobacco and Nicotine-related Products, Second-hand Smoke, and Alcohol and Cancer. Cancer Epidemiology 86: 102413.
- Saina S, Senthil P, Prakash O (2023) Burden of Illness, Risk Factor and Physical Activity in Cardiovascular Disease-A Review. Biomedicine 43: 1080-1093.
- Shaw I, Shaw BS, Krasilshchikov O (2009) Comparison of Aerobic and Combined Aerobic and Resistance Training on Low-density Lipoprotein Cholesterol Concentrations in Men: Cardiovascular Topic. Cardiovascular Journal of Africa 20: 290-295.
- Peto R, Lopez AD (2004) The Future Worldwide Health Effects of Current Smoking Patterns. Tobacco and Public Health: Science and Policy 281-286.
- Shandu NM, Mathunjwa ML, Shaw BS, Shaw I. (2023) Effects of High-Intensity Interval Training on Health-Fitness, Health Related Quality of Life, and Psychological Measures in College-aged Smokers. Journal of. Physical. Education and Sport 23: 200-209.
- Shandu NM, Mathunjwa ML, Shaw I (2023) Exercise Effects on Health-Related Quality of Life (HRQOL), Muscular Function, Cardiorespiratory Function, and Body Composition in Smokers: A Narrative Review. International Journal of Environmental Research and Public Health 20: 6813.
- Kolci KÜBRA, Garipkuş SN, Rengin REİS (2023) Thirdhand Smoke Exposure and its Toxicological Impacts: A Review on Target Organ-based Studies. Fabad Journal of Pharmaceutical Sciences 48: 303-318.
- Hendriks T, van Dijk R, Alsabaan NA, Harst PV (2020) Active Tobacco Smoking Impairs Cardiac Systolic Function. Scientific Reports 10: 6608.
- Qian Y, Ye D, Wu DJ, Feng C, Zeng Z, et al. (2019) Role of Cigarette Smoking in the Development of Ischemic Stroke and its Subtypes: A Mendelian Randomization Study. Clinical Epidemiology 11: 725-731. [CrossRef]
- Choudhary S, Gupta A, Kumari S (1995) Impact of Smoking and Alcohol Consumption on Blood Pressure and Anthropometric Parameters. Hip 7.
- Kugbey N (2023) Prevalence and Correlates of Substance Use Among School-Going Adolescents (11-18years) in Eight Sub-Saharan Africa Countries. Substance abuse treatment, prevention, and policy 18: 44.
- Britton M, Derrick JL, Shepherd JM, Haddad S, Garey L, et al. (2021). Associations Between Alcohol Consumption and Smoking Variables among Latinx Daily Smokers. Addictive behaviours 113: 106672. [CrossRef]
- Jee Y, Park S, Yuk E, Cho SI (2021) Alcohol Consumption and Cigarette Smoking among Young Adults: An Instrumental Variable Analysis Using Alcohol Flushing. Int J of Environ Res Pub Health 18: 11392.
- Maserumule OM, Skaal L, Sithole SL (2019) Alcohol Use Among High School Learners in Rural Areas of Limpopo Province. S Afr J Psychiatr 25: 1183.
- Leslie HH, Ahern J, Pettifor AE, Twine R, Kahn K, et al. (2015) Collective Efficacy, Alcohol Outlet Density, and Young Men’s Alcohol Use in Rural South Africa. Health Place 34: 190-198.
- Peltzer K (2006) Prevalence of alcohol use by rural primary care outpatients in South Africa. Psychological Reports 99: 176-178.
- Boua PR, Soo CC, Debpuur C, Maposa I, Nkoana S, et al. (2021) Prevalence and Socio-Demographic Correlates of Tobacco and Alcohol Use in Four Sub-Saharan African Countries: A Cross-Sectional Study of Middle-Aged Adults. BMC Public Health 21: 1126. [CrossRef]
- Popova S, Charness ME, Burd L, Crawford A, Hoyme HE, et al. (2023) Fetal Alcohol Spectrum Disorders. Nature Reviews Disease Primers 9: 11.
- Pisa PT, Vorster HH, Kruger A, Margetts B, Loots du T (2015) Association of Alcohol Consumption with Specific Biomarkers: A Cross-Sectional Study in South Africa. Journal of Health, Population and Nutrition 33: 146-156.
- Yun M, Kim E (2022) Gender Difference in the Association Between Alcohol Consumption and Depressive Symptoms among the Elderly in Rural Areas. Journal of Ethnicity in Substance Abuse 21: 36-54.
- Cibich M, Hines S, Carey TA (2023) Effectiveness of Strategies to Reduce Risky Alcohol Consumption among Youth Living in Rural or Remote Areas: A Systematic Review. JBI evidence synthesis 10: 11124.
- Ebling SBD, Silva MRSD (2020) Alcohol Consumption among Women Living in Rural Contexts. Revista Brasileira de Enfermagem 73.
- Karthijekan K, Cheng HY (2022) Effectiveness of a Motivated, Action-Based Intervention on Improving Physical Activity Level, Exercise Self-Efficacy and Cardiovascular Risk Factors of Patients with Coronary Heart Disease in Sri Lanka: A Randomized Controlled Trial Protocol. Plos one 17: 0270800. [CrossRef]
- Kruger HS, Venter CS, Vorster HH (2003) Physical Inactivity as a Risk Factor for Cardiovascular Disease in Communities Undergoing Rural to Urban Transition: The THUSA Study: Cardiovascular Topics. Cardiovasc J of S Afri 14: 16-23.
- Neethling I, Lambert EV, Cois A, Roomaney RA, Awotiwon OF, et al. (2022) Estimating the Changing Burden of Disease Attributable to Low Levels of Physical Activity in South Africa for 2000, 2006 And 2012. S Afri Med J 112: 639-648.
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, et al. (2012) Effect of Physical Inactivity on Major NonCommunicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 380: 219229. [CrossRef]
- Malambo P, Kengne AP, Lambert EV, De Villiers A, De Villiers A (2016) Prevalence and Socio-demographic Correlates of Physical Activity Levels among South African Adults in Cape Town and MountFrere Communities in 2008-2009. Arch Public Health 74: 54.
- Oyeyemi AL, Moss SJ, Monyeki MA (2016) Measurement of Physical Activity in Urban and Rural South African Adults: A Comparison of Two Self-Report Methods. BMC Public Health 16: 1-13.
- Ajaero CK, De Wet N, Odimegwu CO (2020) Integrating Rural–Urban Differentials in the Appraisal of Prevalence and Risk Factors of Non-Communicable Diseases in South Africa. GeoJournal 1-15.
- Mlangeni L, Makola L, Naidoo I, Chibi B, Sokhela Z, et al. (2018) Factors Associated with Physical Activity in South Africa: Evidence from a National Population-Based Survey. Open Pub Health J 11: 1. [CrossRef]
- Monyeki KD (2021) Selected Papers from the 2nd Ellisras Longitudinal Study and Other NonCommunicable Diseases Studies International Conference” Special Issue Editorial Children 8: 146.
- Mphekgwana PM, Monyeki KD, Mothiba TM, Makgahlela M, Kgatla K, et al. (2022) Screening and Interventions for Cardiovascular Disease Prevention in the Limpopo Province, South Africa: Use of the Community Action Model. Metabolites 12: 1067.
- Omotoso KO (2022) Inequalities in Household Food Expenditures in South Africa: Implications for the Burden of Non-Communicable Diseases (NCDs) and Health Inequality. Afri J of Develop Studies 12: 225.
- Mungal-Singh V (2011) United Nations High Level Meeting and NCD in South Africa. Glob Heart 4: 215-217.
- Sharma JR, Mabhida SE, Myers B, Apalata T, Nicol E, et al. (2021) Prevalence of Hypertension and Its Associated Risk Factors in a Rural Black Population of Mthatha Town, South Africa. International Journal of Environmental Research and Public Health 18: 1215.
- Mitchell J, Bradley C (2006) Quality Of Life in Age-Related Macular Degeneration: A Review of the Literature. Health Qual Life Outcomes 4: 97.
- Marquez PV, Farrington, JL (2013) The Challenge of Non-Communicable Diseases and Road Traffic Injuries in Sub-Saharan Africa: An Overview. Washington DC: World Bank.
- Barnes RY, Jelsma J, Parker R (2019) Improvements in Health-Related Quality of Life and Function in Middle-Aged Women with Chronic Diseases of Lifestyle after Participating in A Non-Pharmacological Intervention Programme: A Pragmatic Randomised Controlled Trial. African Journal of Disability 8: 1-14.
- Igwesi-Chidobe CN, Godfrey EL, Kengne AP (2015) Effective Components of Exercise and Physical Activity-related Behaviour-Change Interventions for Chronic Non-Communicable Diseases in Africa: Protocol for a Systematic Mixed Studies Review with Meta-analysis. BMJ open 5: 008036.
- Sparling PB, Owen N, Lambert EV, et al. (2000) Promoting Physical Activity: The New Imperative for Public Health. Health Education Research 15: 367-376. [CrossRef]
- Igwesi-Chidobe CN, Godfrey EL, Kitchen S, Onwasigwe CN, Sorinola IO (2019) Community-based Selfmanagement of Chronic Low Back Pain in a Rural African Primary Care Setting: A Feasibility Study. Primary Health Care Research & Development 20: 45.
- Santos AC, Willumsen J, Meheus F, Ilbawi A, Bull FC, et al. (2023) The Cost of Inaction on Physical Inactivity to Public Health Care Systems: A Population-Attributable Fraction Analysis. The Lancet Global Health 11: 32-39. [CrossRef]
- Wang H, Zeng W, Kabubei KM, Rasanathan JJK, Kazungu J, et al. (2023) Modelling the Economic Burden of SARSCoV-2 Infection in Health Care Workers in Four Countries. Nature Communications 14: 2791. [CrossRef]
- Narayan KV, Ali MK, Koplan JP (2010) Global Noncommunicable Diseases-Where Worlds Meet. New England Journal of Medicine 363: 11961198.
- Riza Y, Budiarto W, Haksama S, Kuntoro K, Yudhastuti R, et al. (2023) Health Services for Catastrophic Patients Through the National Health Insurance Program: Literature Review. Journal of Public Health in Africa 14: 2559. [CrossRef]
- Jauhari S, Pandit P, Agarwal M, Bajpai M, Kumar P, et al. (2023) Effectiveness of Educational Interventions on Knowledge and Behavioural Practices of Adolescents for Prevention of Non-Communicable Diseases in Low-and Middle-income Countries: A Systematic Review protocol. Int J of Noncommunicable Dis 8: 110-114.
- Evans RW, Smith T, Kay P, McWade D, Angouras N, et al. (2016) The Need for Biokineticists in the South African Public Health Care System. South African Journal of Sports Medicine 28: 85-86.
- Morris LD, Grimmer KA, Twizeyemariya A, Coetzee M, Leibbrandt DC, et al. (2021) Health System Challenges Affecting Rehabilitation Services in South Africa. Disability and Rehabilitation, 43: 877-883. [CrossRef]
- Zungu NP, Mabaso ML, Kumalo F, Sigida S, Wabiri N, et al. (2019) Prevalence of Non-Communicable Diseases (NCDs) and Associated Factors among HIV Positive Educators: Findings from the 2015/6 Survey of Health of Educators in Public Schools in South Africa. PLoS One 14: 0209756.
- Department of Health (2013) Strategic Plan for the Prevention and Control of NonCommunicable Diseases 2013-17. Department of Health, South Africa.
- McGregor D, Latulippe N, Whitlow R, Leora Gansworth K, McGregor L, et al. (2023) Towards Meaningful Research and Engagement: Indigenous Knowledge Systems and Great Lakes Governance. Journal of Great Lakes Research 49: 22-31. [CrossRef]
- Sibandze GF, Dludlu MN (2023) Interfacing Indigenous Knowledge with Scientific Knowledge for Improved Health Outcomes: Lessons from Eswatini. In Socio-Ecological Systems and Decoloniality: Convergence of Indigenous and Western Knowledge 33-49.
- Bucea-Manea-Țoniș R, Păun DG, Mîndrescu V (2023) A Managerial Perspective on Physical Education and Sports. Cambridge Scholars Publishing.
- Maspul KA, Almalki FA (2023) Preserving Local Wisdom: Unaizah’s Coffee Culture and Dates Farming Sustaining Cultural Heritage. J-CEKI: J Cendekia Ilmiah 2: 639-664.
- Burnett C, Hollander WJ (2004) The South African Indigenous Games Research Project of 4802001/2002. South African Journal for Research in Sport, Physical Education and Recreation 26: 9-23.
- Spires M, Delobelle P, Sanders D (2016) Diet-related Non-Communicable Diseases in South Africa: Determinants and Policy Responses. South African Health Review 2016: 35-42.
- Rasmus SM, Whitesell NR, Mousseau A, Allen J, et al. (2020) An Intervention Science to Advance Underrepresented Perspectives and Indigenous Self-Determination in Health. Prevention Science 21: 83-92. [CrossRef]
- Calzada I (2023) Smart Rural Communities: Action Research in Colombia and Mozambique. Sustainability 15: 9521.
- Ndubuisi NE (2021) Noncommunicable Diseases Prevention in Lowand Middle-Income Countries: An Overview of Health in All Policies (HiAP). Inquiry 58.
- Cole A, Pethan J, Evans J (2023) The Role of Agricultural Systems in Teaching Kitchens: An Integrative Review and Thoughts for the Future. Nutrients 15: 4045.
- Walter M, Suina M (2023) Indigenous Data, Indigenous Methodologies and Indigenous Data Sovereignty. Educational Research Practice in Southern Contexts 22: 207-220.
- Tao D, Awan-Scully R, Cole A, Gao Y, Ash G, et al. (2023) Integration of Exercise Prescription into Medical provision as a treatment for non-communicable diseases: A scoping review. Frontiers in Public Health 11. [CrossRef]
- Mohd Salim J, Anuar SN, Omar K, Tengku Mohamad TR Sanusi NA (2023) The Impacts of Traditional Ecological Knowledge towards Indigenous Peoples: A Systematic Literature Review. Sustainability 15: 824.
- Griffiths K, Davies L, Savage C, Shelling M, Dalziel P, et al. (2023) The Value of Recreational Physical Activity in Aotearoa New Zealand: A Scoping Review of Evidence and Implications for Social Value Measurement. International Journal of Environmental Research and Public Health 20: 2906. [CrossRef]
- Hargreaves J (2013) Heroines of Sport: The Politics of Difference and Identity. Routledge.
- Azlan A, Ismail N, Fauzi NFM, Talib RA (2021) Playing Traditional Games vs. Free Play During. Physical Education Lesson to Improve Physical Activity: A Comparison Study. Pedagogy of Physical Culture and Sports 25: 178-187. [CrossRef]
- Natalucci V, Marmondi F, Biraghi M, Bonato M (2023) The Effectiveness of Wearable Devices in Non-Communicable Diseases to Manage Physical Activity and Nutrition: Where We Are?. Nutrients 15: 913.
- Mdiya L, Taruvinga A, Mushunje A, Mopipi K, Ngarava S (2021) Rural Community Use and Perception of Rangeland Products in Eastern Cape Province, South Africa. African J of Sci Tech Inn Dev 13: 757-768.
- Otto J, Zerner C, Robinson J (2013) Natural Connections: Perspectives in Communitybased Conservation. Island press.
- Glover M, Kira A, Kira G, McRobbie H, Breier BH, et al. (2017) An Innovative Team-Based Weightloss Competition to Reduce Cardiovascular and Diabetes Risk Among Māori and Pacific People: Rationale and Method for the Study and its Evaluation. BMC nutrition 3: 1-9. [CrossRef]
- Salter G (2003) Maori Culture and Tradition in the Mainstream: Teaching Te Reo Kori1 in Sport Education. New Zealand Physical Educator 36: 27.
- Bowkett MT (2015) Towards Collaborative Pathways of Leadership in Education for Māori: a Thesis Presented in Partial Fulfilment of the Requirements for the Degree of Doctor of Education, at Massey University, Manawatū, New Zealand (Doctoral dissertation, Massey University).
- Mogamisi MS (2022) Indigenous Games, Dance, and Music for Promoting Health and Wellbeing of the Aged, North-West Province (Doctoral dissertation, North-West University (South Africa)).
- Madima TJ (2021) Exploring the Cultural Heritage Preservation through Digitisation: A Case Study of Traditional Children’s Games in Limpopo Province, South Africa (Doctoral Dissertation).
- Pramanik R (2018) Play and Indigenous Games of Children: A Cultural Heritage of Western Odisha, India. Knowledge Cultures 6: 96-110.
- Mudzielwana TN (2020) Factors Influencing Non-Participation of Youth on Indigenous Games in Thulamela Municipality of Vhembe District in Limpopo Province (Doctoral dissertation).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




