HISTORY OF PRESENTATION:
The patient is a term male infant that failed a newborn congenital heart screen after having a normal fetal ultrasound. A trans-thoracic echocardiogram (TTE) demonstrated Tetralogy of Fallot (ToF) with pulmonary atresia, outlet septal extension of the ventricular septal defect (VSD), and continuous branch pulmonary arteries (PAs). On day of life five, he underwent complete repair with a trans-annular patch, ligation of the patent ductus arteriosus, and reduction of an atrial septal defect. The discharge TTE demonstrated good repair with no right ventricular outflow tract obstruction (RVOTO) (peak gradient 11 mmHg, mean gradient of 6 mmHg), diffusely narrowed branch PAs (gradient 17 mmHg in bilateral PAs), no residual VSD and severe pulmonary valve insufficiency. At one month post discharge follow up, he was doing well clinically with reassuring growth and normal oxygen saturations. At eight months of life, a routine TTE demonstrated new severe pulmonary valve stenosis with a discretely narrowed fibromuscular ridge in the right ventricular outflow tract (RVOT) with a diameter of 5 mm. The peak gradient was 80 mmHg and the mean gradient was 44 mmHg. The echocardiogram demonstrated mildly diminished right ventricular systolic function with moderate right ventricular hypertrophy and a mildly dilated right ventricular cavity.
DIFFERENTIAL DIAGNOSIS:
In a patient with repaired ToF with RVOTO, the differential diagnosis for obstruction can fall into two broad categories: fixed and dynamic obstruction. The location of fixed obstruction can help differentiate the cause of obstruction. Flow can be limited at the level of the valve (native or prosthetic valvar stenosis), in the sub-valvar (conduit stenosis) or supra-valvar areas (branch or main pulmonary artery stenosis). Dynamic obstruction is generally caused by the growth of muscle bundles into the RVOT.
INVESTIGATIONS:
What is the best treatment for a child less than one year old whom has already undergone one major surgery with an extended postoperative length of stay now with echocardiographic imaging showing a peak gradient of 80 mmHg? A team approach was taken to discuss options of re-operation or treatment in the cardiac catheterization lab with ballooning and probable stenting to relieve the obstruction. Traditional stenting is known to relieve the obstruction, but in a child so young, is there an option where relief can be achieved without the need for long term stents? There has been significant investigation into a stent which will resorb into the body in under three years as an alternative to traditional stenting; such a resorbable stent could relieve obstruction without having the long term sequela of a traditional stent.
MANAGEMENT (MEDICAL/INTERVENTIONAL):
Prior to proceeding to the catheterization lab, an application was made to the FDA for compassionate use to place an Iron Bioresorbable Scaffold (IBS AngelTM) (Lifetech Scientific, Shenzhen, Guangdong, China) and approval was granted. Institutional IRB approval was subsequently requested and granted.
At eight months of life, the infant was brought to the catheterization lab for a hemodynamic assessment and for likely stenting of the RVOT. Baseline pressures revealed: right atrial pressure mean of 8 mmHg; right ventricular pressure 77mmHg with end diastolic pressure (EDP) 9 mmHg; right PA 15/9 mmHg with a mean of 12 mmHg; right pulmonary capillary wedge pressure 8 mmHg.
In the catheterization lab, a 10 mm diameter by 18 mm length Angel IBS stent was placed. Initial angiography demonstrated that the stent was mostly distal to the area of focal narrowing. A pullback demonstrated an improved gradient of 20 mmHg. The stent was then ballooned with a 10 mm AthletisTM balloon (Boston Scientific, Marlborough, MA, United States) with good angiographic effect. Due to ongoing sub-valvar narrowing, a second 10 mm by 18 mmHg Angel IBS stent was placed. Angiography demonstrated improvement in obstruction and a pullback demonstrated a final gradient of 8 mmHg. A discharge TTE demonstrated mild pulmonary valve stenosis with a peak gradient of 35 mmHg and a mean of 15 mmHg and stable severe pulmonary valve insufficiency.
DISCUSSION:
After repair of ToF, RVOTO is a common complication; various studies have estimated the incidence of more than moderate stenosis to be between 20 and 37% [
1,
2]. Management techniques can include medical, surgical or catheter based intervention. Surgical or catheter based re-intervention is required in 15-25% of cases [
2,
3]. Catheter based interventions of post-surgical stenosis avoid the need for a full sternotomy and stents can provide durable repair. In rapidly growing pediatric patients however, stents cannot match somatic growth and as such, require re-intervention. Bio-absorbable stents (BAS) are a novel tool that provide radial dilation and then resorb over time, attempting to obviate the need for stent re-ballooning or intentional fracturing. Amongst pediatric interventional cardiologists, there is significant demand for BAS, especially for use in PAs [
4].
The device described in the case, the bio-absorbable IBS Angel
TM, comes in two types, one is made of a low-profile nitride iron (~70 microns) and the second is coated with a zinc and poly-D, L-lactic acid and is sirolimus eluting. In vitro, this device has been shown to have a thin profile allowing for improved maneuverability [
5]. Animal studies have demonstrated safe implementation with durable short term effect and have suggested that these stents will be completely corroded in 1-2 years [
6,
7,
8]. In a porcine model, this device has been shown to have strong radial strength and endothelialize quickly, within 28 days, which suggests a lower risk for scaffold thrombosis [
8].
This paper presents the novel use of a bio-absorbable IBS Angel
TM stent in a pediatric right ventricular outflow tract. This particular stent has been described in the literature in small case series of children with stenotic branch PAs and in maintaining patients’ patent ductus arterioses [
9,
10]. In the case series of patients with Angel IBS stents in the patent ductus, four of eight patients developed blocked or restrictive stent flow at six months, but four were widely patent [
10]. The series of eleven patients with the Angel IBS stent in branch PAs demonstrated improvement in stenosis and no in stent thrombosis, malposition or re-stenosis at three months of follow up. To the authors’ knowledge, this device has not been used in a pediatric RVOT prior to this case.
In this patient, the Angel IBS stent was successfully deployed and the stent achieved immediate angiographic and echocardiographic improvement in the patient’s severe RVOT stenosis. In addition to post-repair RVOT stenosis, there is likely a role for BAS in primary palliation in neonates with ToF with severe RVOTO to allow them to grow and optimize patients prior to complete surgical repair [
3,
5]. Further studies are required to examine the duration and durability of IBS stents’ effects in pediatric patients but this case demonstrates that this stent can provide immediate adequate relief of obstruction.
FOLLOW-UP:
A TTE when the patient was 15 months (seven months status post stent deployment) demonstrated moderate pulmonary valve stenosis, a slight increase from his immediate post-stent level, with a peak gradient of 47 mmHg across the RVOT and a mean gradient of 23 mmHg. At that point, he had qualitatively normal right ventricular function with a mildly dilated right ventricular cavity and moderate right ventricular hypertrophy. Repeat TTE at 29 months of age (21 months status post stent deployment) demonstrated moderate-severe pulmonary valve stenosis with a peak gradient of 73 mmHg and a mean gradient of 35 mmHg. Right ventricular function remains qualitatively normal. Clinically, he is asymptomatic with appropriate growth and development even in the presence of the increasing gradient.
CONCLUSIONS:
Bio-absorbable stents can provide relief of obstruction in pediatric right ventricular outflow tracts.
As compared to metal stents, bio-absorbable stents have a similar profile of benefits and limit the negative long-term effects.
In the short-intermediate term, bio-absorbable stents can provide durable stenosis repair. Further studies are required to determine the in vivo duration of effect.
LEARNING OBJECTIVES:
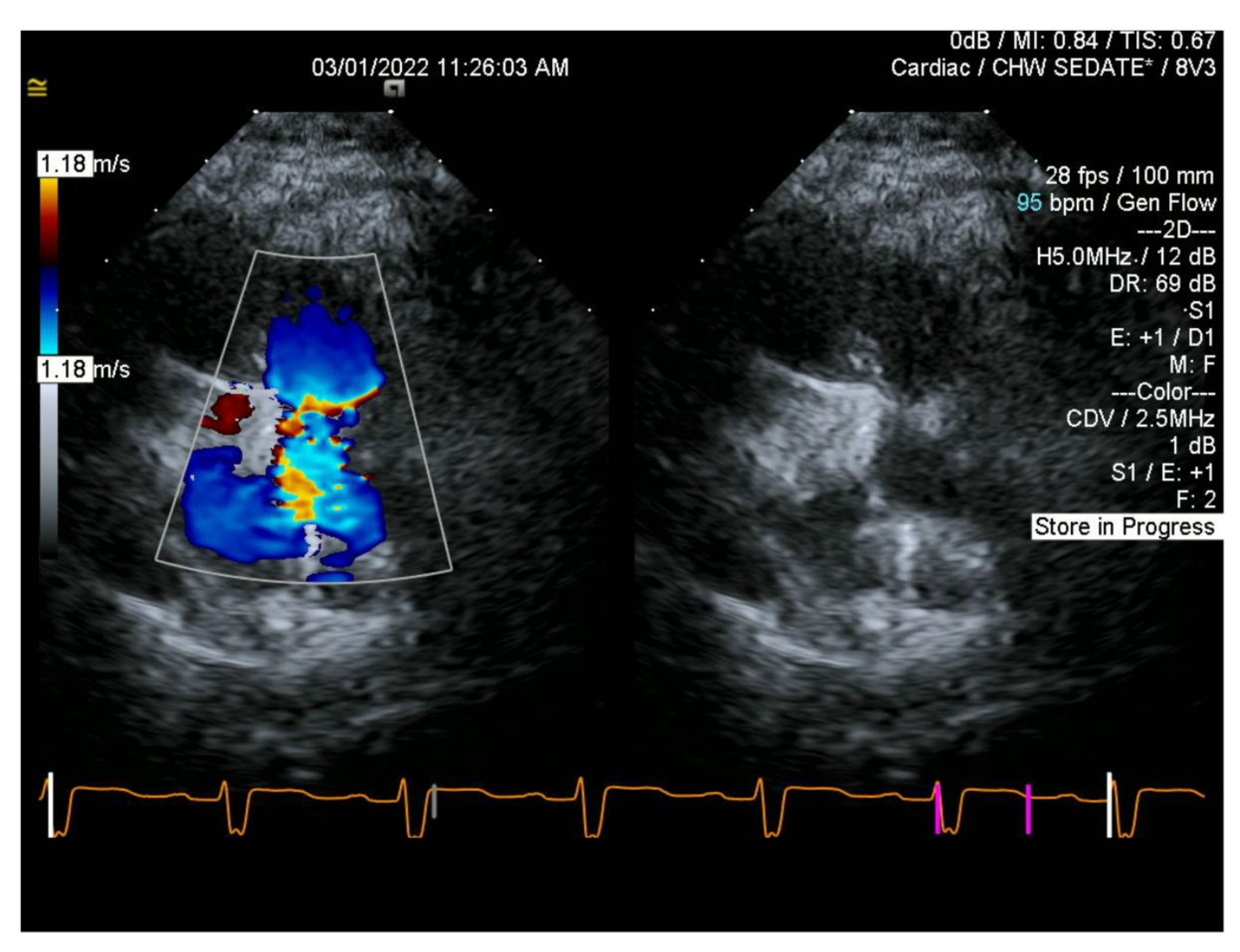
Figure 1.
Parasternal short echocardiography of RVOT pre-stent with Doppler (left) and without (right).
Figure 1.
Parasternal short echocardiography of RVOT pre-stent with Doppler (left) and without (right).
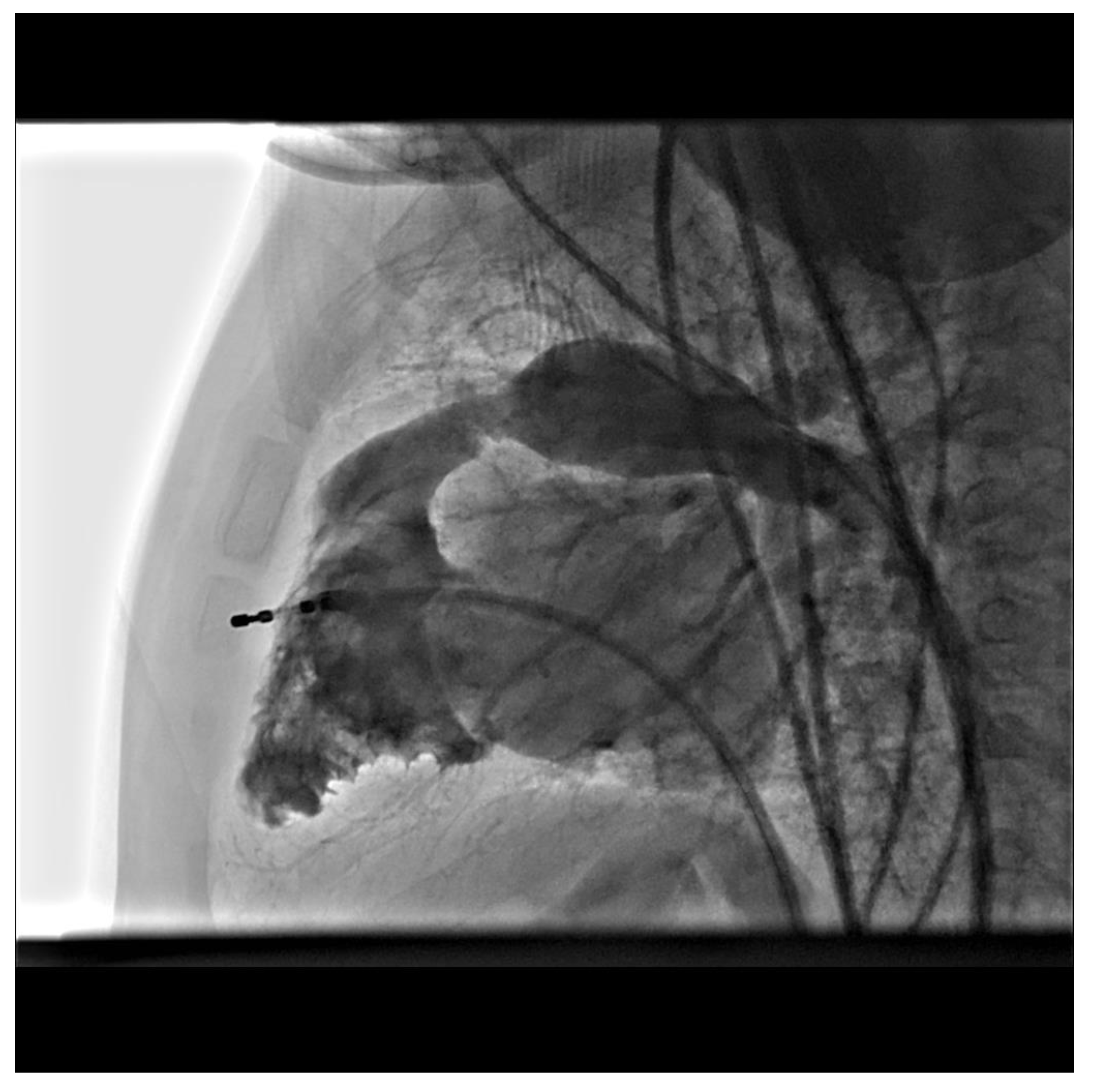
Figure 2.
Lateral imaging of RVOTO taken from 3D angiography.
Figure 2.
Lateral imaging of RVOTO taken from 3D angiography.
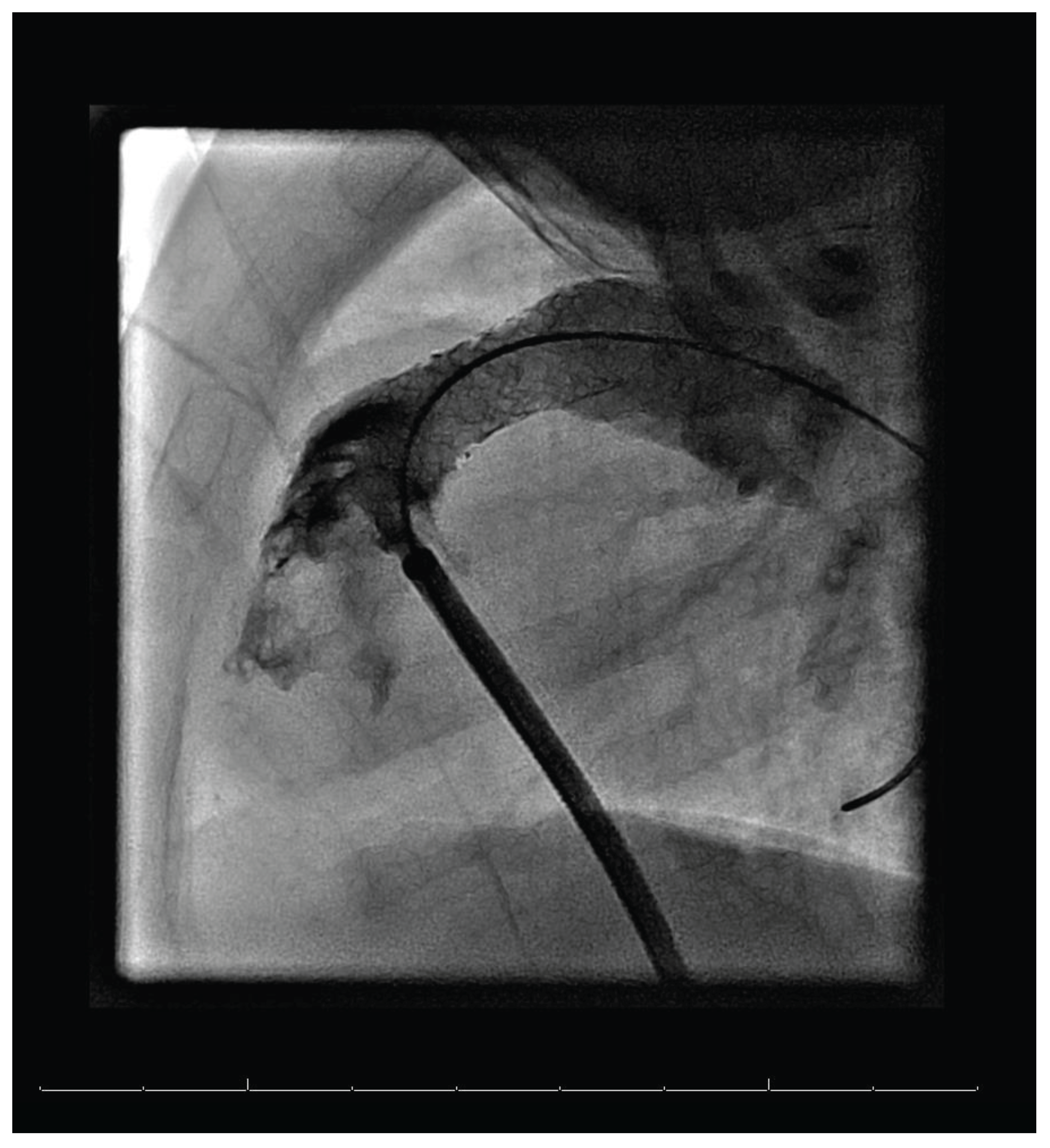
Figure 3.
Lateral imaging of RVOTO after stent implementation, taken from 3D angiography.
Figure 3.
Lateral imaging of RVOTO after stent implementation, taken from 3D angiography.
References
- Borodinova, O.; Mykychak, Y.; Yemets, I. Transesophageal Echocardiographic Predictor of Significant Right Ventricular Outflow Tract Obstruction After Tetralogy of Fallot Repair. Semin Thorac Cardiovasc Surg. 2020, 32, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Soquet, J.; Brizard, C.P.; d’Udekem, Y. Evolution of residual and recurrent right ventricular outflow tract obstruction after tetralogy of Fallot repair. J Thorac Cardiovasc Surg. 2020, 159, e275–e277. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, J.P.; Chaturvedi, R.R.; Benson, L. Right Ventricular Outflow Tract Stenting in Tetralogy of Fallot Infants with Risk Factors for Early Primary Repair. Circ Cardiovasc Interv. 2016, 9, e003979. [Google Scholar] [CrossRef] [PubMed]
- Shibbani, K.; Kenny, D.; McElhinney, D.; Hijazi, Z.M.; Moran, T. Identifying Gaps in Technology for Congenital Interventions: Analysis of a Needs Survey from Congenital Interventional Cardiologists. Pediatr Cardiol. 2016, 37, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Bjorkman, K.; Maldonado, J.R.; Saey, S.; McLennan, D. In vitro performance of Lifetech IBS AngelTM (iron-based bioresorbable scaffold) stents during overdilation for use in pediatric patients. Front Cardiovasc Med. 2022, 9, 1006063. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Qin, L.; Qi, H. Long-term in vivo corrosion behavior, biocompatibility and bioresorption mechanism of a bioresorbable nitrided iron scaffold. Acta Biomater. 2017, 54, 454–468. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Zhang, H.; Zhang, W. In vivo degradation and endothelialization of an iron bioresorbable scaffold. Bioact Mater. 2021, 6, 1028–1039. [Google Scholar] [CrossRef]
- Zheng, J.F.; Qiu, H.; Tian, Y. Preclinical Evaluation of a Novel Sirolimus-Eluting Iron Bioresorbable Coronary Scaffold in Porcine Coronary Artery at 6 Months. JACC Cardiovasc Interv. 2019, 12, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Li, J. jie; Xu, Y. kai; Xie, Y. mei; Wang, S. shui; Zhang, Z. wei. Initial status and 3-month results relating to the use of biodegradable nitride iron stents in children and the evaluation of right ventricular function. Front Cardiovasc Med. 2022, 9, 914370. [Google Scholar] [CrossRef] [PubMed]
- Mood, M.; Niazy, K.; Alwi, M. Feasibility, safety, and efficacy of iron bioresorbable scaffold in neonates with duct-dependent pulmonary circulation. Ann Pediatr Cardiol. 2022, 15, 147. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).