Submitted:
06 March 2024
Posted:
08 March 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
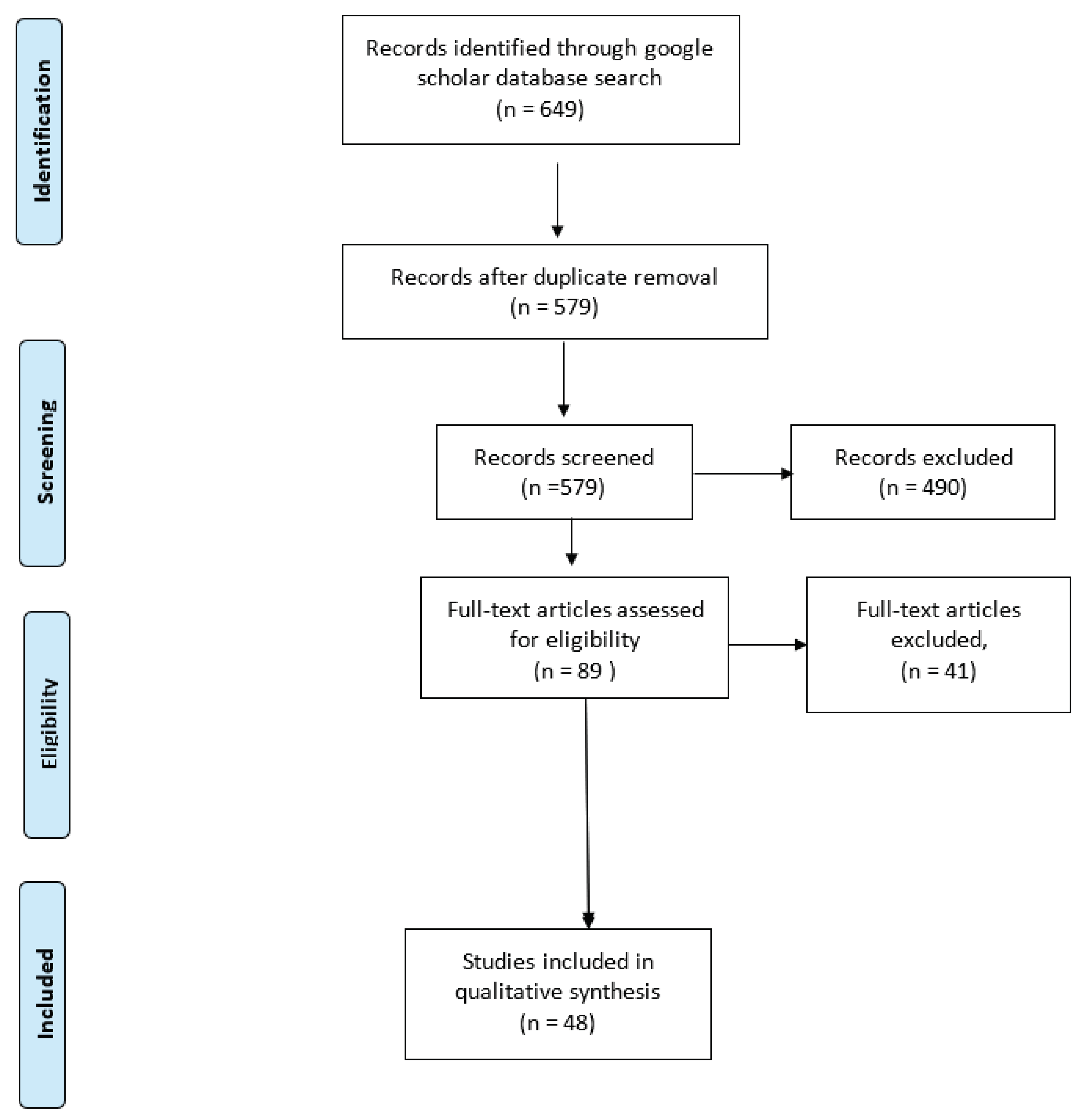
Study design and systematic review protocol
Search strategy
Article selection and data extraction
Analysis
Results
Median Prevalence of abortigenic pathogens
| Disease | Species | Cases (n) | Total tested (N) | Median Prevalence | Min | Max |
|
Brucella |
Sheep | 981 | 9071 | 6.85 | 1.20 | 11.60 |
| Goats | 887 | 17007 | 3.35 | 0.90 | 5.40 | |
| Cattle | 10662 | 171733 | 8.95 | 0.50 | 63.60 | |
|
Neospora |
Sheep | 38 | 555 | 6.80 | 6.80 | 6.80 |
| Goats | 20 | 185 | 10.80 | 10.80 | 10.80 | |
| Cattle | 367 | 3775 | 12.65 | 3.40 | 25.60 | |
|
Toxoplasma |
Sheep | 595 | 2284 | 27.50 | 1.40 | 75.90 |
| Goats | 493 | 1226 | 32.00 | 20.00 | 64.80 | |
| Cattle | 13 | 174 | 7.50 | 7.50 | 7.50 | |
|
Coxiella |
Sheep | 17 | 184 | 9.20 | 9.20 | 9.20 |
| Goats | 22 | 91 | 24.20 | 24.20 | 24.20 | |
| Cattle | 30 | 217 | 13.80 | 13.80 | 13.80 | |
|
Rift Valley Fever Virus |
Sheep | 38 | 874 | 7.70 | 2.40 | 40.00 |
| Goats | 37 | 547 | 20.95 | 2.50 | 40.00 | |
| Cattle | 19 | 309 | 7.45 | 3.60 | 11.30 | |
| BVD | Cattle | 314 | 398 | 78.90 | 78.90 | 78.90 |
| Leptospira | Cattle | 263 | 373 | 70.50 | 70.50 | 70.50 |
| Chlamydia | Sheep | 53 | 803 | 6.60 | 6.60 | 6.60 |
Discussion
Conclusion
Supplementary Materials
Acknowledgement
References
- “Abortion in Cattle - Reproductive System,” Veterinary Manual. https://www.msdvetmanual.com/reproductive-system/abortion-in-large-animals/abortion-in-cattle (accessed Oct. 12, 2021).
- M. D. Givens, “A clinical, evidence-based approach to infectious causes of infertility in beef cattle,” Theriogenology, vol. 66, no. 3, pp. 648–654, Aug. 2006. [CrossRef]
- G. Semango et al., “The Sero-epidemiology of Neospora caninum in Cattle in Northern Tanzania,” Front. Vet. Sci., vol. 6, 2019. [CrossRef]
- N. A. Wardrop et al., “The Sero-epidemiology of Coxiella burnetii in Humans and Cattle, Western Kenya: Evidence from a Cross-Sectional Study,” PLoS Negl. Trop. Dis., vol. 10, no. 10, 2016. [CrossRef]
- O. Madzingira, F. O. Fasina, E. Kandiwa, A. Musilika-Shilongo, F. Chitate, and H. van Heerden, “A retrospective sero-epidemiological survey of bovine brucellosis on commercial and communal farming systems in Namibia from 2004 to 2018,” Trop. Anim. Health Prod., vol. 52, no. 6, pp. 3099–3107, 2020. [CrossRef]
- H. Oyas et al., “Enhanced surveillance for Rift Valley Fever in livestock during El Niño rains and threat of RVF outbreak, Kenya, 2015-2016,” PLoS Negl. Trop. Dis., vol. 12, no. 4, 2018. [CrossRef]
- H. J. Kim et al., “Serological surveillance studies confirm the Rift Valley fever virus free status in South Korea,” Trop. Anim. Health Prod., vol. 47, no. 7, pp. 1427–1430, 2015. [CrossRef]
- S. Esubalew et al., “Seroepidemiology of Toxoplasma gondii in small ruminants in Northwest Ethiopia,” Vet. Parasitol. Reg. Stud. Rep., vol. 22, no. (Esubalew S.) Estie District Livestock and Fishery Development Office, Amhara Regional state, Ethiopia, 2020. [CrossRef]
- S. M. Njiro et al., “A study of some infectious causes of reproductive disorders in cattle owned by resource-poor farmers in Gauteng Province, South Africa.,” J. S. Afr. Vet. Assoc., vol. 82, no. 4, pp. 213–218, 2011. [CrossRef]
- R. R. Nicolino, R. O. Capanema, C. S. F. de Oliveira, M. E. O. Pastrana, L. B. Lopes, and J. P. A. Haddad, “Estimating the abortion risk difference in Neospora caninum seropositive dairy cattle in Brazil,” Ciênc. Rural, vol. 45, no. 9, pp. 1629–1633, Jun. 2015. [CrossRef]
- D. Moore, M. Reichel, E. Spath, and C. Campero, “Neospora caninum causes severe economic losses in cattle in the humid pampa region of Argentina,” Trop. Anim. Health Prod., vol. 45, no. 5, pp. 1237–1241, Jun. 2013. [CrossRef]
- “Berezowski - Veterinary Surveillance.pdf.” Accessed: Oct. 22, 2021. [Online]. Available: https://www.eolss.net/sample-chapters/c10/E5-15A-17.pdf.
- “chapitre_surveillance_general.pdf.” Accessed: Oct. 22, 2021. [Online]. Available: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahc/current/chapitre_surveillance_general.pdf.
- G. Semango et al., “The Sero-epidemiology of Neospora caninum in Cattle in Northern Tanzania,” Front. Vet. Sci., vol. 6, 2019. [CrossRef]
- A. B. N. Tonouhewa et al., “A serological survey of Toxoplasma gondii infection in sheep and goat from Benin, West-Africa,” J. Parasit. Dis., vol. 43, no. 3, pp. 343–349, 2019. [CrossRef]
- N. B. Alhaji, O. O. Babalobi, Y. Wungak, and H. G. Ularamu, “Participatory survey of Rift Valley fever in nomadic pastoral communities of North-central Nigeria: The associated risk pathways and factors,” PLoS Negl. Trop. Dis., vol. 12, no. 10, p. e0006858, Oct. 2018. [CrossRef]
- U. W. Hesterberg, R. Bagnall, K. Perrett, B. Bosch, R. Horner, and B. Gummow, “A serological prevalence survey of Brucella abortus in cattle of rural communities in the province of KwaZulu-natal, South Africa,” J. S. Afr. Vet. Assoc., vol. 79, no. 1, pp. 15–18, Mar. 2008. [CrossRef]
- N. A. Wardrop et al., “The Sero-epidemiology of Coxiella burnetii in Humans and Cattle, Western Kenya: Evidence from a Cross-Sectional Study,” PLoS Negl. Trop. Dis., vol. 10, no. 10, p. e0005032, Oct. 2016. [CrossRef]
- C. Gomo, M. de Garine-Wichatitsky, A. Caron, and D. M. Pfukenyi, “Survey of brucellosis at the wildlife-livestock interface on the Zimbabwean side of the Great Limpopo Transfrontier Conservation Area,” Trop. Anim. Health Prod., vol. 44, no. 1, pp. 77–85, 2012. [CrossRef]
- J. George, B. Häsler, E. Komba, C. Sindato, M. Rweyemamu, and J. Mlangwa, “Towards an integrated animal health surveillance system in Tanzania: making better use of existing and potential data sources for early warning surveillance,” BMC Vet. Res., vol. 17, no. 1, p. 109, Mar. 2021. [CrossRef]
- H. B. Chethan Kumar et al., “Animal disease surveillance: Its importance & present status in India,” Indian J. Med. Res., vol. 153, no. 3, pp. 299–310, Mar. 2021. [CrossRef]
- J. Namayanja, M. Dione, and J. M. Kungu, “Stakeholders’ perceptions on performance of the Livestock Disease Surveillance system in Uganda: A case of Pallisa and Kumi Districts,” Pastoralism, vol. 9, no. 1, p. 12, Sep. 2019. [CrossRef]
- D. Moher, A. Liberati, J. Tetzlaff, and D. G. Altman, “Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement,” BMJ, vol. 339, p. b2535, Jul. 2009. [CrossRef]
- “UNSD — Welcome to UNSD.” https://unstats.un.org/home/ (accessed Aug. 20, 2021).
- “WHO | Neglected zoonotic diseases.” https://www.who.int/neglected_diseases/diseases/zoonoses/en/ (accessed Nov. 02, 2020).
- A. Bronner, V. Hénaux, N. Fortané, P. Hendrikx, and D. Calavas, “Why do farmers and veterinarians not report all bovine abortions, as requested by the clinical brucellosis surveillance system in France?,” BMC Vet. Res., vol. 10, pp. 93–93, Apr. 2014. [CrossRef]
- F.L.GoutardabA.BinotabR.DubozacH.Rasamoelina-AndriamanivodeM.PedronoaeD.HollfM.I.PeyreagJ.CappelleahV.ChevalieraM.FiguiéiS.MoliaajF.L.Rogerab, “How to reach the poor? Surveillance in low-income countries, lessons from experiences in Cambodia and Madagascar,” Prev. Vet. Med., vol. 120, no. 1, pp. 12–26, Jun. 2015. [CrossRef]
- Z. Mtema et al., “Mobile Phones As Surveillance Tools: Implementing and Evaluating a Large-Scale Intersectoral Surveillance System for Rabies in Tanzania,” PLOS Med., vol. 13, no. 4, p. e1002002, Apr. 2016. [CrossRef]
- “A Smartphone App (AfyaData) for Innovative One Health Disease Surveillance from Community to National Levels in Africa: Intervention in Disease Surveillance,” SACIDS. http://www.sacids.org/publications/smartphone-app-afyadata-innovative-one-health-disease-surveillance-community-national-levels-africa-intervention-disease-surveillance/ (accessed Oct. 25, 2020).
- E. Karimuribo et al., “Potential use of mobile phones in improving animal health service delivery in underserved rural areas: Experience from Kilosa and Gairo districts in Tanzania,” BMC Vet. Res., vol. 12, Oct. 2016. [CrossRef]
- D. S. Thomas, K. Daly, E. C. Nyanza, S. E. Ngallaba, and S. Bull, “Health worker acceptability of an mHealth platform to facilitate the prevention of mother-to-child transmission of HIV in Tanzania,” Digit. Health, vol. 6, p. 2055207620905409, Jan. 2020. [CrossRef]
- K. L. L’Engle, H. L. Vahdat, E. Ndakidemi, C. Lasway, and T. Zan, “Evaluating feasibility, reach and potential impact of a text message family planning information service in Tanzania,” Contraception, vol. 87, no. 2, pp. 251–256, Feb. 2013. [CrossRef]
- “Deployment and use of mobile phone technology for real-time reporting of fever cases and malaria treatment failure in areas of declining malaria transmission in Muheza district north-eastern Tanzania.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5540449/ (accessed Nov. 02, 2020).
- J. E. Haberer, J. Kiwanuka, D. Nansera, I. B. Wilson, and D. R. Bangsberg, “Challenges in using mobile phones for collection of antiretroviral therapy adherence data in a resource-limited setting,” AIDS Behav., vol. 14, no. 6, pp. 1294–1301, Dec. 2010. [CrossRef]
- H. Wakadha et al., “The feasibility of using mobile-phone based SMS reminders and conditional cash transfers to improve timely immunization in rural Kenya,” Vaccine, vol. 31, no. 6, pp. 987–993, Jan. 2013. [CrossRef]
- L. W. Chang et al., “Impact of a mHealth intervention for peer health workers on AIDS care in rural Uganda: a mixed methods evaluation of a cluster-randomized trial,” AIDS Behav., vol. 15, no. 8, pp. 1776–1784, Nov. 2011. [CrossRef]
- S. Githinji et al., “Reducing stock-outs of life saving malaria commodities using mobile phone text-messaging: SMS for life study in Kenya,” PloS One, vol. 8, no. 1, pp. e54066–e54066, Jan. 2013. [CrossRef]
- N. Leon, H. Schneider, and E. Daviaud, “Applying a framework for assessing the health system challenges to scaling up mHealth in South Africa,” BMC Med. Inform. Decis. Mak., vol. 12, pp. 123–123, Nov. 2012. [CrossRef]
- T. Horvath, H. Azman, G. E. Kennedy, and G. W. Rutherford, “Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection,” Cochrane Database Syst. Rev., no. 3, p. CD009756, Mar. 2012. [CrossRef]
- V. M. Kiberu, M. Mars, and R. E. Scott, “Barriers and opportunities to implementation of sustainable e-Health programmes in Uganda: A literature review,” Afr. J. Prim. Health Care Fam. Med., vol. 9, no. 1, Art. no. 1, May 2017.
- M. Njoroge, D. Zurovac, E. A. A. Ogara, J. Chuma, and D. Kirigia, “Assessing the feasibility of eHealth and mHealth: a systematic review and analysis of initiatives implemented in Kenya,” BMC Res. Notes, vol. 10, no. 1, p. 90, Feb. 2017. [CrossRef]
- J. O’Donovan and A. Bersin, “Controlling Ebola through mHealth strategies,” Lancet Glob. Health, vol. 3, no. 1, p. e22, Jan. 2015. [CrossRef]
- S. Lee, Y.-M. Cho, and S.-Y. Kim, “Mapping mHealth (mobile health) and mobile penetrations in sub-Saharan Africa for strategic regional collaboration in mHealth scale-up: an application of exploratory spatial data analysis,” Glob. Health, vol. 13, no. 1, pp. 63–63, Aug. 2017. [CrossRef]
- I. Gorski, J. T. Bram, S. Sutermaster, M. Eckman, and K. Mehta, “Value propositions of mHealth projects,” J. Med. Eng. Technol., vol. 40, no. 7–8, pp. 400–421, Nov. 2016. [CrossRef]
- C. Déglise, L. S. Suggs, and P. Odermatt, “SMS for disease control in developing countries: a systematic review of mobile health applications,” J. Telemed. Telecare, vol. 18, no. 5, pp. 273–281, Jul. 2012. [CrossRef]
- T. J. Betjeman, S. E. Soghoian, and M. P. Foran, “mHealth in Sub-Saharan Africa,” Int. J. Telemed. Appl., vol. 2013, p. 482324, 2013. [CrossRef]
- J. Brinkel, A. Krämer, R. Krumkamp, J. May, and J. Fobil, “Mobile phone-based mHealth approaches for public health surveillance in sub-Saharan Africa: a systematic review,” Int. J. Environ. Res. Public. Health, vol. 11, no. 11, pp. 11559–11582, Nov. 2014. [CrossRef]
- “World Bank. Mobile cellular subscriptions (per 100 people).” Accessed: Jun. 20, 2019. [Online]. Available: http://data.worldbank.org/indicator/IT.CEL.SETS.P2.
- J. Walker, “New media methods for syndromic surveillance and disease modelling.,” CAB Rev. Perspect. Agric. Vet. Sci. Nutr. Nat. Resour., vol. 8, no. 031, Sep. 2013. [CrossRef]
- Z. Mtema et al., “Mobile Phones As Surveillance Tools: Implementing and Evaluating a Large-Scale Intersectoral Surveillance System for Rabies in Tanzania,” PLoS Medicine, vol. 13, no. 4. 2016. doi: 10.1371/journal.pmed.1002002.
- E. V. Mbugi et al., “‘One Health’ infectious diseases surveillance in Tanzania: Are we all on board the same flight?,” Onderstepoort J. Vet. Res., vol. 79, no. 2, pp. 1–7, 2012. [CrossRef]
- A. Bernabe-Ortiz et al., “Handheld computers for self-administered sensitive data collection: a comparative study in Peru.,” BMC Med. Inform. Decis. Mak., vol. 8, p. 11, 2008. [CrossRef]
- M. A. Missinou et al., “Short report: Piloting paperless data entry for clinical research in Africa,” Am. J. Trop. Med. Hyg., vol. 72, no. 3, pp. 301–303, 2005. [CrossRef]
- L. Diero et al., “A computer-based medical record system and personal digital assistants to assess and follow patients with respiratory tract infections visiting a rural Kenyan health centre,” BMC Med. Inform. Decis. Mak., vol. 6, p. 21, 2006. [CrossRef]
- K. Shirima et al., “The use of personal digital assistants for data entry at the point of collection in a large household survey in southern Tanzania,” Emerg. Themes Epidemiol., vol. 4, no. 1, p. 5, 2007. [CrossRef]
- C. Robertson, K. Sawford, S. L. A. Daniel, T. A. Nelson, and C. Stephen, “Mobile phone-based infectious disease surveillance system, Sri Lanka,” Emerg. Infect. Dis., vol. 16, no. 10, pp. 1524–1531, 2010. [CrossRef]
- “EMA-i A Mobile App for Timely Animal Disease fiel.pdf.” Accessed: Jul. 23, 2021. [Online]. Available: http://www.fao.org/3/i4853e/i4853e.pdf.
| Search string | Database or further sources | Results | Date | Comments |
| ((((ASIA[Text Word]) OR (AFRICA[Text Word]) AND (1990/1/1:2021/7/1[pdat])) AND (((GOATS[Title/Abstract]) OR (SHEEP[Title/Abstract])) OR (CATTLE[Title/Abstract]) AND (1990/1/1:2021/7/1[pdat]))) AND (ABORT*[Title/Abstract] AND (1990/1/1:2021/7/1[pdat]))) AND (surve*[Title/Abstract]) | PubMed | 29 | 2021-06-26 | PubMed search |
| ( TITLE-ABS-KEY ( asia* ) OR TITLE-ABS-KEY ( africa* ) AND TITLE-ABS-KEY ( goats ) OR TITLE-ABS-KEY ( sheep ) OR TITLE-ABS-KEY ( cattle ) AND TITLE-ABS-KEY ( abort* ) AND TITLE-ABS-KEY ( surve* ) ) AND PUBYEAR > 1989 | SCOPUS | 64 | 2021-06-26 | Scopus database through NM-AIST Library (AGORA) |
| ((abort*:ti AND asia*:ti OR africa*:ti) AND goat:ab,ti OR sheep:ab,ti OR cattle:ab,ti) AND abort*:ti,ab,kw AND surve*:ti,ab,kw AND [1990-2021]/py | Embase | 375 | 2021-06-26 | Embase through NM-AIST |
| abortion surveillance cattle OR sheep OR goats * * * * “Asia OR Africa” -human -people -persons -man -woman -Europe -americas -australia -pacific -”south america” | Google Scholar | 181 | 2021-06-26 | Google Scholar search though NM-AIST |
| Years | |||||
| Pathogen spp. | 1990 - 1999 | 2000 – 2009 | 2010 – 2019 | 2020 - 2021 | Total |
| Brucella spp. | 2 | 4 | 16 | 3 | 25 |
| Coxiella burnetii | 0 | 0 | 1 | 0 | 1 |
| Bluetongue virus | 0 | 0 | 1 | 0 | 1 |
| Chlamydia abortus | 0 | 0 | 0 | 1 | 1 |
| Leptospira spp | 0 | 0 | 1 | 0 | 1 |
| Neospora caninum | 0 | 1 | 3 | 0 | 4 |
| RVFV | 1 | 0 | 5 | 0 | 6 |
| Toxoplasma gondii | 0 | 1 | 1 | 0 | 5 |
| BVDV, Brucella spp., N. caninum | 0 | 0 | 0 | 0 | 1 |
| Brucella spp., Coxiella burnetii, RVFV | 0 | 0 | 1 | 0 | 1 |
| N. caninum, T. gondii | 0 | 0 | 1 | 0 | 1 |
| T. gondii, N. caninum, Brucella spp. | 0 | 0 | 1 | 0 | 1 |
| Total | 48 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





