Submitted:
27 February 2024
Posted:
28 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Hesitancy in delivering a new antidiabetic drug treatment strategy related to postulates of clinical inertia
3. Trends in the ADA/EASD guidelines on T2D patient management strategy and the effect on new antidiabetic drug uptake
4. T2D patient complexity and endeavor towards precision medicine
5. Discussion
6. Future directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| T2D | type 2 diabetes |
| CV | cardiovascular |
| GLP-1ra | glucagon-like peptide 1 receptor agonists |
| SGLT-2in | sodium-glucose cotransporter-2 inhibitors |
| CVD | cardiovascular disease |
| ADA | American Diabetes Association |
| EASD | European Association for the Study of Diabetes |
| HbA1c | hemoglobin A1c |
| LDL | low-density lipoprotein |
| CAD | coronary artery disease |
| ASCVD | atherosclerotic cardiovascular disease |
| CVOT's | cardiovascular outcome trials |
| CHF | chronic hearth failure |
| CKD | chronic kidney disease |
| AI | Artificial Intelligence |
| DKA | diabetic ketoacidosis |
References
- Phillips L.S.; Branch W.T.; Cook C.B.; Doyle J.P.; El-Kebbi I.M.; Gallina D.L.; Miller C.D.; Ziemer D.C.; Barnes C.S. Clinical Inertia. Ann Intern Med. 2001; 135(9): 825-34. [CrossRef]
- O'Connor P.J.; Sperl-Hillen J.M.; Johnson P.E.; Rush W.A.; Biltz G. Clinical Inertia and Outpatient Medical Errors. Henriksen K.; Battles J.B.; Marks E.S.; Lewin D.I.; et al, editors. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Rockville (MD), USA: Agency for Healthcare Research and Quality (US) (2005).
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021 [published correction appears in Lancet. 2023 Sep 30;402(10408):1132]. Lancet. 2023;402(10397):203-234. [CrossRef]
- Bellary S.; Kyrou I.; Brown J.E.; Bailey C.J. Type 2 diabetes mellitus in older adults: clinical considerations and management. Nat Rev Endocrinol. 2021; 17(9) :534-548. [CrossRef]
- Jing X.; Chen J.; Dong Y.; Han D.; Zhao H.; Wang X.; Gao F.; Li C.; Cui Z.; Liu Y.; et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. 2018;16(1):189. [CrossRef]
- Rutten G.E.H.M.; Alzaid A. Person-centred type 2 diabetes care: time for a paradigm shift. Lancet Diabetes Endocrinol. 2018;6(4):264-266. [CrossRef]
- de Belvis A.G.; Pelone F.; Biasco A.; Ricciardi W.; Volpe M. Can Primary Care Professionals' Adherence to Evidence Based Medicine Tools Improve Quality of Care in Type 2 Diabetes Mellitus? A Systematic Review. Diabetes Res Clin Pract. 2009;85(2):119-31. [CrossRef]
- Stone M.A.; Charpentier G.; Doggen K.; Kuss O.; Lindblad U.; Kellner C.; Nolan J.; Pazderska A., Rutten G., Trento M., et al; GUIDANCE Study Group. Quality of care of people with type 2 diabetes in eight European countries: findings from the Guideline Adherence to Enhance Care (GUIDANCE) study. Diabetes Care. 2013;36(9):2628-38. [CrossRef]
- Byrnes P.D. Why Haven't I Changed That? Therapeutic Inertia in General Practice. Aust Fam Physician. 2011;40(1-2):24-8.
- Lavoie K.L.; Rash J.A.; Campbell T.S. Changing Provider Behavior in the Context of Chronic Disease Management: Focus on Clinical Inertia. Annu Rev Pharmacol Toxicol. 2017;57:263-83. [CrossRef]
- Khunti K.; Gomes M.B.; Pocock S.; Shestakova M.V.; Pintat S.; Fenici P.; Hammar N., Medina J. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: A systematic review. Diabetes Obes Metab. 2018;20(2):427-437. [CrossRef]
- Allen J.D.; Curtiss F.R.; Fairman K.A. Nonadherence, Clinical Inertia, or Therapeutic Inertia? J Manag Care Pharm. 2009;15(8):690-5. [CrossRef]
- Inzucchi S.E.; Bergenstal R.M.; Buse J.B.; Diamant M.; Ferrannini E.; Nauck M.; Peters AL.; Tsapas A.; Wender R.; Matthews DR. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140-9. [CrossRef]
- Mitchell S.; Malanda B.; Damasceno A.; Eckel RH.; Gaita D.; Kotseva K.; Januzzi J.L.; Mensah G.; Plutzky J.; Prystupiuk M.; et al. Roadmap on the Prevention of Cardiovascular Disease Among People Living With Diabetes. Glob Heart. 2019;14(3):215-240. [CrossRef]
- Sharma A.; Mittal S.; Aggarwal R.; Chauhan MK. Diabetes and cardiovascular disease: inter-relation of risk factors and treatment. Futur J Pharm Sci. 2020;6:130. [CrossRef]
- Li Y.; Liu Y.; Liu S.; Gao M.; Wang W.; Chen K.; Huang L.; Liu Y. Diabetic vascular diseases: molecular mechanisms and therapeutic strategies. Signal Transduct Target Ther. 2023;8(1):152. [CrossRef]
- Schernthaner G.; Shehadeh N.; Ametov AS.; Bazarova AV.; Ebrahimi F.; Fasching P.; Janež A.; Kempler P.; Konrāde I.; Lalić N.M.; et al. Worldwide inertia to the use of cardiorenal protective glucose-lowering drugs (SGLT2i and GLP-1 RA) in high-risk patients with type 2 diabetes. Cardiovasc Diabetol. 2020;19(1):185. [CrossRef]
- Davies M.J.; D'Alessio D.A.; Fradkin J.; Kernan W.N.; Mathieu C.; Mingrone G.; Rossing P.; Tsapas A.; Wexler D.J.; Buse J.B. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669-701. [CrossRef]
- Davies M.J.; Aroda V.R.; Collins B.S.; Gabbay R.A.; Green J.; Maruthur N.M.; Rosas S.E.; Del Prato S.; Mathieu C.; Mingrone G.; et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753-86. [CrossRef]
- Buse J.B.; Wexler D.J.; Tsapas A.; Rossing P.; Mingrone G.; Mathieu C.; D'Alessio D.A.; Davies M.J.; 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43(2):487-93. [CrossRef]
- Marx N.; Federici M.; Schütt K.; Müller-Wieland D.; Ajjan R.A.; Antunes M.J.; Christodorescu R.M.; Crawford C.; Di Angelantonio.; Eliasson B.; et al; ESC Scientific Document Group. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44(39):4043-4140. [CrossRef]
- Boussageon R.; Bejan-Angoulvant T.; Saadatian-Elahi M.; Lafont S.; Bergeonneau C.; Kassaï B.; Erpeldinger S.; Wright J.M.; Gueyffier F.; Cornu C.; Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343:d4169. [CrossRef]
- Khunti K.; Davies M.J. Clinical Inertia Versus Overtreatment in Glycaemic Management. Lancet Diabetes Endocrinol. 2018;6(4):266-8. [CrossRef]
- Mata-Cases M.; Mauricio D.; Real J.; Vlacho B.; Romera-Liebana L.; Molist-Brunet N.; Cedenilla M.; Franch-Nadal J. Potential Risk of Overtreatment in Patients with Type 2 Diabetes Aged 75 Years or Older: Data from a Population Database in Catalonia, Spain. J Clin Med. 2022;11(17):5134. [CrossRef]
- Gimeno J.A.; Cánovas G.; Durán A. Factors Associated with Adherence to Clinical Practice Guidelines for Patients with Type 2 Diabetes Mellitus: Results of a Spanish Delphi Consensus. J Diabetes Res. 2021:9970859. [CrossRef]
- Pantalone K.M.; Wells B.J.; Chagin K.M.; Ejzykowicz F.; Yu C.; Milinovich A.; Bauman JM.; Kattan MW.; Rajpathak S.; Zimmerman R.S. Intensification of Diabetes Therapy and Time Until A1C Goal Attainment Among Patients With Newly Diagnosed Type 2 Diabetes Who Fail Metformin Monotherapy Within a Large Integrated Health System. Diabetes Care. 2016;39(9):1527-34. [CrossRef]
- Khunti K.; Wolden M.L.; Thorsted B.L.; Andersen M.; Davies M.J. Clinical Inertia in People with Type 2 Diabetes: A Retrospective Cohort Study of More Than 80,000 People. Diabetes Care. 2013 36(11):3411-7. [CrossRef]
- Suraci C.; Mulas F.; Rossi M.C.; Gentile S.; Giorda C.B.; Management of Newly Diagnosed Patients with Type 2 Diabetes: What Are the Attitudes of Physicians? A Subito!Amd Survey on the Early Diabetes Treatment in Italy. Acta Diabetol. 2012;49(6):429-33. [CrossRef]
- Pawaskar M.; Bilir S.P.; Kowal S.; Li Q.; Weiss T.; Davies G. Cost-effectiveness of intensification with SGLT2 inhibitors for type 2 diabetes. Am J Manag Care. 2021;27(8):e269-e277. [CrossRef]
- Farcher R.; Graber S.M.; Thüring N.; Blozik E.; Huber C.A. Does the Implementation of an Incentive Scheme Increase Adherence to Diabetes Guidelines? A Retrospective Cohort Study of Managed Care Enrollees. BMC Health Serv Res. 2023;3(1):707. [CrossRef]
- Höglinger M.; Wirth B.; Carlander M.; Caviglia C.; Frei C.; Rhomberg B.; Rohrbasser A.; Trottmann M.; Eichler K. Impact of a diabetes disease management program on guideline-adherent care, hospitalization risk and health care costs: a propensity score matching study using real-world data. Eur J Health Econ. 2023;24(3):469-478. [CrossRef]
- Qumseya B.; Goddard A.; Qumseya A.; Estores D.; Draganov P.V.; Forsmark C. Barriers to Clinical Practice Guideline Implementation among Physicians: A Physician Survey. Int J Gen Med. 2021; 14:7591-8. [CrossRef]
- Lugtenberg M.; Burgers J.S.; Westert G.P. Effects of Evidence-Based Clinical Practice Guidelines on Quality of Care: A Systematic Review. Qual Saf Health Care. 2009;18(5):385-92. [CrossRef]
- Wang W.; Choi D.; Yu C.H. Effective Web-Based Clinical Practice Guidelines Resources: Recommendations from a Mixed Methods Usability Study. BMC Prim Care. 2023;24(1):29. [CrossRef]
- Thomas H.; Mitchell G.; Rich J.; Best M. Definition of Whole Person Care in General Practice in the English Language Literature: A Systematic Review. BMJ Open. 2018;8(12):e023758. [CrossRef]
- Vlacho B.; Simarro F.L.; Mata-Cases M.; Miravet S.; Escribano-Serrano J.; Asensio D.; Cortes X.; Franch-Nadal J. Adherence to antidiabetic treatment among patients managed in primary care centres in Spain: the INTENSE study. Prim Care Diabetes. 2022;16(6):760-767. [CrossRef]
- Dankers M.; van den Berk-Bulsink M.J.E.; van Dalfsen-Slingerland M.; Nelissen-Vrancken H.J.M.G.; Mantel-Teeuwisse A.K.; van Dijk L. Non-Adherence to Guideline Recommendations for Insulins: A Qualitative Study Amongst Primary Care Practitioners. BMC Prim Care. 2022;23(1):150. [CrossRef]
- Holmes-Truscott E.; Blackberry I.; O'Neal D.N.; Furler J.S.; Speight J. Willingness to Initiate Insulin among Adults with Type 2 Diabetes in Australian Primary Care: Results from the Stepping up Study. Diabetes Res Clin Pract. 2016;114:126-35. [CrossRef]
- Albarracin D.; Shavitt S. Attitudes and Attitude Change. Annu Rev Psychol. 2018;69:299-327. [CrossRef]
- Wangler J.; Jansky M. What Is the Significance of Guidelines in the Primary Care Setting? : Results of an Exploratory Online Survey of General Practitioners in Germany. Wien Med Wochenschr. 2021;171(13-14):321-9. [CrossRef]
- Wang T.; Tan J.B.; Liu X.L.; Zhao I. Barriers and Enablers to Implementing Clinical Practice Guidelines in Primary Care: An Overview of Systematic Reviews. BMJ Open. 2023; 13(1):e062158. [CrossRef]
- Rushforth B.; McCrorie C.; Glidewell L.; Midgley E.; Foy R. Barriers to Effective Management of Type 2 Diabetes in Primary Care: Qualitative Systematic Review. Br J Gen Pract. 2016; 66(643):e114-27. [CrossRef]
- Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD). Evidence-based European recommendations for the dietary management of diabetes. Diabetologia. 2023;66(6):965-85. [CrossRef]
- Cosentino F.; Grant P.J.; Aboyans V.; Bailey C.J.; Ceriello A.; Delgado V.; Federici M.; Filippatos G.; Grobbee D.E.; Hansen T.B.; et al; ESC Scientific Document Group. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020 ;41(2):255-323. [CrossRef]
- McGuire D.K.; Marx N.; Johansen O.E.; Inzucchi S.E.; Rosenstock J.; George J.T.; FDA Guidance on Antihyperglyacemic Therapies for Type 2 Diabetes: One Decade Later. Diabetes Obes Metab 2019;1(5):1073-8. [CrossRef]
- Lundgren J.R.; Janus C.; Jensen S.B.K.; Juhl C.R.; Olsen L.M.; Christensen R.M.; Svane M.S.; Bandholm T.; Bojsen-Møller K.N.; Blond M.B.; et al. Healthy Weight Loss Maintenance with Exercise, Liraglutide, or Both Combined. N Engl J Med. 2021;384(18):1719-1730. [CrossRef]
- Jastreboff A.M.; Aronne L.J.; Ahmad N.N. Wharton S, Connery L, Alves B, Kiyosue A, Zhang S, Liu B, Bunck MC, et al; SURMOUNT-1 Investigators. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022;387(3):205-216. [CrossRef]
- Khunti K.; Jabbour S.; Cos X.; Mudaliar S.; Mende C.; Bonaca M.; Fioretto P. Sodium-Glucose Co-Transporter-2 Inhibitors in Patients with Type 2 Diabetes: Barriers and Solutions for Improving Uptake in Routine Clinical Practice. Diabetes Obes Metab. 2022;24(7):1187-96. [CrossRef]
- Young K.G.; McInnes E.H.; Massey R.J.; Kahkoska A.R.; Pilla S.J.; Raghavan S.; Stanislawski M.A.; Tobias D.K.; McGovern A.P.; Dawed A.Y.; et al. Treatment Effect Heterogeneity Following Type 2 Diabetes Treatment with GLP1-Receptor Agonists and SGLT2-inibitors: A Systematic Review. Commun Med (Lond). 2023;3(1):131. [CrossRef]
- Melo M.; Gavina C.; Silva-Nunes J.; Andrade L.; Carvalho D. Heterogeneity Amongst GLP-1 RA Cardiovascular Outcome Trials Results: Can Definition of Established Cardiovascular Disease Be the Missing Link? Diabetol Metab Syndr. 2021;13(1):81. [CrossRef]
- Schönberger E.; Mihaljević V.; Steiner K.; Šarić S.; Kurevija T.; Majnarić L.T.; Bilić Ćurčić I.; Canecki-Varžić S. Immunomodulatory Effects of SGLT2 Inhibitors-Targeting Inflammation and Oxidative Stress in Aging. Int J Environ Res Public Health. 2023;20(17). [CrossRef]
- Tilinca M.C.; Tiuca R.A.; Tilea I.; Varga A. The SGLT-2 Inhibitors in Personalized Therapy of Diabetes Mellitus Patients. J Pers Med. 2021;11(12):1249. [CrossRef]
- Grant R.; Adams A.S.; Trinacty C.M.; Zhang F.; Kleinman K.; Soumerai S.B.; Meigs J.B.; Ross-Degnan D. Relationship between Patient Medication Adherence and Subsequent Clinical Inertia in Type 2 Diabetes Glycemic Management. Diabetes Care. 2007;30(4):807-12. [CrossRef]
- Khunti K.; Aroda V.R.; Bhatt D.L.; Bozkurt B.; Buse J.B.; Heerspink H.L.; Inzucchi S.E.; Lam C.S.P.; Marx N.; McMurray J.J.V.; et al. Re-examining the widespread policy of stopping sodium-glucose cotransporter-2 inhibitors during acute illness: A perspective based on the updated evidence. Diabetes Obes Metab. 2022;24(11):2071-80. [CrossRef]
- Faillie JL. Pharmacological aspects of the safety of gliflozins. Pharmacol Res. 2017;118:71-81. [CrossRef]
- Bechmann L.E.; Emanuelsson F.; Nordestgaard B.G.; Benn M. SGLT2-inibition increases total, LDL, and HDL cholesterol and lowers triglycerides: Meta-analyses of 60 randomized trials, overall and by dose, ethnicity, and drug type. Atherosclerosis. 2023:117236. [CrossRef]
- Castellana M.; Procino F.; Sardone R.; Trimboli P.; Giannelli G. Generalizability of Sodium-Glucose Co-Transporter-2 Inhibitors Cardiovascular Outcome Trials to the Type 2 Diabetes Population: A Systematic Review and Meta-Analysis. Cardiovasc Diabetol. 2020;19(1):87. [CrossRef]
- Schnell O.; Battelino T.; Bergenstal R.; Birkenfeld A.L.; Ceriello A.; Cheng A.; Davies M.; Edelman S.; Forst T.; Giorgino F.; et al. CVOT Summit 2022 Report: new cardiovascular, kidney, and glycemic outcomes. Cardiovasc Diabetol. 2023;22(1):59. [CrossRef]
- Goldman A.; Fishman B.; Twig G.; Raschi E.; Cukierman-Yaffe T.; Moshkovits Y.; Pomerantz A.; Ben-Zvi I.; Dankner R.; Maor E. The real-world safety profile of sodium-glucose co-transporter-2 inhibitors among older adults (≥ 75 years): a retrospective, pharmacovigilance study. Cardiovasc Diabetol. 2023;22(1):16. [CrossRef]
- Lugtenberg M.; Zegers-van Schaick J.M.; Westert G.P.; Burgers J.S. Why Don't Physicians Adhere to Guideline Recommendations in Practice? An Analysis of Barriers among Dutch General Practitioners. Implement Sci. 2009;4:54. [CrossRef]
- Morley J.E.; Abbatecola A.M.; Woo J. Management of comorbidities in older persons with type 2 diabetes. J. Am. Med. Dir Assoc. 2017;18(8):639–45. [CrossRef]
- Nguyen T.N.; Harris K.; Woodward M.; Chalmers J.; Cooper M.; Hamet P.; Harrap S.; Heller S.; MacMahon S.; Mancia G.; et al. The Impact of Frailty on the Effectiveness and Safety of Intensive Glucose Control and Blood Pressure-Lowering Therapy for People With Type 2 Diabetes: Results From the ADVANCE Trial. Diabetes Care. 2021;44(7):1622-1629. [CrossRef]
- Strain W.D.; Down S.; Brown P.; Puttanna A.; Sinclair A. Diabetes and Frailty: An Expert Consensus Statement on the Management of Older Adults with Type 2 Diabetes. Diabetes Ther. 2021;12(5):1227-47. [CrossRef]
- Abd Ghafar M.Z.A.; O'Donovan M.; Sezgin D.; Moloney E.; Rodríguez-Laso Á.; Liew A.; O'Caoimh R. Frailty and Diabetes in Older Adults: Overview of Current Controversies and Challenges in Clinical Practice. Front Clin Diabetes Healthc. 2022;3:895313. [CrossRef]
- Kondo T.; Adachi T.; Kobayashi K.; Okumura T.; Izawa H.; Murohara T.; et al. Physical Frailty and Use of Guideline-Recommended Drugs in Patients with Heart Failure and Reduced Ejection Fraction. J Am Heart Assoc. 2023;12(12):e026844. [CrossRef]
- Fried L.P.; Tangen C.M.; Walston J.; Newman A.B.; Hirsch C.; Gottdiener J.; Seeman T.; Tracy R.; Kop W.J.; Burke G.; et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-56. [CrossRef]
- Nixon A.C.; Bampouras T.M.; Pendleton N.; Woywodt A.; Mitra S.; Dhaygude A.; Frailty and Chronic Kidney Disease: Current Evidence and Continuing Uncertainties. Clin Kidney J. 2018;11(2):236-45. [CrossRef]
- Kleipool E.E.; Hoogendijk E.O.; Trappenburg M.C.; Handoko M.L.; Huisman M.; Peters M.J.; Muller M. Frailty in Older Adults with Cardiovascular Disease: Cause, Effect or Both? Aging Dis. 2018;9(3):489-97. [CrossRef]
- Abdelhafiz A.H.; Emmerton D., Sinclair A.J. Impact of Frailty Metabolic Phenotypes on the Management of Older People with Type 2 Diabetes Mellitus. Geriatr Gerontol Int. 2021;21(8):614-22. [CrossRef]
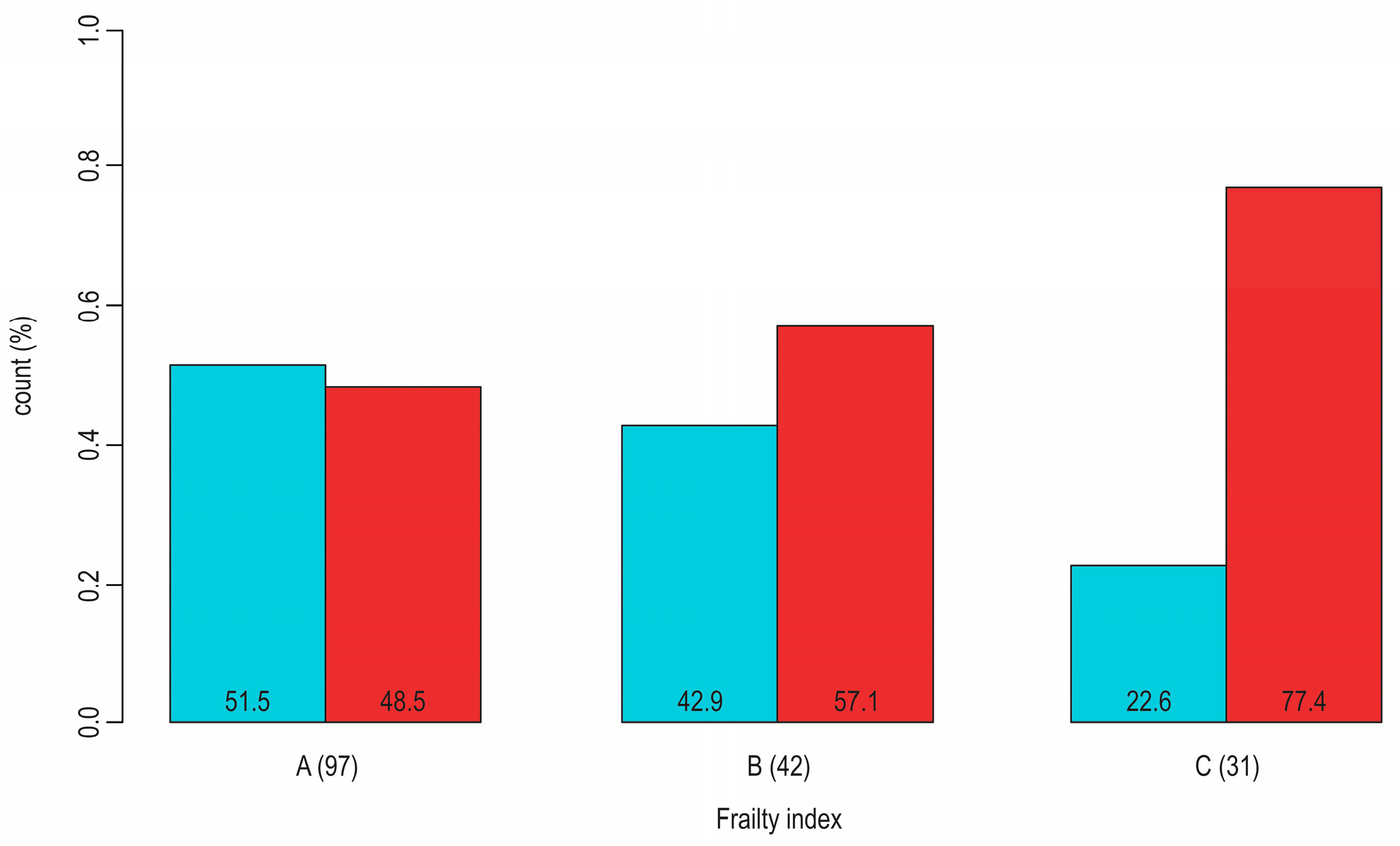
- Gordon E.H.; Peel N.M.; Samanta M.; Theou O.; Howlett S.E.; Hubbard R.E. Sex Differences in Frailty: A Systematic Review and Meta-Analysis. Exp Gerontol. 2017;89:30-40. [CrossRef]
- Cohen A.A.; Legault V.; Li Q.; Fried L.P.; Ferrucci L. Men Sustain Higher Dysregulation Levels Than Women without Becoming Frail. J Gerontol A Biol Sci Med Sci. 2018;73(2):175-84. [CrossRef]
- Wang Y.; O'Neil A.; Jiao Y.; Wang L.; Huang J.; Lan Y.; Zhu Y.; Yu C. Sex differences in the association between diabetes and risk of cardiovascular disease, cancer, and all-cause and cause-specific mortality: a systematic review and meta-analysis of 5,162,654 participants. BMC Med. 2019;17(1):136. [CrossRef]
- Denfeld Q.E.; Habecker B.A.; Camacho S.A.; Roberts Davis M.; Gupta N.; Hiatt S.O.; Medysky M.E.; Purnell J.Q.; Winters-Stone K.; Lee C.S. Characterizing Sex Differences in Physical Frailty Phenotypes in Heart Failure. Circ Heart Fail. 2021;14(9):e008076. [CrossRef]
- Lin T.K.; Lee M.C.; Cheng Y.H.; Ma T.; Chen M.C.; Yang T.Y.; Jong G.P. The Association between SGLT2 Inhibitors and New-Onset Acute Coronary Syndrome in the Elderly: A Population-Based Longitudinal Cohort Study. Diabetol Metab Syndr. 2023;15(1):170. [CrossRef]
- Leong D.P.; Joseph P.; McMurray J.J.V.; Rouleau J.; Maggioni A.P.; Lanas F.; Sharma S.K.; Núñez J.; Mohan B.; Celik A.; et al. Frailty and outcomes in heart failure patients from high-, middle-, and low-income countries. Eur Heart J. 2023;44(42):4435-4444. 4435. [CrossRef]
- Kutz A.; Kim D.H.; Wexler D.J.; Liu J.; Schneeweiss S.; Glynn R.J.; Patorno E. Comparative Cardiovascular Effectiveness and Safety of SGLT-2 Inhibitors, GLP-1 Receptor Agonists, and DPP-4 Inhibitors According to Frailty in Type 2 Diabetes. Diabetes Care. 2023;46(11):2004-14. [CrossRef]
- Strain W.; Griffiths J. A Systematic Review and Meta-Analysis of the Impact of GLP-1 Receptor Agonists and SGLT-2 Inhibitors on Cardiovascular Outcomes in Biologically Healthy Older Adults. The British Journal of Diabetes. 2021;21(1). [CrossRef]
- Karagiannis T.; Tsapas A.; Athanasiadou E.; Avgerinos I.; Liakos A.; Matthews D.R.; Bekiari E. GLP-1 Receptor Agonists and SGLT2 Inhibitors for Older People with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabetes Res Clin Pract. 2021;174:108737. [CrossRef]
- Vart P.; Butt J.H.; Jongs N.; Schechter M.; Chertow G.M.; Wheeler D.C.; Pecoits-Filho R.; Langkilde A.M.; Correa-Rotter R.; Rossing P.; et al. Efficacy and Safety of Dapagliflozin in Patients With Chronic Kidney Disease Across the Spectrum of Frailty. J Gerontol A Biol Sci Med Sci. 2024;79(2):glad181. [CrossRef]
- Chung W.K., Erion K., Florez J.C.; Hattersley A.T.; Hivert M.F.; Lee C.G.; McCarthy M.I.; Nolan J.J.; Norris J.M.; Pearson E.R.; et al. Precision medicine in diabetes: a Consensus Report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2020;63(9):1671-1693. [CrossRef]
- Griffin S. Diabetes precision medicine: plenty of potential, pitfalls and perils but not yet ready for prime time. Diabetologia. 2022;65(11):1913-21. [CrossRef]
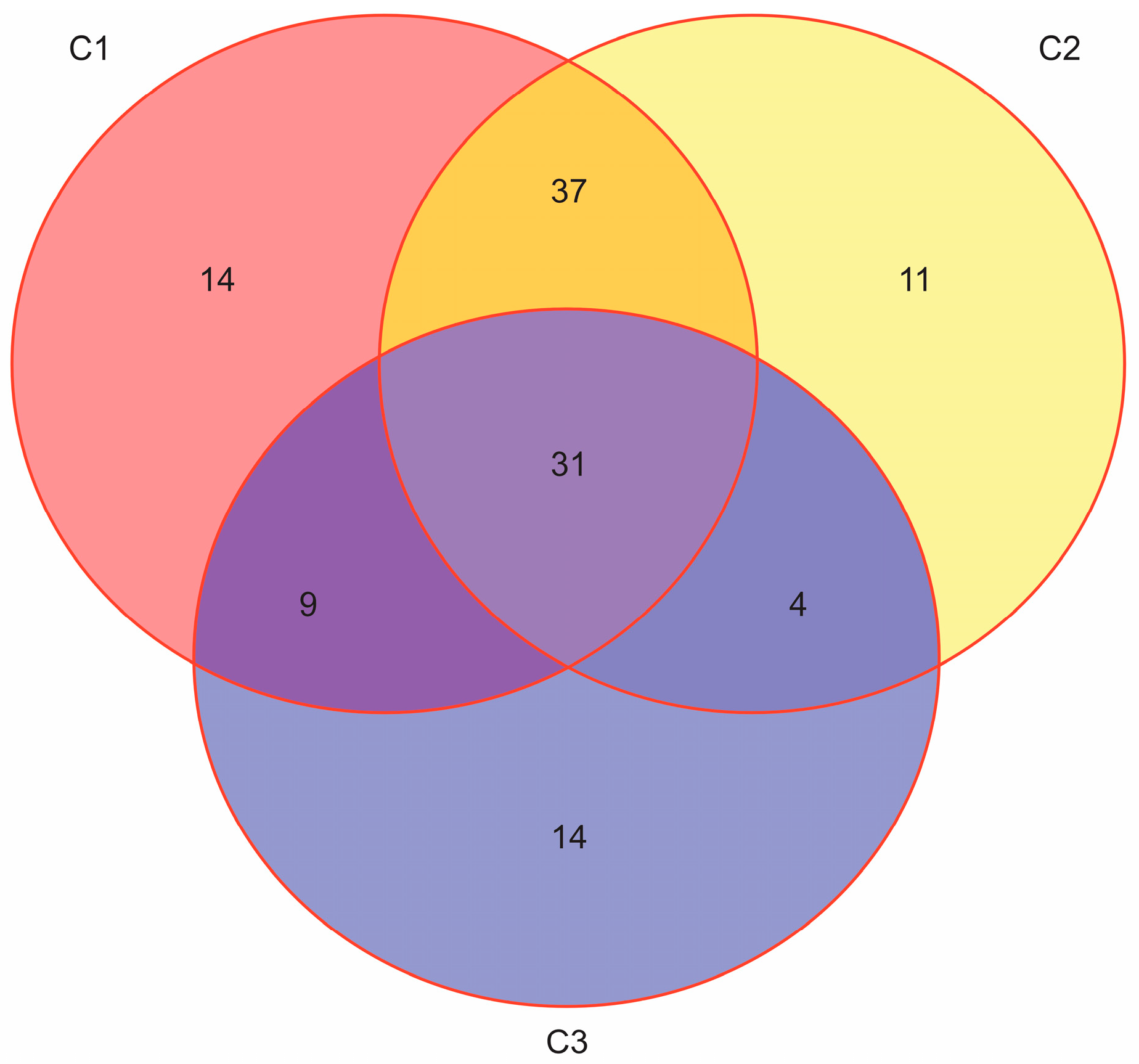
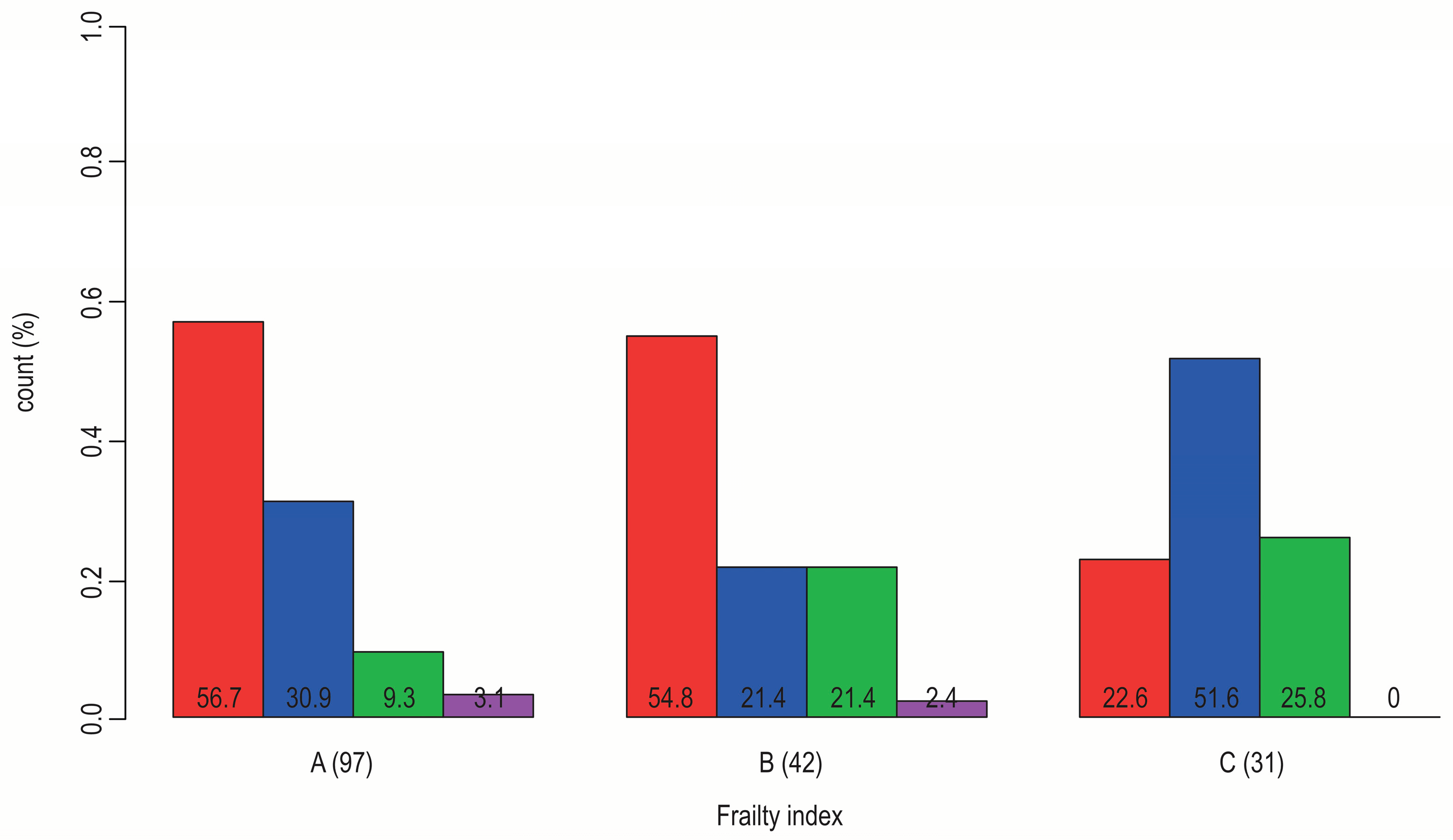
- Bosnić Z.; Yildirim P.; Babič F.; Šahinović I.; Wittlinger T.; Martinović I.; Majnaric L.T.; Clustering Inflammatory Markers with Sociodemographic and Clinical Characteristics of Patients with Diabetes Type 2 Can Support Family Physicians' Clinical Reasoning by Reducing Patients' Complexity. Healthcare (Basel). 2021;9(12). [CrossRef]
- Bosnić Z.; Babič F.; Anderková V.; Štefanić M.; Wittlinger T.; Majnarić L.T. A Critical Appraisal of the Diagnostic and Prognostic Utility of the Anti-Inflammatory Marker IL-37 in a Clinical Setting: A Case Study of Patients with Diabetes Type 2. Int J Environ Res Public Health. 2023;20(4). [CrossRef]
- Bosnić Z.; Babič F.; Wittlinger T.; Anderková V.; Šahinović I.; Majnarić L.T. Influence of Age, Gender, Frailty, and Body Mass Index on Serum IL-17a Levels in Mature Type 2 Diabetic Patients. Med Sci Monit. 2023:29:e940128. [CrossRef]
- Zoungas S.; Woodward M.; Li Q.; Cooper M.E.; Hamet P.; Harrap S.; Heller S.; Marre M.; Patel A.; Poulter N.; et al; ADVANCE Collaborative group. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 2014;57(12):2465-74. [CrossRef]
- Matsushita K.; Kaptoge S.; Hageman S.H.J.; Sang Y.; Ballew S.H.; Grams M.E.; Surapaneni A.; Sun L.; Arnlov J.; Bozic M.; et al. Including measures of chronic kidney disease to improve cardiovascular risk prediction by SCORE2 and SCORE2-OP. Eur J Prev Cardiol. 2023;30(1):8-16. [CrossRef]
- de Boer I.H.; Khunti K.; Sadusky T.; Tuttle K.R.; Neumiller J.J.; Rhee C.M.; Rosas S.E.; Rossing P.; Bakris G. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2022;102(5):974-989. [CrossRef]
- SCORE2-Diabetes Working Group and the ESC Cardiovascular Risk Collaboration, SCORE2-Diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in Europe. European Heart Journal. 2023;44(28):2544-56. [CrossRef]
- Cebrián-Cuenca A.M.; Mata-Cases M.; Franch-Nadal J.; Mauricio D.; Orozco-Beltrán D.; Consuegra-Sánchez L. Half of patients with type 2 diabetes mellitus are at very high cardiovascular risk according to the ESC/EASD: data from a large Mediterranean population. Eur J Prev Cardiol. 2022;28(18):e32-e34. [CrossRef] [PubMed]
- Galbete A.; Tamayo I..; Librero J.; Enguita-Germán M.; Cambra K.; Ibáñez-Beroiz B.; CONCEPT group. Cardiovascular risk in patients with type 2 diabetes: A systematic review of prediction models. Diabetes Res Clin Pract. 2022;184:109089. [CrossRef]
- Dziopa K.; Asselbergs F.W.; Gratton J.; Chaturvedi N.; Schmidt A.F. Cardiovascular Risk Prediction in Type 2 Diabetes: A Comparison of 22 Risk Scores in Primary Care Settings. Diabetologia. 2022;65(4):644-56. [CrossRef]
- Rydén L.; Ferrannini G.; Standl E. Risk prediction in patients with diabetes: is SCORE 2D the perfect solution? Eur Heart J. 2023;44(28):2557-2559. [CrossRef]
- Fang M.; Wang D.; Tang O.; McEvoy J.W.; Echouffo-Tcheugui J.B.; Christenson R.H.; Selvin E. Subclinical Cardiovascular Disease in US Adults With and Without Diabetes. J Am Heart Assoc. 2023;12(11):e029083. [CrossRef]
- De Rosa S.; Arcidiacono B.; Chiefari E.; Brunetti A.; Indolfi C.; Foti DP. Type 2 Diabetes Mellitus and Cardiovascular Disease: Genetic and Epigenetic Links. Front Endocrinol (Lausanne). 2018;9:2. [CrossRef]
- van Bussel E.F.; Richard E.; Busschers W.B.; Steyerberg E.W.; van Gool W.A.; Moll van Charante E.P.; Hoevenaar-Blom M.P. A Cardiovascular Risk Prediction Model for Older People: Development and Validation in a Primary Care Population. J Clin Hypertens (Greenwich). 2019;21(8):1145-52. 1145. [CrossRef]
- van Bussel E.F.; Hoevenaar-Blom M.P.; Poortvliet R.K.E.; Gussekloo J.; van Dalen J.W.; van Gool W.A.; Richard E.; Moll van Charante E.P. Predictive value of traditional risk factors for cardiovascular disease in older people: A systematic review. Prev Med. 2020;132:105986. [CrossRef]
- Madonna R.; Balistreri C.R.; De Rosa S.; Muscoli S.; Selvaggio S.; Selvaggio G.; Ferdinandy P.; De Caterina R. Impact of Sex Differences and Diabetes on Coronary Atherosclerosis and Ischemic Heart Disease. J Clin Med. 2019;8(1):98. [CrossRef]
- Frisoli A. Jr.; Ingham S.J.; Paes Â.T.; Tinoco E.; Greco A.; Zanata N.; Pintarelli V.; Elber I.; Borges J.; Camargo Carvalho A.C. Frailty predictors and outcomes among older patients with cardiovascular disease: Data from Fragicor. Arch Gerontol Geriatr. 2015;61(1):1-7. [CrossRef]
- Khoury M.J.; Galea S. Will Precision Medicine Improve Population Health? JAMA. 2016;316(13):1357-8. [CrossRef]
- Franceschi C.; Garagnani P.; Morsiani C.; Conte M.; Santoro A.; Grignolio A.; Monti D.; Capri M.; Salvioli S. The Continuum of Aging and Age-Related Diseases: Common Mechanisms but Different Rates. Front Med (Lausanne). 2018;5:61. [CrossRef]
- Chaturvedi R.R.; Angrisani M.; Troxel W.M.; Gutsche T.; Ortega E.; Jain M.; Boch A.; Kapteyn A. American Life in Realtime: a benchmark registry of health data for equitable precision health. Nat Med. 2023;29(2):283-286. [CrossRef]
- Majnarić L.T.; Babič F.; O'Sullivan S.; Holzinger A. AI and Big Data in Healthcare: Towards a More Comprehensive Research Framework for Multimorbidity. J Clin Med. 2021;10(4). [CrossRef]
| Physician-related factors: | Patient-related factors: | Healthcare-related factors: |
|---|---|---|
| Lack of knowledge about the illness Overlooking the seriousness of the symptoms Not starting the treatment Inability to identify clinical outcomes Not adjusting the treatment until the intended result has been attained Inability to recognize and address comorbid condition Patient takes over the therapeutic discussion and decision Lack of knowledge about the illness Reactive care as opposed to a proactive treatment strategy |
Refuse to accept having the illness Non-existence of symptoms Inadequate knowledge regarding the health Considering that the illness is not severe Taking too many medications Financial limitation (cost of medications) The negative effects of medications Aspects of lifestyle Ineffective patient-doctor communication (lack of trust) |
The absence of clinical guidelines No database of morbidity or illness registries No visit strategy (not scheduling appointments) Absence of decision assistance and team-based careInsufficient funds and time Technical deficiency |
| Heterogeneous treatment effects | Possible side effects |
|---|---|
|
Higher baseline HbA1c values are associated with greater glycaemic response. GLP-1ra: there is no proof that renal function affects the response to glucose; SGLT2-in: lessened glycaemic response in patients with diminished kidney function. There isn't any reliable proof that body mass index significantly modifies the glycaemic response. GLP-1ra: less glycaemic response is linked to longer duration of diabetes; SGLT2-in: the length of diabetes does not consistently affect glycaemic response. GLP-1ra: no proof that aging affects glycaemic response; SGLT2-in: some research indicates that an older age may be linked to a lower glycaemic response. No reliable proof that gender or ethnicity significantly modifies the glycaemic response. SGLT2-in: no indication of variation in the reaction to treatment for patients with obstructive sleep apnea or for insulin secretion and insulin; GLP-1ra: studies indicate that lower fasting C-peptide and lower urine C-peptide-to-creatinine ratio, are linked to a reduced glycaemic response. |
Concerns regarding the start of SGLT2-in in patients with CVD or kidney illness, as well as the necessity of close observation of diabetic ketoacidosis (DKA) in cases of COVID-19 or other acute conditions requiring hospitalization. There is a higher risk of genital and urinary tract infections, which can be attributed to prolonged and increased glycosuria. Raised concerns about gliflozin-induced cancers (bladder and breast cancer), even though causality cannot be established. More research is required. Gliflozins cannot rule out drug-induced liver damage. Due to SGLT1 transporters' reduced inhibition there may be a lower risk of severe hypoglycemia when using gliflozins. Hypovolemic events are frequent with gliflozins and DKA can appear infrequently and be more challenging to diagnose. Gliflozins-associated fracture risk is likely influenced by a number of variables that require additional research. Symptoms of glucose-galactose malabsorption were uncommon in clinical trials. Renal function needs to be regularly monitored due to a possible reduction in GFR. Elderly patient and with renal impairment should use much more caution. There is a link to a greater rise in the less atherogenic significant LDL-C subfraction. The ratio of LDL-C to HDL-C remains nearly unaltered because of a concurrent rise in HDL-C. |
| Study (design) |
Findings summary |
|---|---|
| Lin TK, et al., 2023. (population-based longitudinal cohort study) [74] |
SGLT2-in use was associated with a non-significantly decreased risk of ACS. No difference in the SGLT2-in subtype was observed in subgroup analyses. The results indicated an increased risk for the incidence of ACS in male and older (> 70 years) patients. |
| Leong DP, et al., 2023. (population-based longitudinal cohort study) [75] |
Frailty confers substantial incremental prognostic information to prognostic variables for predicting death and hospitalization in heart failure patients. The relationship between frailty and these outcomes is consistent across countries at all income levels. |
| Kutz A, et al, 2023. (1:1 propensity score-matched cohort studies) [76] |
SGLT2-in and GLP-1ra safely improved CV outcomes and all-cause mortality, with the largest absolute benefits among frail people. |
|
Young KG, et al., 2023. (a systematic review) [49] |
Current evidence on treatment effect heterogeneity for SGLT2-in and GLP-1ra therapies is limited, likely reflecting the methodological limitations of published studies. Robust and appropriately powered studies are required to understand T2D treatment effect heterogeneity. |
| Strain WD, Griffiths J, 2021. (a systematic review and meta-analysis) [77] |
GLP-1ra and SGLT2-in reduced MACE outcomes in older adults who were eligible to participate in clinical trials. Whereas this is reassuring for the biologically robust, it should not be extrapolated to frail older adults without further investigation. |
|
Karagiannis T, et al., 2021. (a systematic review and meta-analysis) [78] Vart P, et al., 2023. (a randomized controlled trial) [79] |
In older adults (≥65) with T2D, GLP-1ra reduced MACE and its components. SGLT2-in reduced MACE, heart failure, and renal outcomes. The relative benefit of dapagliflozin in patients with chronic kidney disease (with/without T2D) for all outcomes was consistent across all frailty categories, with no difference in associated safety. |
| Research | Guidelines development | Knowledge implementation |
|---|---|---|
| More comprehensive patient profiling for CVOTs Real-world data-driven research Patient clustering based on multiple descriptors (including comorbidity patterns) Research intensification on the treatment effects of non-pharmacological interventions, in particular including psychological factors New biomarkers exploration Integrated models of care Qualitative research – assessing family doctors` attitudes Translation research intensification |
Clear division of areas where there is no support by evidence Case report, Examples dealing with real-life experience Monitoring for the side effects of the treatment regimens The effects of comorbidity and frailty on treatment outcomes Evidence provided by cluster-analyses Clear recommendations on when to intensify and when to de-escalate therapy Clear statements on when to start with the cardio-protective therapy in the course of the disease The effects on outcomes of non-pharmacological interventions, in particular, concerning psychological factors Problem-solving approach Guidelines adaptation for use in primary care |
Continuous knowledge translation Educational training modules for healthcare providers, health policy officials, and patients Learning on case reports Audit analysis of real-world data with the support of information technology Implementation of care protocols and workflows Empowerment of family doctors in life science knowledge The establishment of the platform for data collection and curation from electronic health records, smartphones, and wearables; Data selection for data-driven modeling The results of data modeling become visible in the workplace by using AI visual techniques |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





