Submitted:
22 February 2024
Posted:
24 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Design and Population
2.3. Study Data
- -
- Date of admission to the emergency department.
- -
- Date of admission to the hospital.
- -
- Date of symptom onset.
- -
- Date of microbiological confirmation of SARS-CoV-2 infection.
- -
- Any life support limitations and date implemented.
- -
- Whether the patient needed ICU admission.
- -
- ICU admission date.
- -
- Mortality risk assessed by the CURB-65 scale.
- -
- Level of consciousness evaluated using the Glasgow Coma Scale.
- -
- Other clinical variables in the first 24 hours: fever (≥ 38ºC), RR > 24 breaths/minute, systolic blood pressure < 90 mmHg, SpO2, and number of lung quadrants affected in imaging tests (ranging from 1 to 4).
- -
- Severity of illness assessed using the APACHE II scale within the first 24 hours of admission
- -
- Patient's condition evaluated using the SOFA scale during their ICU stay.
- -
- Affected side (bilateral or unilateral)
- -
- Type of lung injury (ground-glass opacity, consolidation, or mixed)
- -
- Density pattern (patchy, confluent, or mixed)
- -
- Oxygen therapy
- -
- Non-invasive ventilation (NIV)
- -
- IMV
- -
- Prone ventilation
- -
- Hemodialysis/hemofiltration
- -
- Extracorporeal membrane oxygenation
2.4. Method
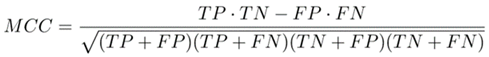
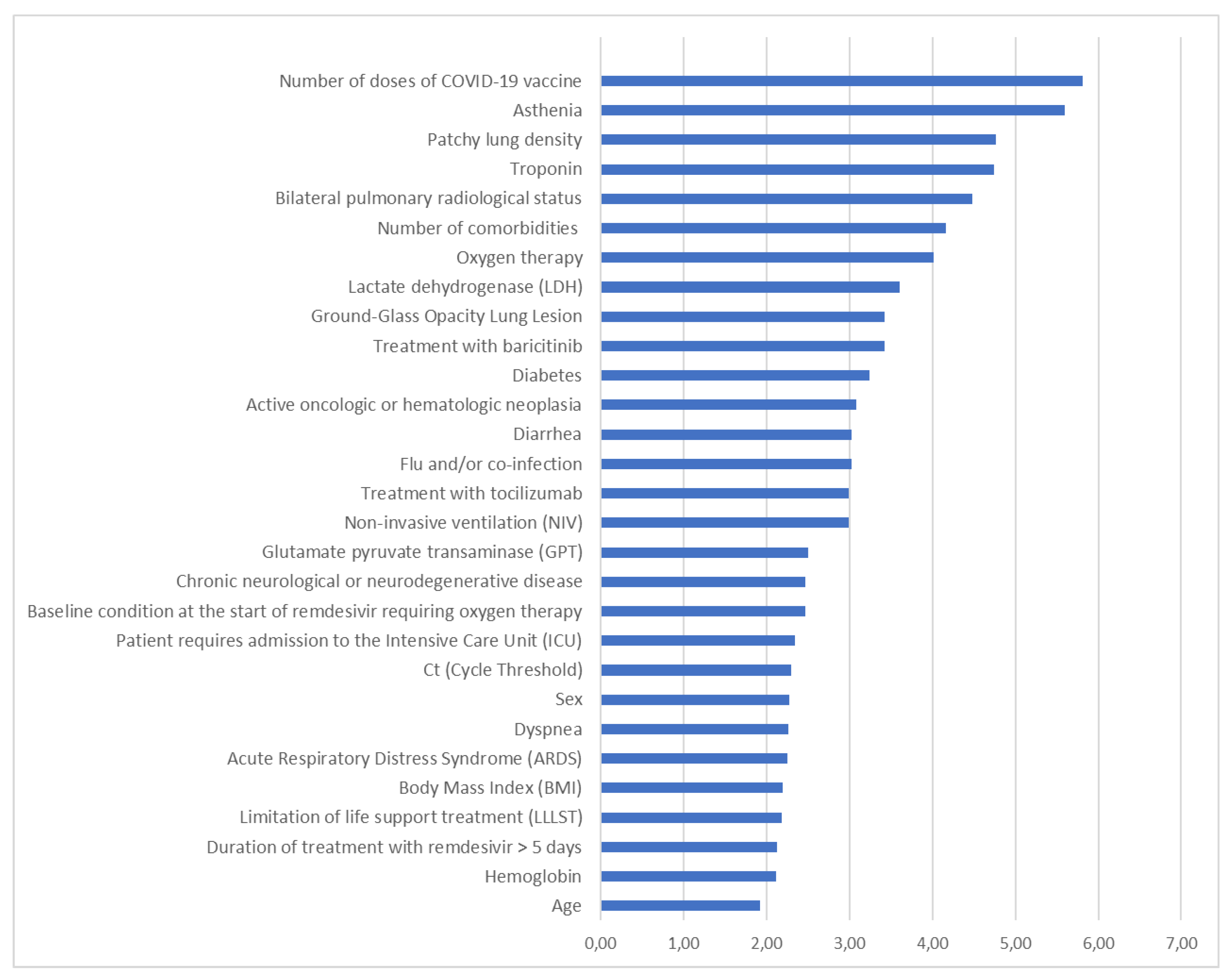
2.4.1. Model Development
2.4.2. Performance Evaluation
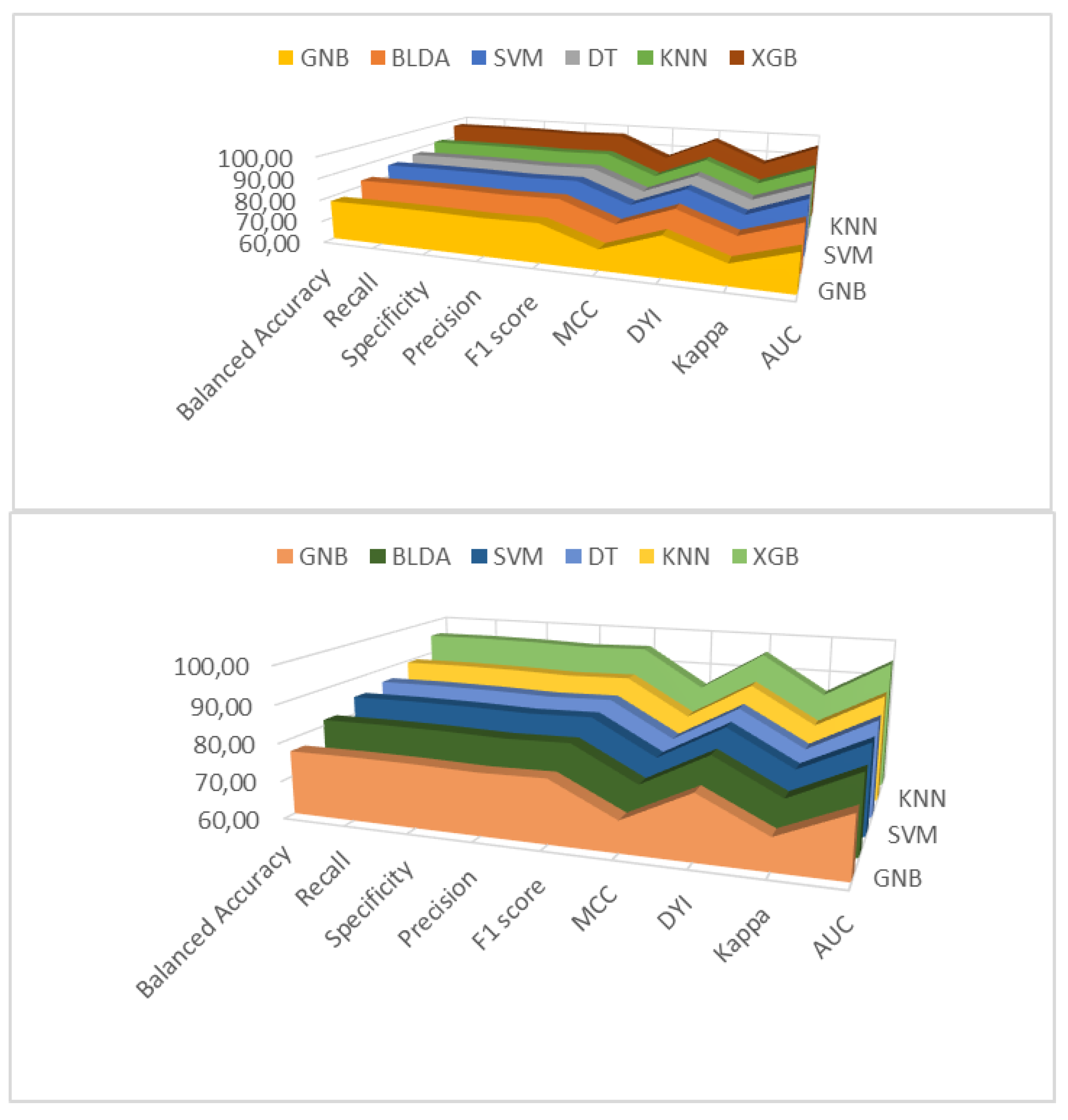
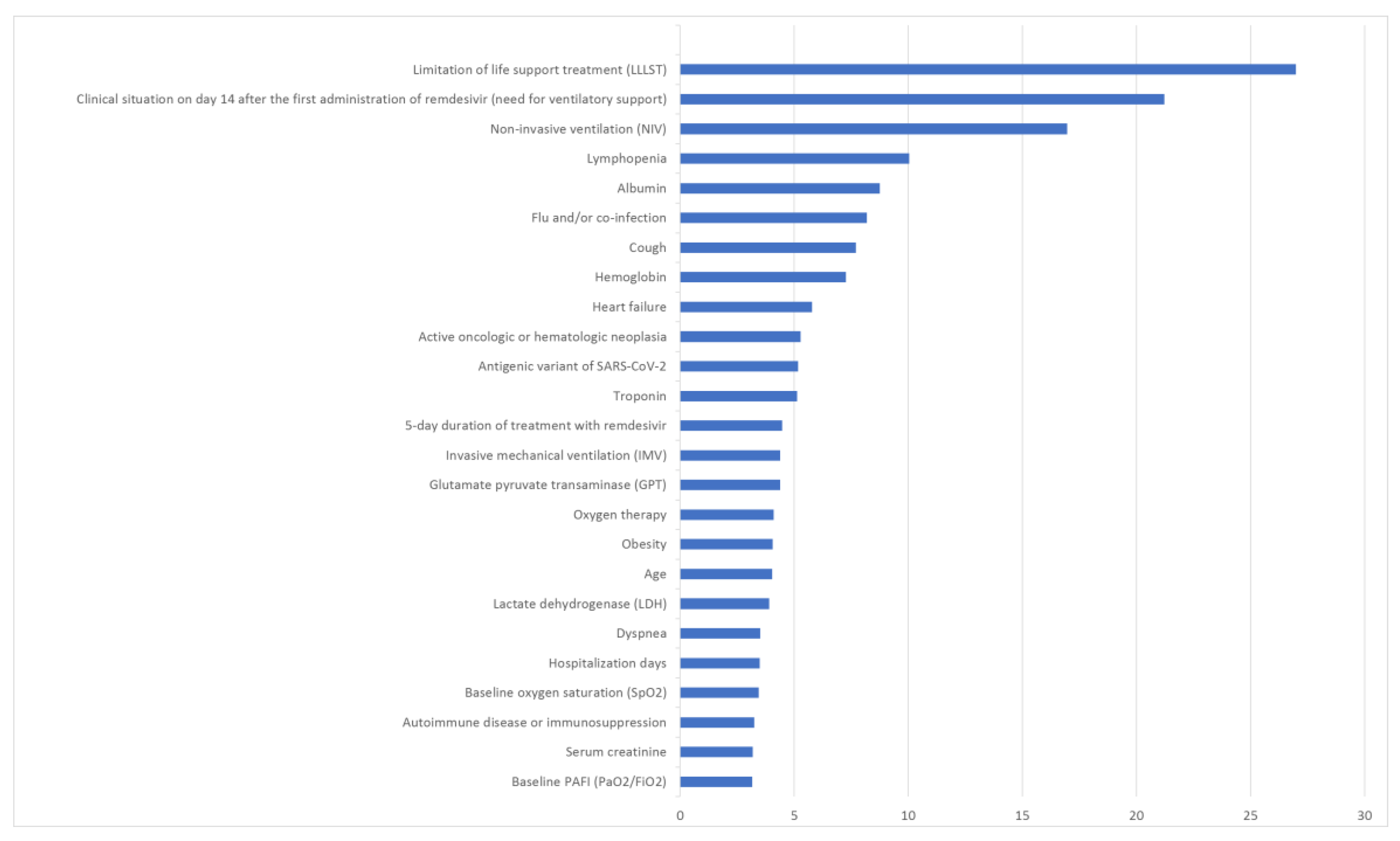
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lu, R.; Zhao, X.; Li, J.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020, 395, 565–574. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Coronavirus disease 2019 (COVID-19) outbreak [Internet]. Geneva: World Health Organization; [cited 2024 Feb 12]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- Yuan, Z.; Shao, Z.; Ma, L.; Guo, R. Clinical Severity of SARS-CoV-2 Variants during COVID-19 Vaccination: A Systematic Review and Meta-Analysis. Viruses. 2023, 15, Published 2023 Sep 26. [Google Scholar] [CrossRef]
- Chen, Z.; Tian, F. Evaluation of oral small molecule drugs for the treatment of COVID-19 patients: a systematic review and network meta-analysis. Ann Med. 2023, 55, 2274511. [Google Scholar] [CrossRef] [PubMed]
- Qin, Z.; Li, Y.; Sun, W.; et al. Effect of anti-inflammatory drugs on the storm of inflammatory factors in respiratory tract infection caused by SARS-CoV-2: an updated meta-analysis. Front Public Health 2023, 11, 1198987, Published 2023 Oct 2. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China [published correction appears in JAMA. 2021 Mar 16;325(11):1113]. JAMA. 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, A.; Hamilton, J.P.; Alqahtani, S.A.; Woreta, T.A. A narrative review of coronavirus disease 2019 (COVID-19): clinical, epidemiological characteristics, and systemic manifestations. Intern Emerg Med. 2021, 16, 815–830. [Google Scholar] [CrossRef]
- Thapa, K.; Verma, N.; Singh, T.G.; Kaur Grewal, A.; Kanojia, N.; Rani, L. COVID-19-Associated acute respiratory distress syndrome (CARDS): Mechanistic insights on therapeutic intervention and emerging trends. Int Immunopharmacol. 2021, 101 (Pt A), 108328. [Google Scholar] [CrossRef]
- Wang, Z.; Deng, H.; Ou, C.; et al. Clinical symptoms, comorbidities and complications in severe and non-severe patients with COVID-19: A systematic review and meta-analysis without cases duplication. Medicine (Baltimore). 2020, 99, e23327. [Google Scholar] [CrossRef]
- Sungnak, W.; Huang, N.; Bécavin, C.; et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020, 26, 681–687. [Google Scholar] [CrossRef]
- Zeng, F.; Huang, Y.; Guo, Y.; et al. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int J Infect Dis. 2020, 96, 467–474. [Google Scholar] [CrossRef]
- Gordon, C.J.; Tchesnokov, E.P.; Woolner, E.; et al. Remdesivir is a direct-acting antiviral that inhibits RNA-dependent RNA polymerase from severe acute respiratory syndrome coronavirus 2 with high potency. J Biol Chem. 2020, 295, 6785–6797. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; et al. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef]
- Spinner, C.D.; Gottlieb, R.L.; Criner, G.J.; et al. Effect of Remdesivir vs Standard Care on Clinical Status at 11 Days in Patients With Moderate COVID-19: A Randomized Clinical Trial. JAMA. 2020, 324, 1048–1057. [Google Scholar] [CrossRef] [PubMed]
- Goldman, J.D.; Lye, D.C.B.; Hui, D.S.; et al. Remdesivir for 5 or 10 Days in Patients with Severe Covid-. N Engl J Med. 2020, 383, 1827–1837. [Google Scholar] [CrossRef]
- WHO Solidarity Trial Consortium; Pan, H.; Peto, R.; et al. Repurposed Antiviral Drugs for Covid-19 - Interim WHO Solidarity Trial Results. N Engl J Med. 2021, 384, 497–511. [Google Scholar] [CrossRef]
- WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: final results of the WHO Solidarity randomised trial and updated meta-analyses [published correction appears in Lancet. 2022 Oct 29;400(10362):1512] [published correction appears in Lancet. 2024 Jan 13;403(10422):146]. Lancet. 2022, 399, 1941–1953. [Google Scholar] [CrossRef]
- Vollmer, S.; Mateen, B.A.; Bohner, G.; et al. Machine learning and artificial intelligence research for patient benefit: 20 critical questions on transparency, replicability, ethics, and effectiveness [published correction appears in BMJ. 2020 Apr 1;369:m1312]. BMJ. 2020, 368, l6927, Published 2020 Mar 20. [Google Scholar] [CrossRef] [PubMed]
- Syeda, H.B.; Syed, M.; Sexton, K.W.; et al. Role of Machine Learning Techniques to Tackle the COVID-19 Crisis: Systematic Review. JMIR Med Inform. 2021, 9, e23811, Published 2021 Jan 11. [Google Scholar] [CrossRef]
- Rasheed, J.; Jamil, A.; Hameed, A.A.; Al-Turjman, F.; Rasheed, A. COVID-19 in the Age of Artificial Intelligence: A Comprehensive Review. Interdiscip Sci. 2021, 13, 153–175. [Google Scholar] [CrossRef]
- Chen, C.; Dong, D.; Qi, B.; Petersen, I.R.; Rabitz, H. Quantum Ensemble Classification: A Sampling-Based Learning Control Approach. IEEE Trans Neural Netw Learn Syst. 2017, 28, 1345–1359. [Google Scholar] [CrossRef]
- Chang, W.; Liu, Y.; Wu, X.; Xiao, Y.; Zhou, S.; Cao, W. A New Hybrid XGBSVM Model: Application for Hypertensive Heart Disease. IEEE Access. 2019, 7, 175248–175258. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. 2016. Xgboost: A scalable tree boosting system, in: Proceedings of the 22nd acm sigkdd international conference on knowledge discovery and data mining, August 13, 2016. San Francisco, California, USA, 785-794.
- Mateo, J.; Rius-Peris, J.M.; Maraña-Pérez, A.I.; Valiente-Armero, A.; Torres, A.M. Extreme gradient boosting machine learning method for predicting medical treatment in patients with acute bronchiolitis. Biocybern Biomed Eng. 2021, 41, 792–801. [Google Scholar] [CrossRef]
- Rivera-Lopez, R.; Canul-Reich, J. Construction of Near-Optimal Axis-Parallel Decision Trees Using a Differential-Evolution-Based Approach. IEEE Access. 2018, 6, 5548–5563. [Google Scholar] [CrossRef]
- Das, B.K.; Dutta, H.S. GFNB: Gini index-based Fuzzy Naive Bayes and blast cell segmentation for leukemia detection using multi-cell blood smear images. Med Biol Eng Comput. 2020, 58, 2789–2803. [Google Scholar] [CrossRef] [PubMed]
- Ma, D.; Yuan, S.; Shang, J.; et al. The Automatic Detection of Seizure Based on Tensor Distance And Bayesian Linear Discriminant Analysis. Int J Neural Syst. 2021, 31, 2150006. [Google Scholar] [CrossRef] [PubMed]
- Xing, W.; Bei, Y. Medical Health Big Data Classification Based on KNN Classification Algorithm. IEEE Access. 2020, 8, 28808–28819. [Google Scholar] [CrossRef]
- Yu, S.; Li, X.; Zhang, X.; Wang, H. The OCS-SVM: An Objective-Cost-Sensitive SVM With Sample-Based Misclassification Cost Invariance. IEEE Access. 2019, 7, 118931–118942. [Google Scholar] [CrossRef]
- Pei, J.; Han, J.; Tong, H. Data Mining: Concepts and Techniques. Elsevier Science & Technology; 2022.
- Zhou, X.H.; McClish, D.K.; Obuchowski, N.A. Statistical Methods in Diagnostic Medicine. Wiley & Sons, Incorporated, John; 2014.
- Marko, M.; Pawliczak, R. Assessment of the available therapeutic approaches for severe COVID-19: a meta-analysis of randomized controlled trials. Sci Rep. 2023, 13, 17114, Published 2023 Oct 10. [Google Scholar] [CrossRef]
- Kuno, T.; Miyamoto, Y.; Iwagami, M.; Ishimaru, M.; Takahashi, M.; Egorova, N.N. The association of remdesivir and in-hospital outcomes for COVID-19 patients treated with steroids. J Antimicrob Chemother. 2021, 76, 2690–2696. [Google Scholar] [CrossRef]
- European Medicines Agency. Veklury: European Public Assessment Report (EPAR). Date of access: February 10, 2024. Available at: https://www.ema.europa.eu/en/medicines/human/EPAR/veklury.
- Abubaker Bagabir, S.; Ibrahim, N.K.; Abubaker Bagabir, H.; Hashem Ateeq, R. Covid-19 and Artificial Intelligence: Genome sequencing, drug development and vaccine discovery. J Infect Public Health. 2022, 15, 289–296. [Google Scholar] [CrossRef]
- Jin, W.; Stokes, J.M.; Eastman, R.T.; et al. Deep learning identifies synergistic drug combinations for treating COVID-19. Proc Natl Acad Sci U S A. 2021, 118, e2105070118. [Google Scholar] [CrossRef] [PubMed]
- Augustin, Y.; Staines, H.M.; Velavan, T.P.; Kamarulzaman, A.; Kremsner, P.G.; Krishna, S. Drug repurposing for COVID-19: current evidence from randomized controlled adaptive platform trials and living systematic reviews. Br Med Bull. 2023, 147, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Basit, S.A.; Qureshi, R.; Musleh, S.; et al. COVID-19Base v3: Update of the knowledgebase for drugs and biomedical entities linked to COVID-19. Front Public Health. 2023, 11, 1125917, Published 2023 Mar 6. [Google Scholar] [CrossRef] [PubMed]
- Imtiaz, F.; Pasha, M.K. A systematic review of RdRp of SARS-CoV-2 through artificial intelligence and machine learning utilizing structure-based drug design strategy. Turk J Chem. 2021, 46, 583–594, Published 2021 Dec 27. [Google Scholar] [CrossRef]
- Gordon, C.J.; Tchesnokov, E.P.; Woolner, E.; et al. Remdesivir is a direct-acting antiviral that inhibits RNA-dependent RNA polymerase from severe acute respiratory syndrome coronavirus 2 with high potency. J Biol Chem. 2020, 295, 6785–6797. [Google Scholar] [CrossRef]
- Abd-Elshafy, D.N.; Nadeem, R.; Nasraa, M.H.; Bahgat, M.M. Analysis of the SARS-CoV-2 nsp12 P323L/A529V mutations: coeffect in the transiently peaking lineage C.36.3 on protein structure and response to treatment in Egyptian records. Z Naturforsch C J Biosci. Published online January 24, 2024. [CrossRef]
- WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: final results of the WHO Solidarity randomised trial and updated meta-analyses [published correction appears in Lancet. 2022 Oct 29;400(10362):1512]. Lancet. 2022, 399, 1941–1953. [Google Scholar] [CrossRef]
- Grundeis, F.; Ansems, K.; Dahms, K.; et al. Remdesivir for the treatment of COVID-19. Cochrane Database Syst Rev. 2023, 1, CD014962, Published 2023 Jan 25. [Google Scholar] [CrossRef]
- Spinner, C.D.; Gottlieb, R.L.; Criner, G.J.; et al. Effect of Remdesivir vs Standard Care on Clinical Status at 11 Days in Patients With Moderate COVID-19: A Randomized Clinical Trial. JAMA. 2020, 324, 1048–1057. [Google Scholar] [CrossRef]
- Goldman, J.D.; Lye, D.C.B.; Hui, D.S.; et al. Remdesivir for 5 or 10 Days in Patients with Severe Covid-19. N Engl J Med. 2020, 383, 1827–1837. [Google Scholar] [CrossRef]
- Chaudhary, B.R.; Dudhrejia, P.J.; Gambhir, R.M.; Rathod, M.M. Study of Efficacy of Injection Remdesivir in Patients of COVID-19. J Assoc Physicians India. 2023, 71, 11–12. [Google Scholar] [CrossRef]
- Libra, A.; Ciancio, N.; Sambataro, G.; et al. Use of Remdesivir in Patients Hospitalized for COVID-19 Pneumonia: Effect on the Hypoxic and Inflammatory State. Viruses. 2023, 15, 2101, Published 2023 Oct 17. [Google Scholar] [CrossRef]
- Lavrentieva, A.; Kaimakamis, E.; Voutsas, V.; Bitzani, M. An observational study on factors associated with ICU mortality in Covid-19 patients and critical review of the literature. Sci Rep. 2023, 13, 7804, Published 2023 May 13. [Google Scholar] [CrossRef]
- Chen, C.; Fang, J.; Chen, S.; et al. The efficacy and safety of remdesivir alone and in combination with other drugs for the treatment of COVID-19: a systematic review and meta-analysis. BMC Infect Dis. 2023, 23, 672, Published 2023 Oct 9. [Google Scholar] [CrossRef]
- Mozaffari, E.; Chandak, A.; Zhang, Z.; et al. Remdesivir Treatment in Hospitalized Patients With Coronavirus Disease 2019 (COVID-19): A Comparative Analysis of In-hospital All-cause Mortality in a Large Multicenter Observational Cohort. Clin Infect Dis. 2022, 75, e450–e458. [Google Scholar] [CrossRef]
- Paules, C.I.; Gallagher, S.K.; Rapaka, R.R.; et al. Remdesivir for the Prevention of Invasive Mechanical Ventilation or Death in Coronavirus Disease 2019 (COVID-19): A Post Hoc Analysis of the Adaptive COVID-19 Treatment Trial-1 Cohort Data. Clin Infect Dis. 2022, 74, 1260–1264. [Google Scholar] [CrossRef] [PubMed]
- Amstutz, A.; Speich, B.; Mentré, F.; et al. Effects of remdesivir in patients hospitalised with COVID-19: a systematic review and individual patient data meta-analysis of randomised controlled trials [published correction appears in Lancet Respir Med. 2023 Aug;11(8):e77]. Lancet Respir Med. 2023, 11, 453–464. [Google Scholar] [CrossRef]
- Huang, C.; Lu, T.L.; Lin, L. Remdesivir Treatment Lacks the Effect on Mortality Reduction in Hospitalized Adult COVID-19 Patients Who Required High-Flow Supplemental Oxygen or Invasive Mechanical Ventilation. Medicina (Kaunas). 2023, 59, 1027, Published 2023 May 26. [Google Scholar] [CrossRef] [PubMed]
- Kaka, A.S.; MacDonald, R.; Linskens, E.J.; et al. Major Update 2: Remdesivir for Adults With COVID-19: A Living Systematic Review and Meta-analysis for the American College of Physicians Practice Points. Ann Intern Med. 2022, 175, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Wei, B.; Zhang, R.; Zeng, H.; et al. Impact of some antiviral drugs on health care utilization for patients with COVID-19: a systematic review and meta-analysis [published online ahead of print, 2023 Sep 5]. Expert Rev Anti Infect Ther. 2023, 1–17. [Google Scholar] [CrossRef]
- Kalil, A.C.; Patterson, T.F.; Mehta, A.K.; et al. Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. N Engl J Med. 2021, 384, 795–807. [Google Scholar] [CrossRef]
- Hariharan, A.; Hakeem, A.R.; Radhakrishnan, S.; Reddy, M.S.; Rela, M. The Role and Therapeutic Potential of NF-kappa-B Pathway in Severe COVID-19 Patients. Inflammopharmacology. 2021, 29, 91–100. [Google Scholar] [CrossRef]
- Osuchowski, M.F.; Winkler, M.S.; Skirecki, T.; et al. The COVID-19 puzzle: deciphering pathophysiology and phenotypes of a new disease entity. Lancet Respir Med. 2021, 9, 622–642. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; Azher, T.; Baqi, M.; et al. Remdesivir for the treatment of patients in hospital with COVID-19 in Canada: a randomized controlled trial. CMAJ. 2022, 194, E242–E251. [Google Scholar] [CrossRef] [PubMed]
- Khosrow-Pour, M. Advanced Methodologies and Technologies in Network Architecture, Mobile Computing, and Data Analytics. IGI Global; 2018.
- Bottino, F.; Tagliente, E.; Pasquini, L.; et al. COVID Mortality Prediction with Machine Learning Methods: A Systematic Review and Critical Appraisal. J Pers Med. 2021, 11, 893, Published 2021 Sep 7. [Google Scholar] [CrossRef] [PubMed]
- Adamidi, E.S.; Mitsis, K.; Nikita, K.S. Artificial intelligence in clinical care amidst COVID-19 pandemic: A systematic review. Comput Struct Biotechnol J. 2021, 19, 2833–2850. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.; Meng, F.; Yan, G.; Yan, H.; Chai, B.; Song, F. Diagnostic classification of cancers using extreme gradient boosting algorithm and multi-omics data. Comput Biol Med. 2020, 121, 103761. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Song, J.Y.; Hyun, H.; et al. Prognostic factors of 30-day mortality in patients with COVID-19 pneumonia under standard remdesivir and dexamethasone treatment. Medicine (Baltimore). 2022, 101, e30474. [Google Scholar] [CrossRef] [PubMed]
- Amiri, P.; Montazeri, M.; Ghasemian, F.; et al. Prediction of mortality risk and duration of hospitalization of COVID-19 patients with chronic comorbidities based on machine learning algorithms. Digit Health 2023, 9, 20552076231170493, Published 2023 Jun 6. [Google Scholar] [CrossRef]
- Georgakopoulou, V.E.; Gkoufa, A.; Makrodimitri, S.; et al. Early 3 day course of remdesivir for the prevention of the progression to severe COVID 19 in the elderly: A single centre, real life cohort study. Exp Ther Med. 2023, 26, 462, Published 2023 Aug 9. [Google Scholar] [CrossRef]
- Vaid, A.; Somani, S.; Russak, A.J.; et al. Machine Learning to Predict Mortality and Critical Events in a Cohort of Patients With COVID-19 in New York City: Model Development and Validation. J Med Internet Res. 2020, 22, e24018, Published 2020 Nov 6. [Google Scholar] [CrossRef]
- Aktar, S.; Talukder, A.; Ahamad, M.M.; et al. Machine Learning Approaches to Identify Patient Comorbidities and Symptoms That Increased Risk of Mortality in COVID-19. Diagnostics (Basel). 2021, 11, 1383, Published 2021 Jul 31. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Zhang, B.; Fu, M.; et al. Clinical and inflammatory features based machine learning model for fatal risk prediction of hospitalized COVID-19 patients: results from a retrospective cohort study. Ann Med. 2021, 53, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Xiong, D.; Wang, J.; Liang, X.; Wang, J.; Chen, Y. The accuracy of the National Early Warning Score 2 in predicting early death in prehospital and emergency department settings: a systematic review and meta-analysis. Ann Transl Med. 2023, 11, 95. [Google Scholar] [CrossRef] [PubMed]
- Richardson, D.; Faisal, M.; Fiori, M.; Beatson, K.; Mohammed, M. Use of the first National Early Warning Score recorded within 24 hours of admission to estimate the risk of in-hospital mortality in unplanned COVID-19 patients: a retrospective cohort study. BMJ Open. 2021, 11, e043721, Published 2021 Feb 22. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Zhou, L.; Hu, Z.; et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef]
- Terkes, V.; Lisica, K.; Marusic, M.; Verunica, N.; Tolic, A.; Morovic, M. Remdesivir Treatment in Moderately Ill COVID-19 Patients: A Retrospective Single Center Study. J Clin Med. 2022, 11, 5066, Published 2022 Aug 29. [Google Scholar] [CrossRef]
- Liu, Y.; Gao, W.; Guo, W.; et al. Prominent coagulation disorder is closely related to inflammatory response and could be as a prognostic indicator for ICU patients with COVID-19. J Thromb Thrombolysis. 2020, 50, 825–832. [Google Scholar] [CrossRef]
- Comoglu, S.; Kant, A. Does the Charlson comorbidity index help predict the risk of death in COVID-19 patients? North Clin Istanb. 2022, 9, 117–121, Published 2022 Apr 12. [Google Scholar] [CrossRef]
- Kurien, S.S.; David, R.; Varma, R.P.; Dev, A.S.; Chellappan, A.; Yadev, I.P. Correlation Between Biomarkers and Age-Adjusted Charlson Comorbidity Index in Patients With COVID-19: A Cross-Sectional Study in a Tertiary Care Center in South India. Cureus. 2023, 15, e36000, Published 2023 Mar 10. [Google Scholar] [CrossRef]
- Carannante, M.; D'Amato, V.; Iaccarino, G. The Future Evolution of the Mortality Acceleration Due to the COVID-19: The Charlson Comorbidity Index in Stochastic Setting. Front Cardiovasc Med. 2022, 9, 938086, Published 2022 Jul 14. [Google Scholar] [CrossRef]
- Raad, I.I.; Hachem, R.; Masayuki, N.; et al. International multicenter study comparing COVID-19 in patients with cancer to patients without cancer: Impact of risk factors and treatment modalities on survivorship. Elife. 2023, 12, e81127, Published 2023 Jan 30. [Google Scholar] [CrossRef] [PubMed]
- Mikulska, M.; Testi, D.; Russo, C.; et al. Outcome of early treatment of SARS-CoV-2 infection in patients with haematological disorders. Br J Haematol. 2023, 201, 628–639. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.M.; Rabbani, S.I.; Halim Mohamed, A.A.; et al. Analysis of potential risk factors associated with COVID-19 and hospitalization. Front Public Health. 2022, 10, 921953, Published 2022 Aug 5. [Google Scholar] [CrossRef] [PubMed]
- Matthay, M.A.; Arabi, Y.; Arroliga, A.C.; et al. A New Global Definition of Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2024, 209, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Georgakopoulou, V.E.; Vlachogiannis, N.I.; Basoulis, D.; et al. A Simple Prognostic Score for Critical COVID-19 Derived from Patients without Comorbidities Performs Well in Unselected Patients. J Clin Med. 2022, 11, 1810, Published 2022 Mar 25. [Google Scholar] [CrossRef] [PubMed]
- Brosh-Nissimov, T.; Hussein, K.; Wiener-Well, Y.; et al. Hospitalized Patients With Severe Coronavirus Disease 2019 During the Omicron Wave in Israel: Benefits of a Fourth Vaccine Dose. Clin Infect Dis. 2023, 76, e234–e239. [Google Scholar] [CrossRef]
- Shimizu, H.; Kawase, J.; Hayashi, M.; Imaizumi, K.; Ito, Y.; Okazawa, M. COVID-19 symptom-onset to diagnosis and diagnosis to treatment intervals are significant predictors of disease progression and hospitalization in high-risk patients: A real world analysis. Respir Investig. 2023, 61, 220–229. [Google Scholar] [CrossRef]
- Kuno, T.; Sahashi, Y.; Kawahito, S.; Takahashi, M.; Iwagami, M.; Egorova, N.N. Prediction of in-hospital mortality with machine learning for COVID-19 patients treated with steroid and remdesivir. J Med Virol. 2022, 94, 958–964. [Google Scholar] [CrossRef]
- Banoei, M.M.; Rafiepoor, H.; Zendehdel, K.; et al. Unraveling complex relationships between COVID-19 risk factors using machine learning based models for predicting mortality of hospitalized patients and identification of high-risk group: a large retrospective study. Front Med (Lausanne). 2023, 10, 1170331, Published 2023 May 4. [Google Scholar] [CrossRef]
- Gutiérrez-Gutiérrez, B.; Del Toro, M.D.; Borobia, A.M.; et al. Identification and validation of clinical phenotypes with prognostic implications in patients admitted to hospital with COVID-19: a multicentre cohort study [published correction appears in Lancet Infect Dis. 2023 Jun;23(6):e198]. Lancet Infect Dis. 2021, 21, 783–792. [Google Scholar] [CrossRef]
- Chen, H.; Xie, J.; Su, N.; et al. Corticosteroid Therapy Is Associated With Improved Outcome in Critically Ill Patients With COVID-19 With Hyperinflammatory Phenotype. Chest. 2021, 159, 1793–1802. [Google Scholar] [CrossRef] [PubMed]
- Ramón, A.; Zaragozá, M.; Torres, A.M.; et al. Application of Machine Learning in Hospitalized Patients with Severe COVID-19 Treated with Tocilizumab. J Clin Med. 2022, 11, 4729, Published 2022 Aug 12. [Google Scholar] [CrossRef] [PubMed]
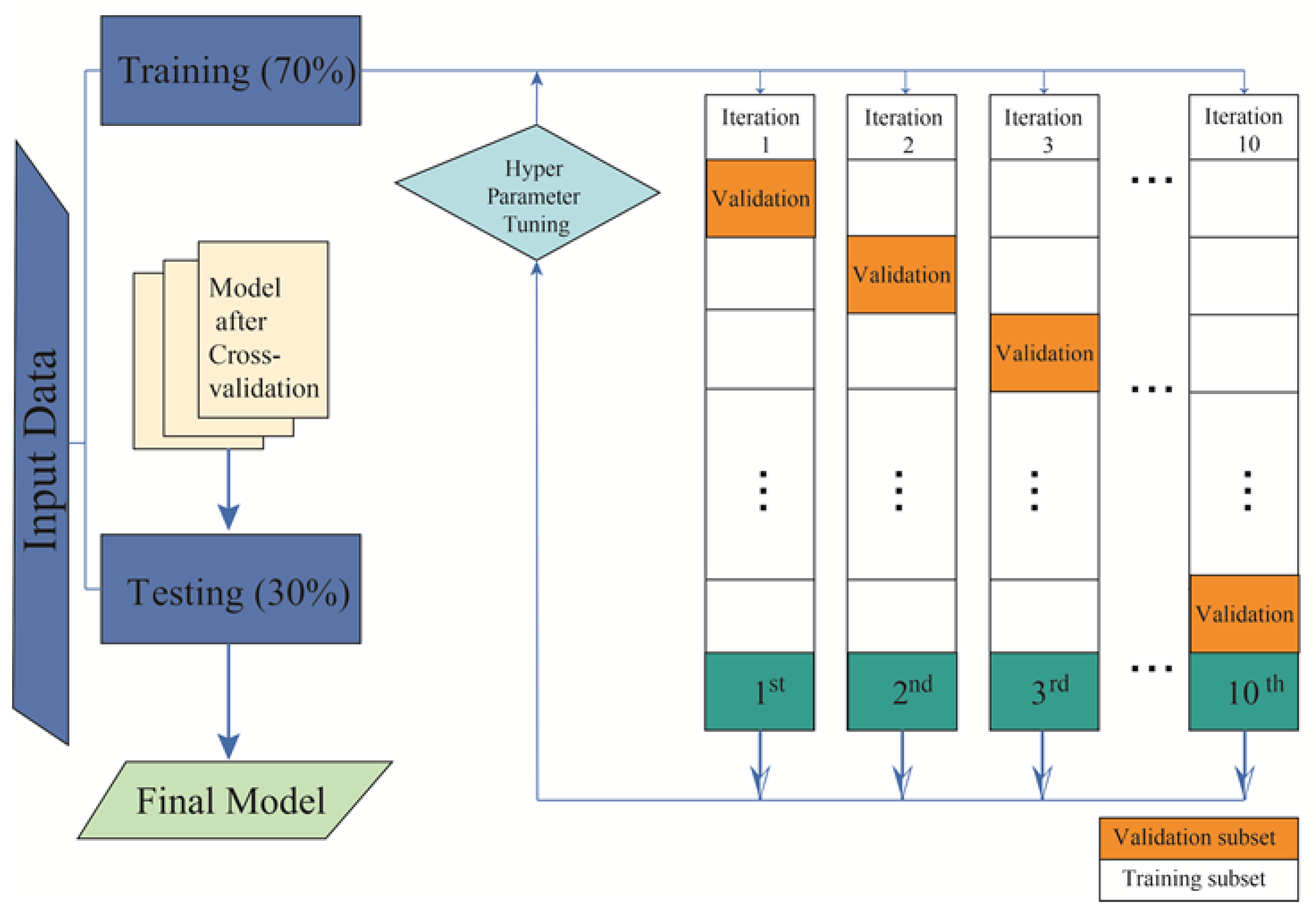
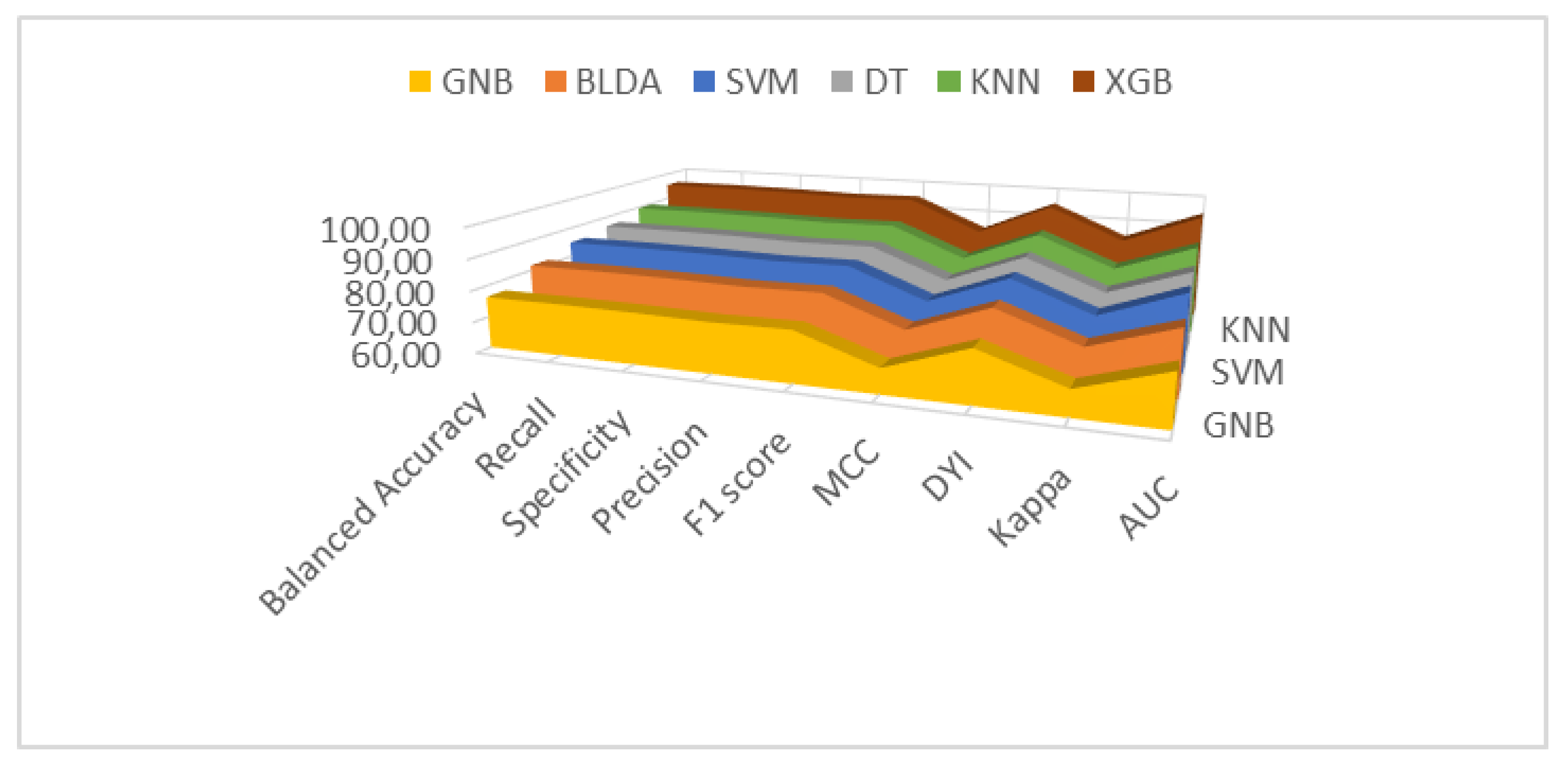
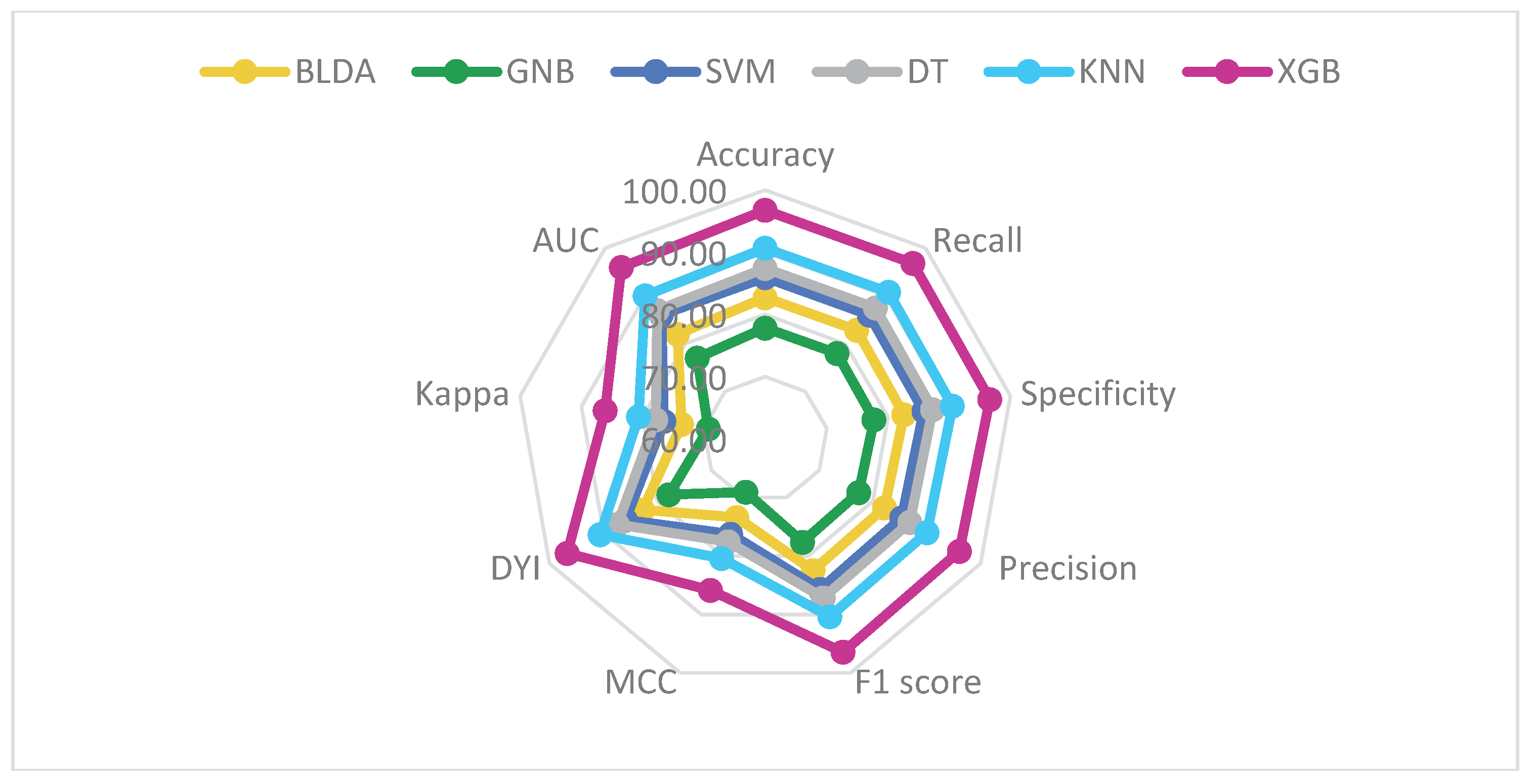
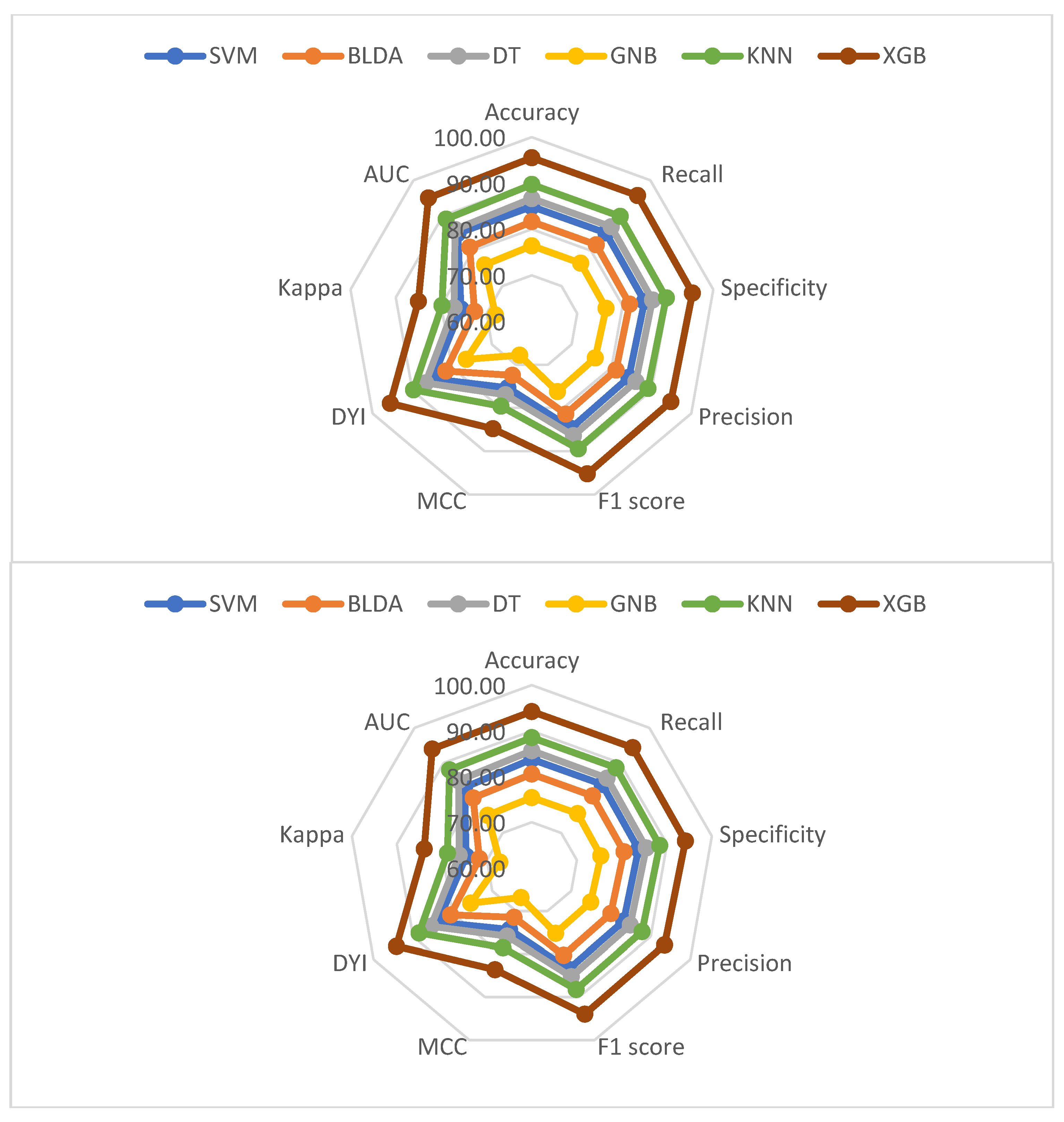
| Methods | Balanced Accuracy | Recall | Precision | F1 Score |
|---|---|---|---|---|
| SVM | 84.80 ± 0.75 | 84.90 ± 0.73 | 84.20 ± 0.74 | 84.55 ± 0.73 |
| BLDA | 81.61 ± 0.84 | 81.70 ± 0.81 | 81.03 ± 0.82 | 81.36 ± 0.81 |
| DT | 86.25 ± 0.71 | 86.35 ± 0.70 | 85.63 ± 0.71 | 85.99 ± 0.70 |
| GNB | 76.80 ± 0.94 | 76.89 ± 0.93 | 76.25 ± 0.95 | 76.57 ± 0.94 |
| KNN | 89.43 ± 0.60 | 89.54 ± 0.58 | 88.79 ± 0.59 | 89.16 ± 0.58 |
| XGB | 95.45 ± 0.46 | 95.56 ± 0.45 | 94.77 ± 0.47 | 95.17 ± 0.44 |
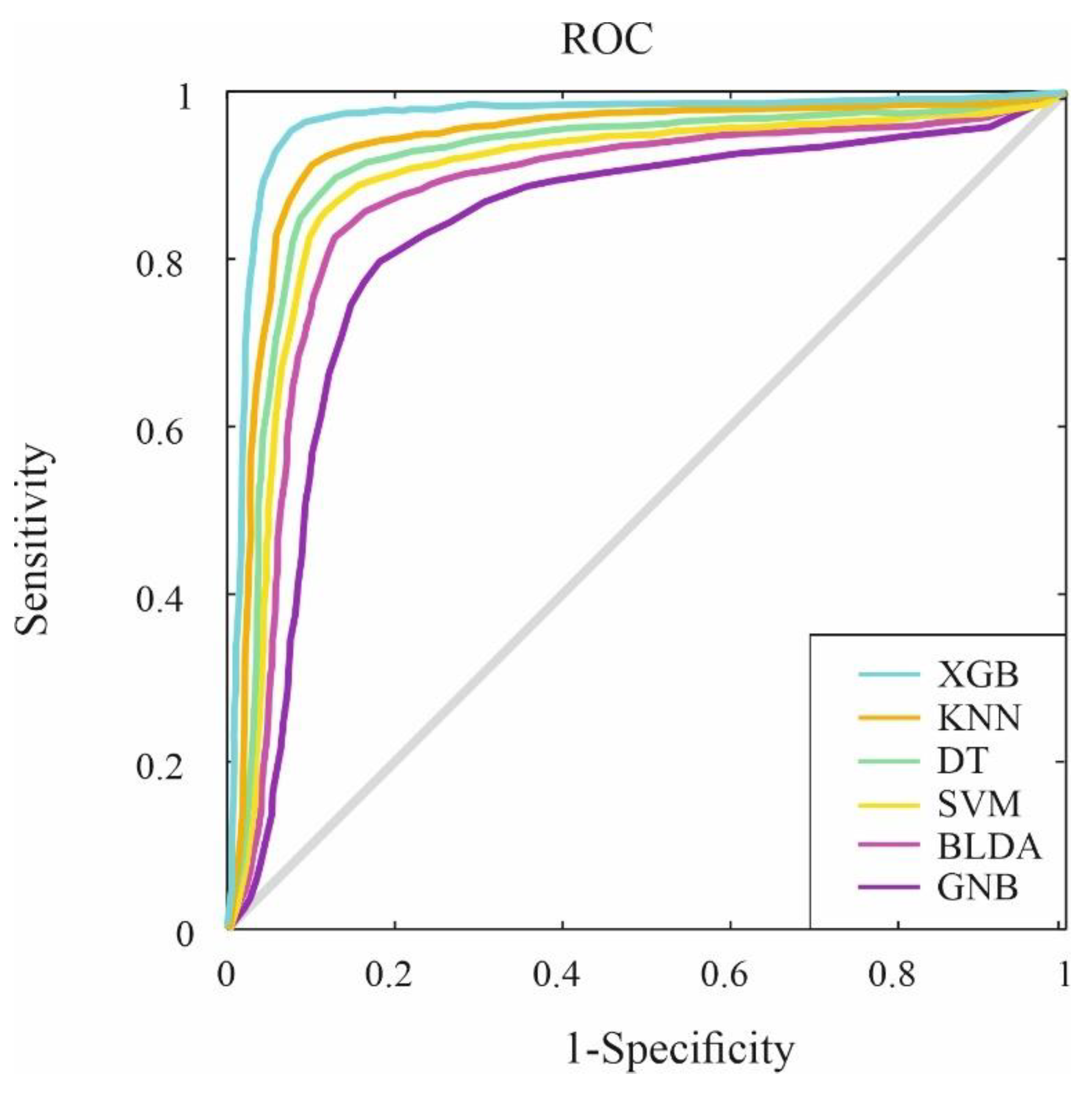
| Methods | AUC | MCC | DYI | Kappa |
| SVM | 0.84 ± 0.02 | 75.25 ± 0.75 | 84.80 ± 0.73 | 75.49 ± 0.74 |
| BLDA | 0.81 ± 0.03 | 72.41 ± 0.82 | 81.61 ± 0.81 | 72.65 ± 0.81 |
| DT | 0.86 ± 0.02 | 76.53 ± 0.71 | 86.25 ± 0.71 | 76.78 ± 0.72 |
| GNB | 0.76 ± 0.03 | 68.15 ± 0.95 | 76.80 ± 0.94 | 68.37 ± 0.94 |
| KNN | 0.89 ± 0.02 | 79.35 ± 0.57 | 89.43 ± 0.58 | 79.62 ± 0.58 |
| XGB | 0.95 ± 0.02 | 84.70 ± 0.42 | 95.45 ± 0.46 | 84.98 ± 0.43 |
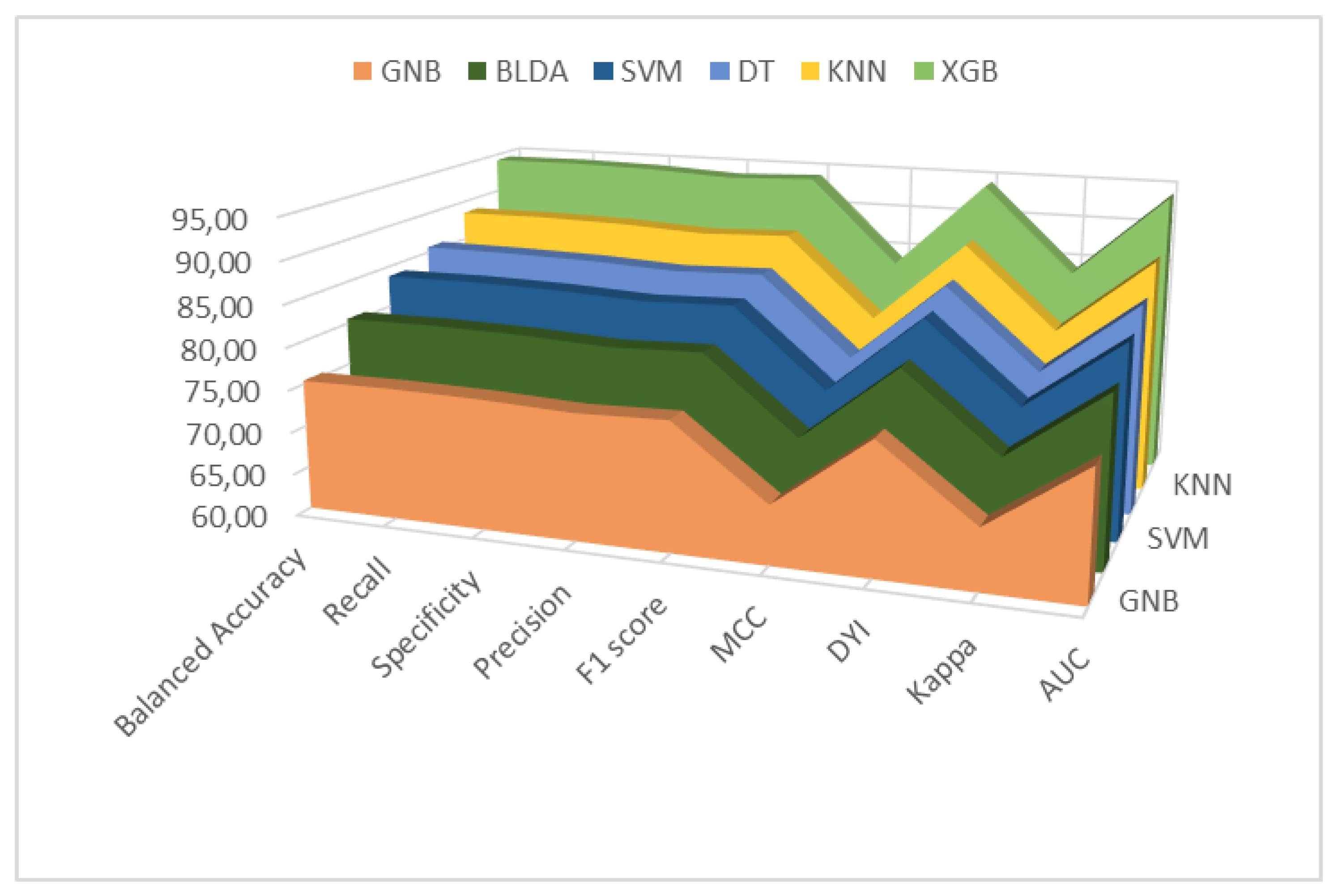
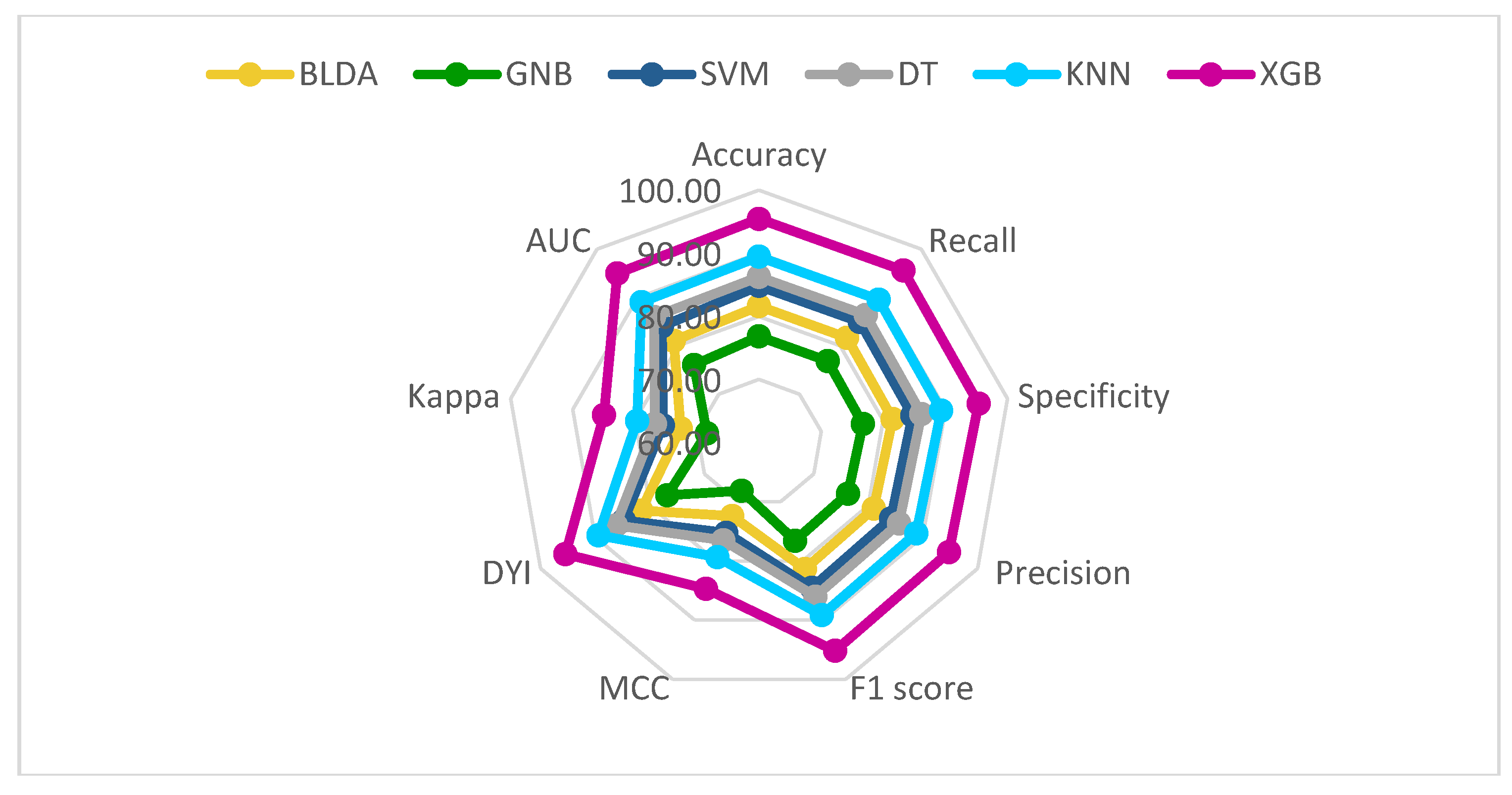
| Methods | Balanced Accuracy | Recall | Precision | F1 Score |
|---|---|---|---|---|
| SVM | 83.80 ± 0.77 | 83.89 ± 0.76 | 83.20 ± 0.78 | 83.54 ± 0.76 |
| BLDA | 80.54 ± 0.85 | 80.64 ± 0.84 | 79.94 ± 0.86 | 80.30 ± 0.85 |
| DT | 85.67 ± 0.73 | 85.61 ± 0.72 | 84.90 ± 0.75 | 85.25 ± 0.74 |
| GNB | 75.41 ± 0.98 | 75.50 ± 0.95 | 74.86 ± 0.96 | 75.18 ± 0.97 |
| KNN | 88.53 ± 0.66 | 88.61 ± 0.64 | 87.85 ± 0.67 | 88.24 ± 0.68 |
| XGB | 94.24 ± 0.48 | 94.35 ± 0.44 | 93.57 ± 0.46 | 93.96 ± 0.47 |
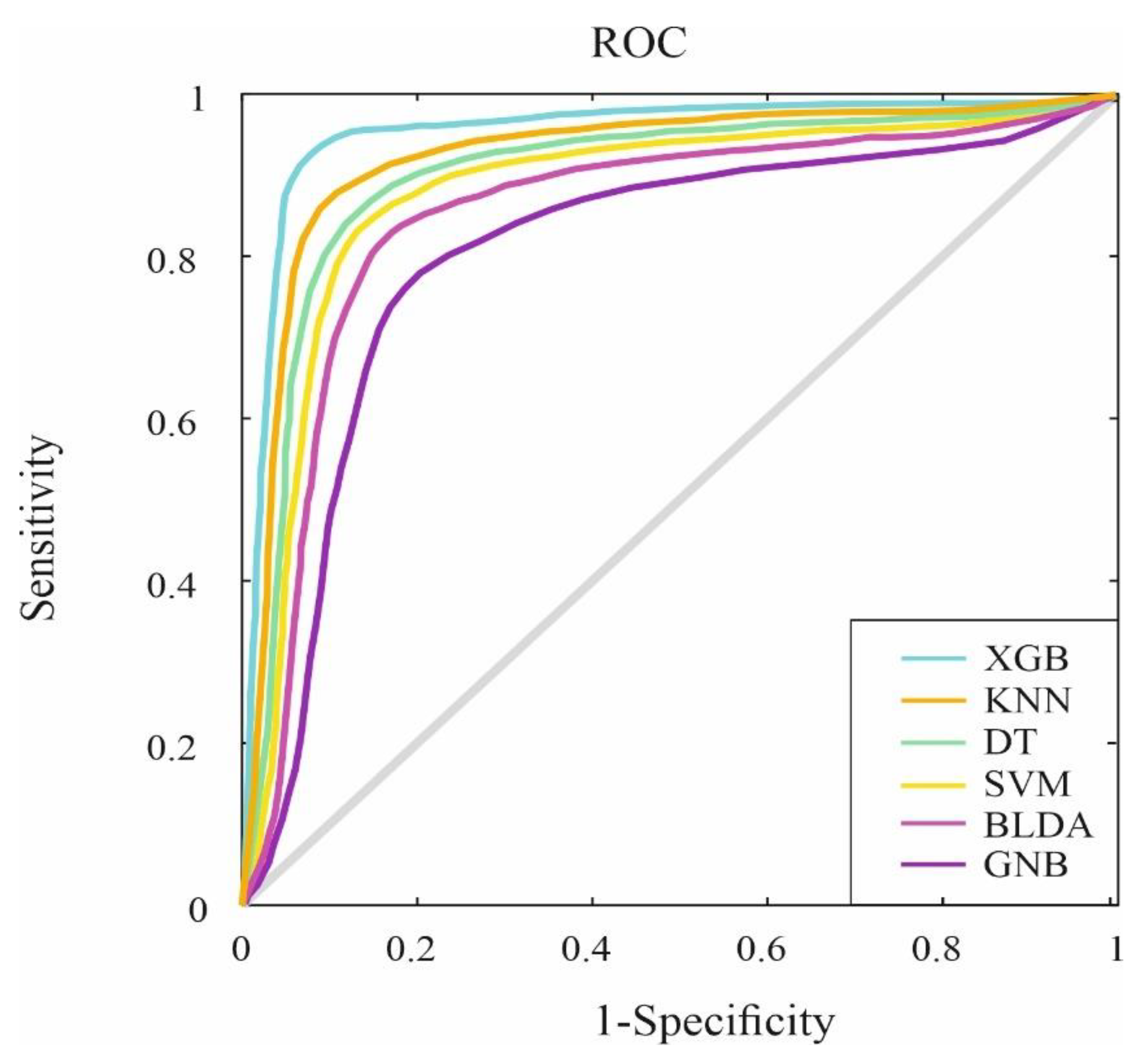
| Methods | AUC | MCC | DYI | Kappa |
| SVM | 0.83 ± 0.02 | 74.35 ± 0.74 | 83.80 ± 0.77 | 74.60 ± 0.73 |
| BLDA | 0.80 ± 0.03 | 71.47 ± 0.83 | 80.54 ± 0.85 | 71.71 ± 0.84 |
| DT | 0.85 ± 0.03 | 75.89 ± 0.71 | 85.51 ± 0.73 | 76.13 ± 0.71 |
| GNB | 0.75 ± 0.03 | 66.91 ± 0.92 | 75.43 ± 0.95 | 67.15 ± 0.93 |
| KNN | 0.88 ± 0.02 | 78.53 ± 0.63 | 88.51 ± 0.66 | 78.79 ± 0.64 |
| XGB | 0.94 ± 0.02 | 83.62 ± 0.41 | 94.24 ± 0.45 | 83.90 ± 0.42 |
| Variable | Cohort |
|---|---|
| Number of patients | 252 |
| Age (years) (IQR) | 77 (66.7–85.2) |
| Male, n (yes %) | 147 (58.3) |
| Hospital admission (days) after remdesivir administration (IQR) | 8 (5–12) |
| Exitus, n (yes %) | 34 (13.5) |
| Patients with duration of remdesivir treatment for 4-5 days, n (yes %) | 194 (76.9) |
| Patients with duration of remdesivir treatment > 5 days, n (yes %) | 14 (5.6) |
| Duration (days) from onset of symptoms to microbiological confirmation (IQR) | 2 (1-4) |
| Oxygen therapy, n (yes %) | 188 (74.6) |
| Patients who need admission to the ICU, n (yes %) | 14 (5.6) |
| Limitation of life support treatment, n (yes %) | 47 (18.6) |
| IMV, n (yes %) | 10 (3.9) |
| Baseline situation at the start of remdesivir: - Patient who does not require supplementary oxygen, n (yes %) - Patient requiring low-flow oxygen therapy, n (yes %) |
|
| 96 (38.1) | |
| 156 (61.9) | |
| Hypertension, n (yes %) | 158 (62.7) |
| Diabetes, n (yes %) | 89 (35.3) |
| Dyslipemia, n (yes %) | 112 (44.4) |
| Smoker, n (yes %) | 55 (21.8) |
| Obesity, n (yes %) | 45 (17.8) |
| COPD, n (yes %) | 35 (13.9) |
| Heart failure, n (yes %) | 51 (20.2) |
| Ischemic heart disease, n (yes %) | 46 (18.2) |
| Chronic kidney disease, n (yes %) | 26 (10.3) |
| Chronic neurological or neurodegenerative disease, n (yes %) | 62 (24.6) |
| Mental health disorder, n (yes %) | 60 (23.8) |
| Active hematological or oncological neoplasia, n (yes %) | 63 (25.0) |
| Patients with ≥ 3 comorbidities, n (yes %) | 193 (76.6) |
| Fever, n (yes %) | 148 (58.7) |
| Cough, n (yes %) | 156 (61.9) |
| Dyspnea, n (yes %) | 158 (62.7) |
| Asthenia, n (yes %) | 106 (42.1) |
| Presence of flu and/or coinfection, n (yes %) | 29 (11.5) |
| Angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, n (yes %) | 109 (43.2) |
| Antibiotics, n (yes %) | 234 (92.8) |
| Immunosuppressants and/or immunomodulators, n (yes %) - Corticoides, n (yes %) - Tocilizumab, n (yes %) - Baricitinib, n (yes %) |
197 (78.2) |
| 124 (49.2) | |
| 33 (13.1) | |
| 32 (12.7) | |
| Albumin (g/dL) (IQR) | 3.4 (2.9-3.6) |
| Hemoglobin (g/dL) (IQR) | 12.4 (10.9-13.7) |
| Troponin (ng/mL) (IQR) | 12 (7-27) |
| CRP (mg/dL) (IQR) | 6.9 (2.4–14.1) |
| LDH (U/L) (IQR) | 463 (359.5–609.5) |
| Ferritin (µg/L) (IQR) | 413 (193–782) |
| D-dimer (ng/mL) (IQR) | 878 (499.7-1,534.2) |
| Creatinina (mg/dL) (IQR) | 0.8 (0.6-1.1) |
| CK (U/L) (IQR) | 98.5 (51.0-192.0) |
| PAFI (IQR) | 323.8 (257.0–368.0) |
| Lymphocytes (109/L) (IQR) | 0.8 (0.6–1.2) |
| Bilateral lung radiological status, n (yes %) | 98 (38.9) |
| Ground-glass opacity lung injury, n (yes %) | 69 (27.4) |
| Patchy lung density, n (yes %) | 64 (25.4) |
| Patients with ≥ 3 doses of COVID-19 vaccine, n (yes %) | 199 (78.9) |
| Acute Respiratory Distress Syndrome, n (yes %) | 56 (22.2) |
| Clinical status on day 14 after the first administration of remdesivir - Hospitalized and requires supplementary oxygen but not IMV, n (yes %) - Hospitalized and requires IMV, n (yes %) |
|
| 23 (9.1) | |
| 5 (1.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





