Submitted:
11 February 2024
Posted:
12 February 2024
You are already at the latest version
Abstract
Keywords:
Introduction
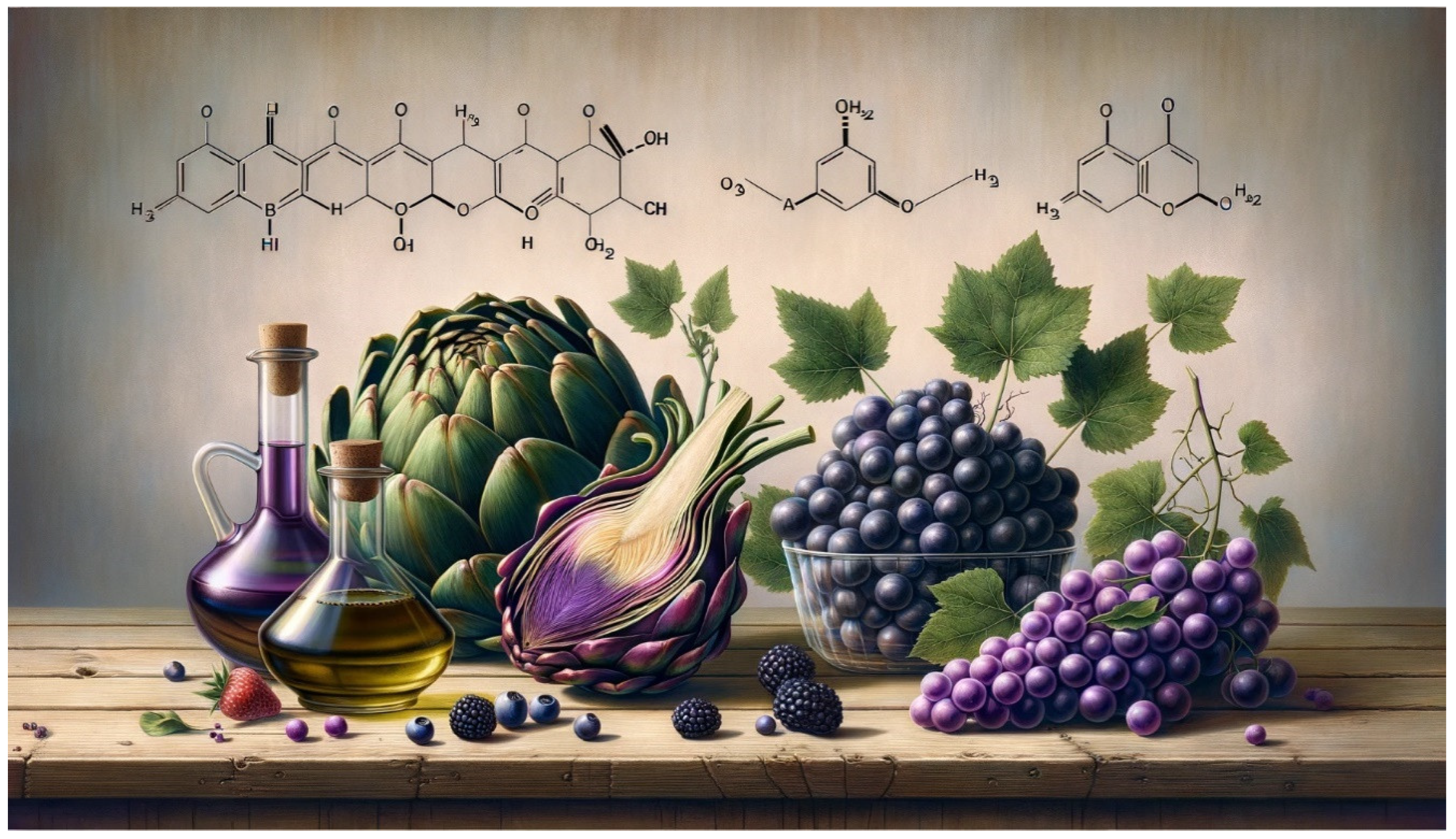
Ellagic Acid (EA) and Neurologic Protection
Red Raspberries (Rubus idaeus L) and the Metabolic Syndrome
Gooseberry (Ribes stenocarpum Maxim. (CBZ)) on Diabetes and Liver Injury
Phytochemicals and Nuclear Factor Erythroid 2-Related Factor 2 (Nrf2) Action on Hepatocarcinoma
Olive Oil and the Regenerative Capacity towards Fibroblast Cells
From (+)-Catechin to ε-Viniferin Gastrointestinal Digestion (GID) Bioaccessibility of Grapevine Bunch Stem and Cane by-Products
Conclusion
Author Contributions
Conflicts of Interest
References
- Kuek, A.; Hazleman, B.L.; Östör, A.J.K. Immune-mediated inflammatory diseases (IMIDs) and biologic therapy: a medical revolution. Postgraduate Medical Journal 2007, 83, 251–260. [Google Scholar] [CrossRef]
- Buckley, C.D.; Chernajovsky, L.; Chernajovsky, Y.; Modis, L.K.; O’Neill, L.A.; Brown, D.; Connor, R.; Coutts, D.; Waterman, E.A.; Tak, P.P. Immune-mediated inflammation across disease boundaries: breaking down research silos. Nat Immunol 2021, 22, 1344–1348. [Google Scholar] [CrossRef] [PubMed]
- Robinson Jr, D.; Hackett, M.; Wong, J.; Kimball, A.B.; Cohen, R.; Bala, M.; Group, I.S. Co-occurrence and comorbidities in patients with immune-mediated inflammatory disorders: an exploration using US healthcare claims data, 2001–2002. Current medical research and opinion 2006, 22, 989–1000. [Google Scholar] [CrossRef] [PubMed]
- Tracey, D.; Klareskog, L.; Sasso, E.H.; Salfeld, J.G.; Tak, P.P. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacology & therapeutics 2008, 117, 244–279. [Google Scholar]
- Cleynen, I.; Vermeire, S. Paradoxical inflammation induced by anti-TNF agents in patients with IBD. Nature reviews Gastroenterology & hepatology 2012, 9, 496–503. [Google Scholar]
- Wijbrandts, C.; Tak, P. Prediction of response to targeted treatment in rheumatoid arthritis. In Proceedings of the Mayo Clinic Proceedings; pp. 1129–1143.
- Corcoran, S.E.; Halai, R.; Cooper, M.A. Pharmacological Inhibition of the Nod-Like Receptor Family Pyrin Domain Containing 3 Inflammasome with MCC950. Pharmacological Reviews 2021, 73, 968–1000. [Google Scholar] [CrossRef] [PubMed]
- Buckley, C.D.; Gilroy, D.W.; Serhan, C.N.; Stockinger, B.; Tak, P.P. The resolution of inflammation. Nat Rev Immunol 2013, 13, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Valko, M.; Leibfritz, D.; Moncol, J.; Cronin, M.T.; Mazur, M.; Telser, J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 2007, 39, 44–84. [Google Scholar] [CrossRef]
- Valko, M.; Rhodes, C.J.; Moncol, J.; Izakovic, M.; Mazur, M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact 2006, 160, 1–40. [Google Scholar] [CrossRef]
- Direito, R.; Rocha, J.; Sepodes, B.; Eduardo-Figueira, M. Phenolic Compounds Impact on Rheumatoid Arthritis, Inflammatory Bowel Disease and Microbiota Modulation. Pharmaceutics 2021, 13, 145. [Google Scholar] [CrossRef]
- Wang, K.; Sun, J.-Z.; Wu, Q.-X.; Li, Z.-Y.; Li, D.-X.; Xiong, Y.-F.; Zhong, G.-C.; Shi, Y.; Li, Q.; Zheng, J.; et al. Long-term anti-inflammatory diet in relation to improved breast cancer prognosis: a prospective cohort study. npj Breast Cancer 2020, 6. [Google Scholar] [CrossRef]
- Barch, D.H.; Fox, C.C. Selective inhibition of methylbenzylnitrosamine-induced formation of esophageal O6-methylguanine by dietary ellagic acid in rats. Cancer Research 1988, 48, 7088–7092. [Google Scholar]
- Nouri, A.; Heibati, F.; Heidarian, E. Gallic acid exerts anti-inflammatory, anti-oxidative stress, and nephroprotective effects against paraquat-induced renal injury in male rats. Naunyn-Schmiedeberg’s Archives of Pharmacology 2021, 394, 1–9. [Google Scholar] [CrossRef]
- Bai, J.; Zhang, Y.; Tang, C.; Hou, Y.; Ai, X.; Chen, X.; Zhang, Y.; Wang, X.; Meng, X. Gallic acid: Pharmacological activities and molecular mechanisms involved in inflammation-related diseases. Biomedicine & Pharmacotherapy 2021, 133, 110985. [Google Scholar]
- Jalili, C.; Korani, M.; Pazhouhi, M.; Ghanbari, A.; Zhaleh, M.; Davoudi, S.; Rashidi, I. Protective effect of gallic acid on nicotine-induced testicular toxicity in mice. Res Pharm Sci 2021, 16, 414–424. [Google Scholar] [CrossRef]
- Nouri, A.; Heibati, F.; Heidarian, E. Gallic acid exerts anti-inflammatory, anti-oxidative stress, and nephroprotective effects against paraquat-induced renal injury in male rats. Naunyn Schmiedebergs Arch Pharmacol 2021, 394, 1–9. [Google Scholar] [CrossRef]
- Nouri, A.; Salehi-Vanani, N.; Heidarian, E. Antioxidant, anti-inflammatory and protective potential of gallic acid against paraquat-induced liver toxicity in male rats. Avicenna J Phytomed 2021, 11, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Owumi, S.E.; Najophe, S.E.; Idowu, T.B.; Nwozo, S.O. Protective mechanisms of gallic acid on hepatorenal dysfunction of zearalenone treated rat. Biologia 2021, 76, 3123–3135. [Google Scholar] [CrossRef]
- Tungmunnithum, D.; Thongboonyou, A.; Pholboon, A.; Yangsabai, A. Flavonoids and Other Phenolic Compounds from Medicinal Plants for Pharmaceutical and Medical Aspects: An Overview. Medicines 2018, 5, 93. [Google Scholar] [CrossRef] [PubMed]
- Allen, C.T.; Peden-Adams, M.M.; EuDaly, J.; Keil, D.E. Subchronic exposure to ellagic acid impairs cytotoxic T-cell function and suppresses humoral immunity in mice. Immunopharmacol Immunotoxicol 2003, 25, 409–422. [Google Scholar] [CrossRef] [PubMed]
- Farbood, Y.; Rashno, M.; Ghaderi, S.; Khoshnam, S.E.; Sarkaki, A.; Rashidi, K.; Rashno, M.; Badavi, M. Ellagic acid protects against diabetes-associated behavioral deficits in rats: Possible involved mechanisms. Life sciences 2019, 225, 8–19. [Google Scholar] [CrossRef]
- Jangra, A.; Datusalia, A.K.; Khandwe, S.; Sharma, S.S. Amelioration of diabetes-induced neurobehavioral and neurochemical changes by melatonin and nicotinamide: implication of oxidative stress–PARP pathway. Pharmacology Biochemistry and Behavior 2013, 114, 43–51. [Google Scholar] [CrossRef]
- Tonoli, C.; Heyman, E.; Roelands, B.; Pattyn, N.; Buyse, L.; Piacentini, M.F.; Berthoin, S.; Meeusen, R. Type 1 diabetes-associated cognitive decline: A meta-analysis and update of the current literature 1型糖尿病相关的认知能力下降:一项对最新文献的meta分析. Journal of Diabetes 2014, 6, 499–513. [Google Scholar] [CrossRef]
- Tabatabaei, S.R.F.; Ghaderi, S.; Bahrami-Tapehebur, M.; Farbood, Y.; Rashno, M. Aloe vera gel improves behavioral deficits and oxidative status in streptozotocin-induced diabetic rats. Biomedicine & Pharmacotherapy 2017, 96, 279–290. [Google Scholar]
- Hamed, S.A. Brain injury with diabetes mellitus: evidence, mechanisms and treatment implications. Expert Review of Clinical Pharmacology 2017, 10, 409–428. [Google Scholar] [CrossRef] [PubMed]
- Mao, X.-Y.; Cao, D.-F.; Li, X.; Yin, J.-Y.; Wang, Z.-B.; Zhang, Y.; Mao, C.-X.; Zhou, H.-H.; Liu, Z.-Q. Huperzine A ameliorates cognitive deficits in streptozotocin-induced diabetic rats. International journal of molecular sciences 2014, 15, 7667–7683. [Google Scholar] [CrossRef] [PubMed]
- Fang, S.-C.; Xie, H.; Chen, F.; Hu, M.; Long, Y.; Sun, H.-B.; Kong, L.-Y.; Hong, H.; Tang, S.-S. Simvastatin ameliorates memory impairment and neurotoxicity in streptozotocin-induced diabetic mice. Neuroscience 2017, 355, 200–211. [Google Scholar] [CrossRef] [PubMed]
- El Sohaimy, S.A. Chemical composition, antioxidant and antimicrobial potential of artichoke. The Open Nutraceuticals Journal 2014, 7. [Google Scholar] [CrossRef]
- Awad, O.M.E.; El-Sohaimy, S.A.; Ghareeb, D.A.; Aboulenein, A.; Saleh, S.R.; El-Aziz, N. Phytochemical Analysis and Toxicity Assessment of Artichoke By-product Extract. Pakistan journal of biological sciences: PJBS 2020, 23, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Aziz, N.M.; Eldin Awad, O.M.; Shehata, M.G.; El-Sohaimy, S.A. Antioxidant and anti-acetylcholinesterase potential of artichoke phenolic compounds. Food Bioscience 2021, 41, 101006. [Google Scholar] [CrossRef]
- Chen, L.; K Morrow, J.; T Tran, H.; S Phatak, S.; Du-Cuny, L.; Zhang, S. From laptop to benchtop to bedside: structure-based drug design on protein targets. Current pharmaceutical design 2012, 18, 1217–1239. [Google Scholar] [CrossRef]
- Javaid, N.; Shah, M.A.; Rasul, A.; Chauhdary, Z.; Saleem, U.; Khan, H.; Ahmed, N.; Uddin, M.S.; Mathew, B.; Behl, T. Neuroprotective effects of Ellagic acid in Alzheimer’s disease: focus on underlying molecular mechanisms of therapeutic potential. Current Pharmaceutical Design 2021, 27, 3591–3601. [Google Scholar]
- Harakeh, S.; Qari, M.H.; Ramadan, W.S.; Al Jaouni, S.K.; Almuhayawi, M.S.; Al Amri, T.; Ashraf, G.M.; Bharali, D.J.; Mousa, S.A. A Novel Nanoformulation of Ellagic Acid is Promising in Restoring Oxidative Homeostasis in Rat Brains with Alzheimer’s Disease. Current drug metabolism 2021, 22, 299–307. [Google Scholar]
- Borges, G.; Degeneve, A.; Mullen, W.; Crozier, A. Identification of Flavonoid and Phenolic Antioxidants in Black Currants, Blueberries, Raspberries, Red Currants, and Cranberries. Journal of Agricultural and Food Chemistry 2010, 58, 3901–3909. [Google Scholar] [CrossRef] [PubMed]
- Figueira, M.; Câmara, M.; Direito, R.; Rocha, J.; Serra, A.; Duarte, C.; Fernandes, A.; Freitas, M.; Fernandes, E.; Marques, M. Chemical characterization of a red raspberry fruit extract and evaluation of its pharmacological effects in experimental models of acute inflammation and collagen-induced arthritis. Food Funct 2014, 5, 3241–3251. [Google Scholar] [CrossRef]
- Gasperotti, M.; Masuero, D.; Vrhovsek, U.; Guella, G.; Mattivi, F. Profiling and Accurate Quantification of Rubus Ellagitannins and Ellagic Acid Conjugates Using Direct UPLC-Q-TOF HDMS and HPLC-DAD Analysis. Journal of Agricultural and Food Chemistry 2010, 58, 4602–4616. [Google Scholar] [CrossRef]
- Yang, J.; Cui, J.; Chen, J.; Yao, J.; Hao, Y.; Fan, Y.; Liu, Y. Evaluation of physicochemical properties in three raspberries (Rubus idaeus) at five ripening stages in northern China. Scientia Horticulturae 2020, 263, 109146. [Google Scholar] [CrossRef]
- Hao, Y.; Yang, J.; Cui, J.; Fan, Y.; Li, N.; Wang, C.; Liu, Y.; Dong, Y. Stability and mechanism of phenolic compounds from raspberry extract under in vitro gastrointestinal digestion. LWT 2021, 139, 110552. [Google Scholar] [CrossRef]
- Seeram, N.P.; Adams, L.S.; Zhang, Y.; Lee, R.; Sand, D.; Scheuller, H.S.; Heber, D. Blackberry, Black Raspberry, Blueberry, Cranberry, Red Raspberry, and Strawberry Extracts Inhibit Growth and Stimulate Apoptosis of Human Cancer Cells In Vitro. Journal of Agricultural and Food Chemistry 2006, 54, 9329–9339. [Google Scholar] [CrossRef]
- Wang, P.-W.; Cheng, Y.-C.; Hung, Y.-C.; Lee, C.-H.; Fang, J.-Y.; Li, W.-T.; Wu, Y.-R.; Pan, T.-L. Red Raspberry Extract Protects the Skin against UVB-Induced Damage with Antioxidative and Anti-inflammatory Properties. Oxidative Medicine and Cellular Longevity 2019, 2019, 9529676. [Google Scholar] [CrossRef] [PubMed]
- Tu, L.; Sun, H.; Tang, M.; Zhao, J.; Zhang, Z.; Sun, X.; He, S. Red raspberry extract (Rubus idaeus L shrub) intake ameliorates hyperlipidemia in HFD-induced mice through PPAR signaling pathway. Food and Chemical Toxicology 2019, 133, 110796. [Google Scholar] [CrossRef] [PubMed]
- Noratto, G.D.; Chew, B.P.; Atienza, L.M. Red raspberry (Rubus idaeus L.) intake decreases oxidative stress in obese diabetic (db/db) mice. Food Chemistry 2017, 227, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Kirakosyan, A.; Seymour, E.M.; Kondoleon, N.; Gutierrez, E.; Wolforth, J.; Bolling, S. The intake of red raspberry fruit is inversely related to cardiac risk factors associated with metabolic syndrome. Journal of Functional Foods 2018, 41, 83–89. [Google Scholar] [CrossRef]
- Nowak, A.; Sójka, M.; Klewicka, E.; Lipińska, L.; Klewicki, R.; Kołodziejczyk, K. Ellagitannins from Rubus idaeus L. Exert Geno- and Cytotoxic Effects against Human Colon Adenocarcinoma Cell Line Caco-2. J Agric Food Chem 2017, 65, 2947–2955. [Google Scholar] [CrossRef] [PubMed]
- Franck, M.; De Toro-Martín, J.; Garneau, V.; Guay, V.; Kearney, M.; Pilon, G.; Roy, D.; Couture, P.; Couillard, C.; Marette, A.; et al. Effects of Daily Raspberry Consumption on Immune-Metabolic Health in Subjects at Risk of Metabolic Syndrome: A Randomized Controlled Trial. Nutrients 2020, 12, 3858. [Google Scholar] [CrossRef]
- Wu, F.-S.; Gibbs, T.T.; Farb, D.H. Dual activation of GABAA and glycine receptors by β-alanine: inverse modulation by progesterone and 5α-pregnan-3α-ol-20-one. European Journal of Pharmacology: Molecular Pharmacology 1993, 246, 239–246. [Google Scholar] [CrossRef]
- Geng, J.; Yang, C.; Wang, B.; Zhang, X.; Hu, T.; Gu, Y.; Li, J. Trimethylamine N-oxide promotes atherosclerosis via CD36-dependent MAPK/JNK pathway. Biomed Pharmacother 2018, 97, 941–947. [Google Scholar] [CrossRef]
- Puupponen-Pimiä, R.; Seppänen-Laakso, T.; Kankainen, M.; Maukonen, J.; Törrönen, R.; Kolehmainen, M.; Leppänen, T.; Moilanen, E.; Nohynek, L.; Aura, A.M.; et al. Effects of ellagitannin-rich berries on blood lipids, gut microbiota, and urolithin production in human subjects with symptoms of metabolic syndrome. Mol Nutr Food Res 2013, 57, 2258–2263. [Google Scholar] [CrossRef]
- Mandal, N.; Grambergs, R.; Mondal, K.; Basu, S.K.; Tahia, F.; Dagogo-Jack, S. Role of ceramides in the pathogenesis of diabetes mellitus and its complications. Journal of Diabetes and its Complications 2021, 35, 107734. [Google Scholar] [CrossRef]
- Dei Cas, M.; Ghidoni, R. Cancer Prevention and Therapy with Polyphenols: Sphingolipid-Mediated Mechanisms. Nutrients 2018, 10, 940. [Google Scholar] [CrossRef]
- Si, X.; Tian, J.; Shu, C.; Wang, Y.; Gong, E.; Zhang, Y.; Zhang, W.; Cui, H.; Li, B. Serum Ceramide Reduction by Blueberry Anthocyanin-Rich Extract Alleviates Insulin Resistance in Hyperlipidemia Mice. Journal of Agricultural and Food Chemistry 2020, 68, 8185–8194. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Mohammad, T.; Khan, P.; Alajmi, M.F.; Hussain, A.; Rehman, M.T.; Hassan, M.I. Evaluation of ellagic acid as an inhibitor of sphingosine kinase 1: A targeted approach towards anticancer therapy. Biomed Pharmacother 2019, 118, 109245. [Google Scholar] [CrossRef] [PubMed]
- Xiao, D.; Zhu, L.; Edirisinghe, I.; Fareed, J.; Brailovsky, Y.; Burton-Freeman, B. Attenuation of Postmeal Metabolic Indices with Red Raspberries in Individuals at Risk for Diabetes: A Randomized Controlled Trial. Obesity 2019, 27, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Schell, J.; Betts, N.M.; Lyons, T.J.; Basu, A. Raspberries Improve Postprandial Glucose and Acute and Chronic Inflammation in Adults with Type 2 Diabetes. Annals of Nutrition and Metabolism 2019, 74, 165–174. [Google Scholar] [CrossRef]
- Clegg, M.E.; Pratt, M.; Meade, C.M.; Henry, C.J. The addition of raspberries and blueberries to a starch-based food does not alter the glycaemic response. Br J Nutr 2011, 106, 335–338. [Google Scholar] [CrossRef]
- Uttra, A.M.; Alamgeer; Shahzad, M.; Shabbir, A.; Jahan, S.; Bukhari, I.A.; Assiri, A.M. Ribes orientale: A novel therapeutic approach targeting rheumatoid arthritis with reference to pro-inflammatory cytokines, inflammatory enzymes and anti-inflammatory cytokines. Journal of Ethnopharmacology 2019, 237, 92–107. [Google Scholar] [CrossRef]
- Burgos-Edwards, A.; Martín-Pérez, L.; Jiménez-Aspee, F.; Theoduloz, C.; Schmeda-Hirschmann, G.; Larrosa, M. Anti-inflammatory effect of polyphenols from Chilean currants (Ribes magellanicum and R. punctatum) after in vitro gastrointestinal digestion on Caco-2 cells: Anti-inflammatory activity of in vitro digested Chilean currants. Journal of Functional Foods 2019, 59, 329–336. [Google Scholar] [CrossRef]
- Jiang, S.; Zhao, X.; Liu, C.; Dong, Q.; Mei, L.; Chen, C.; Shao, Y.; Tao, Y.; Yue, H. Identification of phenolic compounds in fruits of Ribes stenocarpum Maxim. By UHPLC-QTOF/MS and their hypoglycemic effects in vitro and in vivo. Food Chemistry 2021, 344, 128568. [Google Scholar] [CrossRef]
- Elmasry, S.; Moawad, M. The hepatoprotective effect of gooseberry and black mulberry extracts against carbon tetrachloride-induced liver injury in rats. J Basic Appl Zool 2021, 82. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for Clinicians 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Shah, S.A.A.; Bungau, S.; Si, Y.; Xu, H.; Rahman, M.; Behl, T.; Gitea, D.; Pavel, F.-M.; Corb Aron, R.A.; Pasca, B. Chemically diverse and biologically active secondary metabolites from marine Phylum chlorophyta. Marine Drugs 2020, 18, 493. [Google Scholar] [CrossRef]
- Sivasankarapillai, V.S.; Madhu Kumar Nair, R.; Rahdar, A.; Bungau, S.; Zaha, D.C.; Aleya, L.; Tit, D.M. Overview of the anticancer activity of withaferin A, an active constituent of the Indian ginseng Withania somnifera. Environmental Science and Pollution Research 2020, 27, 26025–26035. [Google Scholar] [CrossRef]
- Nugroho, A.; Kim, E.J.; Choi, J.S.; Park, H.J. Simultaneous quantification and peroxynitrite-scavenging activities of flavonoids in Polygonum aviculare L. herb. J Pharm Biomed Anal 2014, 89, 93–98. [Google Scholar] [CrossRef]
- Özbay, H.; Alim, A. Antimicrobial Activity of Some Water Plants from the Northeastern Anatolian Region of Turkey. Molecules 2009, 14, 321–328. [Google Scholar] [CrossRef]
- Chon, S.U.; Heo, B.G.; Park, Y.S.; Cho, J.Y.; Gorinstein, S. Characteristics of the leaf parts of some traditional Korean salad plants used for food. Journal of the Science of Food and Agriculture 2008, 88, 1963–1968. [Google Scholar] [CrossRef]
- Costea, M.; Tardif, F.J. The biology of Canadian weeds. 131. Polygonum aviculare L. Canadian journal of plant science 2005, 85, 481–506. [Google Scholar] [CrossRef]
- Thu, N.N.; Sakurai, C.; Uto, H.; Van Chuyen, N.; Lien, D.T.; Yamamoto, S.; Ohmori, R.; Kondo, K. The polyphenol content and antioxidant activities of the main edible vegetables in northern Vietnam. J Nutr Sci Vitaminol (Tokyo) 2004, 50, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Bolotova, Y.V. Aquatic plants of the Far East of Russia: a review on their use in medicine, pharmacological activity. Bangladesh Journal of Medical Science 2015, 14, 9–13. [Google Scholar] [CrossRef]
- Ravipati, A.S.; Zhang, L.; Koyyalamudi, S.R.; Jeong, S.C.; Reddy, N.; Bartlett, J.; Smith, P.T.; Shanmugam, K.; Münch, G.; Wu, M.J.; et al. Antioxidant and anti-inflammatory activities of selected Chinese medicinal plants and their relation with antioxidant content. BMC Complement Altern Med 2012, 12, 173. [Google Scholar] [CrossRef] [PubMed]
- Orbán-Gyapai, O.; Lajter, I.; Hohmann, J.; Jakab, G.; Vasas, A. Xanthine oxidase inhibitory activity of extracts prepared from Polygonaceae species. Phytother Res 2015, 29, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Sung, Y.Y.; Yoon, T.; Yang, W.K.; Kim, S.J.; Kim, D.S.; Kim, H.K. The Antiobesity Effect of Polygonum aviculare L. Ethanol Extract in High-Fat Diet-Induced Obese Mice. Evid Based Complement Alternat Med 2013, 2013, 626397. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Fu, J.; Yin, X.; Li, X.; Wang, B.; Cao, S.; Zhang, J.; Zhang, H.; Zhao, Y.; Ni, J. Pharmacological and other Bioactivities of the Genus Polygonum-A Review. Tropical Journal of Pharmaceutical Research 2014, 13. [Google Scholar]
- Eid, S.Y.; El-Readi, M.Z.; Wink, M. Synergism of three-drug combinations of sanguinarine and other plant secondary metabolites with digitonin and doxorubicin in multi-drug resistant cancer cells. Phytomedicine 2012, 19, 1288–1297. [Google Scholar] [CrossRef] [PubMed]
- Gao, A.-M.; Ke, Z.-P.; Shi, F.; Sun, G.-C.; Chen, H. Chrysin enhances sensitivity of BEL-7402/ADM cells to doxorubicin by suppressing PI3K/Akt/Nrf2 and ERK/Nrf2 pathway. Chemico-biological interactions 2013, 206, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Jovanović, M.; Tenji, D.; Nikolić, B.; Srdić-Rajić, T.; Svirčev, E.; Mitić-Ćulafić, D. In Vitro Study of Two Edible Polygonoideae Plants: Phenolic Profile, Cytotoxicity, and Modulation of Keap1-Nrf2 Gene Expression. Foods 2021, 10, 811. [Google Scholar] [CrossRef]
- Shafa, M.H.; Jalal, R.; Kosari, N.; Rahmani, F. Efficacy of metformin in mediating cellular uptake and inducing apoptosis activity of doxorubicin. Regulatory Toxicology and Pharmacology 2018, 99, 200–212. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Lee, D.M.; Lee, S.-H. Nrf2 expression and apoptosis in quercetin-treated malignant mesothelioma cells. Molecules and cells 2015, 38, 416. [Google Scholar] [CrossRef]
- Raghunath, A.; Sundarraj, K.; Arfuso, F.; Sethi, G.; Perumal, E. Dysregulation of Nrf2 in hepatocellular carcinoma: role in cancer progression and chemoresistance. Cancers 2018, 10, 481. [Google Scholar] [CrossRef]
- Dong, L.; Han, X.; Tao, X.; Xu, L.; Xu, Y.; Fang, L.; Yin, L.; Qi, Y.; Li, H.; Peng, J. Protection by the total flavonoids from Rosa laevigata Michx fruit against lipopolysaccharide-induced liver injury in mice via modulation of FXR signaling. Foods 2018, 7, 88. [Google Scholar] [CrossRef]
- Jovanović, M.; Srdić-Rajić, T.; Svirčev, E.; Jasnić, N.; Nikolić, B.; Bojić, S.; Stević, T.; Knežević-Vukčević, J.; Mitić-Ćulafić, D. Evaluation of anticancer and antimicrobial activities of the Polygonum maritimum ethanol extract. Archives of Biological Sciences 2018, 70, 665–673. [Google Scholar] [CrossRef]
- Mohd Ghazali, M.A.; Al-Naqeb, G.; Krishnan Selvarajan, K.; Hazizul Hasan, M.; Adam, A. Apoptosis induction by Polygonum minus is related to antioxidant capacity, alterations in expression of apoptotic-related genes, and S-phase cell cycle arrest in HepG2 cell line. BioMed research international 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; An, H.M.; Shen, K.P.; Song, H.Y.; Deng, S. Polygonum cuspidatum Extract Induces Anoikis in Hepatocarcinoma Cells Associated with Generation of Reactive Oxygen Species and Downregulation of Focal Adhesion Kinase. Evid Based Complement Alternat Med 2012, 2012, 607675. [Google Scholar] [CrossRef] [PubMed]
- Raja, S.; Ramya, I. A comprehensive review on Polygonum glabrum. Ijop 2017, 8, 457–467. [Google Scholar]
- Chiu, Y.J.; Chou, S.C.; Chiu, C.S.; Kao, C.P.; Wu, K.C.; Chen, C.J.; Tsai, J.C.; Peng, W.H. Hepatoprotective effect of the ethanol extract of Polygonum orientale on carbon tetrachloride-induced acute liver injury in mice. J Food Drug Anal 2018, 26, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Ow, Y.-Y.; Stupans, I. Gallic acid and gallic acid derivatives: effects on drug metabolizing enzymes. Current Drug Metabolism 2003, 4, 241–248. [Google Scholar] [CrossRef]
- Badhani, B.; Sharma, N.; Kakkar, R. Gallic acid: a versatile antioxidant with promising therapeutic and industrial applications. Rsc Advances 2015, 5, 27540–27557. [Google Scholar] [CrossRef]
- Kim, S.R.; Lee, E.Y.; Kim, D.J.; Kim, H.J.; Park, H.R. Quercetin Inhibits Cell Survival and Metastatic Ability via the EMT-mediated Pathway in Oral Squamous Cell Carcinoma. Molecules 2020, 25. [Google Scholar] [CrossRef] [PubMed]
- Pinmai, K.; Chunlaratthanabhorn, S.; Ngamkitidechakul, C.; Soonthornchareon, N.; Hahnvajanawong, C. Synergistic growth inhibitory effects of Phyllanthus emblica and Terminalia bellerica extracts with conventional cytotoxic agents: doxorubicin and cisplatin against human hepatocellular carcinoma and lung cancer cells. World J Gastroenterol 2008, 14, 1491–1497. [Google Scholar] [CrossRef]
- Gopalakrishnan, A.; Tony Kong, A.N. Anticarcinogenesis by dietary phytochemicals: cytoprotection by Nrf2 in normal cells and cytotoxicity by modulation of transcription factors NF-kappa B and AP-1 in abnormal cancer cells. Food Chem Toxicol 2008, 46, 1257–1270. [Google Scholar] [CrossRef]
- Ramos, S. Cancer chemoprevention and chemotherapy: dietary polyphenols and signalling pathways. Mol Nutr Food Res 2008, 52, 507–526. [Google Scholar] [CrossRef]
- Hybertson, B.M.; Gao, B.; Bose, S.K.; McCord, J.M. Oxidative stress in health and disease: the therapeutic potential of Nrf2 activation. Mol Aspects Med 2011, 32, 234–246. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.J.; Sun, Z.; Villeneuve, N.F.; Zhang, S.; Zhao, F.; Li, Y.; Chen, W.; Yi, X.; Zheng, W.; Wondrak, G.T.; et al. Nrf2 enhances resistance of cancer cells to chemotherapeutic drugs, the dark side of Nrf2. Carcinogenesis 2008, 29, 1235–1243. [Google Scholar] [CrossRef] [PubMed]
- Velmurugan, K.; Alam, J.; McCord, J.M.; Pugazhenthi, S. Synergistic induction of heme oxygenase-1 by the components of the antioxidant supplement Protandim. Free Radical Biology and Medicine 2009, 46, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.; Montella, M. Activation of the Nrf2–ARE signaling pathway: a promising strategy in cancer prevention. Bioessays 2006, 28, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Surh, Y.-J.; Kundu, J.K.; Na, H.-K. Nrf2 as a master redox switch in turning on the cellular signaling involved in the induction of cytoprotective genes by some chemopreventive phytochemicals. Planta medica 2008, 74, 1526–1539. [Google Scholar] [CrossRef] [PubMed]
- Hybertson, B.M.; Gao, B.; Bose, S.K.; McCord, J.M. Oxidative stress in health and disease: The therapeutic potential of Nrf2 activation. Molecular Aspects of Medicine 2011, 32, 234–246. [Google Scholar] [CrossRef]
- Liu, J.; Gu, X.; Robbins, D.; Li, G.; Shi, R.; McCord, J.M.; Zhao, Y. Protandim, a Fundamentally New Antioxidant Approach in Chemoprevention Using Mouse Two-Stage Skin Carcinogenesis as a Model. PLOS ONE 2009, 4, e5284. [Google Scholar] [CrossRef]
- Robbins, D.; Gu, X.; Shi, R.; Liu, J.; Wang, F.; Ponville, J.; McCord, J.M.; Zhao, Y. The Chemopreventive Effects of Protandim: Modulation of p53 Mitochondrial Translocation and Apoptosis during Skin Carcinogenesis. PLOS ONE 2010, 5, e11902. [Google Scholar] [CrossRef]
- Nelson, S.K.; Bose, S.K.; Grunwald, G.K.; Myhill, P.; McCord, J.M. The induction of human superoxide dismutase and catalase in vivo: a fundamentally new approach to antioxidant therapy. Free Radical Biology and Medicine 2006, 40, 341–347. [Google Scholar] [CrossRef]
- Li, J.; Chen, J.; Kirsner, R. Pathophysiology of acute wound healing. Clinics in dermatology 2007, 25, 9–18. [Google Scholar] [CrossRef]
- Bishop, A. Role of oxygen in wound healing. Journal of wound care 2008, 17, 399–402. [Google Scholar] [CrossRef]
- Rodriguez, P.G.; Felix, F.N.; Woodley, D.T.; Shim, E.K. The role of oxygen in wound healing: a review of the literature. Dermatologic surgery 2008, 34, 1159–1169. [Google Scholar] [CrossRef]
- Gompelman, M.; van Asten, S.A.; Peters, E.J. Update on the role of infection and biofilms in wound healing: pathophysiology and treatment. Plastic and reconstructive surgery 2016, 138, 61S–70S. [Google Scholar] [CrossRef]
- Molinas, A.; Turkina, M.V.; Magnusson, K.-E.; Mirazimi, A.; Vikström, E. Perturbation of wound healing, cytoskeletal organization and cellular protein networks during hazara virus infection. Frontiers in cell and developmental biology 2017, 5, 98. [Google Scholar] [CrossRef] [PubMed]
- Kapetanaki, M.G.; Mora, A.L.; Rojas, M. Influence of age on wound healing and fibrosis. The Journal of pathology 2013, 229, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Sgonc, R.; Gruber, J. Age-related aspects of cutaneous wound healing: a mini-review. Gerontology 2013, 59, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Brown, J. The impact of stress on acute wound healing. British journal of community nursing 2016, 21, S16–S22. [Google Scholar] [CrossRef] [PubMed]
- Vegas, Ó.; VanBuskirk, J.; Richardson, S.; Parfitt, D.; Helmreich, D.; Rempel, M.; Moynihan, J.; Tausk, F. Effects of psychological stress and housing conditions on the delay of wound healing. Psicothema 2012, 24, 581–586. [Google Scholar] [PubMed]
- Chandu, A. Diabetes, wound healing and complications. Australian dental journal 2013, 58, 536–536. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Tie, G.; Wang, S.; Tutto, A.; DeMarco, N.; Khair, L.; Fazzio, T.G.; Messina, L.M. Diabetes impairs wound healing by Dnmt1-dependent dysregulation of hematopoietic stem cells differentiation towards macrophages. Nature communications 2018, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pence, B.D.; Woods, J.A. Exercise, obesity, and cutaneous wound healing: evidence from rodent and human studies. Advances in wound care 2014, 3, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Pierpont, Y.N.; Dinh, T.P.; Salas, R.E.; Johnson, E.L.; Wright, T.G.; Robson, M.C.; Payne, W.G. Obesity and surgical wound healing: a current review. International Scholarly Research Notices 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Krischak, G.; Augat, P.; Claes, L.; Kinzl, L.; Beck, A. The effects of non-steroidal anti-inflammatory drug application on incisional wound healing in rats. Journal of wound care 2007, 16, 76–78. [Google Scholar] [CrossRef]
- Levine, J.M. How oral medications affect wound healing. Nursing2020 2018, 48, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Stuermer, E.K.; Besser, M.; Terberger, N.; Bachmann, H.S.; Severing, A.-L. Side effects of frequently used antihypertensive drugs on wound healing in vitro. Skin pharmacology and physiology 2019, 32, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Barbul, A. Nutrition and wound healing. Plastic and reconstructive surgery 2006, 117, 42S–58S. [Google Scholar] [CrossRef]
- Brown, K.L.; Phillips, T.J. Nutrition and wound healing. Clinics in dermatology 2010, 28, 432–439. [Google Scholar] [CrossRef]
- Lozano, S.A.; Bonet, C.M.; Bou, J. Nutrition and chronic wound healing. A clinical case of a patient with a hard to heal venous leg ulcers. Revista de enfermeria (Barcelona, Spain) 2014, 37, 26–30. [Google Scholar]
- Zinder, R.; Cooley, R.; Vlad, L.G.; Molnar, J.A. Vitamin A and wound healing. Nutrition in Clinical Practice 2019, 34, 839–849. [Google Scholar] [CrossRef]
- Mohammed, B.M.; Fisher, B.J.; Kraskauskas, D.; Ward, S.; Wayne, J.S.; Brophy, D.F.; Fowler III, A.A.; Yager, D.R.; Natarajan, R. Vitamin C promotes wound healing through novel pleiotropic mechanisms. International wound journal 2016, 13, 572–584. [Google Scholar] [CrossRef] [PubMed]
- Hobson, R. Vitamin E and wound healing: an evidence-based review. International wound journal 2016, 13, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Campos, A.C.; Groth, A.K.; Branco, A.B. Assessment and nutritional aspects of wound healing. Current Opinion in Clinical Nutrition & Metabolic Care 2008, 11, 281–288. [Google Scholar]
- Polcz, M.E.; Barbul, A. The role of vitamin A in wound healing. Nutrition in Clinical Practice 2019, 34, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Melguizo-Rodríguez, L.; Illescas-Montes, R.; Costela-Ruiz, V.J.; Ramos-Torrecillas, J.; de Luna-Bertos, E.; García-Martínez, O.; Ruiz, C. Antimicrobial properties of olive oil phenolic compounds and their regenerative capacity towards fibroblast cells. Journal of Tissue Viability 2021, 30, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Baldioli, M.; Servili, M.; Perretti, G.; Montedoro, G. Antioxidant activity of tocopherols and phenolic compounds of virgin olive oil. Journal of the American Oil Chemists’ Society 1996, 73, 1589–1593. [Google Scholar] [CrossRef]
- Servili, M.; Esposto, S.; Fabiani, R.; Urbani, S.; Taticchi, A.; Mariucci, F.; Selvaggini, R.; Montedoro, G. Phenolic compounds in olive oil: antioxidant, health and organoleptic activities according to their chemical structure. Inflammopharmacology 2009, 17, 76–84. [Google Scholar] [CrossRef]
- Silva, S.; Sepodes, B.; Rocha, J.; Direito, R.; Fernandes, A.; Brites, D.; Freitas, M.; Fernandes, E.; Bronze, M.R.; Figueira, M.E. Protective effects of hydroxytyrosol-supplemented refined olive oil in animal models of acute inflammation and rheumatoid arthritis. J Nutr Biochem 2015, 26, 360–368. [Google Scholar] [CrossRef]
- Garcia-Martinez, O.; Ruiz, C.; Gutierrez-Ibanez, A.; Illescas-Montes, R.; Melguizo-Rodriguez, L. Benefits of olive oil phenolic compounds in disease prevention. Endocrine, Metabolic & Immune Disorders-Drug Targets (Formerly Current Drug Targets-Immune, Endocrine & Metabolic Disorders) 2018, 18, 333–340. [Google Scholar]
- Melguizo-Rodriguez, L.; Manzano-Moreno, F.J.; De Luna-Bertos, E.; Rivas, A.; Ramos-Torrecillas, J.; Ruiz, C.; Garcia-Martinez, O. Effect of olive oil phenolic compounds on osteoblast differentiation. Eur J Clin Invest 2018, 48, e12904. [Google Scholar] [CrossRef]
- Melguizo-Rodríguez, L.; Manzano-Moreno, F.J.; Illescas-Montes, R.; Ramos-Torrecillas, J.; de Luna-Bertos, E.; Ruiz, C.; García-Martínez, O. Bone protective effect of extra-virgin olive oil phenolic compounds by modulating osteoblast gene expression. Nutrients 2019, 11, 1722. [Google Scholar] [CrossRef] [PubMed]
- Mota, A.H.; Silva, C.O.; Nicolai, M.; Baby, A.; Palma, L.; Rijo, P.; Ascensao, L.; Reis, C.P. Design and evaluation of novel topical formulation with olive oil as natural functional active. Pharm Dev Technol 2017, 1–12. [Google Scholar] [CrossRef]
- Fitó, M.; de la Torre, R.; Covas, M.I. Olive oil and oxidative stress. Mol Nutr Food Res 2007, 51, 1215–1224. [Google Scholar] [CrossRef]
- Kim, S.-K. Marine cosmeceuticals: trends and prospects; CRC Press, 2011. [Google Scholar]
- Castillo-Luna, A.; Criado-Navarro, I.; Ledesma-Escobar, C.A.; López-Bascón, M.A.; Priego-Capote, F. The decrease in the health benefits of extra virgin olive oil during storage is conditioned by the initial phenolic profile. Food Chemistry 2021, 336, 127730. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products, N. Allergies. Scientific Opinion on the substantiation of health claims related to polyphenols in olive and protection of LDL particles from oxidative damage (ID 1333, 1638, 1639, 1696, 2865), maintenance of normal blood HDL cholesterol concentrations (ID 1639), maintenance of normal blood pressure (ID 3781),“anti-inflammatory properties”(ID 1882),“contributes to the upper respiratory tract health”(ID 3468),“can help to maintain a normal function of gastrointestinal tract”(3779), and “contributes to body defences against external agents”(ID 3467) pursuant to Article 13 (1) of Regulation (EC) No 1924/2006. EFSA journal 2011, 9, 2033. [Google Scholar]
- Guasch-Ferré, M.; Hu, F.B.; Martínez-González, M.A.; Fitó, M.; Bulló, M.; Estruch, R.; Ros, E.; Corella, D.; Recondo, J.; Gómez-Gracia, E. Olive oil intake and risk of cardiovascular disease and mortality in the PREDIMED Study. BMC medicine 2014, 12, 1–11. [Google Scholar] [CrossRef]
- Maamoun, M.A.I. An Insight into the Brilliant Benefits of Grape Waste. In Mediterranean Fruits Bio-wastes; Springer, 2022; pp. 433–465. [Google Scholar]
- Barros, A.; Gironés-Vilaplana, A.; Texeira, A.; Baenas, N.; Domínguez-Perles, R. Grape stems as a source of bioactive compounds: application towards added-value commodities and significance for human health. Phytochemistry Reviews 2015, 14, 921–931. [Google Scholar] [CrossRef]
- Teixeira, A.; Baenas, N.; Dominguez-Perles, R.; Barros, A.; Rosa, E.; Moreno, D.A.; Garcia-Viguera, C. Natural bioactive compounds from winery by-products as health promoters: A review. International journal of molecular sciences 2014, 15, 15638–15678. [Google Scholar] [CrossRef] [PubMed]
- Ferreyra, S.; Torres-Palazzolo, C.; Bottini, R.; Camargo, A.; Fontana, A. Assessment of in-vitro bioaccessibility and antioxidant capacity of phenolic compounds extracts recovered from grapevine bunch stem and cane by-products. Food Chemistry 2021, 348, 129063. [Google Scholar] [CrossRef] [PubMed]
- Sáez, V.; Pastene, E.; Vergara, C.; Mardones, C.; Hermosín-Gutiérrez, I.; Gómez-Alonso, S.; Gómez, M.V.; Theoduloz, C.; Riquelme, S.; von Baer, D. Oligostilbenoids in Vitis vinifera L. Pinot Noir grape cane extract: Isolation, characterization, in vitro antioxidant capacity and anti-proliferative effect on cancer cells. Food Chemistry 2018, 265, 101–110. [Google Scholar] [CrossRef] [PubMed]
- ZGHONDA, N.; YOSHIDA, S.; EZAKI, S.; OTAKE, Y.; MURAKAMI, C.; MLIKI, A.; GHORBEL, A.; MIYAZAKI, H. ε-Viniferin Is More Effective Than Its Monomer Resveratrol in Improving the Functions of Vascular Endothelial Cells and the Heart. Bioscience, Biotechnology, and Biochemistry 2012, 76, 954–960. [Google Scholar] [CrossRef] [PubMed]
- Willenberg, I.; Michael, M.; Wonik, J.; Bartel, L.C.; Empl, M.T.; Schebb, N.H. Investigation of the absorption of resveratrol oligomers in the Caco-2 cellular model of intestinal absorption. Food Chemistry 2015, 167, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Guschlbauer, M.; Klinger, S.; Burmester, M.; Horn, J.; Kulling, S.E.; Breves, G. trans-Resveratrol and ε-viniferin decrease glucose absorption in porcine jejunum and ileum in vitro. Comparative Biochemistry and Physiology Part A: Molecular & Integrative Physiology 2013, 165, 313–318. [Google Scholar] [CrossRef]
- Goufo, P.; Singh, R.K.; Cortez, I. A Reference List of Phenolic Compounds (Including Stilbenes) in Grapevine (Vitis vinifera L.) Roots, Woods, Canes, Stems, and Leaves. Antioxidants 2020, 9, 398. [Google Scholar] [CrossRef] [PubMed]
- Ferreyra, S.G.; Antoniolli, A.; Bottini, R.; Fontana, A. Bioactive compounds and total antioxidant capacity of cane residues from different grape varieties. Journal of the Science of Food and Agriculture 2020, 100, 376–383. [Google Scholar] [CrossRef]
- Ferreyra, S.; Bottini, R.; Fontana, A. Assessment of grapevine stems as source of phenolics with antioxidant properties. Revista de la Facultad de Ciencias Agrarias UNCuyo 2019, 51, 417–426. [Google Scholar]
- Jimenez-Lopez, C.; Fraga-Corral, M.; Carpena, M.; Garcia-Oliveira, P.; Echave, J.; Pereira, A.G.; Lourenco-Lopes, C.; Prieto, M.A.; Simal-Gandara, J. Agriculture waste valorisation as a source of antioxidant phenolic compounds within a circular and sustainable bioeconomy. Food & Function 2020, 11, 4853–4877. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




