Introduction
Medication overuse headache (MOH) is a secondary headache classified according to the International Headache Society as a group of headaches attributed to the use or discontinuation of various substances [1]. MOH occurs 15 or more days per month in patients with preexisting headaches. It occurs due to regular (at least three consecutive months) overuse (10 days or 15 days for certain medications) of medicines used for acute or symptomatic headache therapy. MOH can occur due to the excessive use of ergotamine, triptans, ordinary analgesics (pracetamol, acetylsalicylic acid, nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, combined analgesics, or simultaneous use of several types of drugs.
This type of headache most often occurs in the fourth decade (between 30 and 50 years of age) and is more common in women (female-to-male ratio is 3- 4:1) [3]. The estimated prevalence of MOH is approximately 3%. The burden on the patient and his family is a consequence of the impairment of the quality of daily life. The MOH represents a significant burden on the health system and society as a whole and affects the reduction of working capacity, often missing work [1,3].
Although it can occur from any type of headache, MOS is most often caused by the chronic transformation of migraine. The complete mechanism underlying the pathophysiological process that leads to this condition has not been fully elucidated. It is assumed that processes of central sensitization (suppression of endogenous pain modulation, neuronal excitability due to neurotransmitter imbalances [adrenaline, serotonin], etc.) represent the pathogenetic basis of MOH [4–7].
MOH treatment involves educating patients about the necessity of limited use of analgesics, most often with the simultaneous implementation of detoxification therapy and prophylactic support of coanalgetic therapy (valproate, topiramate, amitriptyline, onabotulinum toxin A, etc.). This can be done in an outpatient or hospital setting. During the use of triptans, ergotamine, and NSAIDS, individuals are advised to abruptly stop the excessive use of these drugs. On the other hand, a gradual reduction in the dose of the drug is recommended for previous overuse of barbiturates, benzodiazepines and opioids [9,10].
Although MOH is considered potentially preventable, changeable and unchanging risk factors for MOH have not yet been recognized. Identifying these risk factors could aid in identifying patients with a previous headache who are at higher risk for chronic headache and transforming a previous headache into MOH.
Research Objective
The research aimed to examine the following:
Materials and Methods
This research was conducted as part of a project approved by the Ethics Committee of the Faculty of Medicine in Niš as an observational, cross-sectional study.
The study included all patients examined at the Headache Clinic of the Neurology Clinic, Clinical Center in Nis, during 2019 (January-December), in whom the diagnosis of MOH was made for the first time during this period. Patients gave informed consent to participate in the study.
The diagnosis of MOH was made according to the current diagnostic criteria of the International Classification of Headaches [1]. In all patients, the second etiology of the headache was excluded after complete diagnostic processing (computed tomography, magnetic resonance imaging, etc.).
The following data were collected from the included patients: demographic data; a history of personal life; the presence of other diseases; the presence of previous (primary and/or secondary) headaches (type, characteristics, duration of headache, frequency of occurrence, effectiveness of symptomatic and preventive therapy); and habits and risk factors (physical activity, smoking cigarettes, use of alcohol, caffeine, etc.).
The data related to MOH included the location of pain (frontal, temporal, parietal, occipital), lateralization (unilateral, diffuse), character (dull, pulsating pain), intensity of the pain (using a numerical scale to assess pain), the existence of associated symptoms and signs (nausea/vomiting, photophobia, phonophobia, diplopia, neck and shoulder tightness: blurred vision, ringing in the ears: hyperacusis), type of analgesic therapy used, preventive therapy, frequency of use of this therapy (number of days/month), effectiveness of the therapy, and effect of headaches on the activities of everyday life (headache impact test - HIT).
For the statistical processing of the data, a single database was constructed in which descriptive and analytical statistics were applied. All the statistical analyses were carried out with the SPSS 16.0 software package.
Results
The study included 83 patients with MOH—11 men and 72 women. The mean age of these patients was 40.5±11.6 years (range: 18 to 71 years).
By analyzing the frequency of the parameters studied, it was observed that, in the cohort of patients with MOH, there were more women, nonsmokers, and nondrinkers (daily use/use a greater number of days per week); they were physically inactive (daily/greater number of days per week); and they had comorbidities in the form of cardiovascular, bone and joint diseases (
Table 1).
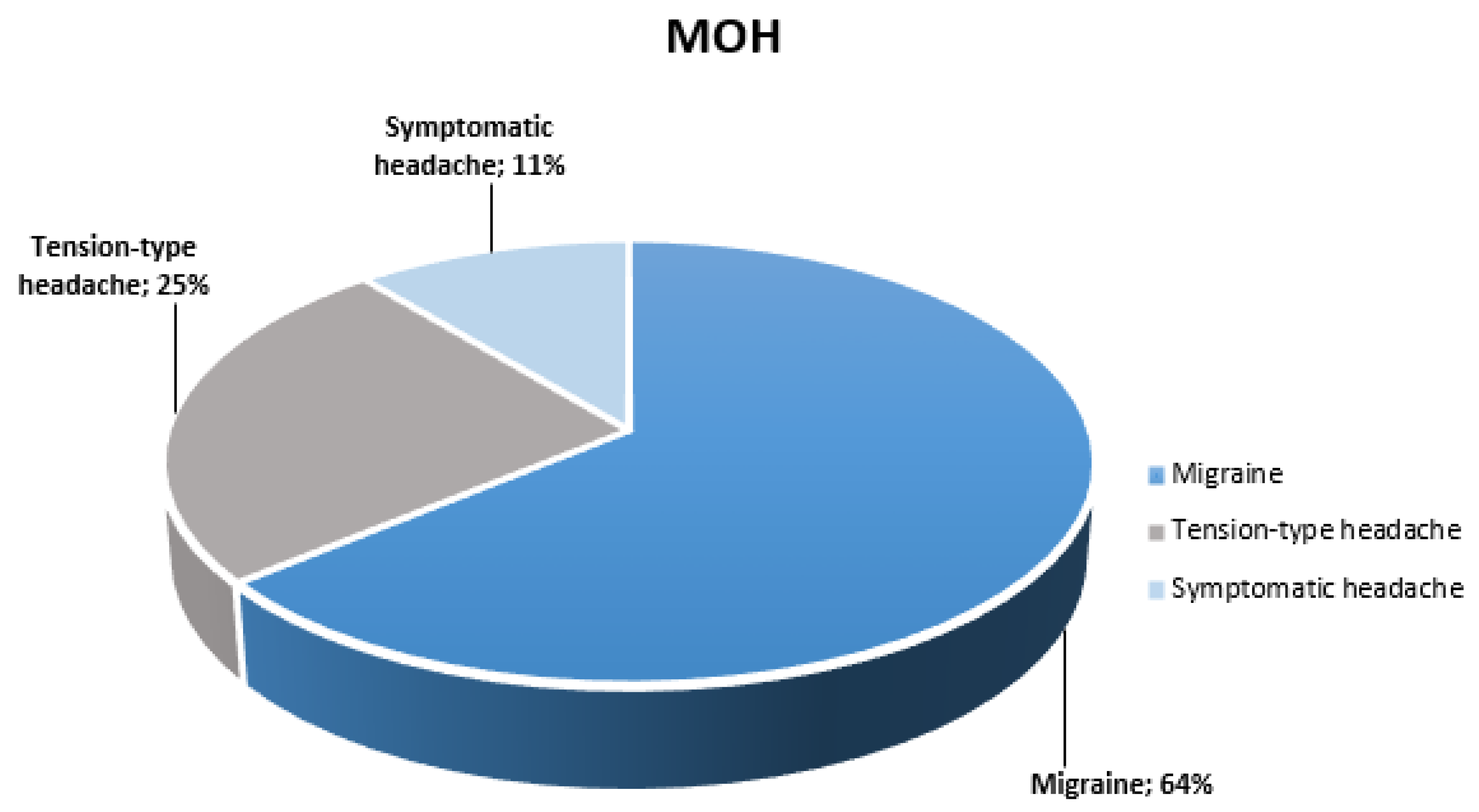
MOH was more common in migraine patients (64%) than in patients with tension-type headache (25%) or symptomatic headache (11%). The duration of the primary headache was 6.5 ± 3.2 years (
Figure 1).
In the study group, the average duration of MOH (up to the time of diagnosis) was more than 5 years, more than half a month was affected by headache, and the duration of individual headache attacks was more than 10 hours per day. Patients described the pain as moderate to severe (45.8%), bilateral (56.6%), mostly temporal (65.1%), or most often accompanied by complaints in the form of neck tightness (81.9%). Most patients used ordinary analgesics (NSAIDs) (41%) or combined analgesics (48.2%), averaging 15 to 25 days per month. This treatment was ineffective in the largest percentage of patients (78.3%).
A large number of patients used prophylactic therapy and antidepressant drugs (83.1%). The effect of headaches on activities of daily living was assessed as significant (HIT - 65.4±5.5) (
Table 2).
The correlation analysis revealed only the association between the duration of the previous headache and the effect of MOH on daily life activities (HIT) (r=0.327, p=0.003).
Discussion
The results of our research confirm the results of earlier studies (1, 3, 11 - 14) that MOH occurs mainly in middle age and more often in women.
Interestingly, the largest percentage of patients in our study did not smoke or consume alcohol, while the majority of them were physically inactive and regularly consumed caffeinated beverages. In the literature reviewed, no significant studies were found, the results of which could be useful for comparison with the results obtained here. A study examining various risk factors for MOH revealed a correlation between physical inactivity and smoking and MOH onset [14]. Our results are partially consistent with those findings. Studies examining the characteristics of patients who have never had a headache in their lives have shown that they were men of younger ages who regularly consumed alcoholic beverages (unpublished results). Our findings on the inverse relationship between alcohol consumption and the occurrence of MOH are consistent with these findings. Although most patients with MOH do not have comorbidities, the incidence of cardiovascular, bone and joint diseases was significantly greater than that of other comorbid conditions. The reasons for these findings should be considered because arterial hypertension and spondylosis of the cervical spine (the most common diagnoses in these patients) are the most common causes of secondary chronic headaches [1]. This headache, due to its chronic course, poses a risk of developing MOH. Previous studies have shown an association between disease involving the osseous joint system and MOH [14].
Although MOH can arise from all primary headaches, MOH is most often caused by the transformation of chronic migraine [1]. The results of our study showed that the highest percentage of patients with MOH previously had chronic migraines.
Our research has shown that MOH is most often caused by the excessive use of combined and ordinary analgesics (NSAIDs). The risk of MOH has previously been shown to be lower with triptans and ergotamine use than with NSAIDs [17]. Although they used prophylactic therapy, for the most part, patients with MOH did not achieve satisfactory therapeutic efficacy.
The high values obtained here on the scale of assessment of the impact of headaches on daily life activities are in agreement with the results of previous studies [13].
Research devoted to examining the pathophysiological mechanisms of MOH has shown morphometric and functional changes in regions crucial for the modulation of nociception (periaqueductal gray matter, posterior cingular cortex, hippocampus, thalamus, orbitofrontal cortex, anterior cingular gyrus, insula, and precuneus) [15,16]). These structures are involved in nociception modulation, cognition, and affective and addictive behavior. The mechanisms of central sensitization (hyperexcitability of pain modulation pathways) are considered crucial in the pathophysiology of MOH [1]. Bilateral, moderately severe pain accompanied by tightness in the neck and shoulders and the absence of so-called migraine features of MOH in our study (even though it is largely due to the transformation of previous chronic migraine) support the previously assumed mechanisms of central sensitization.
Conclusion
MOH results from the transformation of a previous chronic headache due to overuse of analgesic therapy.
It affects the middle-aged population, mostly women, and affects all aspects of the patient's life.
Despite defined therapeutic strategies for treatment, prevention of MOH is considered inviolable (patient education, limiting the use of analgesic therapy, especially in the at-risk group of patients (middle-aged women with chronic migraine)).
However, further investigations of other potentially modifiable risk factors for the development of MOH and its course and outcome after certain therapeutic interventions are necessary.
Declarations
Ethics approval and consent to participate
Author Contributions
SLJ made the initial plan and wrote the abstract, the introduction, and all the sections. RAD and ST participated in the planning of the Manuscript, the litera- ture list, and wrote the sections about medication overuse headache pathology.
Data Availability Statement
On request.
Acknowledgments
Marina Ljubisavljevic for her support in this paper revision.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Consent for Publication
Yes.
References
- Headache Classification Committee of the International Headache Society (2018) Headache Classification Committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia 38:1–211. [CrossRef]
- Headache Classification Subcommittee of the International Headache Society (2004) The international classification of headache disorders: 2nd edition. Cephalalgia 24(Suppl 1):9–160. [CrossRef]
- Westergaard ML, Hansen EH, Glümer C, et al (2014) Definitions of medication-overuse headache in population-based studies and their implications on prevalence estimates: a systematic review. Cephalalgia 34:409–425. [CrossRef]
- Okada-Ogawa A, Porreca F, Meng ID (2009) Sustained morphine- induced sensitization and loss of diffuse noxious inhibitory controls (DNIC) in dura-sensitive medullary dorsal horn neurons. J Neurosci 29:15828–15835. [CrossRef]
- Srikiatkhachorn A, Tarasub N, Govitrapong P (2000) Effect of chronic analgesic exposure on the central serotonin system: a possible mechanism of analgesic abuse headache. Headache 40:343–350. [CrossRef]
- Tohyama Y, Yamane F, Merid MF, Diksic M (2001) Effects of selective 5-HT1 Areceptor antagonists on regional serotonin synthesis in the rat brain: an autoradiographic study with alpha-[14C] methyl-L-tryptophan. Eur Neuropsychopharmacol 11:193–202. [CrossRef]
- Dobson CF, Tohyama Y, Diksic M, Hamel E (2004) Effects of acute or chronic administration of anti-migraine drugs sumatriptan and zolmitriptan serotonin synthesis in the rat brain. Cephalalgia 24:2–11. [CrossRef]
- Rapoport AM (2008) Medication overuse headache: awareness, detection and treatment. CNS Drugs 22:995–1004. [CrossRef]
- Evers S, Jensen R, European Federation of Neurological Societies (2011) Treatment of medication overuse headache??Guideline of the EFNS headache panel. Eur J Neurol 18:1115–1121. [CrossRef]
- de Goffau MJ, Klaver ARE, Willemsen MG, et al (2016) The effectiveness of treatments for patients with medication overuse headache; a systematic review and meta-analysis. J Pain 18:615–627. [CrossRef]
- Ayzenberg I, Katsarava Z, Sborowski A, et al (2012) The prevalence of primary headache disorders in Russia: a countrywide survey. Cephalalgia 32: 373–381. [CrossRef]
- Linde M, Gustavsson A, Stovner LJ, et al (2012) The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol 19:703–711. [CrossRef]
- Mathew NT, Stubits E, Nigam MP (1982) Transformation of episodic migraine into daily headache: analysis of factors. Headache J Head Face Pain 22:66–68. [CrossRef]
- Hagen K, Albretsen C, Vilming ST, et al (2011) A 4-year follow-up of patients with medication-overuse headache previously included in a randomized multicenter study. J Headache Pain 12:315–322. [CrossRef]
- Schwedt TJ, Chong CD (2017) Medication overuse headache: Pathophysiological insights from structural and functional brain MRI research. Headache J Head Face Pain 57(7):1173–1178. [CrossRef]
- Lai T, Wang S (2018) Neuroimaging findings in patients with medication overuse headache. Curr Pain Headache Rep 22:1. [CrossRef]
- de Goffau MJ, Klaver ARE, Willemsen MG, et al (2016) The effectiveness Of treatments for patients with medication overuse headache; a systematic review and meta-analysis. J Pain 18:615–627. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).