1. Introduction
There are approximately 4.5 million shoulder pain patient visits and 250,000 rotator cuff (RC) repairs annually at continuously increasing rates [
1]. The RC provides a wide range of shoulder movement and stabilizes the glenohumeral joint through the contraction of the subscapularis, infraspinatus, teres minor, and supraspinatus muscles [
2]. “Shoulder pain and weakness are often associated with shoulder conditions, including RC disorders, adhesive capsulitis, superior labrum, bicep lesions, acromioclavicular joint disease, and instability” [
3]. The shoulder is the most mobile and unstable joint in the body as it is a ball-and-socket joint that forms an extremely shallow articulation, making it susceptible to injury [
3]. RC injuries can be diagnosed through physical examination and imaging modalities. Diagnostic imaging often includes radiography, ultrasound, and MRI. Common causes of RC tears include falls, shoulder dislocation, violent pull or sudden traction injury, direct trauma or impact to the shoulder, hyperextension, and lifting heavy objects. Factors that increase the risk of RC tears include age, hand dominance, history of trauma, nicotine use, hypercholesterolemia, and genetics [
1]. The impact of age on RC defects has been found to affect up to 70% of people over 70 [
4]. Elderly patients often present multiple risk factors, including decreased bone quality, poor blood supply, and increased medical comorbidities [
5]. Diabetes and other systemic disorders have also been associated with a greater risk of RC defects [
6]. The structural integrity of the connective tissue matrix found in the RC is imperative when considering repair.
Current treatment for RC tears primarily exists as nonsurgical or surgical. Asymptomatic tears are typically managed through nonsurgical techniques determined by tear thickness, size, and morphology [
7]. The most common nonsurgical treatment plans include NSAIDS, physical therapy, and injections. A study by Maman et al. (2009) found that patients older than 60 have a 54% deteriorating rate compared to younger patients with a 17% deteriorating rate [
8]. Although conservative treatments have a typically high rate of success, the older population takes much longer to recover, with high risks of re-injury. When non-surgical treatments are unsuccessful, surgical operations are typically undergone to resolve RC tears. Some major concerns among orthopedic surgeons from rotator cuff surgery include high re-tear rates and decreased range of motion [
9]. The rate of re-tears has shown a strong association between the strength of the repair, the tear size, and the tissue quality of the tendon [
9]. Re-tears are common as the native tissue contains type I collagen fibers. In contrast, the repaired muscle contains more type III collagen fibers, which are more disorganized and have reduced tensile strength. Studies have been conducted to indicate that as the size of the tear increases, the likelihood of regaining the full range of motion of the affected shoulder decreases. Likewise, it is expected to take one year to regain external rotation after small and medium tears [
10]. Given the time it takes for repair and the cost of treatment, the total cost of rotator cuff repair must be considered. Annually, there are more than 250,000 rotator cuff repairs in the United States, accounting for an estimated
$1.2 to 1.6 billion in healthcare expenditures [
11]. As there is no conclusive evidence for the best treatment in elderly patients and given the significant economic burden rotator cuff repairs have on the healthcare system, it is clear there is a need for further treatment research regarding RC repairs.
This study aims to observe the efficacy and safety of Wharton’s jelly tissue allografts applied to structural defects of the rotator cuff. Wharton’s jelly (WJ) primarily comprises collagen fiber types I, III, and V, cytokines, proteoglycans, various growth factors, and hyaluronic acid. In general, each component of the WJ composition can positively impact the repair of musculoskeletal injuries [
12]. The collagen fibers present in WJ are comparable to the extracellular matrices of human articular cartilage, tendons, and dermal tissues [
13]. Studies suggest that WJ is also efficacious in other areas of the body. WJ has shown promising results in the application to defects of the Sacroiliac (SI) Joint. When WJ was applied to the SI joint, there were statistically significant improvements in function, joint mobility, and pain relief [
14]. In addition, when WJ was applied to the knee, data was analyzed to show pain alleviation, function improvement, and a potential delay in total knee replacement in patients with knee osteoarthritis [
15]. While WJ has been successfully applied in humans in over 180 different homologous use sites, it has yet to be published on defects of the human rotator cuff. However, a study by Yuan (2022) utilized WJ in a rabbit rotator cuff tendon defect and produced statistically significant data on improved tendon healing and enhanced biomechanical strength of repaired tendons [
16]. There is a severe need for alternative medical intervention with a lack of core evidence for long-term RC improvement through standard interventions.
2. Materials and Methods
All methods complied with the FDA and American Association of Tissue Banks (AATB) standards. The study was conducted in accordance with the Declaration of Helsinki and had renewed approval by the Institutional Review Board of the Institute of Regenerative and Cellular Medicine (IRCM-2022-311) on 22 February 2023. Informed consent was obtained from all patients. All data were analyzed by analysis of variance (ANOVA) and minimal clinically important difference (MCID).
2.2. Study Population
The patient data sets for this study were pulled from the retrospective repository from the research department at Regenative Labs. The inclusion criteria are as follows: patients with rotator cuff-related defects, at least one 150mg WJ tissue application, and a full 0, 30, and 90-day data set completed within the allotted time constraints. Exclusions were based on incomplete or incorrect data submissions, not on age, gender, or BMI. There were a total of 87 patients in this study. The population was divided into 42 females and 45 males. The average age of the population was 71 years old, with the youngest patient being 36 years old and the oldest patient 89 years old. The average BMI was 27.7, with the smallest being 17.1 and the greatest 38.6.
Table 1 shows the demographic characteristics of participants.
2.3. Allograft Application
Twenty clinics obtained umbilical cord tissue allografts. The application of the allografts was performed in a private medical setting. All patients underwent a professional medical history and physical examination and had exhausted over eight weeks of conservative management. All patients had evidence of structural degeneration of the symptomatic rotator cuff. All patients had failed prior systemic treatments that may have included NSAIDs, muscle relaxants, physical therapy, pain medications, and steroid injections. All patients were examined on the day of Wharton’s Jelly allograft application to confirm symptoms at the site of application, and informed consent was obtained. Under sterile technique, 2cc of Wharton’s jelly flowable allograft, or 150 mg of Wharton’s Jelly, was applied to the specific affected anatomy, the most common being supraspinatus tendon, biceps tendon insertion, labral tear, and subscapularis tear. All patients were monitored for 30 minutes post-procedure. No patients experienced post-procedure complications and were all discharged home in stable condition with instructions to maintain an active and passive range of motion of the shoulder and to avoid strenuous activity.
2.4. Questionnaire Composition
Patients were asked to fill out an initial questionnaire on the day of application, consisting of NPRS, numerical pain rating scale, WOMAC, Western Ontario and McMaster Universities arthritis index, and QOLS, quality of life scales. As this sample is from a large retrospective repository that initially focused on lower extremities, the WOMAC is not ideal for evaluating shoulder-related issues. However, it is still relevant because the patient reports their pain evaluation based on the defect relevant to their WJ application. Patients answered the same questionnaire 30 and 90 days after the initial allograft application. NPRS is a numerical pain scale employed as a subjective measurement of 0–10 for patients to rate their pain. A measurement of 0 indicates no pain, and 10 indicates the worst pain possible. WOMAC, measured on a scale of 0–4, combines three questionnaires that measure pain, stiffness, and function. A measurement of 0 indicates that the patient can perform the activity with ease, and 4 indicates that the patient has extreme difficulty performing the activity. The total WOMAC score is calculated by adding each of the individual question scores together. The scores of these two scales were analyzed individually to allow for a more significant examination of the physical mobility of the affected joint. The reported scores for each patient can be found in Appendix A.
3. Results
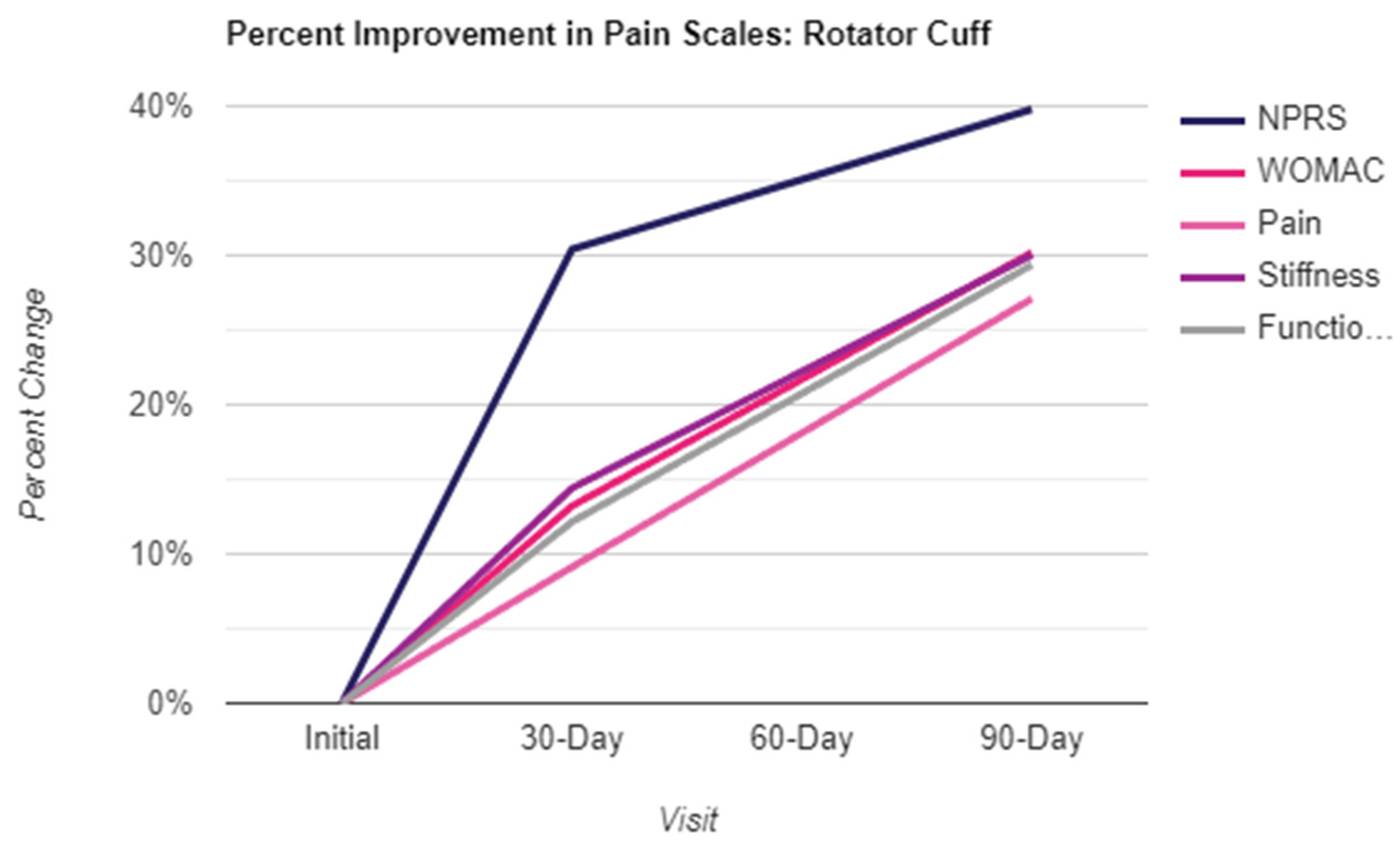
Results were obtained from three intervals, including the initial application day, day 30, and day 90. The six scales utilized to quantize pain were the NPRS, QOLS, WOMAC, and the three WOMAC subsections of pain, stiffness, and function. Shown in the table below (
Table 2) are the calculated mean and standard deviation (SD) of the six pain scales for each interval. Higher values in NPRS, WOMAC, pain, stiffness, and functionality indicate more significant pain, whereas higher values in QOLS indicate a better quality of life (not necessarily related to pain). The mean scores of the six pain scales declined over time from the Initial up to 30 days and day 90, with the most significant decline appearing between the Initial and Day 90 after the first injection. The percent improvement in patient-reported scales displayed in
Figure 1 reflects the decrease in numerical scores, indicating an improvement in pain levels.
Analysis of variance (ANOVA) and Tukey’s test were employed for continuous values, and logistic regression was performed for binary (or classified) outcomes. ANOVA tested the significance level of changes between intervals for the six pain scales. After determining these, test results suggested there were differences between intervals for WOMAC, pain, stiffness, and functionality. Accordingly, Tukey’s test was performed to identify the specific intervals that differed from each other.
Table 3 shows the actual differences in the six scales between each interval with 95% CI and p-values.
There were statistically significant differences between Initial and Day 90 for all six scales. The difference between the Initial and Day 30 is significant only for NPRS and stiffness. A p-value of (0.05) was used to assess the degree of significance.
ANOVA tested the significance level of the effect of changes for any demographic variables on the six scales. However, there was no effect on the six scales based on gender, BMI, and age. Entries in
Table 4 below are the p-values for six scales.
The anchor-based method with receiver operating characteristic (ROC) analysis was used to summarize the minimal clinically important difference (MCID). The NPRS score was recorded at the beginning of the study and rerecorded 90 days after their first injection to define anchor groups as a baseline. After removing the missing NPRS scores for Initial and Day 90, a total of 66 patients for the four pain scales and 59 for QOLS were used to determine the anchor groups. The difference in NPRS score between Initial and Day 90 was used to calculate the difference over time. The anchor question can be expressed as, “How different is your pain compared to before and after the injection?” After determining the changes, the patients were grouped into four categories by the range of changes in their NPRS scores. The grouped answers were “Not better,” negative-zero, “Slightly better,” 1-3, “Better,” 4-5, and “Much better” 6-9,
Table 5 shows the descriptive statistics between the answers.
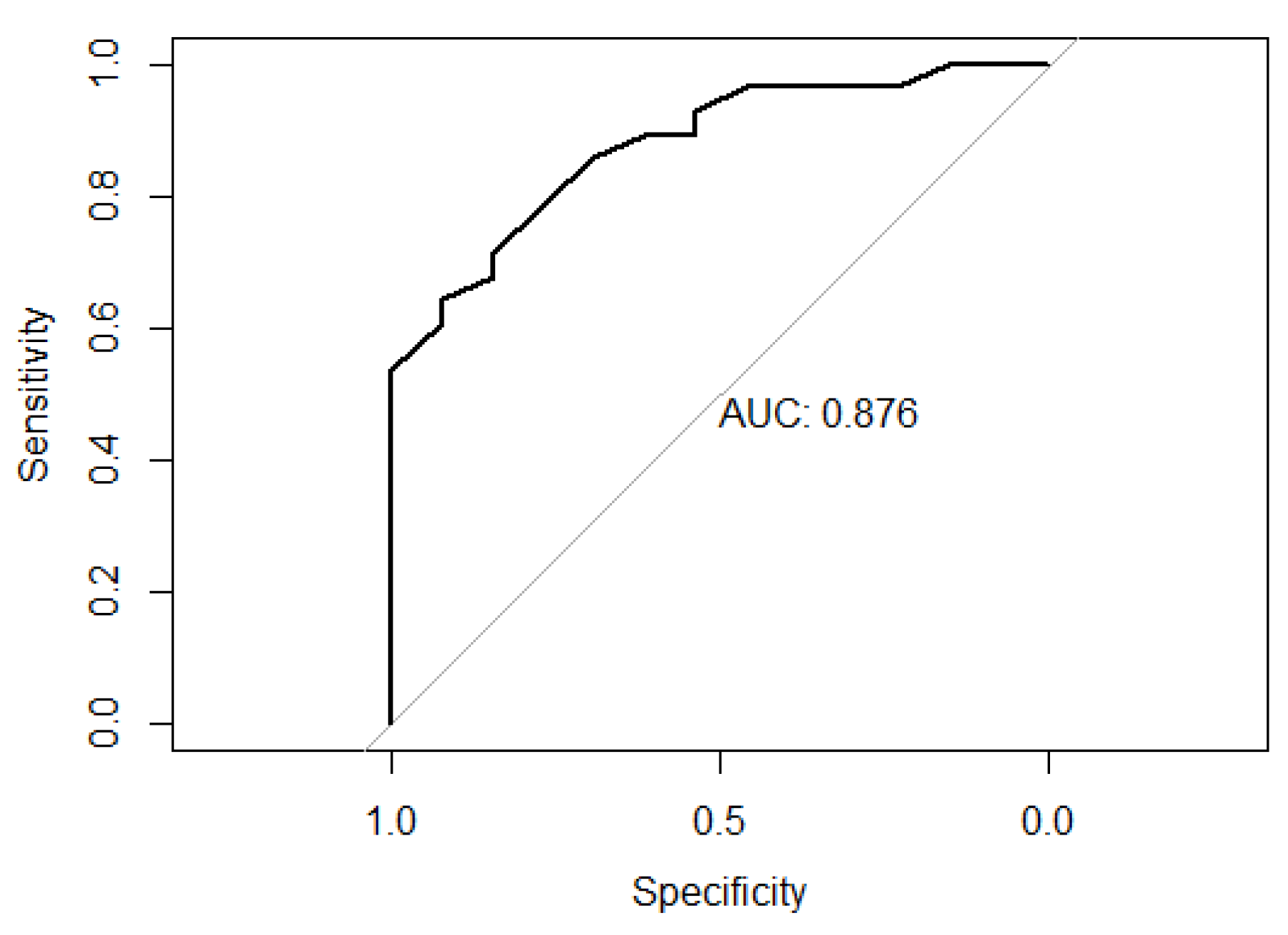
The ROC analysis determined the probability of being “Not better” or “Slightly better” and calculated the best cutoff and Area Under the Curve (AUC) based on the highest Youden’s index with the best sensitivity and specificity. The mean changes for “Slightly better” in the MCID for the five scales were estimated by choosing the Youden’s index that gave the highest AUC values (see
Table 6).
The AUC values were 0.88 for WOMAC (see
Figure 1), 0.79 for pain, 0.79 for stiffness, 0.83 for functionality, and 0.61 for QOLS. Based on the reliability of AUC, the MCID for QOLS is not meaningful in this study.
Figure 2.
ROC plot for WOMAC.
Figure 2.
ROC plot for WOMAC.
The meaningful MCIDs were 10.0 for WOMAC, 2.36 for pain, 1.21 for stiffness, and 6.43 for functionality for the anchor group (see
Table 7).
4. Discussion
The patients in this retrospective study achieved successful results in 90 days after failing standard-of-care practices for at least eight weeks. Typically, patients who fail nonoperative treatment do so in the first 12 weeks [
17]. For all age ranges, most studies show a success rate of 75% for nonoperative treatment [
18]. The sample patient population used in this study represents patients in the remaining 25% who do not benefit from physical therapy and saw minimal improvement in the standard care amount of time. Instead of proceeding with a surgical procedure after failed nonoperative treatments, the patients in this study cut costs and recovery time by not having surgical intervention and subsequent rehab or medications. Another significant factor is that the mean age of the sample is 71 years old, and the statistics showed no differentiation in improvement relating to age. When a patient reaches 60 years or older, current literature shows the progression of a rotator cuff tear or retear increases significantly, further complicating treatment and diminishing success rates.
One of the tests utilized to analyze the data was ANOVA. ANOVA tests whether the difference in mean changes between the groups are equal or not. Even though ANOVA results represent a significant difference in groups, they do not provide the exact pair of groups that are different. Therefore, Tukey’s test was used to identify which specific groups differed from each other. Tukey’s test was used as it functions to compare the mean of each treatment to the mean of all other treatments. In this study, ANOVA tested the significance of change between the intervals of the pain scales. ANOVA results presented a difference between intervals for WOMAC and its subsections. Given this information, Tukey’s test was performed to determine how the intervals differed from each other. There was a reported statistically significant difference between the initial application and Day 90 for all six pain scales.
MCID was used to quantify the importance of the pain relief experienced by the patients. The purpose of MCID is to identify the minimum and meaningful differences that are useful for the interpretation of a patient’s improvement. To establish the MCID on WOMAC (with subsections) and QOLS, the groups “Not better” and “slightly better” were used to define the MCID. AUC was used to quantize the mean changes for “slightly better” in the MCID for the pain scales. Of all the scales, QOLS is the only scale that was not meaningful. AUC is considered to be meaningful if it has a value of 0.7 to 0.8 or above. Any value less than 0.7 is considered to be insignificant. This lack of change was expected as the quality of life scale used focused primarily on aspects of the patient’s life unrelated to physical pain. Future studies might incorporate a quality-of-life scale that better evaluates how the patient’s injury affects the quality of life.
Through this study, the statistically significant improvements found in both NPRS and WOMAC scales show that WJ is effective and safe in its application to structural defects of the rotator cuff. These findings are consistent with the results of a knee osteoarthritis study in 2020, in which a total of 34 out of 42 patients reported significant clinical improvement [
15]. A Sacroiliac Joint study in 2022 reported 32 of 38 patients with a lowered NPRS, and 29 of 38 patients reported a lowered WOMAC score [
14]. In addition to the structural collagen matrix of WJ, the growth factors, cytokines, proteoglycans, and hyaluronic acid may be positive contributing factors to its success as a tissue transplant [
13]. The perinatal tissue is considered immune privileged, not eliciting an immune response. The lack of immune response was reflected in the rotator cuff applications presented, with no adverse reactions reported from any patients. Combining the efficacy and safety of WJ observed, it is clear that WJ is an optimal option in the use of rotator cuff injuries.
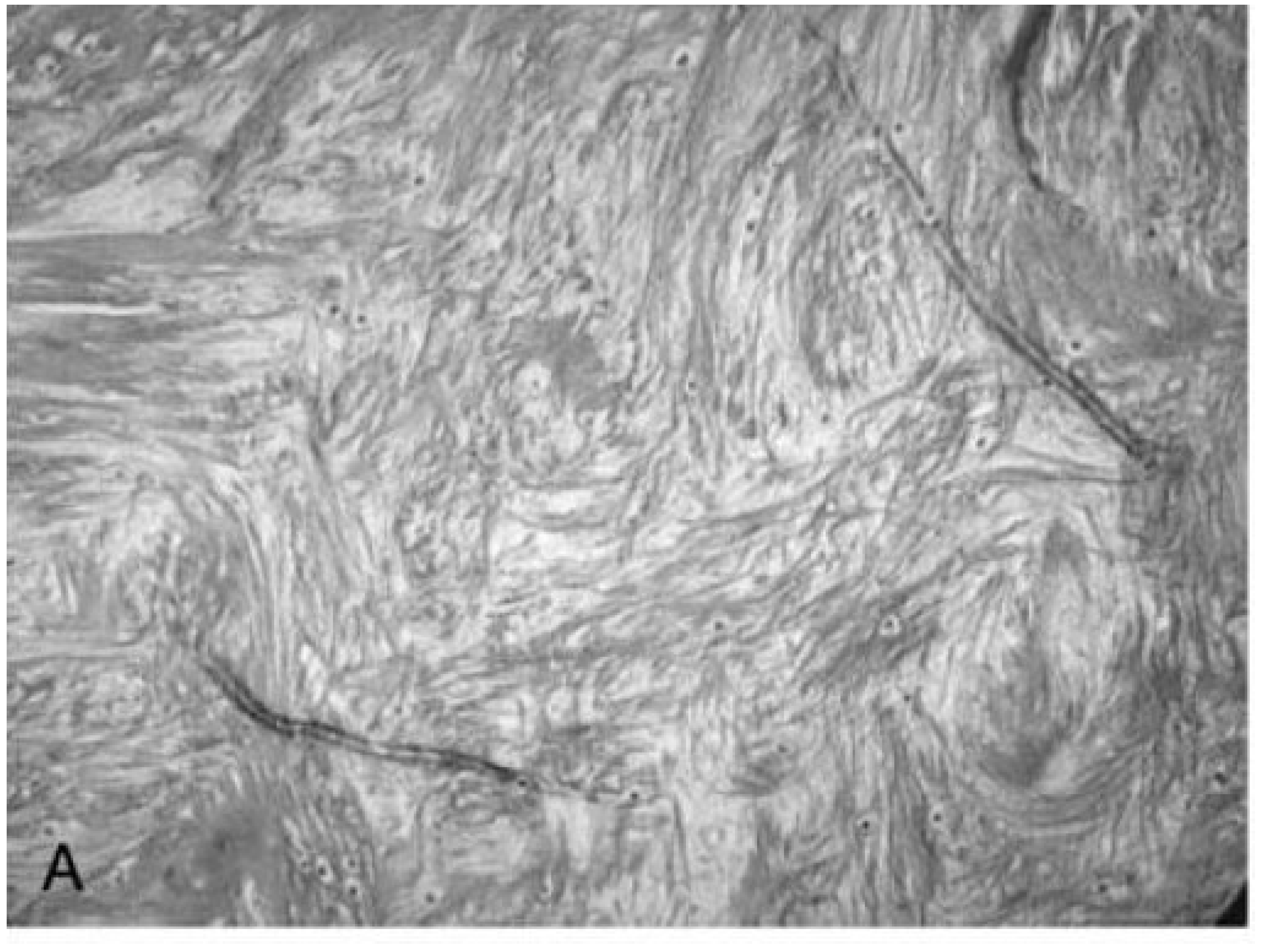
Along with patient-reported improvement, the microstructures of the rotator cuff and WJ allografts can be observed for homologous structures. Collagen accounts for over 80% of the dry weight of human tendons, with the primary types being collagen I and III [
19]. A study by Hashimoto et al. in 2003 performed a histopathologic examination revealing the thinned, snapped, and disorientated collagen fibers of the shoulder tendon in a 74-year-old patient (
Figure A) [
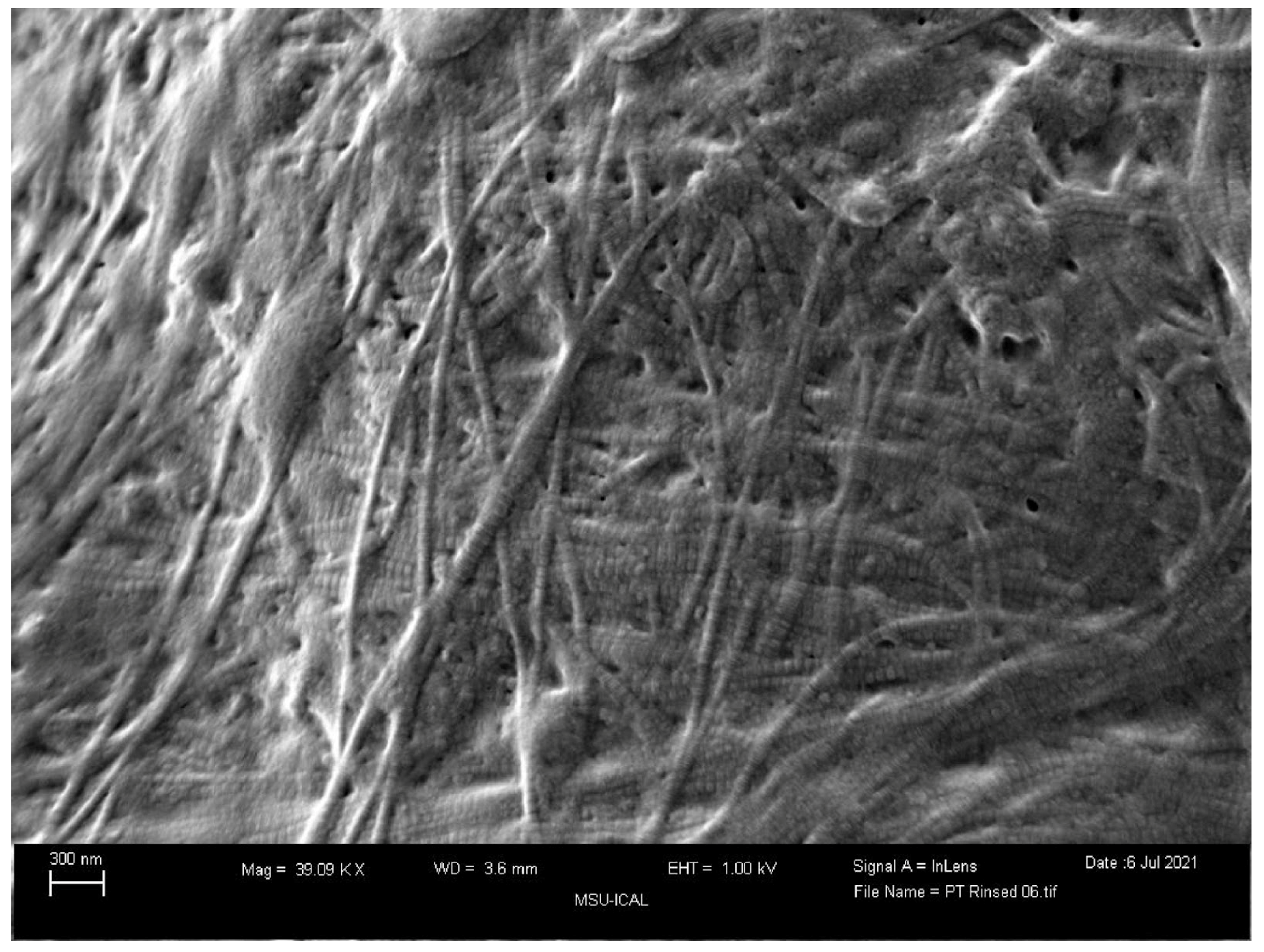
20]. These collagen fibers were split longitudinally in primarily the deep layer of the tendon, with hyaline degeneration evident in the mid layer. The repair process of tendon slows down with age, forming collagen type 3 first and then eventually repairing it with the sturdier collagen type 1. WJ, as pictured below, is primarily comprised of collagen type 1, then 3, then 5 (
Figure A and
Figure B) [
13], all vital to tendon repair; placing this tissue within the defect not only provides the body with the tissues that the body struggles to regenerate but also providing HA and other GAGs to promote this process. Current literature supports the success of using WJ homologously in knees, hips, and other areas to supplement damaged tissue, and that is further confirmed for rotator cuff uses in this study.
Figure A.
A large tear in a 74-year-old man shows thin and disoriented collagen fibers in the torn tendon (Stain, Masson trichrome; original magnification, x 10).
Figure A.
A large tear in a 74-year-old man shows thin and disoriented collagen fibers in the torn tendon (Stain, Masson trichrome; original magnification, x 10).
Figure B.
Scanning electron microscopy image of the Wharton’s jelly tissue product used in this study.
Figure B.
Scanning electron microscopy image of the Wharton’s jelly tissue product used in this study.
However, there were some limitations to the study. The WOMAC questionnaire used by participating clinics was designed for lower extremity use sites but still gives relevant insight into the patient’s pain during daily activities. Future data collection in this retrospective repository will provide additional scales to account for the many homologous use sites discovered over the past three years. This study also covered all application sites within the rotator cuff that could be individually analyzed for more specific efficacy evaluations. Additionally, randomized studies will be beneficial for further confirming the positive results of Wharton’s jelly for rotator cuff defects and standardized application protocols.
5. Conclusions
The application of Wharton’s jelly allografts has been shown to promote decreases in patient-reported NPRS scores, pain, and stiffness in the shoulder and improve function. These improvements were consistent across age groups but are extremely significant for the elderly population, who generally have a slower and less effective recovery rate after conservative treatment and surgical procedures. Given the success shown by NPRS and WOMAC in decreasing pain in the elderly population, more studies are warranted to evaluate the safety and efficacy of Wharton’s Jelly, specifically in patients older than 65. Opportunity exists to apply WJ in other musculoskeletal conditions to ultimately improve quality of life and reduce the healthcare economic burden of multiple conservative treatments or expensive surgical procedures.
Author Contributions
Conceptualization, A.L., C.T, J.S. and T.B.; methodology, A.L., C.T.; software, T.Y.; validation, A.O., J.S., N.L., C.W., O.S., and T.Y.; formal analysis, A.O., J.S., N.L., C.W., O.S.; investigation, A.L., C.T., A.O., J.S..; resources, A.O., N.L., C.W.; data curation, A.L., C.T., A.O., J.S., R.D.; writing—original draft preparation, A.L., C.T., A.., J.S., N.L., C.W., O.S.; writing—review and editing, A.L., C.T., A.., J.S., N.L., C.W., O.S., and T.B.; visualization, A.L., C.T., R.D., T.B.; supervision, J.S., T.B.; project administration, T.B.; funding acquisition, A.L., C.T., T.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Institute of Regenerative and Cellular Medicine (protocol code IRCM-2022-311 and approved on 12 January 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available upon request.
Acknowledgments
The authors would like to thank the PAM Lab at UWF for their support in coordinating the statistical analysis team. They would also like to thank the staff at each clinic who submitted data to the repository for their assistance in data collection and submission.
Conflicts of Interest
John Shou is associated with Baylor College of Medicine and is also the principle investigator of the retrospective repository at Regenative Labs. Crislyn Woods, Naomi Lambert, Orion Schulte, and Tyler Barrett are associated with Regenative Labs. Regenerative Labs was involved in the design of the study, data analysis, and writing. Regenative Labs influenced the decision to publish.
References
- Agha, O.; Diaz, A.; Davies, M.; Kim, H.T.; Liu, X.; Feeley, B.T. Rotator cuff tear degeneration and the role of fibro-adipogenic progenitors. Ann. N. Y. Acad. Sci. 2021, 1490, 13–28. [Google Scholar] [CrossRef]
- Maruvada, S.; Madrazo-Ibarra, A.; Varacallo, M. Anatomy, Rotator Cuff. In StatPearls; StatPearls Publishing, 2022. [Google Scholar]
- Yang, S.; Kim, T.U.; Kim, D.H.; Chang, M.C. Understanding the physical examination of the shoulder: a narrative review. Ann. Palliat. Med. 2021, 10, 2293–2303. [Google Scholar] [CrossRef]
- Herrmann, S.J.; Izadpanah, K.; Südkamp, N.P.; Strohm, P.C. Tears of the Rotator Cuff. Causes - Diagnosis - Treatment. Acta Chir Orthop Traumatol Cech. 2014, 81, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Meng, C.; Jiang, B.; Liu, M.; Kang, F.; Kong, L.; Zhang, T.; Wang, C.; Wang, J.; Han, C.; Ren, Y. Repair of rotator cuff tears in patients aged 75 years and older: Does it make sense? A systematic review. Front. Public Health 2023, 10. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.T.; Fu, S.C.; He, X.; Oh, J.H.; Yamamoto, N.; Hang, S. Risk factors for rotator cuff tendinopathy: A systematic review and meta-analysis. J. Rehabil. Med. 2019, 51, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Dang, A.; Davies, M. Rotator Cuff Disease: Treatment Options and Considerations. Sports Med. Arthrosc. Rev. 2018, 26, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Maman, E.; Harris, C.; White, L.; Tomlinson, G.; Shashank, M.; Boynton, E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Jt. Surg Am. 2009, 91, 1898–906. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, E.; Karaguven, D.; Turhan, E.; Huri, G. Biological augmentation strategies in rotator cuff repair. Med. Glas. Off. Publ. Med. Assoc. Zenica-Doboj Canton Bosnia Herzeg. 2021, 18, 186–191. [Google Scholar] [CrossRef]
- Harris, J.D.; Ravindra, A.; Jones, G.L.; Butler, R.B.; Bishop, J.Y. Setting patients’ expectations for range of motion after arthroscopic rotator cuff repair. Orthopedics 2013, 36, e172–e178. [Google Scholar] [CrossRef] [PubMed]
- Marigi, E.; Kennin, J.; Dholakia, R.; et al. Cost analysis and complication rate comparing open, mini-open, and all arthroscopic rotator cuff repair. JSES Rev. Rep. Tech. 2021, 1, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; El-Amin, S.F.; Levy, H.J.; et al. Umbilical cord-derived Wharton’s jelly for regenerative medicine applications. J Orthop Surg Res 2020, 15, 49. [Google Scholar] [CrossRef] [PubMed]
- Sobolewski, K.; Bańkowski, E.; Chyczewski, L.; Jaworski, S. Collagen and glycosaminoglycans of Wharton’s jelly. Biol. Neonate 1997, 71, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Lai, A.; Shou, J.; Traina, S.A.; Barrett, T. The Durability and Efficacy of Cryopreserved Human Umbilical Cord Tissue Allograft for the Supplementation of Cartilage Defects Associated with the Sacroiliac Joint: A Case Series. Reports 2023, 6, 12. [Google Scholar] [CrossRef]
- Mead, O.G.; Mead, L.P. Intra-Articular Injection of Amniotic Membrane and Umbilical Cord Particulate for the Management of Moderate to Severe Knee Osteoarthritis. Orthop Res Rev. 2020, 12, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Z.; Cao, F.; Gao, C.; Yang, Z.; Guo, Q.; Wang, Y. Decellularized Human Umbilical Cord Wharton Jelly Scaffold Improves Tendon Regeneration in a Rabbit Rotator Cuff Tendon Defect Model. Am. J. Sports Med. 2022, 50, 371–383. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.E.; Dunn, W.R.; Sanders, R.; An, Q.; Baumgarten, K.M.; Bishop, J.Y.; Brophy, R.H.; Carey, J.L.; Holloway, B.G.; Jones, G.L.; et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J. Shoulder Elb. Surg. 2013, 22, 1371–1379. [Google Scholar] [CrossRef] [PubMed]
- Petri, M.; Ettinger, M.; Brand, S.; Stuebig, T.; Krettek, C.; Omar, M. Non-Operative Management of Rotator Cuff Tears. Open Orthop. J. 2016, 10, 349–356. [Google Scholar] [CrossRef]
- Buckley, M.R.; Evans, E.B.; Matuszewski, P.E.; Chen, Y.L.; Satchel, L.N.; Elliott, D.M.; Soslowsky, L.J.; Dodge, G.R. Distributions of types I, II and III collagen by region in the human supraspinatus tendon. Connect Tissue Res. 2013, 54, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Nobuhara, K.; Hamada, T. Pathologic Evidence of Degeneration as a Primary Cause of Rotator Cuff Tear. Clin. Orthop. Relat. Res. 2003, 415, 111–120. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).