Background
Worldwide, countries and their health care systems are facing challenges brought about by the changing demography, increasingly ageing populations, geographical barriers, and rising costs of health care provision [
1].
With increased demands and workforce scarcity, health care systems need to deal with protracted waiting times, generating concern in patients regarding access to care, and leading to a weakening of the doctor–patient relationship and increased dissatisfaction with the quality of health care service provided, and ultimately impacting patient outcomes [
2]. Efficient and effective utilisation of resources invariably affects health and health care experience outcomes.
As health care systems strive to enhance equity in access to care while maintaining quality in the delivery of care and controlling the spiralling costs, the evolving technological environment is leading to the development of new digital tools [
1]. These provide ease of access to care in an affordable manner, leading to enhanced patient autonomy and pushing the take-up of digital alternatives for health care provision [
3]. Policy makers are advocating use of digital consultations to improve access to care while addressing the workforce shortage and the increasing workloads [
4].
The World Health Organisation (WHO) defines “telemedicine” as the utilisation of information and communication technology (ICT) by health care professionals for the purpose of health care delivery where physical distance is a barrier [
5]. The terms “telemedicine” and “telehealth” tend to be used interchangeably. However, the term “telemedicine” tends to restrict the use of digital health technologies to the medical professions while “telehealth” is the use of these technologies by various other health professionals [
5].
As mentioned, through use of ICT, patient outcomes can be improved by overcoming geographical barriers, extending the reach that medical professionals have beyond their physical workplace, enabling telemedicine to offer an alternative way of building capacity [
6]. Telemedicine empowers patients to be actively involved in their medical care, ushering in a paradigm shift in patient involvement and person-centred care [
7].
Digital health care has been adopted in numerous Economic Co-operation and Development (OECD) countries [
6]. For example, Poland started introducing telemedicine in the early 20
th century while in 2013, Korea sought to permit digital consultation use between patients and the medical workforce [
6,
8]. Furthermore, investments in telemedicine are also being spurred by the rapid evolution of ICT, fast internet connectivity and adoption of electronic patient records (EPRs) [
9].
Telemedicine can be stratified according to the complexity of the technology and infrastructure utilised, its temporality in terms of use, and the ease of access for the patient [
10]. Depending on the technology and utilisation, telemedicine can either be “synchronous,” that is, occur in real time as exemplified by video consultations, or “asynchronous,” as in the case of electronic consultations where the data are stored and then addressed later [
2,
11].
The literature shows that telemedicine provides benefits to health systems beyond facilitating access to care and addressing workforce shortages. It allows for a reduction in waiting times through appropriate triaging. It also allows a degree of flexibility to the medical profession by reducing patient numbers in waiting rooms, enabling doctors to focus on complex cases, eventually impacting their work–life balance [
12,
13]. Digital consultations, as adjuncts to traditional medical practice, facilitate the follow-up of patients who suffer from chronic disease and the hospitalised, and are a source of education for both medical professionals and patients through the exchange of evidence-based information [
11,
14,
15].
Telemedicine assumed a particularly significant role during the recent COVID-19 pandemic. It allowed for effective triaging and gate keeping, and continued provision of health care to potentially infected patients while reducing the exposure of the workforce. It maintained access to care despite lockdowns, and limited costs through reduced utilisation of resources such as personal protective equipment [
16]. Furthermore, since the pandemic the barriers to implementation of telemedicine have diminished in importance and the technology is being perceived as central to health care provision, thus presenting a window of opportunity for adoption and implementation [
17].
Digital innovations for health care delivery have been shown to be cost-effective [
18]. Cost-analysis studies have shown that, in terms of the technology used, the training required, and the costs incurred in terms of patient transportation and missed workdays, telemedicine is cheaper than traditional methods of consultation [
19,
20]. Telemedicine has also been shown to reduce the time of completion and the number of consultations in hospital settings, thus reducing overall costs [
21,
22].
Telemedicine is feasible, effective, and safe in providing care [
23]. The technology has been found to be consistent, appropriate, and effective in achieving patient outcomes in different scenarios ranging from acute care to follow-up of patients with chronic illness [
24,
25,
26].
Research has attempted to explore individuals’ inclination to use IT applications [
27]. From an organisational point of view, it is crucial for administrations to make the appropriate decisions on interventions which will lead to enhanced acceptance of IT applications [
28]. Identification of factors that could impact the uptake and utilisation of new IT applications can help in decision making and shape implementation strategies [
28].
Against this background, this paper explored the attitudes of doctors to and their perceptions regarding the adoption, implementation, and utilisation of digital virtual consultations in a tertiary hospital in Malta. Answers to the following research questions were sought: (i) What are the perceptions of doctors working in a secondary- and tertiary-level hospital in Malta, regarding the adoption, implementation and utilisation of video consultations in their work practice?; and (ii) Which are the best predictors of behavioural intention, perceived usefulness and perceived ease of use of video consultations from among the five predictors image, job relevance, perceived ease of use, result demonstrability and subjective norm?
Theoretical framework
The theoretical framework upon which this research was based was adapted from the Technology Acceptance Model (TAM) 3 by [
28], which is grounded on the TAM theory initially proposed by Davis in 1989.
The TAM hypothesises that use of an IT application is initially influenced by the intention to use the application, which in turn is affected by both the individual’s attitude to the application and the perceived usefulness of the application [
29]. The attitude to using the IT application is influenced by the application’s perceived usefulness as well as its perceived ease of use [
30]. Perceived ease of use and perceived usefulness are impacted by external variables that include the user’s demographics, and political and organisational factors, as well as the features of the technology itself [
31].
Davis in 1989 defined “perceived usefulness” as the utilisation of technology by an individual based on whether they think that the technology is advantageous to the performance of the task at hand. [
32] defined “perceived ease of use” as the degree to which the IT application is perceived as easy to use, with minimal effort. Therefore, the easier the technology is to use, the more likely is its uptake. [
32] also postulated that perceived ease of use impacts perceived usefulness. In 2000, Venkatesh and Bala proposed an extension of the original TAM, the TAM 2 [
33], which led to further extensions and, eventually, the development of the TAM 3 model by [
28] from which the research tool for the present study was adapted. For the purpose of this research, the following relationships were studied:
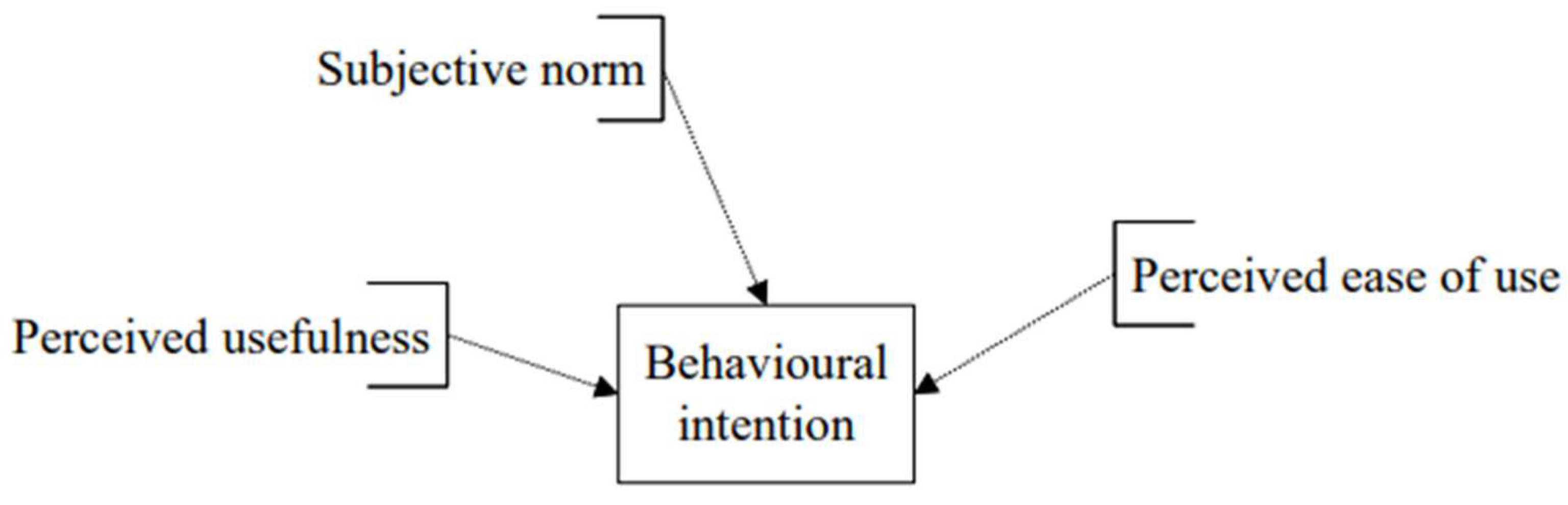
The determinants of behavioural intention (
Figure 1)
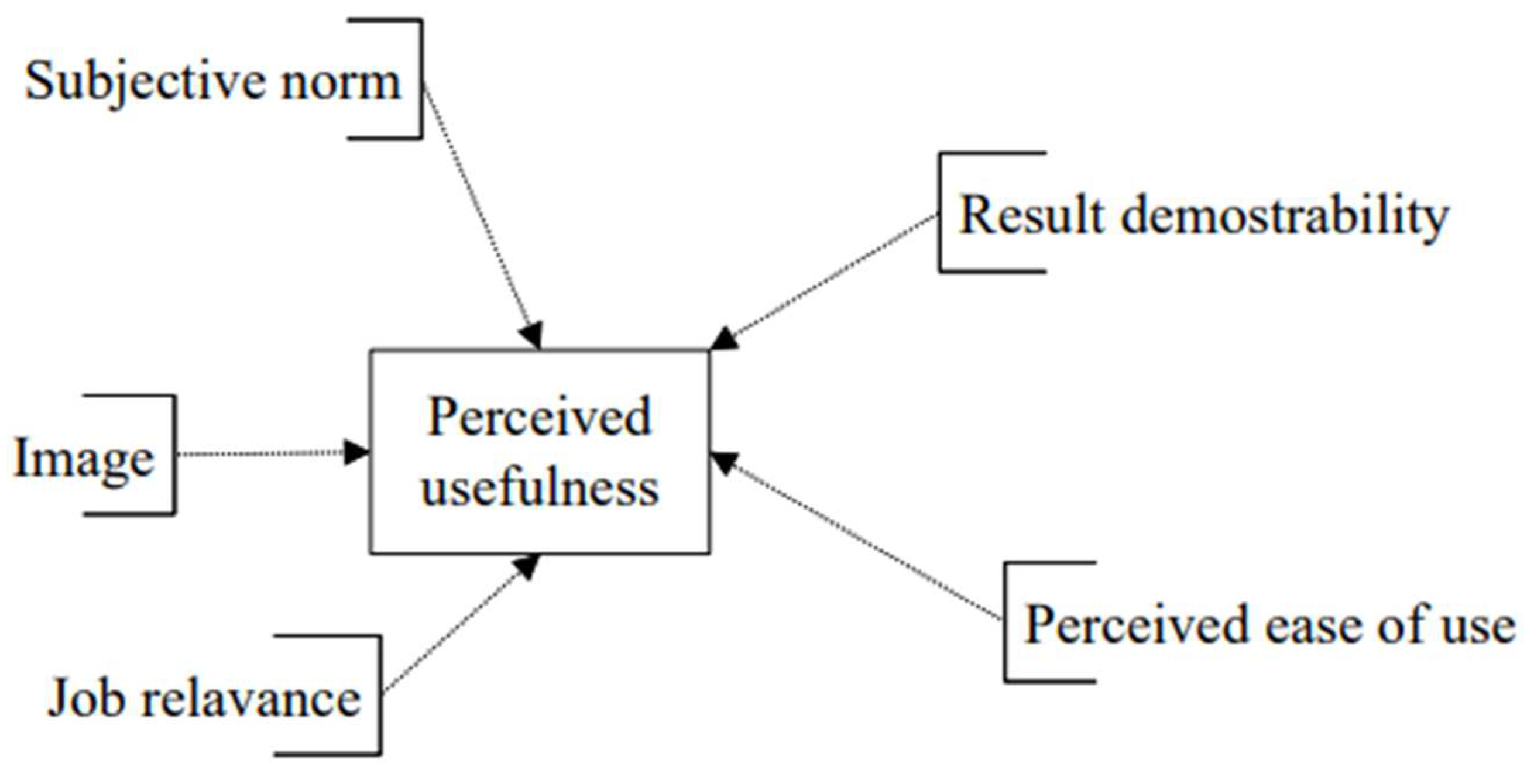
The determinants of perceived usefulness (
Figure 2)
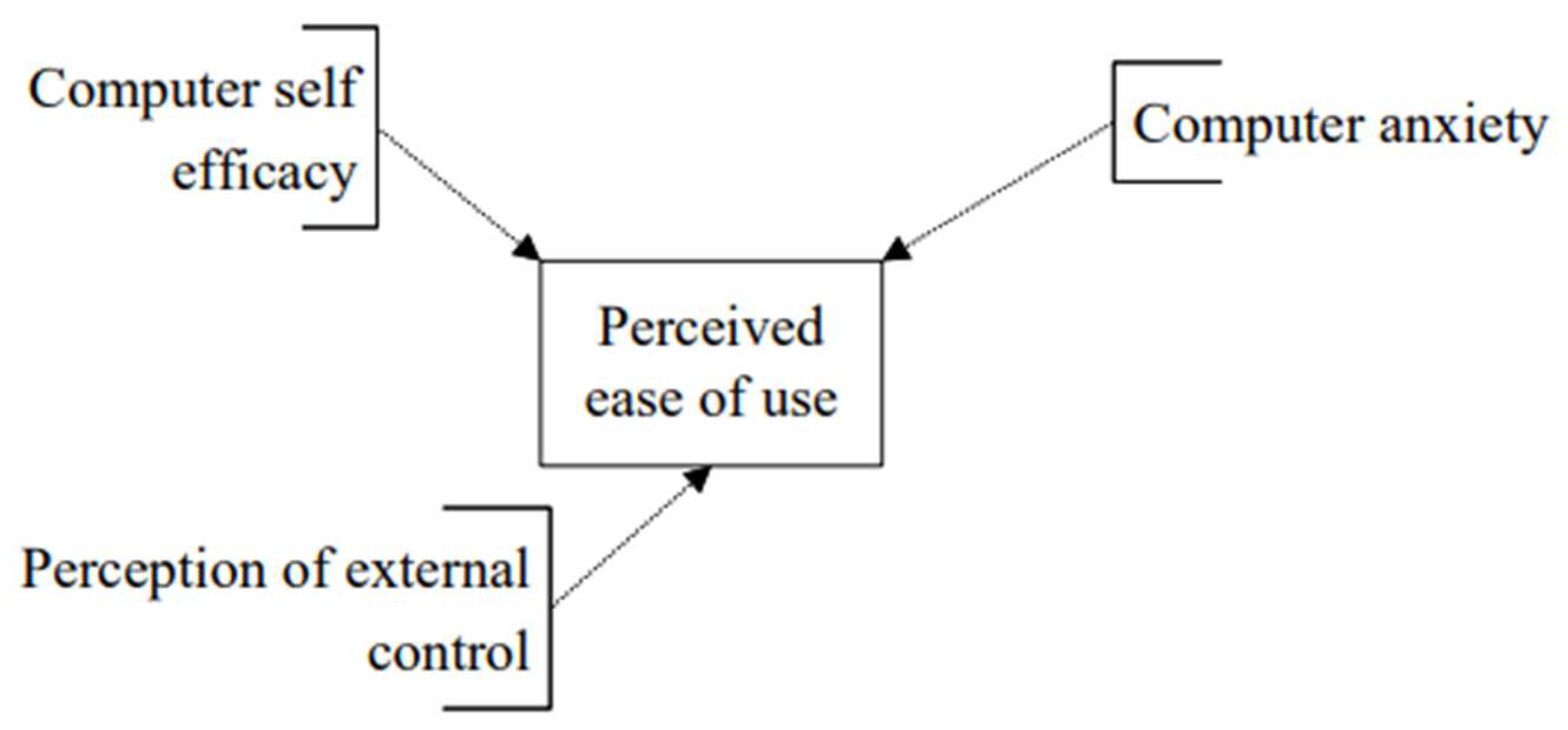
The determinants of perceived ease of use (
Figure 3)
The constructs of perceived enjoyment, object usability and output quality were not included in the adaptation of the research tool as, at the time of the study, video consultations were not yet in place at the analysed hospital. The last aspect of the behavioural intention construct was removed as there was not yet a timeline for implementation of virtual consultations. The construct of computer playfulness was removed as it was deemed not significant for the purposes of this research. The use construct was used to explore any previous experience that the respondents had using the software or platforms that support video consultations.
Methodology
Study design
This research study employed a quantitative design through application of an explanatory sequential mixed method nested within the philosophical worldview of pragmatism [
34,
35].
Participant selection
The sample population included doctors at houseman, basic specialist trainee, higher specialist trainee, registrar, and consultant level, in medical specialties including cardiology and neurophysiology, and in surgical specialties including ophthalmology, otorhinolaryngology and orthopaedics, as well as in obstetrics and gynaecology. Doctors not included in this research were specialties that do not perform out-patient sessions. The sample size amounted to 886 individuals.
Two sampling methods were adopted in selection of the sample population [
36]. Convenience sampling was used to send the email invitation to the sample population [
37]. This method was chosen because of the digital nature of the study [
38].
Data collection
Quantitative data collection was conducted through administration of an online cross-sectional questionnaire. Permission for utilisation of TAM 3 constructs was obtained from the authors and publisher.
The research tool was organised into 13 constructs that explored demographics, current use of video consultations, and perceived usefulness, perceived ease of use, computer self-efficacy, perceptions of external control, computer anxiety, subjective norm, voluntariness of use, image, job relevance, result demonstrability, and behavioural intention. The questionnaire included a comment box at the end, inviting the participants to share opinions and comments. The constructs apart from demographics and current use were addressed through statements which the respondents rated on a 5-point Likert scale ranging from 1 that is “strongly agree” to 5 that is “strongly disagree”.
The questionnaire was constructed on SurveyMonkey.com, an online platform for the creation and distribution of web-based questionnaires, chosen because its interface is comprehensible and customisable, and the data collected can be exported to formats compatible with data analysis software [
39]. The final version of the questionnaire and the method of distribution was reviewed and approved by the Data Protection Office at the analysed hospital. A research intermediary was appointed, who had access to the sampling frame, filtered potential participants by specialty and grade, and emailed the web-based questionnaire to participants. The data collection method was chosen to ensure anonymity.
The questionnaire was accompanied by an approved invitation email and information letter that explained the objectives of the study, the method of data collection, the storage of data, the availability of support if required and consent giving. Respondents were assured that the survey would take less than 15 minutes to complete. The questionnaire was sent to 886 individuals between September and November 2021. Reminders on a fortnightly basis were sent out until no new responses were registered.
Data analysis
The data collected from the questionnaires was transferred from SurveyMonkey.com to Statistical Package for the Social Sciences (SPSS), version 28 (IBM Corporation, Armonk, NY, USA), which was then used to analyse the data. Statistical tests included Fisher’s exact test, Friedman’s test, one-way analysis of variance (ANOVA), and multiple linear regression.
Ethical considerations
The ethical principles of freedom from harm, the right to autonomy, anonymity, confidentiality, and privacy were followed throughout the study.
Ethical approval was obtained from the University Research Ethics Committee (UREC) at the University of Malta (Ref. No. V_150620205465). Permission was also obtained from the Data Protection Office, the Chief Executive Officer, and the Chief Clinical Chairperson at the included hospital. The necessary permissions were also obtained from the relevant heads of departments of the hospital.
Data collection was anonymous and the digital platform SurveyMonkey.com was set up so as not to keep the internet service provider (ISP) addresses of the participants. Data were collected and handled only by the researchers and stored on a secure, password-protected device.
Results
A total of 886 email invitations were sent to potential participants between September and November 2021. Reminders were sent every second week until no further responses were elicited. A total of 133 responses were obtained, giving a response rate of 15%. Altogether 67% of the respondents fully completed the questionnaire.
Seventy-one respondents were female and 62 were male, with the majority of those who responded being junior doctors at foundation level. Respondents’ demographics are presented in
Table 1.
Table 2 gives the respondents’ experience with virtual consultations.
The Friedman test was used to compare the mean rating scores for the items in each construct. The mean scores indicate respondents’ agreement that video consultations can be used in conjunction with face-to-face consultations and are a means of communication between professionals and a way to enhance quality of care. Respondents perceived video consultations as easy to use and as relevant to their medical practice and stated that they would be able to perform a digital consultation in an adequate, supportive environment.
One-way ANOVA was used to compare mean construct scores between several groups of respondents clustered by gender, age, and level of specialisation. With a p-value of 0.028, female participants scored significantly higher on job relevance and there was a statistically significant difference (p=0.024) between the age groups regarding perceived usefulness and subjective norm. Similarly, there was a statistically significant difference (p=0.010) in the mean scores between levels of specialisation for computer self-efficacy.
Multiple regression analysis was applied to evaluate the relationships between perceived usefulness, perceived ease of use, and behavioural intention, and their determinants.
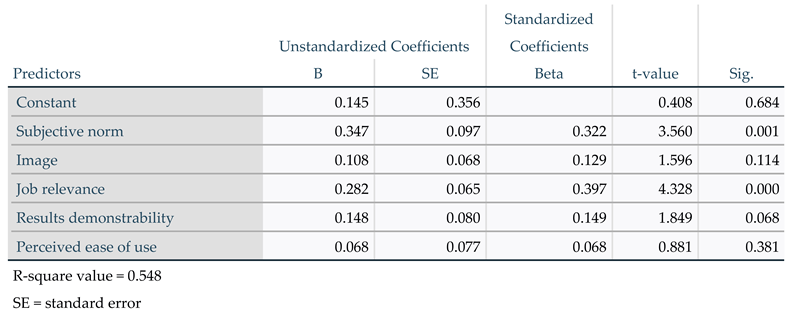
The model relating perceived usefulness to the five predictors subjective norm, image, job relevance, result demonstrability, and perceived ease of use explained 54.8% of the total variability of perceived usefulness. Job relevance was the strongest predictor of perceived usefulness because it has the lowest p-value and the highest t-value (see
Table 3).
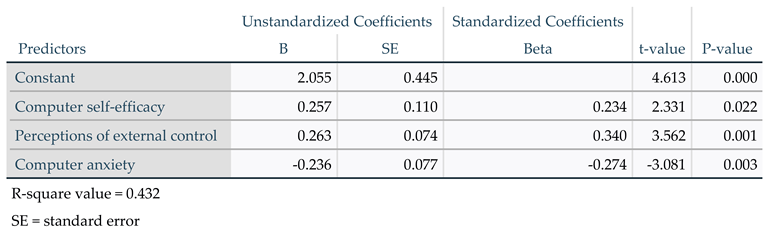
The model relating perceived ease of use to the three predictors computer self-efficacy, perceptions of external control, and computer anxiety explained 43.2% of the total variability of perceived ease of use. Perceptions of external control was the best predictor of perceived ease of use as it had the lowest p-value (
Table 4).
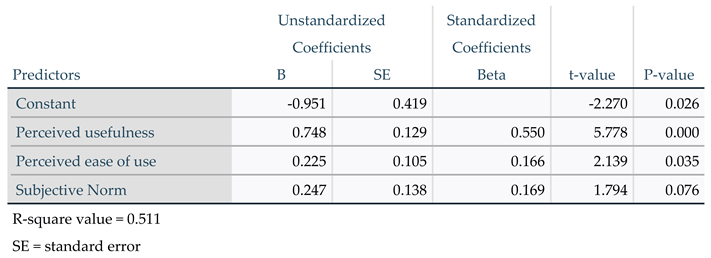
The model relating behavioural intention to the three predictors perceived usefulness, perceived ease of use and subjective norm explained 51.1% of the total variability of behavioural intention. Perceived usefulness was the best predictor of behavioural intention because it has the lowest p-value (
Table 5).
Discussion
Summary of results
This study sought to elicit the perceptions of local doctors working in a secondary and tertiary care hospital, of the role of virtual consultations in medical practice, and the barriers and facilitators to implementation. The study further assessed the readiness of doctors to adopt the practice of and utilise the technology for virtual consultations.
Digital consultations have a role in supporting the balance between health care resource utilisation, access, and provision of care [
40,
41]. Some of the respondents in this study thought that video consultations would be useful to them in their jobs. The mean score of 2.6 indicated agreement on the relevance of video consultations in the local medical practice. Female respondents tended to perceive video consultations as more relevant to their job than their male counterparts (p = 0.28). However, the respondents did not feel that video consultations were appropriate as first point of contact with patients, and there was strong disagreement regarding the question whether video consultations are superior to traditional face-to-face consultations (mean score 3.7). With mean scores of less than 3, respondents did perceive video consultations as adjuncts to face-to-face consultations with a particular role in the follow-up of patients. The implementation of the new technology will invariably lead to changes in work practices. Doctors will need to adapt to change while understanding what will be required of them to initiate and complete a digital consultation [
42].
There was agreement on the construct of perceived ease of use. With a mean score of 2.32, respondents perceived video consultation software as easy to use, and with mean scores of less than 3 there was agreement that operating the software would be easy and understandable and would not require much mental effort. The respondents did not feel that working with technological devices such as computers made them feel anxious or uneasy. The notion of virtual consultations might still be new in the health care system; however, these technologies were already being used informally to initiate communications and some of the respondents stated that they already used video consultations in their practice. The respondents expressed neutrality (mean score of 3.04) regarding the availability of resources required to initiate video consultations; however, there was agreement as to the ease of use of the technology if the resources and knowledge are present.
An improvement in workload, in terms of increased productivity and effectiveness, as discussed by [
43], was not perceived by the respondents in this study. With mean scores of around 3, the respondents were neutral to the perception that video consultations would improve doctors’ performance, productivity, and effectiveness, as well perceptions regarding their impact on doctors’ working hours and work–life balance.
There is the need for health care organisations to guarantee the availability and accessibility of the infrastructure coupled with proper project management and coordination to enhance sustainability of initiatives such as the one discussed here [
44,
45]). With a mean score of 2.46, respondents perceived it to be easy to operate the software if the resources, opportunities, and knowledge are available. They perceived the organisation they worked for as supportive in the utilisation of these digital alternatives, allowing for voluntary use of the technology.
The mean scores obtained on behavioural intention indicate that if the respondents had access to the software, they would, based on their predictions, initiate video consultations. The respondents thought that the utilisation of such technologies would be on a voluntary basis, and they would not find it difficult to communicate the advantages and disadvantages of such alternatives to colleagues.
Lack of acceptance by users was identified by [
43,
46] as a major barrier to adoption and implementation of innovative technologies. As postulated by Davis, intention of use is influenced by perceived usefulness, perceived ease of use, and the subjective norm [
32]. These constructs are in turn influenced by their determinants.
Multiple regression analysis performed for the model evaluating the determinants of perceived usefulness found an association between perceived usefulness and its five predictors. The analysis indicates that the way in which the respondents perceived video consultations as relevant to their practice, followed by the perception that management would be supportive in the utilisation of the technologies, had more impact on the perceived usefulness of these consultations than the ability to communicate the pros and cons of utilisation, the influence of utilisation on the individual’s status within the organisation and the ease of use of the technology.
Regression analysis showed an association between perceived ease of use and three predictors. The extent to which the respondents perceived the necessary resources as being present was the strongest predictor, followed by the extent to which the respondents felt comfortable working with technical infrastructure and the extent to which they believed they were able to initiate video consultations with or without assistance.
Behavioural intention was likewise associated with its three predictors. Of these, perceived usefulness was the strongest predictor, followed by perceived ease of use and, finally, subjective norm.
The findings of this study therefore indicate that targeting these predictors will strengthen the intention to use the technology in the local context. Identifying the factors or determinants that impact intent to use is crucial for the development of implementation strategies [
47].
Factors that facilitate the uptake of modern technologies need to be identified. Also, there should be an understanding of those factors which are perceived as critical by the workforce, and which should therefore be addressed in the implementation process [
43,
46]. There is a need for proper evaluation of the technologies to be adopted, coupled with a feasibility analysis to understand the need and the demand to ensure project sustainability [
48,
49].
Implications
Although the concept of virtual consultations is relatively new to doctors working in the main hospital on the island of Malta, it was acknowledged that they have a role in the current medical practice. There is a need to understand the role of virtual consultations in the follow-up of patients once initial rapport has been established between the doctor and the patient during a traditional consultation, which is still seen as the gold standard for the patient–doctor interaction.
Improved access and enhanced communication between specialists and patients result in enhanced quality of care. Virtual consultations are channels of communication fostering the sharing of medical knowledge and information, leading to a higher level of health care provision in and outside the practice, and therefore to better patient management.
Virtual consultations are of particular importance in the small island state of Malta. The literature highlights the role of digital consultations in overcoming distance barriers; however, it does not address the challenges faced by small countries that have limited resources and are isolated by geography. The small size of Malta limits exposure and may lead to loss of skill over time, while the island’s isolation leads to seeking specialised patient care overseas. Virtual consultations can help reduce these barriers by lessening the need for patients to go abroad while supporting the delivery of specialised care.
In analogy to findings in the literature, this study has identified the need for investment in appropriate technological infrastructure that is simple to use, easily accessible and robust so as to support virtual consultations. The new technologies should fit with the way local doctors practise. They should also be easily integrated into existing digital infrastructure, with the appropriate level of technical support made available.
Apart from making the initial investment, the health care organisation was seen as having an essential role in the sustainability of the initiative. There is a need for investment in technical support and training, which would heighten the intention of use of the new technologies and maintain their utilisation as the workforce becomes familiar with the new practices.
The literature has shown that the uptake of virtual consultations is influenced by the understanding that users have of its benefits. As postulated in the TAM (Davis, 1989), individuals’ intention to use technology is influenced by the usefulness and relevance of the technology, as well as by how easy and effortless the technology is to use. This research study has shown that the participants’ perception of the technology’s usefulness and ease of use did have an association with their intention of use, and that, with the appropriate resources and access to the technology, the respondents would make use of these alternatives to traditional methods.
Significance for Public Health
As population demographics change, individuals become more knowledgeable, increasingly demanding, and progressively dependent on technology. As individuals seek innovative approaches to treatment, health care systems seek innovative ways of providing care. In this respect, virtual consultations have a significant impact on public health, offering numerous advantages such as accessibility and continuity of care, equity, more efficient resource utilisation and patient management, improved quality of care. Furthermore, in line with the Sustainable Development Goals (SDGs) of the United Nations (UN), digital health has been widely recognized as a means of improving the sustainability of the healthcare sector. Specifically, the use of ICT and digital technology in healthcare organizations can help achieve universal health coverage (SDG 3).
Strengths and limitations
This study has both strengths and limitations. The sampling process may have introduced a bias in that the study population may not be representative of all doctors working in this environment. The online questionnaires may have excluded potential respondents who were not familiar with or had only limited access to the technology. The digital nature of the study, however, has allowed for easier access to the population of interest in the context of the COVID pandemic.
The researchers sought to carry out a pilot study and tests for internal consistency to enhance the quality of the tool; however, the sampling frame was relatively inaccurate in terms of specificity on doctors’ specialties. As such, the data collected concerning the respondents’ specialty could not be used to make statistical inferences.
The researchers made every effort to be rigorous throughout the stages of the study and followed the set ethical procedures in terms of data collection, storage, analysis and reporting so as to protect the identity of the respondents.
To the authors’ knowledge, this is one the first studies of its kind to explore perceptions of doctors working in a secondary and tertiary care hospital in an island setting.
Conclusions
This study aimed to explore the attitudes of doctors to and their perceptions of the adoption, implementation, and utilisation of digital virtual consultations in a tertiary hospital in Malta. The findings reveal that respondents viewed digital virtual consultations as supplements to in-person consultations, reducing obstacles related to distance and time. With the necessary infrastructure and technology in place, doctors would be willing to use these options. To determine the technological fit and the influence of utilisation of the technology on the workforce, feasibility and cost-effectiveness studies would be advised, along with a stakeholder analysis to include all the actors involved in such a strategy.
The study presents preliminary results of ongoing research, the next phase of which will be directed towards expanding the sample of respondents and implementing a mixed qualitative–quantitative methodology approach.