Submitted:
17 January 2024
Posted:
18 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Case Report
3. Discussion
4. Conclusions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Vitolo U, Seymour JF, Martelli M, Illerhaus G, Illidge T, Zucca E, et al. Extranodal diffuse large B-cell lymphoma (DLBCL) and primary mediastinal B-cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v91-v102. [CrossRef]
- Ferri GM, Specchia G, Mazza P, Ingravallo G, Intranuovo G, Guastadisegno CM, et al. Risk of lymphoma subtypes by occupational exposure in Southern Italy. J Occup Med Toxicol. doi: 2017;1231. [CrossRef]
- Morton LM, Slager SL, Cerhan JR, Wang SS, Vajdic CM, Skibola CF, et al. Etiologic heterogeneity among non-Hodgkin lymphoma subtypes: the InterLymph Non-Hodgkin Lymphoma Subtypes Project.J Natl Cancer Inst Monogr. 2014;2014(48):130-144. [CrossRef]
- Non-Hodgkin’s lymphoma as an unexpected diagnosis in a shoulder arthroplasty. J Arthroplasty. 1999;14(1):108-111. [CrossRef]
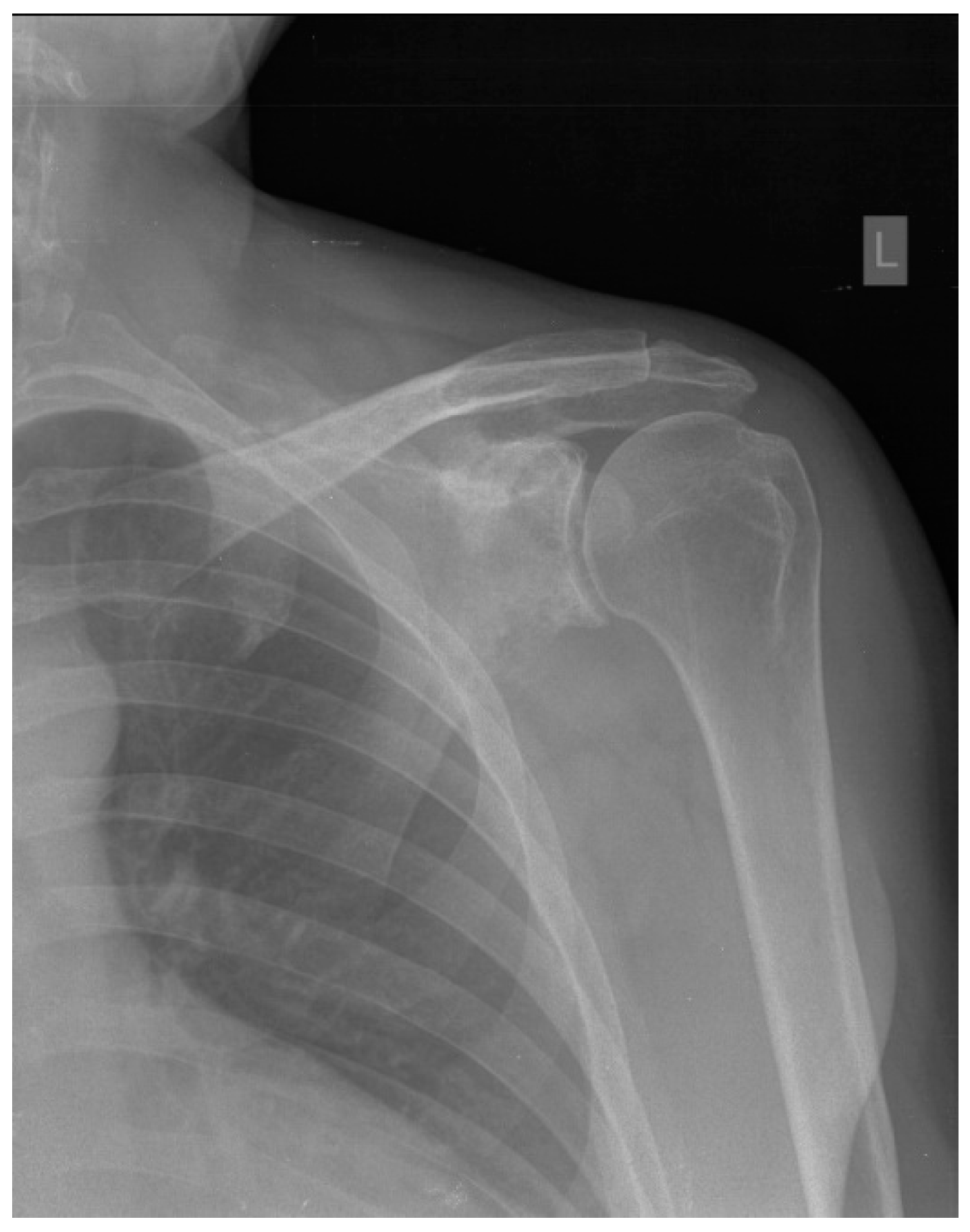
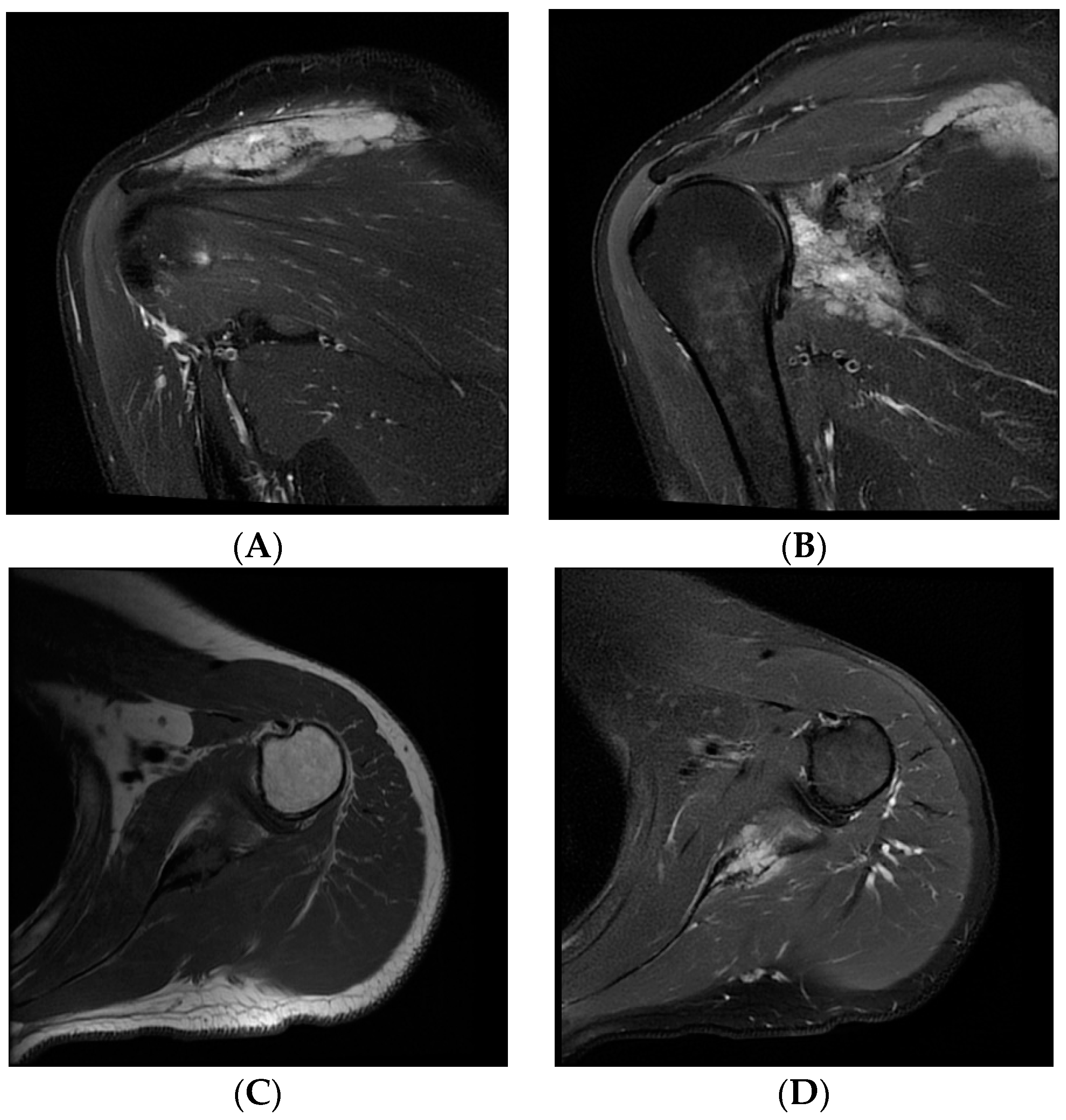
- Chauhan NR, Chick JF, Khurana B. Annihilation of the acromion: a rare case of primary scapular lymphoma. J Emerg Med. 2013;44(6):e389-390. [CrossRef]
- Carroll G, Breidahl W, Robbins P. Musculoskeletal lymphoma: MRI of bone or soft tissue presentations. J Med Imaging Radiat Oncol. 2013;57(6):663–73. [CrossRef]
- Boulytcheva IV, Sciotto C, Soloviev Y., Kushlinskii NE. Diffuse large B-cell lymphoma presented as bone lesions. A study of 21 cases and review of the literature. Кoллектив автoрoв. 2013;44–7.
- Das DK, Pathan SK, Al-Waheeb SKM, Ali AE, Joneja M, Al-Kanderi MG, et al. Chest wall lymphomas: fine needle aspiration cytodiagnosis and review of the literature. Cytopathology. 2017;28(5):364–70. [CrossRef]
- Yousef MHAH, Audat Z, Al-Shorafat DM, Al-Khatib S, Daoud AK. Primary za.
- of bone: a single-center experience. J Blood Med. 2022;13:143–9. [CrossRef]
- Nikonova A, Guirguis HR, Buckstein R, Cheung MC. Predictors of delay in diagnosis and treatment in diffuse large B-cell lymphoma and impact on survival. Br J Haematol. 2015;168(4):492-500. [CrossRef]
- Messina C, Christie D, Zucca E, Gospodarowicz M, Ferreri AJ. Primary and secondary bone lymphomas. Cancer Treat Rev. 2015;41(3):235-246. [CrossRef]
- Zelenetz AD, Gordon LI, Chang JE, Christian B, Abramson JS, Advani RH, et al. NCCN guidelines(R) insights: B-cell lymphomas, version 5.2021. J Natl Compr Canc Netw. 2021;19(11):1218-1230. [CrossRef]
- Subramanian S, Viswanathan VK. Lytic bone lesions. StatPearls (electronic book section). Treasure Island (FL): StatPearls Publishing; 2022.
- Häussler MD, Fenstermacher MJ, Johnston DA, Harle TS. MRI of primary lymphoma of bone: cortical disorder as a criterion for differential diagnosis. J Magn Reson Imaging. 1999;9(1):93-100. [CrossRef]
- Mengiardi B, Honegger H, Hodler J, Exner UG, Csherhati MD, Brühlmann W. Primary lymphoma of bone: MRI and CT characteristics during and after successful treatment. AJR Am J Roentgenol. 2005;184(1):185-192. [CrossRef]
- Dabaja BS, Vanderplas AM, Crosby-Thompson AL, Abel GA, Czuczman MS, Friedberg JW, et al. Radiation for diffuse large B-cell lymphoma in the rituximab era: analysis of the National Comprehensive Cancer Network lymphoma outcomes project. Cancer. 2015;121(7):1032-1039. [CrossRef]
- Huang H, Li X, Zhu J, Ye S, Zhang H, Wang W, et al. Entecavir vs lamivudine for prevention of hepatitis B virus reactivation among patients with untreated diffuse large B-cell lymphoma receiving R-CHOP chemotherapy: a randomized clinical trial. JAMA. 2014;312(23):2521-2530. [CrossRef]
- Dong HJ, Ni LN, Sheng GF, Song HL, Xu JZ, Ling Y. Risk of hepatitis B virus (HBV) reactivation in non-Hodgkin lymphoma patients receiving rituximab-chemotherapy: a meta-analysis. J Clin Virol. 2013;57(3):209-214. [CrossRef]
- Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50(3):661-662. [CrossRef]
- Gutfreund KS, Williams M, George R, Bain VG, Ma MM, Yoshida EM, et al. Genotypic succession of mutations of the hepatitis B virus polymerase associated with lamivudine resistance. J Hepatol. 2000;33(3):469-475. [CrossRef]
- Santini D, Vincenzi B, Dicuonzo G, Avvisati G, Massacesi C, Battistoni F, et al. Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res. 2003;9(8):2893-2897.
- Winter MC, Holen I, Coleman RE. Exploring the anti-tumour activity of bisphosphonates in early breast cancer. Cancer Treat Rev. 2008;34(5):453-475. [CrossRef]
- Inoue N, Nishimura N, Takahashi A, Kusano Y, Yamauchi H, Ueda K, et al. Negative impact of zoledronic acid in R-CHOP treated DLBCL with bone metastasis. Hematol Oncol. 2017;35(S2):340–1. [CrossRef]
- Valachis A, Polyzos NP, Coleman RE, Gnant M, Eidtmann H, Brufsky AM, et al. Adjuvant therapy with zoledronic acid in patients with breast cancer:asystematic review and meta-analysis.Oncologist.2013;18(4):353-361. [CrossRef]
- Himelstein AL, Foster JC, Khatcheressian JL, Roberts JD, Seisler DK, Novotny PJ, et al. Effect of longer-interval vs standard dosing of zoledronic acid on skeletal events in patients with bone metastases: a randomized clinical trial. JAMA. 2017;317(1):48-58. [CrossRef]
- Iversen PO, Negaard H, Østenstad B, Sandset PM, Kolset SO. Evidence for long-term hypercoagulopathy, but normalization of markers of extracellular matrix turnover, in patients with non-Hodgkin lymphoma. Vol. 56, Leukemia and Lymphoma. 2015. p. 2479–81. [CrossRef]
- Negaard HFS, Iversen PO, Østenstad B, Iversen N, Holme PA, Sandset PM. Hypercoagulability in patients with haematological neoplasia: No apparent initiation by tissue factor. Thromb Haemost. 2008;99(6):1040–8. [CrossRef]
| 1st author and year of publication | Sex/age | Presentation | Time between symptoms onset and diagnosis / Time between first hospital visit and diagnosis | Involvement of other sites | Treatment | Outcome |
| Chauhan [6], 2013 | F/84y | Pain | Two months/ days-weeks |
Surrounding soft tissue | R-CHOP chemotherapy | Remission |
| Carroll [7], 2013 |
M/29y | Lump | Nd/Nd | Nd | Nd | Nd |
| Boulytcheva [8], 2013 | F/73y | Nd | Nd | Nd | Radiotherapy | Death |
| Das [9], 2017 | M/73y | Nd | Nd | Nd | Nd | Nd |
| Ayesh Haj Yousef [10], 2022 | F/46y | Mass | Two months/ Nd | Nd | R-CHOP chemotherapy + radiotherapy |
Remission |
| Our patient | M/45y | Paresthesia, tingling, numbness and edema of the little and ring finger | Two years/ two years |
Surrounding soft tissue | R-CHOP chemotherapy + radiotherapy | Remission |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





