INTRODUCTION:
Borreliosis, also known as Lyme disease, is an infection caused by spirochete Borrelia burgdorferi. It is a vector-borne disease transmitted by infected Ixodes scapularis tick bite [
1]. The disease is endemic in the United States, Europe, and some parts of Asia like Korea, Nepal, and China. Patients typically present with fever, headache, fatigue, and a characteristic annular skin rash called erythema migrans. Diagnosis of Lyme disease is based on clinical features and the endemicity of the disease [
2]. Laboratory tests like Antibody-based tests like ELISA, IFA, etc. can be done. Treatment includes the removal of ticks using forceps and antibiotics (drugs of choice being doxycycline and amoxicillin) [
3]. Untreated Lyme disease can result in many complications like peripheral neuropathy, encephalopathy, carditis, heart blocks and arthritis.
CASE PRESENTATION:
A 60-year-old Indian male patient was admitted to SVP hospital with the complaint of left-sided facial weakness and asymmetry and increased muscle tone for 15 days. The patient was asymptomatic before 8 months, following which he developed left lower limb weakness and paresthesia in both lower limbs for 1 month, behavioural changes for 15 days and diplopia for 5 days. The left lower limb weakness was gradual in onset, starting from the calf and extending above and below and it was associated with difficulty in walking and standing, loss of sensations and tingling in both lower limbs. He also had behavioural changes in the form of crying spells and aggression over trivial matters. He also complained of double vision for 5 days which was associated with blurring of vision and occasional blackout sensation. During this period, the patient consulted many doctors and MRI brain, NCV and EMG studies were advised. MRI showed signs of age-related atrophy, and NCV and EMG studies were suggestive of bilateral lumbosacral plexopathy. He was given steroids in tapering doses which led to an 80% improvement in his condition. The patient was in remission for 5 months after which his condition deteriorated and so he was admitted to our institute. For the last 10 days, the patient has also experienced urinary complaints in the form of increased frequency, urinary hesitancy and feeling of incomplete evacuation.
Negative history of fever, rash, joint pain, swallowing problems, speech, and hearing difficulty.
PAST HISTORY:
The patient has a history of Hypertension and Asthma for 20 years and he is on medication for the same.
PHYSICAL EXAMINATION:
On examination, the patient's general condition was good. He was conscious and well-oriented to time, place and person. A nervous system examination revealed that the Glass Glow Coma Scale (GCS) score was E4 M6 V5. His pupils were bilaterally equal in size and diameter and reactive to light. Extraocular Movements (EOM) were normal. Muscle tone is increased in all four limbs (spastic) and strength of the limbs was level 3. Deep Tendon reflexes were present in both the upper limbs with +3/+3 and absent in both the lower limbs. The patient had mild left-sided facial weakness, no stiff neck, and no other biological pathological signs.
LAB EXAMINATION:
Table 1.
Blood examination.
Table 1.
Blood examination.
| Test |
Observed value |
Reference Range |
| Haemoglobin |
9.5 g/dl |
(12-18) |
| WBC |
6.44 kU/L |
(5.2-12.4) |
| RBC |
3.45*106/ul |
(4.5-5.5) |
| Haematocrit |
30.7% |
(40-50) |
| Platelet counts |
370 kU/L |
(130-400) |
| Neutrophile |
85% |
(49-74) |
| Lymphocyte |
07% |
(26-46) |
| Monocyte |
06% |
(2-12) |
| Eosinophil |
02% |
(0-5) |
| Basophil |
00% |
(0-2) |
Table 2.
Renal Function Test.
Table 2.
Renal Function Test.
| Test |
Observed value |
Reference Range |
| Blood Urea |
22.0 mg/dl |
(15-45) |
| Creatinine serum |
0.55 mg/dl |
(0.5-1.1) |
| Sodium serum |
140 mmol/L |
(132-146) |
| Potassium serum |
3.14 mmol/L |
(3.5-5.5) |
| Chlorine serum |
109 mmol/L |
(99-109) |
Table 3.
CSF examination.
Table 3.
CSF examination.
| Test |
Observed value |
| Quantity |
0.5 ml |
| Color |
Colorless |
| Appearance |
Clear |
| Blood |
Absent |
| Cobweb |
Absent |
| Total count |
00 |
| Polymorphs |
- |
| Lymphocytes |
- |
| RBC |
Occasional |
| CSF sugar |
37 mg/dl |
| CSF protein |
85 mg/dl |
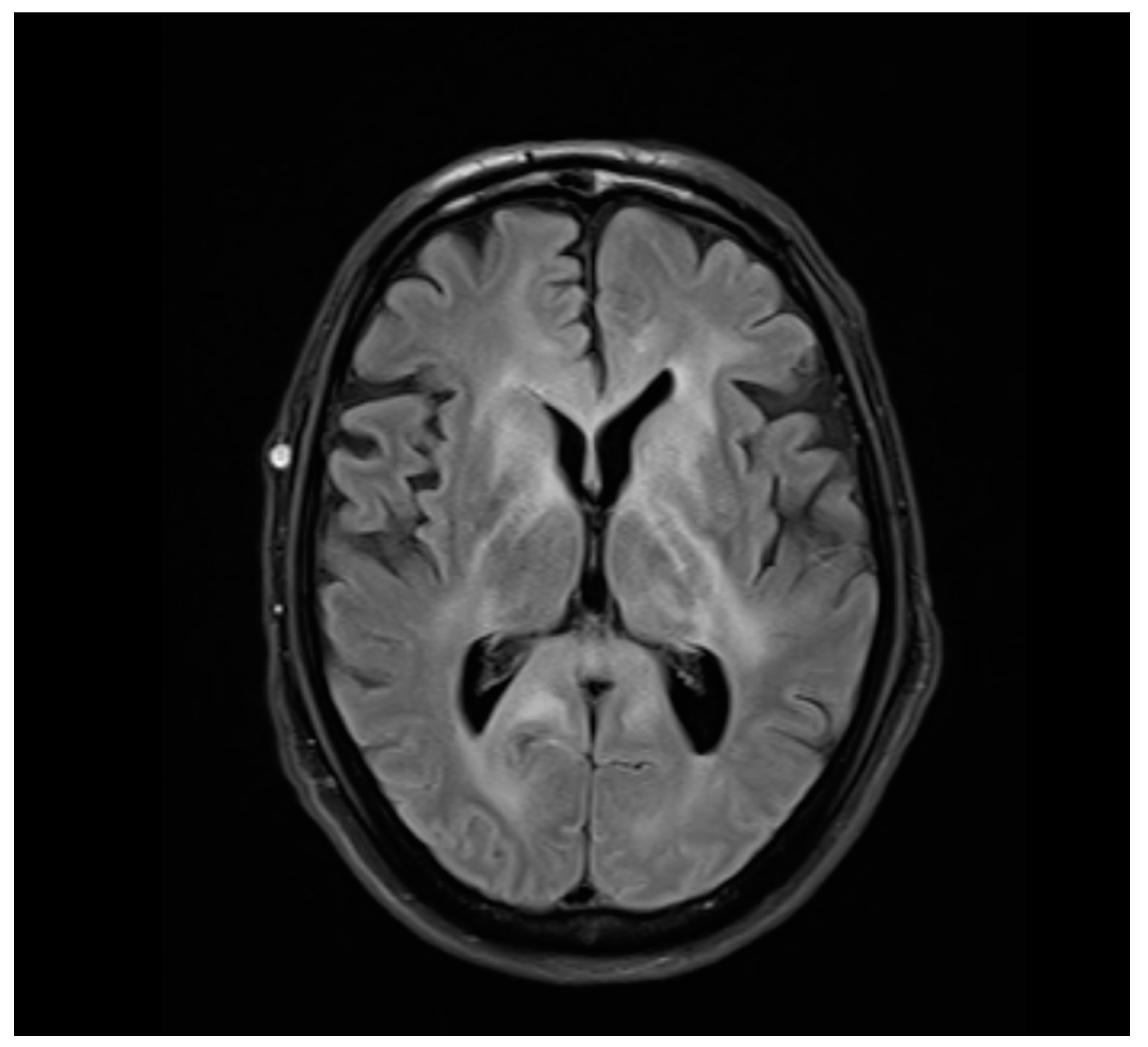
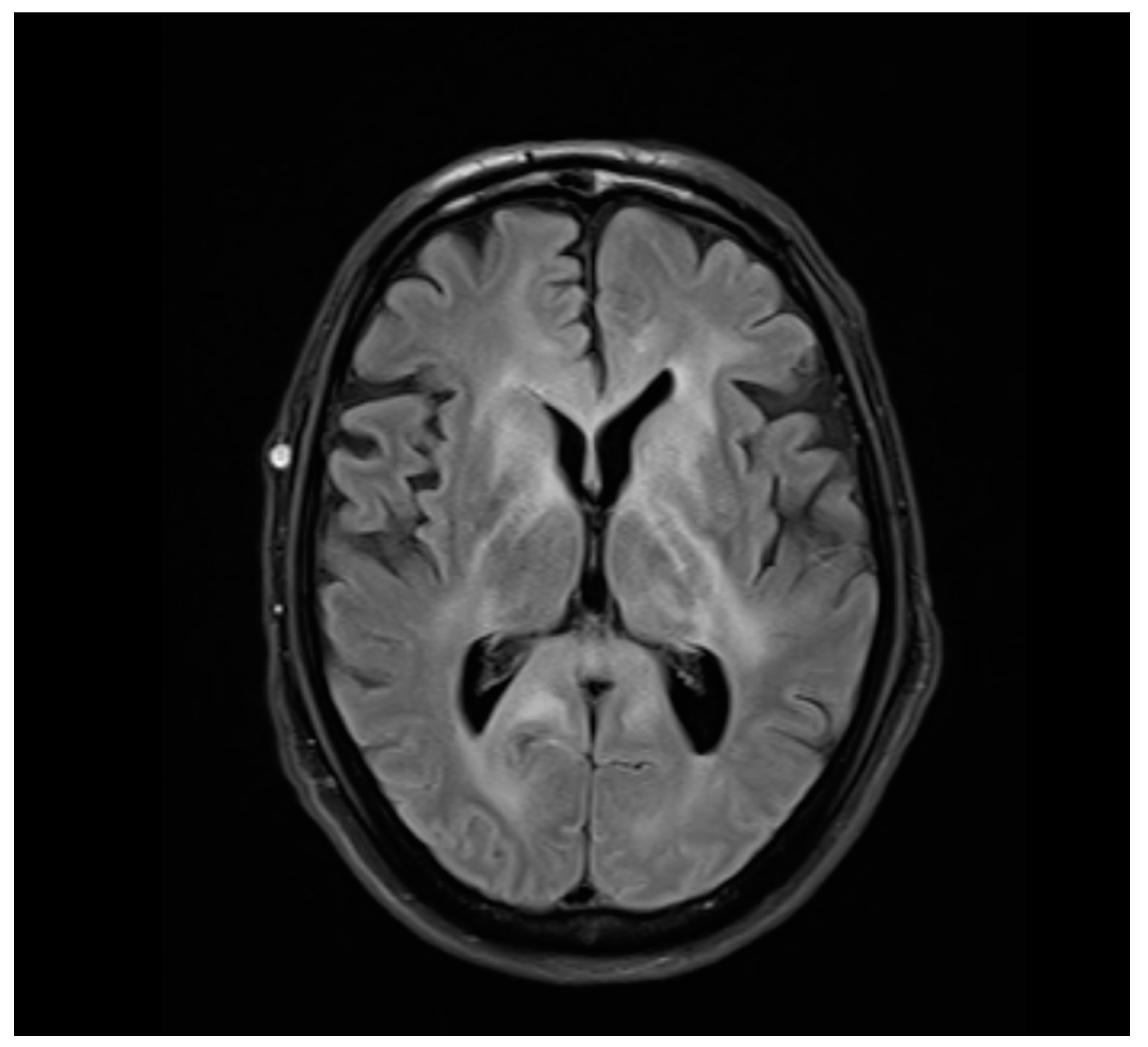
RADIOLOGICAL IMAGING (MRI Brain Plain):
Observation:
Abnormal asymmetrical T2WI/FLAIR hyperintensity noted in bilateral fronto-parieto-temporal subcortical and periventricular white matter, centrum semiovale, corona radiata, corpus callosum, ganglio-capsular region, thalami, mid-brain, pons and superior cerebellar peduncle. There is no evidence of any diffusion restriction or GRE blooming.
Dilatation of the ventricular system, cerebral sulci, basal cisterns and cerebellar folia, suggestive of cerebral and cerebellar atrophy.
A few discrete T2WI and FLAIR hyperintensities are noted in bilateral periventricular deep white matter in the frontoparietal region, suggesting chronic ischemic changes.
TREATMENT:
The patient was started on plasma exchange and injection Rituximab along with Prednisone 20 mg once a day for 8 days, syrup potassium chloride 2 tbsp thrice a day (till potassium levels normalize). He was also given injection ceftriaxone and tablet doxycycline 100 mg twice a day for 28 days and injection Linezolid 600 mg twice a day for 14 days. Supportive therapy like Pantoprazole 40mg, Folic acid and Vitamin B complex, Vitamin D3 and Calcium tablets once a day for 28 days were also given. The patient was discharged once her condition was stabilised and symptoms improved.
FOLLOW UP CASE:
The patient was followed up for around 6 months and there has been no recurrence or aggravation.
DIAGNOSIS:
The patient was given appropriate antibiotic treatment for 28 days and there was significant improvement in his condition. Based on the clinical presentation, imaging findings, and response to antibiotic therapy, the patient was diagnosed with Lyme disease.
DISCUSSION AND LITERATURE:
Borreliosis is a multisystem tick-borne bacterial disease caused by Borrelia burgdorferi, a corkscrew-shaped spirochete. The bite of the Ixodes tick plays an important role in disease transmission. Since its diagnosis 50 years ago, its cases have continued to increase till date and its distribution has widened worldwide [
4].
B. burgdorferi enters the body at the site of the tick bite. After an incubation period of about 30 days, it spreads via lymphatics and blood throughout the body resulting in disease manifestation [
5]. The disease has 3 stages: early localized, early disseminated, and late stages [
6]. The early localized stage lasts for days to months. It is characterized by non-specific symptoms like fatigue, headache, regional lymphadenopathy, myalgias, and arthralgias along with classic spreading, annular, erythematous rash with central clearing called erythema migrans (bull’s eye appearance). The next stage is early disseminated which lasts for weeks to months and consists of disease spread throughout the body and thus has the following clinical manifestations: multiple erythema migrans, unilateral/bilateral cranial nerve palsies, meningitis, carditis, migratory arthralgias, etc. If the disease is left untreated, most cases recover without sequelae but some may progress to the late stage of Lyme disease. The clinical features of this stage depend on the organ system being affected. The most common systems that are affected include the central nervous system (causing encephalitis, peripheral neuropathy, etc.), cardiovascular (AV blocks) and musculoskeletal system (Lyme arthritis) [
7].
The diagnosis of Lyme disease is quite challenging and is based on clinical findings, disease endemicity and serology testing [
8]. Serologic tests are not sensitive but are used for disease confirmation. For testing, an enzyme-linked immunoassay (ELISA) followed by a more specific Western immunoblot test is done. IgG and IgM antibodies against specific Borrelial proteins are measured. Cultures of blood and other body fluids (e.g., CSF, joint fluid) may be taken to rule out other diseases. CSF sampling shows elevated cell counts (predominantly neutrophils) with low glucose and elevated proteins [
9].
Since erythema migrans is nonspecific to Lyme disease, disorders like inflammation due to insect bites, ringworm, and cellulitis. Other disorders like Bell’s palsy, fibromyalgia, myocarditis, SLE, etc. should also be ruled out.
The treatment of choice for Lyme disease is an antibiotic taken for 10-14 days. The classes of antibiotics that have shown the greatest efficacy against Borrelia are beta-lactams, tetracyclines and macrolides [
10]. The most used antibiotic is oral doxycycline but alternatives include oral amoxicillin and azithromycin. For severe cases or disseminated stage, parenteral antibiotics are given. The treatment of Lyme disease during pregnancy is oral amoxicillin (as doxycycline is contraindicated).
A single prophylactic dose of doxycycline is given if the following criteria are fulfilled [
11]:
The disease infection rates are greater than 20%.
The tick has remained attached for more than 36 hours.
Tick removed within 72 hours.
There are no contraindications to doxycycline.
Lyme disease can be prevented in endemic areas by wearing long-sleeved shirts and closed shoes. The use of insect repellents also significantly reduces the chances of tick bites [
12]. The active ingredient in these insect repellents is DEET (diethyltoluamide). Remove the ticks, if found, as soon as possible. Despite all these preventive techniques, most people with Lyme disease do not remember being bitten by a tick.
CONCLUSION:
In conclusion, Borreliosis caused by Borrelia burgdorferi remains a health concern with gradually increasing cases. The diagnosis of this disease is quite challenging due to diverse clinical features and no specific available tests. Antibiotic therapy remains the mainstay of treatment. There are preventive strategies available too but most of the patients with tick bites present with no clinical complaint which further results in the dissemination of the disease throughout the body. Despite many studies, there are many unresolved questions regarding the disease diagnosis and treatment. This thus requires further research and increasing public awareness regarding Lyme disease.
Funding
None of the authors are financially interested in any of the products, devices or drugs mentioned in this manuscript.
Institutional Review Board Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bush LM, Vazquez-Pertejo MT. Tick borne illness—Lyme disease. Disease-a-Month. 2018 May 1;64(5):195–212. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0011502918300075.
- Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP. Diagnosis of lyme borreliosis. Clin Microbiol Rev [Internet]. 2005 Jul [cited 2023 Dec 8];18(3):484–509. Available from: https://journals.asm.org/doi/10.1128/cmr.18.3.484-509.2005.
- Dana AN. Diagnosis and treatment of tick infestation and tick-borne diseases with cutaneous manifestations. Dermatol Ther [Internet]. 2009 Jul 1 [cited 2023 Dec 8];22(4):293–326. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1529-8019.2009.01244.x.
- Kilpatrick AM, Dobson ADM, Levi T, Salkeld DJ, Swei A, Ginsberg HS, et al. Lyme disease ecology in a changing world: consensus, uncertainty and critical gaps for improving control. Available from: https://royalsocietypublishing.org/doi/pdf/10.1098/rstb.2016.0117.
- Steere AC, Coburn J, Glickstein L. Lyme Borreliosis. Tick-Borne Diseases of Humans [Internet]. 2014 Apr 8 [cited 2023 Dec 8];176–206. Available from: https://onlinelibrary.wiley.com/doi/full/10.1128/9781555816490.ch11.
- Sehgal VN, Khurana A. Lyme disease/borreliosis as a systemic disease. Clin Dermatol. 2015 Sep 1;33(5):542–50. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0738081X15001212.
- Lyme Disease: A Multisystem Infection That Affects the Nervo... : CONTINUUM: Lifelong Learning in Neurology [Internet]. [cited 2023 Dec 8]. Available from: https://journals.lww.com/continuum/abstract/2012/12000/lyme_disease__a_multisystem_infection_that_affects.6.aspx.
- Waddell LA, Greig J, Mascarenhas M, Harding S, Lindsay R, Ogden N. The Accuracy of Diagnostic Tests for Lyme Disease in Humans, A Systematic Review and Meta-Analysis of North American Research. PLoS One. 2016;11(12):168613. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0738081X15001212.
- Angel TE, Jacobs JM, Smith RP, Pasternack MS, Elias S, Gritsenko MA, et al. Cerebrospinal fluid proteome of patients with acute Lyme disease. J Proteome Res [Internet]. 2012 Oct 5 [cited 2023 Dec 8];11(10):4814–22. Available from: https://pubs.acs.org/doi/epdf/10.1021/pr300577p.
- BMC Veterinary Research. Available from: https://link.springer.com/article/10.1186/s12917-017-1212-3.
- Harms MG, Hofhuis A, Sprong H, Bennema SC, Ferreira JA, Fonville M, et al. A single dose of doxycycline after an ixodes ricinus tick bite to prevent Lyme borreliosis: An open-label randomized controlled trial. Journal of Infection. 2021 Jan 1;82(1):98–104. Available from: https://www.sciencedirect.com/science/article/abs/pii/S016344532030414X.
- Mitchell C, Dyer M, Lin FC, Bowman N, Mather T, Meshnick S. Protective Effectiveness of Long-Lasting Permethrin Impregnated Clothing Against Tick Bites in an Endemic Lyme Disease Setting: A Randomized Control Trial Among Outdoor Workers. J Med Entomol [Internet]. 2020 Sep 7 [cited 2023 Dec 8];57(5):1532–8. Available from:. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).