Submitted:
26 November 2023
Posted:
27 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
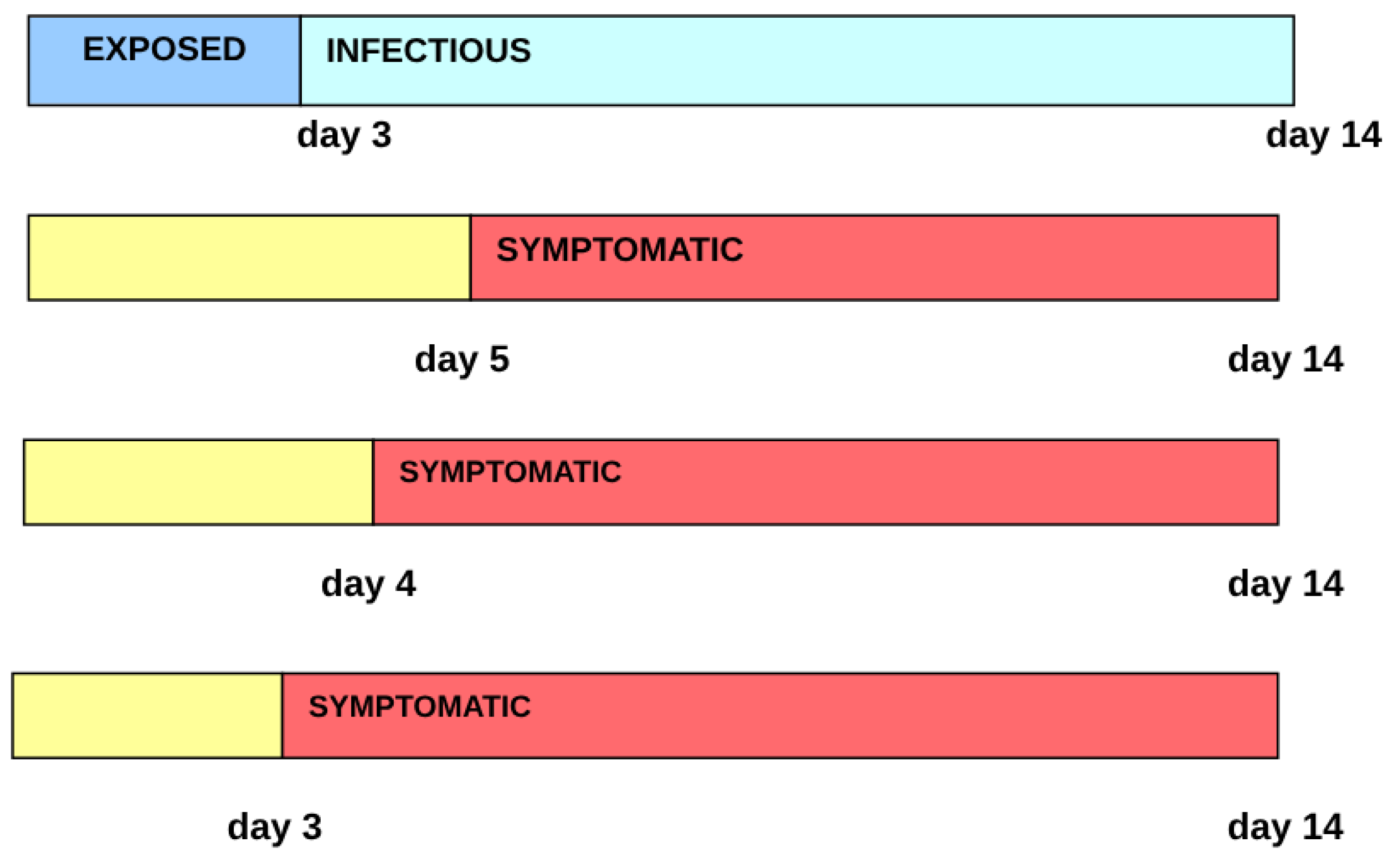
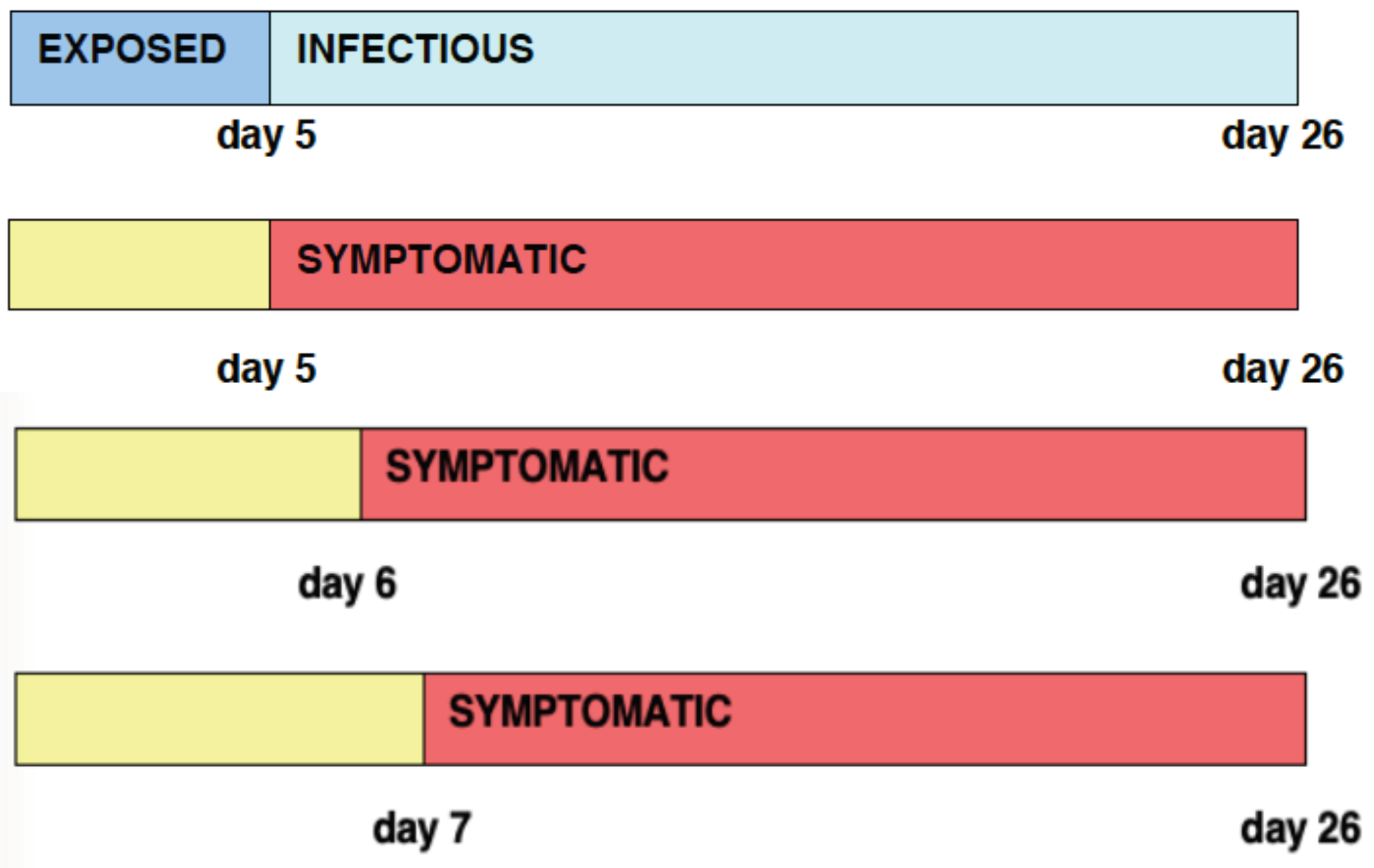
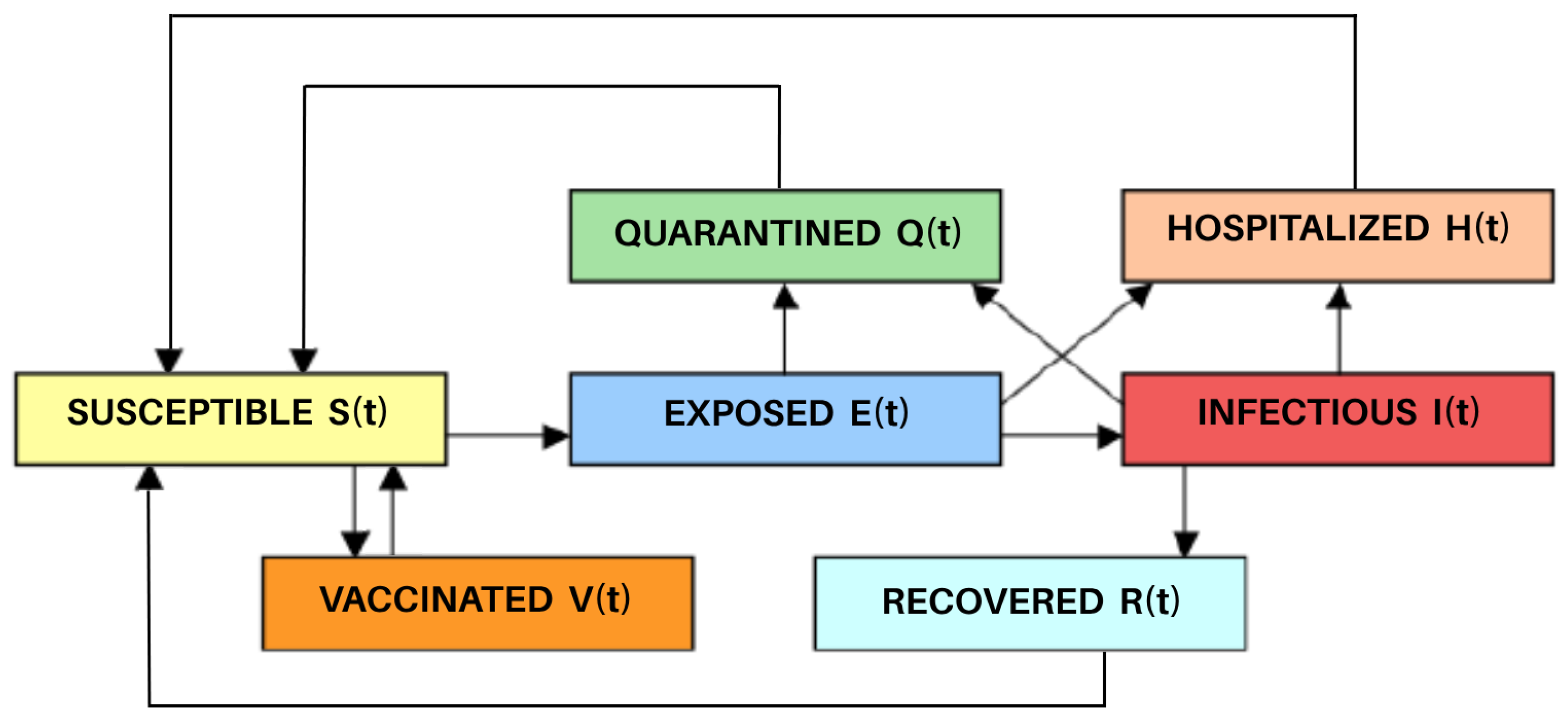
2.1. Equations of the Model
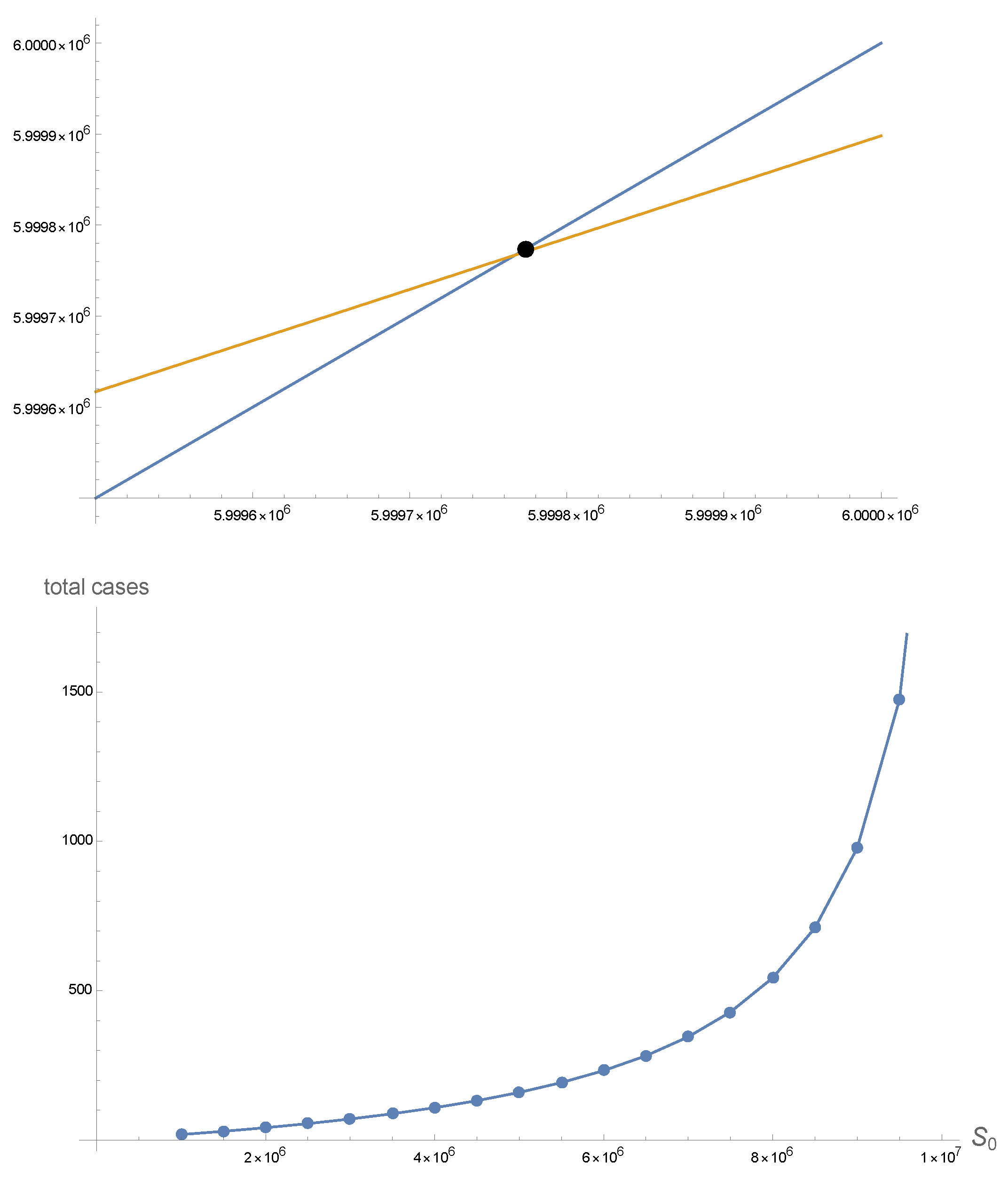
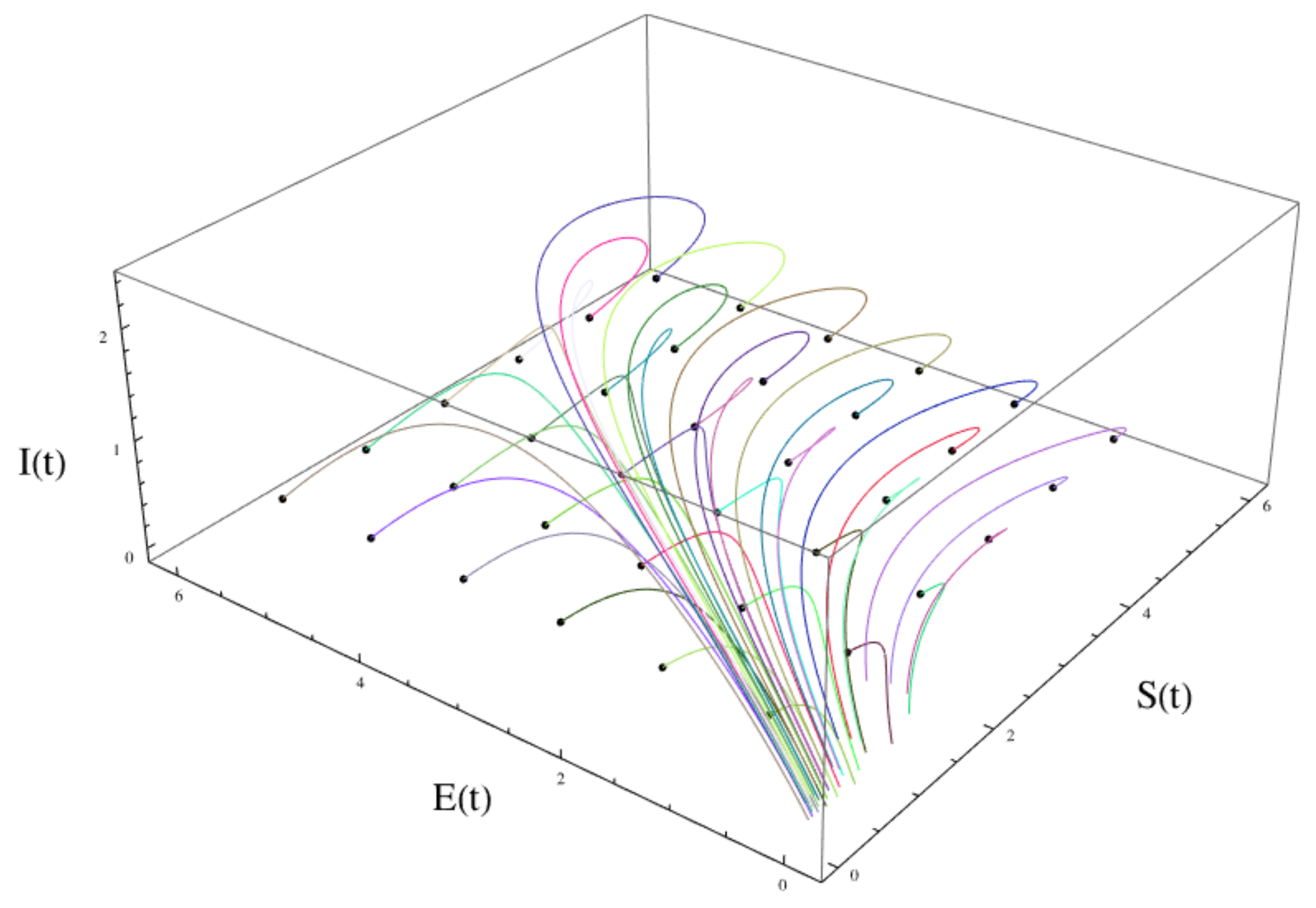
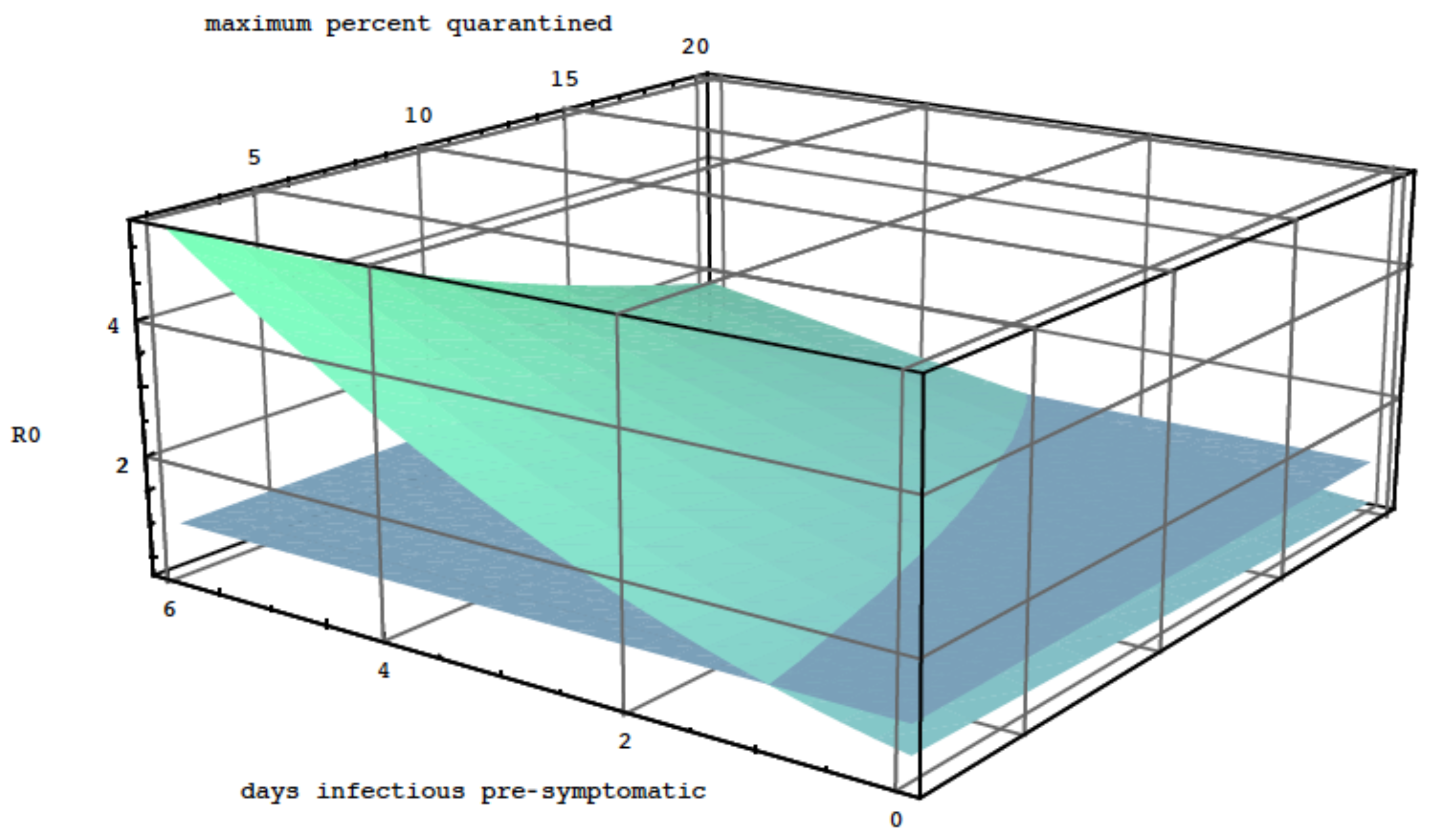
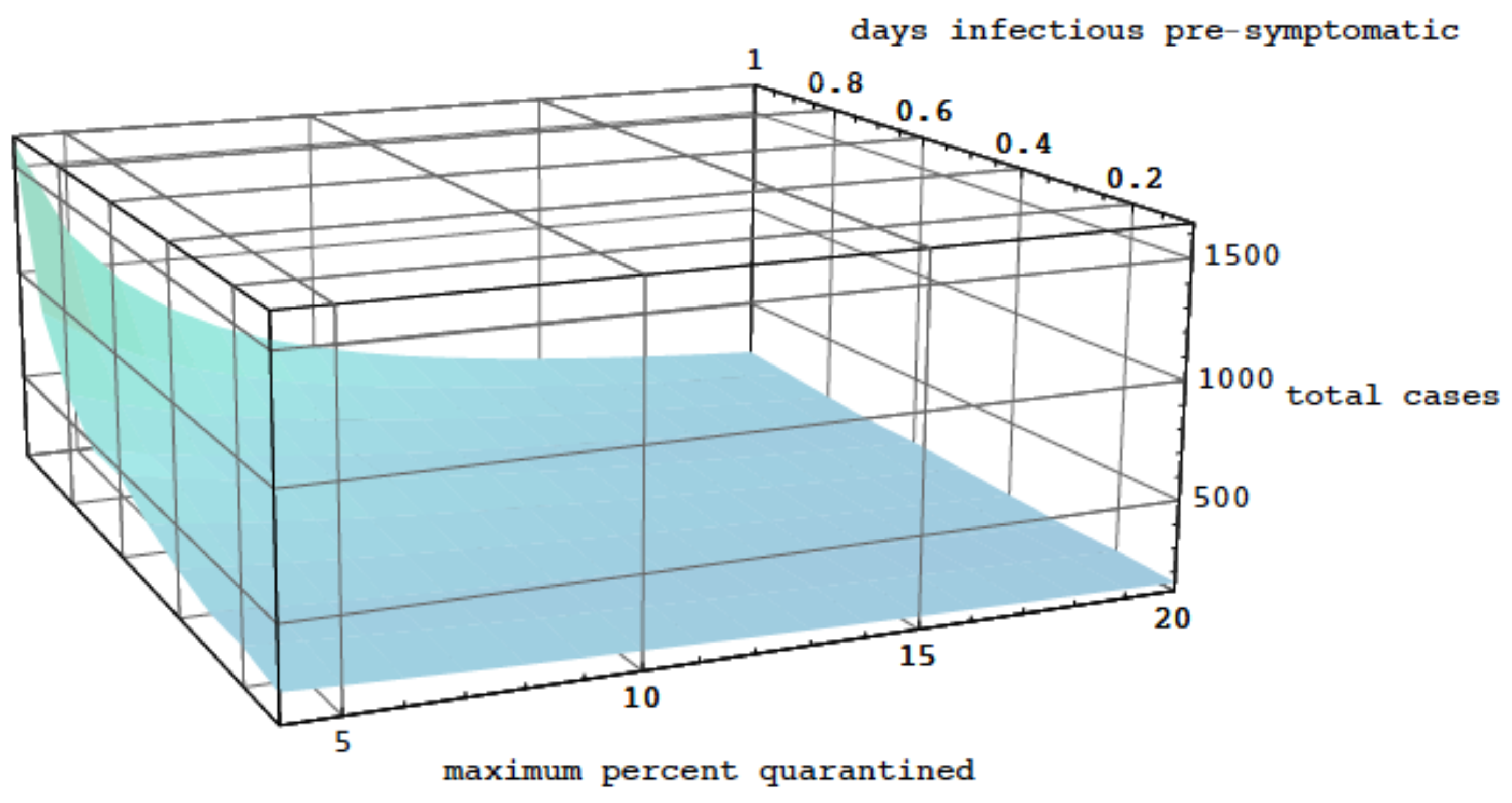
2.2. Analysis of the Model
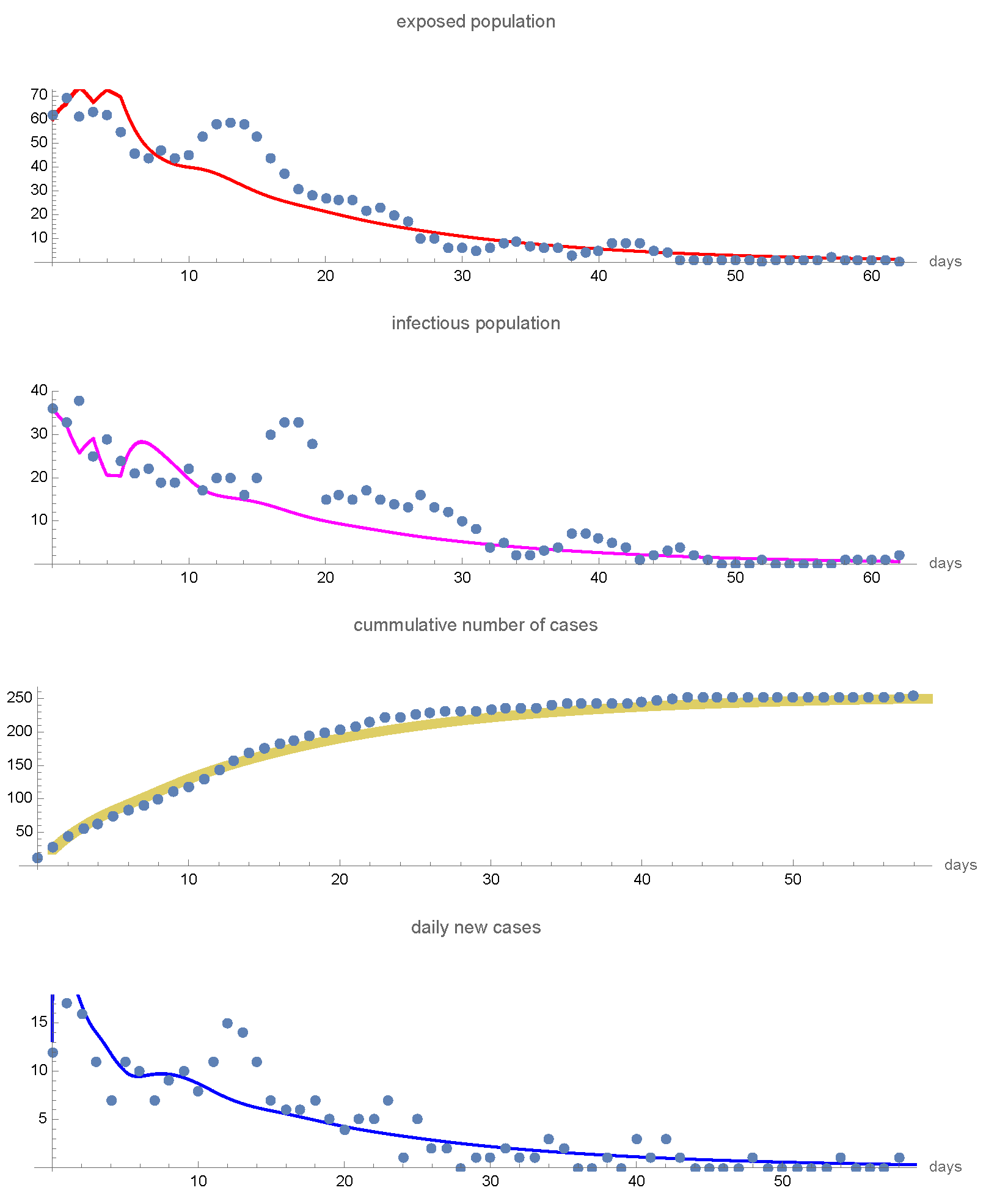
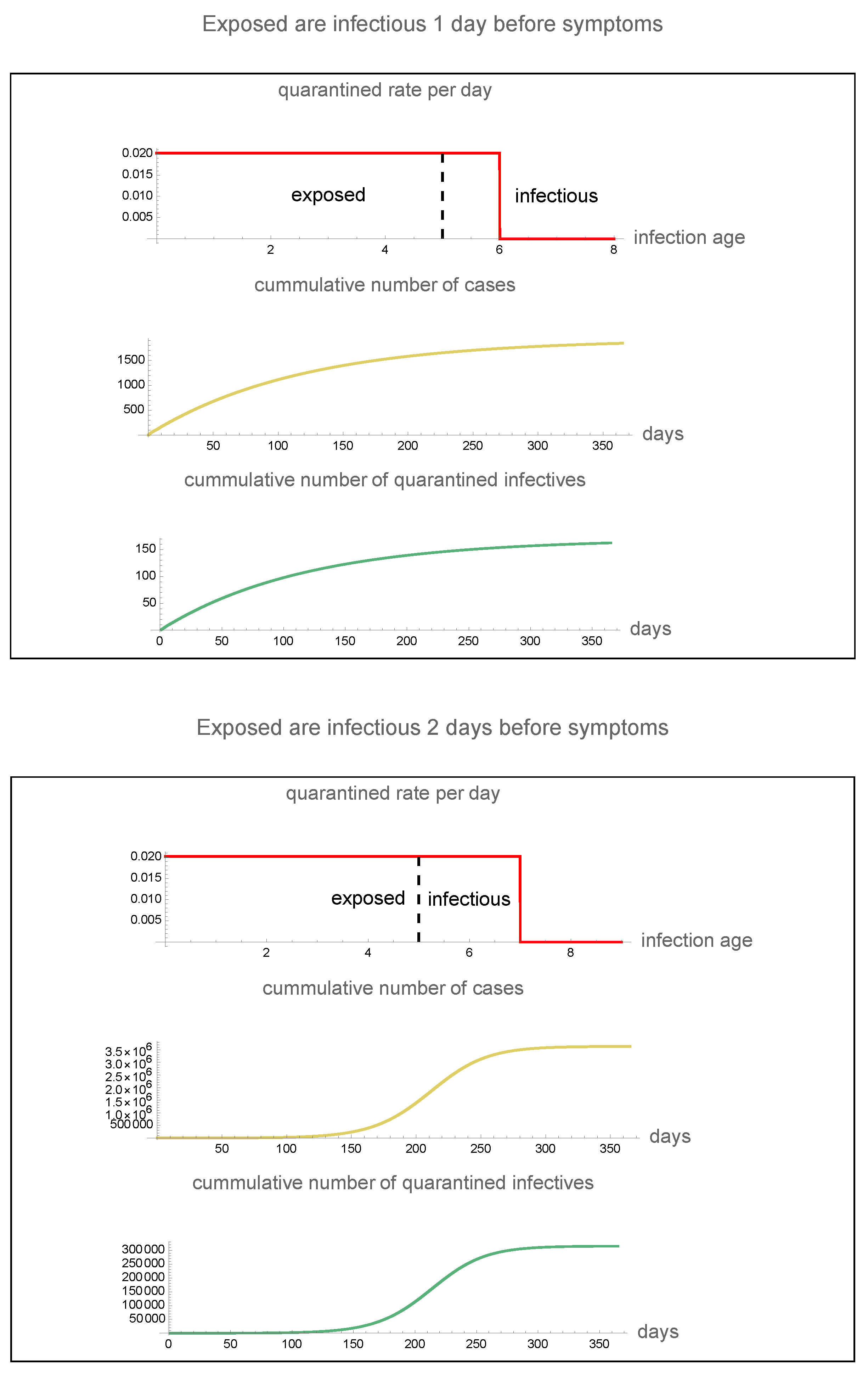
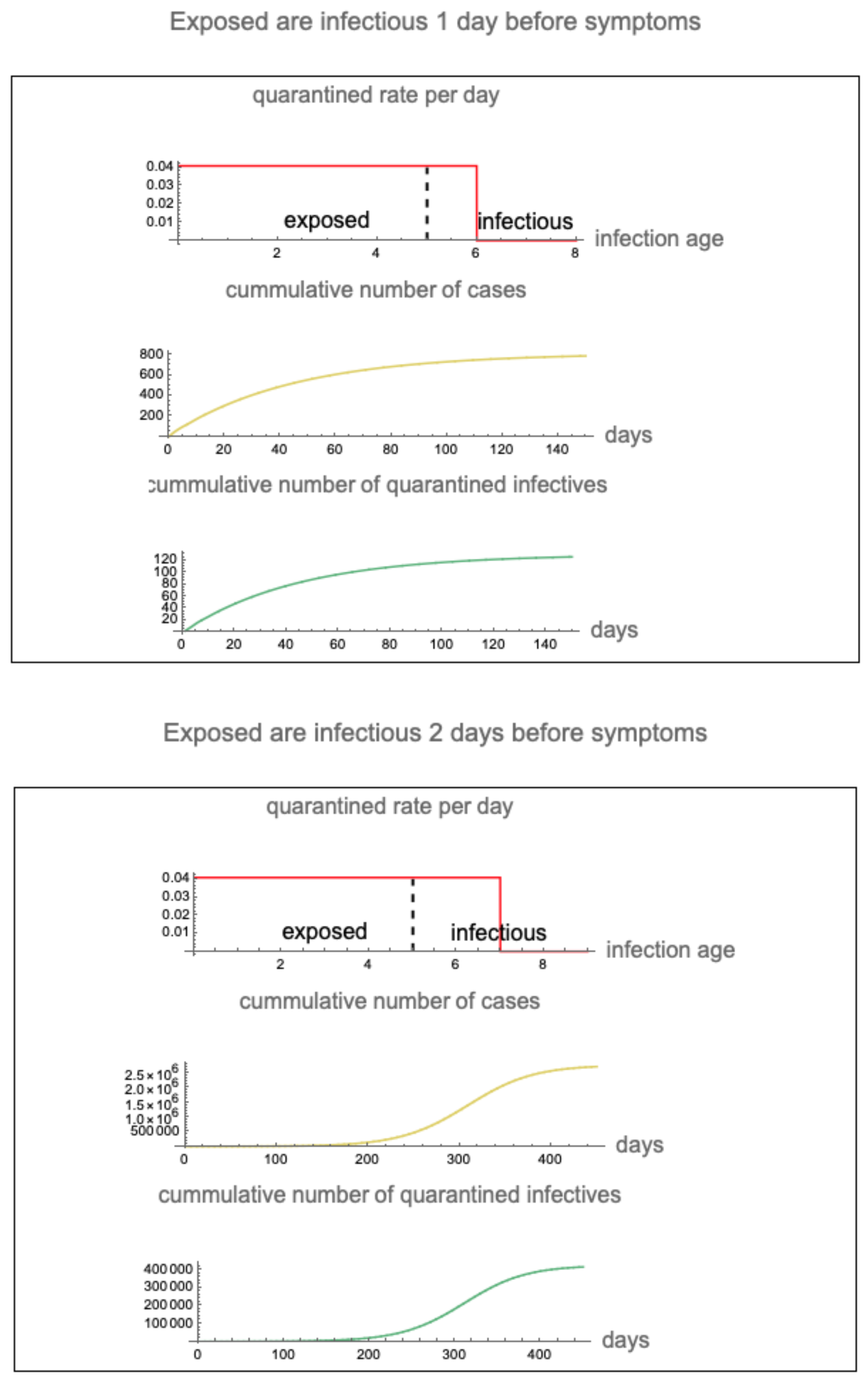
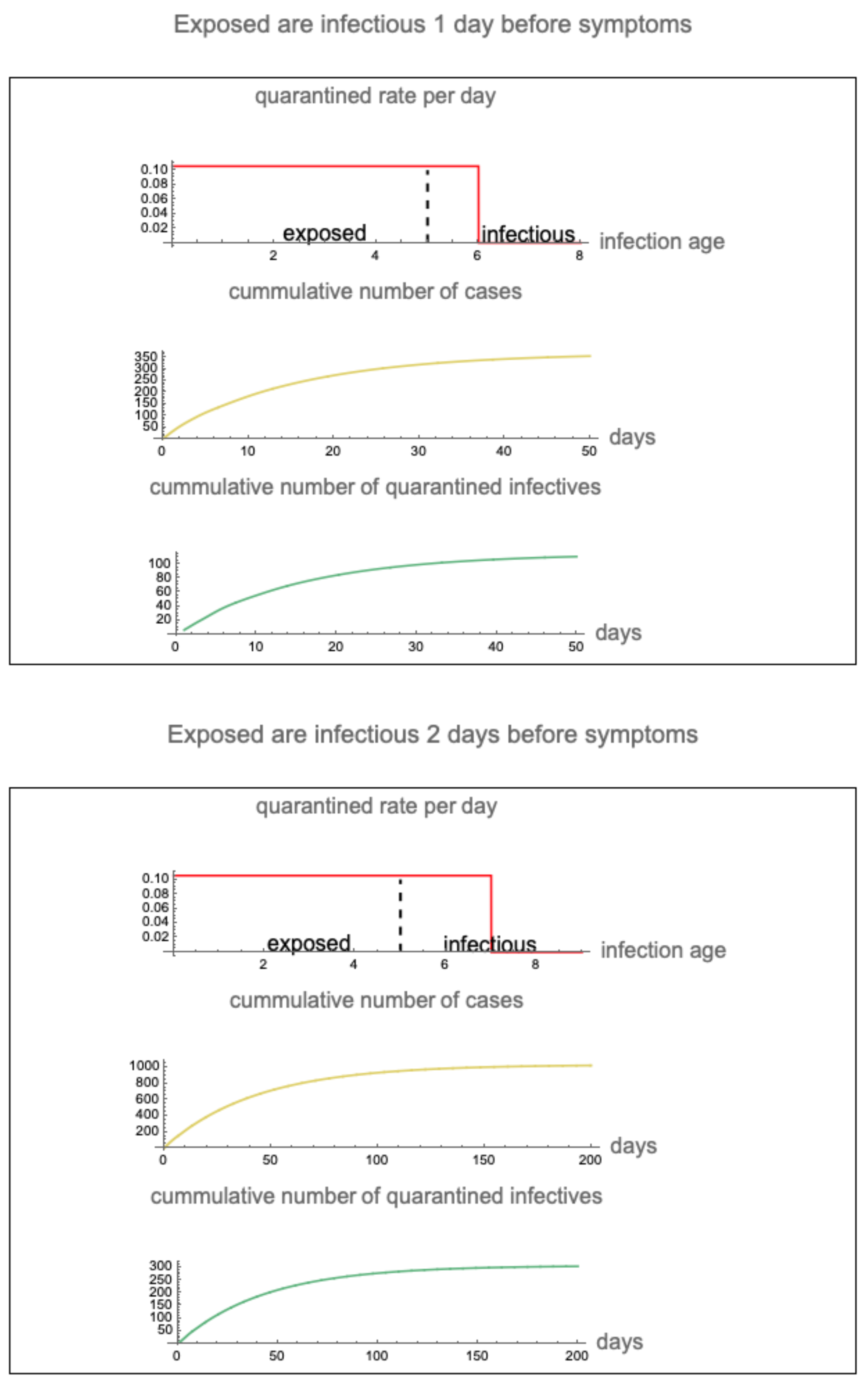
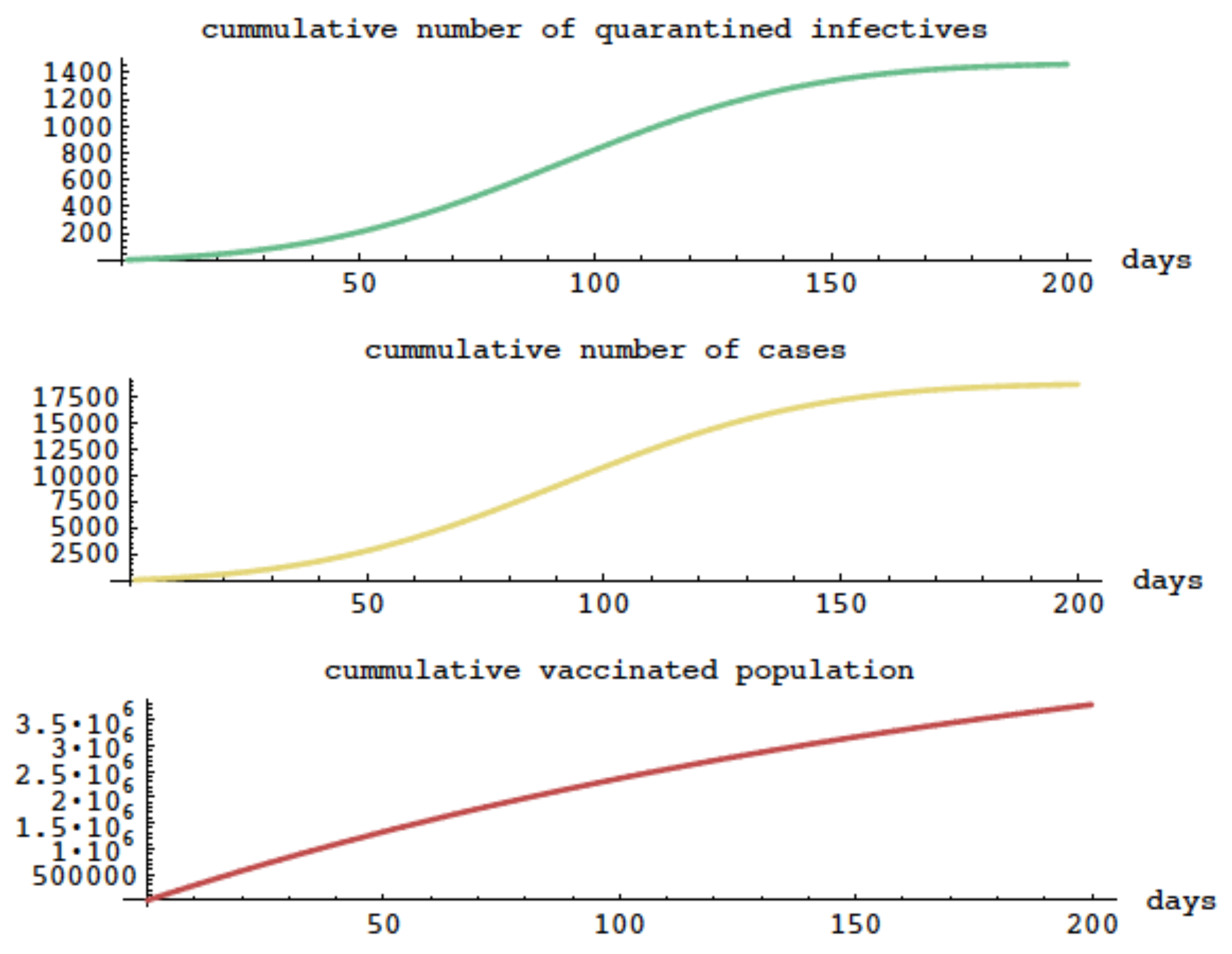
2.3. Application of the Model to the 2003 SARS Epidemic in Taiwan
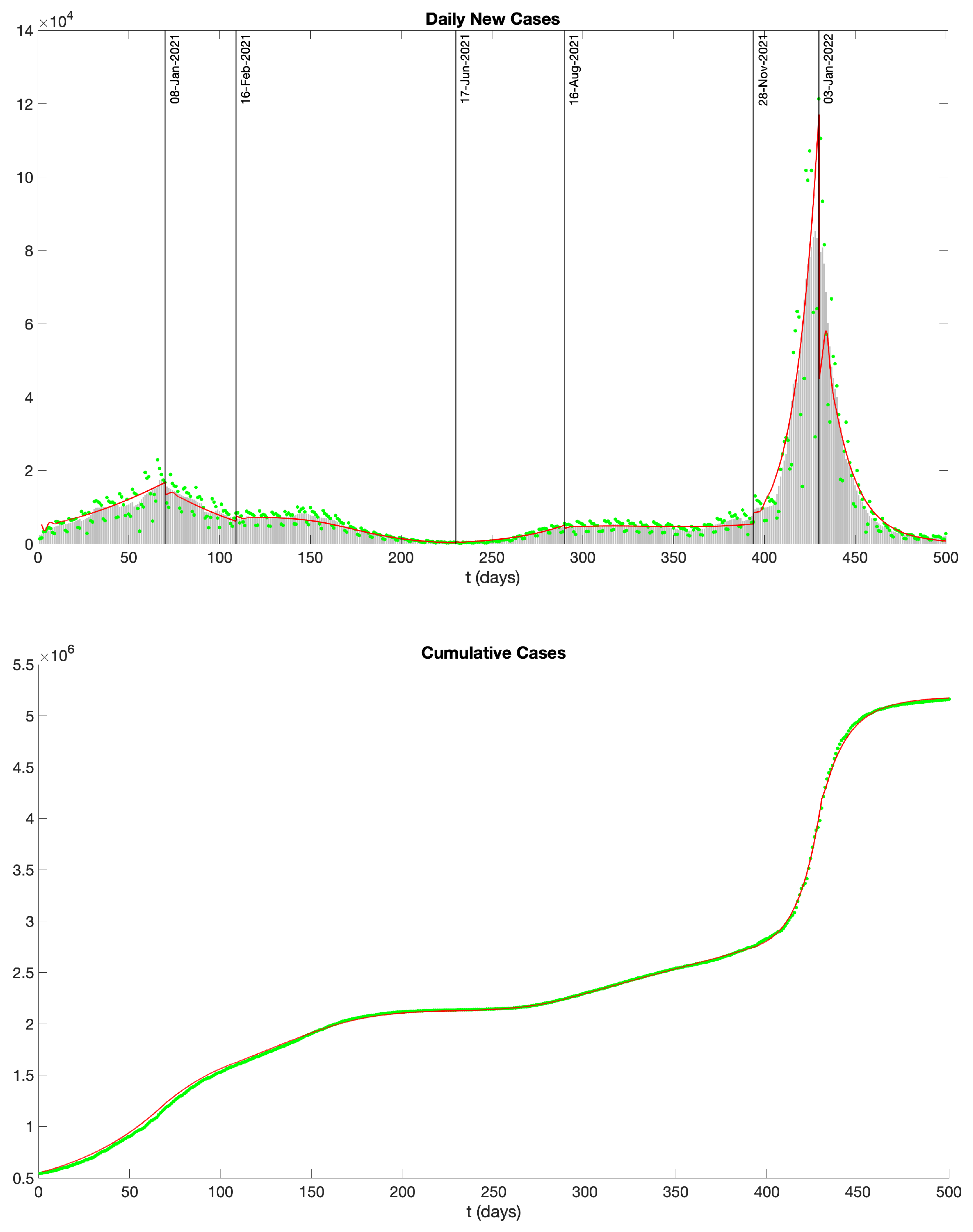
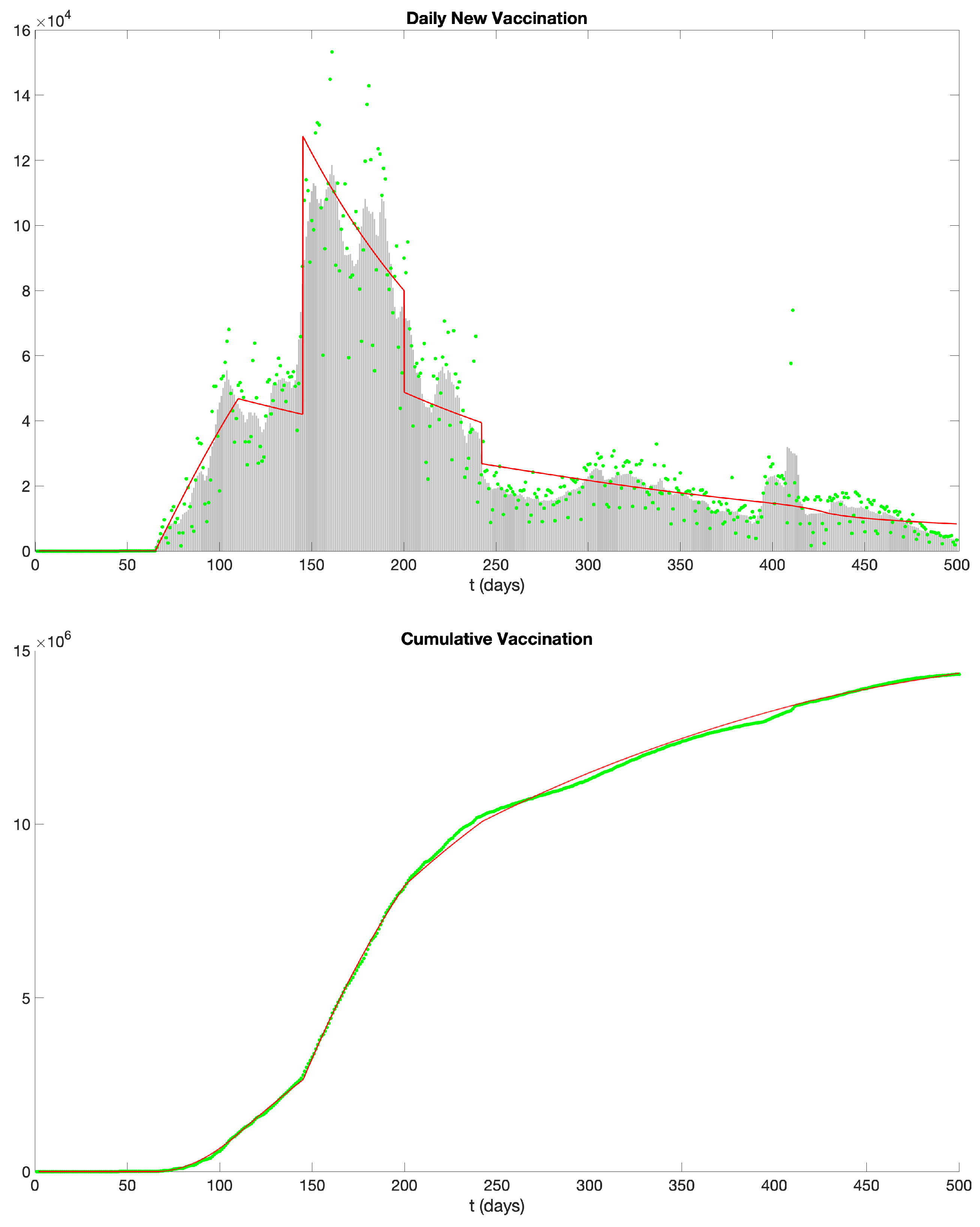
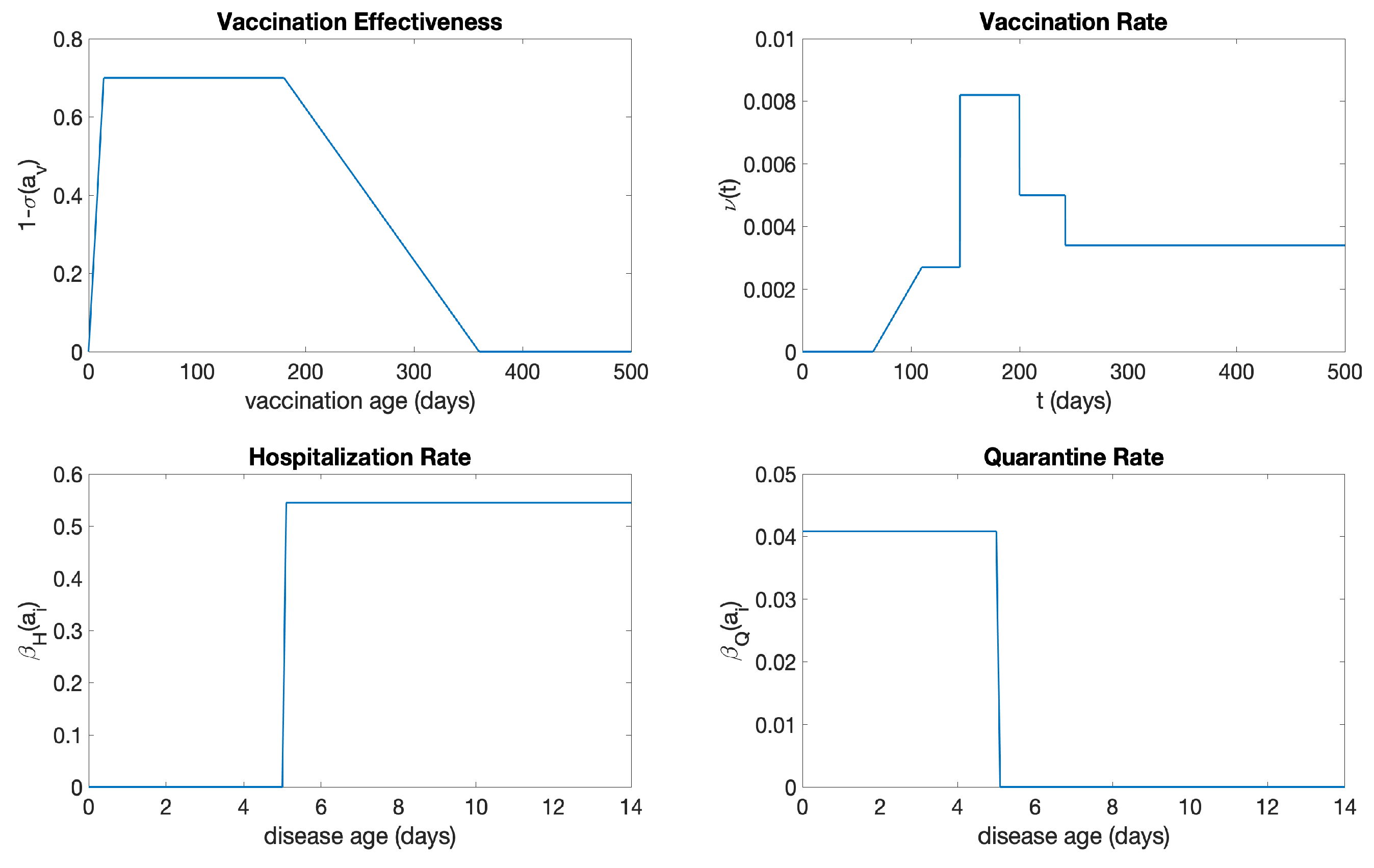
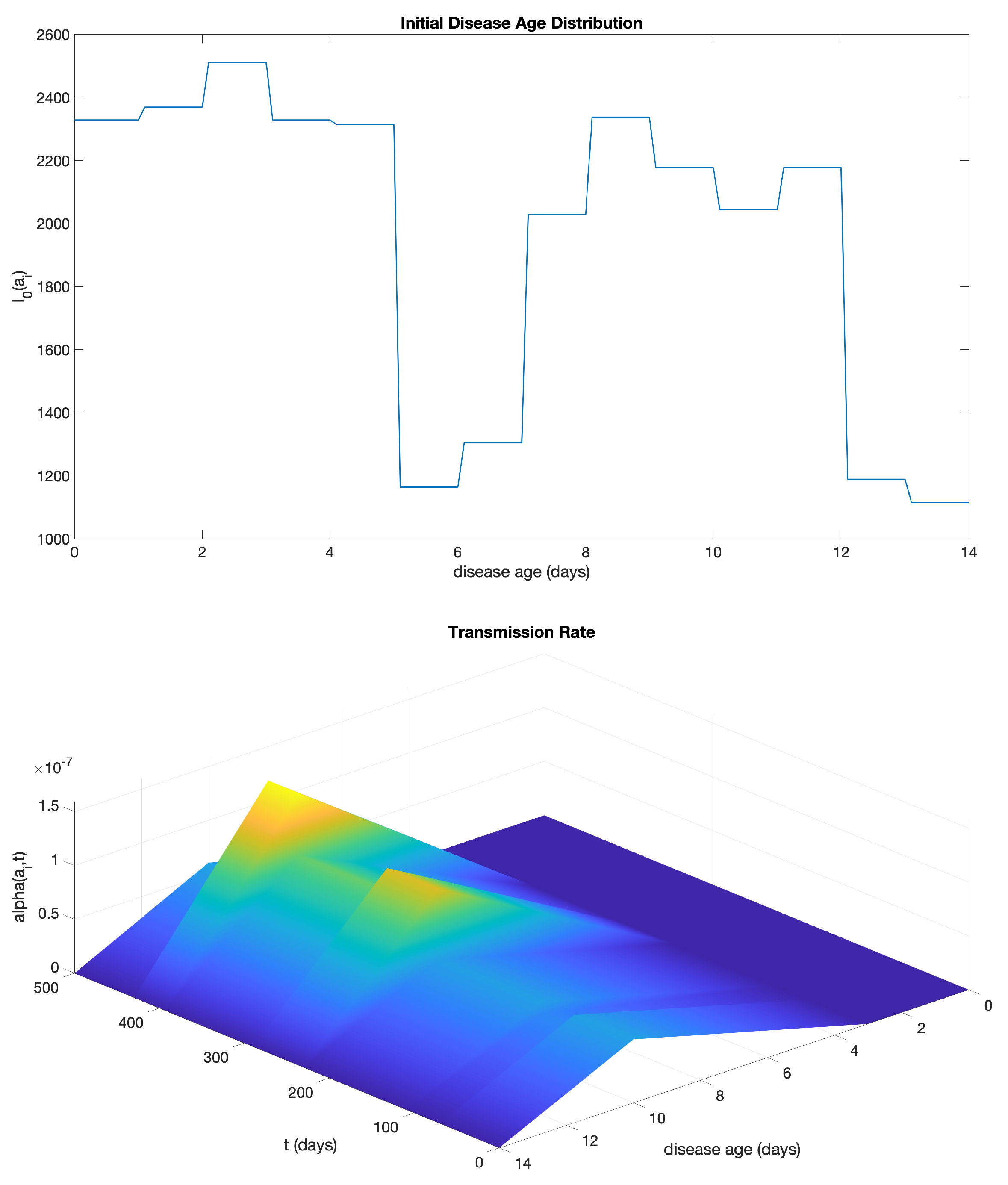
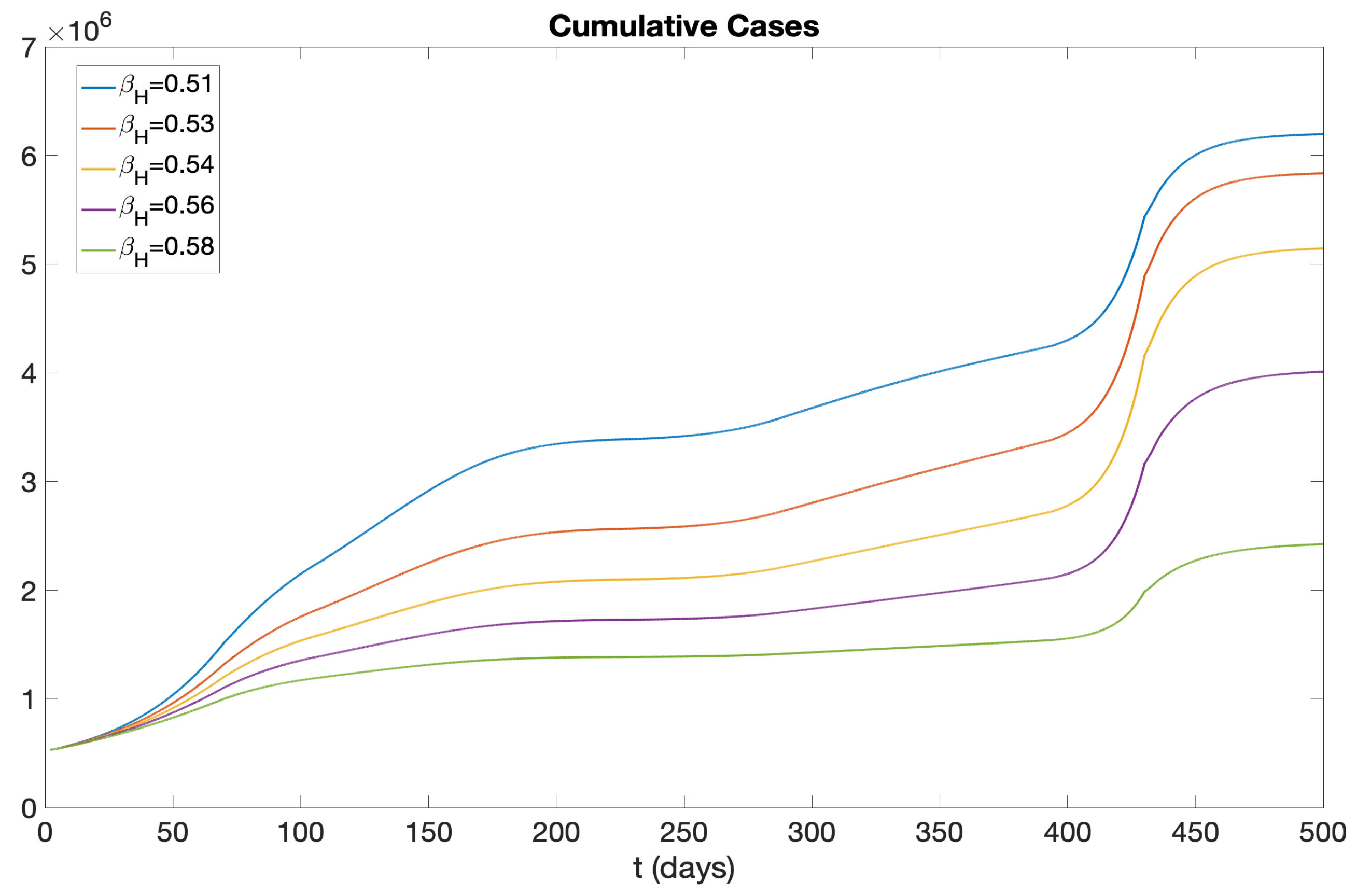
2.4. Application of the Model to the COVID-19 Epidemic in New York State
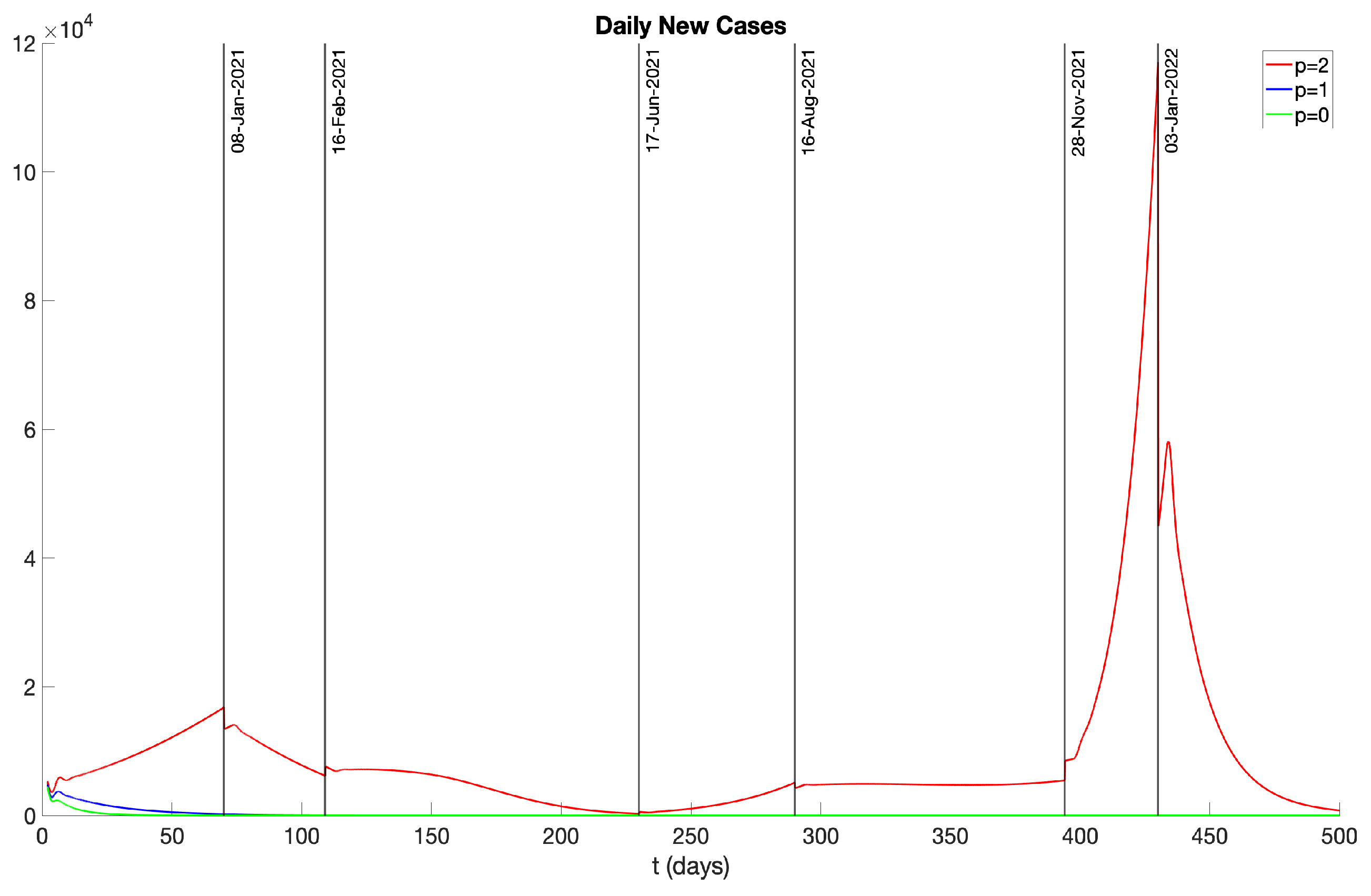
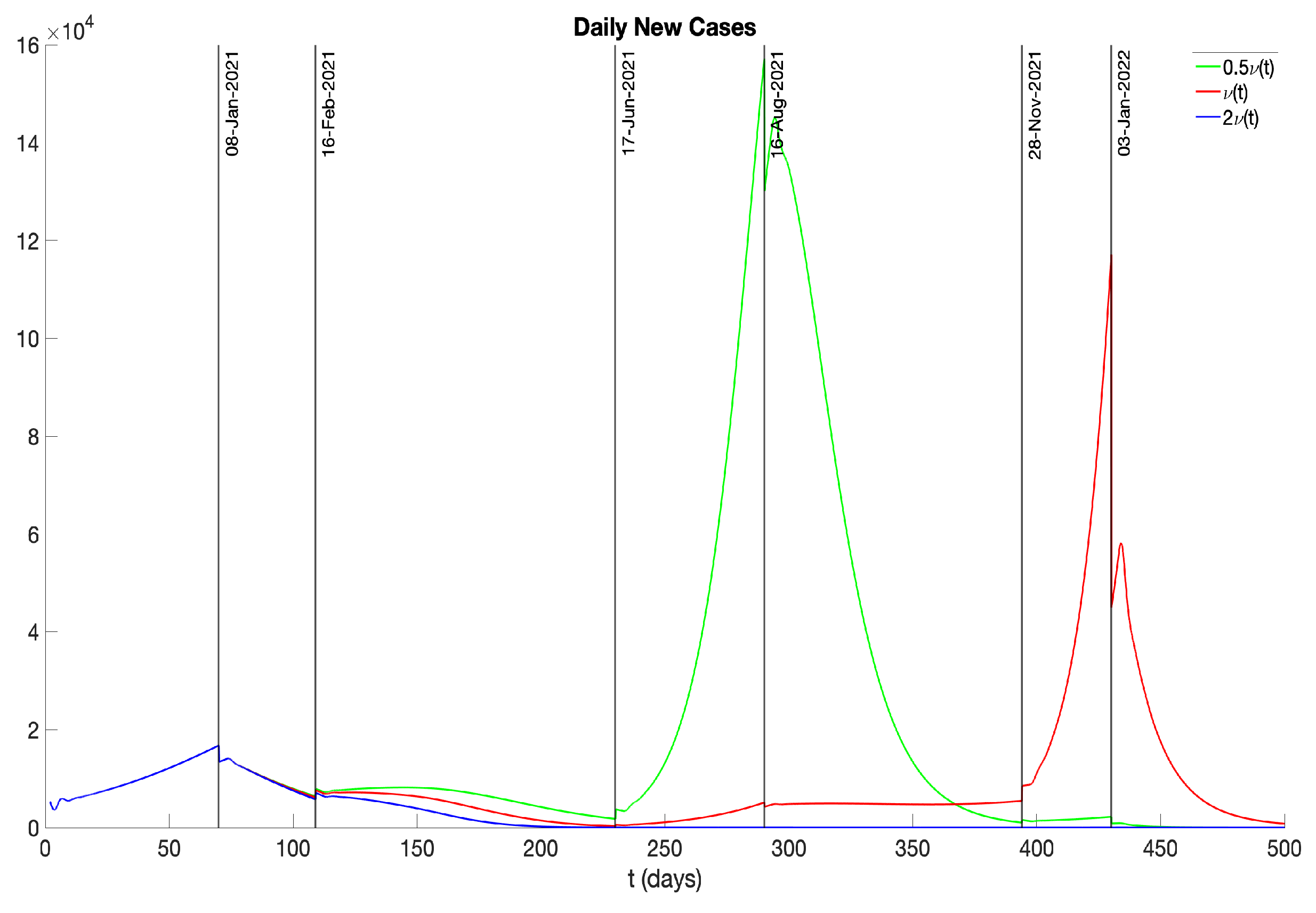
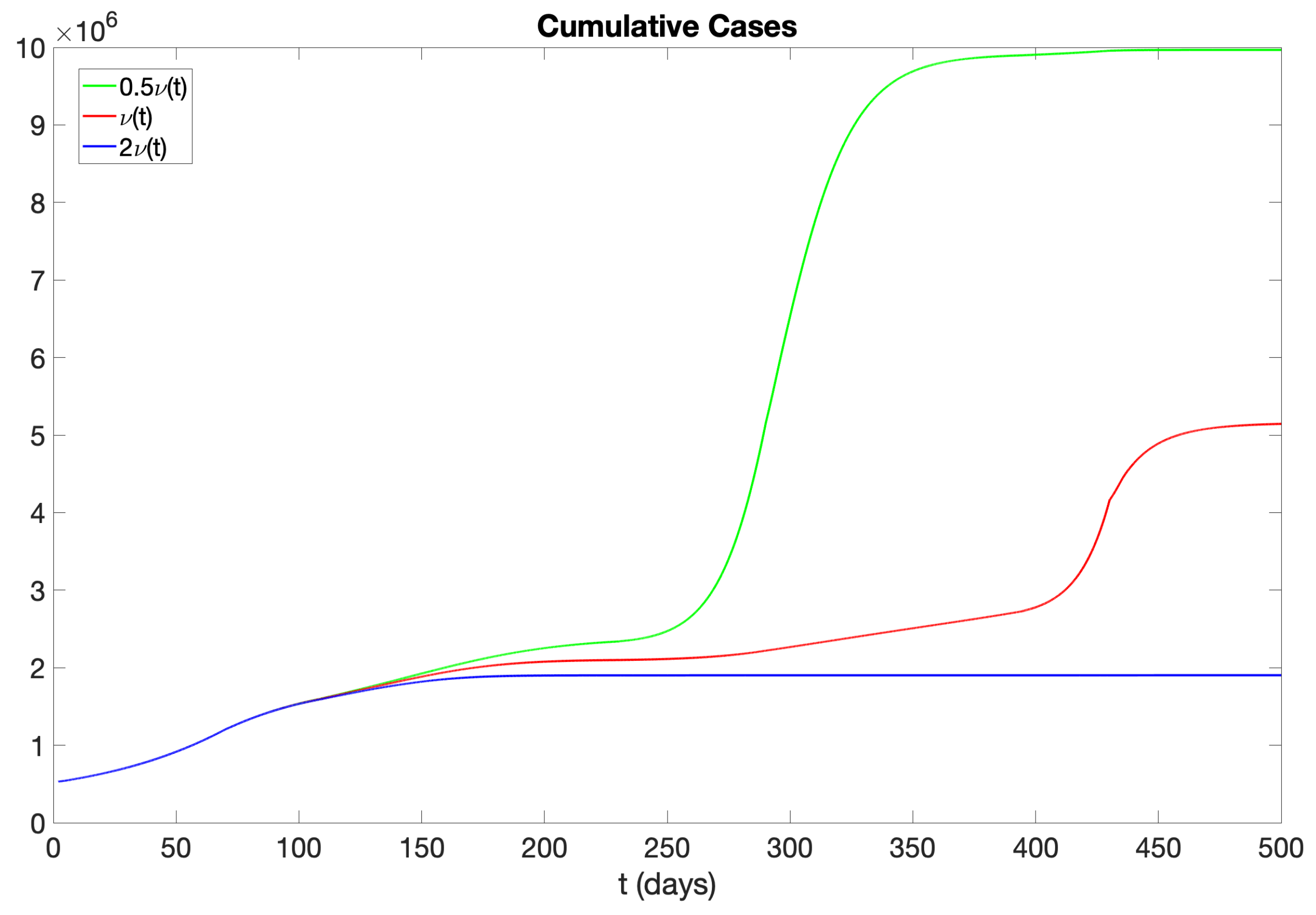
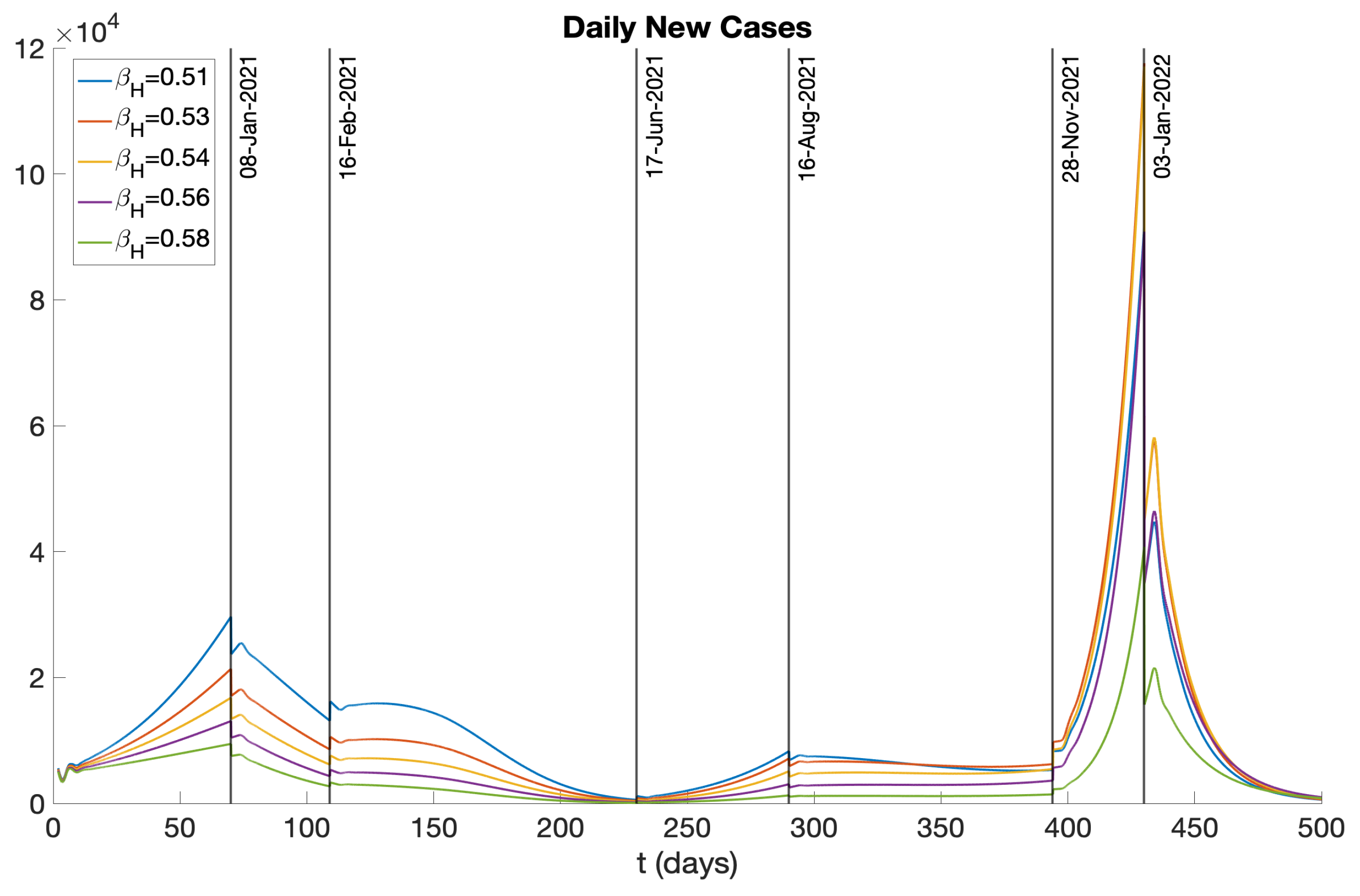
- Phase 1 (11/01/2020 – 01/08/2021) There was no vaccination in this phase.
- Phase 2 (01/08/2021 – 02/16/2021) With the commencement of vaccination campaigns and growing public caution, there was a small decrease in the COVID-19 transmission rate.
- Phase 3 (02/16/2021 – 06/17/2021) The emergence and prevalence of the Alpha variant [10] brought a small increase in the transmission rate.
- Phase 5 (08/16/2021 – 11/28/2021) In response to the rise of the Delta variant in August 2021, policies such as a universal mask mandate for all public and private schools were implemented [9], leading to a reduced transmission rate.
- Phase 6 (11/28/2021 – 01/03/2022) The Omicron variant [13] was first discovered in Botswana and South Africa in November 2021 and quickly spread to other countries, including the United States. In December 2021, the emergence of the Omicron variant led to a significant surge in COVID-19 cases.
- Phase 7 (01/03/2022 – 03/13/2022) Reacting to the emergence of the Omicron variant, various preventive policies, such as mask mandates and “Comprehensive Winter Surge Plans”, were introduced [9], leading to a decrease in the transmission rate.
3. Conclusions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sinestrari, E.; Webb, G. Nonlinear hyperbolic systems with nonlocal boundary conditions. J. Math. Anal. Appl., 1987, 121:449–464. [CrossRef]
- Farkas, J. Stability conditions for the non-linear McKendrick equations. Appl. Math. Comp. 2004, 156 (3),771-777. [CrossRef]
- Demongeot, J.; Griette, Q.; Maday, Y.; Magal, P. A Kermack?McKendrick model with age of infection starting from a single or multiple cohorts of infected patients. Proc. R. Soc. A 2023, 479: 2022038120220381. [CrossRef]
- Hsieh, Y-H,; Chen, C,; Hsu, S-B. SARS Outbreak, Taiwan, 2003. Emer. Inf. Dis., 2003, 10(2):201-206. [CrossRef]
- Hsieh, Y-H,; King, C-C; Chen, C,; Ho, M-S.; Hsu, S-B,; Wu, Y-C. Impact of quarantine on the 2003 SARS Outbreak: A retrospective modeling study. J. Theoret. Biol., 2007, 10(2):201-206. [CrossRef]
- Webb, G.; Blazer, M.; Zhu, H.; Ardal S.; Wu, J. Critical role of nonsocomial transmission in the Toronto SARS outbreak. Math. Bios. Eng. 2004, 1(1), 1-13. [CrossRef]
- Webb, G.; Hsieh, Y-H.; Wu, J.; Blaser, M. Pre-symptomatic influenza transmission, surveillance, and school closings: Implications for novel influenza A (H1N1). Math. Mod. Nat. Phen. 2010, 5(3). [CrossRef]
- Kermack, W.; McKendrick, A. A contribution to the mathematical theory of epidemics. Proc. Roy. Soc. Ser. A, 1927, 115(772):700–721. [CrossRef]
- Wikipedia, Compartmental Models in Epidemiology, 2023. https://en.wikipedia.org/wiki/Compartmental_models_in_epidemiology.
- Wikipedia. Sars-cov-2 alpha variant, 2023. [Online; accessed 15-Octorber-2023].
- Wikipedia. Sars-cov-2 delta variant, 2023. [Online; accessed 15-Octorber-2023].
- Yale Medicine. Omicron, delta, alpha, and more: What to know about the coronavirus variants, 2023. [Online;September 1,2023].
- Wikipedia. Sars-cov-2 omicron variant, 2023. [Online; accessed 15-Octorber-2023].
- Centers for Disease Control and Prevention. What is covid-19 reinfection?, 2023. [Online; accessed 3-November-2023].
- Ma. K. Trends in laboratory-confirmed SARS-CoV-2 reinfections and associated hospitalizations and deaths among adults aged >= 18 years 18 US jurisdictions, September 2021–December 2022. MMWR. Morbidity and Mortality Weekly Report, 72, 2023. [CrossRef]
- Centers for Disease Control and Prevention. Stay up to date with COVID-19 vaccines, 2023. [Online; accessed 3-November-2023].
- Ram, R.; Schaposnik, L-P. A modified age-structured SIR model for COVID-19 type viruses. Sci. Rep., 2021, 11(1):15194. [CrossRef]
- Calafiore, G-C.; Fracastoro, G. Age structure in SIRD models for the COVID-19 pandemic - A case study on Italy data and effects on mortality. PloS ONE, 2022, 17(2):e0264324. [CrossRef]
- Luebben, G.; González-Parra, G.; Cervantes, B. Study of optimal vaccination strategies for earlyCOVID -19 pandemic using an age-structured mathematical model: A case study of the USA. Math.Biosci. Eng., 2023 20(6),10828–10865. [CrossRef]
- Aldila, D.; Samiadji, B.; Simorangkir, G.; Khosnaw, S.; Shahzad, M. Impact of early detection and vaccination strategy in COVID-19 eradication program in Jakarta, Indonesia. Bmc Res. Notes 2021, 14, 132. [CrossRef]
- Andrews, M; Bausch, C. Parameterizing a dynamic influenza model using longitudinal versus age-stratified case notifications yields different predictions of vaccine impacts.Math. Biosci. Eng. 2019, 16, 5, 3753-3770. [CrossRef]
- Angulo, M.; Castanos, F.; Moreno-Morton, R.; Velasco-Hernandez, J.; Moreno, J. A simple criterion to design optimal non-pharmaceutical interventions for mitigating epidemic outbreaks.Roy. Soc. Int. 2021, 18, 20200803. [CrossRef]
- Arino, J.; Portet, S. A simple model for COVID-19.Infect. Dis. Model. 2021, 5, 309–315. [CrossRef]
- Ayoub, H.; Chemaitelly, H.; Mikhail, M.; Kanaani, Z.; Kuwari, E.; Butt, A.; Coyle, P.; Jeremijenko, A.; Kaleeckal, A.; Latif, A.; Shaik, R.; Rahim, H.; Nasrallah, G.; Yassine, H.; Kuwari, M.; Romaihi, H.; Al–Thani, M.; Bertollin, R.; Khai, A.; Abu–Raddad, L Epidemiological impact of prioritising SARS-CoV-2 vaccination by antibody status: mathematical modelling analyses.BMJ Innov. 2021, 7–327–336. [CrossRef]
- Betti, M.; Hefferman, J. A simple model for fitting mild, severe, and known cases during an epidemic with an application to the current SARS-CoV-2 pandemic.Infect. Dis. Model. 2021,5,313–323. [CrossRef]
- Bonanca, P.; Angelillo, I.; Villani, A.; Biasci, P.; Scotti, S.; Russo, R.; Maio, T.; Rosati, G.; Barretta, M.; Bozzola, E.; Castiglia, P.; Chiamenti, G.; Conforti, G.; Conversano, M.; Ferro, A.; Francia, F.; Azzari, C. Maintain and increase vaccination coverage in children, adolescents, adults and elderly people: Let’s avoid adding epidemics to the pandemic: Appeal from the Board of the Vaccination Calendar for Life in Italy: Maintain and increase coverage also by re-organizing vaccination services and reassuring the population. Vaccine 2021, 39,1187-1189. [CrossRef]
- Bracis, C.; Burns, E.; Moore, M; Swan, D.; Reeves, D.; Schiffer, J.; Dimitrov, D. Widespread testing, case isolation and contact tracing may allow safe school reopening with continued moderate physical distancing: A modeling analysis of King County, WA data. Infect. Dis. Model. 2021, 6,24–35. [CrossRef]
- Britton, T.; Ball, F.; Trapman, P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science 2020, 369, 846–849. [CrossRef]
- Bubar, K.; Reinholt, K.; Kessler, S.; Lipsitch, M.; Cobey, S.; Grad, Y.; Larremore, D. Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. Science 2021, 371,916–921. [CrossRef]
- Byambasuren, O.; Cardona, M.; Bell, K.; Clark, J.; McLaws, M-L.; Glasziou, P. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. Off. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2020, 5, 223–234. [CrossRef]
- Byrne, A.; McEvoy, D.; Collins, A.; Hunt, K.; Casey, M.; Barber, A.; Butler, F.; Griffin, J.; Lane, E.; McAloon, C.; O’Brien, K.; Wall, P.; Walsh, K.; More, S. Inferred duration of infectious period of SARS-CoV-2: Rapid scoping review and analysis of available evidence for asymptomatic and symptomatic COVID-19 cases.Inferred duration of infectious period of SARS-CoV-2: Rapid scoping review and analysis of available evidence for asymptomatic and symptomatic COVID-19 cases. BMJ Open 2020, 10,e039856. [CrossRef]
- Cai, J; Deng, X.; Yang, J.; Sun, K.; Liu, H.; Chen, Z.; Peng, C.; Chen, X.; Wu, Q.; Zou, J.; Sun, R.; Zheng, W.; Zhao, Z.; Lu, W.; Liang, Y.; Zhou, X.; Ajelli, M.; Yu, H. Modeling transmission of SARS-CoV-2 Omicron in China. Nature Medicine 2022, 28,1468?1475. [CrossRef]
- Caldwell, J; Le, X.; McIntosh, L.; Meehan, M.; Ogunlade, S.; Ragonnet, R.; O’Neill, G.; Trauer, J.; McBryde, E. Vaccines and variants: Modelling insights into emerging issues in COVID-19 epidemiology. Paediatric Resp. Rev. 2021, 39,32–39. [CrossRef]
- Carlsson R.; Childs, L.; Feng, Z.; Glasser, J.; Heffernan, J.; Li, J.; Rost, G. Modeling the waning and boosting of immunity from infection or vaccination. J. Theoret. Biol. 2020, 497,110265. [CrossRef]
- Choi, Y.; Kim, J.; Kim, J.E.; Choi, H.; Lee, C. Vaccination prioritization strategies for COVID-19 in Korea: A mathematical modeling approach. Int. J. Environ. Res. P. H. 2021, 18,4240. [CrossRef]
- Contreras, S.; Priesemann, V. Risking further COVID-19 waves despite vaccination. Lancet Infect. Dis. 2021, 21,6,745–746. [CrossRef]
- Das, P.; Upadhyay, R.; Misra, A.; Rihan, F.; Das, P.; Ghosh, D. Mathematical model of COVID-19 with comorbidity and controlling using non-pharmaceutical interventions and vaccination. Nonl. Dyn. 2021, 106(2):1213–1227. [CrossRef]
- Dashtbali, M.; Mirzaie, M. A compartmental model that predicts the effect of social distancing and vaccination on controlling COVID-19. Sci. Rep. UK 2021, 11,8191. [CrossRef]
- Dean, N.; Pastore, Y.; Piontti, A.; Madewell, Z.; Cummings, D.; Hitchings, M.; Joshi, K.; Kahn, R.; Vespignani, A.; Halloran, M.; Longini, I. Ensemble forecast modeling for the design of COVID-19 vaccine efficacy trials. Vaccine 2020, 38,7213–7216. [CrossRef]
- De la Sen, M.; Ibeas, A. On an SE(Is)(Ih)AR epidemic model with combined vaccination and antiviral controls for COVID-19 pandemic. Adv. Dif. Eq. 2021, 2021(1):92. [CrossRef]
- Demongeot, J.; Griette, Q.; Magal, P. SI epidemic model applied to COVID-19 data in mainland China. Roy. Soc. Open Sci. 2021, 7,21878. [CrossRef]
- Demongeot, J.; Griette, Q.; Magal, P.; Webb, G. Modeling vaccine efficacy for COVID-19 outbreak in New York City. Biology 2022, 11,345. [CrossRef]
- Duan, X.; Yuan, S.; Li, X. Global stability of an SVIR model with age of vaccination. Appl. Math. Comp. 2014, 226,1, 528-540. [CrossRef]
- Duan, X.; Yuan, S.; Qiu, Z; Ma, J. Global Stability of an SVEIR epidemic model with ages of vaccination and latency. Comp. Math. Appl. 2014, 68,268-309. [CrossRef]
- Eikenberry, S.; Muncuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gummel, A. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2021, 5,293–308. [CrossRef]
- Elhia, M.; Chokri, K.; Alkama, M. Optimal control and free optimal time problem for a COVID-19 model with saturated vaccination function. Commun. Math. Biol. Neurosci. 2021, 35. [CrossRef]
- Firth, J.; Hellewell, J.; P. Klepac, P.; Kissler, S.; CMMID COVID-19 Working Group; Kucharski, A.; Spurgin, L. Using a real-world network to model localized covid-19 control strategies. Nat. Med 2020, 26,1616–1622. [CrossRef]
- Fontanet , A.; Cauchemez, S. COVID-19 herd immunity: where are we? Nat. Rev. Immunol. 2020, 20,583–584. [CrossRef]
- Forien, R.; Pang, G.; Pardoux, E. Estimating the state of the COVID-19 epidemic in France using a model with memory. Roy. Soc. Open Sci. 2021, 8(3):202327. [CrossRef]
- Foy, B.; Wahl, B.; Mehta, K.; Shet, A.; Menon, G.; Britto, C. Comparing COVID-19 vaccine allocation strategies in India: A mathematical modelling study. Int. J. Infect. Dis. 2021, 103,431–438. [CrossRef]
- Ghosh, S.; Ghosh, S. A mathematical model for COVID-19 considering waning immunity, vaccination and control measures. Sci. Rep. 2023, 13,3610. [CrossRef]
- Giordano, G.; Colaneri, M.; Di Filippo, A.; Bianchini, F.; Bolzern, P.; Nicolao, G.; Sacchi, P.; Colaneri, P.; Bruno, R. Modeling vaccination rollouts, SARS-CoV-2 variants and the requirement for non-pharmaceutical interventions in Italy. Nat. Med. 2021, 27,993?998. [CrossRef]
- Gokbulut, N.; Kuymakamzade, B.; Sanlidag, T.; Hincal, E. Mathematical modelling of Covid-19 with the effect of vaccine. Aip Conf. Proc. 2021, 2325, 020065. [CrossRef]
- Goldstein, Cassidy, T.; Wachter, K. Vaccinating the oldest against COVID-19 saves both the most lives and most years of life. Proc. Natl. Acad. Sci. USA 2021, 118 (11) e2026322118. [CrossRef]
- Griette, Q.; Magal, P. Clarifying predictions for COVID-19 from testing data: the example of New-York State. Infect. Dis. Model., 2021, 6,273–283. [CrossRef]
- Griette, Q.; Liu, Z.; Magal, P.; Thompson, R. Real-time prediction of the end of an epidemic wave: COVID-19 in China as a case-study. Mathematics of Public Health. Fields Institute Communications, Vol 85, 2020. [CrossRef]
- Gumel, A.; Ibio, E.; Ngonghala, C.; Elbas, E. A primer on using mathematics to understand COVID-19 dynamics: Modeling, analysis and simulations. Infect. Dis. Model. 2021, 6,148-168. [CrossRef]
- Hellewell, J.; Abbott, S.; Gimma, A.; Bosse, N.; Jarvis, C.; Russell, T.; Munday, J.; Kucharski, A.; Edmunds, W. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health 2020, 8,E488–E496. [CrossRef]
- Huo, X.; Chen, J.; Ruan, S. Estimating asymptomatic, undetected and total cases for the COVID-19 outbreak in Wuhan: a mathematical modeling study. Bmc Infect Dis. 2021, 21(10:476. [CrossRef]
- Huo, X.; Sun, X.; Bragazzi, N.; Wu, J. Effectiveness and feasibility of convalescent blood transfusion to reduce COVID-19 fatality ratio. Roy. Soc. Open Sci. 2021, 8:202248. [CrossRef]
- Iboi, E.; Ngonghala, C.; Gumel, A. Will an imperfect vaccine curtail the COVID-19 pandemic in the US? Infect. Dis. Model. 2021, 5,510–524. [CrossRef]
- IHME COVID-19 Forecasting Team; Modeling COVID-19 scenarios for the United States. Nat Med. 2021, 27,94–105. [CrossRef]
- Inayaturohmat, F.; Zikkah, R.; Supriatna, A.; Anggriani, N. Mathematical model of COVID-19 transmission in the presence of waning immunity. J. Phys. Conf. Ser. 2021, 1722, 012038. [CrossRef]
- Jackson, L.; Anderson, E.; Rouphael, N. An mRNA Vaccine against SARS-CoV-2 - Preliminary Report. New Engl. J. Med. 2021, 383,1920–1931. [CrossRef]
- Jentsch, P.; Anand, M.; Bauch, C. Prioritising COVID-19 vaccination in changing social and epidemiological landscapes: A mathematical modelling study. Lancet Infect. Dis. 2021, 8:1097-1106. [CrossRef]
- Jewell, N.; Lewnard, J.; Jewell, B. Predictive mathematical models of the COVID-19 pandemic: Underlying principles and value of projections. JAMA, 2020, 323,1893–1894. [CrossRef]
- Johansson, M.; Quandelacy, T.; Kada, S.; Prasad, P.; Steele, M.; Brooks, J.; Slayton, R.; Biggerstaff, M.; Butler, J. SARS-CoV-2 Transmission From People Without COVID-19 Symptoms. JAMA Netw. Open 2021, 4(1):e2035057. [CrossRef]
- Johnston, M.; Pell, B.; Nelson, P. A mathematical study of COVID-19 spread by vaccination status in Virginia. Appl. Sci. 2022, 12,1723. [CrossRef]
- Kalyan, D.; Kumar, G.; Reddy K.; Lakshminarayand, K. Sensitivity and elasticity analysis of novel corona virus transmission model: A mathematical approach. Sensors Int. 2021, 2,100088. [CrossRef]
- Keeling, M.; Hill, E.; Gorsich, E.; Penman, B.; Guyver-Fletcher, G.; Holmes, A.; Leng, T.; McKimm, H.; Tamborrino, M.; Dyson, L.; Tildesley, M. Predictions of COVID-19 dynamics in the UK: Short-term forecasting and analysis of potential exit strategies. PLoS Comput. Biol. 2021, 17(1): e1008619. [CrossRef]
- Krueger, T,; Gogolewski, K.; Bodych, M., Gambin, A.,; Giordano,G.; Cuschieri, S.; Czypionka, T,; Perc, M.; Petelos,E.; Rosinska, M.; Szczurek, E. Risk assessment of COVID-19 epidemic resurgence in relation to SARS-CoV-2 variants and vaccination passes. Comm. Med.(Lond) 2022, 2, 23. [CrossRef]
- Kucharski, A.; Russell, T.; Diamond, C.; Liu, Y.; Edmunds, J.; Funk, S.; Eggo, R. Early dynamics of transmission and control of covid-19: A mathematical modelling study. Lancet Infect. Dis. 2020, 20, 553–558. [CrossRef]
- Lauer, S.; Grantz K.; Bi, Q.; Jones, F.; Zheng, Q.; Meredith, H.; Azman, A.; Reich, N.; Lesser, J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann. Intern. Med. 2020, 172,577–582. [CrossRef]
- Libotte, G.; Lobato, F.; Platt, G.; Neto, A. Determination of an optimal control strategy for vaccine administration in COVID-19 pandemic treatment. Comput. Meth. Prog. Biol. 2020, 196,105664. [CrossRef]
- Lipsitch, M.; Dean, N. Understanding COVID-19 vaccine efficacy. Science 2020, 370,763–765. [CrossRef]
- Liu, Z.; Magal, P.; Seydi, O.; Webb, G. Understanding unreported cases in the 2019 -n Cov epidemic outbreak in Wuhan, China, and the importance of major public health interventions. Biology 2020, 9(3):50. [CrossRef]
- Liu, Z.; Magal, P.; Seydi, O.; Webb, G. A COVID-19 epidemic model with latency period. Infect. Dis. Mod. 2021, 5,323–337. [CrossRef]
- Magal, P.; Webb, G. The parameter identification problem for SIR epidemic models: Identifying unreported cases. J. Math. Biol. 2018, 77,1629–1648. [CrossRef]
- Majeed, B.; David, J.; Bragazzi, N.; McCarthy, Z.; Grunnill, M.; Heffernan, J.; Wu, J.; Woldegerima, W. Mitigating co-circulation of seasonal influenza and COVID-19 pandemic in the presence of vaccination: A mathematical modeling approach. Front. Pub. Health 2023, 10,1086849. [CrossRef]
- Makhoul, M.; Chemaitelly, H.; Ayoub, H.; Seedat, S.; Abu-Raddad, L. Epidemiological Differences in the Impact of COVID-19 Vaccination in the United States and China. Vaccines 2021, 9,223. [CrossRef]
- Mancuso, M,; Eikenberry, S.; Gumel, A. Will vaccine-derived protective immunity curtail COVID-19 variants in the US? Inf. Dis. Mod. 2021, 6,1110-1134. [CrossRef]
- Mandal, M.; Jana, S.; Nandi, S.; Khatua, A.; Adak, S.; Kar, T. A model based study on the dynamics of COVID-19: Prediction and control. Chaos Soliton. Fract. 2020, 136,109889. [CrossRef]
- Martinez-Rodriguez, D.; Gonzalez-Parra, G.; Villanueva, R-J. Analysis of key factors of a SARS-CoV-2 vaccination program: A mathematical modeling approach. Epidemiologia 2021, 2,140–161. [CrossRef]
- Matrajt, L.; Halloran, M.; Antia, M. Successes and failures of the live-attenuated influenza vaccine: Can we do better? Clin. Infect. Dis. 2020, 70,1029–1037. [CrossRef]
- Matrajt, L.; Eaton, J.; Leung, T.; Brown, E. Vaccine optimization for COVID-19: Who to vaccinate first? Sci. Adv. 2020, 7(6). [CrossRef]
- McDonnell, A.; Van Exan, R.; Lloyd, S.; Subramanian, L.; Chalkidou, K.; La Porta, A.; Li, J.; Maiza, E.; Reader, D.; Rosenberg, J.; Scannell, J.; Thomas, V.; Weintraub, R.; Yadav, P. COVID-19 vaccine predictions: using mathematical modelling and expert opinions to estimate timelines and probabilities of success of COVID-19 vaccines. Cent. Glob. Dev. 2020, CGD Policy Paper 183, October 2020. covid19.ariadnelabs.org.
- Mizumoto, K.; Chowell, G. Transmission potential of the novel coronavirus (COVID-19) onboard the diamond Princess Cruises Ship, 2020. Infect. Dis. Mod. 2021 5,264–270. [CrossRef]
- Moghadas, S.; Fitzpatrick, M.; Sah, P.; Pandey, A.; Shoukat, A.; Singer, B.; Galvani, A. The implications of silent transmissin for the control of COVID-19 outbreaks. Proc. Natl. Acad. Sci. USA 2020, 117,17513–17515. [CrossRef]
- Moore, S.; Hill, E.; Dyson, L.; Tildesley, M.; Keeling, M. Modelling optimal vaccination strategy for SARS-CoV-2 in the UK. PLOS Comput. Biol. 2021. [CrossRef]
- Moore, S.; Hill, E.; Tildesley, M.; Dyson, L.; Keeling, M. Vaccination and non-pharmaceutical interventions for COVID-19: A mathematical modelling study. Lancet Infect. Dis. 2021, 21(6):793-802. [CrossRef]
- Olivares, A.; Steffetti, E. Uncertainty quantification of a mathematical model of COVID-19 transmission dynamics with mass vaccination strategy. Chaos Soliton. Fract. 2021, 146:110895. [CrossRef]
- Ng V.; Fazil, A.; Waddell, L.; Turgeon, P.; Otten, A.; Ogden, N. Modelling the impact of shutdowns on resurging SARS-CoV-2 transmission in Canada. Roy. Soc. Open Sci. 2021, 8,5. [CrossRef]
- Ngonghala, C.; Iboi, E.; Eikenberry, S.; Scotch, M.; MacIntyre, C.; Bonds, M.; Gumel, A. Mathematical assessment of the impact of non-pharmaceutical interventions on curtailing the 2019 novel coronavirus. Math. Biosci. 2020, 9,108364. [CrossRef]
- Ngonghala, C.; Iboi, E.; Gumel, A. Could masks curtail the post-lockdown resurgence of covid-19 in the US? Math. Biosci. 2020, 329,108452. [CrossRef]
- Ngonghala, C; Gumel, A. Mathematical assessment of the role of vaccination against COVID-19 in the United States. Mathematical Modelling, Simulations, and AI for Emergent Pandemic Diseases Science Direct 2023, 221-249. [CrossRef]
- Noh, J.; Danuser, G. Estimation of the fraction of COVID-19 infected people in U.S. states and countries worldwide. PLoS ONE 2021, 16. [CrossRef]
- Paget, J.; Caini, S.; Cowling, B.; Esposito, S.; Falsey, A.; Gentile, A.; Kynci, J.; Macintyre, C.; Pitman, R.; Lina, B. The impact of influenza vaccination on the COVID-19 pandemic? Evidence and lessons for public health policies. Vaccine 2021, 38,6485–6486. [CrossRef]
- Paltiel, A.; Schwartz, J.; Zheng, A.; Walensky, R. Clinical outcomes of a COVID-19 vaccine: Implementation over efficacy. Health Aff. 2021, 40(1):42-52. [CrossRef]
- Peak, C.; Kahn, R.; Grad, H.; Childs, L.; Li, R.; Lipstich, M.; Buckee, C. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: a modelling study. Lancet Infect. Dis. 2020, 20,1025–1033. [CrossRef]
- Poonia, R.; Saudagar A.; Altameem, A.; Alkhathami, M.; Khan, M.; Hasanat, M. An enhanced SEIR model for prediction of COVID-19 with vaccination effect. Life 2022, 12,647. [CrossRef]
- Roosa, K.; Lee, Y.; Luo, R.; Kirpich, A.; Rothenberg, R.; Hyman, M.; Yan, P.; Chowell, G. Real-time forecasts of the COVID-19 epidemic in China from February 5th to February 24th, 2020. Infect. Dis. Mod. 2021, 5,256–263. [CrossRef]
- Rosenberg, E.; Dorabawila, V.; Easton, D.; Bauer, U.; Kumar, J.; Hoen, R.; Hoefer, D.; Wu, M.; Lutterloh,E.; Conroy, M.; Greene, D.; Zucker, H. Covid-19 effectiveness in New York State. N. Engl. J. Med. 2022, 86,116-127. [CrossRef]
- Saldana, F.; Fiores-Arguedas, H.; Camacho-Gutierrez, J.; Barradas, I. Modeling the transmission dynamics and the impact of the control interventions for the COVID-19 epidemic outbreak. Math. Biosci. Eng. 2020, 17,4165–4183. [CrossRef]
- Saldana, F.; Velasco-Hernandez, J. The trade-off between mobility and vaccination for COVID-19 control: A metapopulation modelling approach. Roy. Soc. Open Sci. 2021, 8,202240. [CrossRef]
- Shim, E.; Tariq, A.; Choi, W.; Lee, Y.; Chowell, G. Transmission potential and severity of COVID-19 in South Korea. Int. J. Infect. Dis. 2020, 93,339–344. [CrossRef]
- Shim, E. Optimal allocation of the limited COVID-19 vaccine supply in South Korea. J. Clin. Med. 2021, 10,591. [CrossRef]
- Sun, D.; Teng, Z.; Wang, K.; Zhang, T. Stability and Hopf bifurcation in delayed age-structured SVIR epidemic model with vaccination and incubation. Chaos, Soliton. Fract. 2023, 168,113206. [CrossRef]
- Sung-mok, J.; Akira, E.; Ryo, K.; Hiroshi, N. Projecting a second wave of COVID-19 in Japan with variable interventions in high-risk settings. Roy. Soc. Open Sci. 2021, 8:202169. [CrossRef]
- Tang, B.; Bragazzi, N.; Li, Q.; Tang, S.; Xiao, Y.; Wu, J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect. Dis. Mod. 2021 5,248–255. [CrossRef]
- Tang, B.; Zhang, X.; Li, Q.; Bragazzi, N.; Golemi-Kotra, D.; Wu, J. The minimal COVID-19 vaccination coverage and efficacy to compensate for a potential increase of transmission contacts, and increased transmission probability of the emerging strains. .BMC Public Health 2022, 22,1258. [CrossRef]
- Tang, J.; Jin, Z.; Wang, L.; Xu, F. A note on an age-of-infection SVIR model with nonlinear incidence. Int. J. Biomath. 10,05, 750064. [CrossRef]
- Tariq, A.; Lee, L.; Roosa, K.; Blumberg, S.; Yan, P.; Ma, S.; Chowell, G. Real-time monitoring the transmission potential of COVID-19 in Singapore. BMC Med. 2020, 18,1–14. [CrossRef]
- Troiano, G.; Nordi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194,245-251. [CrossRef]
- Thunstrom, L.; Ashworth, M.; Newbold, S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. SSRN Elect. J. 2020. [CrossRef]
- Thurmer, S.; Klimek, P.; Hanel, R. A network-based explanation of why most covid-19 infection curves are linear. Proc. Natl. Acad. Sci. USA 2020, 17,22684–22689. [CrossRef]
- Usherwood, T.; LaJoie, Z.; Srivastava, V. c. Sci. Rep. 2021, 11(1):12051. [CrossRef]
- Waku, J.; Oshinubi, K.; Adam, U.; Demongeot, J. Forecasting the endemic/epidemic transition in COVID-19 in some countries: Influence of the vaccination. Nature 2023 11,135. [CrossRef]
- Wang, J.; Zhang, R; Kuniya, I. The dynamics of an SVIR epidemiological model with infection age. IMA J. Appl. Math. 2016, 81,2,321-343. [CrossRef]
- Wang, J.; Lang, J.;Chen, Y. Global threshold dynamics of an SVIR model with age-dependent infection and relapse. J. Biol. Dyn. 2017, 11,1850068. [CrossRef]
- Wang, C..; Fan, D; Xia, L.; Yi, X. Global stability for a multi-group SIVR model with age of vaccination. Int. J. Biomath. 2018, 11,05,1850068. [CrossRef]
- Wang, Z.; Muecksch, F.; Schaefer-Babajew, D.; Finkin, S.; Viant, C.; Gaebler, C.; Hoffman, H.; Barnes, C.; Cipolla, M.; Ramos, V.; Oliveira T.; Cho A.; Schmidt F.; Da Silva J.; Bednarski E.; Aguado L.; Yee J.; Daga M.; Turroja M.; Millard K.; Jankovic M.; Gazumyan A.; Zhao Z.; Rice C.; Bieniasz P.; Caskey M.; Hatziioannou T.; Nussenzweig M. Naturally enhanced neutralising breadth against SARS-CoV-2 one year after infection. Nature 2021, 595(7867):426-431. [CrossRef]
- Wang, S.; Wu, Y.; Li, L.; Li, Y.; Sun, G. Forecast for peak infections in the second wave of the Omicron after the adjustment of zero-COVID policy in the mainland of China. Infect. Dis. Rep. 2023, 8 562-573. [CrossRef]
- Webb, G. A COVID-19 epidemic model predicting the effectiveness of vaccination. Math. Appl. Sci. Eng. 2021, 2(2):1-15. [CrossRef]
- Webb, G. A COVID-19 epidemic model predicting the effectiveness of vaccination in the US. Infect. Dis. Rep. 2021, 13,654-657. [CrossRef]
- Wilder, B.; Champignon, M.; Killian, J.; Ou, H-C.; Mate, A.; Jabbari, S.; Perrault, A.; Desai, A.; Taube, M.; Majumder, M. Modelling between-population variation in COVID-19 dynamics in Hubei, Lombardy, and New York City. Proc. Natl. Acad. Sci. USA 2020, 117,25904–25910. [CrossRef]
- Xing, Y.; Li, H. Almost periodic solutions for a SVIR epidemic model with relapse. Math. Bios. Eng. 2021, 18,6,7191-7217. [CrossRef]
- Xue, L.; Jing, S.; Miller, J.; Sun, W.; Li, H.; Estrada-Franco, J.; Hyman, J.; Zhu, H. A data-driven network model for the emerging covid-19 epidemics in Wuhan, Toronto and Italy. Math. Biosci. 2020, 326,108391. [CrossRef]
- Yang, J.; Yang, L.; Jin, Z. Optimal strategies of the age-specific vaccination and antiviral treatment against influenza. Chaos Soliton. Fract. 2023, 68,113199. [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



