Submitted:
22 November 2023
Posted:
23 November 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Copper Metabolism
1.1.1. Copper Uptake
1.1.2. Copper Distribution
1.1.3. Copper Excretion
1.2. Copper Homeostasis
1.3. Copper and Pathogenesis
1.3.1. Copper and Cell Proliferation
1.3.2. Copper and Angiogenesis
1.3.3. Copper and Metastasis
2. Copper in Gynecological Diseases
2.1. Ovarian Diseases
2.1.1. Ovarian Cancer
2.1.2. Polycystic Ovary Syndrome
2.2. Uterine Diseases
2.2.1. Uterine Cervix Cancer
2.2.2. Endometrial Cancer
2.2.3. Benign’ Diseases
3. Therapeutic Strategies
3.1. Copper Chelators
3.1.1. D-penicillamine
3.1.2. Trientine
3.1.3. Tetrathiomolybdate
| Disease | Trial Phase | Intervention | Trial ID | Status | Study completion |
|---|---|---|---|---|---|
| Breast Cancer | Phase 2 | TM | NCT00195091 | Active, not recruiting |
2025/06 |
| Wilson’s Disease | Phase 2 | ALXN1840 | NCT04422431 | Completed | 2023/05 |
| EOC, TC, PPC | Phase 1-2 | Trientine 2HC + PLD + carboplatin |
NCT03480750 | Completed | 2019/12 |
| Advanced cancers | Phase 1 | Trientine 4HC + carboplatin |
NCT01178112 | Completed | 2014/08 |
| EOC, TC, PPC | Phase 2 | Elesclomol + paclitaxel | NCT00888615 | Completed | 2016/08 |
| CC | Phase 2 | 64CuII(atsm) | NCT00794339 | Termined | 2011/12 |
| CIN | Phase 2 | Curcumin | NCT04266275 | Not yet recruiting |
2025/03 |
| CC | Phase 1-2 | Curcumin + radiotherapy |
NCT05947513 | Not yet recruiting |
2024/11 |
| CC | Phase 2 | Curcumin | NCT04294836 | Withdrawn | 2023/12 |
| EDT | Phase 2 | Curcumin | NCT04493476 | Unknown status |
2022/12 |
| CC, EC | Phase 2 | Pembrolizumab + radiation + curcumin + immune modulatory cocktail |
NCT03192059 | Completed | 2021/06 |
| EC | Phase 2 | Curcumin | NCT02017353 | Completed | 2016/10 |
3.2. Copper Ionophores
3.2.1. Disulfiram and Dithiocarbamates
3.2.2. Clioquinol
3.2.3. Elesclomol and Derivatives
3.2.4. Bis(thiosemicarbazones)
3.3. New Therapeutic Strategies
3.3.1. Cu-Based Nanoparticles
3.3.2. Natural Compounds Derived from Plants
Curcumin
Coumarins
4. Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Akt | Protein kinase B |
| ALDH | Aldehyde dehydrogenase |
| ALXN1840 | Bis-choline tetrathiomolybdate |
| ARID1A | AT-rich interactive domain-containing protein 1A |
| Arp | Actin-related proteins |
| ATOX1 | Antioxidant chaperone 1 |
| ATP7A | Copper-transporting ATPase alpha |
| ATP7B | Copper-transporting ATPase beta |
| BRAF | Serine/threonine-protein kinase B-raf |
| CA-9 | Carbonic anhydrase 9 |
| Cas9 | CRISPR-associated protein 9 |
| CC | Cervical cancer |
| CCDC | Coiled-coil domain containing protein |
| CCS | Copper chaperone for superoxide dismutase |
| CD31 | Cluster of differentiation 31 |
| CDDP | Cisplatin |
| CIN | Cervical intraepithelial neoplasia |
| CMRGs | Copper-metabolism related genes |
| COMMD | Copper metabolism MURR1 domain-containing protein |
| CCO | Cytochrome C oxidase |
| COX11 | CCO copper chaperone 11 |
| COX17 | CCO copper chaperone 17 |
| COX19 | CCO assembly factor 19 |
| Cp | Ceruloplasmin |
| CRISPR | Clustered regularly interspaced short palindromic repeats |
| CTR1 | Copper transporter 1 |
| CTR2 | Copper transporter 2 |
| Cu | Copper |
| CXCR | C-X-C motif chemokine receptor |
| DβH | Dopamine-β-hydroxylase |
| DCYTB | Duodenal cytochrome B |
| DHA | Docosahexaenoic acid |
| DMT1 | Divalent metal transporter 1 |
| DSF | Disulfiram |
| EC | Endometrial cancer |
| ECM | Extracellular matrix |
| EDT | Endometriosis |
| EGFR | Epidermal growth factor receptor |
| EMT | Epithelial-mesenchymal transition |
| EOC | Epithelial ovarian cancer |
| ERK | Extracellular signal-regulated kinase |
| FDX1 | Ferredoxin-1 |
| FGF | Fibroblast growth factor |
| GSH | Glutathione |
| HIF-1α | Hypoxia-inducible factor 1-alpha |
| HO-1 | Heme oxygenase 1 |
| HOMA-IR | Homeostatic model assessment for insulin resistance |
| HPV | Human papillomavirus |
| HREs | Hypoxia response elements |
| ICAM | Intercellular adhesion molecule |
| IKKs | Inhibitory kappa B kinases |
| IL | Interleukin |
| IMS | Mitochondrial intermembrane space |
| IR | Insulin resistance |
| JNK | c-Jun N-terminal kinase |
| LC3 | Microtubule-associated protein light chain 3 |
| LDH | Lactate dehydrogenase |
| LOX | Lysyl oxidase |
| LOXL | LOX-like proteins |
| MAPK | Mitogen-activated protein kinase |
| MCP-1 | Monocyte chemoattractant protein-1 |
| MEK | Mitogen-activated protein kinase kinase |
| MEMO1 | Mediator of cell motility 1 |
| MMP | Matrix metalloproteinase |
| MT | Metallothionein |
| MTF1 | Metal-regulatory transcription factor 1 |
| NADPH | Nicotinamide adenine dinucleotide phosphate |
| NF-κB | Nuclear factor kappa B |
| NO | Nitric oxide |
| NPs | Nanoparticles |
| Nrf2 | Nuclear factor erythroid 2-related factor 2 |
| NSAID | Non-steroidal anti-inflammatory drug |
| OC | Ovarian cancer |
| p53 | Tumor protein p53 |
| PARP | Poly (ADP-ribose) polymerase |
| PBT2 | 5,7-dichloro-2-[(dimethylamino)methyl]-8-hydroxyquinoline |
| PCOS | Polycystic ovary syndrome |
| PDGF | Platelet-derived growth factor |
| PI3K | Phosphoinositide 3-kinase |
| PLD | Pegylated liposomal doxorubicin |
| PPAR | Peroxisome proliferator-activated receptor |
| RAF | Rapidly accelerated fibrosarcoma |
| ROS | Reactive oxygen species |
| SCO1 | Synthesis of cytochrome C oxidase 1 |
| SDF-1 | Stromal cell-derived factor 1 |
| SOD | Superoxide dismutase |
| STAT | Signal transducer and activator of transcription |
| STEAP | Six-transmembrane epithelial antigen of the prostate |
| TCA | Tricarboxylic acid |
| TGF-β | Transforming growth factor beta |
| TGN | Trans-Golgi network |
| TM | Ammonium tetrathiomolybdate |
| TMD | Transmembrane domain |
| TNF | Tumor necrosis factor |
| TNFR | TNF receptor |
| TRAMP | Transgenic adenocarcinoma of the mouse prostate |
| ULK | Unc-51 like autophagy activating kinase |
| VCAM | Vascular cell adhesion protein |
| VEGF | Vascular endothelial growth factor |
| VEGFR | VEGF receptor |
| WASH | Wiskott–Aldrich syndrome protein and SCAR homolog |
| XIAP | X-linked inhibitor of apoptosis protein |
References
- Nevitt, T.; Öhrvik, H.; Thiele, D.J. Charting the Travels of Copper in Eukaryotes from Yeast to Mammals. Biochim. Biophys. Acta (BBA)-Molecular Cell Res. 2012, 1823, 1580–1593. [CrossRef]
- Trumbo, P.; Yates, A.A.; Schlicker, S.; Poos, M. Dietary Reference Intakes. J. Am. Diet. Assoc. 2001, 101, 294–301. [CrossRef]
- Moshfegh, A.J.; Goldman, J.D.; Rhodes, D.G.; Friday, J.E. Usual Nutrient Intake from Food and Beverages, by Gender and Age, What We Eat in America, NHANES 2017-March 2020 Prepandemic; 2023.
- Myint, Z.W.; Oo, T.H.; Thein, K.Z.; Tun, A.M.; Saeed, H. Copper Deficiency Anemia. Ann. Hematol. 2018, 97, 1527–1534. [CrossRef]
- Grochowski, C.; Blicharska, E.; Baj, J.; Mierzwińska, A.; Brzozowska, K.; Forma, A.; Maciejewski, R. Serum Iron, Magnesium, Copper, and Manganese Levels in Alcoholism: A Systematic Review. Molecules 2019, 24, 1361. [CrossRef]
- Feng, Y.; Zeng, J.-W.; Ma, Q.; Zhang, S.; Tang, J.; Feng, J.-F. Serum Copper and Zinc Levels in Breast Cancer: A Meta-Analysis. J. Trace Elem. Med. Biol. 2020, 62. [CrossRef]
- Linder, M.C. Ceruloplasmin and Other Copper Binding Components of Blood Plasma and Their Functions: An Update. Metallomics 2016, 8, 887–905. [CrossRef]
- Tsang, T.; Davis, C.I.; Brady, D.C. Copper Biology. Curr. Biol. 2021, 31, R421–R427. [CrossRef]
- Shi, H.; Jiang, Y.; Yang, Y.; Peng, Y.; Li, C. Copper Metabolism in Saccharomyces Cerevisiae: An Update. Biometals 2021, 34, 3–14. [CrossRef]
- Ge, E.J.; Bush, A.I.; Casini, A.; Cobine, P.A.; Cross, J.R.; DeNicola, G.M.; Dou, Q.P.; Franz, K.J.; Gohil, V.M.; Gupta, S.; et al. Connecting Copper and Cancer: From Transition Metal Signalling to Metalloplasia. Nat. Rev. Cancer 2022, 22, 102–113. [CrossRef]
- Grubman, A.; White, A.R. Copper as a Key Regulator of Cell Signalling Pathways. Expert Rev. Mol. Med. 2014, 16. [CrossRef]
- Shanbhag, V.C.; Gudekar, N.; Jasmer, K.; Papageorgiou, C.; Singh, K.; Petris, M.J. Copper Metabolism as a Unique Vulnerability in Cancer. Biochim. Biophys. Acta (BBA)-Molecular Cell Res. 2021, 1868, 118893. [CrossRef]
- Shawki, A.; Anthony, S.R.; Nose, Y.; Engevik, M.A.; Niespodzany, E.J.; Barrientos, T.; Öhrvik, H.; Worrell, R.T.; Thiele, D.J.; Mackenzie, B. Intestinal DMT1 Is Critical for Iron Absorption in the Mouse but Is Not Required for the Absorption of Copper or Manganese. Am. J. Physiol. Liver Physiol. 2015, 309, G635–G647. [CrossRef]
- Wyman, S.; Simpson, R.J.; McKie, A.T.; Sharp, P.A. Dcytb (Cybrd1) Functions as Both a Ferric and a Cupric Reductase in Vitro. FEBS Lett. 2008, 582, 1901–1906. [CrossRef]
- Ozumi, K.; Sudhahar, V.; Kim, H.W.; Chen, G.-F.; Kohno, T.; Finney, L.; Vogt, S.; McKinney, R.D.; Ushio-Fukai, M.; Fukai, T. Role of Copper Transport Protein Antioxidant 1 in Angiotensin II–Induced Hypertension: A Key Regulator of Extracellular Superoxide Dismutase. Hypertension 2012, 60, 476–486. [CrossRef]
- Nose, Y.; Wood, L.K.; Kim, B.-E.; Prohaska, J.R.; Fry, R.S.; Spears, J.W.; Thiele, D.J. Ctr1 Is an Apical Copper Transporter in Mammalian Intestinal Epithelial Cells in Vivo That Is Controlled at the Level of Protein Stability. J. Biol. Chem. 2010, 285, 32385–32392. [CrossRef]
- Zimnicka, A.M.; Maryon, E.B.; Kaplan, J.H. Human Copper Transporter HCTR1 Mediates Basolateral Uptake of Copper into Enterocytes: Implications for Copper Homeostasis. J. Biol. Chem. 2007, 282, 26471–26480. [CrossRef]
- Galler, T.; Lebrun, V.; Raibaut, L.; Faller, P.; Wezynfeld, N.E. How Trimerization of CTR1 N-Terminal Model Peptides Tunes Cu-Binding and Redox-Chemistry. Chem. Commun. 2020, 56, 12194–12197. [CrossRef]
- Schushan, M.; Barkan, Y.; Haliloglu, T.; Ben-Tal, N. Cα-Trace Model of the Transmembrane Domain of Human Copper Transporter 1, Motion and Functional Implications. Proc. Natl. Acad. Sci. USA 2010, 107, 10908–10913. [CrossRef]
- Nose, Y.; Kim, B.-E.; Thiele, D.J. Ctr1 Drives Intestinal Copper Absorption and Is Essential for Growth, Iron Metabolism, and Neonatal Cardiac Function. Cell Metab. 2006, 4, 235–244. [CrossRef]
- Kuo, Y.-M.; Zhou, B.; Cosco, D.; Gitschier, J. The Copper Transporter CTR1 Provides an Essential Function in Mammalian Embryonic Development. Proc. Natl. Acad. Sci. USA 2001, 98, 6836–6841. [CrossRef]
- Lelièvre, P.; Sancey, L.; Coll, J.-L.; Deniaud, A.; Busser, B. The Multifaceted Roles of Copper in Cancer: A Trace Metal Element with Dysregulated Metabolism, but Also a Target or a Bullet for Therapy. Cancers 2020, 12, 3594. [CrossRef]
- Lutsenko, S.; Barnes, N.L.; Bartee, M.Y.; Dmitriev, O.Y. Function and Regulation of Human Copper-Transporting ATPases. Physiol. Rev. 2007, 87, 1011–1046. [CrossRef]
- Chen, L.; Min, J.; Wang, F. Copper Homeostasis and Cuproptosis in Health and Disease. Signal Transduct. Target. Ther. 2022, 7, 378. [CrossRef]
- Ramos, D.; Mar, D.; Ishida, M.; Vargas, R.; Gaite, M.; Montgomery, A.; Linder, M.C. Mechanism of Copper Uptake from Blood Plasma Ceruloplasmin by Mammalian Cells. PLoS ONE 2016, 11, e0149516. [CrossRef]
- Moriya, M.; Ho, Y.-H.; Grana, A.; Nguyen, L.; Alvarez, A.; Jamil, R.; Ackland, M.L.; Michalczyk, A.; Hamer, P.; Ramos, D.; et al. Copper Is Taken up Efficiently from Albumin and A2-Macroglobulin by Cultured Human Cells by More than One Mechanism. Am. J. Physiol. Physiol. 2008, 295, C708–C721. [CrossRef]
- Pierson, H.; Yang, H.; Lutsenko, S. Copper Transport and Disease: What Can We Learn from Organoids? Annu. Rev. Nutr. 2019, 39, 75–94. [CrossRef]
- Heaton, D.N.; George, G.N.; Garrison, G.; Winge, D.R. The Mitochondrial Copper Metallochaperone Cox17 Exists as an Oligomeric, Polycopper Complex. Biochemistry 2001, 40, 743–751. [CrossRef]
- Calvo, J.; Jung, H.; Meloni, G. Copper Metallothioneins. IUBMB Life 2017, 69, 236–245. [CrossRef]
- Nývltová, E.; Dietz, J. V.; Seravalli, J.; Khalimonchuk, O.; Barrientos, A. Coordination of Metal Center Biogenesis in Human Cytochrome c Oxidase. Nat. Commun. 2022, 13, 3615. [CrossRef]
- Horng, Y.-C.; Cobine, P.A.; Maxfield, A.B.; Carr, H.S.; Winge, D.R. Specific Copper Transfer from the Cox17 Metallochaperone to Both Sco1 and Cox11 in the Assembly of Yeast Cytochrome C Oxidase. J. Biol. Chem. 2004, 279, 35334–35340. [CrossRef]
- Zischka, H.; Einer, C. Mitochondrial Copper Homeostasis and Its Derailment in Wilson Disease. Int. J. Biochem. /& Cell Biol. 2018, 102, 71–75. [CrossRef]
- Skopp, A.; Boyd, S.D.; Ullrich, M.S.; Liu, L.; Winkler, D.D. Copper–Zinc Superoxide Dismutase (Sod1) Activation Terminates Interaction between Its Copper Chaperone (Ccs) and the Cytosolic Metal-Binding Domain of the Copper Importer Ctr1. Biometals 2019, 32, 695–705. [CrossRef]
- Bertinato, J.; L’Abbé, M.R. Copper Modulates the Degradation of Copper Chaperone for Cu, Zn Superoxide Dismutase by the 26 S Proteosome. J. Biol. Chem. 2003, 278, 35071–35078. [CrossRef]
- Reuter, S.; Gupta, S.C.; Chaturvedi, M.M.; Aggarwal, B.B. Oxidative Stress, Inflammation, and Cancer: How Are They Linked? Free Radic. Biol. Med. 2010, 49, 1603–1616. [CrossRef]
- Inesi, G.; Pilankatta, R.; Tadini-Buoninsegni, F. Biochemical Characterization of P-Type Copper ATPases. Biochem. J. 2014, 463, 167–176. [CrossRef]
- Jayakanthan, S.; Braiterman, L.T.; Hasan, N.M.; Unger, V.M.; Lutsenko, S. Human Copper Transporter ATP7B (Wilson Disease Protein) Forms Stable Dimers in Vitro and in Cells. J. Biol. Chem. 2017, 292, 18760–18774. [CrossRef]
- Polishchuk, E. V.; Concilli, M.; Iacobacci, S.; Chesi, G.; Pastore, N.; Piccolo, P.; Paladino, S.; Baldantoni, D.; van IJzendoorn, S.C.D.; Chan, J.; et al. Wilson Disease Protein ATP7B Utilizes Lysosomal Exocytosis to Maintain Copper Homeostasis. Dev. Cell 2014, 29, 686–700. [CrossRef]
- Hamza, I.; Prohaska, J.; Gitlin, J.D. Essential Role for Atox1 in the Copper-Mediated Intracellular Trafficking of the Menkes ATPase. Proc. Natl. Acad. Sci. USA 2003, 100, 1215–1220. [CrossRef]
- Maryon, E.B.; Molloy, S.A.; Kaplan, J.H. Cellular Glutathione Plays a Key Role in Copper Uptake Mediated by Human Copper Transporter 1. Am. J. Physiol. Physiol. 2013, 304, C768–C779. [CrossRef]
- Singleton, W.C.J.; McInnes, K.T.; Cater, M.A.; Winnall, W.R.; McKirdy, R.; Yu, Y.; Taylor, P.E.; Ke, B.-X.; Richardson, D.R.; Mercer, J.F.B.; et al. Role of Glutaredoxin1 and Glutathione in Regulating the Activity of the Copper-Transporting P-Type ATPases, ATP7A and ATP7B. J. Biol. Chem. 2010, 285, 27111–27121. [CrossRef]
- Jiang, X.; Chen, J.; Bajić, A.; Zhang, C.; Song, X.; Carroll, S.L.; Cai, Z.-L.; Tang, M.; Xue, M.; Cheng, N.; et al. Quantitative Real-Time Imaging of Glutathione. Nat. Commun. 2017, 8, 16087. [CrossRef]
- Harvey, L.J.; Ashton, K.; Hooper, L.; Casgrain, A.; Fairweather-Tait, S.J. Methods of Assessment of Copper Status in Humans: A Systematic Review. Am. J. Clin. Nutr. 2009, 89, 2009S–2024S. [CrossRef]
- Hordyjewska, A.; Popiołek, Ł.; Kocot, J. The Many “Faces” of Copper in Medicine and Treatment. Biometals 2014, 27, 611–621. [CrossRef]
- Mercer, J.F.B.; Barnes, N.; Stevenson, J.; Strausak, D.; Llanos, R.M. Copper-Induced Trafficking of the Cu-ATPases: A Key Mechanism for Copper Homeostasis. Biometals 2003, 16, 175–184. [CrossRef]
- Valko, M.; Morris, H.; Cronin, M.T.D. Metals, Toxicity and Oxidative Stress. Curr. Med. Chem. 2005, 12, 1161–1208. [CrossRef]
- Denoyer, D.; Masaldan, S.; La Fontaine, S.; Cater, M.A. Targeting Copper in Cancer Therapy: “Copper That Cancer.” Metallomics 2015, 7, 1459–1476. [CrossRef]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxid. Med. Cell. Longev. 2017, 2017. [CrossRef]
- Tosco, A.; Fontanella, B.; Danise, R.; Cicatiello, L.; Grober, O.; Ravo, M.; Weisz, A.; Marzullo, L. Molecular Bases of Copper and Iron Deficiency-Associated Dyslipidemia: A Microarray Analysis of the Rat Intestinal Transcriptome. Genes Nutr. 2010, 5, 1–8. [CrossRef]
- Bonham, M.; O’Connor, J.M.; Hannigan, B.M.; Strain, J.J. The Immune System as a Physiological Indicator of Marginal Copper Status? Br. J. Nutr. 2002, 87, 393–403. [CrossRef]
- Gaetke, L.M.; Chow-Johnson, H.S.; Chow, C.K. Copper: Toxicological Relevance and Mechanisms. Arch. Toxicol. 2014, 88, 1929–1938. [CrossRef]
- Molloy, S.A.; Kaplan, J.H. Copper-Dependent Recycling of HCTR1, the Human High Affinity Copper Transporter. J. Biol. Chem. 2009, 284, 29704–29713. [CrossRef]
- Clifford, R.J.; Maryon, E.B.; Kaplan, J.H. Dynamic Internalization and Recycling of a Metal Ion Transporter: Cu Homeostasis and CTR1, the Human Cu+ Uptake System. J. Cell Sci. 2016, 129, 1711–1721. [CrossRef]
- Liang, Z.D.; Tsai, W.-B.; Lee, M.-Y.; Savaraj, N.; Kuo, M.T. Specificity Protein 1 (Sp1) Oscillation Is Involved in Copper Homeostasis Maintenance by Regulating Human High-Affinity Copper Transporter 1 Expression. Mol. Pharmacol. 2012, 81, 455–464. [CrossRef]
- Kuo, Y.-M.; Gybina, A.A.; Pyatskowit, J.W.; Gitschier, J.; Prohaska, J.R. Copper Transport Protein (Ctr1) Levels in Mice Are Tissue Specific and Dependent on Copper Status. J. Nutr. 2006, 136, 21–26. [CrossRef]
- Öhrvik, H.; Logeman, B.; Turk, B.; Reinheckel, T.; Thiele, D.J. Cathepsin Protease Controls Copper and Cisplatin Accumulation via Cleavage of the Ctr1 Metal-Binding Ectodomain. J. Biol. Chem. 2016, 291, 13905–13916. [CrossRef]
- Logeman, B.L.; Wood, L.K.; Lee, J.; Thiele, D.J. Gene Duplication and Neo-Functionalization in the Evolutionary and Functional Divergence of the Metazoan Copper Transporters Ctr1 and Ctr2. J. Biol. Chem. 2017, 292, 11531–11546. [CrossRef]
- Chen, G.-F.; Sudhahar, V.; Youn, S.-W.; Das, A.; Cho, J.; Kamiya, T.; Urao, N.; McKinney, R.D.; Surenkhuu, B.; Hamakubo, T.; et al. Copper Transport Protein Antioxidant-1 Promotes Inflammatory Neovascularization via Chaperone and Transcription Factor Function. Sci. Rep. 2015, 5, 14780. [CrossRef]
- Itoh, S.; Kim, H.W.; Nakagawa, O.; Ozumi, K.; Lessner, S.M.; Aoki, H.; Akram, K.; McKinney, R.D.; Ushio-Fukai, M.; Fukai, T. Novel Role of Antioxidant-1 (Atox1) as a Copper-Dependent Transcription Factor Involved in Cell Proliferation. J. Biol. Chem. 2008, 283, 9157–9167. [CrossRef]
- Kamiya, T.; Takeuchi, K.; Fukudome, S.; Hara, H.; Adachi, T. Copper Chaperone Antioxidant-1, Atox-1, Is Involved in the Induction of SOD3 in THP-1 Cells. Biometals 2018, 31, 61–68. [CrossRef]
- Palmiter, R.D. Regulation of Metallothionein Genes by Heavy Metals Appears to Be Mediated by a Zinc-Sensitive Inhibitor That Interacts with a Constitutively Active Transcription Factor, MTF-1. Proc. Natl. Acad. Sci. USA 1994, 91, 1219–1223. [CrossRef]
- Song, M.O.; Mattie, M.D.; Lee, C.-H.; Freedman, J.H. The Role of Nrf1 and Nrf2 in the Regulation of Copper-Responsive Transcription. Exp. Cell Res. 2014, 322, 39–50. [CrossRef]
- Hartwig, C.; Zlatic, S.A.; Wallin, M.; Vrailas-Mortimer, A.; Fahrni, C.J.; Faundez, V. Trafficking Mechanisms of P-Type ATPase Copper Transporters. Curr. Opin. Cell Biol. 2019, 59, 24–33. [CrossRef]
- Ojha, R.; Prasad, A.N. Menkes Disease: What a Multidisciplinary Approach Can Do. J. Multidiscip. Healthc. 2016, 371–385. [CrossRef]
- Dev, S.; Kruse, R.L.; Hamilton, J.P.; Lutsenko, S. Wilson Disease: Update on Pathophysiology and Treatment. Front. Cell Dev. Biol. 2022, 10, 871877. [CrossRef]
- Członkowska, A.; Litwin, T.; Dusek, P.; Ferenci, P.; Lutsenko, S.; Medici, V.; Rybakowski, J.K.; Weiss, K.H.; Schilsky, M.L. Wilson Disease. Nat. Rev. Dis. Prim. 2018, 4, 21. [CrossRef]
- Gromadzka, G.; Tarnacka, B.; Flaga, A.; Adamczyk, A. Copper Dyshomeostasis in Neurodegenerative Diseases—Therapeutic Implications. Int. J. Mol. Sci. 2020, 21, 9259. [CrossRef]
- Gil-Bea, F.J.; Aldanondo, G.; Lasa-Fernández, H.; de Munain, A.L.; Vallejo-Illarramendi, A. Insights into the Mechanisms of Copper Dyshomeostasis in Amyotrophic Lateral Sclerosis. Expert Rev. Mol. Med. 2017, 19, e7. [CrossRef]
- Chen, X.; Cai, Q.; Liang, R.; Zhang, D.; Liu, X.; Zhang, M.; Xiong, Y.; Xu, M.; Liu, Q.; Li, P.; et al. Copper Homeostasis and Copper-Induced Cell Death in the Pathogenesis of Cardiovascular Disease and Therapeutic Strategies. Cell death /& Dis. 2023, 14, 105. [CrossRef]
- Pal, I.; Dey, S.G. The Role of Heme and Copper in Alzheimer’s Disease and Type 2 Diabetes Mellitus. JACS Au 2023, 3, 657–681. [CrossRef]
- Tang, X.; Yan, Z.; Miao, Y.; Ha, W.; Li, Z.; Yang, L.; Mi, D. Copper in Cancer: From Limiting Nutrient to Therapeutic Target. Front. Oncol. 2023, 13, 1209156. [CrossRef]
- Kong, R.; Sun, G. Targeting Copper Metabolism: A Promising Strategy for Cancer Treatment. Front. Pharmacol. 2023, 14. [CrossRef]
- Michalczyk, K.; Cymbaluk-Płoska, A. The Role of Zinc and Copper in Gynecological Malignancies. Nutrients 2020, 12, 3732. [CrossRef]
- Barresi, V.; Trovato-Salinaro, A.; Spampinato, G.; Musso, N.; Castorina, S.; Rizzarelli, E.; Condorelli, D.F. Transcriptome Analysis of Copper Homeostasis Genes Reveals Coordinated Upregulation of SLC 31A1, SCO 1, and COX 11 in Colorectal Cancer. FEBS Open Bio 2016, 6, 794–806. [CrossRef]
- Mulware, S.J. Comparative Trace Elemental Analysis in Cancerous and Noncancerous Human Tissues Using PIXE. J. Biophys. 2013, 2013. [CrossRef]
- Ishida, S.; Andreux, P.; Poitry-Yamate, C.; Auwerx, J.; Hanahan, D. Bioavailable Copper Modulates Oxidative Phosphorylation and Growth of Tumors. Proc. Natl. Acad. Sci. USA 2013, 110, 19507–19512. [CrossRef]
- Lopez, J.; Ramchandani, D.; Vahdat, L. Copper Depletion as a Therapeutic Strategy in Cancer. Met. Ions Life Sci 2019, 19, 303–330. [CrossRef]
- Zowczak, M.; Iskra, M.; Torliński, L.; Cofta, S. Analysis of Serum Copper and Zinc Concentrations in Cancer Patients. Biol. Trace Elem. Res. 2001, 82, 1–8. [CrossRef]
- Gupte, A.; Mumper, R.J. Elevated Copper and Oxidative Stress in Cancer Cells as a Target for Cancer Treatment. Cancer Treat. Rev. 2009, 35, 32–46. [CrossRef]
- Yaman, M.; Kaya, G.; Simsek, M. Comparison of Trace Element Concentrations in Cancerous and Noncancerous Human Endometrial and Ovary Tissues. Int. J. Gynecol. Cancer 2007, 17. [CrossRef]
- Zimnicka, A.M.; Tang, H.; Guo, Q.; Kuhr, F.K.; Oh, M.-J.; Wan, J.; Chen, J.; Smith, K.A.; Fraidenburg, D.R.; Choudhury, M.S.R.; et al. Upregulated Copper Transporters in Hypoxia-Induced Pulmonary Hypertension. PLoS ONE 2014, 9, e90544. [CrossRef]
- Su, Y.; Zhang, X.; Li, S.; Xie, W.; Guo, J. Emerging Roles of the Copper–CTR1 Axis in Tumorigenesis. Mol. Cancer Res. 2022, 20, 1339–1353. [CrossRef]
- Boutry, J.; Tissot, S.; Ujvari, B.; Capp, J.-P.; Giraudeau, M.; Nedelcu, A.M.; Thomas, F. The Evolution and Ecology of Benign Tumors. Biochim. Biophys. Acta (BBA)-Reviews Cancer 2022, 1877, 188643. [CrossRef]
- Li, Y.; Liang, R.; Zhang, X.; Wang, J.; Shan, C.; Liu, S.; Li, L.; Zhang, S. Copper Chaperone for Superoxide Dismutase Promotes Breast Cancer Cell Proliferation and Migration via ROS-Mediated MAPK/ERK Signaling. Front. Pharmacol. 2019, 10, 356. [CrossRef]
- Wang, J.; Luo, C.; Shan, C.; You, Q.; Lu, J.; Elf, S.; Zhou, Y.; Wen, Y.; Vinkenborg, J.L.; Fan, J.; et al. Inhibition of Human Copper Trafficking by a Small Molecule Significantly Attenuates Cancer Cell Proliferation. Nat. Chem. 2015, 7, 968–979. [CrossRef]
- Pham, V.N.; Chang, C.J. Metalloallostery and Transition Metal Signaling: Bioinorganic Copper Chemistry Beyond Active Sites. Angew. Chemie 2023, 62, e202213644. [CrossRef]
- Brady, D.C.; Crowe, M.S.; Greenberg, D.N.; Counter, C.M. Copper Chelation Inhibits BRAFV600E-Driven Melanomagenesis and Counters Resistance to BRAFV600E and MEK1/2 Inhibitors. Cancer Res. 2017, 77, 6240–6252. [CrossRef]
- Polishchuk, E. V.; Merolla, A.; Lichtmannegger, J.; Romano, A.; Indrieri, A.; Ilyechova, E.Y.; Concilli, M.; De Cegli, R.; Crispino, R.; Mariniello, M.; et al. Activation of Autophagy, Observed in Liver Tissues from Patients with Wilson Disease and from ATP7B-Deficient Animals, Protects Hepatocytes from Copper-Induced Apoptosis. Gastroenterology 2019, 156, 1173–1189. [CrossRef]
- Tsang, T.; Posimo, J.M.; Gudiel, A.A.; Cicchini, M.; Feldser, D.M.; Brady, D.C. Copper Is an Essential Regulator of the Autophagic Kinases ULK1/2 to Drive Lung Adenocarcinoma. Nat. Cell Biol. 2020, 22, 412–424. [CrossRef]
- Zhao, Y.; Adjei, A.A. Targeting Angiogenesis in Cancer Therapy: Moving beyond Vascular Endothelial Growth Factor. Oncologist 2015, 20, 660–673. [CrossRef]
- McAuslan, B.R.; Reilly, W. Endothelial Cell Phagokinesis in Response to Specific Metal Ions. Exp. Cell Res. 1980, 130, 147–157. [CrossRef]
- Urso, E.; Maffia, M. Behind the Link between Copper and Angiogenesis: Established Mechanisms and an Overview on the Role of Vascular Copper Transport Systems. J. Vasc. Res. 2015, 52, 172–196. [CrossRef]
- Feng, W.; Ye, F.; Xue, W.; Zhou, Z.; Kang, Y.J. Copper Regulation of Hypoxia-Inducible Factor-1 Activity. Mol. Pharmacol. 2009, 75, 174–182. [CrossRef]
- Kim, K.K.; Abelman, S.; Yano, N.; Ribeiro, J.R.; Singh, R.K.; Tipping, M.; Moore, R.G. Tetrathiomolybdate Inhibits Mitochondrial Complex IV and Mediates Degradation of Hypoxia-Inducible Factor-1α in Cancer Cells. Sci. Rep. 2015, 5, 14296. [CrossRef]
- Pan, Q.; Kleer, C.G.; Van Golen, K.L.; Irani, J.; Bottema, K.M.; Bias, C.; De Carvalho, M.; Mesri, E.A.; Robins, D.M.; Dick, R.D.; et al. Copper Deficiency Induced by Tetrathiomolybdate Suppresses Tumor Growth and Angiogenesis. Cancer Res. 2002, 62, 4854–4859.
- Pan, Q.; Bao, L.W.; Merajver, S.D. Tetrathiomolybdate Inhibits Angiogenesis and Metastasis through Suppression of the NFκB Signaling Cascade. Mol. Cancer Res. 2003, 1, 701–706.
- Denoyer, D.; Clatworthy, S.A.S.; Cater, M.A. Copper Complexes in Cancer Therapy. In Metal Ions in Life Sciences; 2018; Vol. 18, pp. 469–506 ISBN 9783110470734.
- Das, A.; Ash, D.; Fouda, A.Y.; Sudhahar, V.; Kim, Y.-M.; Hou, Y.; Hudson, F.Z.; Stansfield, B.K.; Caldwell, R.B.; McMenamin, M.; et al. Cysteine Oxidation of Copper Transporter CTR1 Drives VEGFR2 Signalling and Angiogenesis. Nat. Cell Biol. 2022, 24, 35–50. [CrossRef]
- Narayanan, G.; Vuyyuru, H.; Muthuvel, B.; Konerirajapuram Natrajan, S. CTR1 Silencing Inhibits Angiogenesis by Limiting Copper Entry into Endothelial Cells. PLoS ONE 2013, 8, e71982. [CrossRef]
- Kohno, T.; Urao, N.; Ashino, T.; Sudhahar, V.; McKinney, R.D.; Hamakubo, T.; Iwanari, H.; Ushio-Fukai, M.; Fukai, T. Novel Role of Copper Transport Protein Antioxidant-1 in Neointimal Formation after Vascular Injury. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 805–813. [CrossRef]
- Ash, D.; Sudhahar, V.; Youn, S.-W.; Okur, M.N.; Das, A.; O’Bryan, J.P.; McMenamin, M.; Hou, Y.; Kaplan, J.H.; Fukai, T.; et al. The P-Type ATPase Transporter ATP7A Promotes Angiogenesis by Limiting Autophagic Degradation of VEGFR2. Nat. Commun. 2021, 12, 3091. [CrossRef]
- Fukai, T.; Ushio-Fukai, M.; Kaplan, J.H. Copper Transporters and Copper Chaperones: Roles in Cardiovascular Physiology and Disease. Am. J. Physiol. Physiol. 2018, 315, C186–C201. [CrossRef]
- Dongre, A.; Weinberg, R.A. New Insights into the Mechanisms of Epithelial–Mesenchymal Transition and Implications for Cancer. Nat. Rev. Mol. cell Biol. 2019, 20, 69–84. [CrossRef]
- Li, S.; Zhang, J.; Yang, H.; Wu, C.; Dang, X.; Liu, Y. Copper Depletion Inhibits CoCl2-Induced Aggressive Phenotype of MCF-7 Cells via Downregulation of HIF-1 and Inhibition of Snail/Twist-Mediated Epithelial-Mesenchymal Transition. Sci. Rep. 2015, 5, 12410. [CrossRef]
- Xiao, Q.; Ge, G. Lysyl Oxidase, Extracellular Matrix Remodeling and Cancer Metastasis. Cancer Microenviron. 2012, 5, 261–273. [CrossRef]
- Yang, N.; Cao, D.-F.; Yin, X.-X.; Zhou, H.-H.; Mao, X.-Y. Lysyl Oxidases: Emerging Biomarkers and Therapeutic Targets for Various Diseases. Biomed. /& Pharmacother. 2020, 131, 110791. [CrossRef]
- El-Haibi, C.P.; Bell, G.W.; Zhang, J.; Collmann, A.Y.; Wood, D.; Scherber, C.M.; Csizmadia, E.; Mariani, O.; Zhu, C.; Campagne, A.; et al. Critical Role for Lysyl Oxidase in Mesenchymal Stem Cell-Driven Breast Cancer Malignancy. Proc. Natl. Acad. Sci. USA 2012, 109, 17460–17465. [CrossRef]
- Barker, H.E.; Chang, J.; Cox, T.R.; Lang, G.; Bird, D.; Nicolau, M.; Evans, H.R.; Gartland, A.; Erler, J.T. LOXL2-Mediated Matrix Remodeling in Metastasis and Mammary Gland Involution. Cancer Res. 2011, 71, 1561–1572. [CrossRef]
- Osawa, T.; Ohga, N.; Akiyama, K.; Hida, Y.; Kitayama, K.; Kawamoto, T.; Yamamoto, K.; Maishi, N.; Kondoh, M.; Onodera, Y.; et al. Lysyl Oxidase Secreted by Tumour Endothelial Cells Promotes Angiogenesis and Metastasis. Br. J. Cancer 2013, 109, 2237–2247. [CrossRef]
- Semenza, G.L. Molecular Mechanisms Mediating Metastasis of Hypoxic Breast Cancer Cells. Trends Mol. Med. 2012, 18, 534–543. [CrossRef]
- Pez, F.; Dayan, F.; Durivault, J.; Kaniewski, B.; Aimond, G.; Le Provost, G.S.; Deux, B.; Clézardin, P.; Sommer, P.; Pouysségur, J.; et al. The HIF-1–Inducible Lysyl Oxidase Activates HIF-1 via the Akt Pathway in a Positive Regulation Loop and Synergizes with HIF-1 in Promoting Tumor Cell Growth. Cancer Res. 2011, 71, 1647–1657. [CrossRef]
- MacDonald, G.; Nalvarte, I.; Smirnova, T.; Vecchi, M.; Aceto, N.; Doelemeyer, A.; Frei, A.; Lienhard, S.; Wyckoff, J.; Hess, D.; et al. Memo Is a Copper-Dependent Redox Protein with an Essential Role in Migration and Metastasis. Sci. Signal. 2014, 7, ra56. [CrossRef]
- Lukanović, D.; Herzog, M.; Kobal, B.; Černe, K. The Contribution of Copper Efflux Transporters ATP7A and ATP7B to Chemoresistance and Personalized Medicine in Ovarian Cancer. Biomed. /& Pharmacother. 2020, 129, 110401. [CrossRef]
- Mok, S.C.; Wong, K.K.; Lu, K.H.; Munger, K.; Nagymanyoki, Z. Molecular Basis of Gynecologic Diseases. In Essential Concepts in Molecular Pathology; Elsevier, 2020; pp. 409–424 ISBN 9780128132579.
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2021, 71, 209–249. [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2022. CA. Cancer J. Clin. 2022, 72, 7–33. [CrossRef]
- Wang, Q.; Peng, H.; Qi, X.; Wu, M.; Zhao, X. Targeted Therapies in Gynecological Cancers: A Comprehensive Review of Clinical Evidence. Signal Transduct. Target. Ther. 2020, 5, 137. [CrossRef]
- Savant, S.S.; Sriramkumar, S.; O’Hagan, H.M. The Role of Inflammation and Inflammatory Mediators in the Development, Progression, Metastasis, and Chemoresistance of Epithelial Ovarian Cancer. Cancers (Basel). 2018, 10, 251. [CrossRef]
- Ritch, S.J.; Telleria, C.M. The Transcoelomic Ecosystem and Epithelial Ovarian Cancer Dissemination. Front. Endocrinol. (Lausanne). 2022, 13, 886533. [CrossRef]
- Nayak, S.B.; Bhat, V.R.; Mayya, S.S. Serum Copper, Ceruloplasmin and Thiobarbituric Acid Reactive Substance Status in Patients with Ovarian Cancer. Indian J. Physiol. Pharmacol. 2004, 48, 486–488.
- Korun, Z.E.U.; Erdem, M.; Erdem, A.; Onan, A.; Bozkurt, N.; Öktem, M.; Biberoğlu, K. Use of Serum Copper and Zinc Levels in the Diagnostic Evaluation of Endometrioma and Epithelial Ovarian Carcinoma. Česká Gynekol. 2023, 88. [CrossRef]
- Lin, S.; Yang, H. Ovarian Cancer Risk According to Circulating Zinc and Copper Concentrations: A Meta-Analysis and Mendelian Randomization Study. Clin. Nutr. 2021, 40, 2464–2468. [CrossRef]
- Zhao, S.; Zhang, X.; Gao, F.; Chi, H.; Zhang, J.; Xia, Z.; Cheng, C.; Liu, J. Identification of Copper Metabolism-Related Subtypes and Establishment of the Prognostic Model in Ovarian Cancer. Front. Endocrinol. (Lausanne). 2023, 14, 1145797. [CrossRef]
- González-Martín, A.; Harter, P.; Leary, A.; Lorusso, D.; Miller, R.E.; Pothuri, B.; Ray-Coquard, I.; Tan, D.S.P.; Bellet, E.; Oaknin, A.; et al. Newly Diagnosed and Relapsed Epithelial Ovarian Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2023, 34, 833–848. [CrossRef]
- Christie, E.L.; Bowtell, D.D.L. Acquired Chemotherapy Resistance in Ovarian Cancer. Ann. Oncol. 2017, 28, viii13–viii15. [CrossRef]
- Pignata, S.; Pisano, C.; Di Napoli, M.; Cecere, S.C.; Tambaro, R.; Attademo, L. Treatment of Recurrent Epithelial Ovarian Cancer. Cancer 2019, 125, 4609–4615. [CrossRef]
- Katano, K.; Kondo, A.; Safaei, R.; Holzer, A.; Samimi, G.; Mishima, M.; Kuo, Y.-M.; Rochdi, M.; Howell, S.B. Acquisition of Resistance to Cisplatin Is Accompanied by Changes in the Cellular Pharmacology of Copper. Cancer Res. 2002, 62, 6559–6565.
- Ishida, S.; McCormick, F.; Smith-McCune, K.; Hanahan, D. Enhancing Tumor-Specific Uptake of the Anticancer Drug Cisplatin with a Copper Chelator. Cancer Cell 2010, 17, 574–583. [CrossRef]
- Lee, Y.-Y.; Choi, C.H.; Do, I.-G.; Song, S.Y.; Lee, W.; Park, H.S.; Song, T.J.; Kim, M.K.; Kim, T.-J.; Lee, J.-W.; et al. Prognostic Value of the Copper Transporters, CTR1 and CTR2, in Patients with Ovarian Carcinoma Receiving Platinum-Based Chemotherapy. Gynecol. Oncol. 2011, 122, 361–365. [CrossRef]
- Samimi, G.; Safaei, R.; Katano, K.; Holzer, A.K.; Rochdi, M.; Tomioka, M.; Goodman, M.; Howell, S.B. Increased Expression of the Copper Efflux Transporter ATP7A Mediates Resistance to Cisplatin, Carboplatin, and Oxaliplatin in Ovarian Cancer Cells. Clin. Cancer Res. 2004, 10, 4661–4669. [CrossRef]
- Dolgova, N. V.; Nokhrin, S.; Yu, C.H.; George, G.N.; Dmitriev, O.Y. Copper Chaperone Atox1 Interacts with the Metal-Binding Domain of Wilson’s Disease Protein in Cisplatin Detoxification. Biochem. J. 2013, 454, 147–156. [CrossRef]
- Palm-Espling, E.M.; Lundin, C.; Bjorn, E.; Naredi, P.; Wittung-Stafshede, P. Interaction between the Anticancer Drug Cisplatin and the Copper Chaperone Atox1 in Human Melanoma Cells. Protein Pept. Lett. 2014, 21, 63–68. [CrossRef]
- Bompiani, K.M.; Tsai, C.-Y.; Achatz, F.P.; Liebig, J.K.; Howell, S.B. Copper Transporters and Chaperones CTR1, CTR2, ATOX1, and CCS as Determinants of Cisplatin Sensitivity. Metallomics 2016, 8, 951–962. [CrossRef]
- Siddiqui, S.; Mateen, S.; Ahmad, R.; Moin, S. A Brief Insight into the Etiology, Genetics, and Immunology of Polycystic Ovarian Syndrome (PCOS). J. Assist. Reprod. Genet. 2022, 39, 2439–2473. [CrossRef]
- Kiel, I.A.; Lionett, S.; Parr, E.B.; Jones, H.; Røset, M.A.H.; Salvesen, Ø.; Vanky, E.; Moholdt, T. Improving Reproductive Function in Women with Polycystic Ovary Syndrome with High-Intensity Interval Training (IMPROV-IT): Study Protocol for a Two-Centre, Three-Armed Randomised Controlled Trial. BMJ Open 2020, 10, e034733. [CrossRef]
- Wang, Z.; Zhai, D.; Zhang, D.; Bai, L.; Yao, R.; Yu, J.; Cheng, W.; Yu, C. Quercetin Decreases Insulin Resistance in a Polycystic Ovary Syndrome Rat Model by Improving Inflammatory Microenvironment. Reprod. Sci. 2017, 24, 682–690. [CrossRef]
- Torshizi, F.F.; Chamani, M.; Khodaei, H.R.; Sadeghi, A.A.; Hejazi, S.H.; Heravi, R.M. Therapeutic Effects of Organic Zinc on Reproductive Hormones, Insulin Resistance and MTOR Expression, as a Novel Component, in a Rat Model of Polycystic Ovary Syndrome. Iran. J. Basic Med. Sci. 2020, 23, 36. [CrossRef]
- Palomba, S.; De Wilde, M.A.; Falbo, A.; Koster, M.P.H.; La Sala, G.B.; Fauser, B.C.J.M. Pregnancy Complications in Women with Polycystic Ovary Syndrome. Hum. Reprod. Update 2015, 21, 575–592. [CrossRef]
- Naderpoor, N.; Shorakae, S.; Joham, A.; Boyle, J.; De Courten, B.; Teede, H.J. Obesity and Polycystic Ovary Syndrome. Minerva Endocrinol. 2014, 40, 37–51.
- Chen, C.; Jing, G.; Li, Z.; Juan, S.; Bin, C.; Jie, H. Insulin Resistance and Polycystic Ovary Syndrome in A Chinese Population. Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2017. [CrossRef]
- Ollila, M.-M.; West, S.; Keinänen-Kiukaanniemi, S.; Jokelainen, J.; Auvinen, J.; Puukka, K.; Ruokonen, A.; Järvelin, M.-R.; Tapanainen, J.S.; Franks, S.; et al. Overweight and Obese but Not Normal Weight Women with PCOS Are at Increased Risk of Type 2 Diabetes Mellitus—A Prospective, Population-Based Cohort Study. Hum. Reprod. 2017, 32, 423–431. [CrossRef]
- Berni, T.R.; Morgan, C.L.; Rees, D.A. Women with Polycystic Ovary Syndrome Have an Increased Risk of Major Cardiovascular Events: A Population Study. J. Clin. Endocrinol. /& Metab. 2021, 106, e3369–e3380. [CrossRef]
- Barry, J.A.; Azizia, M.M.; Hardiman, P.J. Risk of Endometrial, Ovarian and Breast Cancer in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Hum. Reprod. Update 2014, 20, 748–758. [CrossRef]
- Joham, A.E.; Norman, R.J.; Stener-Victorin, E.; Legro, R.S.; Franks, S.; Moran, L.J.; Boyle, J.; Teede, H.J. Polycystic Ovary Syndrome. Lancet Diabetes /& Endocrinol. 2022, 10, 668–680. [CrossRef]
- Günalan, E.; Yaba, A.; Yılmaz, B. The Effect of Nutrient Supplementation in the Management of Polycystic Ovary Syndrome-Associated Metabolic Dysfunctions: A Critical Review. J. Turkish Ger. Gynecol. Assoc. 2018, 19, 220–232. [CrossRef]
- Dapas, M.; Lin, F.T.J.; Nadkarni, G.N.; Sisk, R.; Legro, R.S.; Urbanek, M.; Hayes, M.G.; Dunaif, A. Distinct Subtypes of Polycystic Ovary Syndrome with Novel Genetic Associations: An Unsupervised, Phenotypic Clustering Analysis. PLoS Med. 2020, 17, e1003132. [CrossRef]
- Jiang, Q.; Zhang, F.; Han, L.; Zhu, B.; Liu, X. Serum Copper Level and Polycystic Ovarian Syndrome: A Meta-Analysis. Gynecol. Obstet. Invest. 2021, 86, 239–246. [CrossRef]
- Yin, J.; Hong, X.; Ma, J.; Bu, Y.; Liu, R. Serum Trace Elements in Patients with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front. Endocrinol. (Lausanne). 2020, 11, 572384. [CrossRef]
- Mohmmed, A.H.; Awad, N.A.; AL-Fartosy, A.J.M. Study of Trace Elements Selenium, Copper, Zinc and Manganese Level in Polycystic Ovary Syndrome (PCOS). Int. J. Res. Appl. Sci. Biotechnol. 2019, 6, 16–22.
- Kanafchian, M.; Esmaeilzadeh, S.; Mahjoub, S.; Rahsepar, M.; Ghasemi, M. Status of Serum Copper, Magnesium, and Total Antioxidant Capacity in Patients with Polycystic Ovary Syndrome. Biol. Trace Elem. Res. 2020, 193, 111–117. [CrossRef]
- Sun, Y.; Wang, W.; Guo, Y.; Zheng, B.; Li, H.; Chen, J.; Zhang, W. High Copper Levels in Follicular Fluid Affect Follicle Development in Polycystic Ovary Syndrome Patients: Population-Based and in Vitro Studies. Toxicol. Appl. Pharmacol. 2019, 365, 101–111. [CrossRef]
- Li, M.; Tang, Y.; Lin, C.; Huang, Q.; Lei, D.; Hu, Y. Serum Macroelement and Microelement Concentrations in Patients with Polycystic Ovary Syndrome: A Cross-Sectional Study. Biol. Trace Elem. Res. 2017, 176, 73–80. [CrossRef]
- Spritzer, P.M.; Lecke, S.B.; Fabris, V.C.; Ziegelmann, P.K.; Amaral, L. Blood Trace Element Concentrations in Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis. Biol. Trace Elem. Res. 2017, 175, 254–262. [CrossRef]
- Zheng, G.; Wang, L.; Guo, Z.; Sun, L.; Wang, L.; Wang, C.; Zuo, Z.; Qiu, H. Association of Serum Heavy Metals and Trace Element Concentrations with Reproductive Hormone Levels and Polycystic Ovary Syndrome in a Chinese Population. Biol. Trace Elem. Res. 2015, 167, 1–10. [CrossRef]
- Celik, C.; Bastu, E.; Abali, R.; Alpsoy, S.; Guzel, E.C.; Aydemir, B.; Yeh, J. The Relationship between Copper, Homocysteine and Early Vascular Disease in Lean Women with Polycystic Ovary Syndrome. Gynecol. Endocrinol. 2013, 29, 488–491. [CrossRef]
- Mehde, A.A.; Resan, A.K. Study of Several Biochemical Features in Sera of Patients with Polycystic Ovaries and Compared with the Control Group. Aust. J. Basic Appl. Sci. 2014, 8, 620–627.
- Sharif, M.E.; Adam, I.; Ahmed, M.A.; Rayis, D.A.; Hamdan, H.Z. Serum Level of Zinc and Copper in Sudanese Women with Polycystic Ovarian Syndrome. Biol. Trace Elem. Res. 2017, 180, 23–27. [CrossRef]
- Khalaf, B.H.; Ouda, M.H.; Alghurabi, H.S.; Shubbar, A.S. Zinc and Copper Levels and Their Correlation with Polycystic Ovary Syndrome Biochemical Changes. Int. J. Pharm. Sci. Res 2018, 9, 3036–3041. [CrossRef]
- Schmalbrock, L.J.; Weiss, G.; Rijntjes, E.; Reinschissler, N.; Sun, Q.; Schenk, M.; Schomburg, L. Pronounced Trace Element Variation in Follicular Fluids of Subfertile Women Undergoing Assisted Reproduction. Nutrients 2021, 13, 4134. [CrossRef]
- Chakraborty, P.; Ghosh, S.; Goswami, S.K.; Kabir, S.N.; Chakravarty, B.; Jana, K. Altered Trace Mineral Milieu Might Play an Aetiological Role in the Pathogenesis of Polycystic Ovary Syndrome. Biol. Trace Elem. Res. 2013, 152, 9–15. [CrossRef]
- Bizoń, A.; Tchórz, A.; Madej Pawełand Leśniewski, M.; Wójtowicz, M.; Piwowar, A.; Franik, G. The Activity of Superoxide Dismutase, Its Relationship with the Concentration of Zinc and Copper and the Prevalence of Rs2070424 Superoxide Dismutase Gene in Women with Polycystic Ovary Syndrome—Preliminary Study. J. Clin. Med. 2022, 11, 2548. [CrossRef]
- Kirmizi, D.A.; Baser, E.; Turksoy, V.A.; Kara, M.; Yalvac, E.S.; Gocmen, A.Y. Are Heavy Metal Exposure and Trace Element Levels Related to Metabolic and Endocrine Problems in Polycystic Ovary Syndrome? Biol. Trace Elem. Res. 2020, 198, 77–86. [CrossRef]
- Wang, Q.; Sun, Y.; Zhao, A.; Cai, X.; Yu, A.; Xu, Q.; Liu, W.; Zhang, N.; Wu, S.; Chen, Y.; et al. High Dietary Copper Intake Induces Perturbations in the Gut Microbiota and Affects Host Ovarian Follicle Development. Ecotoxicol. Environ. Saf. 2023, 255, 114810. [CrossRef]
- Ojha, P.S.; Maste, M.M.; Tubachi, S.; Patil, V.S. Human Papillomavirus and Cervical Cancer: An Insight Highlighting Pathogenesis and Targeting Strategies. VirusDisease 2022, 33, 132–154. [CrossRef]
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Collado, J.; Gómez, D.; Muñoz, J.; Bosch, F.; de Sanjosé, S. Human Papillomavirus and Related Diseases in the World; 2023.
- Kamolratanakul, S.; Pitisuttithum, P. Human Papillomavirus Vaccine Efficacy and Effectiveness against Cancer. Vaccines 2021, 9, 1413. [CrossRef]
- Wentzensen, N.; Schiffman, M.; Palmer, T.; Arbyn, M. Triage of HPV Positive Women in Cervical Cancer Screening. J. Clin. Virol. 2016, 76, S49–S55. [CrossRef]
- Preci, D.P.; Almeida, A.; Weiler, A.L.; Franciosi, M.L.M.; Cardoso, A.M. Oxidative Damage and Antioxidants in Cervical Cancer. Int. J. Gynecol. Cancer 2021, 31, 265–271. [CrossRef]
- Cunzhi, H.; Jiexian, J.; Xianwen, Z.; Jingang, G.; Shumin, Z.; Lili, D. Serum and Tissue Levels of Six Trace Elements and Copper/Zinc Ratio in Patients with Cervical Cancer and Uterine Myoma. Biol. Trace Elem. Res. 2003, 94, 113–122. [CrossRef]
- Naidu, M.S.K.; Suryakar, A.N.; Swami, S.C.; Katkam, R. V.; Kumbar, K.M. Oxidative Stress and Antioxidant Status in Cervical Cancer Patients. Indian J. Clin. Biochem. 2007, 22, 140–144. [CrossRef]
- Zhang, M.; Shi, M.; Zhao, Y. Association between Serum Copper Levels and Cervical Cancer Risk: A Meta-Analysis. Biosci. Rep. 2018, 38. [CrossRef]
- Okonkwo, C.A.; Amegor, F.O.; Gbolade, J.O. Relationship between Trace Elements and Major Gynaecological Malignancies. Asian J. Med. Sci. 2013, 5, 124–127. [CrossRef]
- Hijam, D.; Dubey, A.; Laishram, V.; Jaichand, L.; Devi, T.I. Serum Copper Levels in Different Stages of Cervical Cancer in Manipur. 2016, 2, 3–6. [CrossRef]
- Shah, S.; Kalal, B.S. Oxidative Stress in Cervical Cancer and Its Response to Chemoradiation. Turkish J. Obstet. Gynecol. 2019, 16, 124–128. [CrossRef]
- Brooks, R.A.; Fleming, G.F.; Lastra, R.R.; Lee, N.K.; Moroney, J.W.; Son, C.H.; Tatebe, K.; Veneris, J.L. Current Recommendations and Recent Progress in Endometrial Cancer. CA. Cancer J. Clin. 2019, 69, 258–279. [CrossRef]
- Lee, Y.C.; Lheureux, S.; Oza, A.M. Treatment Strategies for Endometrial Cancer: Current Practice and Perspective. Curr. Opin. Obstet. Gynecol. 2017, 29, 47–58. [CrossRef]
- Atakul, T.; Altinkaya, S.O.; Abas, B.I.; Yenisey, C. Serum Copper and Zinc Levels in Patients with Endometrial Cancer. Biol. Trace Elem. Res. 2020, 195, 46–54. [CrossRef]
- Rzymski, P.; Niedzielski, P.; Rzymski Pawełand Tomczyk, K.; Kozak, L.; Poniedziałek, B. Metal Accumulation in the Human Uterus Varies by Pathology and Smoking Status. Fertil. Steril. 2016, 105, 1511–1518. [CrossRef]
- Wieder-Huszla, S.; Chudecka-Głaz, A.; Cymbaluk-Płoska, A.; Karakiewicz, B.; Bosiacki, M.; Chlubek, D.; Jurczak, A. Evaluation of the Concentration of Selected Elements in Patients with Cancer of the Reproductive Organs with Respect to Treatment Stage—Preliminary Study. Nutrients 2022, 14, 2368. [CrossRef]
- Michalczyk, K.; Kapczuk, P.; Kupnicka, P.; Witczak, G.; Michalczyk, B.; Bosiacki, M.; Chlubek, D.; Cymbaluk-Płoska, A. Assessment of Serum Zn, Cu, Mn, and Fe Concentration in Women with Endometrial Cancer and Different Endometrial Pathologies. Nutrients 2023, 15, 3605. [CrossRef]
- Raz, N.; Feinmesser, L.; Moore, O.; Haimovich, S. Endometrial Polyps: Diagnosis and Treatment Options–a Review of Literature. Minim. Invasive Ther. /& Allied Technol. 2021, 30, 278–287. [CrossRef]
- Yang, Q.; Ciebiera, M.; Bariani, M.V.; Ali, M.; Elkafas, H.; Boyer, T.G.; Al-Hendy, A. Comprehensive Review of Uterine Fibroids: Developmental Origin, Pathogenesis, and Treatment. Endocr. Rev. 2022, 43, 678–719. [CrossRef]
- Taylor, H.S.; Kotlyar, A.M.; Flores, V.A. Endometriosis Is a Chronic Systemic Disease: Clinical Challenges and Novel Innovations. Lancet 2021, 397, 839–852. [CrossRef]
- Hart, R.J. Physiological Aspects of Female Fertility: Role of the Environment, Modern Lifestyle, and Genetics. Physiol. Rev. 2016, 96, 873–909. [CrossRef]
- Lee, S.C.; Kaunitz, A.M.; Sanchez-Ramos, L.; Rhatigan, R.M. The Oncogenic Potential of Endometrial Polyps: A Systematic Review and Meta-Analysis. Obstet. Gynecol. 2010, 116, 1197–1205. [CrossRef]
- Peng, X.; Li, T.; Xia, E.; Xia, C.; Liu, Y.; Yu, D. A Comparison of Oestrogen Receptor and Progesterone Receptor Expression in Endometrial Polyps and Endometrium of Premenopausal Women. J. Obstet. Gynaecol. 2009, 29, 340–346. [CrossRef]
- Liu, Z.; Kuokkanen, S.; Pal, L. Steroid Hormone Receptor Profile of Premenopausal Endometrial Polyps. Reprod. Sci. 2010, 17, 377–383. [CrossRef]
- Yin, P.; Ono, M.; Moravek, M.B.; Coon, J.S.; Navarro, A.; Monsivais, D.; Dyson, M.T.; Druschitz, S.A.; Malpani, S.S.; Serna, V.A.; et al. Human Uterine Leiomyoma Stem/Progenitor Cells Expressing CD34 and CD49b Initiate Tumors in Vivo. J. Clin. Endocrinol. /& Metab. 2015, 100, E601–E606. [CrossRef]
- Mas, A.; Stone, L.; O’Connor, P.M.; Yang, Q.; Kleven, D.; Simon, C.; Walker, C.L.; Al-Hendy, A. Developmental Exposure to Endocrine Disruptors Expands Murine Myometrial Stem Cell Compartment as a Prerequisite to Leiomyoma Tumorigenesis. Stem Cells 2017, 35, 666–678. [CrossRef]
- Li, D.; Jiang, T.; Wang, X.; Yin, T.; Shen, L.; Zhang, Z.; Zou, W.; Liu, Y.; Zong, K.; Liang, D.; et al. Serum Essential Trace Element Status in Women and the Risk of Endometrial Diseases: A Case–Control Study. Biol. Trace Elem. Res. 2023, 201, 2151–2161. [CrossRef]
- Yılmaz, B.K.; Evliyaoğlu, Ö.; Yorgancı, A.; Özyer, Ş.; Üstün, Y.E. Serum Concentrations of Heavy Metals in Women with Endometrial Polyps. J. Obstet. Gynaecol. 2020, 40, 541–545. [CrossRef]
- Flores, I.; Rivera, E.; Ruiz, L.A.; Santiago, O.I.; Vernon, M.W.; Appleyard, C.B. Molecular Profiling of Experimental Endometriosis Identified Gene Expression Patterns in Common with Human Disease. Fertil. Steril. 2007, 87, 1180–1199. [CrossRef]
- Turgut, A.I.; Ozler, A.; Goruk, N.Y.; Tunc, S.Y.; Evliyaoglu, O.; Gul, T. Copper, Ceruloplasmin and Oxidative Stress in Patients with Advanced-Stage Endometriosis. Eur Rev Med. Pharmacol Sci 2013, 17, 1472–1478.
- Pollack, A.Z.; Louis, G.M.B.; Chen, Z.; Peterson, C.M.; Sundaram, R.; Croughan, M.S.; Sun, L.; Hediger, M.L.; Stanford, J.B.; Varner, M.W.; et al. Trace Elements and Endometriosis: The ENDO Study. Reprod. Toxicol. 2013, 42, 41–48. [CrossRef]
- Delsouc, M.B.; Ghersa, F.; Ramírez, D.; Della Vedova, M.C.; Gil, R.A.; Vallcaneras, S.S.; Casais, M. Endometriosis Progression in Tumor Necrosis Factor Receptor P55-Deficient Mice: Impact on Oxidative/Nitrosative Stress and Metallomic Profile. J. Trace Elem. Med. Biol. 2019, 52, 157–165. [CrossRef]
- Ngô, C.; Chéreau, C.; Nicco, C.; Weill, B.; Chapron, C.; Batteux, F. Reactive Oxygen Species Controls Endometriosis Progression. Am. J. Pathol. 2009, 175, 225–234. [CrossRef]
- Tsang, C.K.; Chen, M.; Cheng, X.; Qi, Y.; Chen, Y.; Das, I.; Li, X.; Vallat, B.; Fu, L.-W.; Qian, C.-N.; et al. SOD1 Phosphorylation by MTORC1 Couples Nutrient Sensing and Redox Regulation. Mol. Cell 2018, 70, 502–515. [CrossRef]
- McKinnon, B.D.; Kocbek, V.; Nirgianakis, K.; Bersinger, N.A.; Mueller, M.D. Kinase Signalling Pathways in Endometriosis: Potential Targets for Non-Hormonal Therapeutics. Hum. Reprod. Update 2016, 22, 382–403. [CrossRef]
- Klevay, L.M.; Christopherson, D.M. Copper Deficiency Halves Serum Dehydroepiandrosterone in Rats. J. trace Elem. Med. Biol. 2000, 14, 143–145. [CrossRef]
- Soni, R.K.; Gupta, P.S.P.; Nandi, S.; Mondal, S.; Ippala, J.R.; Mor, A.; Mishra, A.; Tripathi, S.K. Effect of in Vitro Copper Supplementation on Granulosa Cell Estradiol Synthesis and Associated Genes. Indian J. Anim. Res. 2018, 52, 652–657. [CrossRef]
- Delsouc, M.B.; Conforti, R.A.; Vitale, D.L.; Alaniz, L.; Pacheco, P.; Andujar, S.; Vallcaneras, S.S.; Casais, M. Antiproliferative and Antiangiogenic Effects of Ammonium Tetrathiomolybdate in a Model of Endometriosis. Life Sci. 2021, 287, 120099. [CrossRef]
- Conforti, R.A.; Delsouc, M.B.; Zabala, A.S.; Vallcaneras, S.S.; Casais, M. The Copper Chelator Ammonium Tetrathiomolybdate Inhibits the Progression of Experimental Endometriosis in TNFR1-Deficient Mice. Sci. Rep. 2023, 13, 10354. [CrossRef]
- Vallcaneras, S.; Ghersa, F.; Bastón, J.; Delsouc, M.B.; Meresman, G.; Casais, M. TNFRp55 Deficiency Promotes the Development of Ectopic Endometriotic-like Lesions in Mice. J. Endocrinol. 2017, 234, 269–278. [CrossRef]
- Ghersa, F.; Delsouc, M.B.; Goyeneche, A.A.; Vallcaneras, S.S.; Meresman, G.; Telleria, C.M.; Casais, M. Reduced Inflammatory State Promotes Reinnervation of Endometriotic-like Lesions in TNFRp55 Deficient Mice. Mol. Hum. Reprod. 2019, 25, 385–396. [CrossRef]
- Li, Y. Copper Homeostasis: Emerging Target for Cancer Treatment. IUBMB Life 2020, 72, 1900–1908. [CrossRef]
- Babak, M. V.; Ahn, D. Modulation of Intracellular Copper Levels as the Mechanism of Action of Anticancer Copper Complexes: Clinical Relevance. Biomedicines 2021, 9, 852. [CrossRef]
- Kim, J.-J.; Kim, Y.-S.; Kumar, V. Heavy Metal Toxicity: An Update of Chelating Therapeutic Strategies. J. Trace Elem. Med. Biol. 2019, 54, 226–231. [CrossRef]
- Peisach, J.; Blumberg, W.E. A Mechanism for the Action of Penicillamine in the Treatment of Wilson’s Disease. Mol. Pharmacol. 1969, 5, 200–209.
- Kumar, V.; Singh, A.P.; Wheeler, N.; Galindo, C.L.; Kim, J.-J. Safety Profile of D-Penicillamine: A Comprehensive Pharmacovigilance Analysis by FDA Adverse Event Reporting System. Expert Opin. Drug Saf. 2021, 20, 1443–1450. [CrossRef]
- Matsubara, T.; Saura, R.; Hirohata, K.; Ziff, M.; others Inhibition of Human Endothelial Cell Proliferation in Vitro and Neovascularization in Vivo by D-Penicillamine. J. Clin. Invest. 1989, 83, 158–167. [CrossRef]
- Crowe, A.; Jackaman, C.; Beddoes, K.M.; Ricciardo, B.; Nelson, D.J. Rapid Copper Acquisition by Developing Murine Mesothelioma: Decreasing Bioavailable Copper Slows Tumor Growth, Normalizes Vessels and Promotes T Cell Infiltration. PLoS ONE 2013, 8, e73684. [CrossRef]
- Mammoto, T.; Jiang, A.; Jiang, E.; Panigrahy, D.; Kieran, M.W.; Mammoto, A. Role of Collagen Matrix in Tumor Angiogenesis and Glioblastoma Multiforme Progression. Am. J. Pathol. 2013, 183, 1293–1305. [CrossRef]
- Kim, H.; Jo, S.; Kim, I.-G.; Kim, R.-K.; Kahm, Y.-J.; Jung, S.-H.; Lee, J.H. Effect of Copper Chelators via the TGF-β Signaling Pathway on Glioblastoma Cell Invasion. Molecules 2022, 27, 8851. [CrossRef]
- Chen, S.-J.; Kuo, C.-C.; Pan, H.-Y.; Tsou, T.-C.; Yeh, S.-C.; Chang, J.-Y. Mechanistic Basis of a Combination D-Penicillamine and Platinum Drugs Synergistically Inhibits Tumor Growth in Oxaliplatin-Resistant Human Cervical Cancer Cells in Vitro and in Vivo. Biochem. Pharmacol. 2015, 95, 28–37. [CrossRef]
- Horn, N.; Møller, L.B.; Nurchi, V.M.; Aaseth, J. Chelating Principles in Menkes and Wilson Diseases: Choosing the Right Compounds in the Right Combinations at the Right Time. J. Inorg. Biochem. 2019, 190, 98–112. [CrossRef]
- Weiss, K.H.; Thurik, F.; Gotthardt, D.N.; Schäfer, M.; Teufel, U.; Wiegand, F.; Merle, U.; Ferenci–Foerster, D.; Maieron, A.; Stauber, R.; et al. Efficacy and Safety of Oral Chelators in Treatment of Patients with Wilson Disease. Clin. Gastroenterol. Hepatol. 2013, 11, 1028–1035. [CrossRef]
- Yoshii, J.; Yoshiji, H.; Kuriyama, S.; Ikenaka, Y.; Noguchi, R.; Okuda, H.; Tsujinoue, H.; Nakatani, T.; Kishida, H.; Nakae, D.; et al. The Copper-Chelating Agent, Trientine, Suppresses Tumor Development and Angiogenesis in the Murine Hepatocellular Carcinoma Cells. Int. J. Cancer 2001, 94, 768–773. [CrossRef]
- Moriguchi, M.; Nakajima, T.; Kimura, H.; Watanabe, T.; Takashima, H.; Mitsumoto, Y.; Katagishi, T.; Okanoue, T.; Kagawa, K. The Copper Chelator Trientine Has an Antiangiogenic Effect against Hepatocellular Carcinoma, Possibly through Inhibition of Interleukin-8 Production. Int. J. Cancer 2002, 102, 445–452. [CrossRef]
- Hayashi, M.; Nishiya, H.; Chiba, T.; Endoh, D.; Kon, Y.; Okui, T. Trientine, a Copper-Chelating Agent, Induced Apoptosis in Murine Fibrosarcoma Cells in Vivo and in Vitro. J. Vet. Med. Sci. 2007, 69, 137–142. [CrossRef]
- Liu, J.; Guo, L.; Yin, F.; Zheng, X.; Chen, G.; Wang, Y. Characterization and Antitumor Activity of Triethylene Tetramine, a Novel Telomerase Inhibitor. Biomed. Pharmacother. 2008, 62, 480–485. [CrossRef]
- Guterres, A.N.; Villanueva, J. Targeting Telomerase for Cancer Therapy. Oncogene 2020, 39, 5811–5824. [CrossRef]
- Huang, Y.-F.; Kuo, M.T.; Liu, Y.-S.; Cheng, Y.-M.; Wu, P.-Y.; Chou, C.-Y. A Dose Escalation Study of Trientine plus Carboplatin and Pegylated Liposomal Doxorubicin in Women with a First Relapse of Epithelial Ovarian, Tubal, and Peritoneal Cancer within 12 Months after Platinum-Based Chemotherapy. Front. Oncol. 2019, 9, 437. [CrossRef]
- Ferguson, W.S.; Lewis, A.H.; Watson, S.J. The Teart Pastures of Somerset: I. The Cause and Cure of Teartness. J. Agric. Sci. 1943, 33, 44–51. [CrossRef]
- Bickel, H.; Neale, F.C.; Hall, G. A Clinical and Biochemical Study of Hepatolenticular Degeneration (Wilson’s Disease). QJM An Int. J. Med. 1957, 26, 527–558.
- Dick, A.T.; Dewey, D.W.; Gawthorne, J.M. Thiomolybdates and the Copper–Molybdenum–Sulphur Interaction in Ruminant Nutrition. J. Agric. Sci. 1975, 85, 567–568. [CrossRef]
- Brewer, G.J.; Askari, F.; Lorincz, M.T.; Carlson, M.; Schilsky, M.; Kluin, K.J.; Hedera, P.; Moretti, P.; Fink, J.K.; Tankanow, R.; et al. Treatment of Wilson Disease with Ammonium Tetrathiomolybdate: IV. Comparison of Tetrathiomolybdate and Trientine in a Double-Blind Study of Treatment of the Neurologic Presentation of Wilson Disease. Arch. Neurol. 2006, 63, 521. [CrossRef]
- Cox, C.; Teknos, T.N.; Barrios, M.; Brewer, G.J.; Dick, R.D.; Merajver, S.D. The Role of Copper Suppression as an Antiangiogenic Strategy in Head and Neck Squamous Cell Carcinoma. Laryngoscope 2001, 111, 696–701. [CrossRef]
- Khan, M.K.; Miller, M.W.; Taylor, J.; Gill, N.K.; Dick, R.D.; Van Goled, K.; Brewert, G.J.; Merajver, S.D. Radiotherapy and Antiangiogenic TM in Lung Cancer. Neoplasia 2002, 4, 164–170. [CrossRef]
- Van Golen, K.L.; Bao, L.; Brewert, G.J.; Pienta, K.J.; Kamradt, J.M.; Livant, D.L.; Merajver, S.D. Suppression of Tumor Recurrence and Metastasis by a Combination of the PHSCN Sequence and the Antiangiogenic Compound Tetrathiomolybdate in Prostate Carcinoma. Neoplasia 2002, 4, 373–379. [CrossRef]
- Kim, K.K.; Lange, T.S.; Singh, R.K.; Brard, L.; Moore, R.G. Tetrathiomolybdate Sensitizes Ovarian Cancer Cells to Anticancer Drugs Doxorubicin, Fenretinide, 5-Fluorouracil and Mitomycin C. BMC Cancer 2012, 12, 147. [CrossRef]
- Chan, N.; Willis, A.; Kornhauser, N.; Ward, M.M.; Lee, S.B.; Nackos, E.; Seo, B.R.; Chuang, E.; Cigler, T.; Moore, A.; et al. Influencing the Tumor Microenvironment: A Phase II Study of Copper Depletion Using Tetrathiomolybdate in Patients with Breast Cancer at High Risk for Recurrence and in Preclinical Models of Lung Metastases. Clin. Cancer Res. 2017, 23, 666–676. [CrossRef]
- Alvarez, H.M.; Xue, Y.; Robinson, C.D.; Canalizo-Hernández, M.A.; Marvin, R.G.; Kelly, R.A.; Mondragón, A.; Penner-Hahn, J.E.; O’Halloran, T. V Tetrathiomolybdate Inhibits Copper Trafficking Proteins through Metal Cluster Formation. Science 2010, 327, 331–334. [CrossRef]
- Juarez, J.C.; Betancourt, O.; Pirie-Shepherd, S.R.; Guan, X.; Price, M.L.; Shaw, D.E.; Mazar, A.P.; Doñate, F. Copper Binding by Tetrathiomolybdate Attenuates Angiogenesis and Tumor Cell Proliferation through the Inhibition of Superoxide Dismutase 1. Clin. Cancer Res. 2006, 12, 4974–4982. [CrossRef]
- Baldari, S.; Di Rocco, G.; Heffern, M.C.; Su, T.A.; Chang, C.J.; Toietta, G. Effects of Copper Chelation on BRAFV600E Positive Colon Carcinoma Cells. Cancers 2019, 11, 659. [CrossRef]
- Kim, Y.-J.; Tsang, T.; Anderson, G.R.; Posimo, J.M.; Brady, D.C. Inhibition of BCL2 Family Members Increases the Efficacy of Copper Chelation in BRAFV600E-Driven Melanoma. Cancer Res. 2020, 80, 1387–1400. [CrossRef]
- Ryumon, S.; Okui, T.; Kunisada, Y.; Kishimoto, K.; Shimo, T.; Hasegawa, K.; Ibaragi, S.; Akiyama, K.; Thu Ha, N.T.; Monsur Hassan, N.M.; et al. Ammonium Tetrathiomolybdate Enhances the Antitumor Effect of Cisplatin via the Suppression of ATPase Copper Transporting Beta in Head and Neck Squamous Cell Carcinoma. Oncol. Rep. 2019, 42, 2611–2621. [CrossRef]
- Schneider, B.J.; Lee, J.S.-J.; Hayman, J.A.; Chang, A.C.; Orringer, M.B.; Pickens, A.; Pan, C.C.; Merajver, S.D.; Urba, S.G. Pre-Operative Chemoradiation Followed by Post-Operative Adjuvant Therapy with Tetrathiomolybdate, a Novel Copper Chelator, for Patients with Resectable Esophageal Cancer. Invest. New Drugs 2013, 31, 435–442. [CrossRef]
- Kim, K.K.; Han, A.; Yano, N.; Ribeiro, J.R.; Lokich, E.; Singh, R.K.; Moore, R.G. Tetrathiomolybdate Mediates Cisplatin-Induced P38 Signaling and EGFR Degradation and Enhances Response to Cisplatin Therapy in Gynecologic Cancers. Sci. Rep. 2015, 5, 1–11. [CrossRef]
- Kim, K.K.; Kawar, N.M.; Singh, R.K.; Lange, T.S.; Brard, L.; Moore, R.G. Tetrathiomolybdate Induces Doxorubicin Sensitivity in Resistant Tumor Cell Lines. Gynecol. Oncol. 2011, 122, 183–189. [CrossRef]
- Nan, L.; Yuan, W.; Guodong, C.; Yonghui, H. Multitargeting Strategy Using Tetrathiomolybdate and Lenvatinib: Maximizing Antiangiogenesis Activity in a Preclinical Liver Cancer Model. Anti-Cancer Agents Med. Chem. 2023, 23, 786–793. [CrossRef]
- Rogers, P.A.W.; Adamson, G.D.; Al-Jefout, M.; Becker, C.M.; D’Hooghe, T.M.; Dunselman, G.A.J.; Fazleabas, A.; Giudice, L.C.; Horne, A.W.; Hull, M.L.; et al. Research Priorities for Endometriosis. Reprod. Sci. 2017, 24, 202–226. [CrossRef]
- Richter, O.N.; Dorn, C.; Rösing, B.; Flaskamp, C.; Ulrich, U. Tumor Necrosis Factor Alpha Secretion by Peritoneal Macrophages in Patients with Endometriosis. Arch. Gynecol. Obstet. 2005, 271, 143–147. [CrossRef]
- Braun, D.P.; Ding, J.; Dmowski, W.P. Peritoneal Fluid-Mediated Enhancement of Eutopic and Ectopic Endometrial Cell Proliferation Is Dependent on Tumor Necrosis Factor-α in Women with Endometriosis. Fertil. Steril. 2002, 78, 727–732. [CrossRef]
- Sheng, Y.; Li, F.; Qin, Z. TNF Receptor 2 Makes Tumor Necrosis Factor a Friend of Tumors. Front. Immunol. 2018, 9, 1–9. [CrossRef]
- Gough, P.; Myles, I.A. Tumor Necrosis Factor Receptors: Pleiotropic Signaling Complexes and Their Differential Effects. Front. Immunol. 2020, 11, 585880. [CrossRef]
- Rivas, M.A.; Carnevale, R.P.; Proietti, C.J.; Rosemblit, C.; Beguelin, W.; Salatino, M.; Charreau, E.H.; Frahm, I.; Sapia, S.; Brouckaert, P.; et al. TNFα Acting on TNFR1 Promotes Breast Cancer Growth via P42/P44 MAPK, JNK, Akt and NF-ΚB-Dependent Pathways. Exp. Cell Res. 2008, 314, 509–529. [CrossRef]
- Islimye, M.; Kilic, S.; Zulfikaroglu, E.; Topcu, O.; Zergeroglu, S.; Batioglu, S. Regression of Endometrial Autografts in a Rat Model of Endometriosis Treated with Etanercept. Eur. J. Obstet. /& Gynecol. Reprod. Biol. 2011, 159, 184–189. [CrossRef]
- Oliveri, V. Selective Targeting of Cancer Cells by Copper Ionophores: An Overview. Front. Mol. Biosci. 2022, 9, 841814. [CrossRef]
- Trachootham, D.; Alexandre, J.; Huang, P. Targeting Cancer Cells by ROS-Mediated Mechanisms: A Radical Therapeutic Approach? Nat. Rev. Drug Discov. 2009, 8, 579–591. [CrossRef]
- Shimada, K.; Reznik, E.; Stokes, M.E.; Krishnamoorthy, L.; Bos, P.H.; Song, Y.; Quartararo, C.E.; Pagano, N.C.; Carpizo, D.R.; DeCarvalho, A.C.; et al. Copper-Binding Small Molecule Induces Oxidative Stress and Cell-Cycle Arrest in Glioblastoma-Patient-Derived Cells. Cell Chem. Biol. 2018, 25, 585–594. [CrossRef]
- Tsvetkov, P.; Coy, S.; Petrova, B.; Dreishpoon, M.; Verma, A.; Abdusamad, M.; Rossen, J.; Joesch-Cohen, L.; Humeidi, R.; Spangler, R.D.; et al. Copper Induces Cell Death by Targeting Lipoylated TCA Cycle Proteins. Science (80-. ). 2022, 375, 1254–1261. [CrossRef]
- Xiao, Y.A.N.; Chen, D.I.; Zhang, X.I.A.; Cui, Q.; Fan, Y.; Bi, C.; Dou, Q.P. Molecular Study on Copper-Mediated Tumor Proteasome Inhibition and Cell Death. Int. J. Oncol. 2010, 37, 81–87. [CrossRef]
- Denoyer, D.; Pearson, H.B.; Clatworthy, S.A.S.; Smith, Z.M.; Francis, P.S.; Llanos, R.M.; Volitakis, I.; Phillips, W.A.; Meggyesy, P.M.; Masaldan, S.; et al. Copper as a Target for Prostate Cancer Therapeutics: Copper-Ionophore Pharmacology and Altering Systemic Copper Distribution. Oncotarget 2016, 7, 37064–37080. [CrossRef]
- Lu, C.; Li, X.; Ren, Y.; Zhang, X. Disulfiram: A Novel Repurposed Drug for Cancer Therapy. Cancer Chemother. Pharmacol. 2021, 87, 159–172. [CrossRef]
- Lewison, E.F. Spontaneous Regression of Breast Cancer. Prog. Clin. Biol. Res. 1977, 12, 47–53.
- Ekinci, E.; Rohondia, S.; Khan, R.; Dou, Q.P. Repurposing Disulfiram as an Anti-Cancer Agent: Updated Review on Literature and Patents. Recent Pat. Anticancer. Drug Discov. 2019, 14, 113–132. [CrossRef]
- Jia, Y.; Huang, T. Overview of Antabuse®(Disulfiram) in Radiation and Cancer Biology. Cancer Manag. Res. 2021, 13, 4095–4101. [CrossRef]
- Kannappan, V.; Ali, M.; Small, B.; Rajendran, G.; Elzhenni, S.; Taj, H.; Wang, W.; Dou, Q.P. Recent Advances in Repurposing Disulfiram and Disulfiram Derivatives as Copper-Dependent Anticancer Agents. Front. Mol. Biosci. 2021, 8, 741316. [CrossRef]
- Li, H.; Wang, J.; Wu, C.; Wang, L.; Chen, Z.-S.; Cui, W. The Combination of Disulfiram and Copper for Cancer Treatment. Drug Discov. Today 2020, 25, 1099–1108. [CrossRef]
- Li, Y.; Wang, L.-H.; Zhang, H.-T.; Wang, Y.-T.; Liu, S.; Zhou, W.-L.; Yuan, X.-Z.; Li, T.-Y.; Wu, C.-F.; Yang, J.-Y. Disulfiram Combined with Copper Inhibits Metastasis and Epithelial–Mesenchymal Transition in Hepatocellular Carcinoma through the NF-ΚB and TGF-β Pathways. J. Cell. Mol. Med. 2018, 22, 439–451. [CrossRef]
- Caminear, M.W.; Harrington, B.S.; Kamdar, R.D.; Kruhlak, M.J.; Annunziata, C.M. Disulfiram Transcends ALDH Inhibitory Activity When Targeting Ovarian Cancer Tumor-Initiating Cells. Front. Oncol. 2022, 12, 762820. [CrossRef]
- Guo, F.; Yang, Z.; Sehouli, J.; Kaufmann, A.M. Blockade of ALDH in Cisplatin-Resistant Ovarian Cancer Stem Cells in Vitro Synergistically Enhances Chemotherapy-Induced Cell Death. Curr. Oncol. 2022, 29, 2808–2822. [CrossRef]
- Dinavahi, S.S.; Bazewicz, C.G.; Gowda, R. Aldehyde Dehydrogenase Inhibitors for Cancer Therapeutics. Trends Pharmacol. Sci. 2019, 1–16. [CrossRef]
- Silva, I.A.; Bai, S.; McLean, K.; Yang, K.; Griffith, K.; Thomas, D.; Ginestier, C.; Johnston, C.; Kueck, A.; Reynolds, R.K.; et al. Aldehyde Dehydrogenase in Combination with CD133 Defines Angiogenic Ovarian Cancer Stem Cells That Portend Poor Patient Survival. Cancer Res. 2011, 71, 3991–4001. [CrossRef]
- Çelik, Ö.; Erşahin, A.; Acet, M.; Çelik, N.; Baykuş, Y.; Deniz, R.; Özerol, E.; Özerol, İ. Disulfiram, as a Candidate NF-Kappa B and Proteasome Inhibitor, Prevents Endometriotic Implant Growing in a Rat Model of Endometriosis. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4380–4389.
- Meraz-Torres, F.; Plöger, S.; Garbe, C.; Niessner, H.; Sinnberg, T. Disulfiram as a Therapeutic Agent for Metastatic Malignant Melanoma—Old Myth or New Logos? Cancers (Basel). 2020, 12, 3538. [CrossRef]
- Jiao, Y.; Hannafon, B.N.; Zhang, R.R.; Fung, K.-M.; Ding, W.-Q. Docosahexaenoic Acid and Disulfiram Act in Concert to Kill Cancer Cells: A Mutual Enhancement of Their Anticancer Actions. Oncotarget 2017, 8, 17908–17920. [CrossRef]
- Tang, B.; Wu, M.; Zhang, L.; Jian, S.; Lv, S.; Lin, T.; Zhu, S.; Liu, L.; Wang, Y.; Yi, Z.; et al. Combined Treatment of Disulfiram with PARP Inhibitors Suppresses Ovarian Cancer. Front. Oncol. 2023, 13, 1154073. [CrossRef]
- Du, R.; Sun, F.; Li, K.; Qi, J.; Zhong, W.; Wang, W.; Sun, Q.; Deng, Q.; Wang, H.; Nie, J.; et al. Proteomics Analysis Revealed Smad3 as A Potential Target of the Synergistic Anti-Tumor Activity of Disulfiram and Cisplatin in Ovarian Cancer. Anticancer. Agents Med. Chem. 2023, 23, 1754–1764. [CrossRef]
- Liu, Y.; Guan, X.; Wang, M.; Wang, N.; Chen, Y.; Li, B.; Xu, Z.; Fu, F.; Du, C.; Zheng, Z. Disulfiram/Copper Induces Antitumor Activity against Gastric Cancer via the ROS/MAPK and NPL4 Pathways. Bioengineered 2022, 13, 6579–6589. [CrossRef]
- Safi, R.; Nelson, E.R.; Chitneni, S.K.; Franz, K.J.; George, D.J.; Zalutsky, M.R.; McDonnell, D.P. Copper Signaling Axis as a Target for Prostate Cancer Therapeutics. Cancer Res. 2014, 74, 5819–5831. [CrossRef]
- Lun, X.; Wells, J.C.; Grinshtein, N.; King, J.C.; Hao, X.; Dang, N.-H.; Wang, X.; Aman, A.; Uehling, D.; Datti, A.; et al. Disulfiram When Combined with Copper Enhances the Therapeutic Effects of Temozolomide for the Treatment of Glioblastoma. Clin. Cancer Res. 2016, 22, 3860–3875. [CrossRef]
- Oliveri, V. Biomedical Applications of Copper Ionophores. Coord. Chem. Rev. 2020, 422, 213474. [CrossRef]
- Liu, X.; Wang, L.; Cui, W.; Yuan, X.; Lin, L.; Cao, Q.; Wang, N.; Li, Y.; Guo, W.; Zhang, X.; et al. Targeting ALDH1A1 by Disulfiram/Copper Complex Inhibits Non-Small Cell Lung Cancer Recurrence Driven by ALDH-Positive Cancer Stem Cells. Oncotarget 2016, 7, 58516–58530. [CrossRef]
- Xu, B.; Wang, S.; Li, R.; Chen, K.; He, L.; Deng, M.; Kannappan, V.; Zha, J.; Dong, H.; Wang, W. Disulfiram/Copper Selectively Eradicates AML Leukemia Stem Cells in Vitro and in Vivo by Simultaneous Induction of ROS-JNK and Inhibition of NF-ΚB and Nrf2. Cell death /& Dis. 2017, 8, e2797. [CrossRef]
- Serra, R.; Zhao, T.; Huq, S.; Gorelick, N.L.; Casaos, J.; Cecia, A.; Mangraviti, A.; Eberhart, C.; Bai, R.; Olivi, A.; et al. Disulfiram and Copper Combination Therapy Targets NPL4, Cancer Stem Cells and Extends Survival in a Medulloblastoma Model. PLoS ONE 2021, 16, e0251957. [CrossRef]
- Sun, T.; Yang, W.; Toprani, S.M.; Guo, W.; He, L.; DeLeo, A.B.; Ferrone, S.; Zhang, G.; Wang, E.; Lin, Z.; et al. Induction of Immunogenic Cell Death in Radiation-Resistant Breast Cancer Stem Cells by Repurposing Anti-Alcoholism Drug Disulfiram. Cell Commun. Signal. 2020, 18, 1–14. [CrossRef]
- Falls-Hubert, K.C.; Butler, A.L.; Gui, K.; Anderson, M.; Li, M.; Stolwijk, J.M.; Rodman III, S.N.; Solst, S.R.; Tomanek-Chalkley, A.; Searby, C.C.; et al. Disulfiram Causes Selective Hypoxic Cancer Cell Toxicity and Radio-Chemo-Sensitization via Redox Cycling of Copper. Free Radic. Biol. Med. 2020, 150, 1–11. [CrossRef]
- Guo, W.; Zhang, X.; Lin, L.; Wang, H.; He, E.; Wang, G.; Zhao, Q. The Disulfiram/Copper Complex Induces Apoptosis and Inhibits Tumour Growth in Human Osteosarcoma by Activating the ROS/JNK Signalling Pathway. J. Biochem. 2021, 170, 275–287. [CrossRef]
- Zhang, W.; Zhai, Q.; Li, M.; Huang, S.; Sun, Z.; Yan, Z.; Li, J.; Li, L.; Li, Y. Anti-Cancer Effects of Disulfiram in Cervical Cancer Cell Lines Are Mediated by Both Autophagy and Apoptosis. Bull. Exp. Biol. Med. 2022, 172, 642–648. [CrossRef]
- Shinde, S.D.; Sakla, A.P.; Shankaraiah, N. An Insight into Medicinal Attributes of Dithiocarbamates: Bird’s Eye View. Bioorg. Chem. 2020, 105, 104346. [CrossRef]
- Wykowski, R.; Fuentefria, A.M.; de Andrade, S.F. Antimicrobial Activity of Clioquinol and Nitroxoline: A Scoping Review. Arch. Microbiol. 2022, 204, 535. [CrossRef]
- Ding, W.-Q.; Liu, B.; Vaught, J.L.; Yamauchi, H.; Lind, S.E. Anticancer Activity of the Antibiotic Clioquinol. Cancer Res. 2005, 65, 3389–3395. [CrossRef]
- Chen, D.; Cui, Q.C.; Yang, H.; Barrea, R.A.; Sarkar, F.H.; Sheng, S.; Yan, B.; Reddy, G.P.V.; Dou, Q.P. Clioquinol, a Therapeutic Agent for Alzheimer’s Disease, Has Proteasome-Inhibitory, Androgen Receptor–Suppressing, Apoptosis-Inducing, and Antitumor Activities in Human Prostate Cancer Cells and Xenografts. Cancer Res. 2007, 67, 1636–1644. [CrossRef]
- Tuller, E.R.; Brock, A.L.; Yu, H.; Lou, J.R.; Benbrook, D.M.; Ding, W.-Q. PPARα Signaling Mediates the Synergistic Cytotoxicity of Clioquinol and Docosahexaenoic Acid in Human Cancer Cells. Biochem. Pharmacol. 2009, 77, 1480–1486. [CrossRef]
- Cater, M.A.; Haupt, Y. Clioquinol Induces Cytoplasmic Clearance of the X-Linked Inhibitor of Apoptosis Protein (XIAP): Therapeutic Indication for Prostate Cancer. Biochem. J. 2011, 436, 481–491. [CrossRef]
- Mao, X.; Li, X.; Sprangers, R.; Wang, X.; Venugopal, A.; Wood, T.; Zhang, Y.; Kuntz, D.A.; Coe, E.; Trudel, S.; et al. Clioquinol Inhibits the Proteasome and Displays Preclinical Activity in Leukemia and Myeloma. Leukemia 2009, 23, 585–590. [CrossRef]
- Cao, B.; Li, J.; Zhou, X.; Juan, J.; Han, K.; Zhang, Z.; Kong, Y.; Wang, J.; Mao, X. Clioquinol Induces Pro-Death Autophagy in Leukemia and Myeloma Cells by Disrupting the MTOR Signaling Pathway. Sci. Rep. 2014, 4, 5749. [CrossRef]
- Barrea, R.A.; Chen, D.; Irving, T.C.; Dou, Q.P. Synchrotron X-Ray Imaging Reveals a Correlation of Tumor Copper Speciation with Clioquinol’s Anticancer Activity. J. Cell. Biochem. 2009, 108, 96–105. [CrossRef]
- Du, T.; Filiz, G.; Caragounis, A.; Crouch, P.J.; White, A.R. Clioquinol Promotes Cancer Cell Toxicity through Tumor Necrosis Factor α Release from Macrophages. J. Pharmacol. Exp. Ther. 2008, 324, 360–367. [CrossRef]
- Bareggi, S.R.; Cornelli, U. Clioquinol: Review of Its Mechanisms of Action and Clinical Uses in Neurodegenerative Disorders. CNS Neurosci. /& Ther. 2012, 18, 41–46. [CrossRef]
- Khan, R.; Khan, H.; Abdullah, Y.; Dou, Q.P. Feasibility of Repurposing Clioquinol for Cancer Therapy. Recent Pat. Anticancer. Drug Discov. 2020, 15, 14–31. [CrossRef]
- Jiang, H.; Taggart, J.E.; Zhang, X.; Benbrook, D.M.; Lind, S.E.; Ding, W.-Q. Nitroxoline (8-Hydroxy-5-Nitroquinoline) Is More a Potent Anti-Cancer Agent than Clioquinol (5-Chloro-7-Iodo-8-Quinoline). Cancer Lett. 2011, 312, 11–17. [CrossRef]
- Summers, K.L.; Dolgova, N. V.; Gagnon, K.B.; Sopasis, G.J.; James, A.K.; Lai, B.; Sylvain, N.J.; Harris, H.H.; Nichol, H.K.; George, G.N.; et al. PBT2 Acts through a Different Mechanism of Action than Other 8-Hydroxyquinolines: An X-Ray Fluorescence Imaging Study. Metallomics 2020, 12, 1979–1994. [CrossRef]
- Chen, S.; Sun, L.; Koya, K.; Tatsuta, N.; Xia, Z.; Korbut, T.; Du, Z.; Wu, J.; Liang, G.; Jiang, J.; et al. Syntheses and Antitumor Activities of N′ 1, N′ 3-Dialkyl-N′ 1, N′ 3-Di-(Alkylcarbonothioyl) Malonohydrazide: The Discovery of Elesclomol. Bioorganic Med. Chem. Lett. 2013, 23, 5070–5076. [CrossRef]
- Kwan, S.-Y.; Cheng, X.; Tsang, Y.T.M.; Choi, J.-S.; Kwan, S.-Y.; Izaguirre, D.I.; Kwan, H.-S.; Gershenson, D.M.; Wong, K.-K. Loss of ARID1A Expression Leads to Sensitivity to ROS-Inducing Agent Elesclomol in Gynecologic Cancer Cells. Oncotarget 2016, 7, 56933–56943. [CrossRef]
- Buccarelli, M.; D’Alessandris, Q.G.; Matarrese, P.; Mollinari, C.; Signore, M.; Cappannini, A.; Martini, M.; D’Aliberti, P.; De Luca, G.; Pedini, F.; et al. Elesclomol-Induced Increase of Mitochondrial Reactive Oxygen Species Impairs Glioblastoma Stem-like Cell Survival and Tumor Growth. J. Exp. /& Clin. Cancer Res. 2021, 40, 1–17. [CrossRef]
- Nagai, M.; Vo, N.H.; Ogawa, L.S.; Chimmanamada, D.; Inoue, T.; Chu, J.; Beaudette-Zlatanova, B.C.; Lu, R.; Blackman, R.K.; Barsoum, J.; et al. The Oncology Drug Elesclomol Selectively Transports Copper to the Mitochondria to Induce Oxidative Stress in Cancer Cells. Free Radic. Biol. Med. 2012, 52, 2142–2150. [CrossRef]
- Hasinoff, B.B.; Yadav, A.A.; Patel, D.; Wu, X. The Cytotoxicity of the Anticancer Drug Elesclomol Is Due to Oxidative Stress Indirectly Mediated through Its Complex with Cu (II). J. Inorg. Biochem. 2014, 137, 22–30. [CrossRef]
- Tsvetkov, P.; Detappe, A.; Cai, K.; Keys, H.R.; Brune, Z.; Ying, W.; Thiru, P.; Reidy, M.; Kugener, G.; Rossen, J.; et al. Mitochondrial Metabolism Promotes Adaptation to Proteotoxic Stress. Nat. Chem. Biol. 2019, 15, 681–689. [CrossRef]
- Yadav, A.A.; Patel, D.; Wu, X.; Hasinoff, B.B. Molecular Mechanisms of the Biological Activity of the Anticancer Drug Elesclomol and Its Complexes with Cu (II), Ni (II) and Pt (II). J. Inorg. Biochem. 2013, 126, 1–6. [CrossRef]
- Lu, J.; Ling, X.; Sun, Y.; Liu, L.; Liu, L.; Wang, X.; Lu, C.; Ren, C.; Han, X.; Yu, Z. FDX1 Enhances Endometriosis Cell Cuproptosis via G6PD-Mediated Redox Homeostasis. Apoptosis 2023, 28, 1128–1140. [CrossRef]
- Takeda, T.; Banno, K.; Okawa, R.; Yanokura, M.; Iijima, M.; Irie-Kunitomi, H.; Nakamura, K.; Iida, M.; Adachi, M.; Umene, K.; et al. ARID1A Gene Mutation in Ovarian and Endometrial Cancers. Oncol. Rep. 2016, 35, 607–613. [CrossRef]
- Nie, X.; Chen, H.; Xiong, Y.; Chen, J.; Liu, T. Anisomycin Has a Potential Toxicity of Promoting Cuproptosis in Human Ovarian Cancer Stem Cells by Attenuating YY1/Lipoic Acid Pathway Activation. J. Cancer 2022, 13, 3503–3514. [CrossRef]
- Harrington, B.S.; Ozaki, M.K.; Caminear, M.W.; Hernandez, L.F.; Jordan, E.; Kalinowski, N.J.; Goldlust, I.S.; Guha, R.; Ferrer, M.; Thomas, C.; et al. Drugs Targeting Tumor-Initiating Cells Prolong Survival in a Post-Surgery, Post-Chemotherapy Ovarian Cancer Relapse Model. Cancers (Basel). 2020, 12, 1645. [CrossRef]
- Monk, B.J.; Kauderer, J.T.; Moxley, K.M.; Bonebrake, A.J.; Dewdney, S.B.; Secord, A.A.; Ueland, F.R.; Johnston, C.M.; Aghajanian, C. A Phase II Evaluation of Elesclomol Sodium and Weekly Paclitaxel in the Treatment of Recurrent or Persistent Platinum-Resistant Ovarian, Fallopian Tube or Primary Peritoneal Cancer: An NRG Oncology/Gynecologic Oncology Group Study. Gynecol. Oncol. 2018, 151, 422–427. [CrossRef]
- Hedley, D.; Shamas-Din, A.; Chow, S.; Sanfelice, D.; Schuh, A.C.; Brandwein, J.M.; Seftel, M.D.; Gupta, V.; Yee, K.W.L.; Schimmer, A.D. A Phase I Study of Elesclomol Sodium in Patients with Acute Myeloid Leukemia. Leuk. /& lymphoma 2016, 57, 2437–2440. [CrossRef]
- O’Day, S.; Gonzalez, R.; Lawson, D.; Weber, R.; Hutchins, L.; Anderson, C.; Haddad, J.; Kong, S.; Williams, A.; Jacobson, E. Phase II, Randomized, Controlled, Double-Blinded Trial of Weekly Elesclomol plus Paclitaxel versus Paclitaxel Alone for Stage IV Metastatic Melanoma. J. Clin. Oncol. 2009, 27, 5452–5458. [CrossRef]
- O’Day, S.J.; Eggermont, A.M.M.; Chiarion-Sileni, V.; Kefford, R.; Grob, J.J.; Mortier, L.; Robert, C.; Schachter, J.; Testori, A.; Mackiewicz, J.; et al. Final Results of Phase III SYMMETRY Study: Randomized, Double-Blind Trial of Elesclomol plus Paclitaxel versus Paclitaxel Alone as Treatment for Chemotherapy-Naive Patients with Advanced Melanoma. J. Clin. Oncol. 2013, 31, 1211–1218. [CrossRef]
- Zheng, P.; Zhou, C.; Lu, L.; Liu, B.; Ding, Y. Elesclomol: A Copper Ionophore Targeting Mitochondrial Metabolism for Cancer Therapy. J. Exp. Clin. Cancer Res. 2022, 41, 1–13. [CrossRef]
- Helsel, M.E.; Franz, K.J. Pharmacological Activity of Metal Binding Agents That Alter Copper Bioavailability. Dalt. Trans. 2015, 44, 8760–8770. [CrossRef]
- Xiao, Z.; Donnelly, P.S.; Zimmermann, M.; Wedd, A.G. Transfer of Copper between Bis (Thiosemicarbazone) Ligands and Intracellular Copper-Binding Proteins. Insights into Mechanisms of Copper Uptake and Hypoxia Selectivity. Inorg. Chem. 2008, 47, 4338–4347. [CrossRef]
- Cater, M.A.; Pearson, H.B.; Wolyniec, K.; Klaver, P.; Bilandzic, M.; Paterson, B.M.; Bush, A.I.; Humbert, P.O.; La Fontaine, S.; Donnelly, P.S.; et al. Increasing Intracellular Bioavailable Copper Selectively Targets Prostate Cancer Cells. ACS Chem. Biol. 2013, 8, 1621–1631. [CrossRef]
- Donnelly, P.S.; Liddell, J.R.; Lim, S.; Paterson, B.M.; Cater, M.A.; Savva, M.S.; Mot, A.I.; James, J.L.; Trounce, I.A.; White, A.R.; et al. An Impaired Mitochondrial Electron Transport Chain Increases Retention of the Hypoxia Imaging Agent Diacetylbis (4-Methylthiosemicarbazonato) CopperII. Proc. Natl. Acad. Sci. USA 2012, 109, 47–52. [CrossRef]
- Holland, J.P.; Barnard, P.J.; Collison, D.; Dilworth, J.R.; Edge, R.; Green, J.C.; McInnes, E.J.L. Spectroelectrochemical and Computational Studies on the Mechanism of Hypoxia Selectivity of Copper Radiopharmaceuticals. Chem. Eur. J. 2008, 14, 5890–5907. [CrossRef]
- Paterson, B.M.; Donnelly, P.S. Copper Complexes of Bis (Thiosemicarbazones): From Chemotherapeutics to Diagnostic and Therapeutic Radiopharmaceuticals. Chem. Soc. Rev. 2011, 40, 3005–3018. [CrossRef]
- Boschi, A.; Martini, P.; Janevik-Ivanovska, E.; Duatti, A. The Emerging Role of Copper-64 Radiopharmaceuticals as Cancer Theranostics. Drug Discov. Today 2018, 23, 1489–1501. [CrossRef]
- Lewis, J.S.; Laforest, R.; Buettner, T.L.; Song, S.-K.; Fujibayashi, Y.; Connett, J.M.; Welch, M.J. Copper-64-Diacetyl-Bis (N 4-Methylthiosemicarbazone): An Agent for Radiotherapy. Proc. Natl. Acad. Sci. USA 2001, 98, 1206–1211. [CrossRef]
- Dehdashti, F.; Grigsby, P.W.; Lewis, J.S.; Laforest, R.; Siegel, B.A.; Welch, M.J. Assessing Tumor Hypoxia in Cervical Cancer by PET with 60Cu-Labeled Diacetyl-Bis (N4-Methylthiosemicarbazone). J. Nucl. Med. 2008, 49, 201–205. [CrossRef]
- Grigsby, P.W.; Malyapa, R.S.; Higashikubo, R.; Schwarz, J.K.; Welch, M.J.; Huettner, P.C.; Dehdashti, F. Comparison of Molecular Markers of Hypoxia and Imaging with 60 Cu-ATSM in Cancer of the Uterine Cervix. Mol. imaging Biol. 2007, 9, 278–283. [CrossRef]
- Lewis, J.S.; Laforest, R.; Dehdashti, F.; Grigsby, P.W.; Welch, M.J.; Siegel, B.A. An Imaging Comparison of 64Cu-ATSM and 60Cu-ATSM in Cancer of the Uterine Cervix. J. Nucl. Med. 2008, 49, 1177–1182. [CrossRef]
- Santini, C.; Pellei, M.; Gandin, V.; Porchia, M.; Tisato, F.; Marzano, C. Advances in Copper Complexes as Anticancer Agents. Chem. Rev. 2014, 114, 815–862. [CrossRef]
- Chaturvedi, V.K.; Singh, A.; Singh, V.K.; Singh, M.P. Cancer Nanotechnology: A New Revolution for Cancer Diagnosis and Therapy. Curr. Drug Metab. 2019, 20, 416–429. [CrossRef]
- Ameh, T.; Sayes, C.M. The Potential Exposure and Hazards of Copper Nanoparticles: A Review. Environ. Toxicol. Pharmacol. 2019, 71, 103220. [CrossRef]
- Dou, L.; Zhang, X.; Zangeneh, M.M.; Zhang, Y. Efficient Biogenesis of Cu2O Nanoparticles Using Extract of Camellia Sinensis Leaf: Evaluation of Catalytic, Cytotoxicity, Antioxidant, and Anti-Human Ovarian Cancer Properties. Bioorg. Chem. 2021, 106, 104468. [CrossRef]
- Tabrez, S.; Khan, A.U.; Mirza, A.A.; Suhail, M.; Jabir, N.R.; Zughaibi, T.A.; Alam, M. Biosynthesis of Copper Oxide Nanoparticles and Its Therapeutic Efficacy against Colon Cancer. Nanotechnol. Rev. 2022, 11, 1322–1331. [CrossRef]
- Zhao, H.; Maruthupandy, M.; Al-mekhlafi, F.A.; Chackaravarthi, G.; Ramachandran, G.; Chelliah, C.K. Biological Synthesis of Copper Oxide Nanoparticles Using Marine Endophytic Actinomycetes and Evaluation of Biofilm Producing Bacteria and A549 Lung Cancer Cells. J. King Saud Univ. 2022, 34, 101866. [CrossRef]
- Zughaibi, T.A.; Jabir, N.R.; Khan, A.U.; Khan, M.S.; Tabrez, S. Screening of Cu4O3 NPs Efficacy and Its Anticancer Potential against Cervical Cancer. Cell Biochem. Funct. 2023. [CrossRef]
- Chen, H.; Feng, X.; Gao, L.; Mickymaray, S.; Paramasivam, A.; Abdulaziz Alfaiz, F.; Almasmoum, H.A.; Ghaith, M.M.; Almaimani, R.A.; Aziz Ibrahim, I.A. Inhibiting the PI3K/AKT/MTOR Signalling Pathway with Copper Oxide Nanoparticles from Houttuynia Cordata Plant: Attenuating the Proliferation of Cervical Cancer Cells. Artif. Cells, Nanomedicine, Biotechnol. 2021, 49, 240–249. [CrossRef]
- Goswami, U.; Dutta, A.; Raza, A.; Kandimalla, R.; Kalita, S.; Ghosh, S.S.; Chattopadhyay, A. Transferrin–Copper Nanocluster–Doxorubicin Nanoparticles as Targeted Theranostic Cancer Nanodrug. ACS Appl. Mater. /& interfaces 2018, 10, 3282–3294. [CrossRef]
- Aboeita, N.M.; Fahmy, S.A.; El-Sayed, M.M.H.; Azzazy, H.M.E.-S.; Shoeib, T. Enhanced Anticancer Activity of Nedaplatin Loaded onto Copper Nanoparticles Synthesized Using Red Algae. Pharmaceutics 2022, 14, 418. [CrossRef]
- Li, N.; Sun, Q.; Yu, Z.; Gao, X.; Pan, W.; Wan, X.; Tang, B. Nuclear-Targeted Photothermal Therapy Prevents Cancer Recurrence with near-Infrared Triggered Copper Sulfide Nanoparticles. ACS Nano 2018, 12, 5197–5206. [CrossRef]
- Zhou, M.; Melancon, M.; Stafford, R.J.; Li, J.; Nick, A.M.; Tian, M.; Sood, A.K.; Li, C. Precision Nanomedicine Using Dual PET and MR Temperature Imaging–Guided Photothermal Therapy. J. Nucl. Med. 2016, 57, 1778–1783. [CrossRef]
- Shah, M.; Murad, W.; Mubin, S.; Ullah, O.; Rehman, N.U.; Rahman, M.H. Multiple Health Benefits of Curcumin and Its Therapeutic Potential. Environ. Sci. Pollut. Res. 2022, 29, 43732–43744. [CrossRef]
- Yang, Y.; Liang, S.; Geng, H.; Xiong, M.; Li, M.; Su, Q.; Jia, F.; Zhao, Y.; Wang, K.; Jiang, J.; et al. Proteomics Revealed the Crosstalk between Copper Stress and Cuproptosis, and Explored the Feasibility of Curcumin as Anticancer Copper Ionophore. Free Radic. Biol. Med. 2022, 193, 638–647. [CrossRef]
- Giordano, A.; Tommonaro, G. Curcumin and Cancer. Nutrients 2019, 11, 2376. [CrossRef]
- Pourhanifeh, M.H.; Darvish, M.; Tabatabaeian, J.; Fard, M.R.; Mottaghi, R.; Azadchehr, M.J.; Jahanshahi, M.; Sahebkar, A.; Mirzaei, H. Therapeutic Role of Curcumin and Its Novel Formulations in Gynecological Cancers. J. Ovarian Res. 2020, 13, 1–16. [CrossRef]
- Greish, K.; Pittalà, V.; Taurin, S.; Taha, S.; Bahman, F.; Mathur, A.; Jasim, A.; Mohammed, F.; El-Deeb, I.M.; Fredericks, S.; et al. Curcumin–Copper Complex Nanoparticles for the Management of Triple-Negative Breast Cancer. Nanomaterials 2018, 8, 884. [CrossRef]
- Luo, C.-Q.; Xing, L.; Cui, P.-F.; Qiao, J.-B.; He, Y.-J.; Chen, B.-A.; Jin, L.; Jiang, H.-L. Curcumin-Coordinated Nanoparticles with Improved Stability for Reactive Oxygen Species-Responsive Drug Delivery in Lung Cancer Therapy. Int. J. Nanomedicine 2017, 12, 855–869. [CrossRef]
- Sirohi, V.K.; Popli, P.; Sankhwar, P.; Kaushal, J.B.; Gupta, K.; Manohar, M.; Dwivedi, A. Curcumin Exhibits Anti-Tumor Effect and Attenuates Cellular Migration via Slit-2 Mediated down-Regulation of SDF-1 and CXCR4 in Endometrial Adenocarcinoma Cells. J. Nutr. Biochem. 2017, 44, 60–70. [CrossRef]
- Chen, Q.; Gao, Q.; Chen, K.; Wang, Y.; Chen, L.; Li, X.U. Curcumin Suppresses Migration and Invasion of Human Endometrial Carcinoma Cells. Oncol. Lett. 2015, 10, 1297–1302. [CrossRef]
- Sun, M.-X.; Yu, F.; Gong, M.-L.; Fan, G.-L.; Liu, C.-X. Effects of Curcumin on the Role of MMP-2 in Endometrial Cancer Cell Proliferation and Invasion. Eur. Rev. Med. /& Pharmacol. Sci. 2018, 22, 5033–5041. [CrossRef]
- Ghasemi, F.; Shafiee, M.; Banikazemi, Z.; Pourhanifeh, M.H.; Khanbabaei, H.; Shamshirian, A.; Moghadam, S.A.; ArefNezhad, R.; Sahebkar, A.; Avan, A.; et al. Curcumin Inhibits NF-KB and Wnt/β-Catenin Pathways in Cervical Cancer Cells. Pathol. Pract. 2019, 215, 152556. [CrossRef]
- Kim, B.; Kim, H.S.; Jung, E.-J.; Lee, J.Y.; K.; Tsang, B.; Lim, J.M.; Song, Y.S. Curcumin Induces ER Stress-Mediated Apoptosis through Selective Generation of Reactive Oxygen Species in Cervical Cancer Cells. Mol. Carcinog. 2016, 55, 918–928. [CrossRef]
- Liu, X.; Qi, M.; Li, X.; Wang, J.; Wang, M. Curcumin: A Natural Organic Component That Plays a Multi-Faceted Role in Ovarian Cancer. J. Ovarian Res. 2023, 16, 47. [CrossRef]
- Reddy, P.S.; Begum, N.; Mutha, S.; Bakshi, V. Beneficial Effect of Curcumin in Letrozole Induced Polycystic Ovary Syndrome. Asian Pacific J. Reprod. 2016, 5, 116–122. [CrossRef]
- Mohammadi, S.; Kayedpoor, P.; Karimzadeh-Bardei, L.; Nabiuni, M. The Effect of Curcumin on TNF-α, IL-6 and CRP Expression in a Model of Polycystic Ovary Syndrome as an Inflammation State. J. Reprod. /& Infertil. 2017, 18, 352–360.
- Abuelezz, N.Z.; Shabana, M.E.; Abdel-Mageed, H.M.; Rashed, L.; Morcos, G.N.B. Nanocurcumin Alleviates Insulin Resistance and Pancreatic Deficits in Polycystic Ovary Syndrome Rats: Insights on PI3K/AkT/MTOR and TNF-α Modulations. Life Sci. 2020, 256, 118003. [CrossRef]
- Jamilian, M.; Foroozanfard, F.; Kavossian, E.; Aghadavod, E.; Shafabakhsh, R.; Hoseini, A.; Asemi, Z. Effects of Curcumin on Body Weight, Glycemic Control and Serum Lipids in Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Clin. Nutr. ESPEN 2020, 36, 128–133. [CrossRef]
- Sohaei, S.; Amani, R.; Tarrahi, M.J.; Ghasemi-Tehrani, H. The Effects of Curcumin Supplementation on Glycemic Status, Lipid Profile and Hs-CRP Levels in Overweight/Obese Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Complement. Ther. Med. 2019, 47, 102201. [CrossRef]
- Kim, K.-H.; Lee, E.N.; Park, J.K.; Lee, J.-R.; Kim, J.-H.; Choi, H.-J.; Kim, B.-S.; Lee, H.-W.; Lee, K.-S.; Yoon, S. Curcumin Attenuates TNF-α-Induced Expression of Intercellular Adhesion Molecule-1, Vascular Cell Adhesion Molecule-1 and Proinflammatory Cytokines in Human Endometriotic Stromal Cells. Phyther. Res. 2012, 26, 1037–1047. [CrossRef]
- Ding, J.; Mei, S.; Cheng, W.; Ni, Z.; Yu, C. Curcumin Treats Endometriosis in Mice by the HIF Signaling Pathway. Am. J. Transl. Res. 2022, 14, 2184–2198.
- Chowdhury, I.; Banerjee, S.; Driss, A.; Xu, W.; Mehrabi, S.; Nezhat, C.; Sidell, N.; Taylor, R.N.; Thompson, W.E. Curcumin Attenuates Proangiogenic and Proinflammatory Factors in Human Eutopic Endometrial Stromal Cells through the NF-ΚB Signaling Pathway. J. Cell. Physiol. 2019, 234, 6298–6312. [CrossRef]
- Cao, H.; Wei, Y.-X.; Zhou, Q.; Zhang, Y.; Guo, X.-P.; Zhang, J. Inhibitory Effect of Curcumin in Human Endometriosis Endometrial Cells via Downregulation of Vascular Endothelial Growth Factor. Mol. Med. Rep. 2017, 16, 5611–5617. [CrossRef]
- Zhang, Y.; Cao, H.; Yu, Z.; Peng, H.-Y.; Zhang, C. Curcumin Inhibits Endometriosis Endometrial Cells by Reducing Estradiol Production. Iran. J. Reprod. Med. 2013, 11, 415–422.
- Jana, S.; Paul, S.; Swarnakar, S. Curcumin as Anti-Endometriotic Agent: Implication of MMP-3 and Intrinsic Apoptotic Pathway. Biochem. Pharmacol. 2012, 83, 797–804. [CrossRef]
- Fadin, M.; Nicoletti, M.C.; Pellizzato, M.; Accardi, M.; Baietti, M.G.; Fratter, A. Effectiveness of the Integration of Quercetin, Turmeric, and N-Acetylcysteine in Reducing Inflammation and Pain Associated with Endometriosis. In-Vitro and in-Vivo Studies. Minerva Ginecol. 2020, 72, 285–291. [CrossRef]
- Meresman, G.F.; Götte, M.; Laschke, M.W. Plants as Source of New Therapies for Endometriosis: A Review of Preclinical and Clinical Studies. Hum. Reprod. Update 2021, 27, 367–392. [CrossRef]
- Zhu, J.-J.; Jiang, J.-G. Pharmacological and Nutritional Effects of Natural Coumarins and Their Structure–Activity Relationships. Mol. Nutr. /& food Res. 2018, 62, e1701073. [CrossRef]
- Pivetta, T.; Valletta, E.; Ferino, G.; Isaia, F.; Pani, A.; Vascellari, S.; Castellano, C.; Demartin, F.; Cabiddu, M.G.; Cadoni, E. Novel Coumarins and Related Copper Complexes with Biological Activity: DNA Binding, Molecular Docking and in Vitro Antiproliferative Activity. J. Inorg. Biochem. 2017, 177, 101–109. [CrossRef]
- Khan, S.; Zafar, A.; Naseem, I. Redox Cycling of Copper by Coumarin-Di (2-Picolyl) Amine Hybrid Molecule Leads to ROS-Mediated Modulation of Redox Scavengers, DNA Damage and Cell Death in Diethylnitrosamine Induced Hepatocellular Carcinoma. Bioorg. Chem. 2020, 99, 103818. [CrossRef]
- Stepanenko, I.; Babak, M. V.; Spengler, G.; Hammerstad, M.; Popovic-Bijelic, A.; Shova, S.; Büchel, G.E.; Darvasiova, D.; Rapta, P.; Arion, V.B. Coumarin-Based Triapine Derivatives and Their Copper (II) Complexes: Synthesis, Cytotoxicity and MR2 RNR Inhibition Activity. Biomolecules 2021, 11, 862. [CrossRef]
- Lu, W.; Tang, J.; Gu, Z.; Sun, L.; Wei, H.; Wang, Y.; Yang, S.; Chi, X.; Xu, L. Crystal Structure, in Vitro Cytotoxicity, DNA Binding and DFT Calculations of New Copper (II) Complexes with Coumarin-Amide Ligand. J. Inorg. Biochem. 2023, 238, 112030. [CrossRef]
- An, G.; Park, S.; Lee, M.; Lim, W.; Song, G. Antiproliferative Effect of 4-Methylumbelliferone in Epithelial Ovarian Cancer Cells Is Mediated by Disruption of Intracellular Homeostasis and Regulation of PI3K/AKT and MAPK Signaling. Pharmaceutics 2020, 12, 640. [CrossRef]
- Liang, J.; Zhou, J.; Xu, Y.; Huang, X.; Wang, X.; Huang, W.; Li, H. Osthole Inhibits Ovarian Carcinoma Cells through LC3-Mediated Autophagy and GSDME-Dependent Pyroptosis except for Apoptosis. Eur. J. Pharmacol. 2020, 874, 172990. [CrossRef]
- Che, Y.; Li, J.; Li, Z.; Li, J.; Wang, S.; Yan, Y.; Zou, K.; Zou, L. Osthole Enhances Antitumor Activity and Irradiation Sensitivity of Cervical Cancer Cells by Suppressing ATM/NF-ΚB Signaling. Oncol. Rep. 2018, 40, 737–747. [CrossRef]
- Su, J.; Zhang, F.; Li, X.; Liu, Z. Osthole Promotes the Suppressive Effects of Cisplatin on NRF2 Expression to Prevent Drug-Resistant Cervical Cancer Progression. Biochem. Biophys. Res. Commun. 2019, 514, 510–517. [CrossRef]
- Zhu, M.-L.; Li, J.-C.; Wang, L.; Zhong, X.; Zhang, Y.-W.; Tan, R.-Z.; Wang, H.-L.; Fan, J.-M.; Wang, L. Decursin Inhibits the Growth of HeLa Cervical Cancer Cells through PI3K/Akt Signaling. J. Asian Nat. Prod. Res. 2021, 23, 584–595. [CrossRef]
- Tian, Q.; Wang, L.; Sun, X.; Zeng, F.; Pan, Q.; Xue, M. Scopoletin Exerts Anticancer Effects on Human Cervical Cancer Cell Lines by Triggering Apoptosis, Cell Cycle Arrest, Inhibition of Cell Invasion and PI3K/AKT Signalling Pathway. J BUON 2019, 24, 997–1002.
- Ma, T.; Liu, P.; Wei, J.; Zhao, M.; Yao, X.; Luo, X.; Xu, S. Imperatorin Alleviated Endometriosis by Inhibiting the Activation of PI3K/Akt/NF-ΚB Pathway in Rats. Life Sci. 2021, 274, 119291. [CrossRef]
- Abizadeh, M.; Novin, M.G.; Amidi, F.; Ziaei, S.A.; Abdollahifar, M.A.; Nazarian, H. Potential of Auraptene in Improvement of Oocyte Maturation, Fertilization Rate, and Inflammation in Polycystic Ovary Syndrome Mouse Model. Reprod. Sci. 2020, 27, 1742–1751. [CrossRef]
- Kim, Y.H.; Lee, S.Y.; Kim, E.Y.; Kim, K.H.; Koong, M.K.; Lee, K.A. The Antioxidant Auraptene Improves Aged Oocyte Quality and Embryo Development in Mice. Antioxidants 2023, 12. [CrossRef]
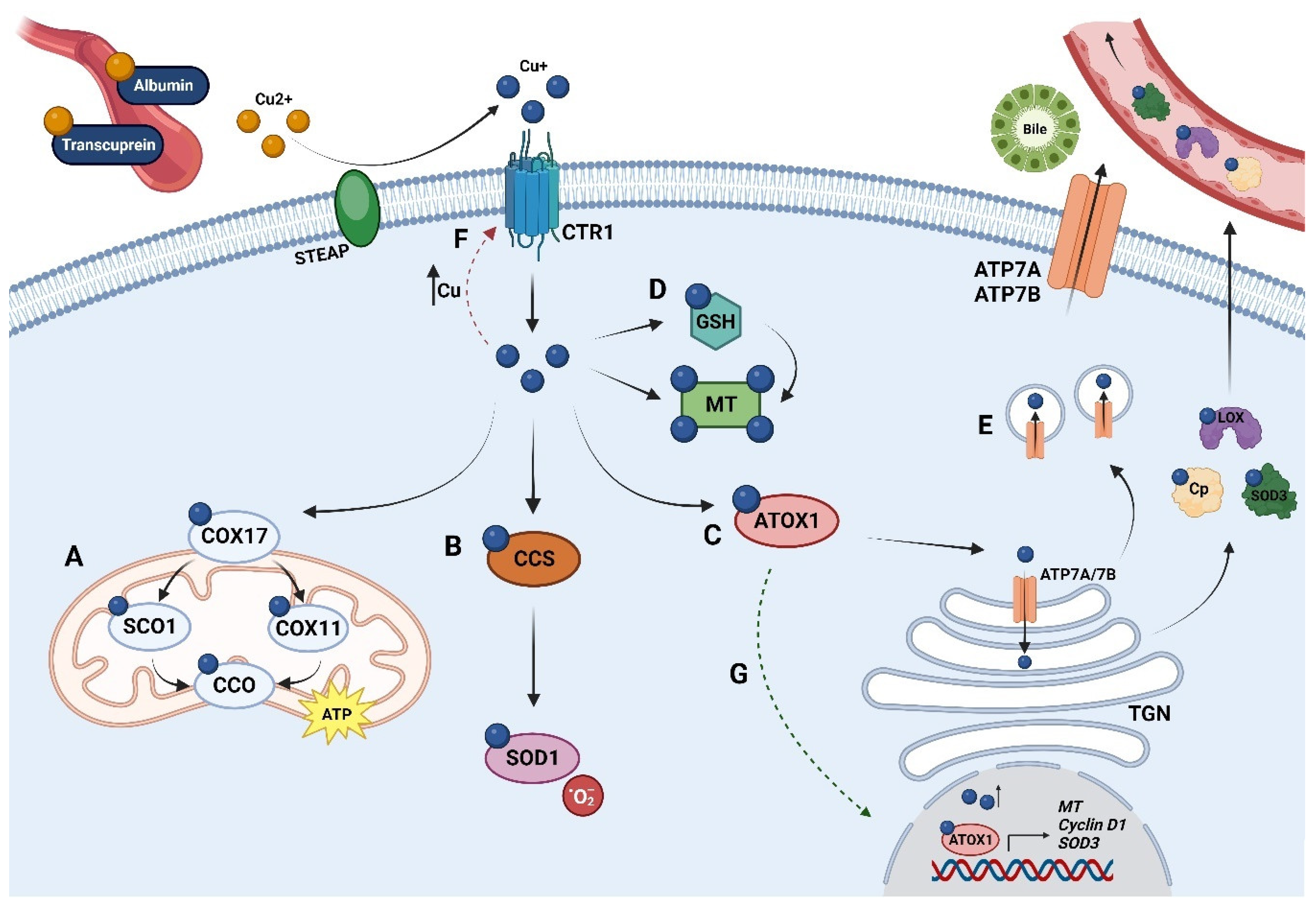
| Cuproenzyme | Function |
|---|---|
| LOX | Required for the formation of the extracellular matrix. |
| SOD | Catalyzes the conversion of superoxide radicals to molecular oxygen and hydrogen peroxide. |
| Cp | Multicopper ferroxidase; principal Cu carrier in serum. |
| Hephaestin | Multicopper ferroxidase. It supports the transportation of Fe released from intestinal enterocytes. |
| CCO | Electron transfer protein. It catalyzes ATP production. |
| Tyrosinase | Catalyzes phenol oxidation; it is required for melanin synthesis, a fundamental pigment for hair, skin, and eyes. |
| DβH | Oxidoreductase. It catalyzes the conversion of dopamine to epinephrine. |
| MEK | Kinases that belong to the mitogen-activated protein kinase cascade and that mainly promote cell proliferation and survival. |
| ULK1/2 | Autophagy-initiating kinases. |
| MEMO1 | Regulation of cell motility and ROS production. |
| Compound name | Chemical formula | Structural formula 1 |
|---|---|---|
| D-penicillamine | C5H11NO2S |  |
| Trientine | C6H18N4 |  |
| Tetrathiomolybdate | MoS4 |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





