1. Introduction
Stroke remain the second leading cause of death (11·6% of total deaths) and the third-leading cause of death and disability combined (5·7% of total disability-adjusted life-years) worldwide. Globally, the incidence of strokes is increasing due to the growth of the elderly population, as well as the costs related with this disease [
1]. The 2015 stroke statistical reports showed that in Europe, the country with the highest rates of new strokes and deaths due to stroke is Romania [
2].
Although intravenous tissue plasminogen activator (rt-PA) has been shown to be effective in the treatment of acute ischemic stroke (AIS) by administration within the first 4.5 hours of the onset of symptoms [
3], only a small proportion of stroke patients receive this drug [
4]. Low administration rate is mainly due to delayed presentation of patients to the emergency department (ED) or lack of a stroke team/unit in most of the hospitals [
4].
The current guidelines and local protocols for the early management of patients with acute ischemic stroke highlight the importance of recognition of stroke symptoms and signs as early as possible by the prehospital services. Moreover, the use of prehospital emergency medical services was associated with earlier admission to the emergency department (<3 hours), faster clinical assessment, shorter door-to-imaging time (<25 min), faster administration of rt-PA (<60 min), thus increasing the number of patients eligible for the administration of thrombolytics [
5,
6].
Despite this knowledge, there is a lack of implementation and awareness of medical staff regarding ED time targets in the initial admission of AIS patients to a hospital emergency department without a stroke team or unit. Therefore, it is critical to investigate how to increased rt-PA administration rate, even more that in Romania according to the National Program of Priority Actions in the Interventional Treatment of Patients with Acute Cerebral Vascular Accident (PA-CVA) registry, founded in 2018 by the Romanian Neurology Society board [
7,
8] the rate of thrombolysis is lower than 10 % (around 8.7%).
For this reason, the objective of this study is to analyze ED time targets and the rate of rt-PA intravenous administration after the initial admission of patients with AIS in a ED from a traditional healthcare center (without a neurologist or stroke team/unit).
2. Materials and Methods
2.1. Study Population, inclusion, and exclusion criteria
This is an observational study with a retrospective cohort design that included patients with code stroke activated who address our Emergency Department located in a hospital without neurologists or stroke unit. The study was carried out in Timisoara, Romania, at the Emergency Municipal Clinical Hospital, the second-largest hospital in county with about 30.000 annual ED patient admission and access to CT imaging possible 24/7.
Consecutive patients on whom all medical records (electronic and paper) were available with an ED diagnosis of acute ischemic stroke were identified (n=270), and only 202 patients that meet the inclusion criteria were included in time of thrombolysis (and in whom according to the local protocol [
6], intravenous thrombolysis with rt-PA was initiated only when the time interval from the first symptoms of stroke to the time of administration is less than 4.5 hours). The study data was collected from January 2019 to December 2022. Due to analyze which factors influence administration of rt-PA we split the sample into two groups: group No rt-PA (n=137) and group rt-PA (n=65) based on performing or no intravenous thrombolysis.
Were excluded from this study patients aged below 18 years and/or had an initial diagnosis of intracerebral hemorrhage and/or brain tumor. Patients who address our ED after more than 3 hours from stroke onset symptoms were also excluded from this study. We included only patients with less than 3 hours from the onset of stroke symptoms in order that performing or no intravenous thrombolysis to not be influence due to their initial admission to an ED from a hospital with no stroke team or unit and interhospital transfer time.
The time of onset of stroke-related symptoms and the time of arrival at the ED were recorded at admission. The time of onset of symptoms was defined as the time when the first stroke- related symptoms were noticed according to the patients or their relatives. In patients who experienced symptoms during sleep, time of onset of symptoms was defined as the last time when they were without symptoms. The time of arrival at the ED was defined as the time of registration at the ED triage office. The Door-in-Door-out Time was calculated as the interval between hospital arrival and transfer out of the emergency department to another hospital with stroke team and where the thrombolysis was performed or not. All times analyzed was measured in minutes. The Joint Commission and Brain Attack Coalition have recommended a target door-in-door-out time of ≤120 minutes, but limited data have been available on this important process metric [
9]. Our local protocol [
6], recommend the same time target for stroke management.
2.2. Evaluation of stroke
As soon as possible after admission in our Emergency Department a cerebral computed tomography (CT) examination with or without contrast, complete blood count, International normalized ratio (INR), prothrombin time, partial prothrombin time, blood glucose, and electrolytes test was performed for all patients. We do not include patients without medical data. The subtype, severity, and location of the stroke were diagnosed by the radiologist who performed the brain imaging in collaboration with the emergency medicine physician who performed the clinical examination.
All patients in time of thrombolysis (according to our local protocol - symptoms onset < 4.5 h [
6]) were immediately transfer to the largest near county hospital that has stroke teams but not dedicated stroke unit and where thrombolysis was performed. The distance between both hospitals is 3.5 km and around 7-10 minutes by ambulance.
The diagnosis of AIS was made based on The World Health Organization definition of stroke (introduced in 1970 and still used) defined as a “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death (unless interrupted by surgery or medication), with no apparent cause other than that of vascular origin” [
10,
11].
Neurological deficit was assessed by the neurologist and categorized using the National Institutes of Health Stroke Scale (NIHSS) at the time of admission in Neurology Department, at 1 h, 2 h and at 24 hours. NIHSS which 0 = no stroke symptoms, 1 − 4 = minor stroke, 5 − 15 = moderate stroke, 16–20 = moderate/severe stroke, and 21–42 = severe stroke [
12].
2.3. Data Analysis
Continuous variables were presented as mean and standard deviation or median and interquartile range (IQR), and categorical variables were presented as frequency and percentages. To check the distribution of continuous variables we employed Shapiro-Wilk test. To compare patient’s characteristics with and without thombolysis we employed unparied T-test or Mann-Whitney U test and Chi-square test. In order to check the independent factors associated with performing or no thombolysis we employed several models of multivariate logistic regression. Odd ratio and 95% confidence interval were presented. A p-value < 0.05 was considered statistically significant. Data analysis was performed using IBM SPSS Statistics version 26.0 (IBM Corp, Armonk, NY, USA).
3. Results
3.1. Baseline characteristics of patients who arrived at the emergency department.
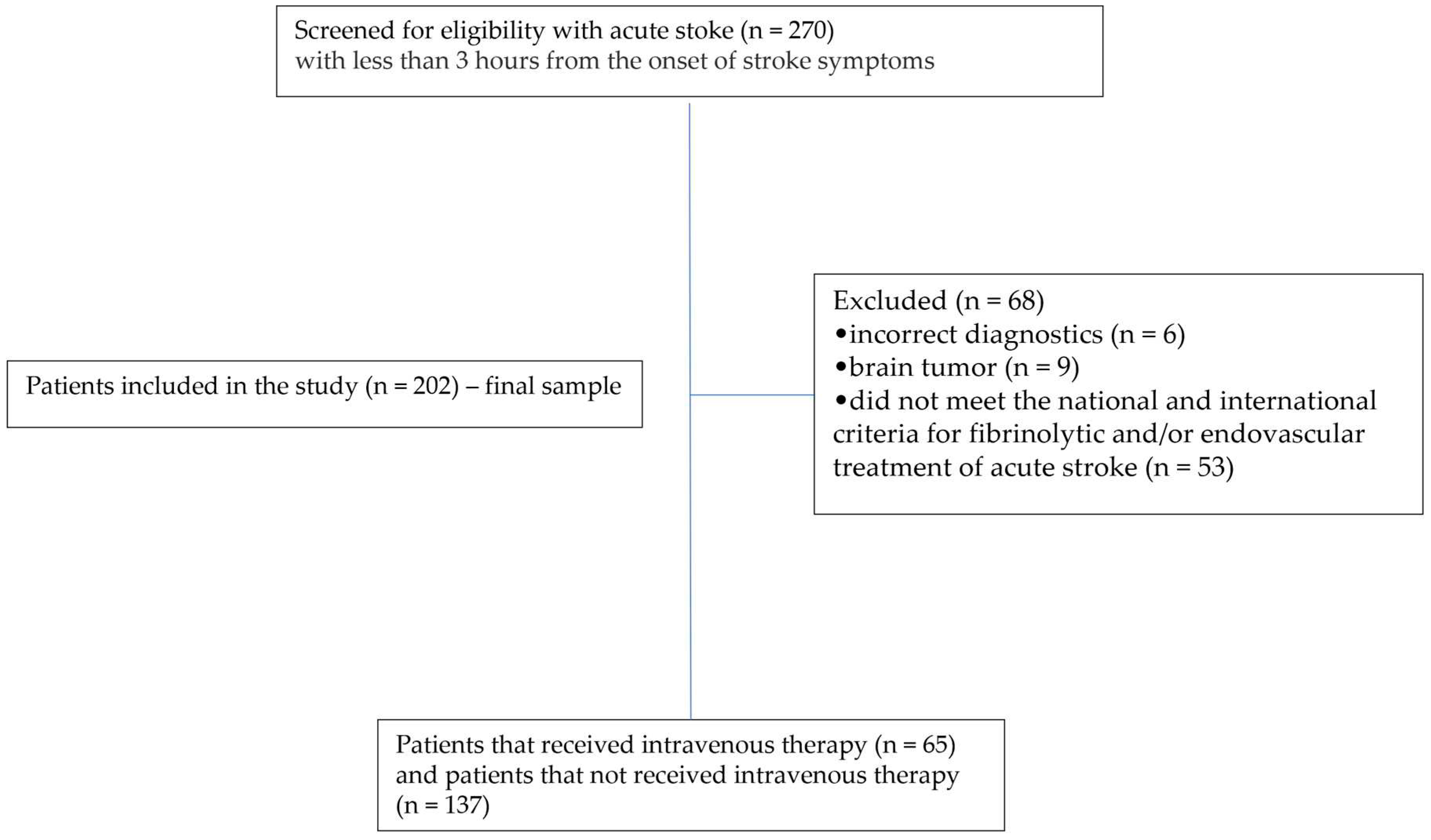
As is seen in the study flowchart represented in
Figure 1, where a total of 270 patients
with less than 3 hours from the onset of stroke symptoms were screened for eligibility to performed intravenous reperfusion therapy. Only patients (n=202) were included in the final sample of this study. Sixty-eight patients were excluded because the CT examination showed brain tumor, four because of the incorrect diagnostics and 330 patients because they do not
meet the national and international criteria for fibrinolytic and/or endovascular treatment of acute stroke. Among 202 consecutive patients included in the final sample, 65 received intravenous thrombolytic therapy (rt-PA group) and 137 patients did not receive intravenous thrombolytic therapy (No rt-PA group).
The study cohort consisted of 202 patients with acute stroke, 51.98 % (n=105) of whom were women and 60.40 % (n=122) had urban origin. The median age was 74 years with an interquartile range of 62-81 years. Systolic blood pressure had a mean of 160 mmHg with an interquartile range of 140-190 mmHg, diastolic blood pressure a mean of 90 mmHg with an interquartile range of 80-100 mmHg. INR had an interquartile range of 1.03-1.4 with a mean of 1.13. (
Table 1)
Analyzing ED time targets we found that the median onset-to-ED door time was 180 minutes (IQR, 120-217.5 minutes), door-to-physician time was 4 minutes (IQR, 3-7 minutes), door-to-CT time was 52 minutes (IQR, 48-55 minutes), and door-in-door-out time was 61 minutes (IQR, 59-65 minutes). NIHSS at admission to stroke team was 13.5 (IQR, 10-18) and at 24 h was 11 (4-18). Only 32.18 % (n=65) performed thrombolysis. The most frequent symptom of AIS was right hemiparesis present in 35.14% (n=71) of patients and the rarest symptom was headache present in only 7 patients (3.47%). Arterial hypertension (82.18 % of patients) was the most frequent risk factors for stroke, followed by diabetes mellitus (26.73% of patients) and smoking (18.32 % of patients). About 14.39 % arrived by private vehicle at the ED, while the majority (68.32 %) arrived by ambulance with doctor and 17.33 % arrived by ambulance with assistant/paramedic. From all patients with AIS, 35.15 % (n=71) had died during hospitalization, 4.95 % (n= 10) remained with dependent disability and 59.90 % (n=121) was discharged with absence of disability. (
Table 1)
Figure 1. This is a figure. Schemes follow the same formatting.
3.2. Analysis of patients’ characteristics between the two groups
By applying the Mann-Whitney U Test we observed that age (p=0.525), INR values (p=0.328), ED time targets such as door-to physician time (p=0.245), door-to-CT time (p=0.219), door-to-transfer (p=0.24), or NIHSS at admission to Neurology department (p=0.405), or NIHSS after 24 h (p=0.9) did not have a statistically significant effect on administration or no rt-PA treatment in patients included in our study. (
Table 2)
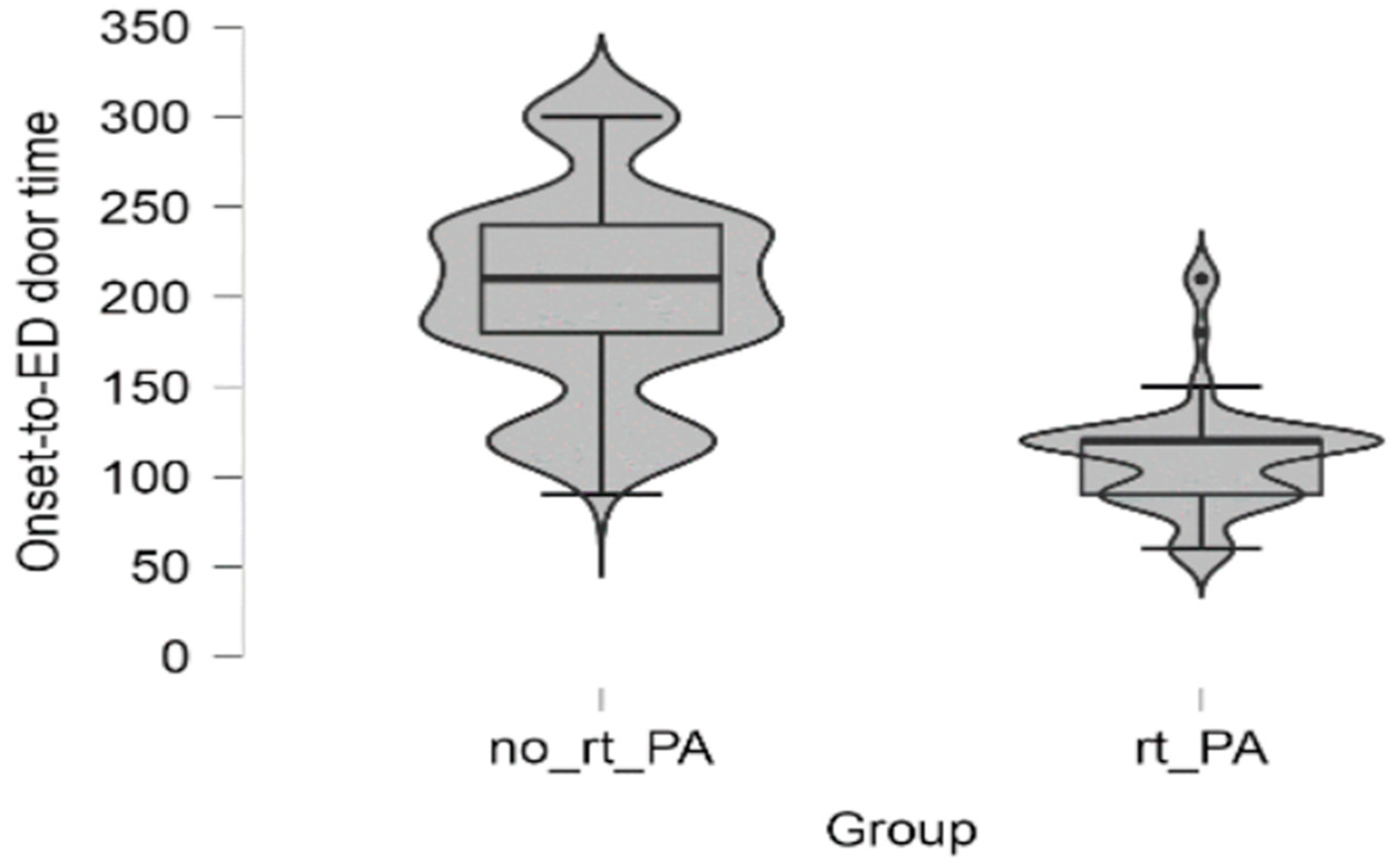
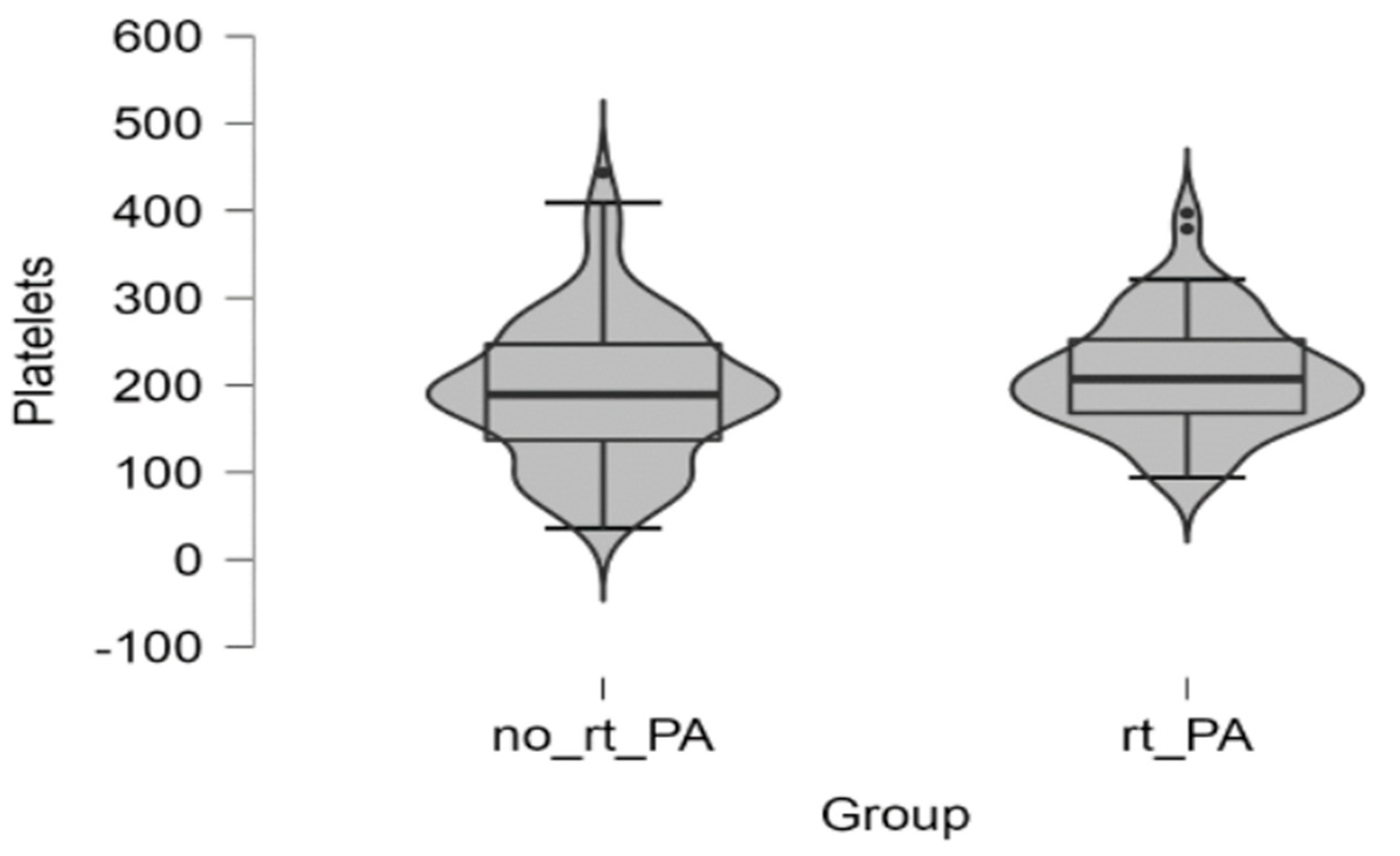
Only high platelets count (p=0.044) and lower onset-to-ED door time were statistically significant correlated with administration of rt-PA treatment (p<0.001). (
Figure 2A and
Figure 2B)
3.3. Analysis of outcomes and factors frequency associated with administration of intravenous rt-PA between the two groups.
No statistically significant correlation was found between the two groups regarding arrival mode type at ED (p=0.958), or risk factor like presence of obesity (p=0.755), smoking (p=0.971), alcohol (p=0.068), arterial hypertension (p=0.237), diabetes mellitus (p=0.866), atrial fibrillation (p=0.308) or vitamin K antagonists’ treatment (p=0.334).
Totally, seventy-one patients (33.6% patients from No rt-PA group and 38.5 % from rt-PA group) died. Ten patients, six patients (4.4 % from No rt-PA group) and four patients (6.2 % from rt-PA group) remained with disability after hospitalization period. After comparing outcomes between groups, it was observed no statistically significant correlation (p=0.636).
Table 3.
Outcomes and factors frequency between two groups.
Table 3.
Outcomes and factors frequency between two groups.
| Variable |
No rt-PA (n = 137) |
rt-PA (n = 65) |
P Chi2 test |
| Arrival Mode |
| Ambulance with assistant/paramedic (yes) |
24 (17.5 %) |
11 (15.9 %) |
0.958 |
| Ambulance with doctor (yes) |
94 (68.6 %) |
44 (67.7%) |
| Private vehicle (yes) |
19 (13.9 %) |
10 (15.4%) |
| Risk factors |
| Obesity (yes) |
9 (75.0 %) |
3 (25.0 %) |
0.755 |
| Smoking (yes) |
25 (67.6 %) |
12 (32.4%) |
0.971 |
| Alcohol (yes) |
27 (81.8%) |
6 (18.2 %) |
0.068 |
| Arterial hypertension (yes) |
116 (69.9%) |
50 (30.1%) |
0.237 |
| Diabetes mellitus (yes) |
36 (66.7%) |
18 (33.3%) |
0.866 |
| Atrial fibrillation |
40 (74.1%) |
14 (25.5%) |
0.308 |
|
Vitamin K antagonists’ treatment (yes)
|
27 (75.0%) |
9 (25.0%) |
0.334 |
| Outcomes |
|
Dependent (disability)
|
6 (4.4 %) |
4 (6.2 %) |
0.636 |
| Death |
46 (33.6 %) |
25 (38.5%) |
|
Independent (absence of disability)
|
36 (55.4%) |
85 (62.0%) |
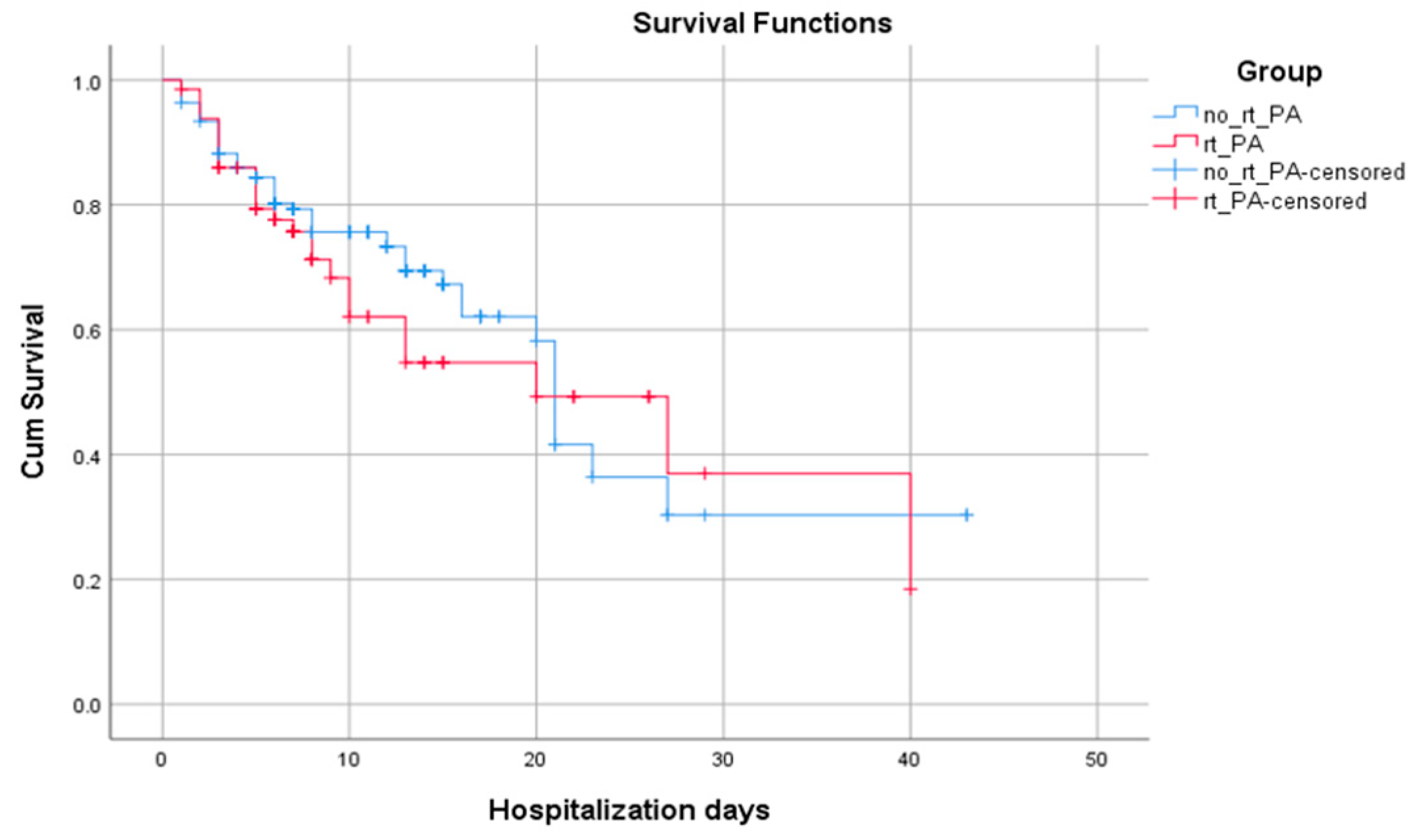
3.4. The association between administration or no of rt-PA treatment with hospitalization days and length of survival
In the context of analyze patient survival we compare the cum survival curves of those who received intravenous rt-PA and those who did not by performing logistic regression analysis and we found that the mean of hospitalization days is insignificantly higher for the No rt-PA group (p=0.455) (
Figure 3).
Table 4.
Mean survival time between the two groups.
Table 4.
Mean survival time between the two groups.
| Means and Medians for Survival Time |
| Group |
Meana
|
Median |
| Estimate |
Std. Error |
95% Confidence Interval |
Estimate |
Std. Error |
95% Confidence Interval |
| Lower Bound |
Upper Bound |
Lower Bound |
Upper Bound |
| No rt-PA |
23,100 |
2,190 |
18,807 |
27,393 |
21,000 |
0,506 |
20,008 |
21,992 |
| rt-PA |
22,313 |
2,766 |
16,893 |
27,734 |
20,000 |
6,010 |
8,220 |
31,780 |
| Overall |
23,364 |
1,744 |
19,946 |
26,782 |
21,000 |
1,407 |
18,241 |
23,759 |
4. Discussion
In this study of consecutive acute ischemic stroke patients admitted within 3 h of symptom onset, only 32.18 % (n=65) receive intravenous thrombolysis. Administration of rt-PA remains largely underutilized, with only 10-20% of all eligible patients estimated by recent international studies to receive the treatment [
13]. However, reporting at mean rt-PA administration rate from Romania according to the National Program of Priority Actions in the Interventional Treatment of Patients with Acute Cerebral Vascular Accident (PA-CVA) registry [
7,
8], that showed a thrombolysis rate lower than 10 % (around 8.7%), our study founding rate is increased.
Moreover, the same low rate of national thrombolysis for AIS reported by China, almost 2.4%, with a the rate of intravenous rt-PA usage only about 1.6% [
14]
.
These low administration rates have determined the evaluation of the use of rt-PA in different medical assistance settings and the elaboration of different methods to improve the proportion of patients who received this treatment. To improve ED care, in a study that analyzed all patients who present at the EDs from a city for a period of 3 years, it was noted that about 73% of patients with AIS address to ED outside the treatment window, because they waited to see if the symptoms will improve on their own [
15].
Despite the absence of a stroke team, most of the recommendations [
16] that are adopted by stroke unit centers in developed countries to achieve good outcomes in acute stroke care were also adopted in the our ED. These include "the availability and interpretation of CT scans 24/7 and the rapid performance of laboratory tests, in addition to administrative support, strong leadership and continuing education."
Among the factors associated with no receiving rt-PA in our study, no statistically significant correlation was found between the two groups regarding arrival mode type at ED (p=0.958), or risk factor like presence of obesity (p=0.755), smoking (p=0.971), alcohol (p=0.068), arterial hypertension (p=0.237), diabetes mellitus (p=0.866), atrial fibrillation (p=0.308) or
vitamin K antagonists’ treatment (p=0.334). Referring to the data from the literature, were it is reporting different proportion of arrival mode type or risk factors between groups, such as arriving during the night shift (p < 0.0001) and not by arriving with the emergency medical system (p = 0.0080) [
17] or that about 18.1% reported arriving at the ED by ambulance, while the majority arrived by private car [
18]; the fact that the proportion of risk factors and arrival mode are statistically insignificant between our study groups, we consider a strength of this study, because we can better analyze the impact of ED time targets on receiving or no rt-PA treatment in patients with AIS.
Therefore, our study sought to analyze the factors that influence ED time targets in patients with AIS. The data show that for all sample patients the median onset-to-ED door time was 180 minutes (IQR, 120-217.5 minutes), door-to-physician time was 4 minutes (IQR, 3-7 minutes), door-to-CT time was 52 minutes (IQR, 48-55 minutes), and door-in-door-out time was 61 minutes (IQR, 59-65 minutes). ED time targets such as door-to physician time (p=0.245), door-to-CT time (p=0.219), door-to-transfer (p=0.24), or NIHSS at admission to Neurology department (p=0.405), or NIHSS after 24 h (p=0.9) did not have a statistically significant effect on administration or no rt-PA treatment in patients included in our study. Only high platelets count (p=0.044) and lower onset-to-ED door time were statistically significant correlated with administration of rt-PA treatment (p<0.001). The mean door-to-CT time of 52 minutes in our study is double the target time recommended of < 25 minutes. Almost the same value of door-to-CT time (49.4 minutes) was registered in a study from Lebanon [
19]. When Stamm et al. [
9], evaluate door-in-door-out times for acute stroke transfers among 108 913 patients (mean age, 66.7years; 71.7% non-Hispanic White; 50.6% male) transferred from 1925 hospitals, the median door-in-door-out time was 174 minutes, a value almost triple compared to door-in-door-out time from present study that found a mean of 61 minutes (IQR, 59-65 minutes).
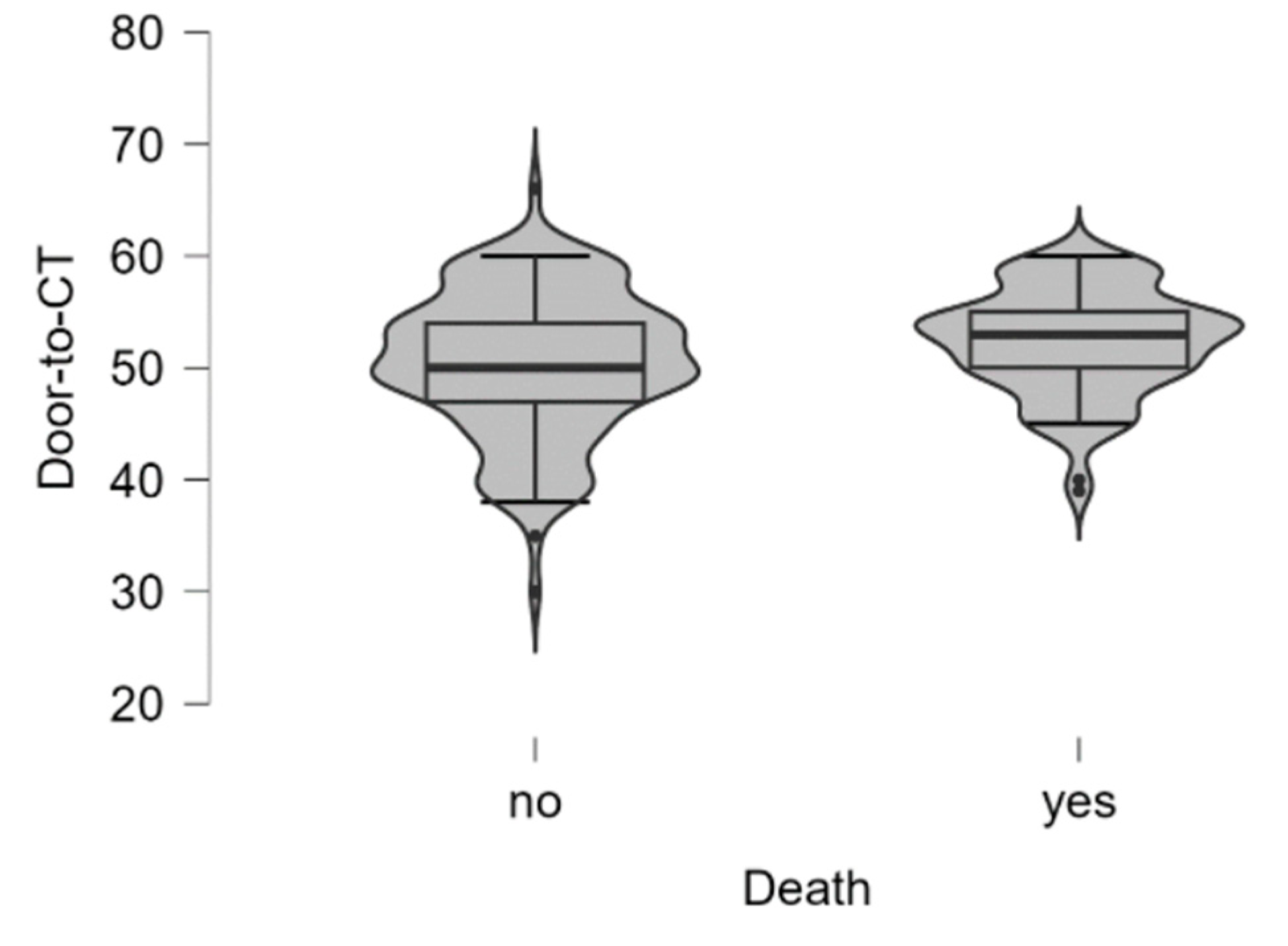
Analyzing ED time targets and death outcome for all study patients only highest Door-to-CT time (
Figure 4) was statistically significantly correlated with this outcome. In the context of analyze patient survival we compare the cum survival curves of those who received intravenous rt-PA and those who did not by performing logistic regression analysis and we found that the mean of hospitalization days is insignificantly higher for the No rt-PA group (p=0.455). In a study that also analyzed
treatment outcomes in hospitals with and without stroke units, hospitalization time was also similar in both groups (p = .191), regarding receiving or no rt-PA treatment. Neither did they observe differences between groups in the number of patients presenting disability at discharge (mRS > 2; P = .986), however, they did observe a lower rate of disability at discharge among patients who received IV-tPA than among those who did not, in both hospital groups (group A: 19 vs 30, P < .05; group B: 2 vs 41, P < .001) [
20]
.
Study limitation:
Several limitations should be considered when interpreting these data. As this study was a single hospital-based study conducted on patients belonging to a city where emergency medical systems are trained to activate stroke code and archived ED time targets, these results cannot be applied to the general population. Finally, we could not control every possible lifestyle factor, and the observational nature of this design leaves the possibility of residual confounding.
5. Conclusions
In our study, rt-PA administration rate was higher than expected. Statistically significant correlation between ED time targets was found between lower Onset-to-ED door time with administration of rt-PA treatment (p<0.001) and between highest Door-to-CT time and death outcome. Taken together, our findings suggest that hospitals without a stroke unit should restructure their AIS management by archived ED time targets as much as possible to enable a better response in AIS cases, with impact on interhospital transfer.
Public education regarding stroke is needed to reduce preadmission to ED barriers and rt-PA administration, decrease time from symptoms onset to ED presentation, and potentially improve outcomes further. A larger study would help delineate more clearly other areas for possible interventions to improve outcomes and ED management in patients with AIS.
Author Contributions
Conceptualization D.I.P., F.B. and A.I.; methodology, D.P., A.P., D.S., C.G.W., O.A.M., A.T., F.B..; software, A.T., F.B., and D.S.; validation, O.A.M.,A.I.,F.B. and C.G.W.; investigation, A.P., D.I.P., A.I and O.A.M.; resources, D.I.P. and F.B.;.; writing—original draft preparation, D.I.P, A.I. and F.B.; writing—review and editing, F.B., C.G.W., D.S and A.I, O.A.M.; visualization, O.A.M., D.S. and A.P and A.T.; supervision, O.A.M. and A.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of “Victor Babes” University of Medicine and Pharmacy Timisoara.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Feigin, V.L., et al., Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet Neurology, 2021. 20(10): p. 795-820.
-
Stroke Alliance for Europe.The Burden of Stroke in Europe—Challenges for Policy Makers. . Available online: https://www.stroke.org.uk/sites/default/files/the_burden_of_stroke_in_europe_-_challenges_for_policy_makers.pdf (accessed on 14 January 2022).
- Toyoda, K., [Intravenous rt-PA therapy for acute ischemic stroke: efficacy and limitations]. Rinsho Shinkeigaku, 2009. 49(11): p. 801-3. [CrossRef]
- Fugate, J.E. and A.A. Rabinstein, Absolute and Relative Contraindications to IV rt-PA for Acute Ischemic Stroke. Neurohospitalist, 2015. 5(3): p. 110-21. [CrossRef]
- Jauch, E.C., et al., Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 2013. 44(3): p. 870-947.
-
Priority action for interventional treatment of patients with acute stroke. Standard operating procedure regarding the patient track and therapeutic protocol in Romania. . https://legislatie.just.ro/Public/DetaliiDocument/209994 (acces on 12 octomber 2023).
- Uivarosan, D., et al., Financial Burden of Stroke Reflected in a Pilot Center for the Implementation of Thrombolysis. Medicina, 2020. 56(2): p. 54. [CrossRef]
- Sabau, M., et al., Legal medicine implications in fibrinolytic therapy of acute ischemic stroke. BMC Medical Ethics, 2019. 20(1): p. 70. [CrossRef]
- Stamm, B., et al., Door-in-Door-out Times for Interhospital Transfer of Patients With Stroke. JAMA, 2023. 330(7): p. 636-649. [CrossRef]
- Aho, K., et al., Cerebrovascular disease in the community: results of a WHO collaborative study. Bulletin of the World Health Organization, 1980. 58(1): p. 113.
- Sacco, R.L., et al., An Updated Definition of Stroke for the 21st Century. Stroke, 2013. 44(7): p. 2064-2089.
- Goldstein, L.B., C. Bertels, and J.N. Davis, Interrater reliability of the NIH stroke scale. Arch Neurol, 1989. 46(6): p. 660-2.
- de Souza, A.C., et al., Regional and national differences in stroke thrombolysis use and disparities in pricing, treatment availability, and coverage. Int J Stroke, 2022. 17(9): p. 990-996.
- Dong, Q., et al., The Chinese Stroke Association scientific statement: intravenous thrombolysis in acute ischaemic stroke. Stroke and Vascular Neurology, 2017. 2(3): p. 147-159. [CrossRef]
- Al Khathaami, A.M., et al., Factors associated with late arrival of acute stroke patients to emergency department in Saudi Arabia. SAGE Open Med, 2018. 6: p. 2050312118776719. [CrossRef]
- Alberts, M.J., et al., Revised and Updated Recommendations for the Establishment of Primary Stroke Centers. Stroke, 2011. 42(9): p. 2651-2665. [CrossRef]
- Ganti, L., et al., Impact of emergency department arrival time on door-to-needle time in patients with acute stroke. Frontiers in Neurology, 2023. 14. [CrossRef]
- Dimitriou, P., et al., Factors associated with delayed presentation at the emergency department in patients with acute ischemic stroke. Brain Inj, 2019. 33(9): p. 1257-1261. [CrossRef]
- El Sayed, M.J., T. El Zahran, and H. Tamim, Acute stroke care and thrombolytic therapy use in a tertiary care center in Lebanon. Emerg Med Int, 2014. 2014: p. 438737. [CrossRef]
- Masjuan, J., et al., Stroke treatment outcomes in hospitals with and without stroke units. Neurología (English Edition), 2020. 35(1): p. 16-23. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).