1. Introduction
Schistosomiasis is a persistent infectious disease in many low-and middle-income communities (LMICs), particularly in rural and disadvantaged communities (1-3). Nearly 240 million individuals worldwide are infected with schistosomiasis, and more than 700 million people reside in endemic regions (4). It is a common tropical disease and poverty-stricken communities, especially in Sub-Saharan Africa, are affected most adversely. In 2000 it was estimated that schistosomiasis affects almost 120 million individuals in Africa (5). South Africa is a high middle-income country but around 5.2 million individuals are affected with schistosomiasis, particularly among school-aged children and especially those living in poor communities such as Mpumalanga Province (6-9).
The common species of schistosomiasis in South Africa is Schistosoma haematobium. It is responsible for urogenital schistosomiasis characterized by blood in urine and a previous history of bilharzia (10-12). The prevalence of schistosomiasis is higher in Sub-Saharan Africa when compared to other similar tropical areas and high-income countries (5, 13, 14). In 2020, Santos and colleagues reported a 30.5% prevalence amongst the Brazilian population while in Nigeria 93.6% of urine samples tested positive for schistosomiasis (13). A 2010, study in the Eastern Cape Province (South Africa) reported a 73,2% prevalence among school children from a rural community (15).
School children from rural or poor communities are more prone to schistosomiasis infection due to socio-economic status, environmental factors and lack of access to healthcare services and infrastructure (16-18). Schistosomiasis infections are higher among school-aged children especially boys because of exposure to contaminated water sources during their outdoor activities such as swimming and playing in water (1, 19). Many rural areas do not have access to water infrastructure and healthcare services to ensure adequate prevention and prompt clinical diagnosis for appropriate management and treatment of schistosomiasis infection (6, 20).
Children with repeated infections can be affected by anemia, malnutrition, and learning difficulties. The parasite can also harm the lungs, bladder, spleen, liver, and intestines after years of infection (21). In affected areas the World Health Organisation (WHO) advocates for the treatment of preschool children with praziquantel. It is inexpensive, secure, and efficient. Treatment started and repeated in childhood reduces, if not completely reverses, the chance of developing severe illness, even if re-infection may occur following treatment (22).
Ehlanzeni District Municipality (EDM) is characterized by a high population living in rural areas (72%) and the majority lack access to safe potable water supply (23). In addition, a study reviewing prevalence between 2011-2018 in other South African provinces highlighted a concerning schistosomiasis prevalence in similar settings (rural areas) within KwaZulu-Natal, Eastern Cape, Mpumalanga and Limpopo provinces (6). Hence, this study focused on determining and describing the prevalence of schistosomiasis in a poverty-stricken district municipality (EDM) among school-aged children.
2. Materials and Methods
2.1. Study design and setting
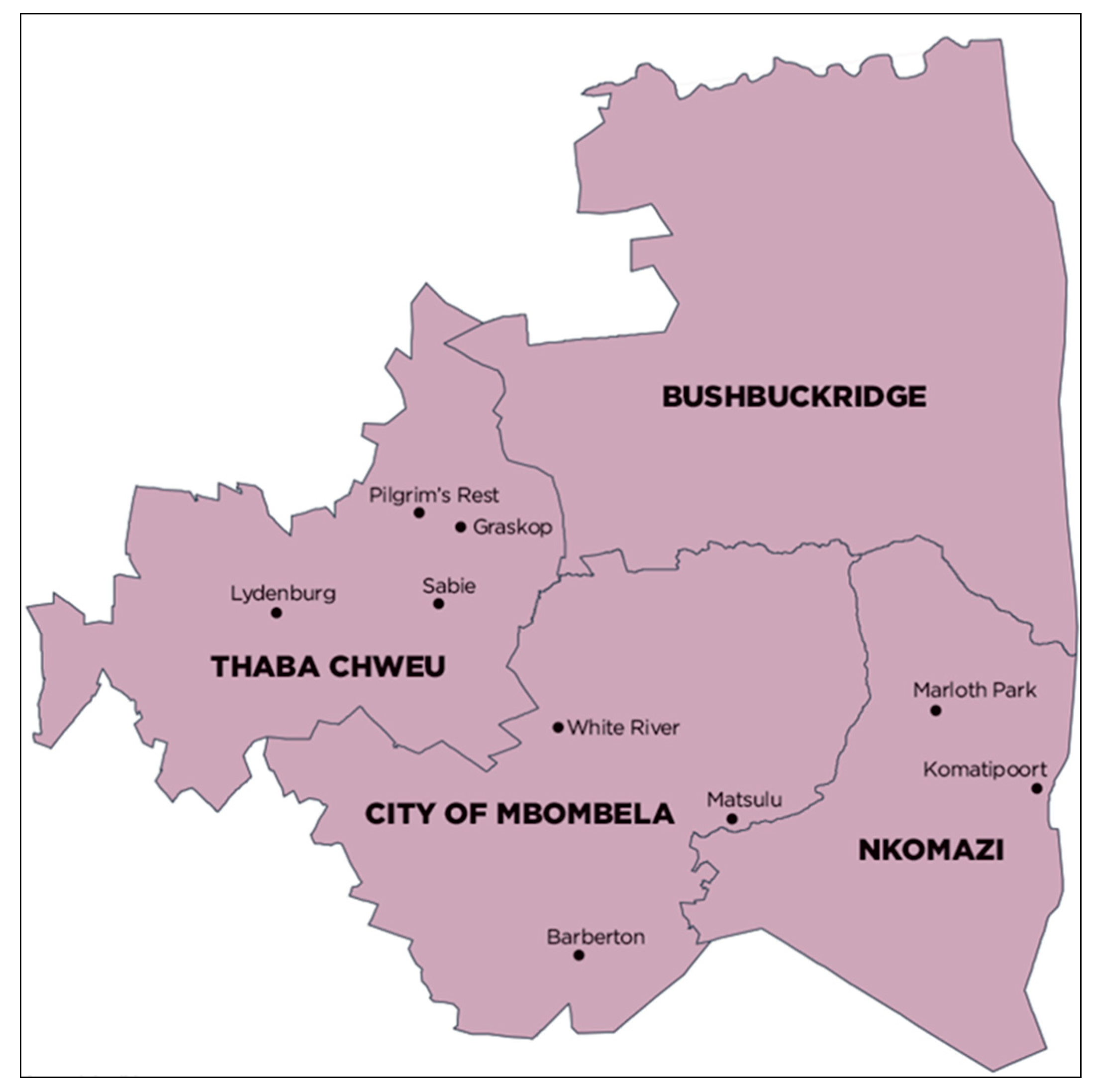
The study employed a single-stage cluster sampling approach, looking at laboratory data of all school-aged children (aged between 5-18 years of age) in Ehlanzeni District Municipality (EDM), (shown in
Figure 1), who had a urine sample tested at the National Health Laboratory Services (NHLS) that yielded a positive result for
Schistosoma haematobium on urine microscopy from 1 January 2015 to 31 December 2021. The NHLS serves more than 80% of South Africa's population as the sole provider of diagnostic pathology services through its national network of quality-assured diagnostic laboratories. Additionally, it offers assistance with surveillance for cancer, occupational health, and communicable diseases (24). The reliability of the results was determined through a quality assurance system employed by the NHLS. The system is called The Method Comparison, where patient samples (urine) are run in lab X using their procedure and the same samples are then run again in lab Y using their own procedure in order to confirm the validity of microscopy results. During validation, internal quality checks are performed. A spreadsheet was used to record the outcomes, and EP9 analysed them. EP9 is an experiment used to compare the performance of two laboratory instruments, with the intention to confirm if the two laboratory techniques provide the same results. The following factors affected reliability: 1. There was complete agreement between results that are positive (P) and negative (N), 2. Cohen's Kappa > 75%, 3. Correlation coefficient was 0.95-1.00, 4.A symmetry test was also successful (25).
Ehlanzeni District Municipality has four sub-districts in the district namely: Nkomazi, City of Mbombela, Bushbuckridge and Thaba Chweu. The estimated population of Ehlanzeni District Municipality was 1 856 753 people in 2019. Ehlanzeni District Municipality is classified as a low- and middle-income area because most of the population resides in rural areas and 77% of households survive on an average of R1600 income per month (26). In 2022, Magagula and colleagues reported that an estimated 72% of the population of the EDM resides in rural areas (23).
2.2. Study Population and Sampling
The study population was school-aged children (between 5-18 years of age) who had a urine test for Schistosoma haematobium ova from 2015 to 2021 in a healthcare facility in EDM. The study included male and female children. The records included demographics, whether there was blood in the urine and previous bilharzia. Children younger than five years old, older than 18 years old and not residing in EDM were excluded from the study.
2.3. Data collection
A respective cross-sectional study was implemented to review secondary data of children tested for Schistosoma haematobium ova in Ehlanzeni District Municipality, Mpumalanga. The review of laboratory data aimed to collect the following variables gender, age, sub-district, patient status (was the participant an outpatient or hospitalized), previous diagnosis of bilharzia (in the last six months), presence of blood in the urine, and results of schistosomiasis. We also collected the physical addresses of the patients (study participants) to determine the area variables (urban, semi-urban and rural).
The study focused on the S. haematobium species as it is the commonest parasite responsible for schistosomiasis in rural areas in similar settings in South Africa (27, 28). The urine samples were collected at the facilities where the patients sought medical attention and were transported to an accredited laboratory (that conforms to international standards) within 24 hours. The laboratory parasitological examination used the urine filtration method, which involved the identification of eggs (29-31). The following steps were followed; 10 mL of urine was mixed and shaken in a tube. Then it was filtered through the filter, thereafter a digital microscope was used to identify the presence of eggs.
2.4. Data Analysis
Secondary data was entered into Microsoft Excel 2021 for cleaning and coding purposes. It was moved to IBM Statistical Package for the Social Sciences (SPSS) version 27 for descriptive and inferential analysis. Duplicated samples (identified through personal identifiers) were removed from the data set even though they were more than three weeks later as it could not be proven whether these children were properly treated on their initial diagnosis or whether they were now subsequently reinfected. Discordant results were disregarded, cases with incomplete data on essential variables were removed, and we also ensured that samples were from Ehlanzeni district by utilizing the laboratory information system (LIS) of the NHLS. Categorical variables were used to arrange socio-demographic characteristics and schistosomiasis prevalence, these variables were presented in frequencies, percentages and proportions. To identify risk factors associated with the prevalence of schistosomiasis, logistic regression models were computed and used. The dependent variable was schistosomiasis (categorical variable: positive/negative) and the dependent variables were gender (male/female), age (1-12/13-18 years old), sub-district (Bushbuckridge/City of Mbombela/Nkomazi/Thaba Chweu), area (urban, semi-urban & rural), patient status (outpatient/hospitalized), previous history of bilharzia (yes/no) and presence of blood in urine (yes/no). A bivariate analysis was conducted and variables that were significantly associated were included in the final model (a multivariate analysis). The relationships or associations that had a p-value of 0.05 were deemed statistically significant.
2.5. Data Analysis
The study received ethical approval from the University of Johannesburg, Faculty of Health Sciences, and Research Ethics Committee with ethical clearance number REC-1867-2022. Access to secondary data was granted through the Academic and Research wing of the (NHLS), and data was received from the Corporate Data Warehouse (CDW) of the NHLS. CDW is a national archive of all data from specimens collected from all public hospitals which is supported by the laboratory information system (LIS), TrakCare.
3. Result
3.1. Socio-demographic characteristics of the study participants
A total of 24 034 children’s samples collected from 2015 -2021 were tested for
Schistosoma haematobium ova in the study. Most participants were males (n=19 795; 84%) and aged between 5-12 years old (n=13 230; 84%). More than half (n=12 179; 51%) of the study participants were from the City of Mbombela Sub-District. There were more outpatient participants (n=23 489; 98%) than those who were hospitalized (n=545; 8%). Based on the clinical diagnosis, patients who had reported a previous history of bilharzia in the last six months were 351 (2%). While urine samples with the presence of blood in the urine were 4512 (19%).
Table 1 shows a detailed description of the participants' socio-demographic characteristics.
3.2. Prevalence and distribution of Schistosoma haematobium
There were 17 095 (71%) children that tested positive for
Schistosoma haematobium and 29% (n=6 939) that tested negative in the study. Three sub-districts reported a positive case count above 50%, however, Thaba Chweu reported a number of positive cases of less than 50% as shown in
Table 2.
3.3. Relationship between the prevalence of Schistosoma haematobium and characteristics
Female children (AOR:0.38; CI 0.35-0.41) were less likely to be diagnosed with
Schistosoma haematobium in the study population. Children aged between 13-18 years old, had a history of bilharzia and had blood in their urine were at higher odds of being diagnosed with
Schistosoma haematobium, as shown in the multivariate logistic regression model (
Table 3).
4. Discussion
A higher prevalence of schistosomiasis infections is common in rural and disadvantaged communities. According to studies, the prevalence of schistosomiasis ranges from 2-85% (5). The study prevalence of schistosomiasis was 71%, which is similar to the EC prevalence in 2010 (15). A study among 4-18-year-old primary and secondary schoolchildren in Nigeria reported a prevalence of 45.6% (32). A study in another district municipality within South Africa found a prevalence of 37.5% (33). The higher prevalence in the study could be attributed to the study population, the study focused on children presenting to healthcare facilities and suspected of being infected with the disease. Most studies with lower prevalence were community surveys. In addition, the areas (sub-district) with more rural communities had a higher prevalence than Bushbuckridge (73%) and Nkomazi (51%). While a more semi-urban sub-district City of Mbombela was high (73%), the cause could be seeking access to better facilities from individuals from more rural sub-districts.
Numerous previous studies have found that being a male child is a risk factor for schistosomiasis infections (1, 34, 35). A study in Lusaka conducted among children aged 5-17 years old found that male children were at higher risk than female children to be infected with schistosomiasis infection (35). This was similar to other studies in Nigeria, Gambia, Côte d'Ivoire and elsewhere (1, 32, 36). Our findings support the narrative that male children are at a higher risk. The study found that being a female child was a protective factor (AOD:0.38,95%CI:0.35-0.41) to being infected with schistosomiasis infection. This can be attributed to girls being less involved in outdoor activities such as swimming in dams (37).
Clinical signs and symptoms such as a history of bilharzia in the past six months and the presence of blood in urine are risk factors for schistosomiasis (1, 38). A study among Eswatini senior primary school children found a significant relationship between the prevalence of urinary schistosomiasis and treatment of bilharzia in the last six months (38). Furthermore, in Gambia, Joof and colleagues found that the presence of blood in urine during urine analysis was a good predisposing indicator for schistosomiasis (1). These are important findings for early indication of suspected schistosomiasis (medical screening) and early diagnosis for appropriate treatment. It also highlights the potential role of preventive care such as health education, environmental sampling of water sources such as dams and access to adequate safe water sources.
The study's strength is the sample size, which is large. While the limitations are the study population which focuses on school children presenting at healthcare facilities and the study was a cross-sectional study. Therefore, cannot be generalized to a larger population.
5. Conclusions
The current study found a high prevalence of schistosomiasis in school-aged children within low-and middle-income communities, especially in rural-dominated areas. The significant risk factors were age, history of bilharzia and presence of blood in urine. While being a female child was a risk factor. We did not find a significant relationship between schistosomiasis with area (rural, semi-urban and urban). Based on the findings, there is a need for an interdisciplinary approach to reduce the prevalence of schistosomiasis in EDM. Tailored health education is required to be offered to children and parents, especially on the signs and symptoms, sources of infection and contributing factors in its spread. We encourage that a community survey is conducted to investigate other contributing factors in these communities.
Author Contributions
Conceptualization, Sunnieboy Njikho; Data curation, Sunnieboy Njikho and Renay Van Wyk; Formal analysis, Sunnieboy Njikho, Vanessa Quan and Renay Van Wyk; Funding acquisition, Thokozani Mbonane and Renay Van Wyk; Investigation, Sunnieboy Njikho, Vanessa Quan and Renay Van Wyk; Methodology, Sunnieboy Njikho, Vanessa Quan and Renay Van Wyk; Project administration, Renay Van Wyk; Resources, Sunnieboy Njikho and Renay Van Wyk; Supervision, Vanessa Quan and Renay Van Wyk; Validation, Vanessa Quan and Renay Van Wyk; Writing – original draft, Sunnieboy Njikho, Vanessa Quan and Renay Van Wyk; Writing – review & editing, Sunnieboy Njikho, Vanessa Quan, Thokozani Mbonane and Renay Van Wyk.
Funding
No external funding was used for this study.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and the research ethics committee of the University of Johannesburg, Faculty of Health Science, South Africa (REC-1867-2022) approved ethics, and permission was obtained from the National Health Laboratory Services. The Mpumalanga Province Health Research and Ethics Committee (MPHREC): MP_202303_001.
Informed Consent Statement
This was a cross-sectional study looking at secondary data.
Data Availability Statement
Data is available upon reasonable request and within the prescripts of the Protection of Personal Information Act (POPIAct).
Acknowledgments
We thank the National Health Laboratory Service for granting access to the secondary data and The Mpumalanga Province Health Research and Ethics Committee for supporting the project. We are thankful to Dr Sindile Ntuli for her hand in the conceptualization of the project and her inputs, as well as Mr. Phuti Sekwadi from the National Institute for Communicable Diseases (NICD) not included in the author’s contribution, who provided support to the project and advised on geo-mapping.
Conflicts of Interest
The authors disclose no conflict of interest.
References
- Joof E, Sanyang AM, Camara Y, Sey AP, Baldeh I, Jah SL, et al. Prevalence and risk factors of schistosomiasis among primary school children in four selected regions of The Gambia. PLoS Neglected Tropical Diseases. 2021;15(5):e0009380. [CrossRef]
- Sacolo H, Chimbari M, Kalinda C. Knowledge, attitudes and practices on Schistosomiasis in sub-Saharan Africa: a systematic review. BMC infectious diseases. 2018;18:1-17. [CrossRef]
- Sumbele IUN, Tabi DB, Teh RN, Njunda AL. Urogenital schistosomiasis burden in school-aged children in Tiko, Cameroon: a cross-sectional study on prevalence, intensity, knowledge and risk factors. Tropical Medicine and Health. 2021;49(1):1-10. [CrossRef]
- Assefa A, Erko B, Gundersen SG, Medhin G, Berhe N. Current status of Schistosoma mansoni infection among previously treated rural communities in the Abbey and Didessa Valleys, Western Ethiopia: Implications for sustainable control. PloS one. 2021;16(2):e0247312. [CrossRef]
- Adenowo AF, Oyinloye BE, Ogunyinka BI, Kappo AP. Impact of human schistosomiasis in sub-Saharan Africa. Brazilian Journal of Infectious Diseases. 2015;19:196-205. [CrossRef]
- De Boni L, Msimang V, De Voux A, Frean J. Trends in the prevalence of microscopically-confirmed schistosomiasis in the South African public health sector, 2011–2018. PLoS Neglected Tropical Diseases. 2021;15(9):e0009669. [CrossRef]
- Magaisa K, Taylor M, Kjetland EF, Naidoo PJ. A review of the control of schistosomiasis in South Africa. South African Journal of Science. 2015;111(11-12):1-6. [CrossRef]
- Sacolo-Gwebu H, Chimbari M, Kalinda C. Prevalence and risk factors of schistosomiasis and soil-transmitted helminthiases among preschool aged children (1–5 years) in rural KwaZulu-Natal, South Africa: a cross-sectional study. Infectious diseases of poverty. 2019;8:1-12. [CrossRef]
- Bengu MD, Dorsamy, V, Moodley, J. Schistosomiasis infections in South African pregnant women: A review.. Southern African Journal of Infectious Diseases. 2020;23(35 (1)). [CrossRef]
- Cimini A, Ricci M, Gigliotti PE, Pugliese L, Chiaravalloti A, Danieli R, et al. Medical imaging in the diagnosis of schistosomiasis: a review. Pathogens. 2021;10(8):1058. [CrossRef]
- Gray DJ, Ross AG, Li Y-S, McManus DP. Diagnosis and management of schistosomiasis. Bmj. 2011;342. [CrossRef]
- Olveda DU, Li Y, Olveda RM, Lam AK, Chau TN, Harn DA, et al. Bilharzia: pathology, diagnosis, management and control. Tropical medicine & surgery. 2013;1(4). [CrossRef]
- Santos IGdA, Bezerra LP, Cirilo TM, Silva LO, Machado JPV, Lima PD, et al. New epidemiological profile of schistosomiasis from an area of low prevalence in Brazil. Revista da Sociedade Brasileira de Medicina Tropical. 2020;53. [CrossRef]
- Houweling TA, Karim-Kos HE, Kulik MC, Stolk WA, Haagsma JA, Lenk EJ, et al. Socioeconomic inequalities in neglected tropical diseases: a systematic review. PLoS neglected tropical diseases. 2016;10(5):e0004546. [CrossRef]
- Meents EF, Boyles T. Schistosoma haematobium prevalence in school children in the rural Eastern Cape Province, South Africa. Southern African Journal of Epidemiology and Infection. 2010;25(4):28-9. [CrossRef]
- Grimes JE, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR. The roles of water, sanitation and hygiene in reducing schistosomiasis: a review. Parasites & vectors. 2015;8(1):1-16. [CrossRef]
- Angora EK, Boissier J, Menan H, Rey O, Tuo K, Touré AO, et al. Prevalence and risk factors for schistosomiasis among schoolchildren in two settings of Côte d’Ivoire. Tropical medicine and infectious disease. 2019;4(3):110. [CrossRef]
- Gazzinelli A, Velasquez-Melendez G, Crawford SB, LoVerde PT, Correa-Oliveira R, Kloos H. Socioeconomic determinants of schistosomiasis in a poor rural area in Brazil. Acta Trop. 2006;99(2-3):260-71. [CrossRef]
- Krauth SJ, Musard C, Traoré SI, Zinsstag J, Achi LY, N’Goran EK, et al. Access to, and use of, water by populations living in a schistosomiasis and fascioliasis co-endemic area of northern Côte d’Ivoire. Acta tropica. 2015;149:179-85. [CrossRef]
- Aula OP, McManus DP, Jones MK, Gordon CA. Schistosomiasis with a Focus on Africa. Tropical Medicine and Infectious Disease. 2021;6(3):109. [CrossRef]
- Centers for Disease Prevention and Control. Parasites - Schistosomiasis 2020 [cited 2020. Available from: https://www.cdc.gov/parasites/schistosomiasis/health_professionals/index.html (accessed on 25 June 2023).
- World Health Organization. Schistisomiasis 1 February 2023 [. Available from: https://www.who.int/news-room/fact-sheets/detail/schistosomiasis#:~:text=Praziquantel%20is%20the%20recommended (accessed on 25 June 2023).
- Magagula DN, Mukonza RM, Manyaka RK, Moeti K. The role of district municipalities in service provision in South Africa: Dissecting challenges faced by Ehlanzeni District Municipality. Africa’s Public Service Delivery and Performance Review. 2022;10(1):628. [CrossRef]
- National Health Laboratory Service. About Us 2023 [. Available from: https://www.nhls.ac.za/about-us/ (accessed on 25 June 2023).
- National Health Laboratory Service. Verification protocol for instrument /reagent/method number: GPL1530 Version number :11 Q Pulse. 2019 [. Available from: http://nhlssandqpulse01.nhls.ac.za/QPulse5Web/UI/Common/ModuleWrapper.aspx?module=home (accessed on 25 June 2023). [CrossRef]
- Nxesi TW. Socio-economic impact of land restitution in the Ehlanzeni District, Mpumalanga: University of the Witwatersrand, Faculty of Commerce, Law and Management …; 2016.
- Appleton C, Kvalsvig J. A school-based helminth control programme successfully implemented in KwaZulu-Natal. Southern African Journal of Epidemiology and Infection. 2006;21(2):55-67. [CrossRef]
- Berge ST, Kabatereine N, Gundersen SG, Taylor M, Kvalsvig JD, Mkhize-Kwitshana Z, et al. Generic praziquantel in South Africa: The necessity for policy change to provide cheap, safe and effcacious schistosomiasis drugs for the poor, rural population. Southern African Journal of Epidemiology and Infection. 2011;26(1):22-5. [CrossRef]
- Utzinger J, Becker S, Van Lieshout L, Van Dam G, Knopp S. New diagnostic tools in schistosomiasis. Clinical microbiology and infection. 2015;21(6):529-42. [CrossRef]
- Ibironke OA, Phillips AE, Garba A, Lamine SM, Shiff C. Diagnosis of Schistosoma haematobium by detection of specific DNA fragments from filtered urine samples. The American journal of tropical medicine and hygiene. 2011;84(6):998. [CrossRef]
- Ajibola O, Gulumbe BH, Eze AA, Obishakin E. Tools for detection of schistosomiasis in resource limited settings. Medical Sciences. 2018;6(2):39. [CrossRef]
- Abdulkareem BO, Habeeb KO, Kazeem A, Adam AO, Samuel UU. Urogenital schistosomiasis among schoolchildren and the associated risk factors in selected rural communities of Kwara state, Nigeria. Journal of tropical medicine. 2018;2018. [CrossRef]
- Kabuyaya M, Chimbari MJ, Manyangadze T, Mukaratirwa S. Schistosomiasis risk factors based on the infection status among school-going children in the Ndumo area, uMkhanyakude district, South Africa. Southern African Journal of Infectious Diseases. 2017;32(2):67-72.
- M’Bra RK, Kone B, Yapi YG, Silué KD, Sy I, Vienneau D, et al. Risk factors for schistosomiasis in an urban area in northern Côte d’Ivoire. Infectious diseases of poverty. 2018;7:1-12. [CrossRef]
- Agnew-Blais J, Carnevale J, Gropper A, Shilika E, Bail R, Ngoma M. Schistosomiasis haematobium prevalence and risk factors in a school-age population of peri-urban Lusaka, Zambia. Journal of Tropical Pediatrics. 2010;56(4):247-53. [CrossRef]
- Coulibaly, J. N′ Gbesso YK, N′ Guessan NA, Winkler MS, Utzinger J, N′ Goran EK. 2013. Epidemiology of schistosomiasis in two high-risk communities of south Côte d'ivoire with particular emphasis on pre-school-aged children Am J Trop Med Hyg.89:32-41. [CrossRef]
- Ajayi, A. Evaluation of outdoor activities in residential environments: The role of urban open spaces. Town and Regional Planning. 2022;80(1):6-20. [CrossRef]
- Maseko T, Masuku S, Dlamini S, Fan C-K. Prevalence and distribution of urinary schistosomiasis among senior primary school pupils of Siphofaneni area in the low veld of Eswatini: A cross-sectional study. Helminthologia. 2023;60(1):28-35. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).