Introduction
Intussusception is a medical condition characterized by the telescoping of one segment of the gastrointestinal tract or bowel loop into an adjacent portion. [
1] The segment or loop inside is called Intussusceptum and the receiving loop is called Intussuscipens. [
2] It is an important cause of acute abdomen pain in children. When occurring in the adult population, intussusception is usually caused by a focal lesion acting as a lead point. [
3]
Intussusception is a type of dynamic obstruction within the gastrointestinal system, primarily affecting two age groups: children and adults [
4]. Understanding the differences in presentation, etiology, and management between these age groups is essential for clinicians to provide timely and effective care.
This report narrates a specific case of duodeno-duodenal intussusception, a subtype of adult enteroenteric intussusception, in a 17-year-old female patient. It shows the importance of recognizing the different clinical scenarios that intussusception can manifest and highlights the critical role of timely radiological examination and surgical reduction to preclude significant sequelae, including bowel necrosis, particularly in cases as rare and complex as duodeno-duodenal intussusception.
Case Presentation
A 17-year-old female patient came to surgery OPD of SVP hospital, Ahmedabad with a complaint of upper abdominal pain for the last 4 days associated with vomiting containing food particles and with a history of similar complaints multiple times previously.
History of past illness
The patient had no previous medical history.
Physical examination
The patient’s temperature was 37.8 °C, heart rate was 84 bpm, respiratory rate was 18 breaths per minute and blood pressure was 122/76 mmHg. On per-abdominal examination, the patient had epigastric tenderness and pain aggravated when the legs were raised, there were no other typical pathological signs. Our first clinical considerations for the abdominal pain were as follows: Space-occupying lesions of the small intestine (possible tumor), followed by possible choledocholithiasis.
Laboratory examinations
Blood examination revealed a hemoglobin level of 11.0 g/dL (normal range > 12.0 g/dL) with a normal leukocyte count and platelet count. The serum C-reactive protein level and the prothrombin and partial thromboplastin times, the blood biochemistry, and urine analyses were normal. The electrocardiogram result was also normal. An X-ray abdomen was done but it turned out to be normal. Hence Whole abdomen USG and Abdomen CECT were done for further evaluation of the patient's condition.
Investigation & Diagnosis
On USG Examination, there is evidence of bowel within bowel appearance noted in the left hypochondriac region, suggestive of intussusception. Intussusceptum is the 3rd & 4th part of the duodenum, ampulla of Vater, head, and the uncinate process of the pancreas while Intussusipens is a jejunal loop. The Intussusceptum shows normal vascularity.
No evidence of any abnormal wall thickening of the Intussusceptum and Intussuscipens. No evidence of any discrete lesion is identified to suggest a lead point of intussusception.
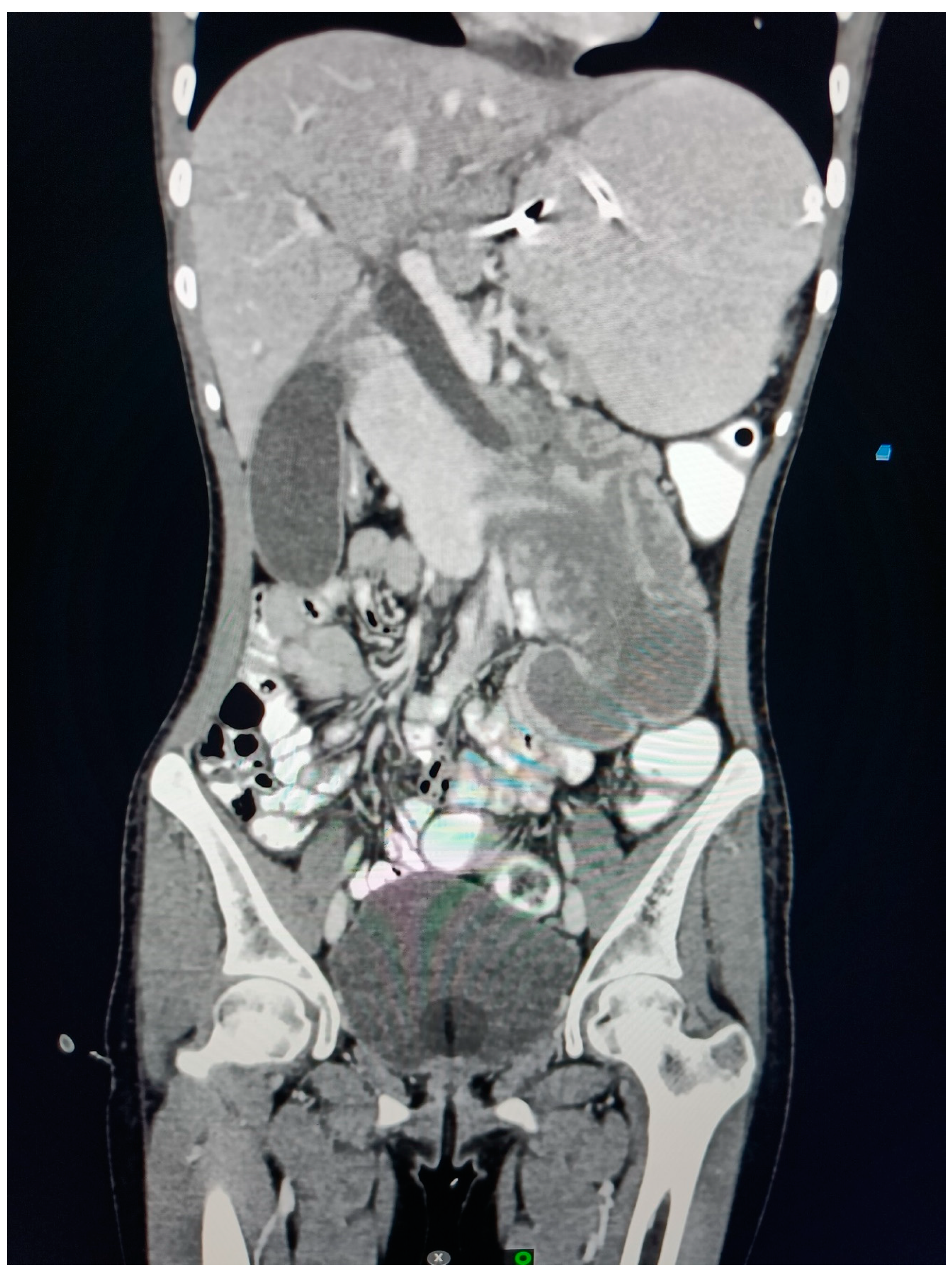
Proximal CBD measures 11 mm, Mid-CBD measures 8 mm, dilated. There is evidence of smooth tapering of distal CBD and opening into the ampulla of the Vater in the Intussusceptum. No evidence of any intraluminal calculus, or possibility of stricture formation secondary to intussusception.
A few subcentimeter-sized lymph nodes were noted in the epigastric region. The superior mesenteric vein appears to be on the right side of the superior mesenteric artery, a normal relationship. Terminal, ICJ, and caecum appear to be on the right side.
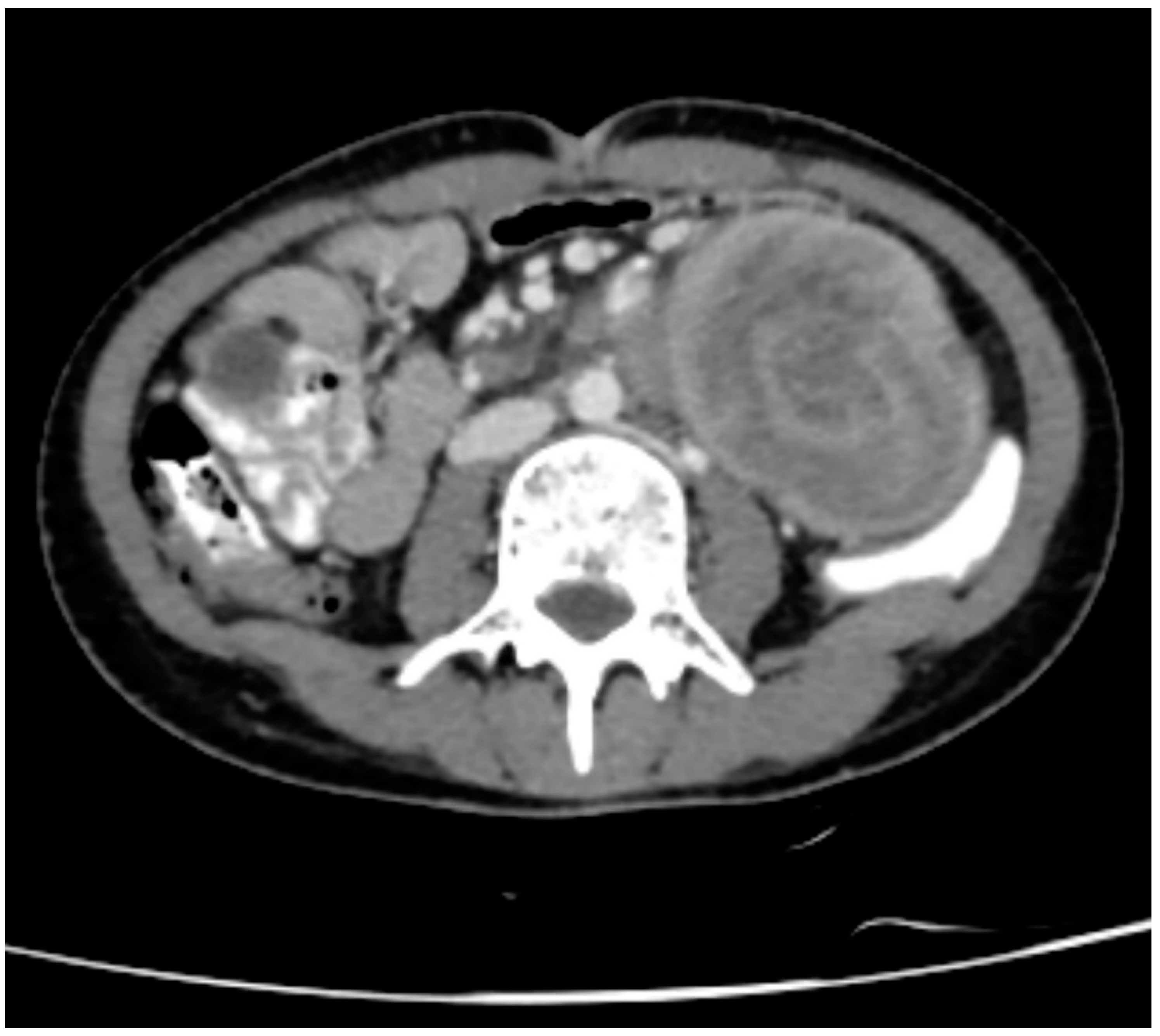
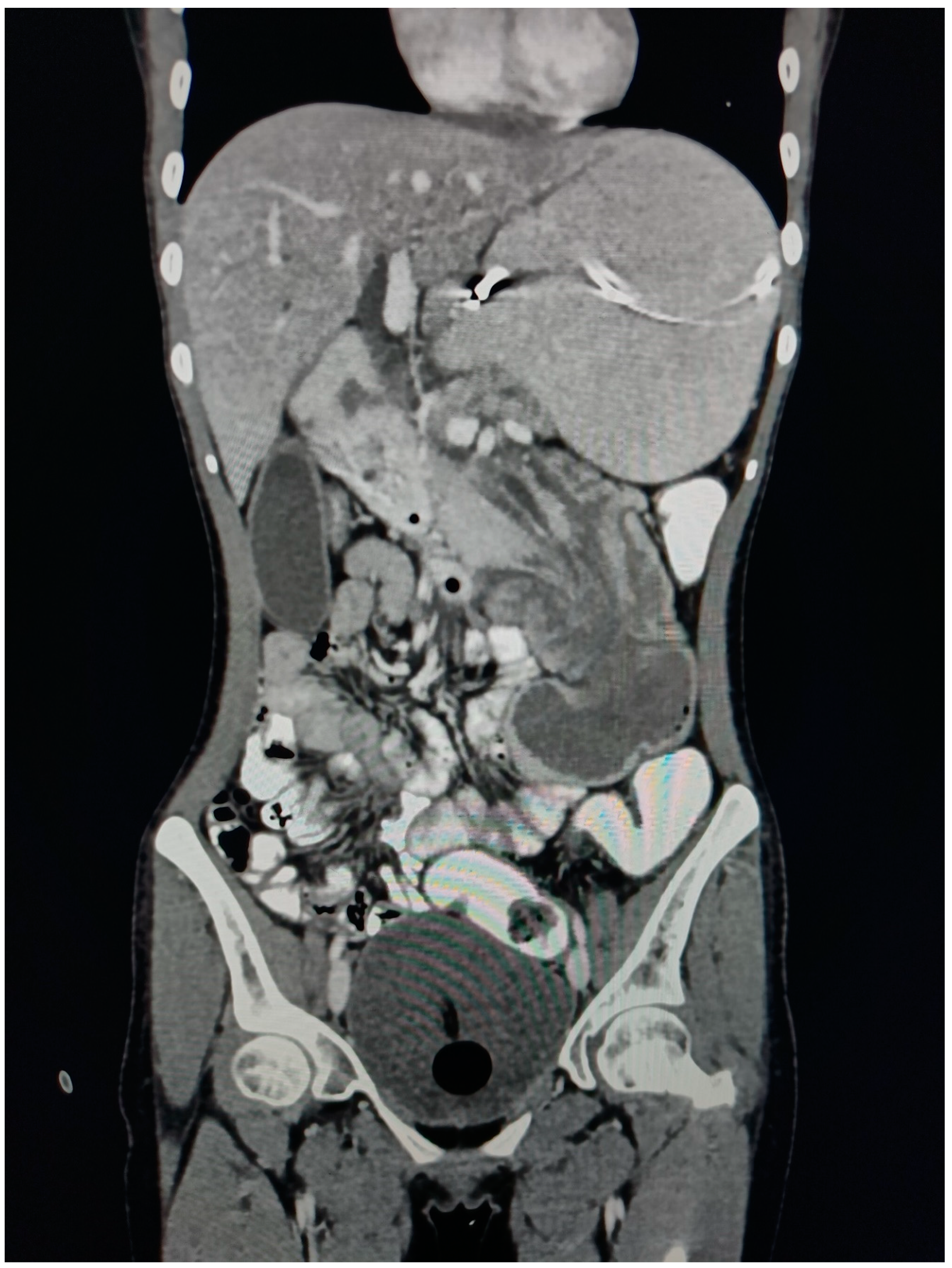
On CECT examination, there is evidence of long segmental intussusception noted at the level of the distal 2nd part of the duodenum with resultant proximal dilated proximal duodenum and stomach. These findings are compatible with the duodenal-duodenal type of enteroenteric intussusception.
The Intussusceptum is 2nd part of the duodenum, the ampulla of the Vater, the head, and the uncinate process of the pancreas while the intussusipens is 3rd and 4th part of the duodenum. The content of the Intussusceptum shows homogenous post-contrast enhancement. The length of the Intussusceptum measures approximately 7 cm.
The Intussuscipens shows enhancing reactionary wall thickening of the 3rd and 4th part of the duodenum and proximal jejunum, maximum wall thickness measures approximately 8 mm of the 4th part of the duodenum. The Intussusceptum does not show any obvious mass lesion or lead point, however underlying ampullary lesion cannot be ruled out owing to the presence of a double duct sign.
Figure 1.
CECT Axial Abdomen showing Bowel within bowel appearance giving TARGET/ DOUNUT sign.
Figure 1.
CECT Axial Abdomen showing Bowel within bowel appearance giving TARGET/ DOUNUT sign.
Figure 2.
CECT Axial Abdomen showing Head of the pancreas, 2nd part of the duodenum, and ampulla of Vater entering into 3rd part of the duodenum.
Figure 2.
CECT Axial Abdomen showing Head of the pancreas, 2nd part of the duodenum, and ampulla of Vater entering into 3rd part of the duodenum.
Figure 3.
CT Coronal section Abdomen Suggestive of Duodeno-Duodenal Intussusception.
Figure 3.
CT Coronal section Abdomen Suggestive of Duodeno-Duodenal Intussusception.
Figure 4.
CT Coronal section Abdomen showing dilated common Bile Duct, Right and left Hepatic Duct and Intra Hepatic Biliary Radicles.
Figure 4.
CT Coronal section Abdomen showing dilated common Bile Duct, Right and left Hepatic Duct and Intra Hepatic Biliary Radicles.
Figure 5.
Ultrasonography of abdomen showing classical Donut/Target Sign of bowel within bowel appearance.
Figure 5.
Ultrasonography of abdomen showing classical Donut/Target Sign of bowel within bowel appearance.
Treatment
After symptomatic support treatment, such as fasting, rehydration, and stomach protection, the patient's abdominal pain was relieved, and exploratory laparotomy was performed. The patient was operated on under GA and OT findings were consistent with the radiological finding of a long segmental duodeno-duodenal type of enteroenteric intussusception. It was found that the 3rd & 4th parts of the duodenum, ampulla of Vater, head, and the uncinate process of the pancreas were inserted into the junction of the horizontal part of the duodenum and the ascending part. At the intussusception, the intestinal wall was cut open. Intestinal anastomosis was performed, and a jejunal nutrition tube was placed to end the operation. After the operation, the patient was given symptomatic support treatment, such as liver protection, stomach protection, and fluid replacement.
Follow Up Care
On the 9th postoperative day (POD), the patient fully recovered and was discharged from the hospital. The patient was followed for 2 years, and no recurrence episode was noted any further.
Discussion:
Intussusception is a type of mechanical obstruction of gastrointestinal bowels, where one portion of the gut invaginates into an immediate adjacent segment mostly its proximal loop enters into the distal loop. It requires careful consideration mainly because of striking variations in its modes of presentation and age-specific distinct clinical features.
An intussusception is composed of two parts, Intussusceptum which is the entering loop, and the Intussuscipiens, receiving loop. The neck of intussusception is the Narrowest part and the apex is the most common site of ischemia. Intussusception anatomically defines accordingly to the site and extent of invagination.
This condition is more common in children with peak incidence at 5-10 months to 6 years of age [
5]. Intussusception is recognized as one of the leading causes of acute abdominal pain and gastrointestinal obstruction. The most common form observed in children is ileocolic intussusception, where a portion of the ileum telescopes into the colon. It is believed that hyperplasia of Peyer’s patches in the terminal ileum triggers this process [
6]. While precise etiology remains exclusive in most cases, viral infections such as rotavirus have been implicated as potential triggers [
5]. Timely diagnosis and prompt intervention are important in pediatric cases to prevent complications like bowel necrosis and perforation.
Intussusception in adults is a rare occurrence, often associated with an underlying structural abnormality or lesion acting as a "lead point.". The variety of lead points include benign or malignant tumors, polyps, Meckel's diverticulum, or postoperative adhesions [
7]. Such structural abnormalities need careful evaluation and proper management strategies.
There are distinct subtypes of intussusception based on the anatomy of the site and extent of invagination, including entero-enteric (involving small bowel), colo-colic (involving colon), ileocecal (involving the junction of the ileum and cecum), and duodeno-duodenal (involving the duodenum) [
8]. In the pediatric group, ileo-colic is more common, while in the adult age group, colo-colic is more common. [
9]
Symptoms of intussusception can include nausea, vomiting, bowel distention, or vague abdominal pain, which leads to a misdiagnosis of other gastrointestinal disorders. In the pediatric age group, a classic triad of colicky abdominal pain, vomiting, and palpable abdominal mass is observed in up to 50% of pediatric cases; however, this triad is less common in adults [
10].
The diagnosis of intussusception is difficult, especially in adults, because of its variable clinical presentation. Investigation methods like Ultrasound (USG) are an investigation of choice in children. Classical Signs of intussusception on USG include the Target Sign or Donut sign [
11]. Computed tomography (CT) is highly sensitive and specific in identifying intussusception and any potential lead points. CECT is an investigation of choice in adults [
12].
The management of intussusception involves a prompt intervention to treat symptoms, prevent complications, and address any underlying etiological factors. Pediatric cases typically respond well to non-operative reduction using contrast enemas or air insufflation, while surgical intervention may be necessary if reduction attempts fail. In contrast enema, the Claw Sign is a classic Sign for Intussusception [
13]. In Adults, intussusception often needs surgical exploration due to the higher chance of an underlying lead point. Surgical intervention includes Resection and Anastomosis. Indications of surgery include Recurrent Intussusception, secondary pathological lead point, perforation, and Strangulation.
Conclusion:
Intussusception is an interesting topic in the field of gastroenterology and shows distinct presentations in pediatric and adult populations. This case of duodenal-duodenal intussusception emphasizes the significance of considering rare subtypes of intussusception, especially when associated with atypical clinical symptoms. Accurate diagnosis through imaging techniques such as USG and CECT is essential for timely intervention. Surgical management is often required in adult intussusception, due to the complexity of the condition and the importance of a skilled surgical team. Further research and case studies are required to learn more about the variability of this condition, especially in the adult population where it remains a diagnostic and therapeutic challenge.
Author Contributions
Dr. Tushar Terariya was responsible for taking imaging scans of the patients in the radiology department. Dr. Vismit Gami was responsible for collecting, compiling, and writing the whole manuscript. Dr. Sahil Shah was our professor and helped in the correct identification and interpretation of radiological scans and making the USG and CT reports. Dr. Dev Desai was responsible for Collecting all the relevant references and citations of them.
Funding and Sponsorship
None of the authors have a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Patient Consent
The patient in the study was provided with detailed information about the purpose, procedures, risks, benefits, and confidentiality measures associated with the research. The patient was given ample time to review the informed consent, ask questions, and make an informed decision regarding their participation. Written informed consent was obtained from the patient before their involvement in the study.
Conflicts of Interest
The authors of this report declare that they have no conflicts of interest to disclose.
References:
- Marinis et al., “Intussusception of the bowel in adults: A review,” World J Gastroenterol, vol. 15, no. 4, p. 407, 2009. [CrossRef]
- P. Marsicovetere, S. Ivatury, B. White, and S. Holubar, “Intestinal Intussusception: Etiology, Diagnosis, and Treatment,” Clin Colon Rectal Surg, vol. 30, no. 01, pp. 030–039, Dec. 2016. [CrossRef]
- A. Brill and R. A. Lopez, Intussusception in Adults. 2023.
- P. Marsicovetere, S. Ivatury, B. White, and S. Holubar, “Intestinal Intussusception: Etiology, Diagnosis, and Treatment,” Clin Colon Rectal Surg, vol. 30, no. 01, pp. 030–039, Dec. 2016. [CrossRef]
- A. Esteghamati et al., “Incidence of intussusception in children less than five years of age: a pre-rotavirus vaccine survey from Iran, 2010-2015.,” Med J Islam Repub Iran, vol. 34, p. 40, 2020. [CrossRef]
- J. Siaplaouras, J. D. Moritz, L. Gortner, and G. Alzen, “Dünndarminvaginationen im Kindesalter: Diagnostik und Bedeutung,” Klin Padiatr, vol. 215, no. 2, pp. 53–56, Mar. 2003. [CrossRef]
- P. Marsicovetere, S. Ivatury, B. White, and S. Holubar, “Intestinal Intussusception: Etiology, Diagnosis, and Treatment,” Clin Colon Rectal Surg, vol. 30, no. 01, pp. 030–039, Dec. 2016. [CrossRef]
- P. Marsicovetere, S. Ivatury, B. White, and S. Holubar, “Intestinal Intussusception: Etiology, Diagnosis, and Treatment,” Clin Colon Rectal Surg, vol. 30, no. 01, pp. 030–039, Dec. 2016. [CrossRef]
- A. Marinis et al., “Intussusception of the bowel in adults: A review,” World J Gastroenterol, vol. 15, no. 4, p. 407, 2009. [CrossRef]
- P. Rukwong, N. Wangviwat, T. Phewplung, and P. Sintusek, “Cohort analysis of pediatric intussusception score to diagnose intussusception,” World J Clin Cases, vol. 11, no. 21, pp. 5014–5022, Jul. 2023. [CrossRef]
- J. Gardner-Thorpe, “Adult duodenal intussusception associated with congenital malrotation,” World J Gastroenterol, vol. 13, no. 28, p. 3892, 2007. [CrossRef]
- A. Daneman and O. Navarro, “Intussusception,” Pediatr Radiol, vol. 33, no. 2, pp. 79–85, Feb. 2003. [CrossRef]
- V. Raveenthiran, “Solar eclipse sign of intussusception on barium enema,” Pediatr Surg Int, vol. 18, no. 1, pp. 79–80, Jan. 2002. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).