Introduction
Migraine is one of the most common health conditions in the reproductive male and female population. Nearly 20% of the females and around 10% of males were affected with migraine disorder in reproductive age. (1) It is estimated that out of all migraines experienced women three times (70%) more migraine attacks than men. Migraine headaches are characterized by severe throbbing pain or a pulsing sensation, usually on one side of the head. They can be accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last for hours to days and can interfere with daily activities. (2) Migraine is a kind of headache that can occur commonly around 14% of the general population globally. (3) (4)
Premenstrual syndrome (PMS) is a common condition that affects many women during their menstrual cycle. Roughly 50 to 60% have menstrual headaches among the migraineur women. (5) PMS symptoms are experienced by many women before their period and can include physical symptoms such as bloating, cramps, and fatigue, as well as emotional symptoms such as irritability, mood swings, and anxiety. (6)
The symptoms in the majority were mild, but 5–8% may suffer moderate to severe symptoms, these are accompanied by considerable distress or functional dysfunction. (7) These symptoms can be distressing and can interfere with daily activities and quality of life. (8)
In women, Migraine has been classified into menstrual-related migraine (MRM), menstrual migraine (MM), and non-menstrual migraine (NMM). (9) The Menstrual migraine typically occurs in two days before or during menstruation up to 3 days. The symptoms of a menstrual migraine can include severe headache pain, nausea, vomiting, and light sensitivity. (10) (11)
Premenstrual syndrome (PMS) symptoms can have a significant impact on the occurrence of menstrual migraines. Premenstrual migraine (PMM) refers to migraines that occur with the menstrual cycle. It affects approximately 50% of women with migraine and can be debilitating in terms of both frequency and severity of symptoms. (12) (13) In Premenstrual migraine women 70% are predisposed to pain two days before menstruation, compared to other days of the menstrual cycle, and nearly half of them were experiencing migraine headaches on the first day of the menstrual cycle. (14) Of these migraineurs women, most of them >60% confirmed that the migraine attacks and their menstrual cycles have a connection. (15) True menstrual migraine arises solely on the first day or second day of menstruation in 2 out of 3 menstrual cycles and the symptoms should not be any other time of the menstrual cycle. Whereas menstrual-related migraine occurs at any time of the menstruation (on day one or two and at other times of the cycle). (16)
The researchers observed that the frequency, intensity, and duration of migraines increased during the premenstrual phase in women who had PMS. They also noted that PMS symptoms, such as bloating, mood swings, and fatigue, were likely to trigger migraines. These symptoms can contribute to the onset of menstrual migraines, menstrual migraines have symptoms of a dull throbbing or severe pulsing headache, fatigue, dizziness, nausea, and sensitivity to light. (10) The exact etiology of PM is not well understood, but it is thought to involve complex interactions between hormonal, genetic, and environmental factors. Hormonal factors are thought to play a major role in the development of PM. Migraine attacks in women tend to occur during the late luteal phase of the menstrual cycle, which is the phase preceding menstruation. Fluctuations in estrogen and progesterone levels during the menstrual cycle can trigger migraines by affecting the balance of neurotransmitters such as serotonin, which is believed to play a role in pain regulation. (17) Some women may also be more susceptible to these conditions due to factors such as genetics, stress, and diet. (18) Estrogen withdrawal has also been shown to trigger migraines in animal models, suggesting that decreases in estrogen levels before menstruation may be a trigger for PM. (19)
Genetic factors have also been found to be associated with PM. A family history of migraine is a strong predictor of PM. Premenstrual Migraine Syndrome, it is hypothesized that the female preponderance of migraine results from the influence of female sex hormones on neurotransmitter systems and neuropeptide release involved in migraine pathophysiology, neuronal excitability, and underlying genetic and environmental factors. (20)
Research has shown that hormonal fluctuations that occur during the menstrual cycle can trigger migraines in some women and that PMS symptoms can exacerbate this effect. (17) One study found that women who experienced PMS symptoms were more likely to also experience menstrual migraines than those who did not experience PMS symptoms. (20) It is important for women who experience menstrual migraines to track their symptoms and work with their healthcare provider to develop a personalized treatment plan that addresses both the migraine headaches and any PMS symptoms that may be exacerbating them. (21)
Premenstrual dysphoric disorder (PMDD) is a severe form of premenstrual syndrome (PMS) that affects some women. It is characterized by a range of physical and emotional symptoms that occur in the week or two before menstruation and typically resolve once the period starts. Symptoms of PMDD can include difficulty concentrating, depression, anxiety, sadness, feelings of hopelessness, anger or irritability, lethargy, loss of interest in normal activities, food cravings, insomnia, or hypersomnia. The exact causes of PMDD are unknown, but it is usually associated with hormonal changes in the menstrual cycle. (22)
Burden of PMM
According to a study published in the Journal of Headache and Pain, there is a strong link between premenstrual syndrome (PMS) and menstrual migraines (MM). The study analyzed the data of 160 women who had been diagnosed with MM and found that 77% of them also reported symptoms of PMS. (20) The World Health Organization, it is estimates that up to 80% of women experience premenstrual symptoms at some point in their reproductive lives, with 20-30% experiencing symptoms severe enough to impact daily activities. Regarding menstrual migraines, it is estimated that around 60% of women who suffer from migraines experience attacks associated with their menstrual cycle.
Regarding the prevalence of premenstrual syndrome and menstrual migraines in Saudi Arabia, there is limited data available. it is estimated that around 50% of women in Saudi Arabia who suffer from migraines experience menstrual migraines. According to a study, there is a significant connection between premenstrual syndrome (PMS) and menstrual migraines in Saudi Arabia. (23) However, studies have shown that premenstrual syndrome affects around 35.6% of women in Saudi Arabia, with symptoms such as bloating and mood swings being the most common. (24) Additionally, The study found that women who experience PMS are more likely to suffer from menstrual migraines compared to those who do not experience PMS symptoms.
The study highlights the need for healthcare providers to assess PMS symptoms in women with MM, as managing these symptoms may also help alleviate their migraines. Additionally, lifestyle modifications such as regular exercise, stress management, and dietary changes may also be effective in reducing the frequency and severity of PMS and MM. This information is important for medical professionals in Saudi Arabia to be aware of so, as to provide better medical care and support. Which can significantly improve the affected women’s quality of social and physical life from PMS and menstrual migraines.
Objectives
To estimate the prevalence of menstrual migraines in reproductive women.
To evaluate the severity and frequency of menstrual migraines in women with PMS.
To identify potential aggravating for developing menstrual migraines in women with PMS.
Methodology
Study design: A cross-sectional study was conducted using a self-administered questionnaire between December 2022 to May 2023 in Saudi Arabia.
Study Population
The study population is women aged 18-50 years who have regular menstrual cycles experience migraine headaches and are diagnosed with PMS and menstrual migraine. Participants were recruited from the general population in different regions of Saudi Arabia.
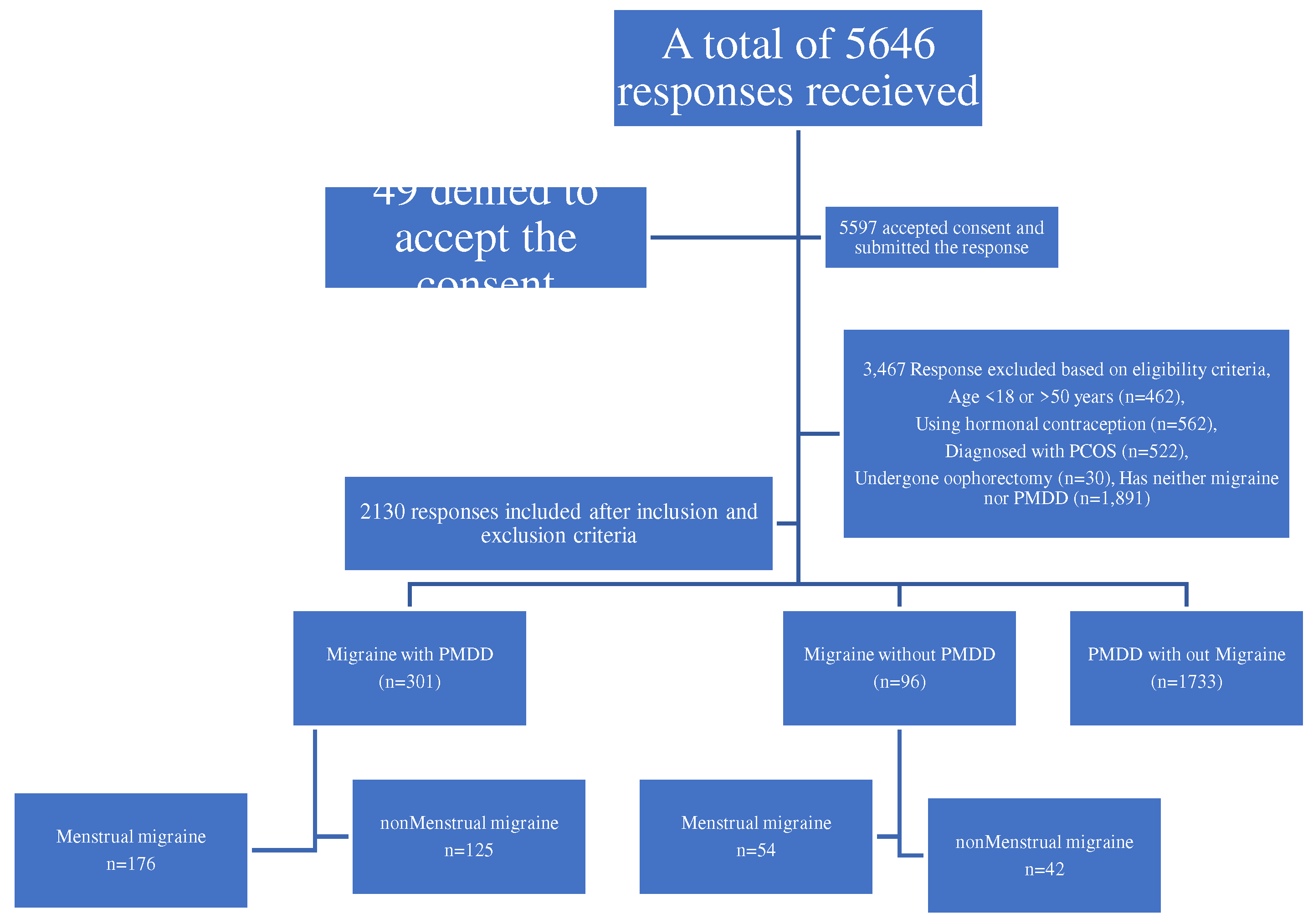
The Menstrual migraine diagnoses were based on self-reported history but not confirmed by their headache and menstruation diaries prospectively. The study sample was recruited through a purposive nonprobability sampling technique. The sample who has been with self-reported migraines and with or without PMDD and willing to spare time to complete the questionnaire accepted the digital consent were included, though the sample may not be truly representative of the migraineur women population alone, it will be provided useful inputs about the PMM with PMS. The study excluded those women who are more than 50 years old, severely ill, currently on hormonal contraceptive therapy, Illiterates, diagnosed with polycystic ovarian syndrome, women who underwent hysterectomy or oophorectomy, and severe depression and hospitalized were excluded from the study.
Methods
The validated questionnaire was obtained from the previous studies, this research tool was translated and back-translated into the local Arabic language with the help of Arabic scholars. The survey questionnaire includes questions on demography, anthropometric profile, lifestyle habits, aggravating factors, symptoms and the severity of PMS and menstrual migraines, MIDAS score, Headache Impact Test-6 (HIT-6), and the prophylactic treatment details. Data was acquired through the survey, and the link to the online Google form tool was shared through WhatsApp with the selected individuals and groups, requesting them to complete the questionnaire after reading the study description and accepting the digital consent.
Diagnostic criteria according to International Classification of Headache Disorders, 3rd edition: (9)
Pure menstrual migraine:
Migraine attacks in a reproductive-age woman fulfilling the criteria without aura.
-
Migraine headache attacks during menstruation days or two days before menstruation and last till the third day of menstruation.
- o
Attacks present at least 2 out of 3 menstrual cycles.
- o
Do not present at other times of the cycle.
Menstrual-related migraine:
Migraine attacks in a reproductive-age woman fulfilling the criteria without aura.
-
Attacks occur on menstruation days, or two days before, and last till the third day of menstruation.
- o
Occur in at least 2 out of 3 menstrual cycles.
- o
Can also occur at any time of the cycle.
Ethical Issues
The authors explained the objectives and brief description of the study in the local Arabic language before proceeding to fill out the questionnaire. As per the Declaration of Helsinki, digital consent was obtained from the participants before the study proceeded. Institutional Ethical approval (ECM#2022-2505 approval duration from 15-09-2022 To 14-09-2023) was acquired from the Research Ethics Committee (HAPO-06-B-001) of King Khalid University, Abha, KSA.
Statistical Analysis
The validated data were analyzed using Statistical Package for the Social Sciences (IBM SPSS Statistics) for Windows, version 21 (IBM Corp., Armonk, N.Y., USA). All the collected data was downloaded in a Microsoft Office 2019 Excel spreadsheet from Google Forms. Categorical variables, like demographic data, educational data, PMM, PMS, clinical features, and aggravating factors, were expressed in proportions to test the hypothesis Chi-square test, and other appropriate tests were applied. The p-value of < 0.05 was considered significant at the 95% confidence interval level.
Results
This study focused on finding the prevalence of menstrual migraines in women with PMS. Out of 2130, most participants 1733(81.4%) suffered from PMDD without migraines, nearly 301 (14.1%) were suffering from migraine with Premenstrual symptoms, and very minimal participants 96 (4.5%) had migraine without PMDD. The average age for the participants is 24 years interquartile range of 21-35, PMS with or without Migraine is experienced in the early ages. Out of 301 migraines with PMS more than half of the participants were either overweight or obese. Of the 301 migraines with PMS, more than half of them 164(54.5) were single and most of them were educated 221(73.4%) graduated and above, and nonsmokers 271(90%). Of the 96 migraines without PMDD, nearly three-fourths of them 68(70.8%) had a family history of headaches, of the 301 migraines with PMDD majority 189(62.8%) had a family history of headaches. Around 10% of them had the habit of smoking with PMDD-associated migraine (
Table 1).
Among the Migraine with PMDD, more than half of them 58.5% were having Menstrual migraines and among the Migraine without PMDD also nearly equal proportion were having menstrual migraines. Of the 230 menstrual migraine individuals, 159 (40.0%) experienced migraines two days before menstruation, and nearly one-fifth (17.89%) of them experienced headaches in the first three days of menstruation. Most of the victims of PMDD felt Unilateral localization 318(80.1%) pulsatile pain 301(75.8%) and Nausea 269 (67.8%). Of these participants the Migraines with or without PMDD the aggravating factors were sleep disturbance 325(81.9%), menstruation 260 (65.5%), and prolonged fasting 216 (54.4%), etc. (
Table 2)
Out of 2130 women participants, 397 were suffering from migraine which is 18.6%. Of the total 397(18.6%) Migraineurs individuals 230 (57.9%) were suffering from menstrual migraine and 167 (42.1%) were non-menstrual migraineurs. The prevalence of Menstrual Migraine is 10.8% and non-menstrual Migraine is 7.8%. the menstrual migraine among the migraineurs is 57.9%. The menstrual migraine sufferers were middle-aged women average of 33 years with an interquartile range of 24-40 years. Whereas non-menstrual migraine individuals were in the younger age group 24 years with an interquartile range of 21-34 years. The BMI is increasing the incidence of menstrual migraines is increasing. For those who are living single non-menstrual migraine 101(60.5%) is more common than for those who are menstrual migraine 98 (42.6%). The education advances the more participants suffering from migraine. Among the Migraineurs, symptoms were aggravated by movement among 277 (69.8%), Photophobia is the most common symptom 342 (86.1) followed by unilateral localized pain 318 (80.1). among the aggravating factors sleep disturbance is the commonest 325 (81.9), followed by menstruation 260 (65.5) and prolonged fasting 216 (54.4). Migraine Disability Around one-third of the participants were suffering from III–moderate disability 134 (33.8).
Table 3
Among the 397 migraineurs 301 (76) were having Migraines with PMDD and one-quarter of them were 97(24) without PMDD. Around three-fourths of migraineurs 288 (72.5%) had a very severe form of headache during the episode of migraine. Nearly half of them 199 (50.1) have severe headaches very often and one quarter 89 (22.4) will always be in severe form of headache episodes. The majority 228 (57.5%) replied that they very often/always limit their ability to do usual daily activities. Most of the participants 347 (87.8%) were when they felt a headache they preferred to lie down for a while. In the fast four-week period around 169(45%) frequently tiered due to headaches. Most of the participants 193 (48.7%) commonly had irritated moods due to the headache.
Table 4.
Out of the 397 migraineurs 167 (42%) were menstrual migraine victims and 230 (58%) were having non-menstrual migraines. Most of the menstrual migraine victims at least 3 days in the last three months were absent from their duties due to their menstrual migraines. The menstrual migraine sufferers were more frequently absent from their social activities and family functions.
Table 5.
Discussion
In this study, Females with Menstrual Migraines reported more PMS symptoms than those with non-menstrual Migraine. HIT-6 score and Migraine severity were not significant, the duration of migraine attacks was almost equal in both the groups of women with menstrual Migraine and non-menstrual Migraine, while MIDAS scores were higher among the self-reported Menstrual Migraine compared to the non-menstrual Migraineurs. The overall prevalence of Migraine was 18.6% and the menstrual migraine was 10.8%.
This study observed that a total of 2130, most participants 1733(81.4%) suffered from PMDD without migraines, nearly 301 (14.1%) were suffering from migraine with Premenstrual symptoms, and very minimal participants 96 (4.5%) had migraines without PMDD. The average age of the participants was 28 years with an interquartile range of 22-40, among the Premenstrual migraineurs were 33 years with a 24-40 years interquartile range, whereas non-MM Migraine is experienced in the early ages 24 years (21–35 years). A similar study conducted by Chalmer MA et al also observed similar findings that the women with MM mean age was 38.7 (8.7) years and women with non-MM were 37.0 (9.2) years. (25) Another study by Vetvik KG et al. observed that more than 20% of female migraineurs aged 30–34 years have migraines greater than 50% of migraineurs suffer migraine attacks during menstruation. (26) Another study conducted by Tschudin et al. observed that around age 35 years the peak premenstrual symptoms were observed. (27)
Among the 2130 participants, Migraine with PMDD 14.1% were higher than that of Migraine without PMDD 4.5%. A similar study conducted by Yamada K et al. reported results aligned with this study, 68.7% PMDD with migraine, and 57.8% had migraine without aura. (28) Of the 397 migraineurs, menstrual migraine (57.9%) sufferers were higher than that of non-menstrual migraine (42.1%). A study conducted on the Taiwanese population reported a significantly 57.7% higher prevalence of self-reported MM among migraineurs with PMS compared to 38.9% of migraineurs without PMS. (29)
This study observed the prevalence among study participants, migraine 18.6%. a similar study conducted by Witteveen H et al. also noted in concordance with this study, that the intervention and control arm both had a family history of menstrual migraines around 75%. (30). and another study by Muayqil T et al. reported migraine prevalence is 26.97%, with three times more common in women. (31) Other studies conducted by Bamalan BA et al. (32), Balaha M et al (24), and Hanadi Bakhsh et al. (23) on the Saudi population reported that 70% of the women with menstrual cycle-related migraine headaches, the prevalence of PMS was 35.6% and 47.08% of females had PMS respectively. The current study stated that Menstrual Migraine 10.79% and non-Menstrual Migraine 7.8%. among the migraineurs, the menstrual migraine was 57.9%. a similar study conducted by Kjersti G Vetvik et al reported that menstrual migraines in women 7.6% prevalence and 22.0% in female migraineurs. (20) Vetvik KG, study reported 34.8% prevalence among self-reported migraine, and of the 34,8% migraineurs, 21% reported menstruation-related migraine in at least 2/3 menstrual cycles. Pure menstrual migraine was 7.7% and 13.2% Menstrual Related Migraine. (33) In another study by MacGregor EA et al. reported 7.2% of the women had "menstrual" migraine. (34) In another study conducted by Vetvik KG reported among the migraineur women 20–25% them affected with Menstrual migraine in the general population, and 22–70% of the women reported menstrual migraine among the persons who attended headache clinics. (35)
Among the 301 menstrual migraine sufferers majority of them, 68.4% were graduates, and the non-MM group also the majority were graduates followed by high school-educated women. A study conducted by Pavlovic JM et al. also observed menstrual migraine victims were bachelor’s degrees (32.1%) followed by women educated up to high school (26.9%). (36) Of the migraine with PMDD group, 45% of the participants were either overweight (29.6%) or obese (15%), and in migraines without PMDD nearly 50% were either overweight or Obese. Out of 230 menstrual migraineurs, more than half of the participants 122(53%) were either overweight 35.2% or obese (17.8%). Whereas among 167 Non-menstrual migraines, only 36.2% were either overweight (19.9%) or obese (16.3%). It shows that BMI increases the Menstrual migraine attack, and the prevalence is also increasing. In a study conducted by Peterlin BL et al. and Pavlović JM et al. also observed similar findings. In Peterlin BL et al study among reproductive-age women with abdominal obesity, the risk of severe migraine is increased by approximately 39%, (OR 1.39; CI: 1.25–1.56). (37) In Pavlovic JM study the menstrual migraine is associated with high BMI, in Obese the MM prevalence was 39.8%, and in overweight 30.1%. (36) A Family history of Headaches is positively associated with both menstrual migraines 62.8% and non-menstrual migraines 70.8%, whereas PMDD without migraine is only 49%. A study conducted by Russell MB et al. observed that menstrual migraine is more common with the family history the menstrual migraine victims frequently had 2 or more relatives with migraine than other types of migraine. (38)
In most of the studies, menstrual migraineurs reported the headache attacks started two days before menstruation 40% and around one-fifth (17.8%) reported continued headaches during the first three days of menstruation also. Earlier studies have noted an increased risk of migraine and menstrual migraine among women with PMS. (39) Women with MM in this study stated nearly 8(5-12) attacks this year with the menstrual cycle. around 73% of them reported moderate to severe pain, nausea 68%, photophobia 86.1%. a higher impact of migraine in terms of higher HIT-scores 66(63-69), more migraine days, and longer duration of attacks, PMS symptoms were similarly common in women with and without MM. nearly more than half of the menstrual migraineurs were very often they were unable to deliver their protein activities like personal home activities, and academic and occupational activities, and their productivity reduced to half in the last 3 months in nearly 4 (2-6) days. A study conducted by Balah M et al on the Saudi population also stated similar findings that migraine during menstruation leads to poor concentration, cyclical absence to the college, and not performing the homework task. (24) This might indicate some other different pathophysiologic mechanisms underlying MM and PMS.
This study observed that menstrual migraine attacks were aggravated by sleep disturbances at 86.4%, followed by menstruation at 70%, movements at 67.7%, fasting at 60.1%, food at 11.6%, and other due to sensation at 0.6%. a study conducted by Bamalan BA et al. (32) on the Saudi population reported in alignment with these study findings, the most frequently observed trigger factor was 94% deprivation of sleep, 81.6% stress and anxiety, menstruation 70%, hunger 62.3%. Another similar study conducted by Moy G et.al observed that some of the menstrual migraineurs experienced cutaneous allodynia. (40) This study observed that 12(5.2%) women reported that they are using antipsychotic (SSRI) drugs as migraine prophylaxis. This study has not determined the possible comorbid psychiatric illness and use of antipsychotic drugs other than migraine. Another study by Witteveen H et al. noted that the MM attacks were aggravated by physical activity at 63.6% among menstrual migraineurs. (30)
Limitations
The main limitation of this study is that the result mainly depends on the self-reporting criteria to diagnose the health condition under the study. The method of classifying women based on the MM Diary data over several months would be ideal. Since most of the victims were literate, they did not note the data was not available, so the authors relied on self-reported data, this study believed that the self-reported data likely mirrored image of the image of information gathered in clinical settings. This study followed the ICD-10 criteria for the diagnosis of menstrual migraine “migraine attacks happening more frequently two days before or during menses”, without considering the rate of occurrences with menstruation.
Conclusions and Recommendations
This community-based study of Saudi reproductive-aged women is representative of the Saudi Arabian population. This study's results are purely based on the self-report migraine attacks among reproductive-age women and their association with the menstrual cycle. These migraine attacks during the menstrual cycle cause the impairment of their social and physical ability to perform their routine household activities, and academic activities and unable to fulfill their professional commitments. To better understand the MM and nMM large prospective studies are required to plan for the best management methods of the MM and nMM cases and as a result, reduce the burden of migraine-related physical and psychological health problems.
Authors' Contributions
"ZAQ conceptualized the study design, designed the questionnaire, conducted data analysis, contributed to writing the manuscript, and approved the final draft BRN &LKVR data analysis, preparing the initial manuscript, revised the manuscript, and approved the manuscript. HYMA, AHHA, and HAAA conceptualized the study, data collection, and initial drafting of the manuscript and approved the final draft of the manuscript. RAS, NAH, AAHA, and NKAH were study designed, prepared the questionnaire, translated back translation of the questionnaire, data analysis, revised the manuscript language and approved the final draft. HAMA, YYAQ, YAMA & AAS: manuscript revised, contributed actively to data collection, data entry, and data analysis, reviewed the paper with a final copy, and made the final corrections before submitting it. "All authors read and approved the final manuscript."
Availability of Data and Material
The datasets used and/or analyzed during the current study are available with the corresponding author upon reasonable request and will be provided by masking the identification of the individuals.
Conflict of Interests
The authors declare that there is no conflict of interest.
Acknowledgment
The authors extend their appreciation to the Deanship of Scientific Research at King Khalid University for funding this work through a large group Research Project under grant number RGP2/474/44.
References
- Stewert, W.F.; Roy, J.; Lipton, R.B. Migraine prevalence, socioeconomic status, and social causation. Neurology 2013, 81, 948–955. [Google Scholar]
- Pescador Ruschel, M.A.; De Jesus, O. Migraine Headache. [Updated 2023 Feb 13]. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560787/.
- Collaborators, G.H. Global, the regional, and national burden of migraine and tension-type headache, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 954–976. [Google Scholar]
- Rasmussen, B.K. Epidemiology of headache. Cephalalgia 2001, 21, 774–777. [Google Scholar] [CrossRef]
- MacGregor, E.A. Progress in the pharmacotherapy of menstrual migraine. Clin. Med. Insights Therapeutics 2011, 3, 245–273. [Google Scholar] [CrossRef]
- Clinic, M. Diagnosis & Treatment. Premenstrual syndrome (PMS). Last updated Feb. 25, 2022. Accessed on 05/06/2023 available from https://www.mayoclinic.org/diseases-conditions/premenstrual-syndrome/symptoms-causes/syc-20376780.
- Abu Alwafa, R.; Badrasawi, M.; Haj Hamad, R. Prevalence of premenstrual syndrome and its association with psychosocial and lifestyle variables: A cross-sectional study from Palestine. BMC Women's Health 2021, 21, 233. [Google Scholar] [CrossRef] [PubMed]
- JoAnn, V. Pinkerton. Premenstrual Syndrome (PMS), (Premenstrual Dysphoric Disorder; Premenstrual Tension). Last updated on Jan. 2023. Accessed on 05/06/2023. Available from https://www.msdmanuals.com/professional/gynecology-and-obstetrics/menstrual-abnormalities/premenstrual-syndrome-pms.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd ed. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef] [PubMed]
- Ornello, R.; De Matteis, E.; Di Felice, C.; Caponnetto, V.; Pistoia, F.; Sacco, S. Acute and Preventive Management of Migraine during Menstruation and Menopause. J. Clin. Med. 2021, 10, 2263. [Google Scholar] [CrossRef] [PubMed]
- Allais, G.; Del Rio, M.S.; Diener, H.-C.; Benedetto, C.; Pfeil, J.; Schäuble, B.; von Oene, J. Perimenstrual migraines and their response to preventive therapy with topiramate. Cephalalgia 2010, 31, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Amiri, P.; Kazeminasab, S.; Nejadghaderi, S.A.; Mohammadinasab, R.; Pourfathi, H.; Araj-Khodaei, M.; et al. Migraine: A Review of Its History, Global Epidemiology, Risk Factors, and Comorbidities. Front. Neurol. 2022, 12, 800605. [Google Scholar] [CrossRef]
- Dilbaz, B.; Aksan, A. Premenstrual syndrome, a common but underrated entity: Review of the clinical literature. J. Turk. Ger. Gynecol. Assoc. 2021, 22, 139–148. [Google Scholar] [CrossRef]
- MacGregor, E.A. Migraine headache in perimenopausal and menopausal women. Curr. Pain. Headache Rep. 2009, 13, 399–403. [Google Scholar] [CrossRef]
- Clevelandclinc. menstrual migraine (or hormone headache). Last updated on 03/03/2021. Accessed on 05/06/2023 available from https://my.clevelandclinic.org/health/diseases/8260-menstrual-migraines-hormone-headaches.
- Macgregor, E.A. Menstrual migraine: Therapeutic approaches. Ther. Adv. Neurol. Disord. 2009, 2, 327–336. [Google Scholar] [CrossRef]
- Calhoun, A.H. Understanding Menstrual Migraine. Headache 2018, 58, 626–630. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A. Menstrual migraine: A distinct disorder needing greater recognition. Lancet Neurol. 2021, 20, 304–315. [Google Scholar] [CrossRef]
- Ramírez, A.L.; Rubio-Beltrán, E.; Villalón, C.M.; MaassenVanDenBrink, A. Gender aspects of CGRP in migraine. Cephalalgia 2017, 39, 435–444. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A.; Lundqvist, C.; et al. Symptoms of premenstrual syndrome in female migraineurs with and without menstrual migraine. J. Headache Pain. 2018, 19, 97. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.J.; Fuh, J.L.; Lu, S.R.; Juang, K.D.; Wang, P.H. Migraine prevalence during the menopausal transition. Headache 2003, 43, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Elliott, H.; Marwaha, R. Premenstrual Dysphoric Disorder. [Updated 2023 Feb 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532307/.
- Hanadi, B.; Amal, M.A.; Maya, A.A.; Shaden, J.A.; Afrah, A.; Rawabi, A. Prevalence of premenstrual syndrome and its impact on life among women in Princess Nourah Bint Abdul Rahman University in Riyadh, Saudi Arabia. IJMDC 2020, 4, 1307–1312. [Google Scholar]
- Balaha, M.; Amr, M.A.; Moghannum, M.; Muhaida, N. The phenomenology of premenstrual syndrome in female medical students: A cross-sectional study. Pan Afr. Med. J. 2010, 5. [Google Scholar] [CrossRef] [PubMed]
- Chalmer, M.A.; Kogelman, L.J.A.; Ullum, H.; et al. Population-Based Characterization of Menstrual Migraine and Proposed Diagnostic Criteria. JAMA Netw. Open. 2023, 6, e2313235. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A.; Lundqvist, C.; Russell, M.B. Prevalence of menstrual migraine: A population-based study. Cephalalgia 2014, 34, 280–288. [Google Scholar] [CrossRef]
- Tschudin, S.; Bertea, P.C.; Zemp, E. Prevalence and predictors of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample. Arch. Womens Ment. Health 2010, 13, 485–494. [Google Scholar] [CrossRef]
- Yamada, K. High prevalence of menstrual migraine comorbidity in patients with premenstrual dysphoric disorder: Retrospective survey. Cephalalgia. 2016, 36, 294–295. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.J.; Fuh, J.L.; Lu, S.R.; Juang, K.D.; Wang, P.H. Migraine prevalence during menopausal transition. Headache 2003, 43, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Witteveen, H.; van den Berg, P.; Vermeulen, G. Treatment of menstrual migraine; multidisciplinary or mono-disciplinary approach. J. Headache Pain. 2017, 18, 45. [Google Scholar] [CrossRef] [PubMed]
- Muayqil, T.; Al-Jafen, B.N.; Al-Saaran, Z.; Al-Shammari, M.; Alkthiry, A.; Muhammad, W.S.; et al. Migraine and headache prevalence and associated comorbidities in a large Saudi sample. Eur. Neurol. 2018, 79, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Bamalan, B.A.; Khojah, A.B.; Alkhateeb, L.M.; Gasm, I.S.; Alahmari, A.A.; Alafari, S.A.; Sindi, M.A.; Yaghmour, K.A. Prevalence of migraine among the general population, and its effect on the quality of life in Jeddah, Saudi Arabia. Saudi Med. J. 2021, 42, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Vetvik, K.G.; MacGregor, E.A.; Lundqvist, C.; Russell, M.B. Self-reported menstrual migraine in the general population. J. Headache Pain. 2010, 11, 87–92. [Google Scholar] [CrossRef]
- MacGregor, E.A.; Chia, H.; Vohrah, R.C.; Wilkinson, M. Migraine and menstruation: A pilot study. Cephalalgia 1990, 10, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Vetvik, K.G.; MacGregor, E.A. Menstrual migraine: A distinct disorder needing greater recognition. Lancet Neurol. 2021, 20, 304–315. [Google Scholar] [CrossRef]
- Pavlović, J.M.; Stewart, W.F.; Bruce, C.A.; Gorman, J.A.; Sun, H.; Buse, D.C.; Lipton, R.B. The burden of migraine related to menses: Results from the AMPP study. J. Headache Pain. 2015, 16, 24. [Google Scholar] [CrossRef]
- Peterlin, B.L.; Rapoport, A.M.; Kurth, T. Migraine and obesity: Epidemiology, mechanisms, and implications. Headache 2010, 50, 631–648. [Google Scholar] [CrossRef] [PubMed]
- Russell, M.B. Genetics of menstrual migraine: The epidemiological evidence. Curr. Pain. Headache Rep. 2010, 14, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, S.D. Menstrual migraine. J. Womens Health Gend. Based Med. 1999, 8, 919–931. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, P. Hormonal factors in migraine: A population-based study of women aged 40 to 74 years. Headache 2003, 43, 27–35. [Google Scholar] [CrossRef]
- Moy, G.; Gupta, V. Menstrual-Related Headache. [Updated 2022 Oct 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557451/.
Table 1.
Demographic Characteristics of the study population with the PMDD.
Table 1.
Demographic Characteristics of the study population with the PMDD.
| |
Total |
Migraine with PMDD |
Migraine without PMDD |
PMDD without migraine |
|
| Characteristics |
n=2,130 |
n=301 (14.1) |
n=96 (4.5) |
n=1733 (81.4) |
P value |
| Prevalence |
- |
14.1% |
4.5% |
81.3% |
|
| Age, median (IQR), yrs. |
24 (21–35) |
27 (22–39) |
35 (23–40) |
24 (21–33) |
<0.001* |
| Weight, median (IQR), Kg |
60 (51–70) |
60 (51.5–70) |
62 (52–74) |
59 (51–69) |
0.1#
|
| Height, median (IQR), m |
1.6 (1.5–1.6) |
1.6 (1.5–1.6) |
1.6 (1.5–1.6) |
1.6 (1.5–1.6) |
0.04* |
| BMI, median (IQR), kg/m2
|
23.3 (20.4–27.2) |
24.2 (20.7–27.5) |
24.9 (21.5–29.5) |
23.1 (20.4–27.1) |
0.004* |
BMI,
No. (%) |
Underweight (<18.5) |
235 (11) |
27 (9) |
8 (8.3) |
200 (11.5) |
0.003* |
Normal weight
(18.5–24.9) |
1086 (51) |
139 (46.2) |
40 (41.7) |
907 (52.3) |
| Overweight (25–29.9) |
472 (22.9) |
89 (29.6) |
25 (26) |
358 (20.7) |
| Obese (≥30) |
319 (14.9) |
46 (15) |
23 (24) |
250 (14.4) |
| Obesity |
Class–I (30–34.9) |
224(10.5) |
23 (51.1) |
17 (73.7) |
184 (73.6) |
|
| Class–II (35–39.9) |
61 (2.9) |
14 (31.1) |
4 (17.4) |
43 (17.2) |
| Class–III (≥40) |
34 (1.5) |
9 (17.8) |
2 (8.7) |
23 (9.2) |
| Saudi Arabia region, No. (%) |
Central |
399 (18.7) |
49 (16.3) |
16 (16.7) |
334 (19.3) |
0.001* |
| Eastern |
431 (20.2) |
81 (26.9) |
32 (33.3) |
318 (18.3) |
| Northern |
114 (5.4) |
20 (6.6) |
3 (3.1) |
91 (5.3) |
| Southern |
704 (33.1) |
84 (27.9) |
29 (30.2) |
591 (34.1) |
| Western |
482 (22.6) |
67 (22.3) |
16 (16.7) |
399 (23) |
| Marital status, No. (%) |
Divorced |
60 (2.8) |
6 (2) |
4 (4.2) |
50 (2.9) |
0.001* |
| Married |
773 (36.3) |
128 (42.5) |
56 (58.3) |
589 (34) |
| Single |
1289 (60.5) |
164 (54.5) |
35 (36.5) |
1090 (62.9) |
| Widowed |
8 (0.4) |
3 (1) |
1 (1) |
4 (0.2) |
| Education level, No. (%) |
Primary |
1 (0) |
— |
— |
1 (0.1) |
0.2#
|
| Intermediate |
17 (0.8) |
2 (0.7) |
2 (2.1) |
13 (0.8) |
| High school |
424 (19.9) |
51 (16.9) |
20 (20.8) |
353 (20.4) |
| Diploma |
114 (5.4) |
27 (9) |
6 (6.2) |
81 (4.7) |
| Graduate |
1472 (69.1) |
206 (68.4) |
64 (66.7) |
1202 (69.4) |
| Postgraduate |
102 (4.8) |
15 (5) |
4 (4.2) |
38 (4.8) |
| Pregnancy |
No |
2051 (96.3) |
290 (96.3) |
95 (99) |
1666 (96.1) |
0.4 |
| Yes |
79 (3.7) |
11 (3.7) |
1 (1) |
67 (3.9) |
| Smoking |
No |
2002 (94) |
271 (90) |
92 (95.8) |
1639 (94.6) |
0.01* |
| Yes |
128 (6) |
30 (10) |
4 (4.2) |
94 (5.4) |
| Family history of headache |
No |
1026 (48.2) |
112 (37.2) |
28 (29.2) |
886 (51.1) |
0.001* |
| Yes |
1104 (51.8) |
189 (62.8) |
68 (70.8) |
847 (48.9) |
Table 2.
Distribution of PMS and Migraine associate factors.
Table 2.
Distribution of PMS and Migraine associate factors.
| |
Total |
Migraine with PMDD |
Migraine without PMDD |
PMDD without migraine |
|
| Characteristics |
n=2,130 |
n=301 (14.1) |
n=96 (4.5) |
n=1733 (81.4) |
P value |
Menstrual migraine
n=397 |
No |
167 (42.1) |
125 (41.5) |
42 (43.8) |
NA |
0.7#
|
| Yes |
230 (57.9) |
176 (58.5) |
54 (56.2) |
NA |
Time of headache during menstruation
n=397 |
Two days before menstruation |
159
(40.0%) |
123
(40.8) |
36
(37.5%) |
NA |
0.6#
|
| The first Three days of menstruation |
71
(17.8%) |
53
(17.6%) |
18
(18.7%) |
NA |
| Mid of menstruation |
167
(42.2%) |
125
(41.6%) |
42
(43.8%) |
NA |
| Headache attacks frequency with menses in the current year, median (IQR) |
5 (2–10) |
5 (2–10) |
5 (0–10) |
NA |
1#
|
| Migraine symptoms |
Aggravated by movement |
269 (67.7) |
206 (68.4) |
63 (65.6) |
NA |
0.01* |
| Moderate–severe pain |
277 (69.7) |
221 (73.4) |
56 (58.3) |
NA |
0.03* |
| Nausea without vomiting |
79 (19.8) |
63 (20.9) |
16 (16.7) |
NA |
0.6#
|
| Photophobia |
44 (11.1) |
35 (11.6) |
9 (9.4) |
NA |
0.6#
|
| Prolonged symptoms (≥72 hrs.) |
397 (100) |
301 (100) |
96 (100) |
NA |
NA |
| Pulsatile pain |
270 (68.0) |
228 (75.7) |
62 (64.6) |
NA |
0.3#
|
| Unilateral localization |
318 (80.1) |
241 (80.1) |
77 (80.2) |
NA |
1#
|
| Vomiting |
79 (19.9) |
32 (10.6) |
47 (48.9) |
NA |
0.5#
|
| Aggravating factors |
Foods |
44 (11.1) |
35 (11.6) |
9 (9.4) |
NA |
0.7#
|
| Menstruation |
260 (65.5) |
210 (69.8) |
50 (52.1) |
NA |
0.002* |
| Prolonged fasting |
216 (54.4) |
181 (60.1) |
35 (36.5) |
NA |
0.001* |
| Sleep disturbances |
325 (81.9) |
260 (86.4) |
65 (67.7) |
NA |
0.001* |
| Smells |
1 (0.3) |
1 (0.3) |
— |
NA |
1#
|
| Sounds |
1 (0.3) |
— |
1 (1) |
NA |
0.2#
|
| Stress |
3 (0.8) |
1 (0.3) |
2 (2.1) |
NA |
0.1#
|
| Visual |
2 (0.5) |
— |
2 (2.1) |
NA |
0.1#
|
| HIT 6 score, median (IQR) |
66 (62–68) |
66 (63–69) |
65 (61–68) |
NA |
0.3#
|
| Migraine severity |
Minimal (<50) |
3 (0.8) |
1 (0.3) |
2 (2.1) |
NA |
0.1#
|
| Mild (50–55) |
14 (3.5) |
8 (2.7) |
6 (6.2) |
NA |
|
| Moderate (56–59) |
38 (9.6) |
28 (9.3) |
10 (10.4) |
NA |
|
| Severe (≥60) |
342 (86.1) |
264 (87.7) |
78 (81.2) |
NA |
|
| MIDAS score, median (IQR) |
14 (9–24) |
16 (9–27) |
11.5 (7–20) |
NA |
0.02* |
| Migraine disability |
I–Little or no disability |
55 (13.9) |
35 (11.6) |
20 (20.8) |
NA |
0.05* |
| II–Mild disability |
84 (21.2) |
60 (19.9) |
24 (25) |
NA |
|
| III–Moderate disability |
134 (33.8) |
105 (34.9) |
29 (30.2) |
NA |
|
| IV–Severe disability |
124 (31.2) |
101 (33.6) |
23 (24) |
NA |
|
| Prophylaxis therapy |
No |
368 (96.8) |
278 (95.9) |
90 (100) |
NA |
0.1#
|
| Yes |
12 (3.2) |
12 (4.1) |
— |
NA |
| Prophylaxis medication |
Amitriptyline |
4 (33.3) |
4 (33.3) |
— |
NA |
|
| Propranolol |
2 (16.7) |
2 (16.7) |
— |
NA |
| Topiramate |
4 (33.3) |
4 (33.3) |
— |
NA |
| Valproic acid |
2 (16.7) |
2 (16.7) |
— |
NA |
| PMDD symptoms |
Anxiety |
1642 (77.1) |
254 (84.6) |
NA |
1363 (78.6) |
0.02* |
| Apathy and loss of interest |
1117 (52.4) |
188 (62.5) |
NA |
918 (53) |
0.003* |
| Appetite changes |
1280 (60.1) |
202 (67.1) |
NA |
1053 (60.8) |
0.04* |
| Confusion |
690 (32.4) |
124 (41.2) |
NA |
563 (32.5) |
0.004* |
| Depressed mood |
1510 (70.9) |
246 (81.7) |
NA |
1246 (71.9) |
0.001* |
| Easily irritable |
1710 (80.3) |
257 (85.4) |
NA |
1414 (81.6) |
0.1#
|
| Fatigue |
1773 (83.2) |
273 (90.7) |
NA |
1467 (84.7) |
0.01* |
| Loss of concentration |
875 (41.1) |
170 (56.5) |
NA |
700 (40.4) |
0.001* |
| Mood disturbances |
1905 (89.4) |
276 (91.7) |
NA |
1577 (91) |
0.7#
|
| Sleep disturbances |
1152 (54.1) |
188 (62.5) |
NA |
948 (54.7) |
0.01* |
| Somatic symptoms |
1632 (76.6) |
252 (83.7) |
NA |
1333 (76.9) |
0.01* |
|
BMI: Body-mass index; HIT-6: Headache Impact Test; MIDAS: Migraine Disability Assessment questionnaire; NA: Not applicable; PMDD: Premenstrual dysphoric disorder. |
Table 3.
Distribution Migraineur study participants with demography.
Table 3.
Distribution Migraineur study participants with demography.
| |
Total |
Menstrual migraine |
Non-menstrual migraine |
|
| Characteristics |
n=397 |
n=230 (57.9) |
n=167 (42.1) |
P value |
| Age, {IQR} (yrs.) |
28 (22–40) |
33 (24–40) |
24 (21–35) |
<0.001* |
| Weight, (IQR), Kg |
60 (52–70) |
62 (54–72) |
58.5 (50–70) |
0.01* |
| Height, (IQR), m |
1.6 (1.5–1.6) |
1.6 (1.5–1.6) |
1.6 (1.5–1.6) |
0.4#
|
| BMI, (IQR), kg/m2
|
24.3 (21.1–27.6) |
25.2 (21.6–28.7) |
23.2 (20.1–27) |
0.01* |
| BMI, No. (%) |
|
|
|
<0.001* |
| Underweight (<18.5) |
35 (8.8) |
12 (5.9) |
23 (13.9) |
|
| Normal weight (18.5–24.9) |
179 (45.2) |
96 (41.7) |
83 (50) |
|
| Overweight (25–29.9) |
114 (28.8) |
81 (35.2) |
33 (19.9) |
|
| Obese (≥30) |
68 (17.2) |
41 (17.8) |
27 (16.3) |
|
| Obesity, No. (%) |
|
|
|
0.047* |
| Class–I (30–34.9) |
40 (58.8) |
24 (58.5) |
16 (59.3) |
|
| Class–II (35–39.9) |
18 (26.5) |
14 (34.1) |
4 (14.8) |
|
| Class–III (≥40) |
10 (14.7) |
3 (7.3) |
7 (25.9) |
|
| Saudi Arabia region, No. (%) |
|
|
|
0.1#
|
| Central |
65 (16.4) |
35 (15.2) |
30 (18) |
|
| Eastern |
113 (28.5) |
76 (33) |
37 (22.2) |
|
| Northern |
23 (5.8) |
16 (7) |
7 (4.2) |
|
| Southern |
113 (28.5) |
56 (24.3) |
57 (34.1) |
|
| Western |
83 (20.9) |
47 (20.4) |
36 (21.6) |
|
| Marital status, No. (%) |
|
|
|
0.002* |
| Single |
199 (50.1) |
98 (42.6) |
101 (60.5) |
|
| Married |
184 (46.3) |
124 (53.9) |
60 (35.9) |
|
| Divorced |
10 (2.5) |
5 (2.2) |
5 (3) |
|
| Widowed |
4 (1) |
3 (1.3) |
1 (0.6) |
|
| Education level, No. (%) |
|
|
|
0.3#
|
| Primary |
— |
— |
— |
|
| Intermediate |
4 (1) |
3 (1.3) |
1 (0.6) |
|
| High school |
71 (17.9) |
38 (16.5) |
33 (19.8) |
|
| Diploma |
33 (8.3) |
19 (8.3) |
14 (8.4) |
|
| Graduate |
270 (68) |
155 (67.4) |
115 (68.9) |
|
| Postgraduate |
19 (4.8) |
15 (6.5) |
4 (2.4) |
|
| Pregnant, No. (%) |
|
|
|
0.6#
|
| No |
385 (97) |
224 (97.4) |
161 (96.4) |
|
| Yes |
12 (3) |
6 (2.6) |
6 (3.6) |
|
| Smoking, No. (%) |
|
|
|
1#
|
| No |
363 (91.4) |
210 (91.3) |
153 (91.6) |
|
| Yes |
34 (8.6) |
20 (8.7) |
14 (8.4) |
|
| Family history of headache, No. (%) |
|
|
|
0.4#
|
| No |
140 (35.3) |
77 (33.5) |
63 (37.7) |
|
| Yes |
257 (64.7) |
153 (66.5) |
104 (62.3) |
|
| Time of headache during menses, No (%) |
|
|
|
<0.001* |
| Three days before menses |
155 (58.7) |
147 (63.9) |
8 (23.5) |
|
| The first two days of menses |
70 (26.5) |
64 (27.8) |
6 (17.6) |
|
| Mid of menses |
19 (7.2) |
18 (7.8) |
1 (2.9) |
|
| After menses |
20 (7.6) |
1 (0.4) |
19 (55.9) |
|
| Headache attacks frequently with menses in the current year, median (IQR) |
5 (2–10) |
8 (5–12) |
5 (0–5) |
<0.001* |
| Migraine symptoms. No (%) |
|
|
|
|
| Aggravated by movement |
277 (69.8) |
158 (68.7) |
119 (71.3) |
0.7#
|
| Moderate–severe pain |
290 (73) |
167 (72.6) |
123 (73.7) |
0.9#
|
| Nausea without vomiting |
269 (67.8) |
160 (69.6) |
109 (65.3) |
0.4#
|
| Photophobia |
342 (86.1) |
200 (87) |
142 (85) |
0.7#
|
| Prolonged symptoms (≥72 hrs) |
397 (100) |
230 (100) |
167 (100) |
NA |
| Pulsatile pain |
301 (75.8) |
184 (80) |
117 (70.1) |
0.02* |
| Unilateral localization |
318 (80.1) |
187 (81.3) |
131 (78.4) |
0.5#
|
| Vomiting |
79 (19.9) |
45 (19.6) |
34 (20.4) |
0.9#
|
| Aggravating factors, No. (%) |
|
|
|
|
| Foods |
44 (11.1) |
26 (11.3) |
18 (10.8) |
1#
|
| Menstruation |
260 (65.5) |
215 (93.5) |
45 (26.9) |
<0.001* |
| Prolonged fasting |
216 (54.4) |
128 (55.7) |
88 (52.7) |
0.6#
|
| Sleep disturbances |
325 (81.9) |
189 (82.2) |
136 (81.4) |
0.9#
|
| Smells |
1 (0.3) |
— |
1 (0.6) |
0.4 |
| Sounds |
1 (0.3) |
— |
1 (0.6) |
0.4#
|
| Stress |
3 (0.8) |
— |
3 (1.8) |
0.1#
|
| Visual |
2 (0.5) |
— |
2 (1.2) |
0.2#
|
| HIT 6 score, median (IQR) |
66 (62–68) |
66 (63–69) |
65 (61–68) |
0.2#
|
| Migraine severity, No (%) |
|
|
|
0.02* |
| Minimal (<50) |
3 (0.8) |
— |
3 (1.8) |
|
| Mild (50–55) |
14 (3.5) |
5 (2.2) |
9 (5.4) |
|
| Moderate (56–59) |
38 (9.6) |
18 (7.8) |
20 (12) |
|
| Severe (≥60) |
342 (86.1) |
207 (90) |
135 (80.8) |
|
| MIDAS score, median (IQR) |
14 (9–24) |
15 (9–27) |
13 (6–23) |
0.3#
|
| Migraine disability, No. (%) |
|
|
|
<0.001* |
| I–Little or no disability |
55 (13.9) |
17 (7.4) |
38 (22.8) |
|
| II–Mild disability |
84 (21.2) |
58 (25.2) |
26 (15.6) |
|
| III–Moderate disability |
134 (33.8) |
78 (33.9) |
56 (33.5) |
|
| IV–Severe disability |
124 (31.2) |
77 (33.5) |
47 (28.1) |
|
| Prophylaxis therapy, No. (%) |
|
|
|
0.8#
|
| No |
368 (96.8) |
214 (96.4) |
154 (97.5) |
|
| Yes |
12 (3.2) |
8 (3.6) |
4 (2.5) |
|
| Prophylaxis medications, No. (%) |
|
|
|
0.05* |
| Amitriptyline |
4 (33.3) |
2 (25) |
2 (50) |
|
| Propranolol |
2 (16.7) |
2 (25) |
— |
|
| Topiramate |
4 (33.3) |
4 (50) |
— |
|
| Valproic acid |
2 (16.7) |
— |
2 (50) |
|
|
BMI: Body-mass index; HIT-6: Headache Impact Test-6 questionnaire; MIDAS: Migraine Disability Assessment questionnaire. |
Table 4.
Headache Impact Test-6 (HIT-6™) questionnaire across the study participants.
Table 4.
Headache Impact Test-6 (HIT-6™) questionnaire across the study participants.
| |
Total |
Migraine with PMDD |
Migraine without PMDD |
|
| Questions, No. (%) |
n=397 |
n=301 (75.8) |
n=96 (24.2) |
P value |
| 1. When you have headaches, how often is the pain severe? |
0.1#
|
| Never |
— |
— |
— |
|
| Rarely |
11 (2.8) |
6 (2) |
5 (5.2) |
|
| Sometimes |
98 (24.7) |
80 (26.6) |
18 (18.8) |
|
| Very often |
199 (50.1) |
146 (48.5) |
53 (55.2) |
|
| Always |
89 (22.4) |
69 (22.9) |
20 (20.8) |
|
| 2. How often do headaches limit your ability to do usual daily activities including household work, work, school, or social activities? |
0.08#
|
| Never |
2 (0.5) |
2 (0.7) |
— |
|
| Rarely |
30 (7.6) |
17 (5.6) |
13 (13.5) |
|
| Sometimes |
137 (34.5) |
111 (36.9) |
26 (27.1) |
|
| Very often |
165 (41.6) |
124 (41.2) |
41 (42.7) |
|
| Always |
63 (15.9) |
47 (15.6) |
16 (16.7) |
|
| 3. When you have a headache, how often do you wish you could lie down? |
0.4#
|
| Never |
2 (0.5) |
2 (0.7) |
— |
|
| Rarely |
4 (1) |
2 (0.7) |
2 (2.1) |
|
| Sometimes |
44 (11.1) |
30 (10) |
14 (14.6) |
|
| Very often |
131 (33) |
102 (33.9) |
29 (30.2) |
|
| Always |
216 (54.4) |
165 (54.8) |
51 (53.1) |
|
| 4. In the past 4 weeks, how often have you felt too tired to do work or daily activities because of your headaches? |
0.3#
|
| Never |
6 (1.5) |
3 (1) |
3 (3.1) |
|
| Rarely |
36 (9.1) |
26 (8.6) |
10 (10.4) |
|
| Sometimes |
186 (46.9) |
137 (45.5) |
49 (51) |
|
| Very often |
131 (33) |
103 (34.2) |
28 (29.2) |
|
| Always |
38 (9.6) |
32 (10.6) |
6 (6.2) |
|
| 5. In the past 4 weeks, how often have you felt fed up or irritated because of your headaches? |
0.3#
|
| Never |
5 (1.3) |
2 (0.7) |
3 (3.1) |
|
| Rarely |
38 (9.6) |
26 (8.6) |
12 (12.5) |
|
| Sometimes |
161 (40.6) |
115 (38.2) |
46 (47.9) |
|
| Very often |
134 (33.8) |
109 (36.2) |
25 (26) |
|
| Always |
59 (14.9) |
49 (16.3) |
10 (10.4) |
|
| 6. In the past 4 weeks, how often did headaches limit your ability to concentrate on work or daily activities? |
0.1#
|
| Never |
8 (2) |
3 (1) |
8 (4.8) |
|
| Rarely |
27 (6.8) |
19 (6.3) |
11 (6.6) |
|
| Sometimes |
163 (41.1) |
122 (40.5) |
79 (47.3) |
|
| Very often |
153 (38.5) |
120 (39.9) |
50 (29.9) |
|
| Always |
46 (11.6) |
37 (12.3) |
19 (11.4) |
|
Table 5.
Headache Impact Test-6 (HIT-6™) questionnaire across study’s populations.
Table 5.
Headache Impact Test-6 (HIT-6™) questionnaire across study’s populations.
| |
Total |
MM |
NMM |
|
| Questions, median (IQR) |
n=397 |
n=167 (42.1) |
n=230 (57.9) |
P value |
| On how many days in the last 3 months did you miss work or school because of your headaches? |
0 (0–3) |
0 (0–3) |
0 (0–2) |
|
How many days in the last 3 months was your productivity at work or school reduced by half or more because of your headaches?
(Do not include days you counted in question 1 where you missed work or school.) |
3 (1–5) |
3 (1–6) |
0 (0–5) |
0.1#
|
| On how many days in the last 3 months did you not do household work (such as housework, home repairs, and maintenance, shopping, caring for children and relatives) because of headaches? |
4 (2–6) |
4 (2–7) |
3 (1–5) |
0.1#
|
How many days in the last 3 months was your productivity in household work reduced by half or more because of headaches?
(Do not include days you counted in question 3 where you did not do household work.) |
4 (2–6) |
4 (2–6) |
3 (1–5) |
0.1#
|
| On how many days in the last 3 months did you miss family, social, or leisure activities because of your headaches? |
3 (1–5) |
3 (1–5) |
2 (0–4) |
0.01* |
|
MM: Menstrual migraine; NMM: Non-menstrual migraine. |
| a—Mood’s test with exact calculation |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).