1. Introduction
Nature has long been recognized as a valuable repository of compounds possessing unique biological activities relevant to human health (1, 2). Among the vast array of secondary metabolites found in plants, sesquiterpene lactones (SL) have garnered significant attention due to their presence in Asteraceae species and their diverse array of active principles found in traditional phytomedicines (3–7). With a structural foundation of 15 carbons and a fused α-methylene-γ-lactone ring, SL consists of over 8000 compounds, each offering a variety of modifications and structures (4, 8, 9). These compounds exhibit a broad spectrum of potential health benefits, encompassing anti-inflammatory (10), antitumoral (3, 6), antioxidant (11), neuroprotective (12), hepatoprotective (13), immune-stimulating (4, 7), antimicrobial (14), and antiparasitic properties (8).
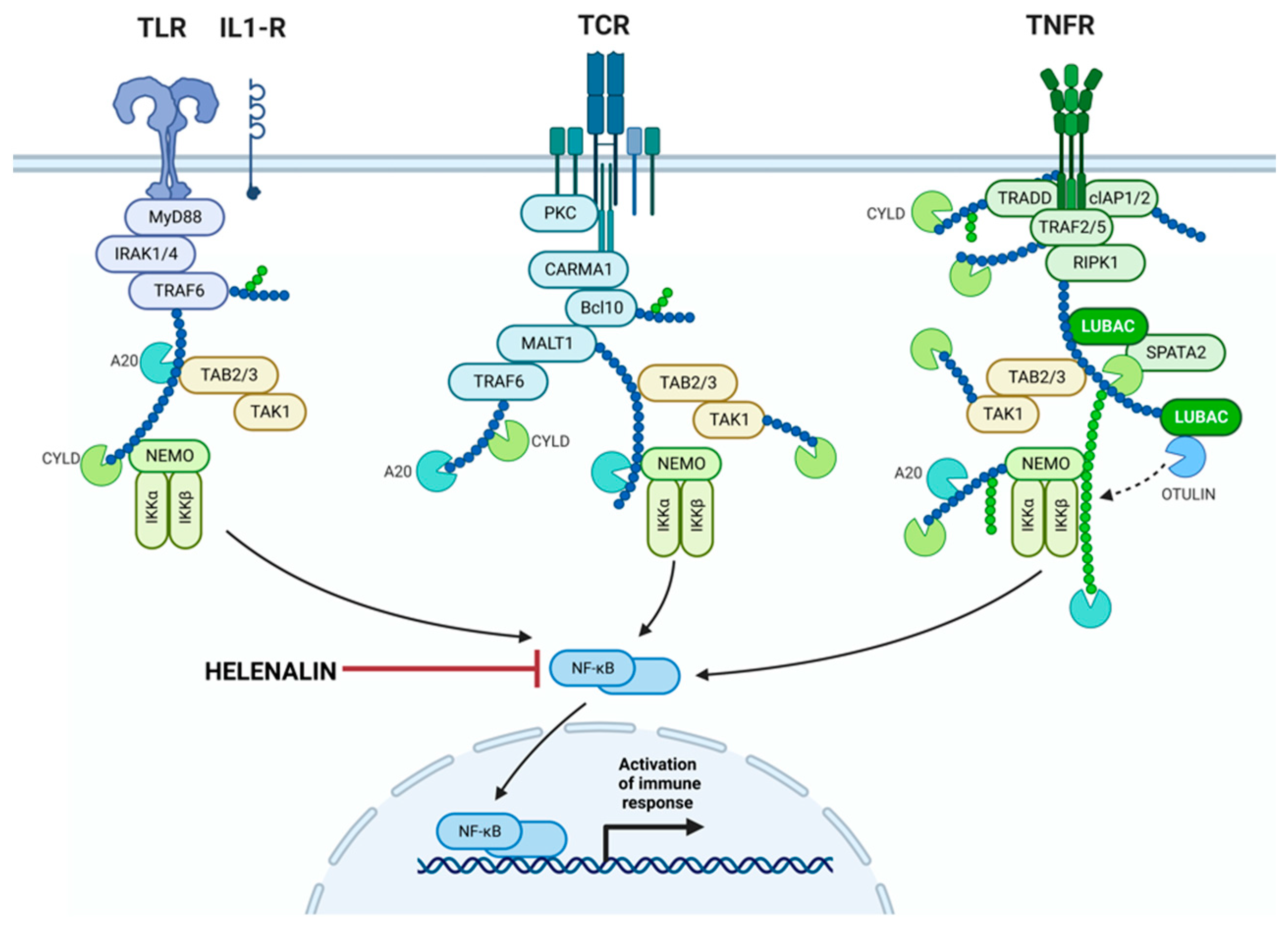
Given their capability to modulate inflammation pathways induced by oxidative stress, SL emerge as promising candidates for addressing chronic inflammatory diseases (4, 11, 15). Notably, helenalin, a pseudoguaianolide sesquiterpene lactone derived from Arnica Montana and Arnica chamissonis ssp. foliosa, has recently regained attention as a lead compound for inflammation treatment (15-19). Its anti-inflammatory mechanism diverges from that of non-steroidal anti-inflammatory drugs (NSAIDs), attributed mainly to its potent inhibition of nuclear transcriptional factor-𝛋ß (NF-𝛋ß) signaling (6, 16). Helenalin-exposed TCD4 cells have shown reduced interleukin-2 (IL-2) production and CD25 expression, suggesting helenalin's potential as an anti-inflammatory therapy (19-21). This is particularly significant in chronic inflammation diseases, where conventional treatments carry risks of adverse events and nonadherence (7, 9, 10, 22-24)
Dry eye disease (DED), characterized by ocular surface inflammation due to hyperosmolarity, is associated with excessive reactive oxygen species (ROS) production, oxidative stress, and inflammation mediated by lymphocytes. This chronic inflammation stems from various ocular factors such as uncorrected refractive errors, prolonged screen usage, systemic conditions, hormonal changes, poor blinking, environmental factors, and aging. The convergence of these factors triggers persistent tear film degradation, leading to microanatomical changes on the ocular surface. In this context, patients experience inflammation affecting both cornea and conjunctiva, marked by T-cell infiltration, increased pro-inflammatory cytokines, and matrix metalloproteinases (MMPs), including MMP-9 (25-27). Pro-inflammatory interleukins (IL-1, IL-6, IL-8) and tumor necrosis factor (TNF) α further contribute to chronic ocular surface damage (25, 27-29). NF-𝛋ß emerges as a key regulator of ocular surface inflammation, responding to diverse stimuli involved in DED (25, 28-30).
Currently, lubricant eye drops represent the standard approach for DED management (28). Although treatments like topical cyclosporine, corticosteroids, and NSAIDs exist, a definitive curative anti-inflammatory therapy for DED remains elusive (28). Despite their efficacy, these treatments are associated with potential adverse effects such as ocular pain, irritation, cataract formation, and ocular hypertension (29, 31, 32). Patient compliance with DED treatment is notably low, with some studies reporting compliance rates as low as 10.2% (27, 28, 33). Up to 60% of patients use treatment on an as-needed basis, highlighting the need for approaches that enhance treatment compliance, alleviate symptoms, and reduce adverse events (33, 34).
To explore a novel anti-inflammatory approach, this clinical study evaluates the, tolerability, safety and efficacy of a patented ophthalmic topical formulation containing Helenalin. The aim is to assess potential clinical effects in patients diagnosed with DED, aiming to enhance treatment compliance, improve patient comfort, and alleviate symptoms while minimizing adverse events (33, 34). Through this investigation, we seek to contribute to the growing body of knowledge surrounding alternative therapies for chronic ocular surface inflammation and dry eye disease.
2.1. Materials and Methods
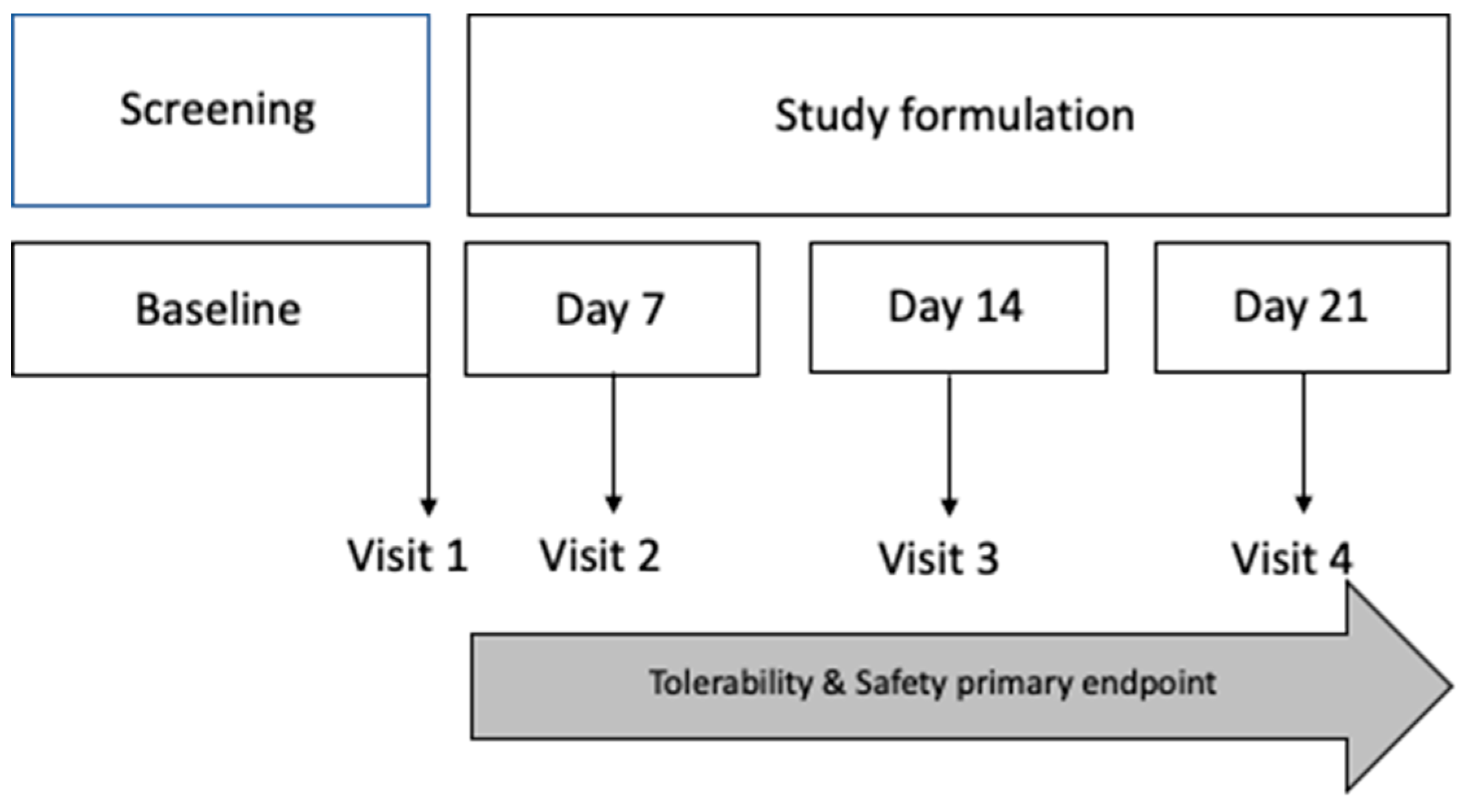
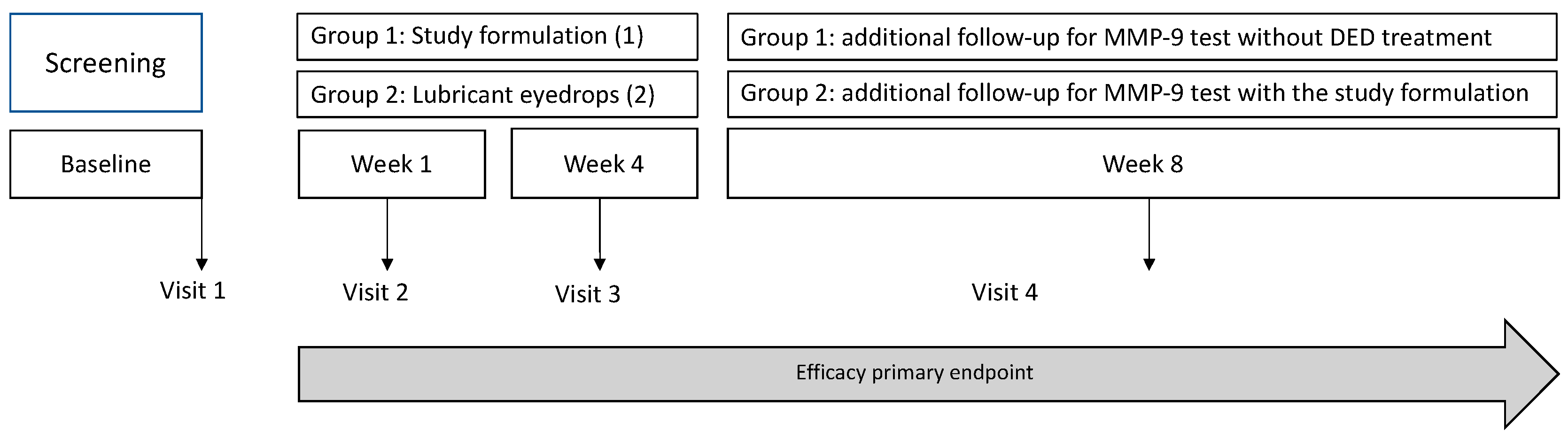
In pursuit of evaluating the tolerability, safety, and efficacy of an innovative ophthalmic topical formulation, a comprehensive single-center, prospective, interventional, double-blinded, randomized, controlled clinical trial was meticulously executed. This clinical investigation engaged the participation of both healthy subjects' eyes (pertaining to the safety and tolerability clinical study) and patients grappling with mild to moderate dry eye disease (DED) (pertaining to the efficacy clinical study), including a confirmation of the presence of Matrix Metalloproteinase 9 (MMP-9) through a positive InflammaDry© test result exceeding 40 ng/ml. The trial, which was undertaken from January to May 2023, adhered to the ethical principles encapsulated in the Declaration of Helsinki and took place in the ISO 9001:2015 certified ASG Clinical Retinal Research S.C., an ophthalmological research center situated in Zapopan, Mexico. Prior to patient enrollment, the study received approval from the internal review board and the CRMQ Ethics and Research Committee (ID: CRMQ-OFT-001-2022), in full alignment with the International Conference on Harmonization on Good Clinical Practices, accompanied by strict adherence to all pertinent local regulatory requisites and laws. Informed written consent was obtained from all participants and their accompanying witnesses, after ensuring a comprehensive understanding of the study's nature and potential adverse events.
2.2. Study Formulation
In congruence with the principles of Good Manufacturing Practice and the Mexican Pharmacopoeia 2020 (FEUM) (35), the ophthalmic formulation under scrutiny was meticulously prepared. This sterile, translucent ophthalmic suspension, ensconced within a 15 ml container, was crafted to incorporate helenalin (0.008% to 0.015%) and dehydroalanine tiglate (5% to 7%), deriving their origins from a 1% extract of
Arnica montana, which is included in the Mexican Herbal Pharmacopoeia (36). The Drug to Extract Ratio (DER) falling within the gamut of 1:5 to 1:7 was achieved. Moreover, this formulation incorporated hyaluronic acid, presenting a concentration of 0.4%. The formulation's pH was set at 7.4, complemented by a viscosity of 20-cPs. Noteworthy additions included ethylene diamine tetra-acetic acid (0.0005 g), benzalkonium chloride as a preservative (0.0002 g), hydroxypropylmethylcellulose (0.01 g), monobasic sodium phosphate (0.0003 g), dibasic sodium phosphate (0.0012 g), sodium chloride (0.009 g), sodium hydroxide (0.0001 g), and grade 2 purified water (0.9647 g). This formulation adhered to Mexican regulations. The full list of compounds can be appreciated in
Table 1.
2.3. Evaluation of Tolerability and Safety in Healthy Volunteers (Phase I clinical study)
A phase I clinical study was designed to assess the safety and tolerability of this ophthalmic formulation. Healthy individuals ranging from 18 to 65 years of age, were selected to participate in this phase I study. Good health was defined as the absence of any medical or surgical history (except for intraocular lens surgery performed more than 12 months prior). A stipulated baseline best-corrected visual acuity (BCVA) of no less than 0.1 in both eyes, an Ocular Surface Disease Index (OSDI) <13 (37, 38), a non-invasive film tear breakup time (NIF-BUT) >10 seconds, absent corneal and conjunctival staining, and a negative result on the InflammaDry® MMP-9 test were part of the inclusion criteria in this phase. Additionally, candidates were scrutinized for any ocular pathologic conditions, which, if present, led to exclusion of the study. It was mandatory for participants to refrain from using any form of eyedrops, particularly ocular lubricants, in both eyes for a minimum duration of six months prior to their enrollment in the study. Key exclusion criteria included systemic diseases associated with DED, history of recurrent ocular inflammation, ocular-lid trauma, active ocular-lid infection, use of systemic trigger-dry eye drugs, and corneal abnormalities that could interfere with the study evaluation tests (such as ocular staining, allergy to fluorescein sodium or lissamine green dyes). Participants´ demographic and baseline clinical data were systematically compiled five days before the onset of the study formulation application. After enrollment, participants were instructed to routinely apply one drop of the formulation three times a day in the study eye, for a period of two weeks. Follow-up was conducted the week after the application period, gauging any potential adverse events in alignment with tolerability and safety guidelines endorsed by FEUM (35, 36) and Comisión para la Protección contra Riesgos Sanitarios-COFEPRIS (
Figure 1). Compliance was also monitored; any value below 90% was tantamount to non-compliance and, thereby, excluded from statistical analysis.
Follow-up ocular evaluations included: the measurement of BCVA adhering to the ETDRS protocol, the determination of intraocular pressure (IOP) employing a tonometer (iCare® TA01i Tonometer), and the quantification of corneal endothelial cell density (cECD) through the utilization of specular microscopy (Perseus endothelial microscope from Costruzione Strumenti Oftalmici, Firenze, Italy). Additionally, a slit lamp examination with ocular surface staining leveraging fluorescein and lissamine green reagents was performed (AK-Fluor®, Akorn, Lake Forest, IL, USA and Rose Stone Enterprises, Alta Loma, CA, USA, respectively). Ocular AEs were reported concurring with NOM-220-SSA1-2016, which contains the Mexican regulatory guidelines for the instillation and handling of commercial and research drugs, herbal medicines, medical devices, and their potential adverse events (including ophthalmic products) (39). To reduce interobserver discrepancies, a single certified technician assessed safety and efficacy.
2.4. Evaluation of Efficacy in Patients with Mild to Moderate DED (Phase II clinical study)
We designed a phase II clinical study to evaluate the efficacy of the ophthalmic formulation. This was a prospective, randomized, double-blinded, crossover, interventional study comparing the study formulation with lubricant eye drops (HA 0.04%). The inclusion criteria for the study were mild to moderate DED, based on OSDI score (37, 38), a non-invasive film tear breakup time (NIF-BUT) <10 seconds, corneal and conjunctival staining, the presence of visual strain, and a daily screen interaction of less than 8 hours. Patients required a positive test result in the InflammaDry© test, as confirmation of elevated levels of MMP-9 (positive test result in levels >40ng/ml). After meeting these criteria, participants were randomly assigned into one of two efficacy study groups, and they were subsequently assigned to either receive the trial ophthalmic formulation (group 1) or a commercially available lubricant eye drop containing hyaluronic acid (group 2) (Linzaug® Laboratorios Opko, México) as control. Both eye drops were administered according to pre-specified protocols and frequencies (1 drop three times a day (TID) in both eyes).
To evaluate the formulation's efficacy, an evaluation strategy was devised, incorporating an array of ophthalmic parameters, tested at day 7, day 14, and day 28. These test included the assessment of best-corrected visual acuity (BCVA), the probing of non-invasive film tear breakup time (NIF-BUT) (using a Schwind Sirius+ topographer) (CSO SRL, Italy), and non-invasive average breakup time (NIAvg-BUT), the evaluation of meibomian gland changes (using the Schwind Sirius® Meibomiography) and the detection of MMP-9 using the InflammaDry® MMP-9 Test. Additional evaluations included conjunctival impression cytology (CIC), Schirmer's test 1, ocular surface staining, and the ocular irritability test (for techniques and technical details, consult Appendix A). To reduce interobserver discrepancies, a single certified technician performed the BCVA measurement. Safety and efficacy assessments were performed by a single, blinded, clinical investigator at each visit.
For the crossover, an additional comprehensive 4-week follow-up period was implemented for MMP-9 testing exclusively, encompassing both study groups. Participants in the treatment group (group 1) were directed to discontinue the application of the study formulation, while those in the control group (group 2) initiated the administration of the study formulation according to the established protocol, employing a crossover design without a washout period.
2.5. Data Analysis and Statistical Methods
The sample size was calculated using a formula for the difference between two independent means where nc is the sample size for the reference group (group 2) and ne is the one for the study group (group 1). D = (Mc-Me) where Mc is the mean of the first group and Me is the mean of the second one, S2 is the variance of both distributions, which are assumed to be equal, Zß is the value of the abscissa axis of the standard normal function where the probability (1 -ß) accumulates; assuming a mean difference in the OSDI value between the treatment group (group 1) and the reference group (group 2) of 22.4 OSDI units and a standard deviation of 15 units (l); the study would require a sample size of 19 subjects for each group, in order to achieve a power of 80% and a significance level of 5%, considering a 10-unit margin of superiority. Considering a loss of 20%, it is concluded that the final sample per group will be a minimum of 23 subjects: nc = ne = 2*S2 / D2 * (Z α/2 *Zß)2
Data was analyzed using the SPSS 22.0 software (IBM SPSS Statistics for Macintosh, version 22.0, IBM Corp, Armonk, NY, USA). Quantitative variables were described using means and standard deviation. Qualitative variables were described using frequencies and percentages. Intra-group analysis: they will be determined through the Wilcoxon rank test, for the quantitative variables. Analysis between groups: the differences between groups will be analyzed utilizing the Student’s T-test or the Mann–Whitney U statistic if applicable. Significance was defined as a p-value < 0.05.
3. Results
3.1. The study formulation is tolerable and safe in healthy volunteers.
Twenty-four female and male healthy volunteers were included in the tolerability and safety study group. The mean age was 36.4 ± 9.82. Thirteen subjects (54.16%) were men and eleven (45.83%) were female, with twelve right eyes (50%), and twelve left eyes (50%), two eyes were pseudophakic (8.33%). Demographic and clinical characteristics of patients and study eyes are shown in
Table 2. Concerning safety and tolerability outcomes, no SAEs were associated with the administration of the ophthalmic study formulation during the 21-day follow-up period.
Table 3 presents a comprehensive overview of all recorded adverse events (AEs), each of which exhibited a transitory nature following drop application and spontaneously resolved within a brief timeframe (<10 minutes). Furthermore, the clinical evaluation revealed no noteworthy ocular abnormalities or significant alterations. None of the 24 subjects exhibited significant changes in BCVA, IOP or cECD (
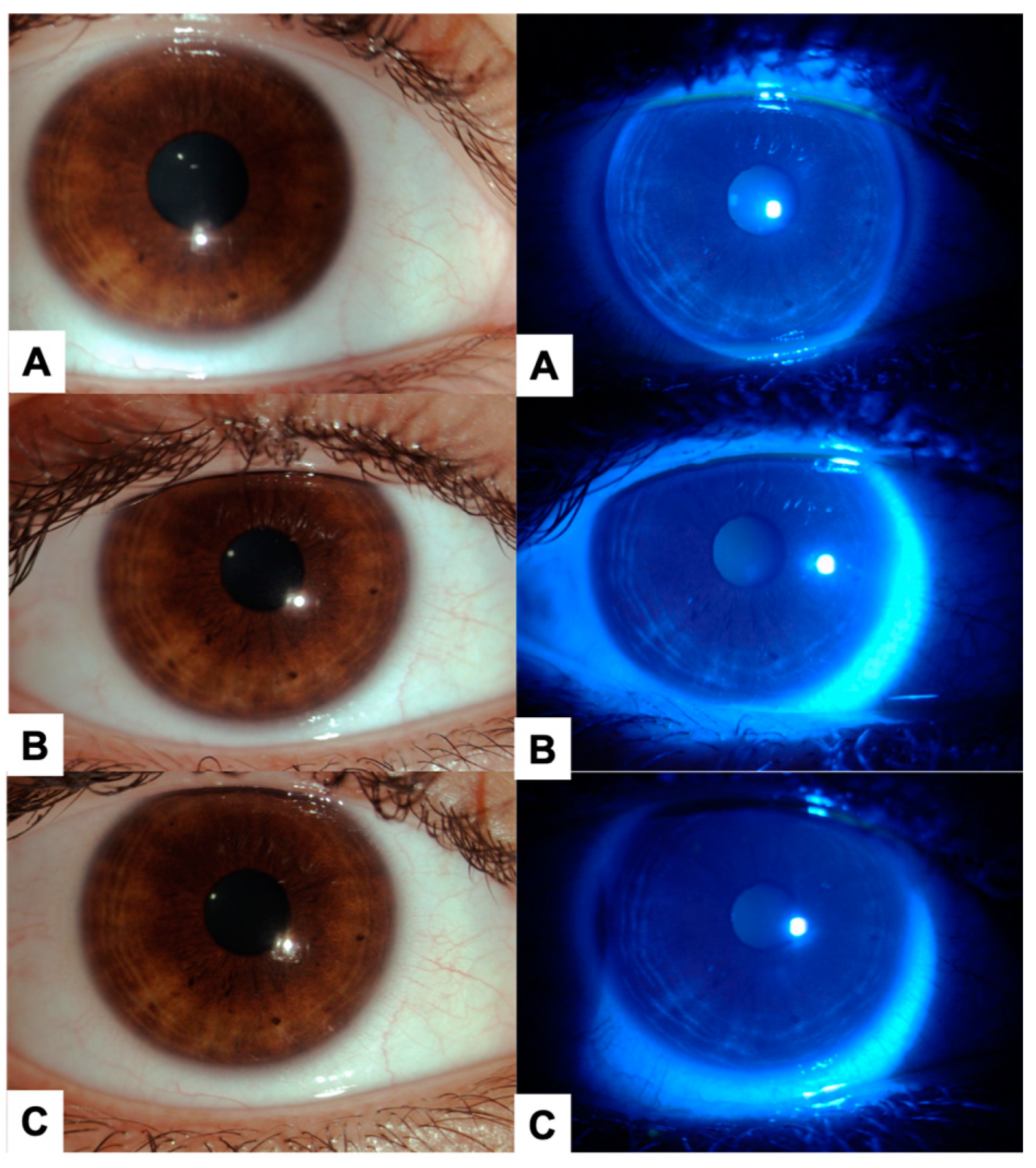
Table 4) throughout the clinical follow-up. Representative images of the ocular surface at baseline and final visit are shown in
Figure 3. Concerning safety and tolerability outcomes, the ophthalmic study formulation was well tolerated, and no SAEs were reported. There were no ocular abnormalities, nor significant changes in the clinical evaluation. With respect to BCVA measurement, there was also no significant difference between the study formulation group (group 1) (82.5 ± 4.2 vs 83.1 ± 2.2) and the commercially available eye lubricant group (group 2) (82.2 ± 5.1 vs 82.8 ± 2.7).
3.2. The Ophthalmic Study Formulation Ameliorates DED Symptoms, Improves Tear Film Objective Evaluations, increased the number of negative MMP-9 tests, and Improves CIC in Patients with Mild to Moderate DED.
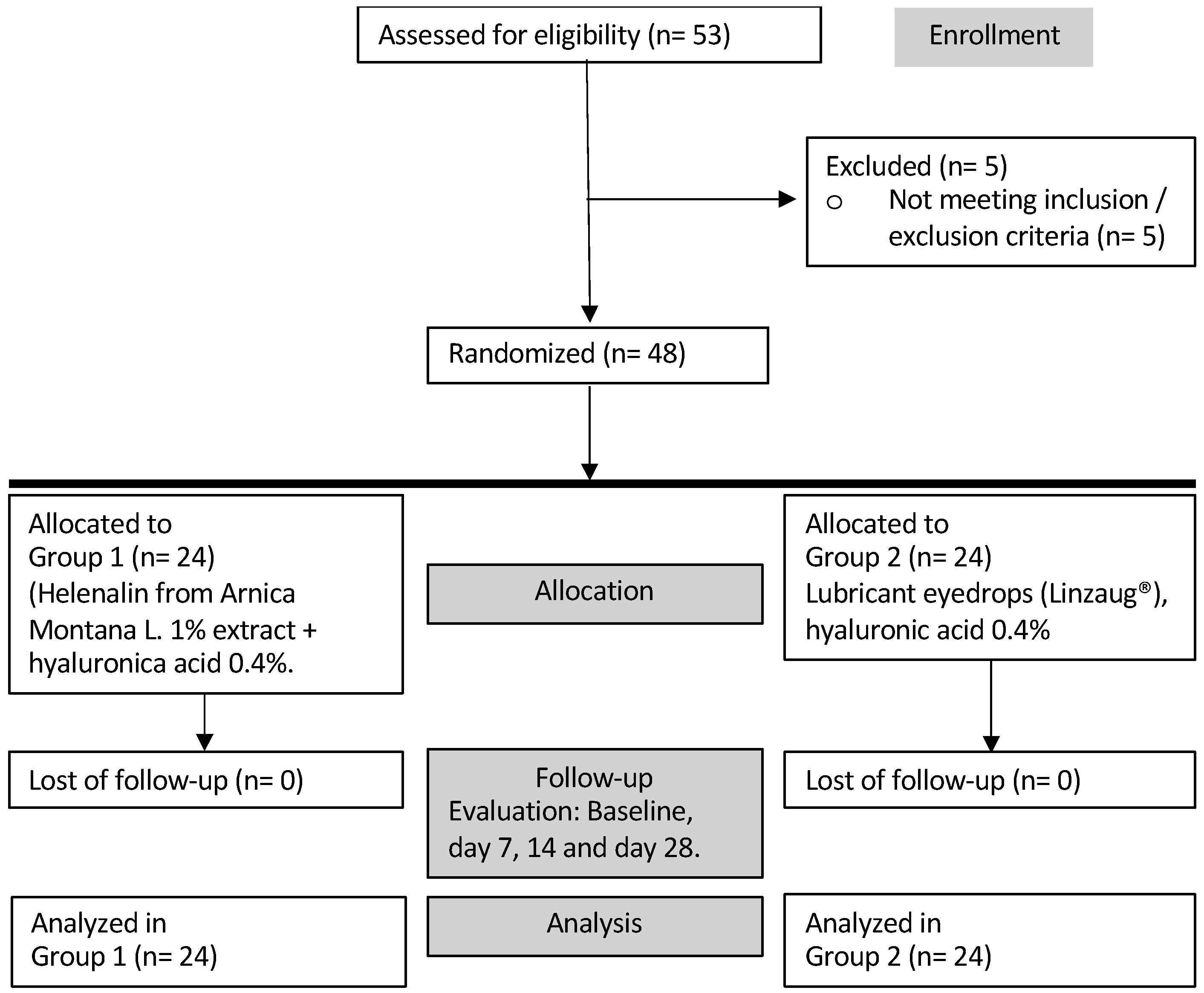
The efficacy study included patients with mild to moderate DED meeting all inclusion criteria. Data analysis for 48 subjects: 24 for the study group (group 1), and 24 for the control group (group 2), completed the follow-up period (
Figure 4).
Concerning the demographic and clinical characteristics of the subjects and the eyes involved in the efficacy assessment study, they are shown in
Table 5. Briefly, there was a similar number of male and female subjects, with an average age of 53.1 ± 9.82 for group 1 and 52.5 ± 13.15 for group 2. Ocular measurements did not show significant dissimilarities. There was no statistical significance between both groups.
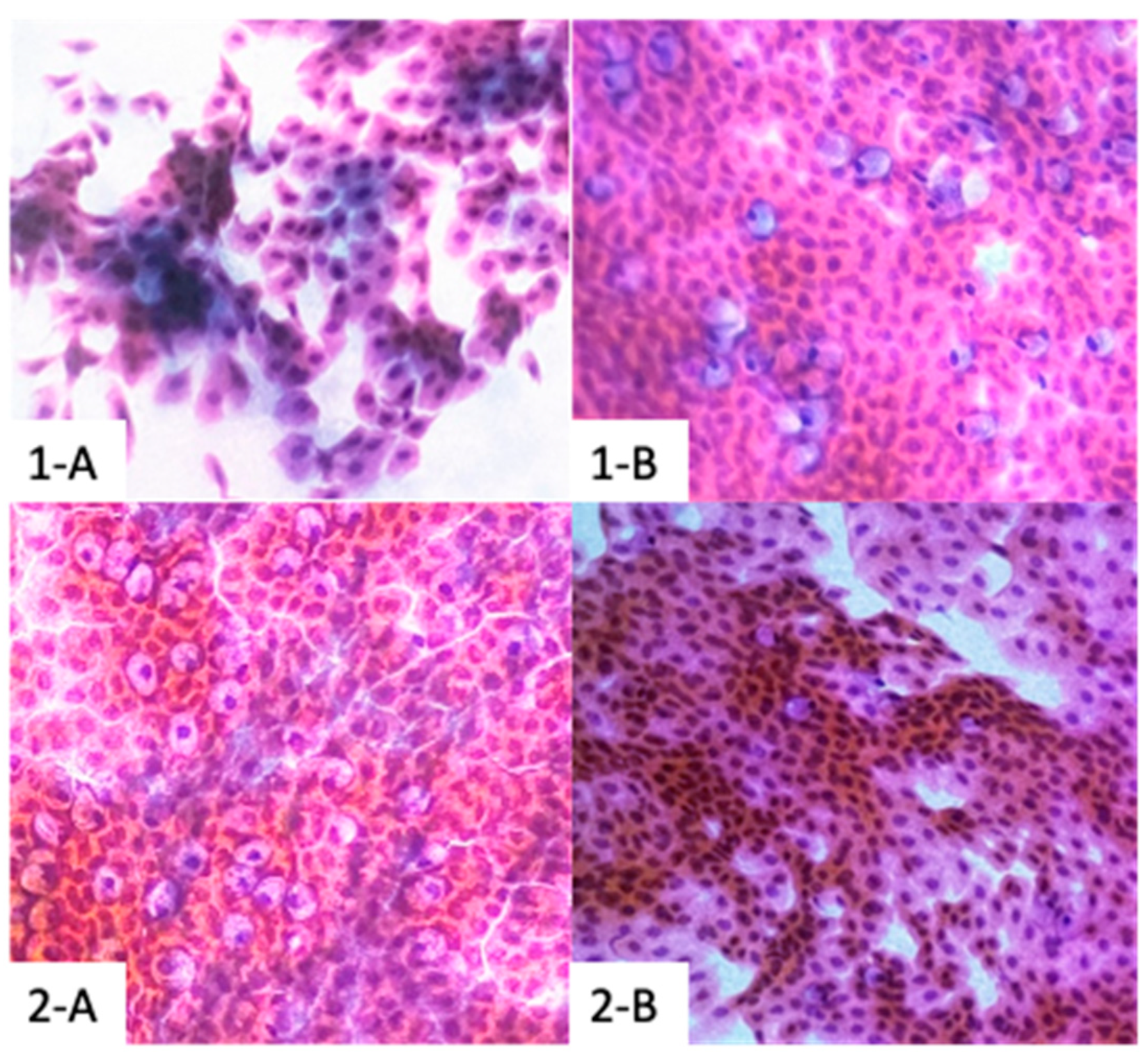
Regarding efficacy, there was a statistically significant difference between baseline and week 4 for the qualitative evaluation (OSDI) results in the study formulation group (group 1) and the commercially available lubricant eyedrop (group 2). Specifically, the results depicted a change from 21.31 ± 3.21 vs. 10.58 ± 4.21 in group 1, and 21.74 ± 15 vs. 11.23 ± 8.95, in group 2. There was also a statistically significant difference for the quantitative evaluation NIF-BUT when comparing baseline and week 4 observations in the study formulation group (group 1) (8.39 ± 5.86 vs. 14.53 ± 4.53) and group 2 (8.43 ± 4.82 vs. 13.83 ± 5.69). Only the study group (group 1) showed a statistically significant difference in the NIAvg-BUT measurement when comparing baseline and week 4 observations (10.46 ± 4.19 vs. 14.24 ± 3.66) whereas group 2 did not (9.85 ± 4.13 vs. 11.73 ± 5.82). The study formulation group exhibited a statistically significant difference in the Schirmer’s test measurements as well (15.83 ± 5.4 vs. 20.05 ± 4.37) whereas the control did not (16.11 ± 5.1 vs. 17.83 ± 6.28). Concerning MMP-9, group 1 showed a clear positive change (statistically significant difference) between baseline and week-4 visit, since only 6 out of 24 subjects presented positive MMP-9 tests by the end of the follow-up at week 4 (100% vs 25%). This difference was not observed in the 2 groups (24/24 100% vs. 21/24 87.5%). Additionally, after a 4-week period of treatment with the study formulation, there was a remarkable improvement in the morphology of the ocular surface since all subjects showed normal impression cytology at the end of the follow-up (8/24 33.3% vs. 0/24 0.0%). The commercially available lubricant eyedrops group (group 1) did not show a statistically significant difference in the impression cytology (7/24 29.1% for both, baseline and week-4 visit). These results are presented in
Table 6 and
Table 7. Impression cytology representative images are shown in
Figure 5. In reference to the OSS with F and LG dye, the study formulation group showed a statistical difference between the baseline vs. week 4 visit (
p = 0.0367
). Group 2 did not show a statistically significant difference (
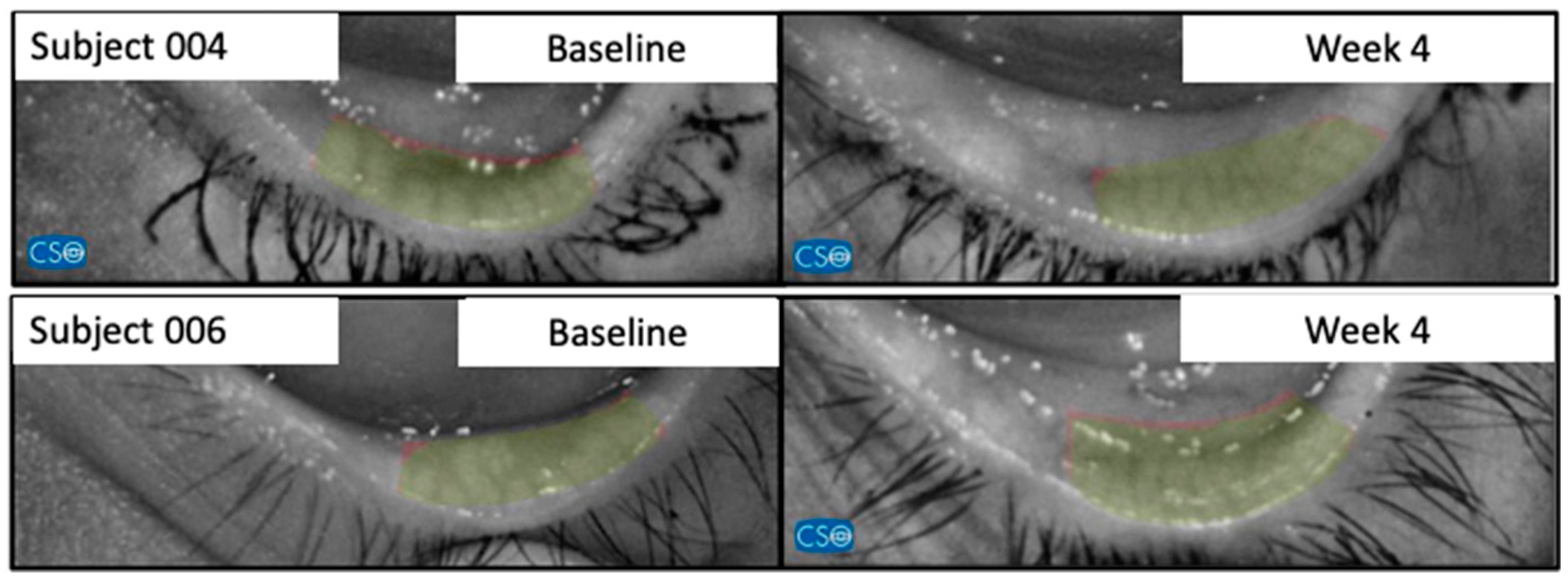
Table 8). Finally, with respect to meibomiography by Schwind Sirius®, all subjects of the study group showed a relevant improvement between baseline and week 4 clinical visits (
Figure 6).
After a cross-over without a washout, there was the supplementary 4-week follow-up period. A noteworthy transformation was evident among subjects in group 1 (without DED treatment) who tested positive for MMP-9 (6/24 – 25%), as their numbers surged to 22/24 (91.6%) after the crossover. Conversely, for participants in group 2, this trend reversed after transitioning to the helenalin-based topical formulation, with the positive MMP-9 cases decreasing from 18/24 (87.5%) to 5/24 (20.8%) after the crossover.
Table 2.
Demographic and clinical characteristics of healthy patients and healthy study eyes.
Table 2.
Demographic and clinical characteristics of healthy patients and healthy study eyes.
| |
Safety Group |
| Age |
36.4 ± 9.82 |
| Gender |
| Male (n) |
13 |
| Female (n) |
11 |
| Right eye (n) |
12 |
| Left eye (n) |
12 |
| Ocular findings |
| Pseudophakic (n) |
2 |
Table 3.
Adverse events reported in healthy eyes of healthy subjects after the application of the study formulation.
Table 3.
Adverse events reported in healthy eyes of healthy subjects after the application of the study formulation.
| |
|
Dry eye sensation |
Burning |
Discharge |
Tearing |
Blurred vision |
| |
|
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
| Frequency |
Not presented |
23 (95.83) |
21 (87.5) |
24 (100) |
22 (91.66) |
23 (95.83) |
| Uncommon |
1 (4.16) |
1 (4.16) |
|
1 (4.16) |
1 (4.16) |
| Occasionally |
|
2 (8.33) |
|
1 (4.16) |
|
| Most of time |
|
|
|
|
|
| All the time |
|
|
|
|
|
| Severity |
Mild |
1 (4.16) |
3 (12.5) |
|
|
1 (4.16) |
| Moderate |
|
|
|
2 (8.33) |
|
| Severe |
|
|
|
|
|
Table 4.
Clinical characteristics of healthy eyes of subjects treated with the ophthalmic study formulation.
Table 4.
Clinical characteristics of healthy eyes of subjects treated with the ophthalmic study formulation.
| |
|
|
|
|
Baseline |
Day 21 |
| |
|
|
|
|
AVMC |
PIO |
cECD |
AVMC |
PIO |
cECD |
| Subject |
Gender |
Study Eye |
Age |
Subject |
(ETDRS-letters) |
(mmHg) |
(mm) |
(ETDRS-letters) |
(mmHg) |
(mm) |
| |
|
|
(Years) |
|
|
|
|
|
|
|
| |
|
|
|
|
83 |
12 |
3189 |
83 |
11 |
3178 |
| 1 |
F |
OD |
26 |
1 |
84 |
11 |
3284 |
85 |
13 |
3190 |
| 2 |
F |
OD |
27 |
2 |
85 |
13 |
3182 |
84 |
17 |
3204 |
| 3 |
M |
OD |
26 |
3 |
83 |
13 |
3472 |
83 |
11 |
3488 |
| 4 |
M |
OD |
26 |
4 |
82 |
11 |
3323 |
84 |
14 |
3339 |
| 5 |
M |
OS |
25 |
5 |
84 |
14 |
3380 |
85 |
12 |
3382 |
| 6 |
M |
OS |
25 |
6 |
84 |
12 |
3452 |
84 |
12 |
3451 |
| 7 |
F |
OS |
24 |
7 |
83 |
12 |
3234 |
85 |
15 |
3230 |
| 8 |
F |
OS |
26 |
8 |
83 |
16 |
3085 |
85 |
13 |
3098 |
| 9 |
F |
OS |
24 |
9 |
83 |
11 |
3119 |
83 |
17 |
3127 |
| 10 |
F |
OS |
25 |
10 |
84 |
16 |
2874 |
84 |
15 |
2890 |
| 11 |
M |
OD |
56 |
11 |
82 |
17 |
2639 |
85 |
14 |
2620 |
| 12 |
M |
OD |
35 |
12 |
84 |
11 |
2572 |
85 |
15 |
2581 |
| 13 |
M |
OD |
47 |
13 |
85 |
18 |
2951 |
85 |
16 |
2947 |
| 14 |
F |
OD |
36 |
14 |
83 |
13 |
2383 |
85 |
14 |
2385 |
| 15 |
F |
OD |
63 |
15 |
83 |
15 |
2742 |
83 |
14 |
2746 |
| 16 |
M |
OS |
56 |
16 |
84 |
16 |
3183 |
84 |
14 |
3180 |
| 17 |
F |
OD |
40 |
17 |
84 |
14 |
2508 |
85 |
11 |
2519 |
| 18 |
M |
OS |
38 |
18 |
83 |
15 |
2823 |
84 |
13 |
2832 |
| 19 |
M |
OD |
45 |
19 |
82 |
12 |
2937 |
84 |
10 |
2926 |
| 20 |
M |
OS |
28 |
20 |
83 |
12 |
3166 |
83 |
16 |
3175 |
| 21 |
F |
OS |
31 |
21 |
82 |
16 |
2593 |
84 |
14 |
2603 |
| 22 |
M |
OD |
39 |
22 |
83 |
11 |
2496 |
84 |
15 |
2509 |
| 23 |
F |
OS |
47 |
23 |
83 |
15 |
2269 |
85 |
16 |
2276 |
| 24 |
M |
OS |
59 |
24 |
|
|
|
|
|
|
| |
|
|
|
|
83.2 ± 1.9 |
13.58 ± 2.59 |
2952.33 ± 396 |
84.20 ± .8 ‡ |
13.83 ± 2.63 ‡ |
2953.16 ± 401 ‡ |
| X ± s |
|
|
36 ± 14.82 |
X ± s |
|
|
|
|
|
|
| ni |
F= 11 M= 13 |
OD= 12 OS= 12 |
|
ni |
|
|
|
0.096 |
0.4853 |
0.2825 |
| P |
|
|
|
P |
|
|
|
|
|
|
Table 5.
Demographic and clinical characteristics of subjects and eyes of the efficacy study.
Table 5.
Demographic and clinical characteristics of subjects and eyes of the efficacy study.
| |
Group 1 (Study Formulation) |
Group 2 (Control / Commercially available eye lubricant) |
| Age |
53.1 ± 9.82 |
52.5 ± 13.15 † |
| Gender |
|
† |
| Male (n) |
12 |
12 |
| Female (n) |
12 |
12 |
| Hypertension (n) |
1 |
2 |
| Ocular findings: |
|
|
| Pseudophakic (n) |
5 |
3 |
| Basal BCVA (ETDRS letters) |
82.5 ± 4.2 |
82.2 ± 5.1 † |
| OSDI (score) |
21.31 ± 3.21 |
21.74 ± 15 † |
| NIF-BUT (s) |
8.39 ± 5.86 |
8.43 ± 4.82 † |
| NIAvg-BUT (s) |
10.46 ± 4.19 |
9.85 ± 4.13 † |
| Schirmer’s test (mm) |
15.83 ± 5.4 |
16.11 ± 5.1 † |
| MMP-9 Test positivity |
(24/24) 100% |
(24/24) 100% † |
| Impression cytology with abnormal characteristics |
8/24 (33.3%) |
7/24 (29.1%) † |
Table 6.
Quantitative variables analysis in DED patients exposed to the study formulation (1) or commercially available lubricant eyedrops (2).
Table 6.
Quantitative variables analysis in DED patients exposed to the study formulation (1) or commercially available lubricant eyedrops (2).
| |
1 |
2 |
| Variable/Visit |
B |
w-4 |
B |
w-4 |
| OSDI (score) |
21.31 ± 3.21 |
10.58 ± 4.21 * |
21.74 ± 15 |
11.23 ± 8.95 * |
| NIF-BUT (s) |
8.39 ± 5.86 |
14.53 ± 4.53 * |
8.43 ± 4.82 |
13.83 ± 5.69 * |
| NIAvg-BUT (s) |
10.46 ± 4.19 |
14.24 ± 3.66 * |
9.85 ± 4.13 |
11.73 ± 5.82 |
| Schirmer’s test (mm) |
15.83 ± 5.4 |
20.05 ± 4.37 * |
16.11 ± 5.1 |
17.83 ± 6.28 |
| MMP-9 elevated levels |
24/24 (100%) |
6/24 (25%) * |
24/24 (100%) |
21/24 (87.5%) |
| Impression cytology with abnormal characteristics |
8/24 (33.3%) |
0/0 (0.0%) * |
7/24 (29.1%) |
7/24 (29.1%) |
Table 7.
Impression cytology of the ocular surface with Millipore membrane impression cytology, grading system by Nelson, for 1 group vs 2 group.
Table 7.
Impression cytology of the ocular surface with Millipore membrane impression cytology, grading system by Nelson, for 1 group vs 2 group.
| |
1-group |
2-group |
| Number of subjects |
Baseline |
Week 4 |
Baseline |
Week 4 |
| 1 |
1 |
0 |
1 |
1 |
| 2 |
2 |
0 |
3 |
3 |
| 3 |
3 |
0 |
2 |
2 |
| 4 |
2 |
0 |
1 |
2 |
| 5 |
2 |
0 |
2 |
2 |
| 6 |
3 |
0 |
3 |
3 |
| 7 |
2 |
0 |
2 |
2 |
| 8 |
2 |
0 |
|
|
Table 8.
Ocular surface staining score (OSS), ocular surface staining with fluorescein and lissamine green in dry-eye patients exposed to the study formulation (Group 1) and control group (Group 2).
Table 8.
Ocular surface staining score (OSS), ocular surface staining with fluorescein and lissamine green in dry-eye patients exposed to the study formulation (Group 1) and control group (Group 2).
| Group 1 Group 2 |
|---|
| Grade/Visit |
Baseline |
Week 4* |
Baseline |
Week 4 |
| 0 |
2 |
18 |
1 |
3 |
| I |
10 |
6 |
11 |
9 |
| II |
9 |
0 |
6 |
8 |
| III |
3 |
0 |
6 |
4 |
| IV |
0 |
0 |
0 |
0 |
| V |
0 |
0 |
0 |
0 |
Figure 5.
Representative images of impression cytology at baseline (1-A) and month 1 (1-B). Millipore membrane impression cytology, Nelson gradation. Staining in Papanicolaou. 1-A: BASELINE, Stage 0, Grade 3. Abundant cellularity, goblet cells of 80-200 cells per mm2, moderate frequent intercellular separations with modified cytoplasmic-nucleus ratio in favor of cytoplasmic. Mild inflammation, slightly increased apoptosis. 1-B: WEEK 4, Stage 0, Grade 0. Abundant cellularity is appreciated, goblet cells of 400 cells or more per mm2, cohesive with normal cytoplasmic nucleus ratio. There are no inflammatory cells or apparent apoptosis. Also, representative images of impression cytology at baseline (2-A) and month 1 (2-B). Millipore membrane impression cytology, Nelson gradation. Staining in Papanicolaou. 2-A: BASELINE, Stage 0, Grade 1. Abundant cellularity, goblet cells of 300-400 cells per mm2, cohesive or discrete intercellular separations with normal nuclear-cytoplasmic relationship. Minimal inflammation, minimal apoptosis. 2-B: WEEK 4, Stage 0, Grade 2. Abundant cellularity, goblet cells of 200-300 cells per mm2, frequent slight intercellular separations with modified cytoplasmic-nucleus relationship in favor of cytoplasmic. Mild inflammation, slightly increased apoptosis.
Figure 5.
Representative images of impression cytology at baseline (1-A) and month 1 (1-B). Millipore membrane impression cytology, Nelson gradation. Staining in Papanicolaou. 1-A: BASELINE, Stage 0, Grade 3. Abundant cellularity, goblet cells of 80-200 cells per mm2, moderate frequent intercellular separations with modified cytoplasmic-nucleus ratio in favor of cytoplasmic. Mild inflammation, slightly increased apoptosis. 1-B: WEEK 4, Stage 0, Grade 0. Abundant cellularity is appreciated, goblet cells of 400 cells or more per mm2, cohesive with normal cytoplasmic nucleus ratio. There are no inflammatory cells or apparent apoptosis. Also, representative images of impression cytology at baseline (2-A) and month 1 (2-B). Millipore membrane impression cytology, Nelson gradation. Staining in Papanicolaou. 2-A: BASELINE, Stage 0, Grade 1. Abundant cellularity, goblet cells of 300-400 cells per mm2, cohesive or discrete intercellular separations with normal nuclear-cytoplasmic relationship. Minimal inflammation, minimal apoptosis. 2-B: WEEK 4, Stage 0, Grade 2. Abundant cellularity, goblet cells of 200-300 cells per mm2, frequent slight intercellular separations with modified cytoplasmic-nucleus relationship in favor of cytoplasmic. Mild inflammation, slightly increased apoptosis.
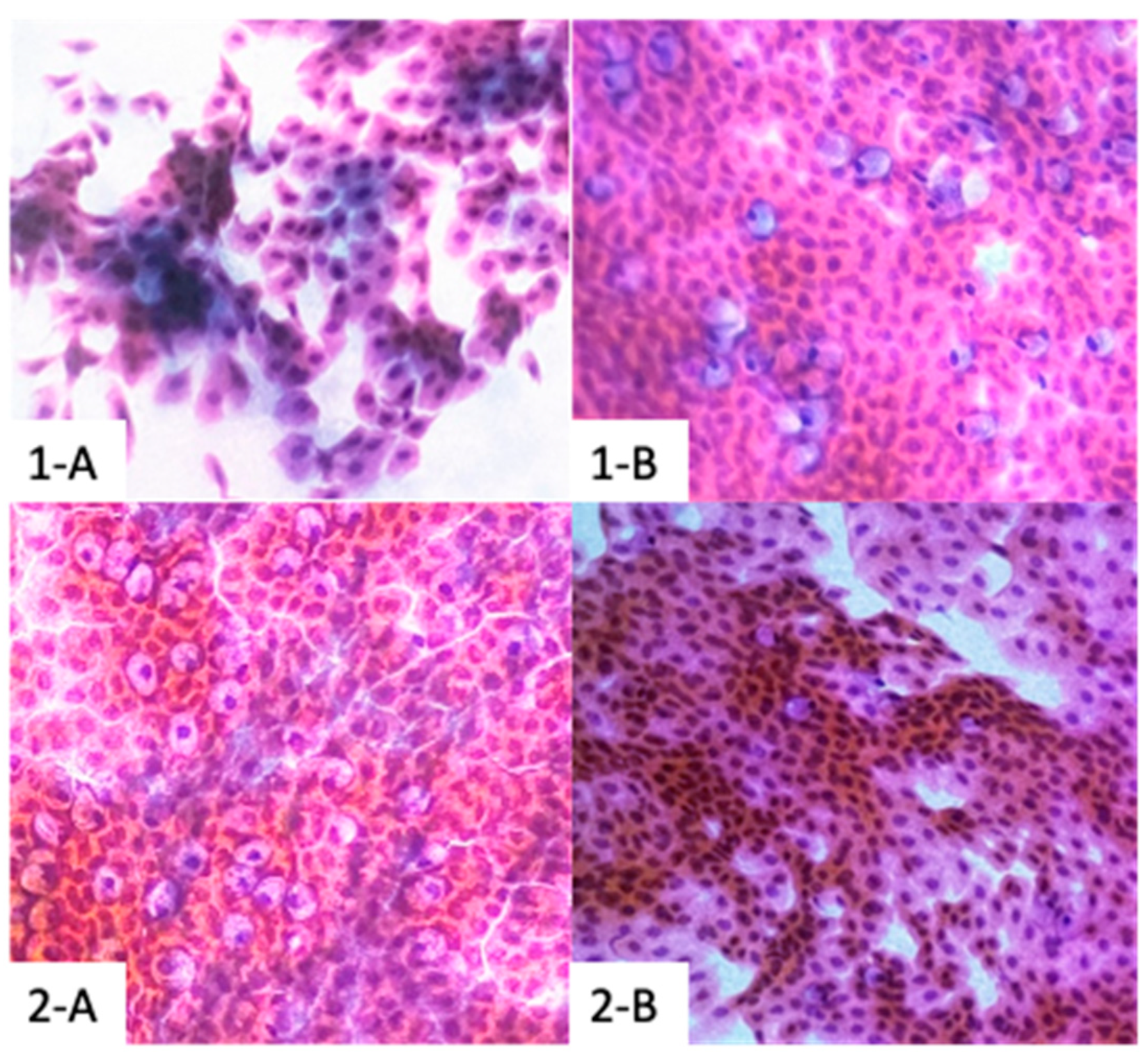
Figure 6.
Representative images of 2 patients of the study formulation group (1) of meibomiography taken with the Schwind Sirius® that shows notable improvement between baseline and week 4. This significative improvement was not observed in the control group (2).
Figure 6.
Representative images of 2 patients of the study formulation group (1) of meibomiography taken with the Schwind Sirius® that shows notable improvement between baseline and week 4. This significative improvement was not observed in the control group (2).
4. Discussion
Dry eye syndrome (DES) is a prevalent ocular condition that impacts tear film stability, production, and quality, resulting in symptoms of discomfort, visual disturbances, and potential harm to the ocular surface (40). The global prevalence of DED varies widely among different populations, with reported rates ranging from 9% to 50% . The emergence of the SARS-CoV-2 pandemic has further exacerbated the prevalence of DED due to increased remote working activities and extended digital screen exposure, leading to a rise in computer vision syndrome and dry eye-related visual strain (41, 42).
Lubricant eye drops are the current gold standard for DED treatment (34). However, patient adherence to these treatments remains a concern, with up to 60% of individuals using DED medications on an as-needed basis (28, 33). Factors contributing to poor adherence include complex treatment routines, lack of immediate symptom relief, and side effects (28, 43). Chronic inflammation of the ocular surface (CIOS) is a critical component of DED, influenced by factors such as environmental conditions, autoimmune disorders, hormonal changes, and digital device use (27, 28, 44, 45).
Oxidative stress and hyperosmolarity contribute to CIOS by activating the NF-κB pathway, resulting in the release of pro-inflammatory cytokines, chemokines, and matrix metalloproteinases (MMPs)(46-49). This chronic inflammation damages the cornea and conjunctiva, leading to symptoms and ocular surface damage (50-54). MMP-9 levels are elevated in DED, contributing to goblet cell depletion and sustained inflammation (55-58). Conjunctival chronic inflammation and goblet cell loss correlate with DED severity and ocular surface inflammation (53, 54).
Safety and tolerability were paramount considerations. The study formulation demonstrated a favorable safety profile, with no serious adverse events reported. Minor and transient adverse events were observed but resolved spontaneously. A combination of hyaluronic acid and Arnica montana extract was previously shown to be safe and effective for treating DED-related symptoms (59).
In this study, a novel ophthalmic formulation containing helenalin from Arnica montana and hyaluronic acid was evaluated for tolerability, safety, efficacy, and anti-inflammatory properties in patients with mild to moderate DED. The formulation showed improvement in objective tear film evaluations, including tear film breakup time (TBUT) and Schirmer's test, consistent with the positive effect of hyaluronic acid on these parameters (60). Notably, the study formulation reduced the MMP-9 positivity rate, which in an indirect marker of inflammation. This anti-inflammatory effect could be attributed to the helenalin component, which inhibits NF-κB activation and the downstream cytokines, including IL-1, IL-6, as well as other pro-inflammatory cytokines. (16, 19).
Impression cytology (IC) revealed improvement in conjunctival morphology with the study formulation, reflected by increased goblet cell density and reduced squamous metaplasia. IC is a valuable tool for objectively assessing DED severity (56, 57). Interestingly, the control group using hyaluronic acid eye drops did not show significant improvements in these parameters.
Inhibiting NF-κB signaling holds promise as a therapeutic approach for DED (10, 16-20). The study formulation's anti-inflammatory effect, likely mediated by helenalin's NF-κB inhibition, supports this strategy. However, further research is needed to fully understand helenalin's mechanisms and efficacy in different disease contexts.
Despite being a prospective, well-conducted investigation, our study's limitations include a limited follow-up and a relatively small sample size. Future studies should explore longer treatment durations and preservative-free formulations. Despite these limitations, this study underscores the potential of the helenalin-based formulation in managing DED, providing a safer and alternative treatment option for patients.
DED is a prevalent condition with diverse etiologies, including chronic inflammation. The novel ophthalmic formulation containing helenalin from Arnica montana and hyaluronic acid demonstrated tolerability, safety, efficacy, and anti-inflammatory properties in patients with mild to moderate DED. The formulation's positive effects on tear film parameters, conjunctival morphology, and MMP-9 levels highlight its potential therapeutic value. Targeting NF-κB signaling through helenalin provides a novel approach to DED management. As patients seek alternative and effective treatments for DED, the helenalin-based formulation could offer new hope in alleviating the burden of this condition.
5. Conclusions
The helenalin-based formulation derived from Arnica montana and sodium hyaluronate has demonstrated excellent tolerability and a good safety profile as a lubricant eye drop in individuals with healthy eyes. Additionally, it exhibits notable clinical efficacy by alleviating dry eye-related symptoms (as indicated by the OSDI score), enhancing tear film stability (measured by NIF-BUT, NIAvg-BUT, OSS, Schirmer's test, and meibomiography), and exerting an anti-inflammatory effect (evidenced by the reduction in MMP-9 positivity rate and the normalization of CIC) in patients afflicted with mild to moderate DED. Considering the favorable clinical outcomes and the acceptable safety profile exhibited by topical helenalin within this study, it is prudent to advocate for further comprehensive investigations on a larger cohort. Furthermore, it is imperative to explore the application of this topical formulation in the context of other ocular surface conditions that are linked to NF-κB activity. It is worth emphasizing that addressing DED necessitates a multifaceted approach, wherein the targeting of NF-κB, while vital, might not be an all-encompassing solution. Effective management requires the integration of a variety of strategies, including the use of lubricant eye drops, proper eyelid hygiene practices, and lifestyle modifications.
Figure 7.
Regulation and activation of the NF-κß cell-signaling pathway: The canonical NF-kß pathway is a key mediator of inflammatory processes through the inducible expression of chemokines and cytokines. The NF-κß pathway responds to multiple immunity cues, such as ligands, pattern- recognition receptors (PRRs), TNF receptor superfamily members, T-cell receptor (TCR) and B-cell receptor. The NF-κß pathway is a highly complex signaling process, marked by multiple forms of elegant, highly preserved forms of regulation. To prevent constant activation of this inflammatory pathway, inhibitory proteins like Iκß normally sequester the NF-kß complex proteins in the cytoplasm. Therefore, to achieve the inducible expression of inflammatory cytokines, canonical NF-κß activation requires degradation of Iκßα. This is achieved by phosphorylation of the Iκß kinase (IKK) complex. It has been previously shown that helenalin modifies the NF-κß/Ικß complex, preventing the release of Ικß.
Figure 7.
Regulation and activation of the NF-κß cell-signaling pathway: The canonical NF-kß pathway is a key mediator of inflammatory processes through the inducible expression of chemokines and cytokines. The NF-κß pathway responds to multiple immunity cues, such as ligands, pattern- recognition receptors (PRRs), TNF receptor superfamily members, T-cell receptor (TCR) and B-cell receptor. The NF-κß pathway is a highly complex signaling process, marked by multiple forms of elegant, highly preserved forms of regulation. To prevent constant activation of this inflammatory pathway, inhibitory proteins like Iκß normally sequester the NF-kß complex proteins in the cytoplasm. Therefore, to achieve the inducible expression of inflammatory cytokines, canonical NF-κß activation requires degradation of Iκßα. This is achieved by phosphorylation of the Iκß kinase (IKK) complex. It has been previously shown that helenalin modifies the NF-κß/Ικß complex, preventing the release of Ικß.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
The study was conducted following the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Centro de Retina Médica y Quirúrgica S.C. Committee (ID: CRMQ-OFT-001-2022); approved in December 2022.
Use of Artificial Intelligence
During the preparation of this work the authors used (
https://chat.openai.com/) to help with text structure and length, grammatical corrections, and spelling checks. No scientific information was retrieved using this tool. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data presented in this study are available upon request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Acknowledgments
We want to thank all technical staff of Centro de Retina Médica y Quirúrgica S.C., especially Oscar Eduardo Sanchez-Aguilar, for their incredible effort in the realization of this project.
Conflicts of Interest
This work was conducted by Centro de Retina Médica y Quirúrgica S.C., of which Juan Carlos Altamirano-Vallejo and Arturo Santos are employees. Centro de Retina Médica y Quirúrgica S.C. is developing products related to the research described in this publication. All other authors report no conflict of interes.
Appendix A
Objective evaluation involved a baseline ophthalmologic clinical examination, with subsequent assessments on day 7, day 14, and day 28. The evaluations encompassed various ophthalmic parameters, including:
- -
Best Corrected Visual Acuity (BCVA), according to ETDRS protocol.
- -
Non-invasive film tear breakup time (NIF-BUT) and non-invasive average breakup time (NIAvg-BUT) using the Schwind Sirius+ topographer (CSO SRL, Italy).
- -
Meibomiography with Schwind Sirius: Meiboscores were assigned based on grades 0 to 3 for meibomian gland changes.
- -
MMP-9 evaluation with InflammaDry MMP-9 Test (right eye only): Sampling fleece dabbed on lower eyelid conjunctiva, test assembled as per manufacturer's instructions.
- -
Conjunctival impression cytology (CIC) (left eye only): Millipore filter pressed onto palpebral conjunctiva, sample fixed with ethyl alcohol, graded using Nelson system.
The following are the Nelson gradation system grades:
Grade 0: Normal or minimal changes, intact goblet cells, normal epithelial cells.
Grade 1: Mild metaplasia, altered cells, increased non-goblet epithelial cells.
Grade 2: Moderate metaplasia, reduced goblet cells, increased non-goblet epithelial cells.
Grade 3: Severe metaplasia, absence of goblet cells, prevalence of squamous epithelial cells.
- -
Schirmer test 1 (without anesthesia) for tear secretion volume (Eagle Vision, Inc., Memphis, TN, USA).
- -
Ocular surface staining: F and LG staining using 1.5 mg strips with 1% reagent, assessed according to SICCA guidelines, employing Ocular Staining Score (OSS).
- -
Intraocular pressure (IOP) with Icare TA01i tonometer, fundus assessment with binocular indirect ophthalmoscope.
- -
Comprehensive safety assessment involved collecting and summarizing ocular and non-ocular AEs across evaluations.
All assessments occurred in a controlled environment (humidity: 40-50%, temperature: 23-25 °C), with compliance monitored through a patient care journal. Adherence <90% led to exclusion. Withdrawal was allowed, but alternative DED treatments weren't. Changes from baseline to day 28 in various tests were considered efficacy endpoints. Diagnostic criteria included OSDI >13, BUT <10 s, Schirmer <10 mm/5 min, and positive staining score.
The OSDI questionnaire (Spanish version) was used for subjective ophthalmic assessment.
A certified technician conducted BCVA measurement, while a blinded clinical investigator performed safety and efficacy assessments. A crossover design included a 4-week follow-up for MMP-9 testing, with group 1 discontinuing the formulation and group 2 initiating it without a washout period.
References
- Matos MS, Anastácio JD, Nunes Dos Santos C. Sesquiterpene Lactones: Promising Natural Compounds to Fight Inflammation. Pharmaceutics. 2021;13(7). Epub 20210630. [CrossRef]
- Cheynier V. Polyphenols in foods are more complex than often thought. Am J Clin Nutr. 2005;81(1 Suppl):223S-9S. [CrossRef]
- Laurella LC, Mirakian NT, Garcia MN, Grasso DH, Sülsen VP, Papademetrio DL. Sesquiterpene Lactones as Promising Candidates for Cancer Therapy: Focus on Pancreatic Cancer. Molecules. 2022;27(11). Epub 20220529. [CrossRef]
- Sülsen VP. Sesquiterpene Lactones and Diterpenes: Promising Therapeutic Candidates for Infectious Diseases, Neoplasms and Other Chronic Disorders. Molecules. 2021;26(5). Epub 20210226. [CrossRef]
- Martino VS, Sülsen VP. Sesquiterpene Lactones : Advances in their Chemistry and Biological Aspects. Cham: Springer International Publishing : Imprint: Springer,; 2018.
- Hoffmann R, von Schwarzenberg K, López-Antón N, Rudy A, Wanner G, Dirsch VM, et al. Helenalin bypasses Bcl-2-mediated cell death resistance by inhibiting NF-κB and promoting reactive oxygen species generation. Biochem Pharmacol. 2011;82(5):453-63. Epub 20110602. [CrossRef]
- Paço A, Brás T, Santos JO, Sampaio P, Gomes AC, Duarte MF. Anti-Inflammatory and Immunoregulatory Action of Sesquiterpene Lactones. Molecules. 2022;27(3). Epub 20220208. [CrossRef]
- Gou J, Hao F, Huang C, Kwon M, Chen F, Li C, et al. Discovery of a non-stereoselective cytochrome P450 catalyzing either 8α- or 8β-hydroxylation of germacrene A acid from the Chinese medicinal plant, Inula hupehensis. Plant J. 2018;93(1):92-106. Epub 20171130. [CrossRef]
- Moujir L, Callies O, Sousa PMC, Sharopov F, Seca AML. Applications of Sesquiterpene Lactones: A Review of Some Potential Success Cases. Applied Sciences. 2020;10(9):3001. [CrossRef]
- Ekenäs C, Zebrowska A, Schuler B, Vrede T, Andreasen K, Backlund A, et al. Screening for anti-inflammatory activity of 12 Arnica (Asteraceae) species assessed by inhibition of NF-kappaB and release of human neutrophil elastase. Planta Med. 2008;74(15):1789-94. Epub 20081030. [CrossRef]
- Bartikova H, Hanusova V, Skalova L, Ambroz M, Bousova I. Antioxidant, pro-oxidant and other biological activities of sesquiterpenes. Curr Top Med Chem. 2014;14(22):2478-94. [CrossRef]
- Tang JJ, Huang LF, Deng JL, Wang YM, Guo C, Peng XN, et al. Cognitive enhancement and neuroprotective effects of OABL, a sesquiterpene lactone in 5xFAD Alzheimer's disease mice model. Redox Biol. 2022;50:102229. Epub 20220108. [CrossRef]
- Fang B, Wen S, Li Y, Bai F, Wei Y, Xiong Y, et al. Prediction and verification of target of helenalin against hepatic stellate cell activation based on miR-200a-mediated PI3K/Akt and NF-κB pathways. Int Immunopharmacol. 2021;92:107208. Epub 20210111. [CrossRef]
- Ibraheim ZZ, Abdel-Mageed WM, Dai H, Guo H, Zhang L, Jaspars M. Antimicrobial antioxidant daucane sesquiterpenes from Ferula hermonis Boiss. Phytother Res. 2012;26(4):579-86. Epub 20110926. [CrossRef]
- Kriplani P, Guarve K, Baghael US. Arnica montana L. - a plant of healing: review. J Pharm Pharmacol. 2017;69(8):925-45. Epub 20170411. [CrossRef]
- Lyss G, Knorre A, Schmidt TJ, Pahl HL, Merfort I. The anti-inflammatory sesquiterpene lactone helenalin inhibits the transcription factor NF-kappaB by directly targeting p65. J Biol Chem. 1998;273(50):33508-16. [CrossRef]
- Jakobs A, Steinmann S, Henrich SM, Schmidt TJ, Klempnauer KH. Helenalin Acetate, a Natural Sesquiterpene Lactone with Anti-inflammatory and Anti-cancer Activity, Disrupts the Cooperation of CCAAT Box/Enhancer-binding Protein β (C/EBPβ) and Co-activator p300. J Biol Chem. 2016;291(50):26098-108. Epub 20161101. [CrossRef]
- Yang M, Zhang W, Yu X, Wang F, Li Y, Zhang Y, et al. Helenalin Facilitates Reactive Oxygen Species-Mediated Apoptosis and Cell Cycle Arrest by Targeting Thioredoxin Reductase-1 in Human Prostate Cancer Cells. Med Sci Monit. 2021;27:e930083. Epub 20210614. [CrossRef]
- Lim CB, Fu PY, Ky N, Zhu HS, Feng X, Li J, et al. NF-κB p65 repression by the sesquiterpene lactone, Helenalin, contributes to the induction of autophagy cell death. BMC Complement Altern Med. 2012;12:93. Epub 20120711. [CrossRef]
- Berges C, Fuchs D, Opelz G, Daniel V, Naujokat C. Helenalin suppresses essential immune functions of activated CD4+ T cells by multiple mechanisms. Mol Immunol. 2009;46(15):2892-901. Epub 20090805. [CrossRef]
- Šadibolová M, Juvonen RO, Auriola S, Boušová I. In vitro metabolism of helenalin and its inhibitory effect on human cytochrome P450 activity. Arch Toxicol. 2022;96(3):793-808. Epub 20220106. [CrossRef]
- Poetker DM, Reh DD. A comprehensive review of the adverse effects of systemic corticosteroids. Otolaryngol Clin North Am. 2010;43(4):753-68. [CrossRef]
- Mah F, Milner M, Yiu S, Donnenfeld E, Conway TM, Hollander DA. PERSIST: Physician's Evaluation of Restasis(®) Satisfaction in Second Trial of topical cyclosporine ophthalmic emulsion 0.05% for dry eye: a retrospective review. Clin Ophthalmol. 2012;6:1971-6. Epub 20121128. [CrossRef]
- Gehlsen U, Siebelmann S, Steven P. Tolerance and Adherence to Cationic 0.1% Cyclosporine in Ocular Graft-versus-Host Disease. Ophthalmic Res. 2021;64(1):77-84. Epub 20200529. [CrossRef]
- Ng D, Altamirano-Vallejo JC, Gonzalez-De la Rosa A, Navarro-Partida J, Valdez-Garcia JE, Acosta-Gonzalez R, et al. An Oral Polyphenol Formulation to Modulate the Ocular Surface Inflammatory Process and to Improve the Symptomatology Associated with Dry Eye Disease. Nutrients. 2022;14(15). Epub 20220807. [CrossRef]
- Deng R, Hua X, Li J, Chi W, Zhang Z, Lu F, et al. Oxidative stress markers induced by hyperosmolarity in primary human corneal epithelial cells. PLoS One. 2015;10(5):e0126561. Epub 20150529. [CrossRef]
- Deng R, Su Z, Hua X, Zhang Z, Li DQ, Pflugfelder SC. Osmoprotectants suppress the production and activity of matrix metalloproteinases induced by hyperosmolarity in primary human corneal epithelial cells. Mol Vis. 2014;20:1243-52.
- Spiegle L. Approaches and Methods for Treating Dry Eye: 2021 2021. Available from: https://www.reviewofophthalmology.com/article/approaches-and-methods-for-treating-dry-eye-2021.
- Hessen M, Akpek EK. Dry eye: an inflammatory ocular disease. J Ophthalmic Vis Res. 2014;9(2):240-50.
- Pflugfelder SC, de Paiva CS. The Pathophysiology of Dry Eye Disease: What We Know and Future Directions for Research. Ophthalmology. 2017;124(11S):S4-S13. [CrossRef]
- Schultz C. Safety and efficacy of cyclosporine in the treatment of chronic dry eye. Ophthalmol Eye Dis. 2014;6:37-42. Epub 20140624. [CrossRef]
- Straub M, Bron AM, Muselier-Mathieu A, Creuzot-Garcher C. Long-term outcome after topical ciclosporin in severe dry eye disease with a 10-year follow-up. Br J Ophthalmol. 2016;100(11):1547-50. Epub 20160128. [CrossRef]
- Uchino M, Yokoi N, Shimazaki J, Hori Y, Tsubota K, On Behalf Of The Japan Dry Eye Society. Adherence to Eye Drops Usage in Dry Eye Patients and Reasons for Non-Compliance: A Web-Based Survey. J Clin Med. 2022;11(2). Epub 20220112. [CrossRef]
- Huang R, Su C, Fang L, Lu J, Chen J, Ding Y. Dry eye syndrome: comprehensive etiologies and recent clinical trials. Int Ophthalmol. 2022;42(10):3253-72. Epub 20220609. [CrossRef]
- Farmacopea de los Estados Unidos Mexicanos, (2020).
- Farmacopea Herbolaria de los Estados Unidos Mexicanos, (2021).
- Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15(3):539-74. Epub 20170720. [CrossRef]
- Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118(5):615-21. [CrossRef]
- NORMA Oficial Mexicana NOM-220-SSA1-2016, Instalación y operación de la farmacovigilancia., (2017).
- Akpek EK, Amescua G, Farid M, Garcia-Ferrer FJ, Lin A, Rhee MK, et al. Dry Eye Syndrome Preferred Practice Pattern®. Ophthalmology. 2019;126(1):P286-P334. Epub 20181023. [CrossRef]
- Boccardo L. Self-reported symptoms of mask-associated dry eye: A survey study of 3,605 people. Cont Lens Anterior Eye. 2022;45(2):101408. Epub 20210120. [CrossRef]
- Ruby D. 61 Screen Time Statistics For 2023 2023.
- Mukamal R. Why Is Dry Eye So Difficult to Treat? 2021. Available from: https://www.aao.org/eye-health/tips-prevention/fix-dry-eye-treatment-eyedrops.
- Kamøy B, Magno M, Nøland ST, Moe MC, Petrovski G, Vehof J, et al. Video display terminal use and dry eye: preventive measures and future perspectives. Acta Ophthalmol. 2022;100(7):723-39. Epub 20220204. [CrossRef]
- Singh S, McGuinness MB, Anderson AJ, Downie LE. Interventions for the Management of Computer Vision Syndrome: A Systematic Review and Meta-analysis. Ophthalmology. 2022;129(10):1192-215. Epub 20220518. [CrossRef]
- Čejková J, Čejka Č. The role of oxidative stress in corneal diseases and injuries. Histol Histopathol. 2015;30(8):893-900. Epub 20150324. [CrossRef]
- de Paiva CS, St Leger AJ, Caspi RR. Mucosal immunology of the ocular surface. Mucosal Immunol. 2022;15(6):1143-57. Epub 20220824. [CrossRef]
- Luo L, Li DQ, Doshi A, Farley W, Corrales RM, Pflugfelder SC. Experimental dry eye stimulates production of inflammatory cytokines and MMP-9 and activates MAPK signaling pathways on the ocular surface. Invest Ophthalmol Vis Sci. 2004;45(12):4293-301. [CrossRef]
- Lan W, Petznick A, Heryati S, Rifada M, Tong L. Nuclear Factor-κB: central regulator in ocular surface inflammation and diseases. Ocul Surf. 2012;10(3):137-48. Epub 20120430. [CrossRef]
- Hong SC, Yu HS, Kim JW, Lee EH, Pan CH, Hong KW, et al. Protective effect of Tisochrysis lutea on dry eye syndrome via NF-κB inhibition. Sci Rep. 2022;12(1):19576. Epub 20221115. [CrossRef]
- Yu H, Lin L, Zhang Z, Zhang H, Hu H. Targeting NF-κB pathway for the therapy of diseases: mechanism and clinical study. Signal Transduct Target Ther. 2020;5(1):209. Epub 20200921. [CrossRef]
- Ouyang W, Wang S, Hu J, Liu Z. Can the cGAS-STING Pathway Play a Role in the Dry Eye? Front Immunol. 2022;13:929230. Epub 20220624. [CrossRef]
- Alam J, de Paiva CS, Pflugfelder SC. Immune - Goblet cell interaction in the conjunctiva. Ocul Surf. 2020;18(2):326-34. Epub 20200114. [CrossRef]
- Portal C, Gouyer V, Gottrand F, Desseyn JL. Ocular mucins in dry eye disease. Exp Eye Res. 2019;186:107724. Epub 20190717. [CrossRef]
- Shoari A, Kanavi MR, Rasaee MJ. Inhibition of matrix metalloproteinase-9 for the treatment of dry eye syndrome; a review study. Exp Eye Res. 2021;205:108523. Epub 20210301. [CrossRef]
- Kumar P, Bhargava R, Kumar M, Ranjan S, Verma P. The correlation of routine tear function tests and conjunctival impression cytology in dry eye syndrome. Korean J Ophthalmol. 2014;28(2):122-9. Epub 20140314. [CrossRef]
- Valencia Castillo SL, Martín ES, García Frade LJ, García-Miguel FJ. Autologous serum eye drops improve tear production, both lachrymal flow and stability tests and conjunctival impression cytology with transfer in dry eye disease. Blood Transfus. 2021;19(1):45-53. Epub 20200610. [CrossRef]
- Ali TK, Gibbons A, Cartes C, Zarei-Ghanavati S, Gomaa M, Gonzalez I, et al. Use of Autologous Serum Tears for the Treatment of Ocular Surface Disease From Patients With Systemic Autoimmune Diseases. Am J Ophthalmol. 2018;189:65-70. Epub 20180219. [CrossRef]
- Buzzonetti L, Petroni S, Federici M. Effectiveness of hyaluronic acid and arnica extract ophthalmic solution in reducing dry eye symptoms in pediatric population. Eur J Ophthalmol. 2022;33(2):11206721221128670. Epub 20221002. [CrossRef]
- Hynnekleiv L, Magno M, Vernhardsdottir RR, Moschowits E, Tønseth KA, Dartt DA, et al. Hyaluronic acid in the treatment of dry eye disease. Acta Ophthalmol. 2022;100(8):844-60. Epub 20220505. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).