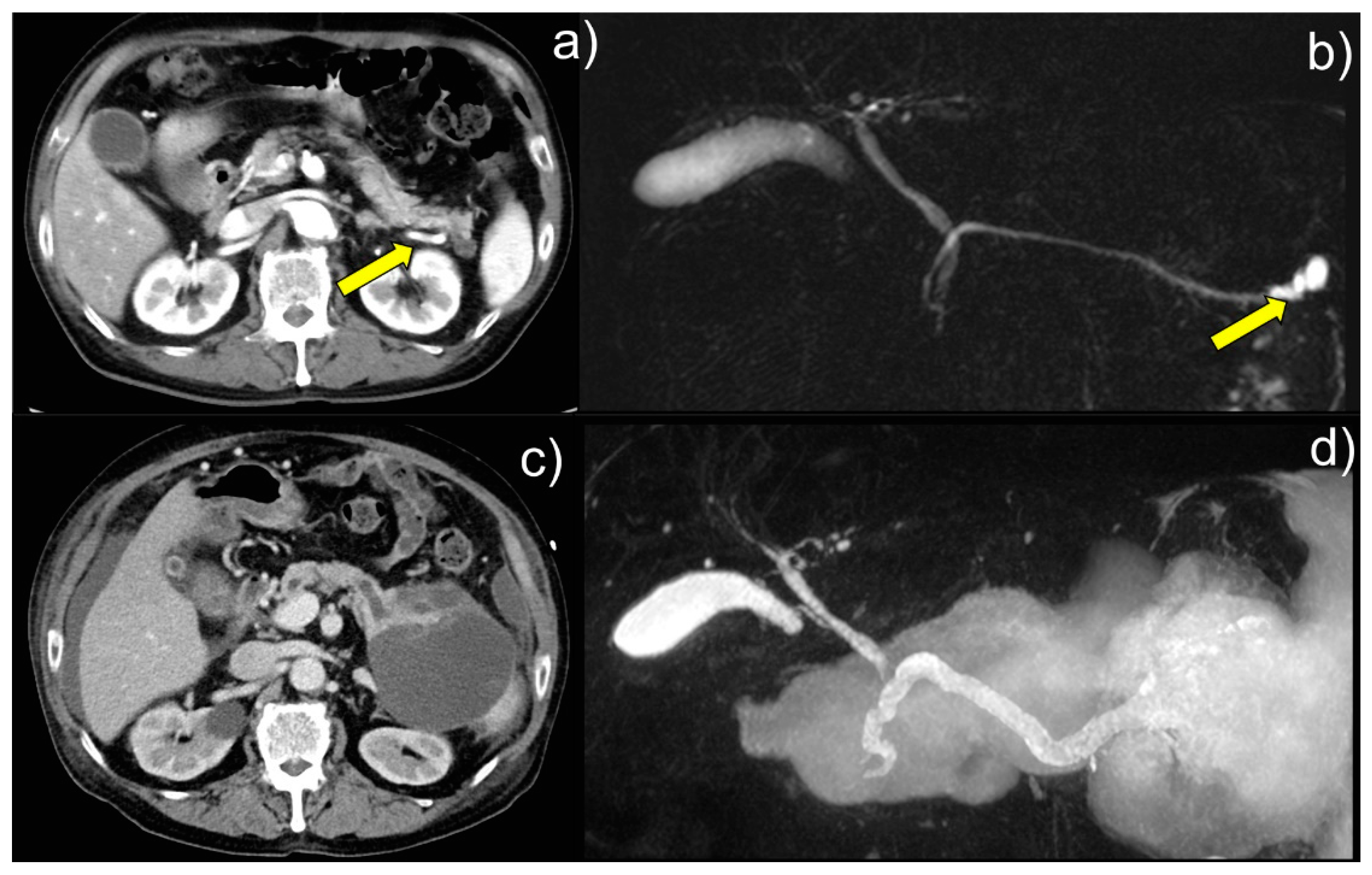
A 62-year-old Japanese man was admitted to our hospital with respiratory distress. Enhanced computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP) showed that the patient had a branch duct-type IPMN 22 mm in size. (a) At the patient’s initial presentation to hospital, CT image showed a cystic lesion in the pancreatic tail (arrow). (b) MRCP image showed a 22-mm cystic lesion in the pancreatic tail (arrow). The mass increased in size over approximately three months but was neglected. Nine years later, during hemodialysis at the Department of Nephrology, Shimada General Medical Center, for respiratory failure caused by acute renal failure, the now 71-year-old patient was found to have a pancreatic cystic mass on a CT scan and was referred to the Department of Gastroenterology for further examination and treatment. Laboratory examination showed serum levels of the tumor markers CEA of 6.4 ng/mL (standard value, ≤5.0) and CA19-9 of 56.6 U/mL (standard value, ≤37.0). MRCP showed that the main pancreatic duct of the patient was dilated to 8 mm in diameter, with a large ruptured pancreatic cyst of over 120 mm in diameter being suspected, and enhanced CT showed possible intraperitoneal penetration. (c) CT image showed suspected intraperitoneal penetration, and (d) MRCP image showed dilation of the patient’s main pancreatic duct to 8 mm in diameter. A large, ruptured pancreatic cyst (≧120 mm in diameter) was also suspected. Although no high-risk stigmata were noted, the cyst diameter increased to ≥30 mm. The contrast-enhanced cyst wall and main pancreatic duct ranging from 5 to 9 mm in diameter indicated a cause for concern [
1]. Therefore, we performed endoscopic nasopancreatic drainage (ENPD) and serial pancreatic juice aspiration cytological examinations (SPACE).
Figure 1.
Intraductal papillary mucinous neoplasms (IPMNs) represent approximately 1% of all pancreatic neoplasms and are cystic pancreatic lesions with mild to severe atypia. They are divided into main-duct IPMN, branch-duct IPMN, and mixed-type IPMN [
1,
2,
3]. Understanding the characteristic cellular findings from cytological examination and referring to appropriate cytological diagnosis and histological subtypes is desirable [
2,
3]. Intestinal-type IPMNs comprise approximately 40 % of IPMNs [
4]. Colloid carcinoma (CC) of the pancreas is a rare subtype of pancreatic cancer, only 1-3% of the malignant tumors of the exocrine pancreas [
5]. Pancreatic CC may arise in an intestinal-type IPMN or mucinous cystic neoplasm [
5]. Cytologically, some malignant floating cells within the mucin of the CC show signet-ring cell features [
5].
Figure 1.
Intraductal papillary mucinous neoplasms (IPMNs) represent approximately 1% of all pancreatic neoplasms and are cystic pancreatic lesions with mild to severe atypia. They are divided into main-duct IPMN, branch-duct IPMN, and mixed-type IPMN [
1,
2,
3]. Understanding the characteristic cellular findings from cytological examination and referring to appropriate cytological diagnosis and histological subtypes is desirable [
2,
3]. Intestinal-type IPMNs comprise approximately 40 % of IPMNs [
4]. Colloid carcinoma (CC) of the pancreas is a rare subtype of pancreatic cancer, only 1-3% of the malignant tumors of the exocrine pancreas [
5]. Pancreatic CC may arise in an intestinal-type IPMN or mucinous cystic neoplasm [
5]. Cytologically, some malignant floating cells within the mucin of the CC show signet-ring cell features [
5].
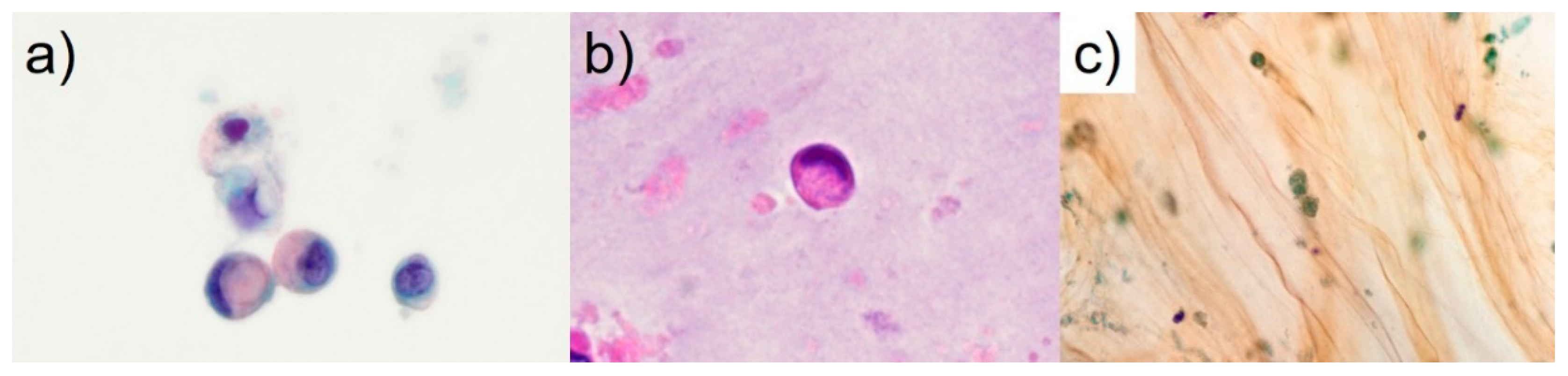
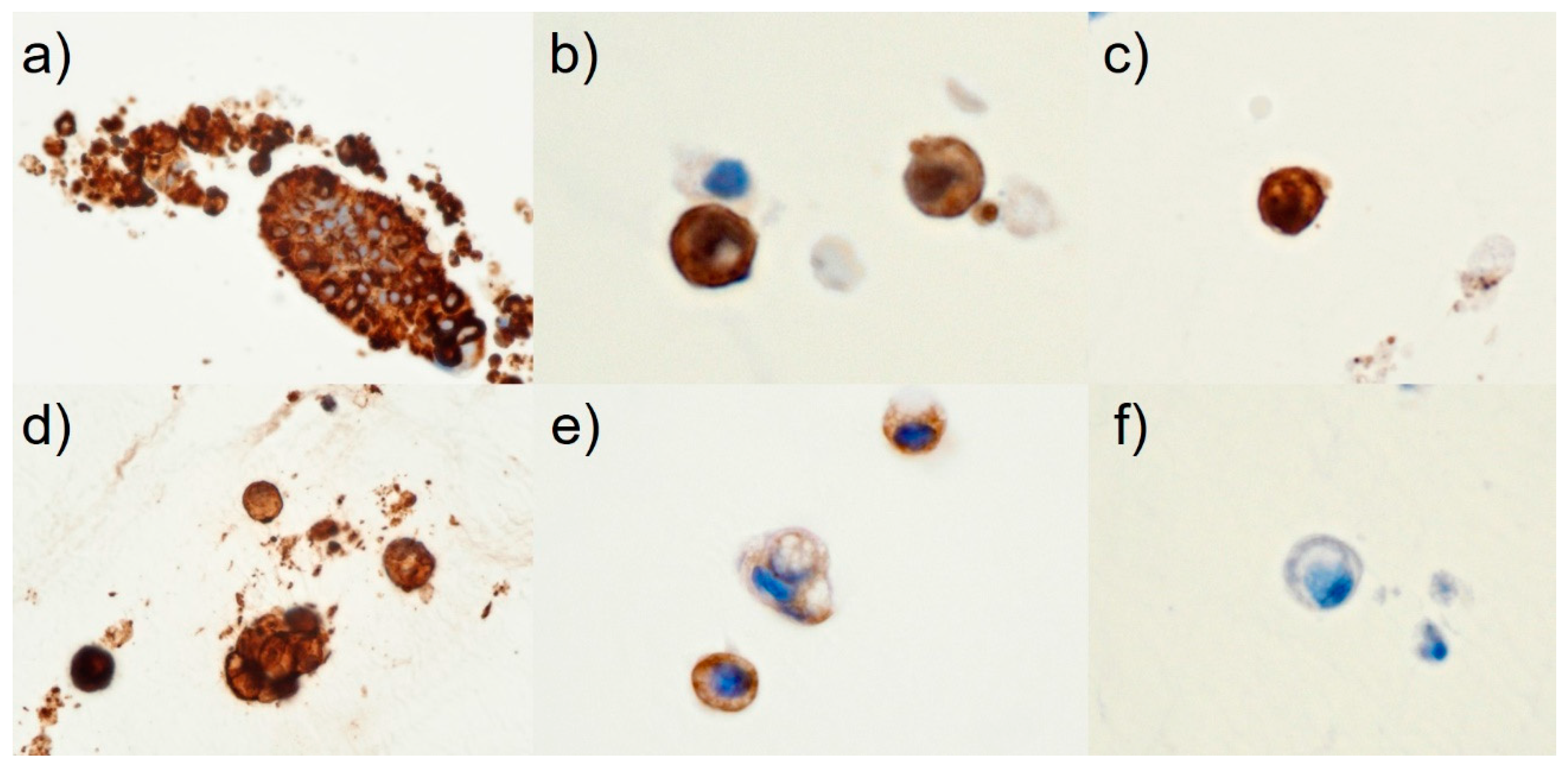
The final cytological diagnosis was CC arising in an intestinal-type IPMNHGD with intraperitoneal penetration. Thus, the patient was ruled ineligible for surgery, and attempts were made to reduce the size of the pancreatic cyst with ENPD. However, the contents of the ENPD tube were highly dense, and drainage was difficult. The patient’s abdominal pain and distension worsened, and respiratory distress developed. The surgeon suggested that the tumor cells derived from the pancreas penetrated the gastrointestinal tract. Open surgery was performed, during which a large amount of mucus accumulated in the abdominal cavity, and a small portion of the omentum was resected. The pathological diagnosis showed that the omental lesions were peritoneal dissemination of CC of pancreatic origin. Unfortunately, the patient died two months postoperatively. Recently, there have been several case reports, mainly from Japan, in which the diagnosis of malignancy was confirmed by SPACE since Iiboshi
et al. first reported its usefulness in preoperative diagnosis [
4]. In pancreatic cancer, mucin-positive signet-ring cells, such as in the current case (
Figure 2), appear to be associated with decreased cell adhesion [
6]. The World Health Organization (WHO) reporting system for pancreaticobiliary cytopathology published in 2022 shows that IPMNHGD is characterized by small cells (similar in size to a 12 μm duodenal enterocyte) [
3]. The present patient had signet-ring cells of 10 to 13 μm in size (
Figure 2). In CC, tumor cells range from bland to signet ring cells [
3,
5]. In our opinion, in pancreatic cytological diagnosis, it is possible to narrow the presumptive lesions to “CC,” “IPMN-derived invasive carcinoma,” “primary signet-ring cell carcinoma,” “anaplastic undifferentiated carcinoma (anaplastic carcinoma),” “neuroendocrine tumor with clear cell features,” and “the clear cell variant of the solid pseudopapillary neoplasm” by focusing on the appearance of the signet-ring cells or signet-ring cell-like cells [
3,
5,
6,
7,
8,
9]. Generally speaking, however, in low-grade IPMNs, discohesive tissue fragments of irregularly arranged columnar cells with low nuclear/cytoplasm ratios are present [
3]. When intestinal-type IPMNs become invasive, they often take the form of CC, as in the present case [
2,
3]. Only two cases of mucin-negative gastric cancer with signet-ring cell-like cells have been reported [
10,
11]. However, to our knowledge, the present case is the first report of mucin-positive signet-ring cells in intestinal-type IPMNHGD evaluated by SPACE cytology. For cytological diagnosis of IPMNHGD, it is essential to observe stacked cell clusters and isolated scattering of atypical cells. Immunohistochemically or immunocytochemically, immunohistochemical staining for maspin and S100P is essential for diagnosing pancreatic adenocarcinoma [
2,
3,
12]. Claudin-18 is often positive in ductal neoplasms, not only in invasive ductal carcinoma but also in IPMNs [
13]. In the present case, immunohistochemically, the tumor cells were immunoreactive for maspin, S100P, and claudin-18 (
Figure 3). Therefore, the patient was diagnosed with a CC of the pancreas. Sahin
et al. revealed in a study in Japan using a monoclonal antibody (clone 43-14A) that claudin-18.2 showed a high rate of expression (87 %) and was also expressed in IPMNs [
14]. An ongoing clinical phase Ib/II trial (NCT04581473) or phase II study (NCT03816163) for metastatic pancreatic cancer was reported that used chimeric antigen receptor T cells against claudin-18.2 in patients with advanced pancreatic adenocarcinoma [
15,
16]. Anti-claudin-18.2-specific monoclonal antibody therapy will likely be used in treating patients with pancreatic cancer, including those with IPMNHGD, in the future [
16].
We report a case of signet-ring cells of CC arising in an intestinal-type IPMNHGD correctly diagnosed using SPACE cytology, which, to our knowledge, is the first to be published in the English literature. Signet-ring cells were one of the cytological features in this case. For the cytopathological diagnosis of CC, it is essential to observe stacked cell clusters and isolated scattering of atypical cells, and some floating atypical cells within the mucinous background show signet-ring features. Diagnosis based on Papanicolaou-staining alone is difficult if only a few atypical cells are present. The specimen should be prepared and stained with maspin, S100P, claudin-18, or other stains to determine whether the cells are benign or malignant. In the future, anti-claudin-18.2-specific monoclonal antibody therapy will likely be used to treat patients with CC arising in an IPMNHGD.
Author Contributions
Conceptualization, M.T.; methodology, T.H.; validation, M.T., T.H., H.H., and K.T.; investigation, M.T., and T.H.; resources, Y.T.; data curation, M.M.; writing—original draft preparation, M.T.; writing—review and editing, H.H. and M.M.; supervision, M.M.; project administration, M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki (1975) and approved by the Ethics Committee of Shimada General Medical Center, Shimada, Shizuoka, Japan (ref: R5-4, approval date: 22 August 2023).
Informed Consent Statement
Because the patient died two months postoperatively, written informed consent was obtained from the patient’s daughter.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank Mr. Naoki Ooishi and Mr. Kuniaki Muramatsu for performing immunohistochemical staining; Dr. Hiroto Ishiki on his valuable advice for preparing a poster session at the 64th annual spring meeting of the Japanese Society of Clinical Cytology in Nagoya, Aichi, Japan; and Prof. Tina Tajima for editing our English manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tanaka, M.; Fernández-del Castillo, C.; Kamisawa, T.; Jang, J.Y.; Levy, P.; Ohtsuka, T.; Salvia, R.; Shimizu, Y.; Tada, M.; Wolfgang, C.L. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 2017, 17, 738–753. [Google Scholar] [CrossRef] [PubMed]
- Basturk, O.; Esposito, I.; Fukushima, N.; et al. Pancreatic intraductal papillary mucinous neoplasm. In WHO classification of tumours. Digestive system tumours., 5th ed.; WHO classification of tumours editorial, board., Ed.; IARC Press: Lyon, France, 2019; pp. 310–314. [Google Scholar]
- Pitman, MB.; Centeno, BA.; Rosenbaum, MW. Pancreatic intraductal papillary mucinous neoplasm, high-grade. In WHO Reporting System for Pancreaticobiliary Cytopathology, 1st ed.; IAC-IARC-WHO Joint Editorial, Board., Ed.; IARC Press: Lyon, France, 2022; pp. 85–86. [Google Scholar]
- Yamaguchi, H.; Inoue, T.; Eguchi, T.; Miyasaka, Y.; Ohuchida, K.; Mizumoto, K.; Yamada, T.; Yamaguchi, K.; Tanaka, M.; Tsuneyoshi, M. Fascin overexpression in intraductal papillary mucinous neoplasms (adenomas, borderline neoplasms, and carcinomas) of the pancreas, correlated with increased histological grade. Mod. Pathol. 2007, 20, 552–561. [Google Scholar] [CrossRef] [PubMed]
- Chen C-H. ; Yeh H-Z.; Li H-N. Colloid carcinoma of the pancreas with a series of radiological and pathological studies for diagnosis: A case report. Diagnostics. 2022, 12, 282.
- Iiboshi, T.; Hanada, K.; Fukuda, T.; et al. Value of cytodiagnosis using endoscopic nasopancreatic drainage for early diagnosis of pancreatic cancer: establishing a new method for the early detection of pancreatic carcinoma in situ. Pancreas. 2012, 41, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Nagayama, D.; Naito, Y.; Tsukamoto, T.; et al. Cytopathological findings of an intraductal papillary mucinous neoplasm with the appearance of signet ring cell-like cells [in Japanese with English abstract]. J Jpn Soc Clin Cytol. 2016, 55, 100–106. [Google Scholar] [CrossRef]
- Hussein, SE.; Knader, SN. Primary signet ring cell carcinoma of the pancreas: Cytopathology review of a rare entity. Diagn Cytopathol. 2019, 47, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Hussein, SE.; Khader, SN. Cytopathology of anaplastic carcinoma of the pancreas: Review of a rare entity and description of a variant with signet ring cell features. Diagn Cytopathol. 2019, 47, 956–960. [Google Scholar] [CrossRef] [PubMed]
- Sugihara, A.; Nakasho, K.; Yamada, N.; Nakagomi, N.; Tsujimura, T.; Terada, N.; Tsuji, M. Neuroendocrine differentiation of periodic?acid Schiff and alcian blue?negative signet?ring cell?like cells and tubular adenocarcinoma cells within a gastric cancer. Scand. J. Gastroenterol. 2004, 39, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Morii, S.; Oka, K.; Hakozaki, H.; Nihei, T.; Mori, N. CEA-Producing Mucin-Negative Gastric Signet-Ring Cell Carcinoma With Neuroendocrine Markers. A case report. J. Clin. Gastroenterol. 1999, 29, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Furuhata, A.; Minamiguchi, S.; Shirahase, H.; Kodama, Y.; Adachi, S.; Sakurai, T.; Haga, H. Immunohistochemical Antibody Panel for the Differential Diagnosis of Pancreatic Ductal Carcinoma From Gastrointestinal Contamination and Benign Pancreatic Duct Epithelium in Endoscopic Ultrasound-Guided Fine-Needle Aspiration. Pancreas 2017, 46, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Li W-T. ; Jeng Y-M.; Yang C-Y. Claudin-18 as a marker for identifying the stomach and pancreatobiliary tract as the primary sites of metastatic adenocarcinoma. Am J Surg Pathol. 2020, 44, 1643–1648.
- Sahin, U.; Koslowski, M.; Dhaene, K.; Usener, D.; Brandenburg, G.; Seitz, G.; Huber, C.; Türeci, O. Claudin-18 Splice Variant 2 Is a Pan-Cancer Target Suitable for Therapeutic Antibody Development. Clin. Cancer Res. 2008, 14, 7624–7634. [Google Scholar] [CrossRef] [PubMed]
- Kyuno, D.; Takasawa, A.; Takasawa, K.; Ono, Y.; Aoyama, T.; Magara, K.; Nakamori, Y.; Takemasa, I.; Osanai, M. Claudin-18.2 as a therapeutic target in cancers: cumulative findings from basic research and clinical trials. Tissue Barriers 2022, 10, 1967080. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; O'Reilly, E.M.; Furuse, J.; Kunieda, F.; Jie, F.; Kindler, H.L. Phase II, open-label, randomized study of first-line zolbetuximab plus gemcitabine and nab-paclitaxel (GN) in Claudin 18.2–positive metastatic pancreatic cancer (mPC). J. Clin. Oncol. 2020, 38, TPS4667–TPS4667. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).