1. Introduction
Rotator cuff (RC) tear is a common disorder of the shoulder. Clinical presentation is characterized by pain and impairment of shoulder function that can affect sleeping and daily living activities [
1]. Non-surgical treatment, such as physical therapy and antiflammatory drugs, can be the first-line approach [
2]. When conservative measures fail or when the tendon lesion is immediately too extensive, surgeons generally proceed with an arthroscopic-assisted repair. After surgery, physical therapy is required to facilitate the healing of the repaired tendon, restoring shoulder function, and allowing the return to social activities and work [
3,
4].
Despite the best repair techniques, the risk of failure after arthoscopic repair (recurrence) is well documented [5-8], ranging from 16% to 94% [
9,
10]. RC re-tear generally occurs within 6 months [
5,
11], while for large tears (i.e. > 4 cm), 78% of failures occur within 3 months [
11]. These studies show that the healing of the repaired tendon is a complex process that lasts over time. A laboratory investigation showed that abnormal scapula motion (i.e. scapular dyskinesis) produces overloads in structures of the cuff, altering the biological compostion of the tendon and therefore their mechanical properties [
12]. Postoperative rehabiliation should correct scapular dyskinesis, thus preventing impairment of tendon healing and risk of re-tear [
12]. The re-education of the scapular movement thus becomes a fundamental aspect of the post-surgical recovery [
13].
Currently this type of re-education is carried out by the physiotherapist who, both in the passive and active mobilization phase, pays attention to the scapular movements performed by the patient, trying to correct scapula dyskinesis with tactile feedbacks and verbal instructions. Unfortunately, the administration of clinical evaluation scales does not provide a substantial support during the evaluation of scapula dyskinesis as they often ignore scapular moments (e.g. the Constant-Murley Score or the American Shoulder and Elbow Score): only movements of humerus elevation and rotation of the gleno-humeral joint are analyzed. Quantitative motion analysis might be considered as an alternative option. While effective to quantify scapula dyskinesis longitudinally at specific time-points of the rehabilitation program [
14,
15], its exploitation as real-time biofeedback tool is extremely limited [
16,
17], with none reporting about the application of kinematic biofeedback for recovering after rotator cuff tear surgical repair.
ISEO (INAIL Shoulder and Elbow Outpatient protocol) is one of the most frequently used and documented motion analysis systems for the evaluation of shoulder biomechanics [
18], including the scapulo-humeral coordination (SHC). ISEO can provide real-time visual representation of scapula dyskinesis on a computer screen while the patient performs arm movements, under the supervision of a physical therapist. Its exploitation as assessment tool is well-described [
19], but its use as visual biofeedback device during physical therapy has never been documented.
Therefore, aim of this Randomized Control Trial (RCT) was to test whether a rehabilitation program including sessions with supervised visual biofeedback can improve shoulder function in patients arthroscopically treated for rotator-cuff tear. As primary outcome, we hypothesized that patients completing this newly developed program exhibit statistically and clinically higher scores in the Scapula-Weighted Constant Marley Score (SW-CMS) [
14,
15] both in the short- and medium-term assessments.
2. Materials and Methods
2.1. Instrumentation
ISEO is an ambulatory motion analysis protocol based on inertial and magnetic sensors (Xsens Technologies, NL), intended to collect kinematic data of the shoulder in every-day-life clinical contexts. For the purpose of this study, ISEO provides a quantitative real-time evaluation of humerus rotations (flexion-extension FL-EX, abduction-adduction AB-AD, internal-external rotation IN-EX), and scapula rotations (protraction-retraction PR-RE, medio-lateral rotation ME-LA and posterior-anterior tilting P-A) with respect to the thorax [
20], based on four wireless sensors placed over thorax, scapula, humerus, and forearm (
Figure 1). Rotations can be visualized either over time or relative to each other on a screen visible both to the therapist and the patient. To visualize the scapula-humeral coordination (SHC), a scapula rotation is reported on the Y axis relative to a humerus rotation on the X axis.
The smallest detectable change, agreement with an optoelectronic system and prediction bands for asymptomatic subjects have been documented in the literature [
21,
22].
2.2. Primary outcome
SW-CMS was the primary outcome to evaluate shoulder function [
14,
15]. With SW-CMS the scores of the conventional CMS assigned for humerus elevation in the sagittal and scapular planes are weighted on the “quality” of patient scapula rotations as measured by ISEO. Specifically, when the patient presents an asymptomatic side, the difference between the patient SHC of the symptomatic and asymptomatic side is calculated, and compared to reference bands of (bilateral) asymptomatic subjects [
15,
19]: the more the differential SHC deviates on multiple scapula rotations, the heavier the (negative) weighing factor, the less the points assigned. Following Fialka et al. 2005 [
23] and consistently with the validation reported in [
15], the final SW-CMS is a normalized value relative to the CMS of the asymptomatic side. This increases the sensitivity and specificity of the score and more closely reflects the patient-specific expectation.
2.3. Study design and experimental treatment
The RCT was approved by AUSL della Romagna Ethics Committee (Comitato Etico della Romagna, CEROM, Italy), and it was conducted at the Cervesi Hospital Biomechanics Laboratory (Cattolica, Italy). The study registration number in clinicaltrial.gov is NCT04521504.
Table 1 reports the inclusion-exclusion criteria.
Importantly, all patients were employed at the time of enrollment, were recruited before arthroscopic surgery for rotator-cuff tear by the same surgical staff and presented a contralateral asymptomatic side.
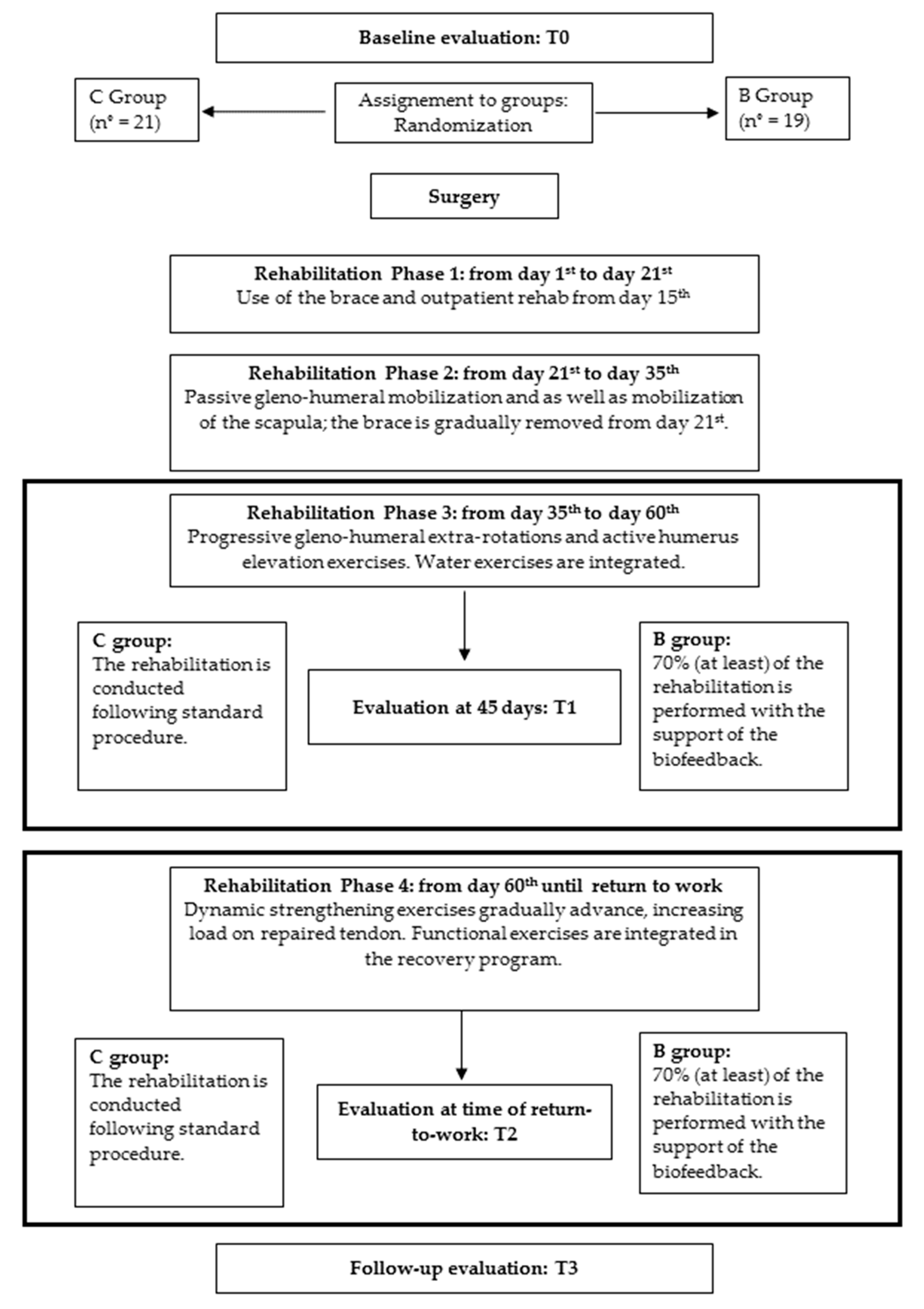
Figure 2 reports the CONSORT diagram with a graphical description of the study.
At the time of enrolment, the orthopaedic surgeon of our equip obtained the informed consent of patients, and, based on a randomization table, they randomly assigned them based to two groups, named C (Controls) and B (Biofeedback). After surgery, group C followed a conventional rehabilitation program, whose details are reported in [
24]. Briefly, the protocol included hydrotherapy and manual therapy, and comprised 4 phases:
Phase 1: from day 1st to day 21st: immobilization in an anti-rotation sling
Phase 2: from day 21st to day 35th : passive gleno-humeral mobilization on scapular plane under 90° is allowed (no rotational movements), as well as mobilization of the scapula
Phase 3: from day 35th to day 60th : patient can starts performing gleno-humeral extra-rotations and active humerus elevation exercises
Phase 4: from day 60th to return-to-work: dynamic strengthening exercises gradually advance, using weights and rubber bands, and increasing load on repaired tendon. Functional exercises are integrated in the recovery program.
Patients of group B followed an experimental rehabilitation program, in which the visual kinematic biofeedback exercises were integrated into the conventional rehabilitation program in phase 3 and 4 (active movements), starting from the session closest the 45th day after surgery. The description of the biofeedback protocol is also reported in [
24]. In summary, the kinematic biofeedback supported the execution of at least the 70% of the non-hydrotherapy rehabilitation.
For both groups, the duration of each session was 30 minutes; for B an extension from 10 to 20 minutes was allowed for the application of the sensors and to train (or remind) patients about the use of the biofeedback tool. The same physical therapy team treated all patients. The number of sessions per subject per week was consistent between both groups.
2.4. Measure of treatment efficacy
To measure the efficacy of the rehabilitation treatments on shoulder function in terms of SW-CMS, all subjects were evaluated in 4 dedicated sessions:
T0: before surgery, as baseline assessment;
T1: 45 days after surgery, i.e. at the beginning of the biofeedback use;
T2: at time of return-to-work, i.e. at the end of the rehabilitation cycle;
T3: at a final follow-up between 6 and 12 months.
For the symptomatic side, during each session the same surgeon completed the conventional CMS [
15]. Then, ISEO was applied on the patient, who was asked to perform 5 consecutive shoulder flexions and abductions in the sagittal and scapular planes, respectively. The central 3 were considered for the computations of the mean SHC pattern. The asymptomatic side was assessed using the same procedure at T0 only. Using this measure as reference, we completed the calculation of SW-CMS for the symptomatic side at each session.
The DASH and ASES score, and EMG analyses of Anterior Deltoid, Posterior Deltoid, Trapezius (superior, middle and inferior fibers), Serratus Anterior and Pectoralis Major completed each assessment. They will not be reported here because they are not necessary to address our primary study outcome.
2.5. Estimation of sample size
Twenty subjects per group were estimated to get greater than 80% power (alpha = 0.05) on the primary outcome (SW-CMS): mean and standard deviation of SW-CMS increments over the course of the conventional rehabilitation protocol were reported in [
15].
2.6. Statistical analysis
Data was analyzed with the MATLAB programming platform (version R2015b).
Statistical differences in SW-CMS between the two groups at baseline (T0) was checked to exclude any initial bias connected to the randomization of subjects in C and B. Similarly, we did not anticipate statistically significant differences at T1 since it is the time of the first biofeedback session. A Mann Whitney test was used.
On the contrary, we hypothesized that patients in B exhibit statistically and clinically higher scores in SW-CMS compared to patients in C in the short and medium term, i.e. at T2 and T3. To test this hypothesis, we completed the following analyses on SW-CMS separately for T2 and T3:
- 1)
statistical differences between the median values of C (SW-CMSmC) and B (SW-CMSmB) were investigated with the Mann Whitney test;
- 2)
to test the clinical effect at group level, the difference of the medians (∆SW-CMS
m) was compared to the correspondent Minimal Clinically Important Difference (MCID = 10 points) [
25].
3. Results
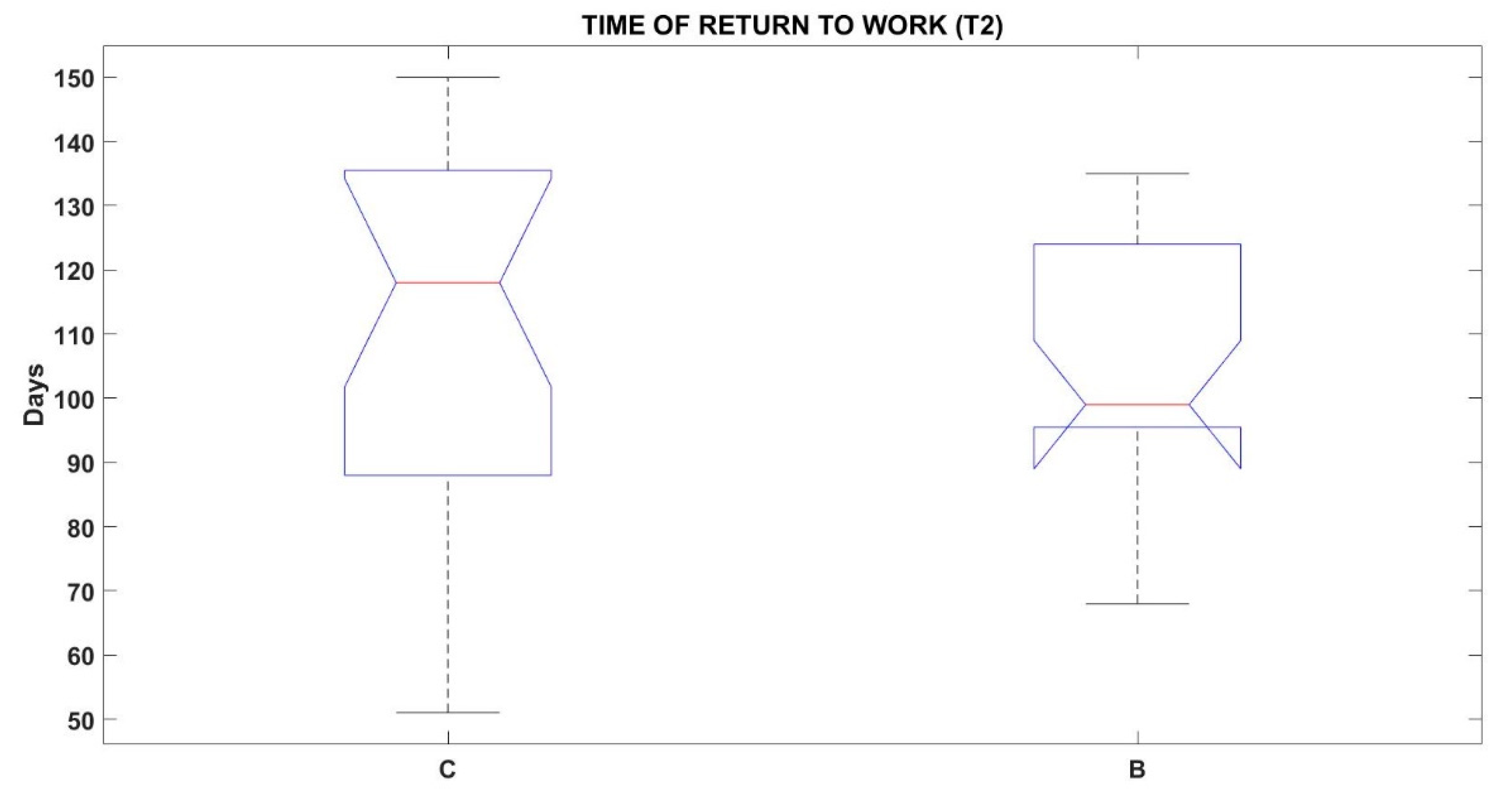
Forty-six patients (36-63 year-old) were recruited for this study after signing the informed consent. Six patients withdrew from the study: 2 patients because of time mobility constraints to participate in the follow-up visits; 1 patient because of a heart failure unrelated to the shoulder rehabilitation; 1 patient because of the emerging addition scapula issues which required further interventions; 2 patients because of they decided to not proceed with the surgery. Therefore, 40 patients completed all assessments and were considered for analyses (21 for C (age 54±5) and 19 for B (age 52÷6)). Median and quartiles of the distribution of Times of return-to-work are shown in
Figure 3: no statistically significant differences emerged between C and B (p=0.6930).
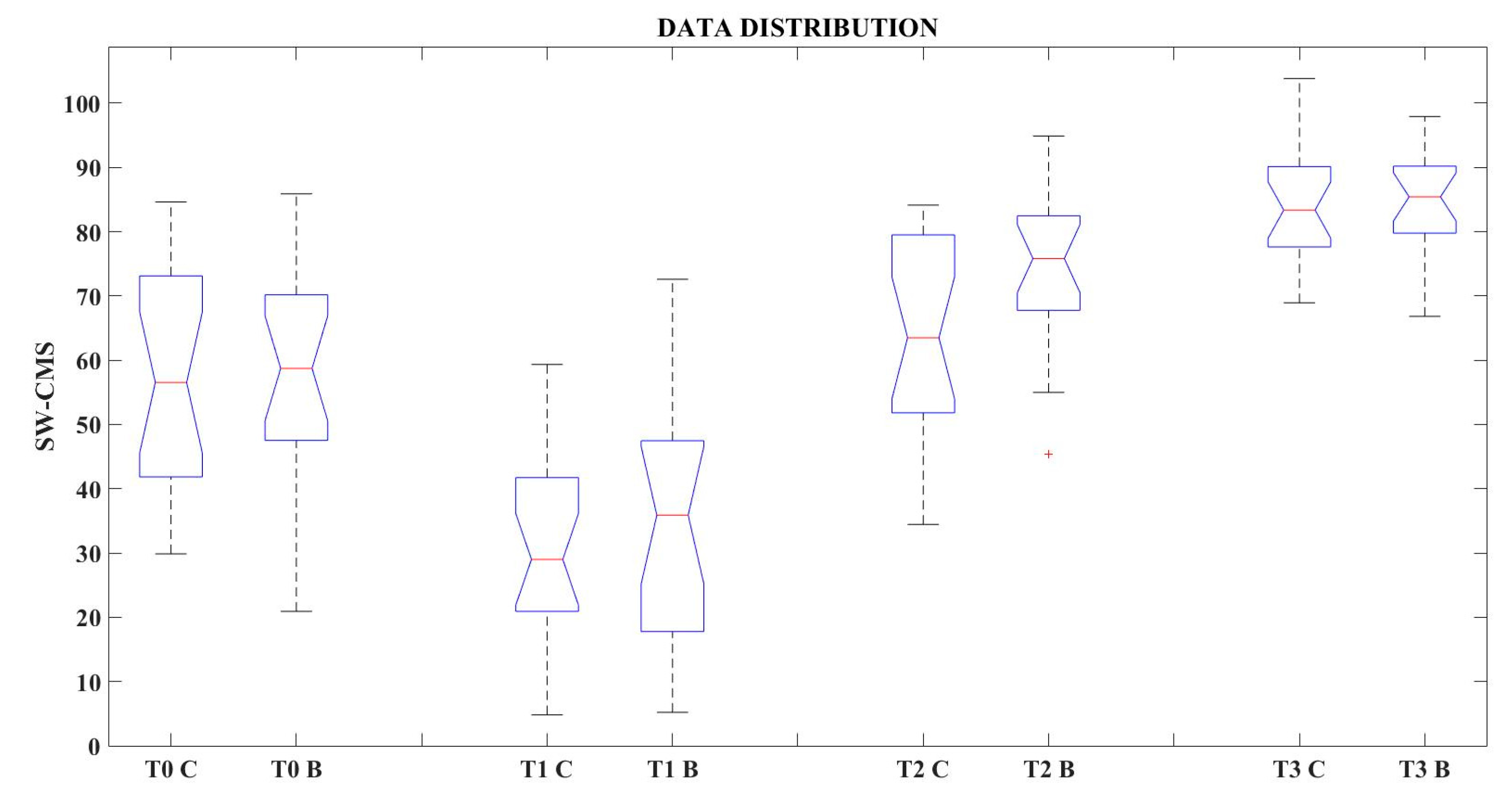
Results for SW-CMS are summarized in
Table 2 and
Figure 4. When comparing the SW-CMS median values of C and B, statistically significant differences were found only at T2 (Time of return-to-work). At T2, ∆SW-CMS
m was also greater than MCID: the C median (63.5) is 12.3 points lower than the B median (75.8). For the other sessions, no clinical differences were found.
4. Discussion and conclusions
This study was developed with the purpose of testing if the combination of a rehabilitative protocol with a kinematic biofeedback tool could improve the functional level of patients after arthroscopic rotator cuff repair. Patients were randomly assigned to two groups (C - Control group and B - Biofeedback group), and compared based on the Scapula-Weighted Constant-Murley Score (SW-CMS).
Results show no significant differences between groups in SW-CMS at T0 and T1, confirming that there were no biases due to the randomization process and that patients started from a comparable functional level post-operatively (i.e. at the start of use of the biofeedback system for group B).
Results for SW-CMS showed that at T2 there were significantly higher scores for B compared to C from a statistical standpoint. To provide a sense of the amplitude of the difference, it should be noticed that this is over the MCID, i.e. clinically relevant. Since the time to return to work is not statistically different, the higher scores for B cannot be attributed to a prolonged rehabilitation. Therefore, we can conclude that the biofeedback training allows patients to return to work in a better functional condition.
Results from the follow-up visit showed that the functional level of patients in B and C continued to improve after the end of the rehabilitation phase, but no statistically significant differences could be detected between the two groups. This seems to indicate that patients were functionally ready to return to a more active lifestyle and that this condition had a beneficial effect on function. This conclusion is consistent with previous observations reported in [
15] on a separate set of 32 patients arthroscopically treated for rotator-cuff tear. In that group, the SW-CMS mean score increased from 90 days to follow-up (6 months to 1 year) from 57.5 to 77.7. In this study, the increment between T2 and T3 in the median value was from 75.8 to 85.4 and the mean value was from 74.3 to 84.5.
In general, the ISEO protocol was easy to master for physical therapists and patients, but therapists pointed out that the stability of the software is crucial for smooth application in clinical settings. Further analysis will be focused on analyzing the effect on muscle activation and correlation between functional outcomes, activity and quality of life.
To our knowledge, there is currently no available literature reporting the application of a rehabilitation protocol with a kinematic visual biofeedback tool, for the recovery of patients arthroscopically treated for rotator cuff tear.
A limitation of the study is due to the outbreak of the Covid-19 pandemic, that precluded the possibility to recruit additional patients and schedule further follow-up visits. Therefore, the effect of the biofeedback therapy beyond 6 months to 1 year is unknown.
Furthermore, the factors leading to an improvement in shoulder function after the return-to-work are still be clarified. A specific study to monitor the shoulder activity of patients after the conclusion of the rehabilitation treatment during their daily life would be highly recommendable.
Author Contributions
Conceptualization, I.P., A.P., V.C., M.V.F, G.M., and A.G.C.; methodology, I.P. and A.G.C.; software, I.P.; validation, I.P. and A.G.C.; formal analysis, I.P, A.G.C., V.C, A.P..; investigation, I.P., M.V.F., A.P. and A.G.C.; resources, P.P. and S.S; data curation, I.P., V.C and A.P.; writing—original draft preparation, I.P., A.G.C.; writing—review and editing, M.V.F, G.M., A.P., P.P. and S.S.; visualization, I.P., A.G.C.; supervision, S.S. and P.P.; project administration, I.P., M.V.F, G.M., S.S. and P.P.; funding acquisition, S.S., P.P. and A.G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Institute for Insurance against Accidents at Work (INAIL), not-for-profit government organization.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the AUSL della Romagna Ethics Committee (Comitato Etico della Romagna, CEROM, Italy), protocol code CPAR01_ISEO of the 12/22/2016.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data are not publicly available due to privacy issues.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kobayashi M; Itoi E; Minagawa H; Yamamoto N; Tuoheti Y; Saito H; Seki N; Aizawa T; Abe H. Prevalence of the shoulder pain in the middle-aged and the elderly and their choices for the treatment. Katakansetsu 2004, 29, 179.
- Brindisino, F.; Salomon, M.; Giagio, S.; Pastore, C.; Innocenti, T. Rotator cuff repair vs. nonoperative treatment: a systematic review with meta-analysis. J. Shoulder Elb. Surg. 2021, 30, 2648–2659. [Google Scholar] [CrossRef] [PubMed]
- Thomson, S.; Jukes, C.; Lewis, J. Rehabilitation following surgical repair of the rotator cuff: a systematic review. Physiotherapy 2015, 102, 20–28. [Google Scholar] [CrossRef]
- Matlak, S.; Andrews, A.B.; Looney, A.; Tepper, K.B. Postoperative Rehabilitation of Rotator Cuff Repair: A Systematic Review. Sports Med. Arthrosc. Rev. 2021, 29, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.S.; Downie, B.K.; Kohen, R.B.; Kijek, T.; Lesniak, B.; Jacobson, J.A.; Hughes, R.E.; Carpenter, J.E. When Do Rotator Cuff Repairs Fail? Serial Ultrasound Examination After Arthroscopic Repair of Large and Massive Rotator Cuff Tears. Am. J. Sports Med. 2011, 39, 2064–2070. [Google Scholar] [CrossRef] [PubMed]
- Nho, S.J.; Brown, B.S.; Lyman, S.; Adler, R.S.; Altchek, D.W.; MacGillivray, J.D. Prospective analysis of arthroscopic rotator cuff repair: Prognostic factors affecting clinical and ultrasound outcome. J. Shoulder Elb. Surg. 2009, 18, 13–20. [Google Scholar] [CrossRef]
- Chona DV; Lakomkin N; Lott A; Workman AD; Henry AC; Kuntz AF; Huffman GR; Glaser DL. The timing of retears after arthroscopic rotator cuff repair. JSES 2017, 26(11), 2054–2059.
- Denard, P.J.; Burkhart, S.S. Arthroscopic Revision Rotator Cuff Repair. J. Am. Acad. Orthop. Surg. 2011, 19, 657–666. [Google Scholar] [CrossRef]
- Cole BJ; McCarty LP III; Kang RW; Alford W; Lewis PB; Hayden JK. Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. JSES 2007, 16, 579–85.
- Meyer, M.; Klouche, S.; Rousselin, B.; Boru, B.; Bauer, T.; Hardy, P. Does arthroscopic rotator cuff repair actually heal? Anatomic evaluation with magnetic resonance arthrography at minimum 2 years follow-up. J. Shoulder Elb. Surg. 2012, 21, 531–536. [Google Scholar] [CrossRef]
- Iannotti JP; Deutsch A; Green A; Rudicel S; Christensen J; Marraffino S; Christensen J; Marraffino S; Rodeo S. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am 2013, 95, 965–71.
- Reuther KE; Tucker JJ; Thomas SJ; Vafa RP; Liu SS; Gordon JA; Caro AC; Yannascoli SM; Kuntz AF; Soslowsky LJ. Effect of scapular dyskinesis on supraspinatus repair healing in a rat model. JSES 2015, 24(8), 1235–42.
- Teixeira, D.C.; Alves, L.; Gutierres, M. The role of scapular dyskinesis on rotator cuff tears: a narrative review of the current knowledge. EFORT Open Rev. 2021, 6, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Merolla, G.; Parel, I.; Cutti, A.G.; Filippi, M.V.; Paladini, P.; Porcellini, G. Assessment of anatomical and reverse total shoulder arthroplasty with the scapula-weighted Constant-Murley score. Int. Orthop. 2018, 43, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Cutti, A.G.; Parel, I.; Pellegrini, A.; Paladini, P.; Sacchetti, R.; Porcellini, G.; Merolla, G. The Constant score and the assessment of scapula dyskinesis: Proposal and assessment of an integrated outcome measure. J. Electromyogr. Kinesiol. 2015, 29, 81–89. [Google Scholar] [CrossRef]
- Hotta, G.H.; Queiroz, P.O.P.; de Lemos, T.W.; Rossi, D.M.; Scatolin, R.d.O.; de Oliveira, A.S. Immediate effect of scapula-focused exercises performed with kinematic biofeedback on scapular kinematics in individuals with subacromial pain syndrome. Clin. Biomech. 2018, 58, 7–13. [Google Scholar] [CrossRef]
- Antunes, A.; Carnide, F.; Matias, R. Real-time kinematic biofeedback improves scapulothoracic control and performance during scapular-focused exercises: A single-blind randomized controlled laboratory study. Hum. Mov. Sci. 2016, 48, 44–53. [Google Scholar] [CrossRef]
- De Baets, L.; van der Straaten, R.; Matheve, T.; Timmermans, A. Shoulder assessment according to the international classification of functioning by means of inertial sensor technologies: A systematic review. Gait Posture 2017, 57, 278–294. [Google Scholar] [CrossRef]
- Cutti, A.; Parel, I.; Raggi, M.; Petracci, E.; Pellegrini, A.; Accardo, A.; Sacchetti, R.; Porcellini, G. Prediction bands and intervals for the scapulo-humeral coordination based on the Bootstrap and two Gaussian methods. J. Biomech. 2014, 47, 1035–1044. [Google Scholar] [CrossRef]
- Kontaxis, A.; Cutti, A.; Johnson, G.; Veeger, H. A framework for the definition of standardized protocols for measuring upper-extremity kinematics. Clin. Biomech. 2009, 24, 246–253. [Google Scholar] [CrossRef]
- Cutti, A.G.; Giovanardi, A.; Rocchi, L.; Davalli, A.; Sacchetti, R. Ambulatory measurement of shoulder and elbow kinematics through inertial and magnetic sensors. Med Biol. Eng. Comput. 2007, 46, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Parel, I.; Cutti, A.; Fiumana, G.; Porcellini, G.; Verni, G.; Accardo, A. Ambulatory measurement of the scapulohumeral rhythm: Intra- and inter-operator agreement of a protocol based on inertial and magnetic sensors. Gait Posture 2012, 35, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Fialka, C.; Oberleitner, G.; Stampfl, P.; Brannath, W.; Hexel, M.; Vécsei, V. Modification of the Constant–Murley shoulder score—introduction of the individual relative Constant score: Individual shoulder assessment. Injury 2005, 36, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Parel, I.; Candoli, V.; Filippi, M.V.; Padolino, A.; Merolla, G.; Sanniti, S.; Galassi, R.; Paladini, P.; Cutti, A.G. Shoulder Rehabilitation Exercises With Kinematic Biofeedback After Arthroscopic Rotator Cuff Repair: Protocol for a New Integrated Rehabilitation Program. JMIR Res. Protoc. 2023, 12, e35757. [Google Scholar] [CrossRef] [PubMed]
- Kukkonen, J.; Kauko, T.; Vahlberg, T.; Joukainen, A.; Äärimaa, V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J. Shoulder Elb. Surg. 2013, 22, 1650–1655. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).