Submitted:
31 August 2023
Posted:
31 August 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Increased binding to the receptor and enhanced immune escape in Omicron
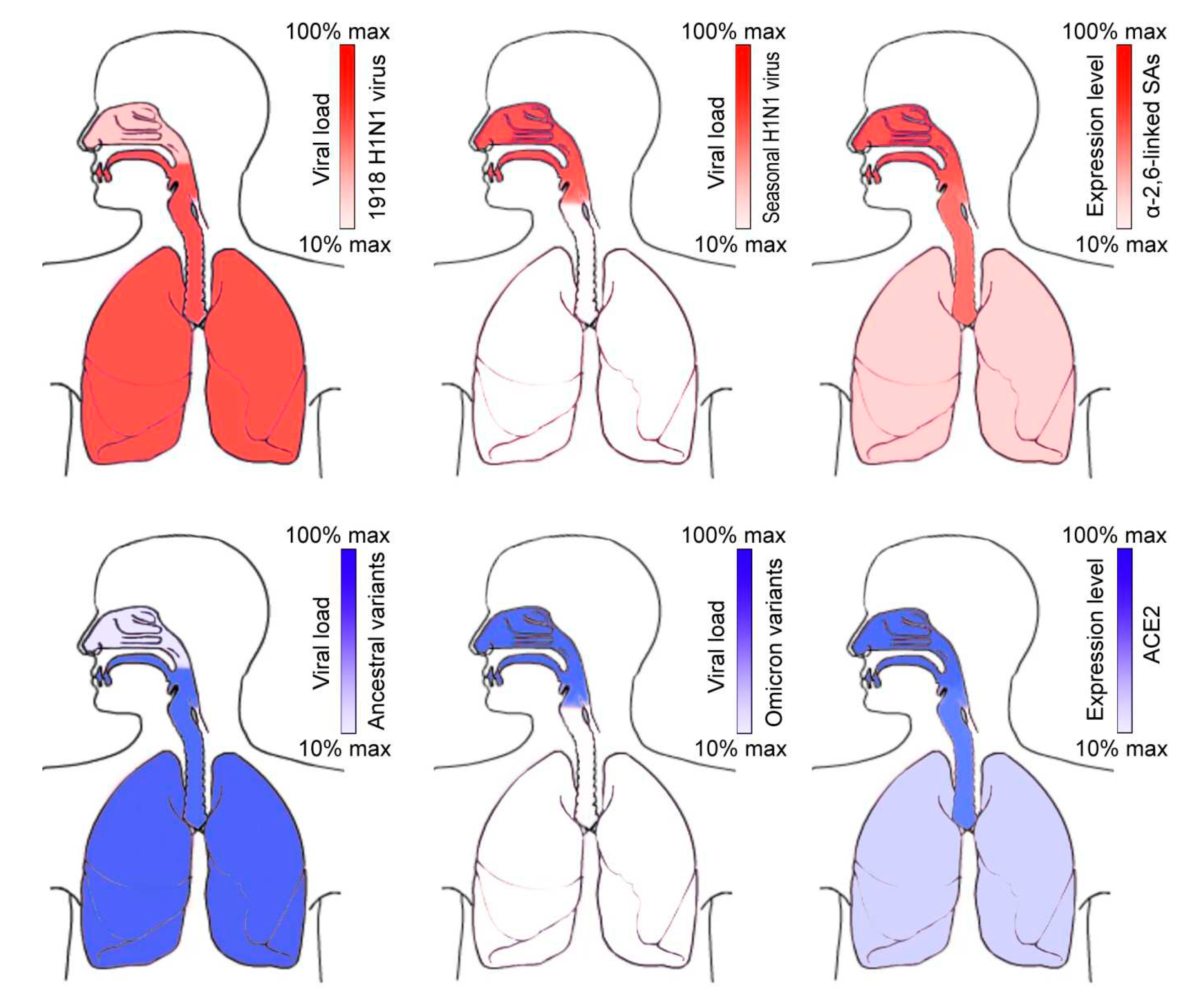
Omicron is more selectively proliferated in the upper respiratory tract (URT)
Similar distribution switch from lungs to URT has been observed for the 1918 H1N1 influenza virus
Future evolutionary direction of SARS-CoV-2
Implications from the URT distribution
Author Contributions
Funding
Conflicts of Interest
References
- Abdoli M, Shafaati M, Ghamsari LK, Abdoli A (2022): Intranasal administration of cold-adapted live-attenuated SARS-CoV-2 candidate vaccine confers protection against SARS-CoV-2. Virus Res. 319, 198857. [CrossRef]
- Arora P, Zhang L, Rocha C, Graichen L, Nehlmeier I, Kempf A, Cossmann A, Ramos GM, Baier E, Tampe B, Moerer O, Dickel S, Winkler MS, Behrens GMN, Pöhlmann S, Hoffmann M (2022): The SARS-CoV-2 Delta-Omicron recombinant lineage (XD) exhibits immune-escape properties similar to the Omicron (BA.1) variant. Int. J. Mol. Sci. 23, 14057. [CrossRef]
- Bansal K, Kumar S (2022): Mutational cascade of SARS-CoV-2 leading to evolution and emergence of omicron variant. Virus Res. 315, 198765. [CrossRef]
- Cameroni E, Bowen JE, Rosen LE, Saliba C, Zepeda SK, Culap K, Pinto D, VanBlargan LA, De Marco A, di Iulio J, Zatta F, Kaiser H, Noack J, Farhat N, Czudnochowski N, Havenar-Daughton C, Sprouse KR, Dillen JR, Powell AE, Chen A, Maher C, Yin L, Sun D, Soriaga L, Bassi J, Silacci-Fregni C, Gustafsson C, Franko NM, Logue J, Iqbal NT, Mazzitelli I, Geffner J, Grifantini R, Chu H, Gori A, Riva A, Giannini O, Ceschi A, Ferrari P, Cippà PE, Franzetti-Pellanda A, Garzoni C, Halfmann PJ, Kawaoka Y, Hebner C, Purcell LA, Piccoli L, Pizzuto MS, Walls AC, Diamond MS, Telenti A, Virgin HW, Lanzavecchia A, Snell G, Veesler D, Corti D (2022): Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shiftNature 602, 664–670. [CrossRef]
- Cao Y, Wang J, Jian F, Xiao T, Song W, Yisimayi A, Huang W, Li Q, Wang P, An R, Wang J, Wang Y, Niu X, Yang S, Liang H, Sun H, Li T, Yu Y, Cui Q, Liu S, Yang X, Du S, Zhang Z, Hao X, Shao F, Jin R, Wang X, Xiao J, Wang Y, Xie XS (2022a): Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature 602, 657–663. [CrossRef]
- Cao Y, Song W, Wang L, Liu P, Yue C, Jian F, Yu Y, Yisimayi A, Wang P, Wang Y, Zhu Q, Deng J, Fu W, Yu L, Zhang N, Wang J, Xiao T, An R, Wang J, Liu L, Yang S, Niu X, Gu Q, Shao F, Hao X, Meng B, Gupta RK, Jin R, Wang Y, Xie XS, Wang X (2022b): Characterization of the enhanced infectivity and antibody evasion of Omicron BA.2.75. Cell Host Microbe 30, 1527–1539.e5. [CrossRef]
- Farrell NF, Klatt-Cromwell C, Schneider JS (2020): Benefits and safety of nasal saline irrigations in a pandemic-washing COVID-19 away. JAMA Otolaryngol. Head Neck Surg. 146, 787–788. [CrossRef]
- Feng F, Wen Z, Chen J, Yuan Y, Wang C, Sun C (2022): Strategies to develop a mucosa-targeting vaccine against emerging infectious diseases. Viruses 14, 520. [CrossRef]
- Granerud BK, Ueland T, Lind A, Søraas A, Fevang B, Steffensen AK, Al-Baldawi H, Lund-Johansen F, Aukrust P, Halvorsen B, Dahl TB, Dudman S, Müller F, Holter JC (2022): Omicron variant generates a higher and more sustained viral load in nasopharynx and saliva than the Delta variant of SARS-CoV-2. Viruses 14, 2420. [CrossRef]
- Herfst, S., Schrauwen, E. J., Linster, M., Chutinimitkul, S., de Wit, E., Munster, V. J., et al. (2012). Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336, 1534–1541. [CrossRef]
- Hikmet F, Méar L, Edvinsson Å, Micke P, Uhlén M, Lindskog C (2020): The protein expression profile of ACE2 in human tissues. Mol. Syst. Biol. 16, e9610. [CrossRef]
- Jester B, Uyeki TM, Jernigan DB, Tumpey TM (2019): Historical and clinical aspects of the 1918 H1N1 pandemic in the United States. Virology 527, 32–37. [CrossRef]
- Joseph U, Su YC, Vijaykrishna D, Smith GJ (2017): The ecology and adaptive evolution of influenza A interspecies transmission. Influenza Other Respir. Viruses 11, 74–84. [CrossRef]
- Kandeel M, Mohamed MEM, Abd El-Lateef HM, Venugopala KN, El-Beltagi HS (2022): Omicron variant genome evolution and phylogenetics. J. Med. Virol. 94, 1627–1632. [CrossRef]
- Kim SM, Kim EH, Casel MAB, Kim YI, Sun R, Kwack MJ, Yoo JS, Yu MA, Yu KM, Jang SG, Rollon R, Choi JH, Gil J, Eun K, Kim H, Ensser A, Hwang J, Song MS, Kim MH, Jung JU, Choi YK (2022): SARS-CoV-2 variants show temperature-dependent enhanced polymerase activity in the upper respiratory tract and high transmissibility. BioRxiv 2022.09.27.50 9689. [CrossRef]
- King D, Mitchell B, Williams CP, Spurling GK (2015): Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database Syst. Rev. 2015, CD006821. [CrossRef]
- Kuchipudi SV, Nelli RK, Gontu A, Satyakumar R, Surendran Nair M, Subbiah M (2021): Sialic acid receptors: the key to solving the enigma of zoonotic virus spillover. Viruses 13, 262. [CrossRef]
- Lam TT, Wang J, Shen Y, Zhou B, Duan L, Cheung CL, Ma C, Lycett SJ, Leung CY, Chen X, Li L, Hong W, Chai Y, Zhou L, Liang H, Ou Z, Liu Y, Farooqui A, Kelvin DJ, Poon LL, Smith DK, Pybus OG, Leung GM, Shu Y, Webster RG, Webby RJ, Peiris JS, Rambaut A, Zhu H, Guan Y (2013): The genesis and source of the H7N9 influenza viruses causing human infections in China. Nature 502, 241–244. [CrossRef]
- Li J, Zheng J, Chen P, Wang B, Zhang Y, Xiong J, You L, Jin Y, Jiang L, Tang F, Wen H, Hong C, Zeng X, Li L, Lu B, Rong B, Wang Z (2023a): Higher SARS-CoV-2 shedding in exhaled aerosol probably contributed to the enhanced transmissibility of Omicron BA.5 subvariant. J. Med. Virol. 95, e28365. [CrossRef]
- Li C, Huang J, Yu Y, Wan Z, Chiu MC, Liu X, Zhang S, Cai JP, Chu H, Li G, Chan JF, To KK, Yang Z, Jiang S, Yuen KY, Clevers H, Zhou J (2023b): Human airway and nasal organoids reveal escalating replicative fitness of SARS-CoV-2 emerging variants. Proc. Natl. Acad. Sci. U.S.A. 120, e2300376120. [CrossRef]
- Mannar D, Saville JW, Zhu X, Srivastava SS, Berezuk AM, Tuttle KS, Marquez AC, Sekirov I, Subramaniam S (2022): SARS-CoV-2 Omicron variant: Antibody evasion and cryo-EM structure of spike protein-ACE2 complex. Science 375, 760–764. [CrossRef]
- Mehle A, Doudna JA (2009): Adaptive strategies of the influenza virus polymerase for replication in humans. Proc. Natl. Acad. Sci. U.S.A. 106, 21312–21316. [CrossRef]
- Migueres M, Dimeglio C, Trémeaux P, Abravanel F, Raymond S, Lhomme S, Mansuy JM, Izopet J (2022): Influence of immune escape and nasopharyngeal virus load on the spread of SARS-CoV-2 Omicron variant. J. Infect. 84, e7–e9. [CrossRef]
- Pascarella S, Ciccozzi M, Bianchi M, Benvenuto D, Cauda R, Cassone A (2022): The value of electrostatic potentials of the spike receptor binding and N-terminal domains in addressing transmissibility and infectivity of SARS-CoV-2 variants of concern. J. Infect. 84, e62–e63. [CrossRef]
- Patrono LV, Vrancken B, Budt M, Düx A, Lequime S, Boral S, Gilbert MTP, Gogarten JF, Hoffmann L, Horst D, Merkel K, Morens D, Prepoint B, Schlotterbeck J, Schuenemann VJ, Suchard MA, Taubenberger JK, Tenkhoff L, Urban C, Widulin N, Winter E, Worobey M, Schnalke T, Wolff T, Lemey P, Calvignac-Spencer S (2022): Archival influenza virus genomes from Europe reveal genomic variability during the 1918 pandemic. Nat. Commun. 13, 2314. [CrossRef]
- Planas D, Saunders N, Maes P, Guivel-Benhassine F, Planchais C, Buchrieser J. Bolland WH, Porrot F, Staropoli I, Lemoine F, Péré H, Veyer D, Puech J, Rodary J, Baele G, Dellicour S, Raymenants J, Gorissen S, Geenen C, Vanmechelen B, Wawina-Bokalanga T, Martí-Carreras J, Cuypers L, Sève A, Hocqueloux L, Prazuck T, Rey FA, Simon-Loriere E, Bruel T, Mouquet H, André E, Schwartz O (2022): Considerable escape of SARS-CoV-2 Omicron to antibody neutralization. Nature 602, 671–675. [CrossRef]
- Resa-Infante P, Jorba N, Coloma R, Ortin J (2011): The influenza virus RNA synthesis machine: advances in its structure and function. RNA Biol. 8, 207–215. [CrossRef]
- Russell CA, Fonville JM, Brown AE, Burke DF, Smith DL, James SL, Herfst S, van Boheemen S, Linster M, Schrauwen EJ, Katzelnick L, Mosterín A, Kuiken T, Maher E, Neumann G, Osterhaus AD, Kawaoka Y, Fouchier RA, Smith DJ (2012): The potential for respiratory droplet–transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 336, 1541–1547. [CrossRef]
- Saifi S, Ravi V, Sharma S, Swaminathan A, Chauhan NS, Pandey R (2022): SARS-CoV-2 VOCs, Mutational diversity and clinical outcome: Are they modulating drug efficacy by altered binding strength? Genomics 114, 110466. [CrossRef]
- Salamanna F, Maglio M, Landini MP, Fini M (2020): Body localization of ACE-2: on the trail of the keyhole of SARS-CoV-2. Front. Med. 7:594495. [CrossRef]
- Salmona M, Chaix ML, Feghoul L, Mahjoub N, Maylin S, Schnepf N, Jacquier H, Walle EM, Helary M, Mellon G, Osinski N, Zebiche W, Achili Y, Amarsy R, Mahé V, Le Goff J, Delaugerre C (2022): Detection of SARS-CoV-2 in saliva and nasopharyngeal swabs according to viral variants. Microbiol. Spectr. 10, e0213322. [CrossRef]
- Salvagno GL, Henry BM, Pighi L, De Nitto S, Montagnana M, Lippi G (2022): SARS-CoV-2 Omicron infection is associated with high nasopharyngeal viral load. J. Infect. 84, 834–872. [CrossRef]
- Scarpa R, Caso F, Costa L, Passavanti S, Vitale MG, Trojaniello C, Del Puente A, Ascierto PA (2020): May the analysis of 1918 influenza pandemic give hints to imagine the possible magnitude of Corona Virus Disease-2019 (COVID-19)? J. Transl. Med. 18, 489. [CrossRef]
- Sentis C, Billaud G, Bal A, Frobert E, Bouscambert M, Destras G, Josset L, Lina B, Morfin F, Gaymard A, The Covid-Diagnosis Hcl Study Group (2022): SARS-CoV-2 Omicron variant, lineage BA.1, is associated with lower viral load in nasopharyngeal samples compared to Delta variant. Viruses 14, 919. [CrossRef]
- Short KR, Kedzierska K, van de Sandt CE (2018): Back to the future: Lessons learned from the 1918 influenza pandemic. Front. Cell. Infect. Microbiol. 8, 343. [CrossRef]
- Stadnytskyi V, Anfinrud P, Bax A (2021): Breathing, speaking, coughing or sneezing: What drives transmission of SARS-CoV-2? J. Intern. Med. 290, 1010–1027. [CrossRef]
- Stauft CB, Sangare K, Wang TT (2023): Differences in new variant of concern replication at physiological temperatures in vitro. J. Infect. Dis. 227, 202–205. [CrossRef]
- Stevens J, Blixt O, Glaser L, Taubenberger JK, Palese P, Paulson JC, Wilson IA (2006): Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J. Mol. Biol. 355, 1143–1155. [CrossRef]
- Suzuki R, Yamasoba D, Kimura I, Wang L, Kishimoto M, Ito J, Morioka Y, Nao N, Nasser H, Uriu K, Kosugi Y, Tsuda M, Orba Y, Sasaki M, Shimizu R, Kawabata R, Yoshimatsu K, Asakura H, Nagashima M, Sadamasu K, Yoshimura K; Genotype to Phenotype Japan (G2P-Japan) Consortium; Sawa H, Ikeda T, Irie T, Matsuno K, Tanaka S, Fukuhara T, Sato K (2022): Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature 603, 700–705. [CrossRef]
- Taubenberger JK, Baltimore D, Doherty PC, Markel H, Morens DM, Webster RG, Wilson IA (2012): Reconstruction of the 1918 influenza virus: unexpected rewards from the past. mBio 3, e00201-12. [CrossRef]
- Taubenberger JK, Kash JC, Morens DM (2019): The 1918 influenza pandemic: 100 years of questions answered and unanswered. Sci. Transl. Med. 11, eaau5485. [CrossRef]
- Tian D, Sun Y, Xu H, Ye Q (2022): The emergence and epidemic characteristics of the highly mutated SARS-CoV-2 Omicron variant. J. Med. Virol. 94, 2376–2383. [CrossRef]
- Tscherne DM, García-Sastre A (2011) Virulence determinants of pandemic influenza viruses. J. Clin. Invest. 121, 6–13. [CrossRef]
- Viana R, Moyo S, Amoako DG, Tegally H, Scheepers C, Althaus CL, Anyaneji UJ, Bester PA, Boni MF, Chand M, Choga WT, Colquhoun R, Davids M, Deforche K, Doolabh D, du Plessis L, Engelbrecht S, Everatt J, Giandhari J, Giovanetti M, Hardie D, Hill V, Hsiao NY, Iranzadeh A, Ismail A, Joseph C, Joseph R, Koopile L, Kosakovsky Pond SL, Kraemer MUG, Kuate-Lere L, Laguda-Akingba O, Lesetedi-Mafoko O, Lessells RJ, Lockman S, Lucaci AG, Maharaj A, Mahlangu B, Maponga T, Mahlakwane K, Makatini Z, Marais G, Maruapula D, Masupu K, Matshaba M, Mayaphi S, Mbhele N, Mbulawa MB, Mendes A, Mlisana K, Mnguni A, Mohale T, Moir M, Moruisi K, Mosepele M, Motsatsi G, Motswaledi MS, Mphoyakgosi T, Msomi N, Mwangi PN, Naidoo Y, Ntuli N, Nyaga M, Olubayo L, Pillay S, Radibe B, Ramphal Y, Ramphal U, San JE, Scott L, Shapiro R, Singh L, Smith-Lawrence P, Stevens W, Strydom A, Subramoney K, Tebeila N, Tshiabuila D, Tsui J, van Wyk S, Weaver S, Wibmer CK, Wilkinson E, Wolter N, Zarebski AE, Zuze B, Goedhals D, Preiser W, Treurnicht F, Venter M, Williamson C, Pybus OG, Bhiman J, Glass A, Martin DP, Rambaut A, Gaseitsiwe S, von Gottberg A, de Oliveira T (2022): Rapid epidemic expansion of the SARS-CoV-2 Omicron variant in southern Africa. Nature 603, 679–686. [CrossRef]
- Viera Braga FKG, Berg M, Carpaij OA, Polanski K, Simon LM, Brouwer S, Gomes T, Hesse L, Jiang J, Fasouli ES, Efremova M, Vento-Tormo R, Talavera-López C, Jonker MR, Affleck K, Palit S, Strzelecka PM, Firth HV, Mahbubani KT, Cvejic A, Meyer KB, Saeb-Parsy K, Luinge M, Brandsma CA, Timens W, Angelidis I, Strunz M, Koppelman GH, van Oosterhout AJ, Schiller HB, Theis FJ, van den Berge M, Nawijn MC, Teichmann SA (2019): A cellular census of human lungs identifies novel cell states in health and in asthma. Nat. Med. 25, 1153–1163. [CrossRef]
- Vlasak J, Ionescu R (2008): Heterogeneity of monoclonal antibodies revealed by charge-sensitive methods. Curr. Pharm. Biotechnol. 9, 468–481. [CrossRef]
- Wang L, Cheng G (2022): Sequence analysis of the emerging SARS-CoV-2 variant Omicron in South Africa. J. Med. Virol. 94, 1728–1733. [CrossRef]
- Watanabe T, Watanabe S, Shinya K, Kim JH, Hatta M, Kawaoka Y (2009): Viral RNA polymerase complex promotes optimal growth of 1918 virus in the lower respiratory tract of ferrets. Proc. Natl. Acad. Sci. U.S.A. 106, 588–592. [CrossRef]
- Xi J, Lei LR, Zouzas W, April Si X (2021): Nasally inhaled therapeutics and vaccination for COVID-19: Developments and challenges. MedComm 2, 569–586. [CrossRef]
- Yao L, Korteweg C, Hsueh W, Gu J (2008): Avian influenza receptor expression in H5N1-infected and noninfected human tissues. FASEB J. 22, 733–740. [CrossRef]
- Yin W, Xu Y, Xu P, Cao X, Wu C, Gu C, He X, Wang X, Huang S, Yuan Q, Wu K, Hu W, Huang Z, Liu J, Wang Z, Jia F, Xia K, Liu P, Wang X, Song B, Zheng J, Jiang H, Cheng X, Jiang Y, Deng SJ, Xu HE (2022): Structures of the Omicron spike trimer with ACE2 and an anti-Omicron antibody. Science 375, 1048–1053. [CrossRef]
- Yuan S (2013): Drugs to cure avian influenza infection--multiple ways to prevent cell death. Cell Death Dis. 4, e835. [CrossRef]
- Yuan S, Jiang SC, Li ZL (2020): Do humidity and temperature impact the spread of the novel coronavirus? Front. Public Health. 8, 240. [CrossRef]
- Yuan S, Jiang SC, Zhang ZW, Fu YF, Hu J, Li ZL (2021a): The role of alveolar edema in COVID-19. Cells 10, 1897. [CrossRef]
- Yuan S, Jiang SC, Zhang ZW, Fu YF, Hu J, Li ZL (2021b): Quantification of cytokine storms during virus infections. Front. Immunol. 12, 659419. [CrossRef]
- Yuan S, Jiang SC, Zhang ZW, Fu YF, Yang XY, Li ZL, Hu J, Du JB, Yuan M, Chen YE (2022a): Surface electrostatic shift on spike protein decreased antibody activities against SARS-CoV-2 Omicron variant. J. Infect. 85, 208–211. [CrossRef]
- Yuan S, Jiang SC, Zhang ZW, Fu YF, Zhu F, Li ZL, Hu J (2022b): Abuse of amantadine in poultry may be associated with higher fatality rate of H5N1 infections in humans. J. Med. Virol. 94, 2588–2597. [CrossRef]
- Yuan L, Zhu H, Zhou M, Ma J, Liu X, Wu K, Ye J, Yu H, Chen P, Chen R, Wang J, Zhang Y, Ge S, Yuan Q, Cheng T, Guan Y, Xia N (2022c): Nasal irrigation efficiently attenuates SARS-CoV-2 Omicron infection, transmission and lung injury in the Syrian hamster model. iScience 25, 105475. [CrossRef]
- Zhang ZW, Liu T, Zeng J, Chen YE, Yuan M, Zhang DW, Zhu F, Yuan S (2015): Prediction of the next highly pathogenic avian influenza pandemic that can cause illness in humans. Infect. Dis. Poverty 4, 50. [CrossRef]
- Zhou Y, Zhi H, Teng Y (2023): The outbreak of SARS-CoV-2 Omicron lineages, immune escape, and vaccine effectivity. J. Med. Virol. 95, e28138. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




