Submitted:
29 August 2023
Posted:
31 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
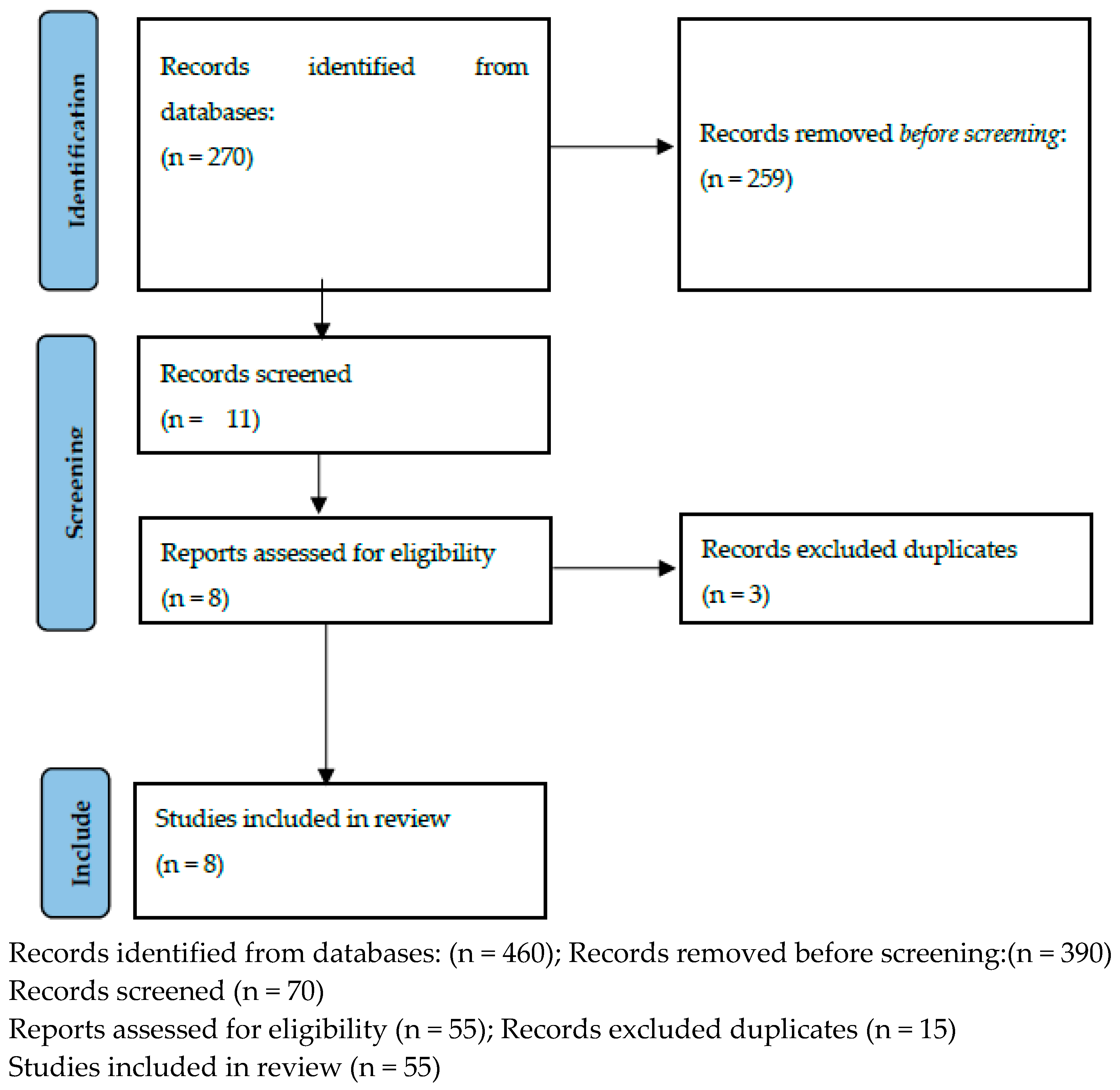
2. Materials and Methods
3. Physiotherapy
3.1. Exercise
3.2. Balneotherapy
3.3. Treatment recommendations for the management of persistent pelvic pain
3.4. Myofascial trigger points, visceral manual therapy
3.5. TENS - Transcutaneous Electrical Nerve Stimulation
3.6. Pelvic Floor Physiotherapy - Pelvic Floor Muscle Physiotherapy
3.7. Physio-EndEA’ Study
| Study | Treatments | Conclusion | Marker assessment (microRNA) |
|---|---|---|---|
| Hansen et al., 2021 [23] | Exercise | Exercise has no positive effect on pain. The authors suggest that randomised trials with properly calculated power, well-defined study groups and training programmes should be conducted. | No |
| Tennford et al., 2021 [24] | Exercise Physical therapy |
Exercise and physical activity have no effect on pain reduction in endometritis patients. The authors also believe that the topic requires a study with a well-designed methodology, using reliable and validated tools. | No |
| Habek et al., 2021 [25] | Balneotherapy | The use of balneotherapy and hyperthermic hydrotherapy in endometriosis is contraindicated. | No |
| Mardon et al., 2022 [26] | Surgical treatment, pharmacotherapy, psychological care, physiotherapy | The most commonly recommended treatment including that for women with endometriosis is surgery, pharmacotherapy, psychological care and physiotherapy. The authors indicate that there is currently no consensus on what should be recommended in clinical practice for persistent pelvic pain. | No |
| Goździewicz et al., 2022 [27] | Myofascial trigger points, visceral manual therapy | The importance of using physiotherapy in the form of working with myofascial trigger points and visceral manual therapy to reduce symptoms of endometriosis disease. The authors note prospective studies in relation to surgical treatment and visceral therapy in patients with endometriosis. | No |
| Mira et al., 2020 [28] | TENS Applied TENS and hormonal therapy for 8 weeks at the S3–S4 region, 30 minutes session. Included a hundred-one participants with DIE in electrotherapy (n=53) (hormonal treatment + electrotherapy) or control group (n=48) (only hormonal treatment) by 8 weeks of follow-up. The primary measurement was chronic pelvic pain (CPP) using a visual analogue scale (VAS) and deep dyspareunia. The secondary outcomes were the quality of life by endometriosis health profile (EHP-30) and sexual function by female sexual function index (FSFI). |
Alleviation of CPP was observed only in the electrotherapy group. In terms of profound dyspareunia, improvement was observed for both groups. Considering the secondary outcomes, a higher post-treatment total score for EHP-30 was observed in both groups.With regard to sexual function, a statistically significant improvement in the FSFI score was observed in the electrotherapy group, with an increase in scores in the domains of lube and pain. | No |
| Del Forno et al., 2021 [29] | Pelvic Floor Muscle Physiotherapy Before the start of therapy, the participants received information on pelvic floor anatomy and function, with the help of anatomical illustrations. In addition, the physiotherapist, experienced in pelvic floor muscle dysfunction, performed a digital evaluation of the pelvic floor muscle tone. This was performed after the TPU, given that digital examination may induce pain with consequent contraction of the pelvic floor, which could affect the LHA assessment. Pubococcygeus and ischiococcygeus muscle tone were assessed bilaterally at rest, and during pelvic floor contraction and relaxation. After the first examination, the women in the study group underwent five individual sessions of PFP, of 30 min each, on weeks 1, 3, 5, 8 and 11. In each session, the women underwent a Thiele massage, which consists of digital pressure and subsequent stretching of the muscles in order to relax them, restoring normal pelvic floor tone and the ability to coordinate muscle behavior. Participants were assigned randomly to no intervention (control group) or to receive PFP sessions (study group) in a 1:1 ratio. Block randomization was computer generated and the allocation was hidden in opaque envelopes until randomized. following inclusion criteria: age between 18 and 45 years, clinical and ultrasound diagnosis of DIE and associated superficial dyspareunia. Exclusion criteria included previous or current genital malignancy, pelvic organ prolapse, previous surgery for DIE, current or previous pregnancy, congenital or acquired abnormalities of the pelvis or pelvic floor, history of sexual abuse, current genitourinary infection and presence of other causes of CPP; written informed consent was obtained from all participating women. Four months after randomization, all participants underwent a second examination, in which they were asked to rank again their endometriosis-related pain symptoms and underwent another 3D/4D-TPU assessment of the LHA at rest, on maximum PFMC and on maximum Valsalva maneuver. In addition, the women in the study group were asked to rate their satisfaction with their physiotherapy treatment using a 5-item scale (1, very dissatisfied; 2, dissatisfied; 3, neither satisfied nor dissatisfied; 4, satisfied; and 5, very satisfied). |
In conclusion PFP seems to be effective in improving pelvic floor muscle relaxation, superficial dyspareunia and CPP in women with DIE. As such, the studied physiotherapy protocol may improve patients’ quality of life and sexual life, which are often compromised in women with DIE11,43. 3D/4D-TPU is a reliable, objective and non-invasive method for assessing the pelvic floor muscles in these women. In the current context of tailored, multidisciplinary care40, PFP may represent an additional valid, minimally invasive, innovative and well-tolerated therapeutic option for women with DIE, particularly those with superficial dyspareunia and CPP. | No |
| del Mar Salinas-Asensio et al., 2022 [30] | Physio-EndEA’ Study A total of 22 symptomatic endometriosis women will be randomized 1:1 to the Physio-EndEA or usual care groups. The Physio-EndEA’ program consist of a one-week lumbopelvic stabilization learning phase followed by an eight-week phase of stretching, aerobic and resistance exercises focused on the lumbopelvic area that will be sequentially instructed and supervised by a trained physiotherapist (with volume and intensity progression) and adapted daily to the potential of each participant. The primary outcome measure is HRQoL. The secondary outcome measures included clinician-reported outcomes (pressure pain thresholds, muscle thickness and strength, flexibility, body balance and cardiorespiratory fitness) and patient-reported outcomes (pain intensity, physical fitness, chronic fatigue, sexual function, gastrointestinal function and sleep quality). |
The establishment of this type of intervention could benefit the HRQoL of symptomatic women with endometriosis. Moreover, it might reduce the direct and indirect costs of this health problem. | No |
4. Discussion
5. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- Niculescu, A.B.; Le-Niculescu, H.; Levey, D.F.; Roseberry, K.; Soe, K.C.; Rogers, J. White, F. A. Towards precision medicine for pain: diagnostic biomarkers and repurposed drugs. Molecular psychiatry. 2019, 24, 501–522. [Google Scholar] [CrossRef] [PubMed]
- Mehedintu, C.; Plotogea, M.N.; Ionescu, S.; Antonovici, M. Endometriosis still a challenge. Journal of Medicine and Life. 2014, 7, 349–357. [Google Scholar] [PubMed]
- Greene, A.D.; Lang, S.A.; Kendziorski, J.A.; Sroga-Rios, J.M.; Herzog, T.J.; Burns, K.A. Endometriosis: Where are We and Where are We Going? Reproduction. 2016, 152, R63–R78. [Google Scholar] [CrossRef] [PubMed]
- Giudice, L.C. Clinical practice. Endometriosis. N Engl J Med. 2010, 362, 2389–98. [Google Scholar] [CrossRef] [PubMed]
- Dun, E.C.; Kho, K.A.; Morozov, V.V.; Kearney, S.; Zurawin, J.L.; Nezhat, C.H. Endometriosis in adolescents. Journal of the Society of Laparoendoscopic Surgeons. 2015, 19, e2015.00019. [Google Scholar] [CrossRef]
- Engeler, D.; Baranowski, A.P.; Borovicka, J.; Cottrell, A.M.; Dinis-Oliveira, P.; Elneil, S.; Hughes, J.; Messelink, E.J.; de C Williams, A.C. Guidelines Associates: Goonewardene, S.; Schneider, M.P. EAU Guidelines on Chronic Pelvic Pain. 2017. [Google Scholar]
- Morotti, M.; Vincent, K.; Becker, Ch.M. Mechanisms of pain in endometriosis. Eur J Obstet Gynecol Reprod Biol. 2017, 209, 8–13. [Google Scholar] [CrossRef]
- Ahn, S.H.; Singh, V.; Tayade, C. Fertil Steril Biomarkers in endometriosis: challenges and opportunities. Fertil Steril. 2017, 107, 523–532. [Google Scholar] [CrossRef]
- Bjorkman, S.; Taylor, H.S. MicroRNAs in endometriosis: biological function and emerging biomarker candidates†. Biol Reprod. 2019, 100, 1135–1146. [Google Scholar] [CrossRef]
- Wang, J.; Cong, S.; Wu, H.; He, Y.; Liu, X.; Sun, L.; Zhao, X.; Zhang, G. Identification and Analysis of Potential Autophagy-Related Biomarkers in Endometriosis by WGCNA. Front Mol Biosci. 2021, 8, 743012. [Google Scholar] [CrossRef]
- Jiang, L.; Zhang, M.; Wu, J.; Wang, S.; Yang, X.; Yi, M.; Zhang, X.; Fang, X. Exploring diagnostic m6A regulators in endometriosis. Aging (Albany NY). 2020, 12, 25916–25938. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, L.M.; Ferreira, M.C.; Rocha, A.L.L.; Carneiro, M.M.; Reis, F.M. New biomarkers in endometriosis. Adv Clin Chem. 2019, 89, 59–77. [Google Scholar] [PubMed]
- Saunders, P.T.K.; Horne, A.W. Endometriosis: Etiology, pathobiology, and therapeutic prospects. Cell. 2021, 27, 2807–2824. [Google Scholar] [CrossRef] [PubMed]
- As-Sanie, S.; Black, R.; Giudice, L.C.; Gray Valbrun, T.; Gupta, J.; Jones, B.; Laufer, M.R.; Milspaw, A.T.; Missmer, S.A.; Norman, A.; Taylor, R.N.; Wallace, K.; Williams, Z.; Yong, P.J.; Nebel, R.A. Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol. 2019, 221, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Buggio, L.; Dridi, D.; Barbara, G.; Merli, C.E.M.; Cetera, G.E. Vercellini P.Novel pharmacological therapies for the treatment of endometriosis. Expert Rev Clin Pharmacol. 2022, 15, 1039–1052. [Google Scholar] [CrossRef]
- Zajec, V.; Mikuš, M.; Vitale, S.G.; D'alterio, M.N.; Gregov, M.; Šarić, M.J.; Carugno, J.; Angioni, S.; Ćorić, M. Current status and challenges of drug development for hormonal treatment of endometriosis: a systematic review of randomized control trials. Gynecol Endocrinol. 2022, 38, 713–720. [Google Scholar] [CrossRef]
- Linzagolix: a new GnRH-antagonist under investigation for the treatment of endometriosis and uterine myomas. Dababou S, Garzon S, Laganà AS, Ferrero S, Evangelisti G, Noventa M, D'Alterio MN, Palomba S, Uccella S, Franchi M, Barra F. Expert Opin Investig Drugs. 2021, 30, 903–911. [CrossRef]
- Donnez, J.; Dolmans, M.M. GnRH Antagonists with or without Add-Back Therapy: A New Alternative in the Management of Endometriosis? Int J Mol Sci. 2021, 22, 11342. [Google Scholar] [CrossRef]
- Legendre, G.; Delbos, L.; Hudon, E.; Chabbert-Buffet, N.; Geoffron, S.; Sauvan, M.; Fernandez, H.; Bouet, P.E.; Descamps, P. New medical treatments for painful endometriosis: CNGOF-HAS Endometriosis Guidelines. Gynecol Obstet Fertil Senol. 2018, 46, 256–263. [Google Scholar]
- Kho, R.M.; Andres, M.P.; Borrelli, G.M.; Neto, J.S.; Zanluchi, A.; Abrão, M.S. Surgical treatment of different types of endometriosis: Comparison of major society guidelines and preferred clinical algorithms. Best Pract Res Clin Obstet Gynaecol. 2018, 51, 102–110. [Google Scholar] [CrossRef]
- Rolla, E. Endometriosis: advances and controversies in classification, pathogenesis, diagnosis, and treatment. F1000 Res. 2019, 8, F1000. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Gibbons, T.; Armour, M.; Wang, R.; Glanville, E.; Hodgson, R.; Cave, A.E.; Ong, J.; Tong, Y.Y.F.; Jacobson, T.Z.; Mol, B.W.; Johnson, N.P.; Condous, G. When to Do Surgery and When Not to Do Surgery for Endometriosis: A Systematic Review and Meta-analysis. J Minim Invasive Gynecol. 2020, 27, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.; Sverrisdóttir, U.A.; Rudnicki, M. Impact of exercise on pain perception in women with endometriosis: A systematic review. Acta Obstet Gynecol Scand. 2021, 100, 1595–1601. [Google Scholar] [CrossRef] [PubMed]
- Tennford, M.K.; Gabrielsen, R.; Tellum, T. Efect of physical activity and exercise on endometriosis-associated symptoms: a systematic review. BMC Women’s Health. 2021, 21, 355. [Google Scholar]
- Habek, D.; Cerovac, A.; Kamerić, L.; Nevačinović, E.; Šerak, A. Balneogynaecology in the 21st century: increasingly recommended primary and complementary treatment of chronic gynaecological diseases. Med Glas (Zenica). 2021, 18, 1–6. [Google Scholar]
- Mardon, A.K.; Leake, H.B.; Szeto, I.K.; Astill, T.; Hilton, S.; Moseley, G.L.; Chalmers, K.J. Treatment recommendations for the management of persistent pelvic pain: a systematic review of international clinical practice guidelines. BJOG. 2022, 129, 1248–1260. [Google Scholar] [CrossRef]
- Goździewicz, T.; Jarzabek-Bielecka, G.; Luwanski, D.; Wójcik, M.; Plagens-Rotman, K.; Mizgier, M.; Pisarska-Krawczyk, M.; Kędzia, W. The Role of Visceral Therapy in the Sexual Health of Women with Endometriosis during the COVID-19 Pandemic: A Literature Review. J. Clin. Med. 2022, 11, 5825. [Google Scholar] [CrossRef]
- Mira, T.A.A.; Yela, D.A.; Podgaec, S.; Baracat, E.C.; Benetti-Pinto, C.L. Hormonal treatment isolated versus hormonal treatment associated with electrotherapy for pelvic pain control in deep endometriosis: Randomized clinical trial. Eur. J. Obstet Gyneacol. Reprod. Biol . 2020, 255, 134–141. [Google Scholar] [CrossRef]
- Del Forno, S.; Arena, A.; Pellizzone, V.; Lenzi, J.; Raimondo, D.; Cocchi, L.; Paradisi, R.; Youssef, A.; Casadio, P.; Seracchioli, R. Assessment of levator hiatal area using 3D/4D transperineal ultrasound in women with deep infiltrating endometriosis and superficial dyspareunia treated with pelvic floor muscle physiotherapy: randomized controlled trial. Ultrasound Obstet Gynecol. 2021, 57, 726–732. [Google Scholar] [CrossRef]
- Del Mar Salinas-Asensio, M.; Ocón-Hernández, O.; Mundo-López, A.; Fernández-Lao, C.; Peinado, F.M.; Padilla-Vinuesa, C.; Álvarez-Salvago, F.; Postigo-Martín, P.; Lozano-Lozano, M.; Lara-Ramos, A.; Arroyo-Morales, M.; Cantarero-Villanueva, I.; Artacho-Cordón, F. 'Physio-EndEA' Study: A Randomized, Parallel-Group Controlled Trial to Evaluate the Effect of a Supervised and Adapted Therapeutic Exercise Program to Improve Quality of Life in Symptomatic Women Diagnosed with Endometriosis. Int J Environ Res Public Health. 2022, 19, 1738. [Google Scholar] [CrossRef]
- Ross, V.; Detterman, C.; Hallisey, A. Myofascial Pelvic Pain: An Overlooked and Treatable Cause of Chronic Pelvic Pain. J Midwifery Womens Health. 2021, 66, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Stone, C.; Williams, A. Visceral and Obstetric Osteopathy; Churchill Livingstone: London, UK, 2007. [Google Scholar]
- Barral, J.P.; Mercier, P. Visceral Manipulation; Eastland Press: Seattle, WA, USA, 1988. [Google Scholar]
- Anthonissen, M.; Daly, D.; Janssens, T.; Van den Kerckhove, E. The effects of conservative treatments on burn scars: A systematic review. Burns. 2016, 42, 508–18. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.S.; Jeon, J.H.; Hong, A.; Yang, H.T.; Yim, H.; Cho, Y.S.; Kim, D.H.; Hur, J.; Kim, J.H.; Chun, W.; Lee, B.C.; Seo, C.H. The effect of burn rehabilitation massage therapy on hypertrophic scar after burn: a randomized controlled trial. Burns. 2014, 40, 1513–20. [Google Scholar] [CrossRef] [PubMed]
- Boden, I.; Sullivan, K.; Hackett, C.; Winzer, B.; Lane, R.; McKinnon, M.; Robertson, I. ICEAGE (Incidence of Complications following Emergency Abdominal surgery: Get Exercising): study protocol of a pragmatic, multicentre, randomised controlled trial testing physiotherapy for the prevention of complications and improved physical recovery after emergency abdominal surgery. World J Emerg Surg. 2018, 13, 29. [Google Scholar]
- Brown, J.; Crawford, T.J.; Allen, C.; Hopewell, S.; Prentice, A. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst Rev. 2017, 23, 1–CD004753. [Google Scholar] [CrossRef]
- Jarrell, J.; Brant, R.; Leung, W.; Taenzer, P. Women's Pain Experience Predicts Future Surgery for Pain Associated With Endometriosis. J Obstet Gynaecol Can. 2007, 29, 988–991. [Google Scholar] [CrossRef]
- Jarrell, J.; Mohindra, R.; Ross, S.; Taenzer, P.; Brant, R. Laparoscopy and reported pain among patients with endometriosis. J Obstet Gynaecol Can. 2005, 27, 477–85. [Google Scholar] [CrossRef]
- Amini, L.; Chekini, R.; Nateghi, M.R.; Haghani, H.; Jamialahmadi, T.; Sathyapalan, T.; Sahebkar, A. The Effect of Combined Vitamin C and Vitamin E Supplementation on Oxidative Stress Markers in Women with Endometriosis: A Randomized, Triple-Blind Placebo-Controlled Clinical Trial. Pain Res Manag. 2021, 5529741. [Google Scholar] [CrossRef]
- Anastasiu, C.V.; Moga, M.A.; Neculau, A.E.; Bălan, A.; Scârneciu, I.; Dragomir, R.M.; Dull, A.M.; Chicea, L.M. Biomarkers for the Noninvasive Diagnosis of Endometriosis: State of the Art and Future Perspectives. Int J Mol Sci. 2020, 21, 1750. [Google Scholar] [CrossRef]
- Shcherbina, N.A.; Potapova, L.V.; Shcherbina, I.N.; Lipko, O.P.; Mertsalova, O.V.; Chekhunova, A.A. Modern methods of complex correction of psychosomatic disorders in patients with external genital endometriosis. Wiad Lek. 2020, 73, 2623–2626. [Google Scholar] [CrossRef]
- Thabet, A.A.E.; Alshehri, M.A. Effect of Pulsed High-Intensity Laser Therapy on Pain, Adhesions, and Quality of Life in Women Having Endometriosis: A Randomized Controlled Trial. Photomed Laser Surg. 2018, 36, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Mira, T.A.; Giraldo, P.C.; Yeala, D.A.; Benetti- Pinto, C. Effectiveness of complementary pain treatment for women with deep endometriosis through Transcutaneous Electrical Nerve Stimulation (TENS): randomized controlled trial. Eur. J. Obstet Gyneacol. Reprod. Biol. 2015, 194, 1–6. [Google Scholar] [CrossRef]
- Zhang, Z.Y.; Wang, J.; Fan, Y.L.; Wang, B.Y.; Zhang, W.T. Effectiveness of neuromuscular electrical stimulation for endometriosis-related pain: A protocol of systematic review and meta-analysis. Medicine (Baltimore). 2020, 99, e20483. [Google Scholar] [CrossRef] [PubMed]
- de Mira, T.A.A.; Yela, D.A.; Podgaec, S.; Baracat, E.C.; Benetti-Pinto, C.L. Reply to Letter to the Editor entitled Re: Hormonal treatment isolated versus hormonal treatment associated with electrotherapy for pelvic pain control in deep endometriosis: Randomized clinical trial. Eur J Obstet Gynecol Reprod Biol. 2021, 258, 463–464. [Google Scholar] [CrossRef]
- Jorgensen, W.A.; Frome, B.M.; Wallach, C. Electrochemical therapy of pelvic pain: effects of pulsed electromagnetic fields (PEMF) on tissue trauma. Eur J Surg Suppl. 1994, 574, 83–6. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





