Background: Cataract and Age-related Macular Degeneration are two characteristic diseases of the so-called elderly age (75-90 years and older). Both determine an important visual impairment, so it is often difficult to understand how much of the visual loss is given by the cataract opacities and how much by the degeneration of the macula and this assumes a relevant medico-legal query in clinical practice.
Considering the history of cataract extraction surgery, intracapsular cataract extraction, and extracapsular techniques certainly in the past were cause of dramatic worsening of macular clinical conditions for the hypotony during the surgery which meant that in patients with CNV new formed vessels were filled with blood and for long lasting exposition to microscope light.
Many ophthalmologists, even talented surgeons, in that time had a scared terror of operating on a patient with maculopathy, considering the surgeons who ventured into this surgery very unconscious and crazy people.
Starting from the 90s phacoemulsification techniques reduced the surgery time and hypotony. With this revolutionary technique the surgeon worked during the whole surgery in a "closed space" in the anterior chamber. This step, working in a closed anterior chamber and at high infusion pressure, made it possible to reduce or virtually eliminate the risk of subretinal hemorrhage in the intra- or peri-operative phase.
Furthermore, today we have the possibility of using VEGF inhibitors at the end of surgery, which allow for the neutralization of any activation of the growth factor cascade.
But what it is the correct behavior if we find ourselves with a patient with maculopathy and cataract, are there any guidelines that can give us greater safety of the procedures? Unfortunately, no help comes from the study of the literature, so we decided in case of wAMD to apply a specifical protocol before the surgery.
1. Material and Methods
Since year 2018 in our Clinical Department were operated 2318 patients with clinical signs of wAMD recognized with AngioOCT and evaluated with line analysis and 4798 patients without clinical markers of wAMD.
From that pool we randomized in two groups 735 eyes with wAMD signs at different evolutionary conditions (males 328, females 407) Average age: 76.23±13.87 years, and 819 eyes without clear signs of wAMD (males 361, females 451) Average age: was 75.88±18.21 years to randomize them we used the online randomization program (
http://www.graphpad.com/quickcalcs/index.cfm) selecting random numbers and then randomly assign subjects to groups to undergo our observational study.
All patients were examined with full ophtalmological visit including Best Corrected Visual Acuity (with Bailey-Lawson Chart), Anterior Segment examination, Fundus Examination, in all cases was also performed OCT (Heidelberg Gmbh GER. Spectralis) scans.
Surgery eligibility criteria were the visual Acuity worse than 0.40 LogMAR, nucleus value 3+, subcortical opacities. Exclusion criteria were previous retinal surgery, myopia higher than 6 diopters, history of toxic or traumatic etiology of cataracts. All eyes were followed for a 3-month period or more at the 90 days examination the value of visual acuity of more than 2 lines at Bailey-Lawson chart was considered as positive outcome, a worsening more than a line was considered as negative outcome, other values were considered as stationary.
All patients approved the intervention by signing a dedicated informed consent as described above, and the study was conducted according to the tenant of Helsinki declaration for clinical studies, data availability was in the Archives of UOC Ophthalmology University in “Fiorini Hospital” Terracina. Department ethical committee approved the study on 12 Dec. 2022.
Statistical evaluation was drawn with SPSS software (IBM ltd. USA), using ANOVA multivariate test, significative level was p=0.05.
We considered each eye as a single case because in our opinion baseline clinical conditions, surgery events (duration, ultrasound, light exposure) differ in substantial way.
During the surgery were taken all necessary measures finalized to reduce the onset of inflammatory processes and activation of cytokines at the level of maculopathy, particularly we tried to reduce operating times, lower the amount of light on the central area of the red reflex, especially after inserting the IOL, apply for smaller of surgical cut considering that if there are leaks the IOP tends to decrease in this way would be possible a break in new vessels wall. Optionally in some cases cataract surgery was combined with intravitreal (IVT) injection of anti-VEGF molecule, Use anti-inflammatory drugs (Cortisone and/or NSAIDs) two hours before surgery. After the surgery all patients were examined at one day, one week, one and three months. very early OCT and angioOCT were repeated regularly at each follow up step, was used Amsler grid for patient self-monitoring, If CNV is found, early intervention with anti-VEGF was scheduled.
To evaluate clinical outcome we considered visual performances in terms of BCVA, considering improved cases with increase of at least 10 letters, unchanged patients with visual performances between a loss of 5 letters and an increase of 10, while we considered as unsatisfactory outcome a visual loss of more than 5 letters.
2. Results
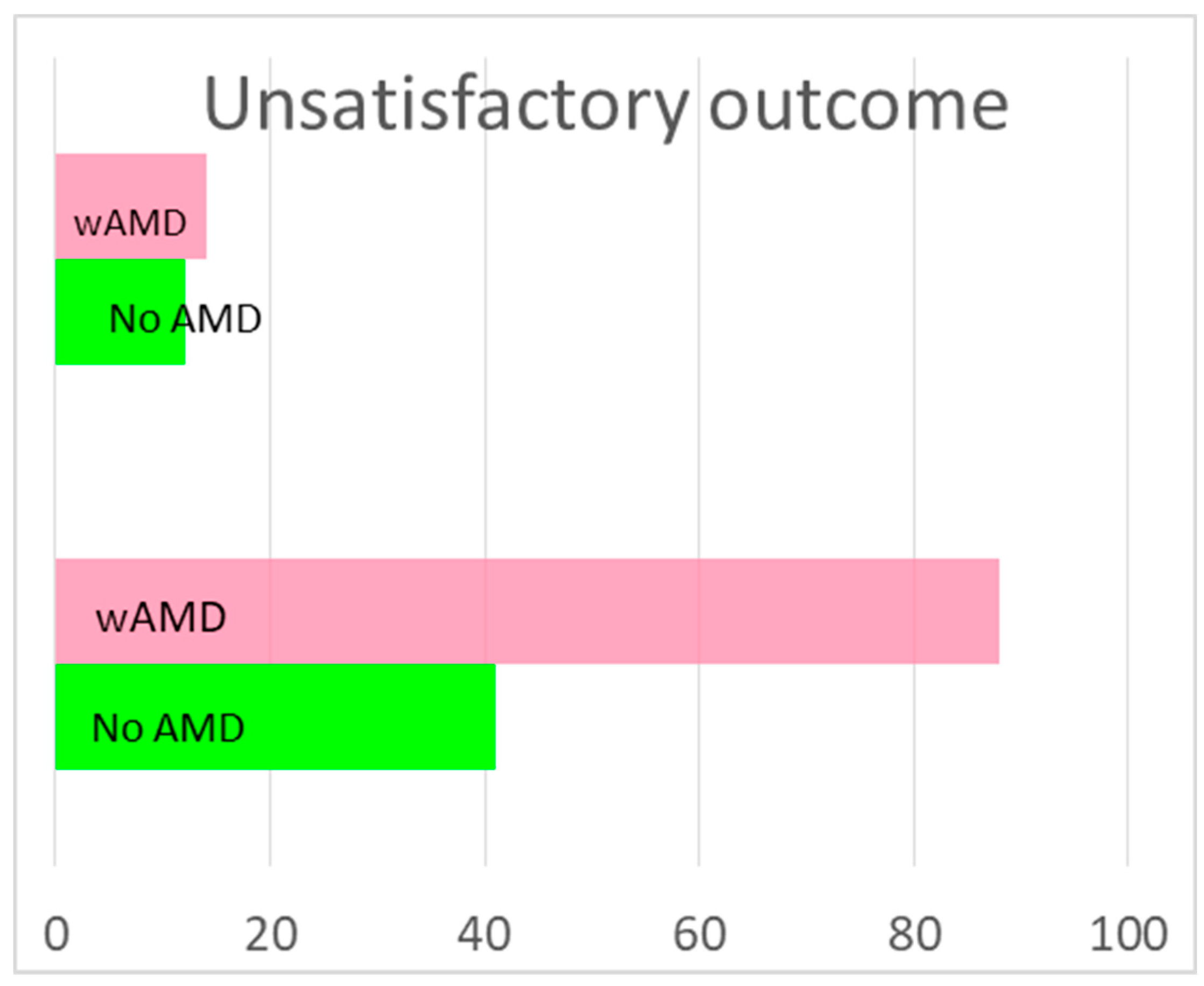
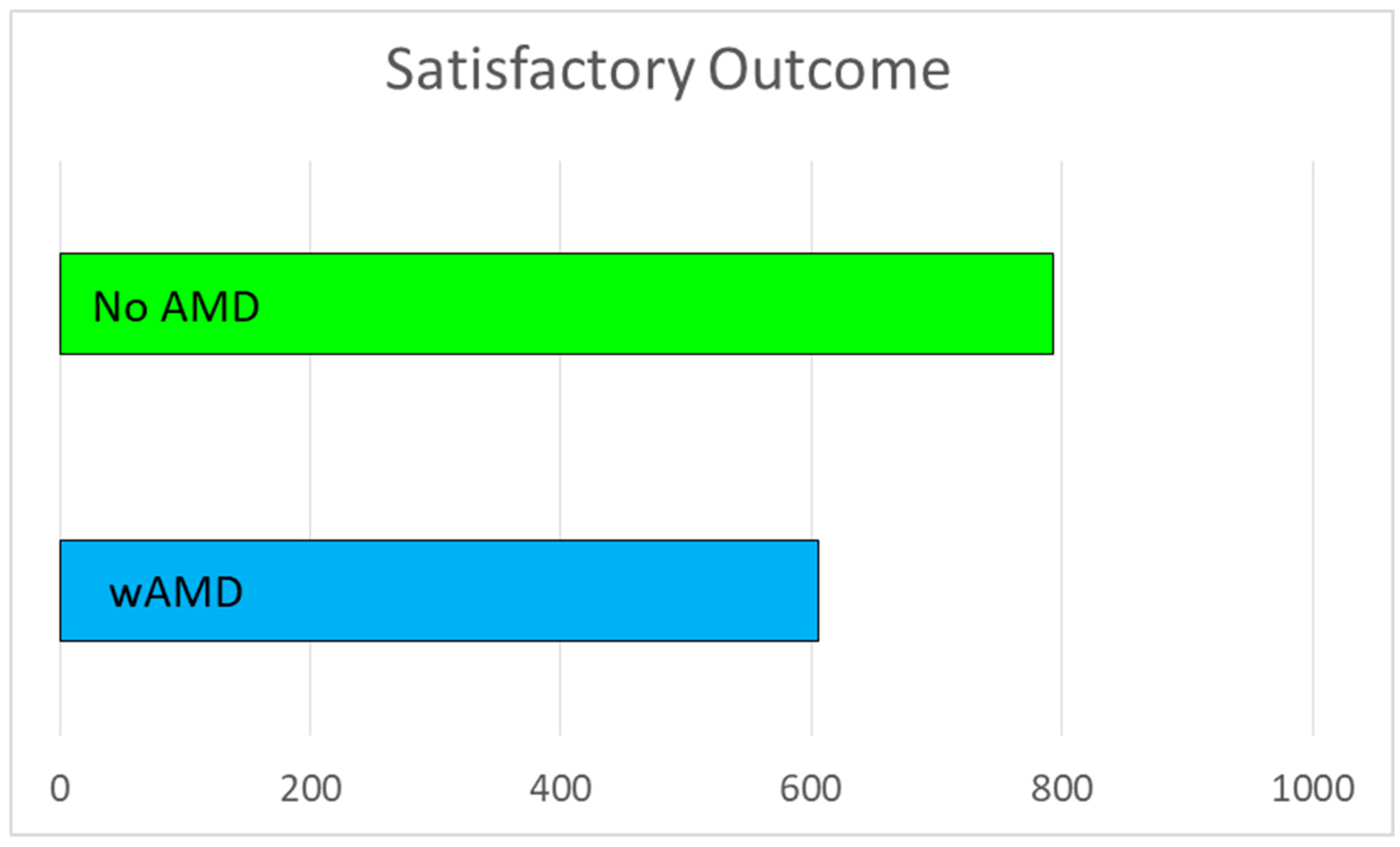
In group of eyes with wAMD, after the surgery 606 (82.44%) eyes were Improved, 41 (5.58%) Unchanged and 88 (11.97%) Worsened (
Figure 1)
Of these last 88 patients, 56 (63.63%) presented a morphological worsening of the maculopathy with reactivation of the CNV and were reinserted into a treatment line with intra-vitreal injections of VEGF inhibitors. None of these patients received an injection at the same time as the surgery.
In group of patients without wAMD were Improved: 793 (96.83%) eyes, were Unchanged: 12 (1.47%) and Worsened: 14 (1.71%) Of these last 14 patients, 6 (42.86%) presented the appearance of a maculopathy with activation of a CNV and were included in a treatment loading phase with intra-vitreal VEGF inhibitors. In our opinion these patients probably already had a subclinical and initial form of undiagnosed NVC, that the surgery did accelerate but this view could not be confirmed because preoperative OCT did not show clinical alterations suggesting wAMD. (
Figure 1)
Difference between two groups were statistically highly significant (p=0.00001).
As can be easily seen from the graphs in
Figure 1, the number of patients with unsatisfactory surgery is significantly higher in the group of AMD patients, and this is easily understandable from what has been said above, but I would like to underline that in most patients there are very positive results, therefore cataract surgery is also indicated in AMD patients.
It is also clear that nevertheless the increased percentage of worsening risk more than half of eyes, as presented in
Figure 2, has a relevant benefit from the surgery and this is consistent with the idea that could be useful perform in wAMD eyes cataract extraction with more precautions and delicacy than the eyes with cataract only.
As secondary outcome in our study must be considered that in wAMD patients after the surgery have less glare and better reading speed even with unchanged visual performances.
3. Discussion
Considering the history of cataract extraction surgery, few years ago (not so many) at the time of the intracapsular extraction, until about the end of 1980’, and of the extracapsular or until the dawn of the new century, a cut of 9-12 millimeters usually caused a hypotony which meant that in patients with CNV new formed vessels were filled with blood. Frequently capillary blood pressure was higher than the vessel resistance causing postoperative haemorrhagic maculopathy that was frequently found after surgery independently from the outcome of surgery. Therefore, in those days, operating on a patient with maculopathy was a kind of "Russian roulette" in which were possible achieve after the surgery a worse visual acuity than before the intervention.
Many ophthalmologists, even talented surgeons, had a scared terror of operating on a patient with maculopathy, considering the surgeons who ventured into this surgery very unconscious and crazy people, to avoid the possibility to have a macular hemorrhage, some surgeons recommended a very accurate blood pressure control with very risky values (PAO max at 60 mmHg). Starting from the 90s and gradually involving an increasing number of ophthalmologists, the phacoemulsification came into action. With this revolutionary technique stitches were not applied; local or general anesthesia was not necessary, and the surgeon worked during the whole surgery in a "closed space" in the anterior chamber.
This step, working in a closed anterior chamber and at high infusion pressure, made it possible to reduce or virtually eliminate the risk of subretinal hemorrhage in the intra- or peri-operative phase. In fact, actually, during the operation, even in the most intense aspiration phases, an average intraocular pressure of 25-45 mmHg is worked on (obviously for few seconds) which prevents the rupture of a CNV even in the active phase.
In our opinion the use of the femtolaser in cataract surgery is dangerous in patients with wAMD, due to the high impact energies required, in fact these electromagnetic radiations are transformed into very dangerous thermal energy which could even reach the retina and activate recovery grow factors like VEGF, PDEGF and others or activating apoptotic cascade.
Furthermore, today we have the possibility of using VEGF inhibitors at the end of surgery, which allow for the neutralization of any activation of the growth factor cascade. However, intervention should always be done in a quiet phase of the CNV.
But what it is the correct behavior if a patient shows maculopathy and cataract, are there any guidelines that can give us greater safety of the procedures? As evident from this report we think that in a classic surgical time window there are things to carefully do:
Prior the surgery it is mandatory a complete retinal diagnosis, both functional and morphological: Visual acuity for distance and overall, for near, if possible also with a pinhole to evaluate the better performances of the macula, also in 6 patients (0.73%) in which at baseline there were no clinical signs of wAMD during the follow up there was a CNV onset. Was also proposed the use of microperimetry to evaluate fixation and sensitivity of the central retina before cataract surgery9, An Amsler grating may also be helpful to obtain information on the arrangement of macular photoreceptors, and for self-control of visual performances during the follow up10.
It is important during the operatory time putting in place all necessary measures to reduce the onset of inflammatory processes and activation of cytokines at the level of maculopathy, we believe that the most necessary are reduction of operating times, the longer the operation the more maneuvers on the macula (light, instruments, ultrasounds, etc.), reduction of light on the central area of the red reflex, especially after inserting the IOL (first the cataract and the defocus protect the retinal structures), reduction of the length of the surgical cut, if there are leaks the IOP tends to decrease in this way would be possible a break in new vessels wall, use the lower number of instruments that are inserted into the eye, because they cause a decrease in IOP with the risk of rupture of the newly formed vessels, Choice of the IOL and suitable material, Optionally combine an intravitreal (IVT) injection of anti-VEGF molecule, it is very important ALWAYS leave the eye hypertonic in the first 6-8 hours, Use anti-inflammatory drugs (Cortisone and/or NSAIDs) before and after surgery,
Other crucial point is to be sure that in the informed consent it is written that there is the possibility that the maculopathy will reactivate after the operation, and the need for close monitoring of the patient in the post-operative period.
The period after surgery is crucial, in fact the mechanisms activated with surgery determine the production of cytokines and growth factors (including VEGF) which significantly accelerate the processes of neovascularization, therefore post-operative monitoring has a predominant role in the primary prevention of CNV reactivation,
But how to monitor? with very early OCT and angioOCT (within 1-10 days), repeated regularly in the first 6 months after surgery, Microperimetry with assessment of retinal sensitivity and fixation within the first 30 days, repeating it regularly 3 and 6 months after surgery, Amsler grid for patient self-monitoring, If CNV is found, early intervention with anti-VEGF.
Generally, with such close monitoring it is quite frequent to intercept the reactivation of the CNV in an initial phase, i.e. when they are very sensitive to a therapy with antiVEGF drugs.
It must always be remembered that, if it is necessary to perform a YAG capsulotomy, the same pro-angiogenic mechanisms of the intervention can be reactivated and therefore the eye must be pre-treated with an NSAID active on the retina (bromfenac).
An important aspect of cataract surgery in maculopathy patients is its importance in the rehabilitation process, in fact the choice of the post-operative target refraction and/or the type of implanted IOL (monofocal, trifocal, EDOF, Multifocal, Toric) can have very positive effects on the patient's autonomy.
Our considerations apply particularly to the interpretation of what means “success” in cataract surgery in patients with AMD. in fact, the difference of one line more than before in a normally sighted person can mean little progress, while for a visually impaired patient it can mean the passage from a 4x to 1x magnification with the possibility of using more usable and comfortable aids. If we then evaluate parameters such as reading speed, scotometry or reading in recovery after glare, we realize that even with the same visual acuity, the functional condition of the patient can be much better than in the preoperative period. Finally, all treatments with biofeedback have a better outcome after cataract surgery even if "apparently" there is no change in vision (as we usually conceive it).
The AREDS 2 study considered that Cataract surgery did not increase the risk of developing late AMD among AREDS2 participants with up to 10 years of follow-up. This study provides data for counseling AMD patients who might benefit from cataract surgery ().Wang () in a study with the goal of clarify possible associations between cataract surgery and progression of age-related macular degeneration (AMD) following cataract surgery, in the Australian Cataract Surgery and Age-related Macular Degeneration (CSAMD) study, including Patients unilaterally phakic for 24 months after recruitment, showed that prospective follow-up data and paired eye comparisons has no increased risk of developing late AMD, early AMD, or soft/reticular drusen over 3 years, even he noted a 60% increased detection of retinal pigmentary changes in operated eyes.
As evidentiated by Bandhari (2) cataract surgery improves vision in eyes with co-existing age-related macular degeneration (AMD), but whether surgery itself pose an increased risk for the progression of AMD has been of concern to both physicians and their patients. Recent evidence suggests that cataract surgery does not really increase the risk for progression of AMD. Anymore Cataract surgery should be discussed in patients with both AMD and visually significant cataract. Patients should be informed that the cataract surgery will increase the risk of AMD progression. In patients with AMD, especially those with the more severe intermediate stage and those with advanced AMD in the fellow eye, the natural course of progression to late AMD is high and remains difficult to understand if worsening may be part of natural evolution of the disease or if is a consequence of surgery. Furthermore the Authors underline and emphasize the importance of vigilant follow-up for the detection of natural progression of the disease and early initiation of treatment as soon as signs of neovascularization develop.
The OCT is the key examination before performing a cataract surgery in a study performed from Murphy et al (1) evidentiated more than 25% of the patients had occult maculopathy and almost One-tenth of the occult maculopathy were missed without OCT, with ERM, dry AMD, VMT, LMH, CMO and wet AMD being the primary missed diagnosis. Less than 5% had occult maculopathy in fellow eye, and <5% had dense cataracts where neither SLIO nor OCT was not possible.
Microperimetry might also be used to evaluate the retinal function in macular area specially in patients with anatomically compromised anatomy as stated from our (8) and other Authors papers Miura et al (6) we think that can be expected to improve retinal sensitivity and contrast visual acuity after Cataract surgery under various conditions, even if preoperative visual parameters are low, as long as the ellipsoid zone is preserved.
4. Conclusions:
From my considerations on this topic there are certainly some messages that it is good to keep in mind always when it is necessary to properly evaluate a patient suffering from cataract and maculopathy (with active CNV or not it matters little).
Cataract surgery has a positive impact on the patient's life in most cases, you shouldn't be afraid to operate. However, it is necessary to find surgical measures capable of minimizing the consequences of the intervention on the retina, for medico-legal purposes it is always important to have a clear clinical picture (OCT) before and after the operation, and it is always useful to suggest to the patient the possibility of an unsatisfactory result and/or the reactivation of the maculopathy.
Rehabilitation process must always be set up at a distance from the intervention in stabilized functional conditions. It is extremely important in the primary prevention of CNV to carry out accurate and frequent monitoring of the patient in the first 6 months after surgery and it is very important to intervene early in case of CNV The improvement of a patient with maculopathy should not refer to visual acuity alone.
References
- Murphy, G.; Owasil, R.; Kanavati, S.; Ashena, Z.; Nanavaty, M.A. Preoperative fundoscopy versus optical coherence tomography to detect occult maculopathy during cataract surgery preassessment. Eye (Lond) 2023, 37, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, S.; Vitale, S.; Agrón, E.; Clemons, T.E.; Chew, E.Y. Age-Related Eye Disease Study 2 Research Group Cataract Surgery and the Risk of Developing Late Age-Related Macular Degeneration: The Age-Related Eye Disease Study 2 Report Number 27. Ophthalmology 2022, 129, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.J.; Fong CS, U.; Rochtchina, E.; Cugati, S.; De Loryn, T.; Kaushik, S.; Tan, J.S.L.; Arnold, J.; Smith, W.; Mitchell, P. Risk of age-related macular degeneration 3 years after cataract surgery: paired eye comparisons. Ophthalmology. 2012, 119, 2298–303. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Li, H.; Zhao, X.; Pan, Y. Association between Cataract Surgery and Age-Related Macular Degeneration: A Systematic Review and Meta-Analysis. J Ophthalmol 2022, 2022, 6780901. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, S.; Chew, E.Y. Cataract surgery and the risk of progression of macular degeneration. Curr Opin Ophthalmol 2023, 34, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Miura, G.; Baba, T.; Tatsumi, T.; Yokouchi, H.; Yamamoto, S. The Impact of Cataract Surgery on Contrast Visual Acuity and Retinal Sensitivity in Patients with Retinitis Pigmentosa. J Ophthalmol 2021, 2021, 2281834. [Google Scholar] [CrossRef] [PubMed]
- Giusti, C.; Forte, R.; Vingolo, E.M. Clinical pathogenesis of macular holes in patients affected by Retinitis Pigmentosa. European Review for Medical and Pharmacological Sciences 2002, 6, 45–48. [Google Scholar]
- Verboschi, F.; Domanico, D.; Nebbioso, M.; Corradetti, G.; Scalinci, S.Z.; Vingolo, E.M. New trends in visual rehabilitation with MP-1 microperimeter biofeedback: Optic neural dysfunction. Functional Neurology 2014, 28, 285–291. [Google Scholar]
- McKeague, M.; Sharma, P.; Ho, A.C. Evaluation of the macula prior to cataract surgery. Curr Opin Ophthalmol. 2018, 29, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, K.; Salini, B. Amsler Grid. 2023 Jul 24. In StatPearls [Internet]; StatPearls Publishing: Treasure Island (FL), 2023. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).