Submitted:
18 August 2023
Posted:
22 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
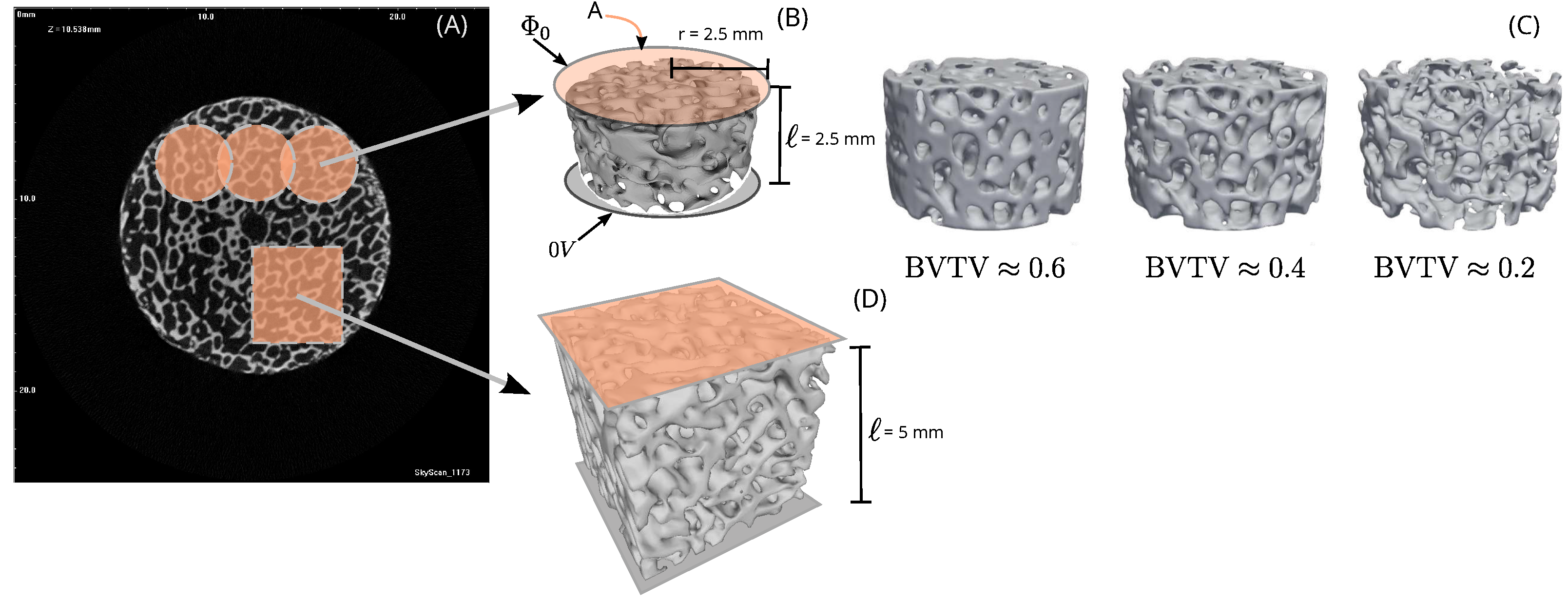
2.1. Sample preparation for building model geometries
2.2. Modeling and computer simulations
2.2.1. Governing equations and boundary conditions
2.2.2. Estimation of electrical conductivities
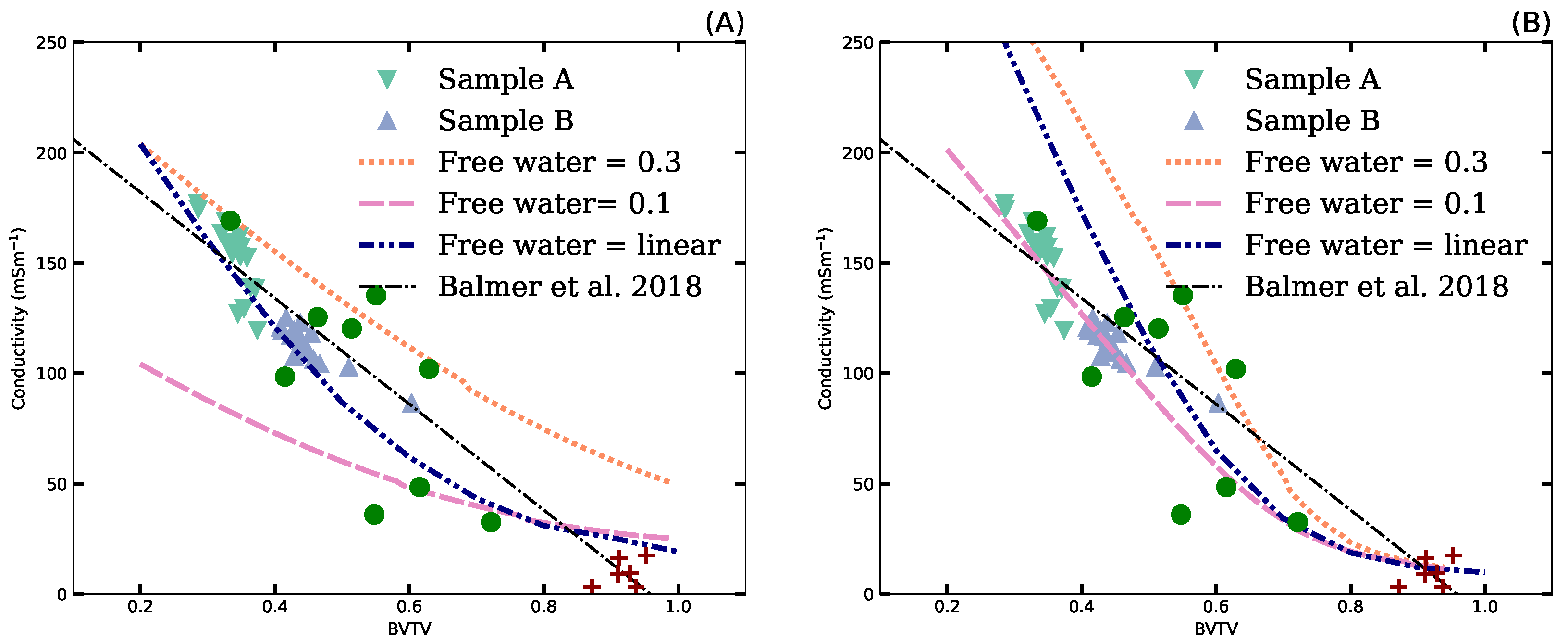
2.2.3. Mixing theory
2.3. Tissue characteristics
3. Results
3.1. Microstructure parameters
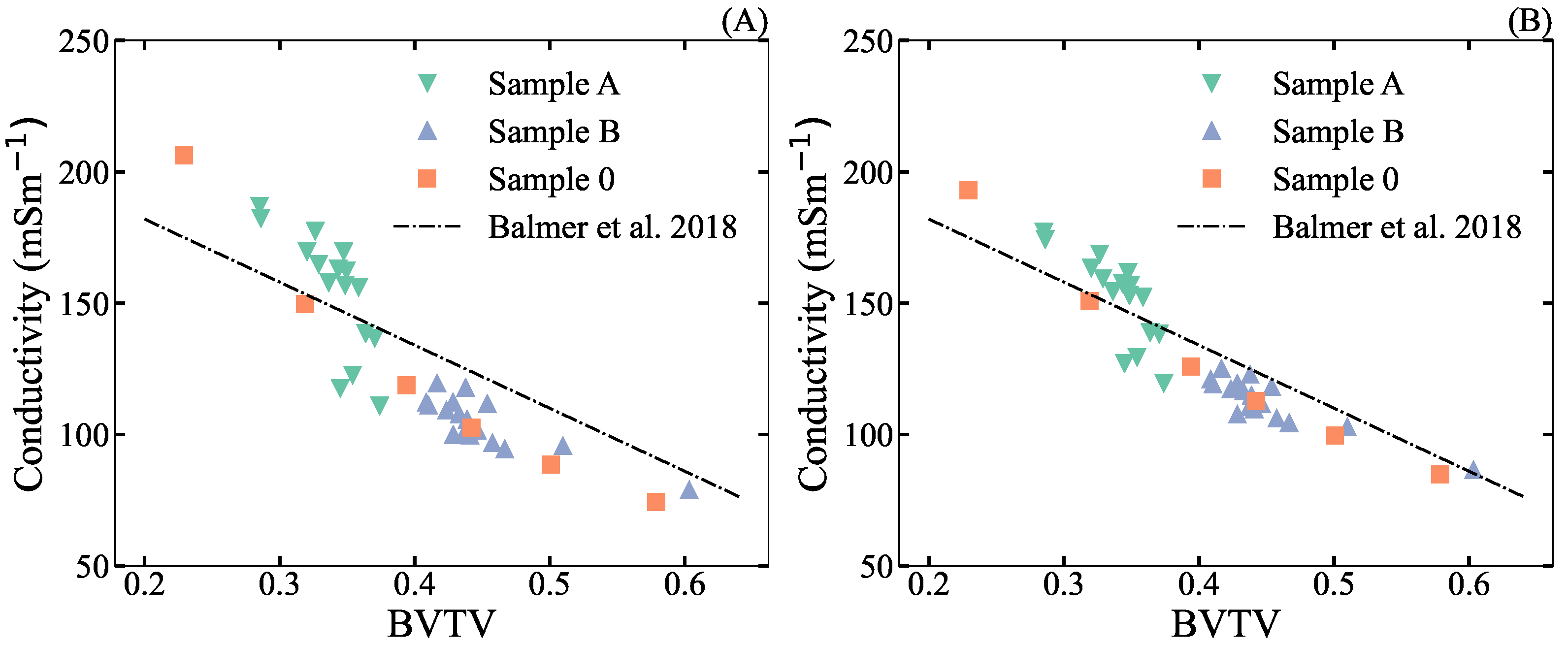
3.2. Estimation of effective electrical conductivity by FEM
3.3. Mixture models
3.4. Prediction of potential sources of measurement errors
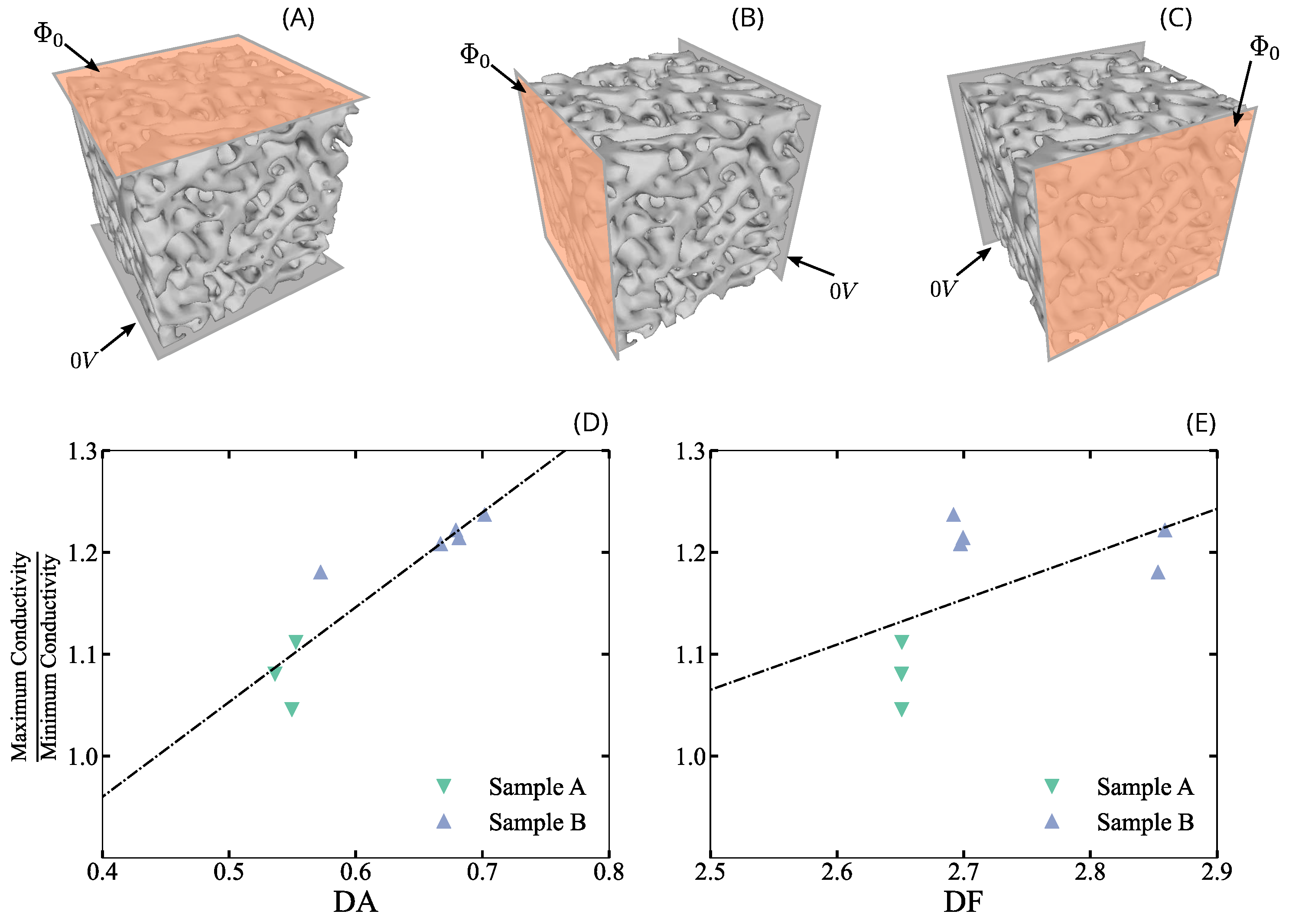
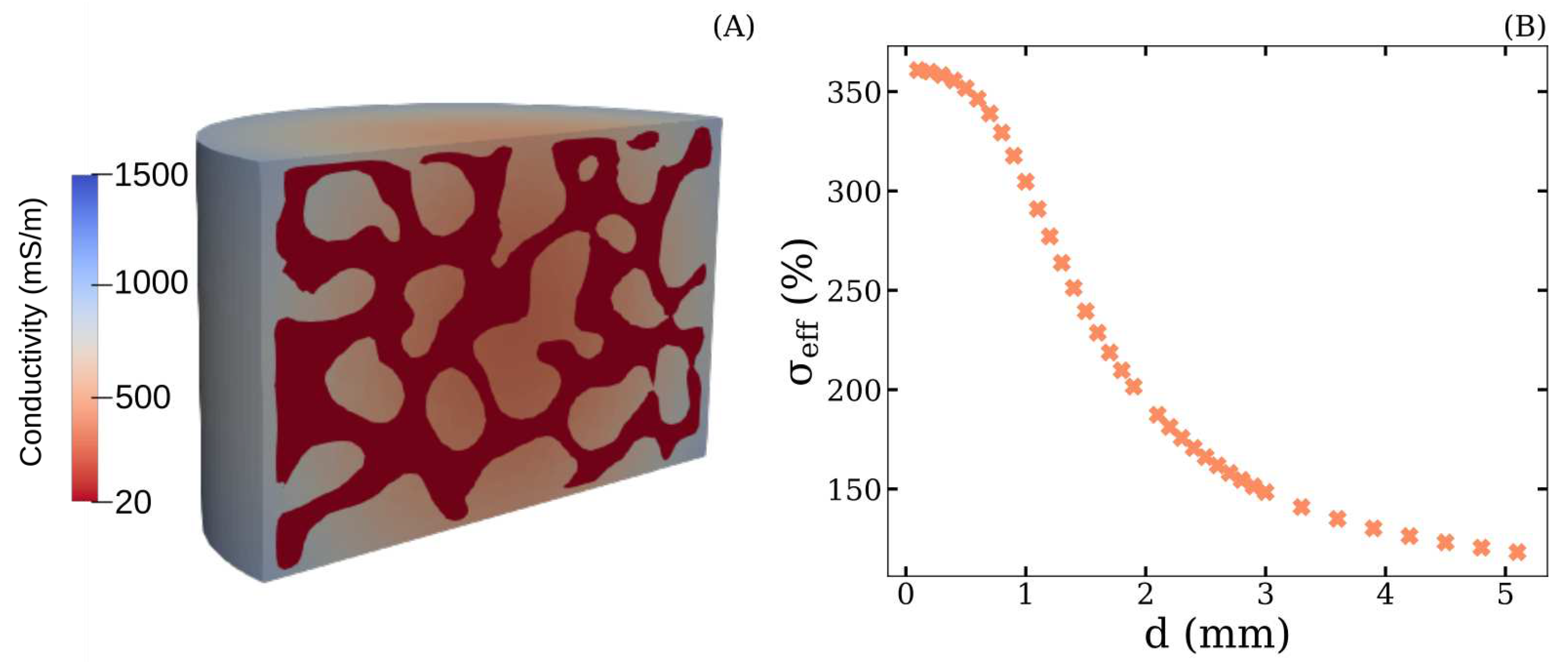
3.4.1. Anitsotropy
3.4.2. Influence of washing the samples
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kimel-Naor, S.; Abboud, S.; Arad, M. Parametric electrical impedance tomography for measuring bone mineral density in the pelvis using a computational model. Medical Engineering & Physics 2016, 38, 701–707. [Google Scholar]
- Lin, M.C.; Hu, D.; Marmor, M.; Herfat, S.T.; Bahney, C.S.; Maharbiz, M.M. Smart bone plates can monitor fracture healing. Scientific reports 2019, 9, 1–15. [Google Scholar] [CrossRef]
- Khalifeh, J.M.; Zohny, Z.; MacEwan, M.; Stephen, M.; Johnston, W.; Gamble, P.; Zeng, Y.; Yan, Y.; Ray, W.Z. Electrical stimulation and bone healing: A review of current technology and clinical applications. IEEE reviews in biomedical engineering 2018, 11, 217–232. [Google Scholar] [CrossRef]
- Ramos, A.; Dos Santos, M.P.S. Capacitive stimulation-sensing system for instrumented bone implants: Finite element model to predict the electric stimuli delivered to the interface. Computers in Biology and Medicine 2023, 154, 106542. [Google Scholar] [CrossRef]
- Balmer, T.W.; Vesztergom, S.; Broekmann, P.; Stahel, A.; Büchler, P. Characterization of the electrical conductivity of bone and its correlation to osseous structure. Scientific reports 2018, 8, 1–8. [Google Scholar] [CrossRef]
- Sierpowska, J.; Lammi, M.; Hakulinen, M.; Jurvelin, J.; Lappalainen, R.; Töyräs, J. Effect of human trabecular bone composition on its electrical properties. Medical engineering & physics 2007, 29, 845–852. [Google Scholar]
- Rho, J.Y.; Kuhn-Spearing, L.; Zioupos, P. Mechanical properties and the hierarchical structure of bone. Medical engineering & physics 1998, 20, 92–102. [Google Scholar]
- Ron, A.; Abboud, S.; Arad, M. Home monitoring of bone density in the wrist—a parametric EIT computer modeling study. Biomedical Physics & Engineering Express 2016, 2, 035002. [Google Scholar]
- Wong, P.; George, S.; Tran, P.; Sue, A.; Carter, P.; Li, Q. Development and validation of a high-fidelity finite-element model of monopolar stimulation in the implanted guinea pig cochlea. IEEE Transactions on Biomedical Engineering 2015, 63, 188–198. [Google Scholar] [CrossRef]
- Zimmermann, U.; Ebner, C.; Su, Y.; Bender, T.; Bansod, Y.D.; Mittelmeier, W.; Bader, R.; van Rienen, U. Numerical simulation of electric field distribution around an instrumented total hip stem. Applied Sciences 2021, 11, 6677. [Google Scholar] [CrossRef]
- Feng, C.; Yao, J.; Wang, L.; Zhang, X.; Fan, Y. Idealized conductance: A new method to evaluate stiffness of trabecular bone. International Journal for Numerical Methods in Biomedical Engineering 2021, 37, e3425. [Google Scholar] [CrossRef] [PubMed]
- Blaszczyk, M.; Hackl, K. Multiscale modeling of cancellous bone considering full coupling of mechanical, electric and magnetic effects. Biomechanics and Modeling in Mechanobiology 2022, 21, 163–187. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Shi, F.; Kolb, J. Impedimetric Analysis of Trabecular Bone Based on Cole and Linear Discriminant Analysis. Frontiers in Physics 2020, 8, 662. [Google Scholar] [CrossRef]
- Wei, W.; Shi, F.; Zhuang, J.; Kolb, J.F. Comprehensive characterization of osseous tissues from impedance measurements by effective medium approximation. AIP Advances 2021, 11, 105316. [Google Scholar] [CrossRef]
- Ciuchi, I.V.; Olariu, C.S.; Mitoseriu, L. Determination of bone mineral volume fraction using impedance analysis and Bruggeman model. Materials Science and Engineering: B 2013, 178, 1296–1302. [Google Scholar] [CrossRef]
- Sierpowska, J.; Hakulinen, M.; Töyräs, J.; Day, J.; Weinans, H.; Kiviranta, I.; Jurvelin, J.; Lappalainen, R. Interrelationships between electrical properties and microstructure of human trabecular bone. Physics in Medicine & Biology 2006, 51, 5289. [Google Scholar]
- Sierpowska, J.; Töyräs, J.; Hakulinen, M.; Saarakkala, S.; Jurvelin, J.; Lappalainen, R. Electrical and dielectric properties of bovine trabecular bone—relationships with mechanical properties and mineral density. Physics in Medicine & Biology 2003, 48, 775. [Google Scholar]
- Sihvola, A.H. Electromagnetic mixing formulas and applications; Number 47, Iet, 1999.
- Smith, S.R.; Foster, K.R. Dielectric properties of low-water-content tissues. Physics in Medicine & Biology 1985, 30, 965. [Google Scholar]
- Kosterich, J.D.; Foster, K.R.; Pollack, S.R. Dielectric permittivity and electrical conductivity of fluid saturated bone. IEEE Transactions on biomedical engineering 1983, pp. 81–86.
- Domander, R.; Felder, A.; Doube, M. BoneJ2 - refactoring established research software [version 2; peer review: 3 approved]. Wellcome Open Research 2021, 6. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magnetic resonance imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- van der Walt, S.; Schönberger, J.L.; Nunez-Iglesias, J.; Boulogne, F.; Warner, J.D.; Yager, N.; Gouillart, E.; Yu, T.; the scikit-image contributors. scikit-image: Image processing in Python. PeerJ 2014, 2, e453. [Google Scholar] [CrossRef] [PubMed]
- Cignoni, P.; Callieri, M.; Corsini, M.; Dellepiane, M.; Ganovelli, F.; Ranzuglia, G. MeshLab: An Open-Source Mesh Processing Tool. In Proceedings of the Eurographics Italian Chapter Conference; Scarano, V.; Chiara, R.D.; Erra, U., Eds. The Eurographics Association, 2008. [CrossRef]
- Geuzaine, C.; Remacle, J.F. Gmsh: A 3-D finite element mesh generator with built-in pre-and post-processing facilities. International journal for numerical methods in engineering 2009, 79, 1309–1331. [Google Scholar] [CrossRef]
- Langtangen, H.P.; Logg, A. Solving PDEs in Python; Springer, 2017. [CrossRef]
- Irastorza, R.M.; Blangino, E.; Carlevaro, C.M.; Vericat, F. Modeling of the dielectric properties of trabecular bone samples at microwave frequency. Medical & biological engineering & computing 2014, 52, 439–447. [Google Scholar]
- Storn, R.; Price, K. Differential evolution–a simple and efficient heuristic for global optimization over continuous spaces. Journal of global optimization 1997, 11, 341–359. [Google Scholar] [CrossRef]
- Kameo, Y.; Ootao, Y.; Ishihara, M. Poroelastic analysis of interstitial fluid flow in a single lamellar trabecula subjected to cyclic loading. Biomechanics and modeling in mechanobiology 2016, 15, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Unal, M.; Cingoz, F.; Bagcioglu, C.; Sozer, Y.; Akkus, O. Interrelationships between electrical, mechanical and hydration properties of cortical bone. Journal of the mechanical behavior of biomedical materials 2018, 77, 12–23. [Google Scholar] [CrossRef]
- Amin, B.; Elahi, M.A.; Shahzad, A.; Porter, E.; O’Halloran, M. A review of the dielectric properties of the bone for low frequency medical technologies. Biomedical Physics & Engineering Express 2019, 5, 022001. [Google Scholar]
- Gabriel, C.; Peyman, A. Dielectric properties of biological tissues; variation with age. Conn’s Handbook of Models for Human Aging 2018, pp. 939–952.
- Hasgall, P.; Di Gennaro, F.; Baumgartner, C.; Neufeld, E.; Gosselin, M.; Payne, D.; Klingenböck, A.; Kuster, N. Itis database for thermal and electromagnetic parameters of biological tissues, version 3.0, 2015.
- Gabriel, C. Compilation of the dielectric properties of body tissues at RF and microwave frequencies. Technical report, King’s Coll London (United Kingdom) Dept of Physics, 1996.
- Surowiec, R.K.; Allen, M.R.; Wallace, J.M. Bone hydration: How we can evaluate it, what can it tell us, and is it an effective therapeutic target? Bone reports 2022, 16, 101161. [Google Scholar] [CrossRef]
- Domander, R.; Felder, A.A.; Doube, M. BoneJ2-refactoring established research software. Wellcome Open Research 2021, 6. [Google Scholar] [CrossRef]
- Abbasi-Rad, S.; Akbari, A.; Malekzadeh, M.; Shahgholi, M.; Arabalibeik, H.; Rad, H.S. Quantifying cortical bone free water using short echo time (STE-MRI) at 1.5 T. Magnetic resonance imaging 2020, 71, 17–24. [Google Scholar] [CrossRef]
- Saha, S.; Williams, P. Effect of various storage methods on the dielectric properties of compact bone. Medical and Biological Engineering and Computing 1988, 26, 199–202. [Google Scholar] [CrossRef] [PubMed]
| Sample | BV/TV | DA | FD |
|---|---|---|---|
| # 1 A | 0.348 | 0.536 | 2.651 |
| # 2 A | 0.339 | 0.549 | 2.651 |
| # 3 A | 0.419 | 0.553 | 2.651 |
| # 1 B | 0.473 | 0.679 | 2.859 |
| # 2 B | 0.515 | 0.572 | 2.853 |
| # 3 B | 0.485 | 0.681 | 2.699 |
| # 4 B | 0.460 | 0.702 | 2.692 |
| # 5 B | 0.447 | 0.667 | 2.697 |
| Range (mS/m) | Results (mS/m) | |||||
| Simulation | Residue | Reference | ||||
| # 1 | 20 -700 | 9.1 | 344.8 | 9.1 | 0.050 | [5] |
| # 2 | 230 | 0.2-21 | 230.0 | 21.0 | 0.065 | [5] |
| # 3 | 3.82 (yellow) | 0.2-21 | 3.8 | 21.0 | 0.308 | [34] |
| # 4 | 103 (red) | 0.2-21 | 103.0 | 21.0 | 0.183 | [34] |
| # 5 | 20-700 | 0.2-21 | 298.4 | 21.0 | 0.025 | [19,34] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





