Submitted:
09 August 2023
Posted:
10 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and methods
2.1. Patients
2.2. Evaluations of choroidal thickness by UWF SS-OCT
2.3. Statistical analyses
3. Results
3.1. Characteristics and AMD subtypes of the enrolled patients
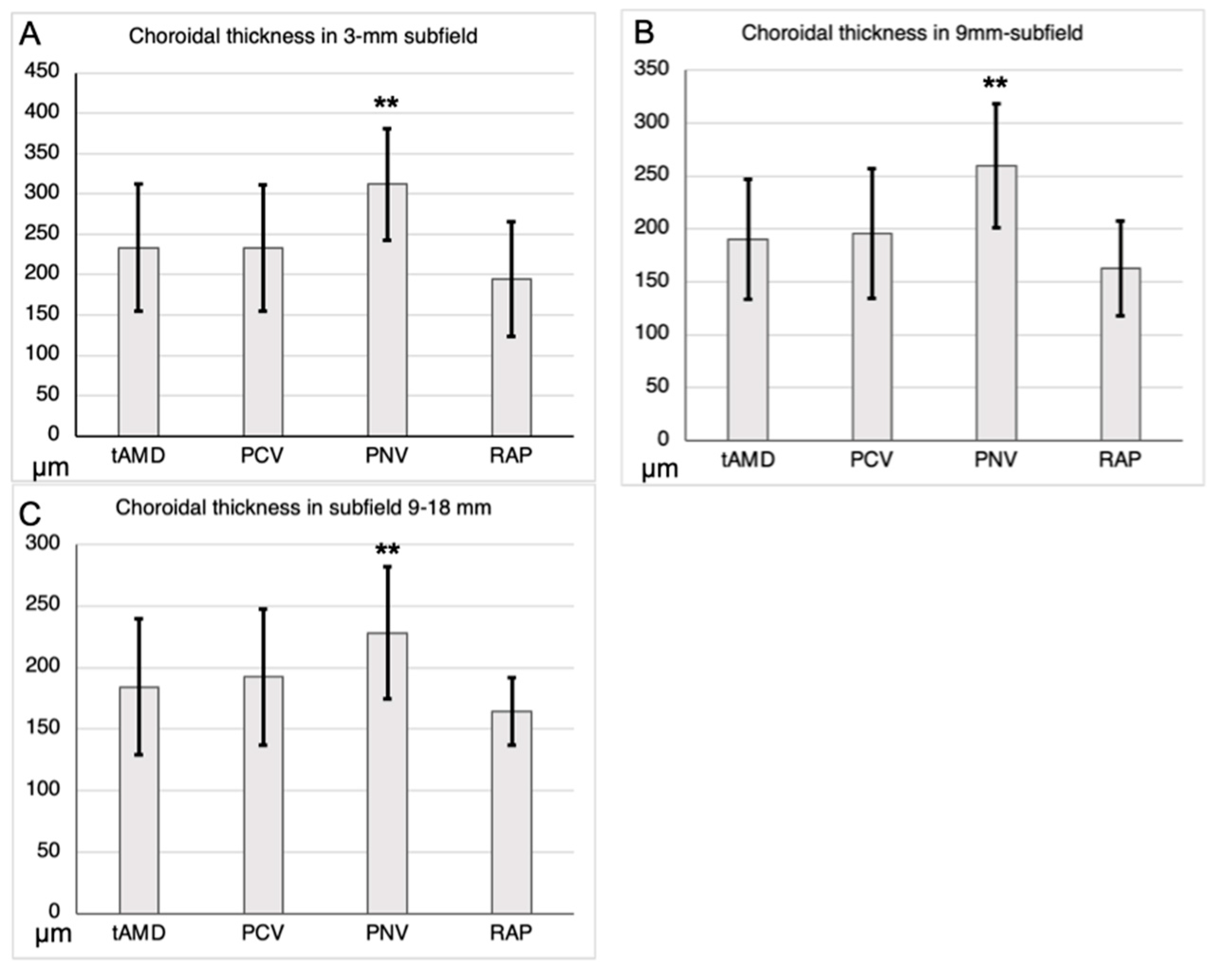
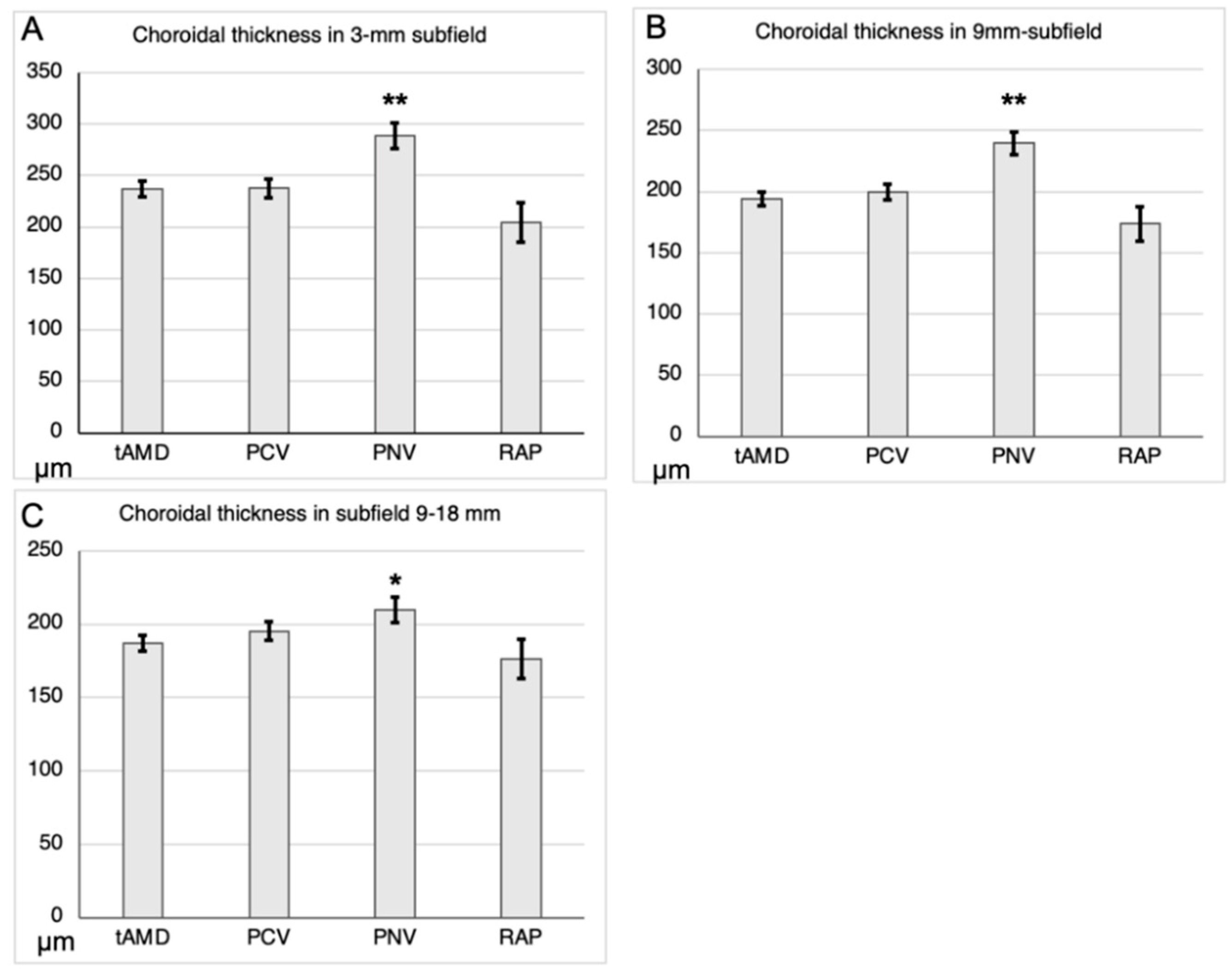
3.2. Choroidal thickness in the central, posterior, and peripheral subfields
3.3. Choroidal thickness adjusted by age and axial length among AMD subtypes
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.; Klein, R.; Cheng, C.Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2014, 2, e106–116. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.; Klein, B.E.; Knudtson, M.D.; Wong, T.Y.; Cotch, M.F.; Liu, K.; Burke, G.; Saad, M.F.; Jacobs, D.R., Jr. Prevalence of age-related macular degeneration in 4 racial/ethnic groups in the multi-ethnic study of atherosclerosis. Ophthalmology 2006, 113, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Coscas, G.; Yamashiro, K.; Coscas, F.; De Benedetto, U.; Tsujikawa, A.; Miyake, M.; Gemmy Cheung, C.M.; Wong, T.Y.; Yoshimura, N. Comparison of exudative age-related macular degeneration subtypes in Japanese and French Patients: multicenter diagnosis with multimodal imaging. Am J Ophthalmol 2014, 158, 309–318.e302. [Google Scholar] [CrossRef]
- Yanagi, Y.; Foo, V.H.X.; Yoshida, A. Asian age-related macular degeneration: from basic science research perspective. Eye (Lond) 2019, 33, 34–49. [Google Scholar] [CrossRef] [PubMed]
- Yanagi, Y. Pachychoroid disease: a new perspective on exudative maculopathy. Jpn J Ophthalmol 2020, 64, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Gallego-Pinazo, R.; Dolz-Marco, R.; Gómez-Ulla, F.; Mrejen, S.; Freund, K.B. Pachychoroid diseases of the macula. Med Hypothesis Discov Innov Ophthalmol 2014, 3, 111–115. [Google Scholar] [PubMed]
- Takahashi, A.; Ooto, S.; Yamashiro, K.; Tamura, H.; Oishi, A.; Miyata, M.; Hata, M.; Yoshikawa, M.; Yoshimura, N.; Tsujikawa, A. Pachychoroid Geographic Atrophy: Clinical and Genetic Characteristics. Ophthalmol Retina 2018, 2, 295–305. [Google Scholar] [CrossRef]
- Pang, C.E.; Freund, K.B. Pachychoroid neovasculopathy. Retina 2015, 35, 1–9. [Google Scholar] [CrossRef]
- Spaide, R.F. DISEASE EXPRESSION IN NONEXUDATIVE AGE-RELATED MACULAR DEGENERATION VARIES WITH CHOROIDAL THICKNESS. Retina 2018, 38, 708–716. [Google Scholar] [CrossRef]
- Hiroe, T.; Kishi, S. Dilatation of Asymmetric Vortex Vein in Central Serous Chorioretinopathy. Ophthalmol Retina 2018, 2, 152–161. [Google Scholar] [CrossRef]
- Shiihara, H.; Sonoda, S.; Terasaki, H.; Kakiuchi, N.; Yamashita, T.; Uchino, E.; Murao, F.; Sano, H.; Mitamura, Y.; Sakamoto, T. Quantitative analyses of diameter and running pattern of choroidal vessels in central serous chorioretinopathy by en face images. Sci Rep 2020, 10, 9591. [Google Scholar] [CrossRef] [PubMed]
- Spaide, R.F.; Gemmy Cheung, C.M.; Matsumoto, H.; Kishi, S.; Boon, C.J.F.; van Dijk, E.H.C.; Mauget-Faysse, M.; Behar-Cohen, F.; Hartnett, M.E.; Sivaprasad, S.; et al. Venous overload choroidopathy: A hypothetical framework for central serous chorioretinopathy and allied disorders. Prog Retin Eye Res 2022, 86, 100973. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.M.G.; Lai, T.Y.Y.; Ruamviboonsuk, P.; Chen, S.J.; Chen, Y.; Freund, K.B.; Gomi, F.; Koh, A.H.; Lee, W.K.; Wong, T.Y. Polypoidal Choroidal Vasculopathy: Definition, Pathogenesis, Diagnosis, and Management. Ophthalmology 2018, 125, 708–724. [Google Scholar] [CrossRef] [PubMed]
- Dansingani, K.K.; Gal-Or, O.; Sadda, S.R.; Yannuzzi, L.A.; Freund, K.B. Understanding aneurysmal type 1 neovascularization (polypoidal choroidal vasculopathy): a lesson in the taxonomy of 'expanded spectra' - a review. Clin Exp Ophthalmol 2018, 46, 189–200. [Google Scholar] [CrossRef]
- Uyama, M.; Wada, M.; Nagai, Y.; Matsubara, T.; Matsunaga, H.; Fukushima, I.; Takahashi, K.; Matsumura, M. Polypoidal choroidal vasculopathy: natural history. Am J Ophthalmol 2002, 133, 639–648. [Google Scholar] [CrossRef]
- Spaide, R.F.; Fisher, Y.L.; Ngo, W.K.; Barbazetto, I. REGIONAL SCLERAL THICKNESS AS A RISK FACTOR FOR CENTRAL SEROUS CHORIORETINOPATHY. Retina 2022, 42, 1231–1237. [Google Scholar] [CrossRef]
- Kishi, S.; Matsumoto, H. A new insight into pachychoroid diseases: Remodeling of choroidal vasculature. Graefes Arch Clin Exp Ophthalmol 2022, 260, 3405–3417. [Google Scholar] [CrossRef]
- Zeng, Q.; Yao, Y.; Tu, S.; Zhao, M. Quantitative analysis of choroidal vasculature in central serous chorioretinopathy using ultra-widefield swept-source optical coherence tomography angiography. Sci Rep 2022, 12, 18427. [Google Scholar] [CrossRef]
- Choma, M.; Sarunic, M.; Yang, C.; Izatt, J. Sensitivity advantage of swept source and Fourier domain optical coherence tomography. Opt Express 2003, 11, 2183–2189. [Google Scholar] [CrossRef]
- Spaide, R.F.; Koizumi, H.; Pozzoni, M.C. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 2008, 146, 496–500. [Google Scholar] [CrossRef]
- Ishikura, M.; Muraoka, Y.; Nishigori, N.; Takahashi, A.; Miyake, M.; Ueda-Arakawa, N.; Miyata, M.; Ooto, S.; Tsujikawa, A. Widefield Choroidal Thickness of Eyes with Central Serous Chorioretinopathy Examined by Swept-Source OCT. Ophthalmol Retina 2022, 6, 949–956. [Google Scholar] [CrossRef]
- Funatsu, R.; Sonoda, S.; Terasaki, H.; Shiihara, H.; Mihara, N.; Horie, J.; Sakamoto, T. Choroidal morphologic features in central serous chorioretinopathy using ultra-widefield optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 2023, 261, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Imanaga, N.; Terao, N.; Nakamine, S.; Tamashiro, T.; Wakugawa, S.; Sawaguchi, K.; Koizumi, H. Scleral Thickness in Central Serous Chorioretinopathy. Ophthalmol Retina 2021, 5, 285–291. [Google Scholar] [CrossRef]
- Matsumoto, H.; Hoshino, J.; Mukai, R.; Nakamura, K.; Kishi, S.; Akiyama, H. Clinical characteristics and pachychoroid incidence in Japanese patients with neovascular age-related macular degeneration. Sci Rep 2022, 12, 4492. [Google Scholar] [CrossRef] [PubMed]
- Shao, L.; Xu, L.; Chen, C.X.; Yang, L.H.; Du, K.F.; Wang, S.; Zhou, J.Q.; Wang, Y.X.; You, Q.S.; Jonas, J.B.; et al. Reproducibility of subfoveal choroidal thickness measurements with enhanced depth imaging by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2013, 54, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Ooto, S.; Hangai, M.; Yoshimura, N. Effects of sex and age on the normal retinal and choroidal structures on optical coherence tomography. Curr Eye Res 2015, 40, 213–225. [Google Scholar] [CrossRef]
- Xie, J.; Ye, L.; Chen, Q.; Shi, Y.; Hu, G.; Yin, Y.; Zou, H.; Zhu, J.; Fan, Y.; He, J.; et al. Choroidal Thickness and Its Association With Age, Axial Length, and Refractive Error in Chinese Adults. Invest Ophthalmol Vis Sci 2022, 63, 34. [Google Scholar] [CrossRef]
- Ying, G.S.; Huang, J.; Maguire, M.G.; Jaffe, G.J.; Grunwald, J.E.; Toth, C.; Daniel, E.; Klein, M.; Pieramici, D.; Wells, J.; et al. Baseline predictors for one-year visual outcomes with ranibizumab or bevacizumab for neovascular age-related macular degeneration. Ophthalmology 2013, 120, 122–129. [Google Scholar] [CrossRef]
- Maguire, M.G.; Martin, D.F.; Ying, G.S.; Jaffe, G.J.; Daniel, E.; Grunwald, J.E.; Toth, C.A.; Ferris, F.L., 3rd; Fine, S.L. Five-Year Outcomes with Anti-Vascular Endothelial Growth Factor Treatment of Neovascular Age-Related Macular Degeneration: The Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology 2016, 123, 1751–1761. [Google Scholar] [CrossRef]
- Ohji, M.; Takahashi, K.; Okada, A.A.; Kobayashi, M.; Matsuda, Y.; Terano, Y. Efficacy and Safety of Intravitreal Aflibercept Treat-and-Extend Regimens in Exudative Age-Related Macular Degeneration: 52- and 96-Week Findings from ALTAIR : A Randomized Controlled Trial. Adv Ther 2020, 37, 1173–1187. [Google Scholar] [CrossRef]
- Maruyama-Inoue, M.; Yamane, S.; Satoh, H.; Sato, S.; Kadonosono, K. Choroidal angioarchitecture according to ultra-widefield indocyanine green angiography in age-related macular degeneration. Journal of VitreoRetinal Diseases 2017, 1, 365–371. [Google Scholar] [CrossRef]
- Matsumoto, H.; Hoshino, J.; Mukai, R.; Nakamura, K.; Kikuchi, Y.; Kishi, S.; Akiyama, H. Vortex Vein Anastomosis at the Watershed in Pachychoroid Spectrum Diseases. Ophthalmol Retina 2020, 4, 938–945. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, T.; Koizumi, H.; Yamagishi, T.; Kinoshita, S. Subfoveal choroidal thickness in retinal angiomatous proliferation. Retina 2014, 34, 1316–1322. [Google Scholar] [CrossRef]
- Kuranami, A.; Maruko, R.; Maruko, I.; Hasegawa, T.; Iida, T. Pachychoroid neovasculopathy has clinical properties that differ from conventional neovascular age-related macular degeneration. Sci Rep 2023, 13, 7379. [Google Scholar] [CrossRef] [PubMed]
- Izumi, T.; Maruko, I.; Kawano, T.; Sakaihara, M.; Iida, T. Morphological differences of choroid in central serous chorioretinopathy determined by ultra-widefield optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 2022, 260, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Nishihara, S.; Maruko, I.; Izumi, T.; Kawano, T.; Iida, T. PERIPHERAL CHOROIDAL THICKNESS DETERMINED BY WIDE-FIELD OPTICAL COHERENCE TOMOGRAPHY IN EYES WITH CENTRAL SEROUS CHORIORETINOPATHY. Retina 2022, 42, 1450–1454. [Google Scholar] [CrossRef]
- Funatsu, R.; Sonoda, S.; Terasaki, H.; Shiihara, H.; Mihara, N.; Horie, J.; Sakamoto, T. NORMAL PERIPHERAL CHOROIDAL THICKNESS MEASURED BY WIDEFIELD OPTICAL COHERENCE TOMOGRAPHY. Retina 2023, 43, 490–497. [Google Scholar] [CrossRef]
- Kakiuchi, N.; Terasaki, H.; Sonoda, S.; Shiihara, H.; Yamashita, T.; Tomita, M.; Shinohara, Y.; Sakoguchi, T.; Iwata, K.; Sakamoto, T. Regional Differences of Choroidal Structure Determined by Wide-Field Optical Coherence Tomography. Invest Ophthalmol Vis Sci 2019, 60, 2614–2622. [Google Scholar] [CrossRef]
- Tan, C.S.; Cheong, K.X.; Lim, L.W.; Li, K.Z. Topographic variation of choroidal and retinal thicknesses at the macula in healthy adults. Br J Ophthalmol 2014, 98, 339–344. [Google Scholar] [CrossRef]
- Kinoshita, T.; Mitamura, Y.; Shinomiya, K.; Egawa, M.; Iwata, A.; Fujihara, A.; Ogushi, Y.; Semba, K.; Akaiwa, K.; Uchino, E.; et al. Diurnal variations in luminal and stromal areas of choroid in normal eyes. Br J Ophthalmol 2017, 101, 360–364. [Google Scholar] [CrossRef]
- Yamashiro, K.; Yanagi, Y.; Koizumi, H.; Matsumoto, H.; Cheung, C.M.G.; Gomi, F.; Iida, T.; Tsujikawa, A. Relationship between Pachychoroid and Polypoidal Choroidal Vasculopathy. J Clin Med 2022, 11. [Google Scholar] [CrossRef] [PubMed]
| tAMD | PCV | PNV | RAP | P-value | |
| N | 75 | 54 | 29 | 12 | |
| Female, n (%) | 20 (26.7%) | 18 (33.3%) | 10 (34.5%) | 7 (58.3%) | NS |
| Age (y) | 73.4 ± 10.4 | 73.6 ± 8.9 | 67.1 ± 12.4 | 78.3 ± 6.7 | 1.00, 0.01, 0.30 |
| Axial length (mm) | 24.7 ± 1.8 | 24.7 ± 1.2 | 24.3 ± 1.1 | 24.3 ± 1.1 | 1.00, 0.60, 0.72 |
| Correlation coefficient | P-value | |||
| Subfield | ||||
| < 3 mm | < 9 mm | 9-18 mm | ||
| Sex | -0.07 | -0.06 | 0.02 | 0.50, 0.45, 0.88 |
| Age | -0.36 | -0.42 | -0.47 | <0.01, <0.01, <0.01 |
| Axial length | -0.28 | -0.26 | -0.18 | <0.01, <0.01, 0.03 |
| tAMD | PCV | PNV | RAP | |
| Ratio of <9mm to 9-18mm choroidal thickness | 1.04 ± 0.15 | 1.02 ± 0.16 | 1.15 ± 0.13 | 0.98 ± 0.16 |
| P-value | 0.82 | < 0.01 | 0.53 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





