Submitted:
05 August 2023
Posted:
07 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. ECM: A Key Player for TE
2.1. ECM Structure
2.2. ECM components
2.3. Cellular Adhesion to the ECM
3. Exploring ECM Biophysical and Biochemical Properties for Enhanced TE
3.1. ECM Biophysical Properties
3.2. ECM Biochemical Properties
4. Modulation of Cell Fate by Cell-Biomaterial Interactions
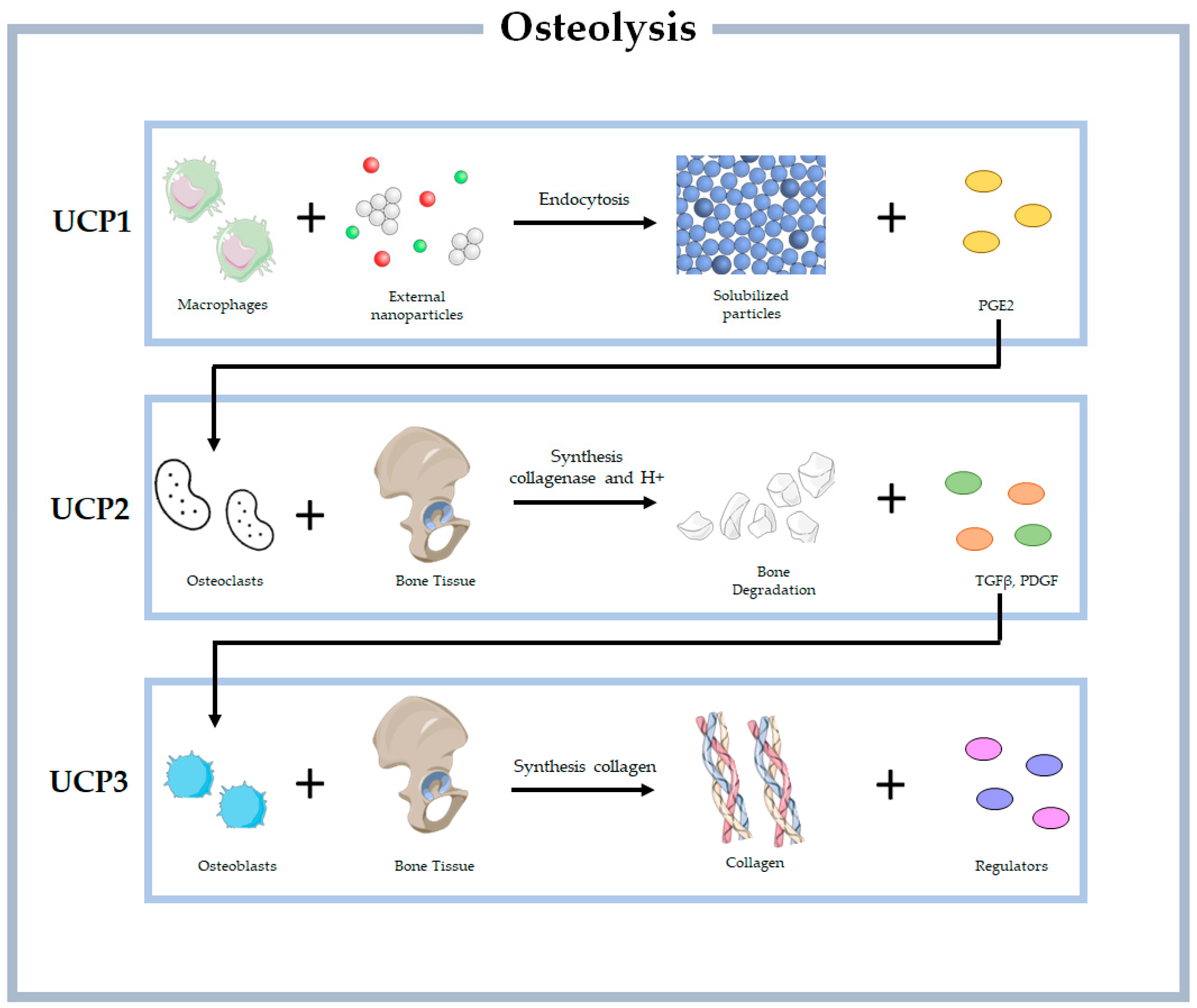
4.1. Unit Cell Process
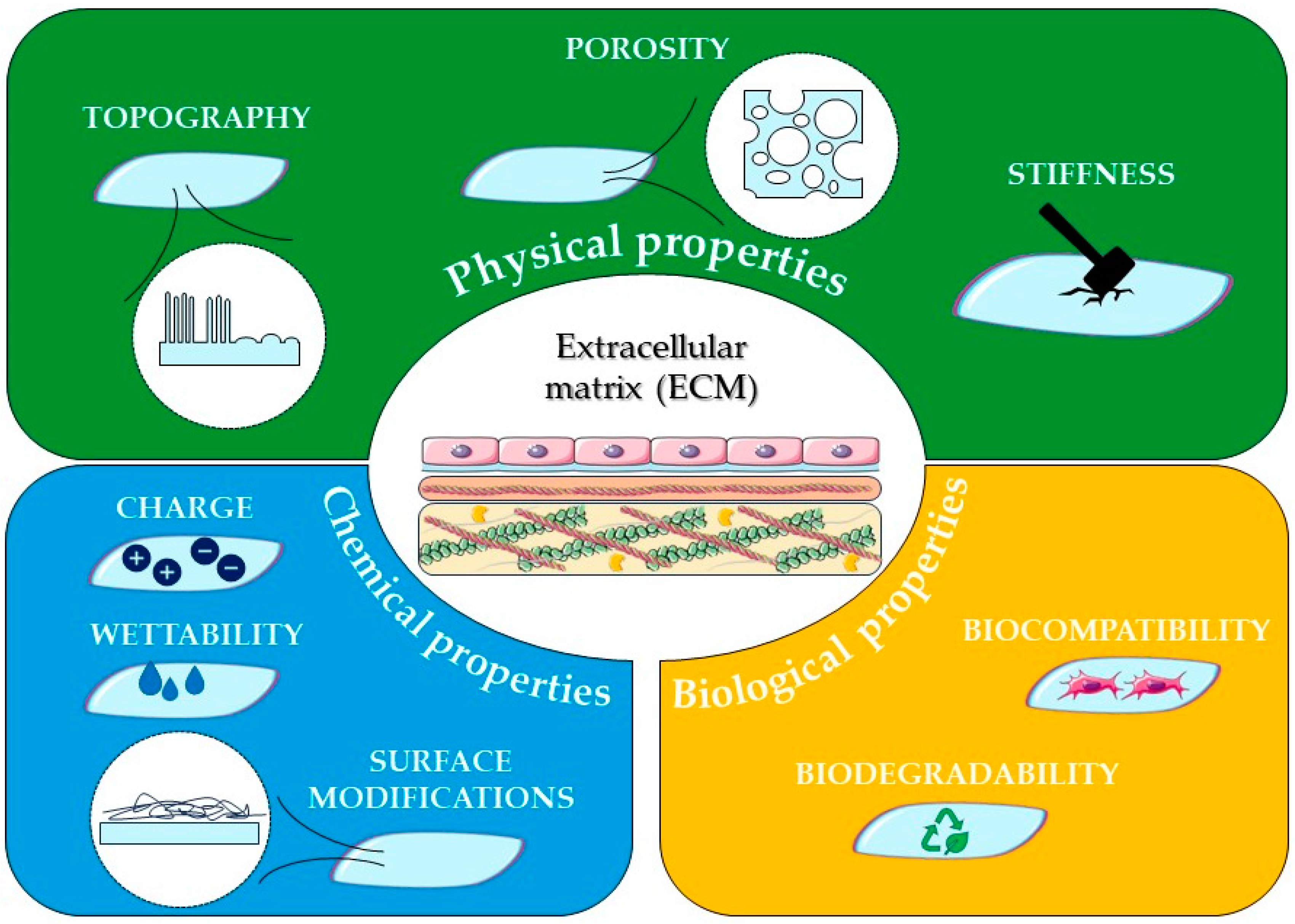
4.2. Biomaterials Physical Properties in TE
4.2.1. Orientation and Porosity
4.2.2. Topography
4.2.3. Stiffness
4.3. Biomaterials Biochemical Properties in TE
| Surface Modification Techniques | Materials | Cell Responses | References |
|---|---|---|---|
| Layer-by-layer assembly | HP and CS-coated PU/DCS scaffolds | Promoted cell attachment and proliferation of endothelial progenitor cells and long in vitro coagulation time and high resistance to platelet adhesion. | [113] |
| BP-NS/CS composite-coated PEEK scaffolds | Enhanced biocompatibility and osteogenesis-associated gene expression. | [114] | |
| HP/Collagen encapsulating NGF coated on PLLA scaffolds | Promoted and directed SCs growth as well as induced the differentiation of PC12 cells and neurite growth along the nanofibrous alignment. | [115] | |
| Nanoparticle assembly | Au NPs on PLGA nanofibrous sheet | Enhanced the osteogenic differentiation of human adipose-derived stem cells and biocompatibility. | [116] |
| PDA NPs on TCP scaffolds | Demonstrated excellent osteoinductivity and bone-regeneration performance. | [117] | |
| SF NPs on PLLA scaffolds | Excellent adhesion, proliferation, and osteogenic differentiation on MC3T3-E1 cells and induced a higher level of osteoblast-specific markers. | [118] | |
| Electrospinning | Core-shell SF/PCL/PVA nanofibrous with CTGF and BMP2 | Excellent improvement in vessel formation and bone tissue recovery and pro-angiogenic effect on bone healing. | [119] |
| PCL/PDS scaffolds | Improved hydrophilicity, a significant increase in proliferation of HUVECs, faster cellularization, and better vascularization. | [120] | |
| PCL/GLA nanofibrous with WS NPs | Showed excellent viability, growth, and proliferation of ASCs. | [121] | |
| UV treatment | GLA nanofibrous scaffolds | Promoted adhesion and proliferation of HaCaT, without causing apparent cytotoxicity and induced a rapid cell migration close to 79% of an artificial wound within 24 h. | [122] |
| PVP-PGS blend fibres | Exhibited good viability and proliferation of human dermal fibroblast cells. | [123] | |
| PV-Ci nanofibers modified with laminin peptides | Enhanced neural adhesion, outgrowth, and regeneration. | [124] | |
| Laser treatment | PLGA- Collagen hybrid constructs | Exhibited good adhesion, and proliferation on HCECs and HKs and maintained their respective phenotypes well. HCECs could form multilayers. | [125] |
| nHA loaded core-shell PCL/PCL and PCL/PVAc nanofibrous scaffolds | Showed high viability, very low mortality, and improved human osteoblast adhesion and proliferation. | [126] | |
| Plasma treatment | PCL nanofibres treated with argon plasma | Enhanced metabolic activity, adhesion, and proliferation of ADSCs. | [127] |
| PLLA/Baghdadite scaffold treated with oxygen plasma | Induced osteogenesis-related genes and enhanced osteogenic differentiation of AD-MSCs. | [128] | |
| PCL/GLA nanofibers treated with cold atmosphere plasma | Improved cell affinity, growth adhesion, and proliferation of MSCs. | [129] | |
| Cross-linked assisted adsorption | PCL/GAGs Scaffolds (EDC/NHS) | Improved adhesion, proliferation, and differentiation of SCs. | [130] |
| Keratin/PEO/nHa nanofibrous membrane (EGDE) | Enhanced the proliferation of L929 cell, hence exhibited an advantage in reducing inflammatory response in the infective stage and enhancing skin repairing process in the following recover stages. | [131] | |
| PCL/GLA/FG scaffolds (GA) | Enhanced hCB-ECs growth and improved maintenance of their EC phenotype in vitro. | [132] | |
| Wet chemical techniques | PCL nanofibres (Hydrolysis-NaOH) | Improved protein adsorption and attachment, viability and elongation of 3T3 fibroblasts. | [133] |
| PCL/Maltose nanofibres | Showed higher proliferation and better morphology of the HUF cells. | [134] | |
| PAN/Fibrin (Hydrolysis-NaOH) | Increased adhesion and proliferation of HUVECs and promoted endothelialization. | [135] | |
| Molecular imprinting | GLA/nHA scaffolds | Promoted osteogenesis of hMSCs and induced the formation of a stable vascular network in the HUVEC-laden hydrogel. | [136] |
| Peptide imprinted Alg/GLA/Ela sponges | Improved cardiac progenitor cell adhesion and differentiation toward myocardial phenotypes. | [137] | |
| tenocyte imprinted PDMS | Induced significant tenogenic differentiation on ADSCs. | [138] | |
| Click chemistry | CM-2 immobilized HA hydrogel | Enhanced chondrogenic differentiation of hPLSCs. | [139] |
| HEC/CA scaffolds | Improved biocompatibility, chondrogenic ability and potential for cartilage repair and regeneration. | [140] | |
| Gellan hydrogels | Promoted MSCs adhesion and metabolic activity. | [141] |
4.3.1. Surface Reactive Functional Groups
4.3.2. Surface Charge
4.3.3. Surface Wettability
4.4. Biological Characteristics of Biomaterial Surface
4.4.1. Functionalization with Biomolecules
4.4.2 Biocompatibility
4.4.3. Biodegradability
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- statista. Available online: URL https://www.statista.com/statistics/808471/organ-transplantation-costs-us/ (accessed on 23 July 2023).
- Niklason, L.E.; Langer, R. Prospects for Organ and Tissue Replacement. JAMA 2001, 285, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Muzzio, N.; Moya, S.; Romero, G. Multifunctional Scaffolds and Synergistic Strategies in Tissue Engineering and Regenerative Medicine. Pharmaceutics 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Frantz, C.; Stewart, K.M.; Weaver, V.M. The extracellular matrix at a glance. Journal of Cell Science 2010, 123, 4195–4200. [Google Scholar] [CrossRef]
- Han, W.M.; Jang, Y.C.; García, A.J. The Extracellular Matrix and Cell–Biomaterial Interactions. In Biomaterials Science; Elsevier, 2020; pp. 701–715. [Google Scholar]
- Masters, K.S.; Anseth, K.S. CELL–MATERIAL INTERACTIONS. In Advances in Chemical Engineering; Elsevier, 2004; Volume 29, pp. 7–46. [Google Scholar]
- Jia, X.; Chen, J.; Lv, W.; Li, H.; Ariga, K. Engineering dynamic and interactive biomaterials using material nanoarchitectonics for modulation of cellular behaviors. Cell Reports Physical Science 2023, 4, 101251. [Google Scholar] [CrossRef]
- Friuli, M.; Nitti, P.; Cafuero, L.; Prete, A.; Zafar, M.S.; Madaghiele, M.; Demitri, C. Cellulose Acetate and Cardanol Based Seed Coating for Intraspecific Weeding Coupled with Natural Herbicide Spraying. Journal of Polymers and the Environment 2020, 28, 2893–2904. [Google Scholar] [CrossRef]
- Gonçalves, S.; Dourado, F.; Rodrigues, L.R. Overview on Cell-Biomaterial Interactions. In Advanced Polymers in Medicine, Puoci, F., Ed.; Springer International Publishing: Cham, 2015; pp. 91–128. [Google Scholar]
- Amani, H.; Arzaghi, H.; Bayandori, M.; Dezfuli, A.S.; Pazoki-Toroudi, H.; Shafiee, A.; Moradi, L. Controlling cell behavior through the design of biomaterial surfaces: a focus on surface modification techniques. Advanced materials interfaces 2019, 6, 1900572. [Google Scholar] [CrossRef]
- Karamanos, N.K.; Theocharis, A.D.; Piperigkou, Z.; Manou, D.; Passi, A.; Skandalis, S.S.; Vynios, D.H.; Orian-Rousseau, V.; Ricard-Blum, S.; Schmelzer, C.E.H.; et al. A guide to the composition and functions of the extracellular matrix. The FEBS Journal 2021, 288, 6850–6912. [Google Scholar] [CrossRef]
- Theocharis, A.D.; Skandalis, S.S.; Gialeli, C.; Karamanos, N.K. Extracellular matrix structure. Advanced Drug Delivery Reviews 2016, 97, 4–27. [Google Scholar] [CrossRef]
- Kular, J.K.; Basu, S.; Sharma, R.I. The extracellular matrix: Structure, composition, age-related differences, tools for analysis and applications for tissue engineering. Journal of Tissue Engineering 2014, 5, 204173141455711. [Google Scholar] [CrossRef]
- LeBleu, V.S.; MacDonald, B.; Kalluri, R. Structure and Function of Basement Membranes. Experimental Biology and Medicine 2007, 232, 1121–1129. [Google Scholar] [CrossRef]
- M, M.P. Basement Membrane Proteins: Structure, Assembly, and Cellular Interactions. Critical Reviews in Biochemistry and Molecular Biology 1992, 27, 93–127. [Google Scholar] [CrossRef] [PubMed]
- Theocharis, A.D.; Manou, D.; Karamanos, N.K. The extracellular matrix as a multitasking player in disease. The FEBS Journal 2019, 286, 2830–2869. [Google Scholar] [CrossRef] [PubMed]
- Yeung, D.A.; Kelly, N.H. The Role of Collagen-Based Biomaterials in Chronic Wound Healing and Sports Medicine Applications. Bioengineering 2021, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Elango, J.; Zamora-Ledezma, C.; Ge, B.; Hou, C.; Pan, Z.; Bao, B.; Pérez Albacete Martínez, C.; Granero Marín, J.M.; De Val, J.E.M.S.; Bao, C.; et al. Paradoxical Duel Role of Collagen in Rheumatoid Arthritis: Cause of Inflammation and Treatment. Bioengineering 2022, 9, 321. [Google Scholar] [CrossRef]
- Tanzer, M.L. Current concepts of extracellular matrix. Journal of Orthopaedic Science 2006, 11, 326–331. [Google Scholar] [CrossRef]
- Burgos-Panadero, R.; Noguera, I.; Cañete, A.; Navarro, S.; Noguera, R. Vitronectin as a molecular player of the tumor microenvironment in neuroblastoma. BMC Cancer 2019, 19, 479. [Google Scholar] [CrossRef]
- Ruzha, Y.; Ni, J.; Quan, Z.; Li, H.; Qing, H. Role of Vitronectin and Its Receptors in Neuronal Function and Neurodegenerative Diseases. International Journal of Molecular Sciences 2022, 23, 12387. [Google Scholar] [CrossRef]
- Heldin, C.-H.; Moustakas, A. Signaling Receptors for TGF-β Family Members. Cold Spring Harbor Perspectives in Biology 2016, 8, a022053. [Google Scholar] [CrossRef]
- Tzavlaki, K.; Moustakas, A. TGF-β Signaling. Biomolecules 2020, 10, 487. [Google Scholar] [CrossRef]
- Chaudhury, A.; Howe, P.H. The tale of transforming growth factor-beta (TGFβ) signaling: A soigné enigma. IUBMB Life 2009, 61, 929–939. [Google Scholar] [CrossRef]
- Gubbiotti, M.A.; Vallet, S.D.; Ricard-Blum, S.; Iozzo, R.V. Decorin interacting network: A comprehensive analysis of decorin-binding partners and their versatile functions. Matrix Biology 2016, 55, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Sainio, A.; Järveläinen, H. Extracellular matrix-cell interactions: Focus on therapeutic applications. Cellular Signalling 2020, 66, 109487. [Google Scholar] [CrossRef] [PubMed]
- Kadry, Y.A.; Calderwood, D.A. Chapter 22: Structural and signaling functions of integrins. Biochimica et Biophysica Acta (BBA) - Biomembranes 2020, 1862, 183206. [Google Scholar] [CrossRef] [PubMed]
- Bachmann, M.; Kukkurainen, S.; Hytönen, V.P.; Wehrle-Haller, B. Cell Adhesion by Integrins. Physiological Reviews 2019, 99, 1655–1699. [Google Scholar] [CrossRef] [PubMed]
- Tsuruta, D.; Hashimoto, T.; Hamill, K.J.; Jones, J.C.R. Hemidesmosomes and focal contact proteins: Functions and cross-talk in keratinocytes, bullous diseases and wound healing. Journal of Dermatological Science 2011, S0923181111000260. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Raynal, N.; Stathopoulos, S.; Myllyharju, J.; Farndale, R.W.; Leitinger, B. Collagen binding specificity of the discoidin domain receptors: Binding sites on collagens II and III and molecular determinants for collagen IV recognition by DDR1. Matrix Biology 2011, 30, 16–26. [Google Scholar] [CrossRef]
- Weng, X.; Maxwell-Warburton, S.; Hasib, A.; Ma, L.; Kang, L. The membrane receptor CD44: novel insights into metabolism. Trends in Endocrinology & Metabolism 2022, 33, 318–332. [Google Scholar] [CrossRef]
- Chaudhry, G.-e.-S.; Akim, A.; Naveed Zafar, M.; Safdar, N.; Sung, Y.Y.; Muhammad, T.S.T. Understanding Hyaluronan Receptor (CD44) Interaction, HA-CD44 Activated Potential Targets in Cancer Therapeutics. Advanced Pharmaceutical Bulletin 2020, 11, 426–438. [Google Scholar] [CrossRef]
- Gopal, S.; Arokiasamy, S.; Pataki, C.; Whiteford, J.R.; Couchman, J.R. Syndecan receptors: pericellular regulators in development and inflammatory disease. Open Biology 2021, 11, 200377. [Google Scholar] [CrossRef]
- Muiznieks, L.D.; Keeley, F.W. Molecular assembly and mechanical properties of the extracellular matrix: A fibrous protein perspective. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 2013, 1832, 866–875. [Google Scholar] [CrossRef]
- Gosline, J.; Lillie, M.; Carrington, E.; Guerette, P.; Ortlepp, C.; Savage, K. Elastic proteins: biological roles and mechanical properties. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences 2002, 357, 121–132. [Google Scholar] [CrossRef]
- Silver, F.H.; Freeman, J.W.; Seehra, G.P. Collagen self-assembly and the development of tendon mechanical properties. Journal of Biomechanics 2003, 36, 1529–1553. [Google Scholar] [CrossRef] [PubMed]
- Aitken, K.J.; Bägli, D.J. The bladder extracellular matrix. Part I: architecture, development and disease. Nature Reviews Urology 2009, 6, 596–611. [Google Scholar] [CrossRef] [PubMed]
- Elosegui-Artola, A. The extracellular matrix viscoelasticity as a regulator of cell and tissue dynamics. Current Opinion in Cell Biology 2021, 72, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Ge, H.; Tian, M.; Pei, Q.; Tan, F.; Pei, H. Extracellular Matrix Stiffness: New Areas Affecting Cell Metabolism. Frontiers in Oncology 2021, 11, 631991. [Google Scholar] [CrossRef]
- Yokota, T.; McCourt, J.; Ma, F.; Ren, S.; Li, S.; Kim, T.-H.; Kurmangaliyev, Y.Z.; Nasiri, R.; Ahadian, S.; Nguyen, T.; et al. Type V Collagen in Scar Tissue Regulates the Size of Scar after Heart Injury. Cell 2020, 182, 545–562. [Google Scholar] [CrossRef]
- Gkretsi, V.; Stylianopoulos, T. Cell Adhesion and Matrix Stiffness: Coordinating Cancer Cell Invasion and Metastasis. Frontiers in Oncology 2018, 8, 145. [Google Scholar] [CrossRef]
- Chaudhuri, O.; Koshy, S.T.; Branco Da Cunha, C.; Shin, J.-W.; Verbeke, C.S.; Allison, K.H.; Mooney, D.J. Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nature Materials 2014, 13, 970–978. [Google Scholar] [CrossRef]
- Lo, C.-M.; Wang, H.-B.; Dembo, M.; Wang, Y.-l. Cell Movement Is Guided by the Rigidity of the Substrate. Biophysical Journal 2000, 79, 144–152. [Google Scholar] [CrossRef]
- Miklavčič, D.; Pavšelj, N.; Hart, F.X. Electric Properties of Tissues. In Wiley Encyclopedia of Biomedical Engineering, Akay, M., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006. [Google Scholar]
- Vining, K.H.; Mooney, D.J. Mechanical forces direct stem cell behaviour in development and regeneration. Nature Reviews Molecular Cell Biology 2017, 18, 728–742. [Google Scholar] [CrossRef]
- Lou, J.; Stowers, R.; Nam, S.; Xia, Y.; Chaudhuri, O. Stress relaxing hyaluronic acid-collagen hydrogels promote cell spreading, fiber remodeling, and focal adhesion formation in 3D cell culture. Biomaterials 2018, 154, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, O.; Cooper-White, J.; Janmey, P.A.; Mooney, D.J.; Shenoy, V.B. Effects of extracellular matrix viscoelasticity on cellular behaviour. Nature 2020, 584, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Doyle, A.D.; Nazari, S.S.; Yamada, K.M. Cell–extracellular matrix dynamics. Physical Biology 2022, 19, 021002. [Google Scholar] [CrossRef]
- Janson, I.A.; Putnam, A.J. Extracellular matrix elasticity and topography: Material-based cues that affect cell function via conserved mechanisms: ECM ELASTICITY AND TOPOGRAPHY. Journal of Biomedical Materials Research Part A 2015, 103, 1246–1258. [Google Scholar] [CrossRef] [PubMed]
- Wolf, K.; Friedl, P. Extracellular matrix determinants of proteolytic and non-proteolytic cell migration. Trends in Cell Biology 2011, 21, 736–744. [Google Scholar] [CrossRef]
- Resende, R.R.; Fonseca, E.A.; Tonelli, F.M.P.; Sousa, B.R.; Santos, A.K.; Gomes, K.N.; Guatimosim, S.; Kihara, A.H.; Ladeira, L.O. Scale/Topography of Substrates Surface Resembling Extracellular Matrix for Tissue Engineering. Journal of Biomedical Nanotechnology 2014, 10, 1157–1193. [Google Scholar] [CrossRef]
- Gupton, S.L.; Waterman-Storer, C.M. Spatiotemporal feedback between actomyosin and focal-adhesion systems optimizes rapid cell migration. Cell 2006, 125, 1361–1374. [Google Scholar] [CrossRef]
- Baei, P.; Hosseini, M.; Baharvand, H.; Pahlavan, S. Electrically conductive materials for in vitro cardiac microtissue engineering. Journal of Biomedical Materials Research Part A 2020, 108, 1203–1213. [Google Scholar] [CrossRef]
- Girigoswami, K.; Saini, D.; Girigoswami, A. Extracellular Matrix Remodeling and Development of Cancer. Stem Cell Reviews and Reports 2021, 17, 739–747. [Google Scholar] [CrossRef]
- Ortiz, C.; Schierwagen, R.; Schaefer, L.; Klein, S.; Trepat, X.; Trebicka, J. Extracellular Matrix Remodeling in Chronic Liver Disease. Current Tissue Microenvironment Reports 2021, 2, 41–52. [Google Scholar] [CrossRef]
- Ruiz, O.; Méndez, G.; Aguilera; Plaza, D. Extracellular Matrix Remodeling of Adipose Tissue in Obesity and Metabolic Diseases. International Journal of Molecular Sciences 2019, 20, 4888. [CrossRef] [PubMed]
- Najafi, M.; Farhood, B.; Mortezaee, K. Extracellular matrix (ECM) stiffness and degradation as cancer drivers. Journal of Cellular Biochemistry 2019, 120, 2782–2790. [Google Scholar] [CrossRef] [PubMed]
- Cabral-Pacheco, G.A.; Garza-Veloz, I.; Castruita-De La Rosa, C.; Ramirez-Acuña, J.M.; Perez-Romero, B.A.; Guerrero-Rodriguez, J.F.; Martinez-Avila, N.; Martinez-Fierro, M.L. The Roles of Matrix Metalloproteinases and Their Inhibitors in Human Diseases. International Journal of Molecular Sciences 2020, 21, 9739. [Google Scholar] [CrossRef] [PubMed]
- Bassiouni, W.; Ali, M.A.M.; Schulz, R. Multifunctional intracellular matrix metalloproteinases: implications in disease. The FEBS Journal 2021, 288, 7162–7182. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, I. Antibiofilm Activity of Biocide Metal Ions Containing Bioactive Glasses (BGs): A Mini Review. Bioengineering 2022, 9, 489. [Google Scholar] [CrossRef]
- Xu, J.; Ma, S.; Zheng, H.; Pang, B.; Li, S.; Li, F.; Feng, L.; Tian, J. Biomanufacturing Biotinylated Magnetic Nanomaterial via Construction and Fermentation of Genetically Engineered Magnetotactic Bacteria. Bioengineering 2022, 9, 356. [Google Scholar] [CrossRef]
- Kang, M.; Lee, C.-S.; Lee, M. Bioactive Scaffolds Integrated with Liposomal or Extracellular Vesicles for Bone Regeneration. Bioengineering 2021, 8, 137. [Google Scholar] [CrossRef]
- McFerran, A.; McIvor, M.J.; Lemoine, P.; Meenan, B.J.; Acheson, J.G. Biocompatible Nanocomposite Coatings Deposited via Layer-by-Layer Assembly for the Mechanical Reinforcement of Highly Porous Interconnected Tissue-Engineered Scaffolds. Bioengineering 2022, 9, 585. [Google Scholar] [CrossRef]
- Nadra, M.; Niu, W.; Kurisawa, M.; Rousson, D.; Spector, M. Platelet-Rich Plasma Lysate-Incorporating Gelatin Hydrogel as a Scaffold for Bone Reconstruction. Bioengineering 2022, 9, 513. [Google Scholar] [CrossRef]
- Olson, L.C.; Redden, J.T.; Gilliam, L.; Nguyen, T.M.; Vossen, J.A.; Cohen, D.J.; Schwartz, Z.; McClure, M.J. Human Adipose-Derived Stromal Cells Delivered on Decellularized Muscle Improve Muscle Regeneration and Regulate RAGE and P38 MAPK. Bioengineering 2022, 9, 426. [Google Scholar] [CrossRef]
- Somers, S.M.; Gilbert-Honick, J.; Choi, I.Y.; K. W. Lo, E.; Lim, H.; Dias, S.; Wagner, K.R.; Mao, H.-Q.; Cahan, P.; Lee, G.; et al. Engineering Skeletal Muscle Grafts with PAX7::GFP-Sorted Human Pluripotent Stem Cell-Derived Myogenic Progenitors on Fibrin Microfiber Bundles for Tissue Regeneration. Bioengineering 2022, 9, 693. [CrossRef]
- Ramos-Rodriguez, D.H.; MacNeil, S.; Claeyssens, F.; Ortega Asencio, I. Delivery of Bioactive Compounds to Improve Skin Cell Responses on Microfabricated Electrospun Microenvironments. Bioengineering 2021, 8, 105. [Google Scholar] [CrossRef] [PubMed]
- Veerasubramanian, P.K.; Joe, V.C.; Liu, W.F.; Downing, T.L. Characterization of Macrophage and Cytokine Interactions with Biomaterials Used in Negative-Pressure Wound Therapy. Bioengineering 2021, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- Winnacker, M.; Beringer, A.J.G.; Gronauer, T.F.; Güngör, H.H.; Reinschlüssel, L.; Rieger, B.; Sieber, S.A. Polyamide/PEG Blends as Biocompatible Biomaterials for the Convenient Regulation of Cell Adhesion and Growth. Macromolecular Rapid Communications 2019, 40, 1900091. [Google Scholar] [CrossRef]
- Malcor, J.-D.; Mallein-Gerin, F. Biomaterial functionalization with triple-helical peptides for tissue engineering. Acta Biomaterialia 2022, 148, 1–21. [Google Scholar] [CrossRef]
- Zhu, Y.; Stark, C.J.; Madira, S.; Ethiraj, S.; Venkatesh, A.; Anilkumar, S.; Jung, J.; Lee, S.; Wu, C.A.; Walsh, S.K.; et al. Three-Dimensional Bioprinting with Alginate by Freeform Reversible Embedding of Suspended Hydrogels with Tunable Physical Properties and Cell Proliferation. Bioengineering 2022, 9, 807. [Google Scholar] [CrossRef]
- Soleas, J.P.; Huang, L.; D’Arcangelo, E.; Nostro, M.C.; Waddell, T.K.; McGuigan, A.P.; Karoubi, G. Guided Self-Assembly of ES-Derived Lung Progenitors into Biomimetic Tube Structures That Impact Cell Differentiation. Bioengineering 2021, 8, 209. [Google Scholar] [CrossRef] [PubMed]
- Mou, X.; Shah, J.; Bhattacharya, R.; Kalejaiye, T.D.; Sun, B.; Hsu, P.-C.; Musah, S. A Biomimetic Electrospun Membrane Supports the Differentiation and Maturation of Kidney Epithelium from Human Stem Cells. Bioengineering 2022, 9, 188. [Google Scholar] [CrossRef]
- Parisi, L.; Toffoli, A.; Bianchi, M.G.; Bergonzi, C.; Bianchera, A.; Bettini, R.; Elviri, L.; Macaluso, G.M. Functional Fibronectin Adsorption on Aptamer-Doped Chitosan Modulates Cell Morphology by Integrin-Mediated Pathway. Materials 2019, 12, 812. [Google Scholar] [CrossRef]
- Suter, N.; Stebel, S.; Rianna, C.; Radmacher, M.; Brüggemann, D. Spatial patterning of nanofibrous collagen scaffolds modulates fibroblast morphology. Biofabrication 2021, 13, 015007. [Google Scholar] [CrossRef]
- Ben Messaoud, G.; Aveic, S.; Wachendoerfer, M.; Fischer, H.; Richtering, W. 3D Printable Gelatin Methacryloyl (GelMA)-Dextran Aqueous Two-Phase System with Tunable Pores Structure and Size Enables Physiological Behavior of Embedded Cells In Vitro. Small 2023, 2208089. [Google Scholar] [CrossRef] [PubMed]
- Mungenast, L.; Nieminen, R.; Gaiser, C.; Faia-Torres, A.B.; Rühe, J.; Suter-Dick, L. Electrospun decellularized extracellular matrix scaffolds promote the regeneration of injured neurons. Biomaterials and Biosystems 2023, 11, 100081. [Google Scholar] [CrossRef] [PubMed]
- Man, K.; Brunet, M.Y.; Federici, A.S.; Hoey, D.A.; Cox, S.C. An ECM-Mimetic Hydrogel to Promote the Therapeutic Efficacy of Osteoblast-Derived Extracellular Vesicles for Bone Regeneration. Frontiers in Bioengineering and Biotechnology 2022, 10, 829969. [Google Scholar] [CrossRef] [PubMed]
- Lavrador, P.; Gaspar, V.M.; Mano, J.F. Mechanochemical Patternable ECM-Mimetic Hydrogels for Programmed Cell Orientation. Advanced Healthcare Materials 2020, 9, 1901860. [Google Scholar] [CrossRef]
- Eltom, A.; Zhong, G.; Muhammad, A. Scaffold Techniques and Designs in Tissue Engineering Functions and Purposes: A Review. Advances in Materials Science and Engineering 2019, 2019, 3429527. [Google Scholar] [CrossRef]
- Echeverria Molina, M.I.; Malollari, K.G.; Komvopoulos, K. Design Challenges in Polymeric Scaffolds for Tissue Engineering. Frontiers in Bioengineering and Biotechnology 2021, 9. [Google Scholar] [CrossRef]
- Chen, G.; Ushida, T.; Tateishi, T. Scaffold Design for Tissue Engineering. Macromolecular Bioscience 2002, 2, 67–77. [Google Scholar] [CrossRef]
- Shattil, S.J.; Newman, P.J. Integrins: dynamic scaffolds for adhesion and signaling in platelets. Blood 2004, 104, 1606–1615. [Google Scholar] [CrossRef]
- Dhandayuthapani, B.; Yoshida, Y.; Maekawa, T.; Kumar, D.S. Polymeric Scaffolds in Tissue Engineering Application: A Review. International Journal of Polymer Science 2011, 2011, 290602. [Google Scholar] [CrossRef]
- Chi, J.; Wang, M.; Chen, J.; Hu, L.; Chen, Z.; Backman, L.J.; Zhang, W. Topographic Orientation of Scaffolds for Tissue Regeneration: Recent Advances in Biomaterial Design and Applications. Biomimetics 2022, 7, 131. [Google Scholar] [CrossRef]
- Yang, G.H.; Lee, J.; Kim, G. The fabrication of uniaxially aligned micro-textured polycaprolactone struts and application for skeletal muscle tissue regeneration. Biofabrication 2019, 11, 025005. [Google Scholar] [CrossRef] [PubMed]
- Niu, Z.; Wang, X.; Meng, X.; Guo, X.; Jiang, Y.; Xu, Y.; Li, Q.; Shen, C. Controllable fiber orientation and nonlinear elasticity of electrospun nanofibrous small diameter tubular scaffolds for vascular tissue engineering. Biomedical Materials 2019, 14, 035006. [Google Scholar] [CrossRef]
- Li, X.; Huang, L.; Li, L.A.-O.; Tang, Y.; Liu, Q.; Xie, H.; Tian, J.; Zhou, S.; Tang, G. Biomimetic dual-oriented/bilayered electrospun scaffold for vascular tissue engineering.
- Ghaderinejad, P.; Najmoddin, N.; Bagher, Z.; Saeed, M.; Karimi, S.; Simorgh, S.; Pezeshki-Modaress, M. An injectable anisotropic alginate hydrogel containing oriented fibers for nerve tissue engineering. Chemical Engineering Journal 2021, 420, 130465. [Google Scholar] [CrossRef]
- Loh, Q.L.; Choong, C. Three-dimensional scaffolds for tissue engineering applications: role of porosity and pore size.
- Kang, Y.; Chang, J. Channels in a porous scaffold: a new player for vascularization. Regenerative Medicine 2018, 13, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Huang, H.; Niu, J.; Chen, C.; Weng, J.; Yu, F.; Wang, D.; Kang, B.; Wang, T.; Yuan, G.; et al. Exploring the interconnectivity of biomimetic hierarchical porous Mg scaffolds for bone tissue engineering: Effects of pore size distribution on mechanical properties, degradation behavior and cell migration ability. Journal of Magnesium and Alloys 2021, 9, 1954–1966. [Google Scholar] [CrossRef]
- Basurto, I.M.; Mora, M.T.; Gardner, G.M.; Christ, G.J.; Caliari, S.R. Aligned and Conductive 3D Collagen Scaffolds for Skeletal Muscle Tissue Engineering. bioRxiv 2004, 2020.2004.2018.048017. [Google Scholar] [CrossRef]
- Guilak, F.; Cohen, D.M.; Estes, B.T.; Gimble, J.M.; Liedtke, W.; Chen, C.S. Control of stem cell fate by physical interactions with the extracellular matrix. Cell stem cell 2009, 5, 17–26. [Google Scholar] [CrossRef]
- Wang, S.; Hashemi, S.; Stratton, S.; Arinzeh, T.L. The Effect of Physical Cues of Biomaterial Scaffolds on Stem Cell Behavior. Advanced Healthcare Materials 2021, 10, 2001244. [Google Scholar] [CrossRef]
- Bianco, P.; Robey, P.G. Stem cells in tissue engineering. Nature 2001, 414, 118–121. [Google Scholar] [CrossRef]
- Chen, P.; Aso, T.; Sasaki, R.; Tsutsumi, Y.; Ashida, M.; Doi, H.; Hanawa, T. Micron/Submicron Hybrid Topography of Titanium Surfaces Influences Adhesion and Differentiation Behaviors of the Mesenchymal Stem Cells. Journal of biomedical nanotechnology 2017, 13, 324–336. [Google Scholar] [CrossRef]
- Yang, S.; Min, J.H.; Cho, K.; Seo, I.H.; Ryu, W.; Koh, W.-G. Fabrication of microgrooved scaffolds using near-field electrospinning-assisted lithography (NFEAL). Journal of Industrial and Engineering Chemistry 2019, 80, 471–478. [Google Scholar] [CrossRef]
- Miyoshi, H.; Adachi, T. Topography design concept of a tissue engineering scaffold for controlling cell function and fate through actin cytoskeletal modulation.
- Zhang, H.; Zhang, H.; Xiong, Y.; Dong, L.; Li, X. Development of hierarchical porous bioceramic scaffolds with controlled micro/nano surface topography for accelerating bone regeneration. Materials Science and Engineering: C 2021, 130, 112437. [Google Scholar] [CrossRef] [PubMed]
- Shams, M.; Karimi, M.; Jahangir, V.; Mohammadian, M.; Salimi, A. Surface modification of nanofibrous polyethersulfone scaffolds with fluorapatite nanoparticles toward improved stem cell behavior and osteogenic activity in vitro. Surfaces and Interfaces 2023, 36, 102512. [Google Scholar] [CrossRef]
- Yi, B.; Xu, Q.; Liu, W. An overview of substrate stiffness guided cellular response and its applications in tissue regeneration. Bioactive Materials 2022, 15, 82–102. [Google Scholar] [CrossRef]
- Breuls, R.G.; Jiya Tu Fau - Smit, T.H.; Smit, T.H. Scaffold stiffness influences cell behavior: opportunities for skeletal tissue engineering.
- Lee, C.R.; Grodzinsky Aj Fau - Spector, M.; Spector, M. The effects of cross-linking of collagen-glycosaminoglycan scaffolds on compressive stiffness, chondrocyte-mediated contraction, proliferation and biosynthesis.
- Zhang, J.; Wehrle, E.; Adamek, P.; Paul, G.R.; Qin, X.-H.; Rubert, M.; Müller, R. Optimization of mechanical stiffness and cell density of 3D bioprinted cell-laden scaffolds improves extracellular matrix mineralization and cellular organization for bone tissue engineering. Acta Biomaterialia 2020, 114, 307–322. [Google Scholar] [CrossRef]
- Keselowsky, B.G.; Collard, D.M.; Garcı́a, A.J. Surface chemistry modulates focal adhesion composition and signaling through changes in integrin binding. Biomaterials 2004, 25, 5947–5954. [Google Scholar] [CrossRef] [PubMed]
- Castner, D.G.; Ratner, B.D. Biomedical surface science: Foundations to frontiers. Surface Science 2002, 500, 28–60. [Google Scholar] [CrossRef]
- Atala, A. Foundations of regenerative medicine: clinical and therapeutic applications; Academic Press, 2009. [Google Scholar]
- Keselowsky, B.G.; Collard, D.M.; García, A.J. Surface chemistry modulates fibronectin conformation and directs integrin binding and specificity to control cell adhesion. Journal of Biomedical Materials Research Part A 2003, 66A, 247–259. [Google Scholar] [CrossRef]
- Tsimbouri, P.; Macnamara, L.; Alakpa, E.; Dalby, M.; Turner, L.-A. Cell-Material Interactions. 2014; pp. 217-251.
- Shen, M.; Horbett, T.A. The effects of surface chemistry and adsorbed proteins on monocyte/macrophage adhesion to chemically modified polystyrene surfaces. Journal of Biomedical Materials Research 2001, 57, 336–345. [Google Scholar] [CrossRef]
- McClary, K.B.; Ugarova, T.; Grainger, D.W. Modulating fibroblast adhesion, spreading, and proliferation using self-assembled monolayer films of alkylthiolates on gold. Journal of Biomedical Materials Research: An Official Journal of The Society for Biomaterials, The Japanese Society for Biomaterials, and The Australian Society for Biomaterials and the Korean Society for Biomaterials 2000, 50, 428–439. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, D.; Jiang, X.; He, L.; Fu, L.; Zhao, Y.; Wang, Y.; Mo, H.; Shen, J. Multistructured vascular patches constructed via layer-by-layer self-assembly of heparin and chitosan for vascular tissue engineering applications. Chemical Engineering Journal 2019, 370, 1057–1067. [Google Scholar] [CrossRef]
- He, M.; Zhu, C.; Sun, D.; Liu, Z.; Du, M.; Huang, Y.; Huang, L.; Wang, J.; Liu, L.; Li, Y.; et al. Layer-by-layer assembled black phosphorus/chitosan composite coating for multi-functional PEEK bone scaffold. Composites Part B: Engineering 2022, 246, 110266. [Google Scholar] [CrossRef]
- Zhang, K.; Huang, D.; Yan, Z.; Wang, C. Heparin/collagen encapsulating nerve growth factor multilayers coated aligned PLLA nanofibrous scaffolds for nerve tissue engineering. Journal of Biomedical Materials Research Part A 2017, 105, 1900–1910. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Heo, D.N.; Lee, S.J.; Heo, M.; Kim, J.; Choi, S.; Park, H.-K.; Park, Y.G.; Lim, H.-N.; Kwon, I.K. Poly (lactide-co-glycolide) nanofibrous scaffolds chemically coated with gold-nanoparticles as osteoinductive agents for osteogenesis. Applied Surface Science 2018, 432, 300–307. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, K.; Zhang, Y.; Jiang, Y.; Lu, X.; Fang, L.; Gan, D.; Lv, C.; Zhang, H.; Qu, S. Protein-affinitive polydopamine nanoparticles as an efficient surface modification strategy for versatile porous scaffolds enhancing tissue regeneration. Particle & Particle Systems Characterization 2016, 33, 89–100. [Google Scholar]
- Chen, B.-Q.; Kankala, R.K.; Chen, A.-Z.; Yang, D.-Z.; Cheng, X.-X.; Jiang, N.-N.; Zhu, K.; Wang, S.-B. Investigation of silk fibroin nanoparticle-decorated poly(l-lactic acid) composite scaffolds for osteoblast growth and differentiation. International Journal of Nanomedicine 2017, 12, 1877–1890. [Google Scholar] [CrossRef]
- Cheng, G.; Yin, C.; Tu, H.; Jiang, S.; Wang, Q.; Zhou, X.; Xing, X.; Xie, C.; Shi, X.; Du, Y.; et al. Controlled Co-delivery of Growth Factors through Layer-by-Layer Assembly of Core–Shell Nanofibers for Improving Bone Regeneration. ACS Nano 2019, 13, 6372–6382. [Google Scholar] [CrossRef]
- Zhou, X.; Pan, Y.; Liu, R.; Luo, X.; Zeng, X.; Zhi, D.; Li, J.; Cheng, Q.; Huang, Z.; Zhang, H.; et al. Biocompatibility and biodegradation properties of polycaprolactone/polydioxanone composite scaffolds prepared by blend or co-electrospinning. Journal of Bioactive and Compatible Polymers 2019, 34, 115–130. [Google Scholar] [CrossRef]
- Sharahi, M.; Hivechi, A.; Bahrami, S.H.; Hemmatinejad, N.; Milan, P.B. Co-electrospinning of lignocellulosic nanoparticles synthesized from walnut shells with poly(caprolactone) and gelatin for tissue engineering applications. Cellulose 2021, 28, 4943–4957. [Google Scholar] [CrossRef]
- Beishenaliev, A.; Lim, S.S.; Tshai, K.Y.; Khiew, P.S.; Moh’d Sghayyar, H.N.; Loh, H.-S. Fabrication and preliminary in vitro evaluation of ultraviolet-crosslinked electrospun fish scale gelatin nanofibrous scaffolds. Journal of Materials Science: Materials in Medicine 2019, 30, 62. [Google Scholar] [CrossRef]
- Keirouz, A.; Fortunato, G.; Zhang, M.; Callanan, A.; Radacsi, N. Nozzle-free electrospinning of Polyvinylpyrrolidone/Poly(glycerol sebacate) fibrous scaffolds for skin tissue engineering applications. Medical Engineering & Physics 2019, 71, 56–67. [Google Scholar] [CrossRef]
- Satish, A.; Korrapati, P.S. Strategic design of peptide-decorated aligned nanofibers impregnated with triiodothyronine for neural regeneration. Journal of Tissue Engineering and Regenerative Medicine 2019, 13, 753–770. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wei, X.; Wang, Q.; Chen, J.; Chang, G.; Kong, L.; Su, J.; Liu, Y. Homogeneous isolation of nanocellulose from sugarcane bagasse by high pressure homogenization. Carbohydrate Polymers 2012, 90, 1609–1613. [Google Scholar] [CrossRef] [PubMed]
- Aragon, J.; Navascues, N.; Mendoza, G.; Irusta, S. Laser-treated electrospun fibers loaded with nano-hydroxyapatite for bone tissue engineering. International Journal of Pharmaceutics 2017, 525, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Ghobeira, R.; Philips, C.; Liefooghe, L.; Verdonck, M.; Asadian, M.; Cools, P.; Declercq, H.; De Vos, W.H.; De Geyter, N.; Morent, R. Synergetic effect of electrospun PCL fiber size, orientation and plasma-modified surface chemistry on stem cell behavior. Applied Surface Science 2019, 485, 204–221. [Google Scholar] [CrossRef]
- Karimi, Z.; Seyedjafari, E.; Mahdavi, F.S.; Hashemi, S.M.; Khojasteh, A.; Kazemi, B.; Mohammadi-Yeganeh, S. Baghdadite nanoparticle-coated poly l-lactic acid (PLLA) ceramics scaffold improved osteogenic differentiation of adipose tissue-derived mesenchymal stem cells. Journal of Biomedical Materials Research Part A 2019, 107, 1284–1293. [Google Scholar] [CrossRef]
- Meghdadi, M.; Atyabi, S.-M.; Pezeshki-Modaress, M.; Irani, S.; Noormohammadi, Z.; Zandi, M. Cold atmospheric plasma as a promising approach for gelatin immobilization on poly(ε-caprolactone) electrospun scaffolds. Progress in Biomaterials 2019, 8, 65–75. [Google Scholar] [CrossRef]
- Idini, M.; Wieringa, P.; Rocchiccioli, S.; Nieddu, G.; Ucciferri, N.; Formato, M.; Lepedda, A.; Moroni, L. Glycosaminoglycan functionalization of electrospun scaffolds enhances Schwann cell activity. Acta Biomaterialia 2019, 96, 188–202. [Google Scholar] [CrossRef]
- Fan, J.; Lei, T.; Yu, M.; Wang, Y.; Cao, F.; Yang, Q.; Tian, F.; Liu, Y. Keratin/PEO/hydroxyapatite Nanofiber Membrane with Improved Mechanical Property for Potential Burn Dressing Application. Fibers and Polymers 2020, 21, 366–375. [Google Scholar] [CrossRef]
- Ardila, D.C.; Liou, J.-J.; Maestas, D.; Slepian, M.J.; Badowski, M.; Wagner, W.R.; Harris, D.; Vande Geest, J.P. Surface Modification of Electrospun Scaffolds for Endothelialization of Tissue-Engineered Vascular Grafts Using Human Cord Blood-Derived Endothelial Cells. Journal of Clinical Medicine 2019, 8. [Google Scholar] [CrossRef]
- Bosworth, L.A.; Hu, W.; Shi, Y.; Cartmell, S.H. Enhancing Biocompatibility without Compromising Material Properties: An Optimised NaOH Treatment for Electrospun Polycaprolactone Fibres. Journal of Nanomaterials 2019, 2019, 4605092. [Google Scholar] [CrossRef]
- Hanuman, S.; Nune, M. Design and Characterization of Maltose-Conjugated Polycaprolactone Nanofibrous Scaffolds for Uterine Tissue Engineering. Regenerative Engineering and Translational Medicine 2022, 8, 334–344. [Google Scholar] [CrossRef]
- Rashidi, N.S.; Sukmana, I.; Mataram, A.; Jasmawati, N.; Rofi, M.R.M.; Kadir, M.R.A. Surface-treated and fibrin-coated electrospun polyacrylonitrile fiber for endothelial cell growth and proliferation. Facta Universitatis, Series: Mechanical Engineering 2018, 16, 307–319. [Google Scholar] [CrossRef]
- Chiesa, I.; De Maria, C.; Lapomarda, A.; Fortunato, G.M.; Montemurro, F.; Di Gesù, R.; Tuan, R.S.; Vozzi, G.; Gottardi, R. Endothelial cells support osteogenesis in an in vitro vascularized bone model developed by 3D bioprinting. Biofabrication 2020, 12, 025013. [Google Scholar] [CrossRef] [PubMed]
- Rosellini, E.; Madeddu, D.; Barbani, N.; Frati, C.; Graiani, G.; Falco, A.; Lagrasta, C.; Quaini, F.; Cascone, M.G. Development of Biomimetic Alginate/Gelatin/Elastin Sponges with Recognition Properties toward Bioactive Peptides for Cardiac Tissue Engineering. Biomimetics 2020, 5. [Google Scholar] [CrossRef] [PubMed]
- Haramshahi, S.M.A.; Bonakdar, S.; Moghtadaei, M.; Kamguyan, K.; Thormann, E.; Tanbakooei, S.; Simorgh, S.; Brouki-Milan, P.; Amini, N.; Latifi, N.; et al. Tenocyte-imprinted substrate: a topography-based inducer for tenogenic differentiation in adipose tissue-derived mesenchymal stem cells. Biomedical Materials 2020, 15, 035014. [Google Scholar] [CrossRef]
- Park, S.H.; Seo, J.Y.; Park, J.Y.; Ji, Y.B.; Kim, K.; Choi, H.S.; Choi, S.; Kim, J.H.; Min, B.H.; Kim, M.S. An injectable, click-crosslinked, cytomodulin-modified hyaluronic acid hydrogel for cartilage tissue engineering. NPG Asia Materials 2019, 11, 30. [Google Scholar] [CrossRef]
- Nouri-Felekori, M.; Nezafati, N.; Moraveji, M.; Hesaraki, S.; Ramezani, T. Bioorthogonal hydroxyethyl cellulose-based scaffold crosslinked via click chemistry for cartilage tissue engineering applications. International Journal of Biological Macromolecules 2021, 183, 2030–2043. [Google Scholar] [CrossRef]
- Battigelli, A.; Almeida, B.; Shukla, S.; Rocha, A.D.; Shukla, A. Inducing mesenchymal stem cell attachment on non-cell adhesive hydrogels through click chemistry. Chemical Communications 2020, 56, 7661–7664. [Google Scholar] [CrossRef]
- Ratner, B.D. Surface modification of polymers: chemical, biological and surface analytical challenges. Biosensors and bioelectronics 1995, 10, 797–804. [Google Scholar] [CrossRef]
- Curran, J.M.; Chen, R.; Hunt, J.A. Controlling the phenotype and function of mesenchymal stem cells in vitro by adhesion to silane-modified clean glass surfaces. Biomaterials 2005, 26, 7057–7067. [Google Scholar] [CrossRef] [PubMed]
- Rahmati, M.; Silva, E.A.; Reseland, J.E.; A. Heyward, C.; Haugen, H.J. Biological responses to physicochemical properties of biomaterial surface. Chemical Society Reviews 2020, 49, 5178–5224. [Google Scholar] [CrossRef] [PubMed]
- Castellanos, M.I.; Mas-Moruno, C.; Grau, A.; Serra-Picamal, X.; Trepat, X.; Albericio, F.; Joner, M.; Gil, F.J.; Ginebra, M.P.; Manero, J.M.; et al. Functionalization of CoCr surfaces with cell adhesive peptides to promote HUVECs adhesion and proliferation. Applied Surface Science 2017, 393, 82–92. [Google Scholar] [CrossRef]
- Cao, S.; Barcellona, M.N.; Pfeiffer, F.; Bernards, M.T. Tunable multifunctional tissue engineering scaffolds composed of three-component polyampholyte polymers. Journal of Applied Polymer Science 2016, 133. [Google Scholar] [CrossRef]
- Totaro, K.A.; Liao, X.; Bhattacharya, K.; Finneman, J.I.; Sperry, J.B.; Massa, M.A.; Thorn, J.; Ho, S.V.; Pentelute, B.L. Systematic investigation of EDC/sNHS-mediated bioconjugation reactions for carboxylated peptide substrates. Bioconjugate chemistry 2016, 27, 994–1004. [Google Scholar] [CrossRef] [PubMed]
- Kosif, I.; Park, E.-J.; Sanyal, R.; Sanyal, A. Fabrication of maleimide containing thiol reactive hydrogels via Diels− Alder/Retro-Diels− Alder strategy. Macromolecules 2010, 43, 4140–4148. [Google Scholar] [CrossRef]
- Tang, W.; Becker, M.L. “Click” reactions: a versatile toolbox for the synthesis of peptide-conjugates. Chemical Society Reviews 2014, 43, 7013–7039. [Google Scholar] [CrossRef]
- Zou, Y.; Zhang, L.; Yang, L.; Zhu, F.; Ding, M.; Lin, F.; Wang, Z.; Li, Y. “Click” chemistry in polymeric scaffolds: Bioactive materials for tissue engineering. Journal of controlled release 2018, 273, 160–179. [Google Scholar] [CrossRef]
- Phillips, J.E.; Petrie, T.A.; Creighton, F.P.; García, A.J. Human mesenchymal stem cell differentiation on self-assembled monolayers presenting different surface chemistries. Acta Biomaterialia 2010, 6, 12–20. [Google Scholar] [CrossRef]
- Anderson, D.G.; Levenberg, S.; Langer, R. Nanoliter-scale synthesis of arrayed biomaterials and application to human embryonic stem cells. Nature Biotechnology 2004, 22, 863–866. [Google Scholar] [CrossRef]
- Yu, T.-T.; Cui, F.-Z.; Meng, Q.-Y.; Wang, J.; Wu, D.-C.; Zhang, J.; Kou, X.-X.; Yang, R.-L.; Liu, Y.; Zhang, Y.S.; et al. Influence of Surface Chemistry on Adhesion and Osteo/Odontogenic Differentiation of Dental Pulp Stem Cells. ACS Biomaterials Science & Engineering 2017, 3, 1119–1128. [Google Scholar] [CrossRef]
- Bai, B.; He, J.; Li, Y.-S.; Wang, X.-M.; Ai, H.-J.; Cui, F.-Z. Activation of the ERK1/2 Signaling Pathway during the Osteogenic Differentiation of Mesenchymal Stem Cells Cultured on Substrates Modified with Various Chemical Groups. BioMed Research International 2013, 2013, 361906. [Google Scholar] [CrossRef]
- Wang, Y.; Yao, S.; Meng, Q.; Yu, X.; Wang, X.; Cui, F. Gene expression profiling and mechanism study of neural stem cells response to surface chemistry. Regenerative Biomaterials 2014, 1, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Zeng, D.; Zhang, X.; Wang, X.; Huang, Q.; Wen, J.; Miao, X.; Peng, L.; Li, Y.; Jiang, X. The osteoimmunomodulatory properties of MBG scaffold coated with amino functional groups. Artificial Cells, Nanomedicine, and Biotechnology 2018, 46, 1425–1435. [Google Scholar] [CrossRef] [PubMed]
- Aziz, G.; De Geyter, N.; Declercq, H.; Cornelissen, R.; Morent, R. Incorporation of amine moieties onto ultra-high molecular weight polyethylene (UHMWPE) surface via plasma and UV polymerization of allylamine. Surface and Coatings Technology 2015, 271, 39–47. [Google Scholar] [CrossRef]
- Shen, Z.; Wu, J.; Yu, Y.; Liu, S.; Jiang, W.; Nurmamat, H.; Wu, B. Comparison of cytotoxicity and membrane efflux pump inhibition in HepG2 cells induced by single-walled carbon nanotubes with different length and functional groups. Scientific Reports 2019, 9, 7557. [Google Scholar] [CrossRef] [PubMed]
- Tohidlou, H.; Shafiei, S.S.; Abbasi, S.; Asadi-Eydivand, M.; Fathi-Roudsari, M. Amine-functionalized Single-walled Carbon Nanotube/Polycaprolactone Electrospun Scaffold for Bone Tissue Engineering: in vitro Study. Fibers and Polymers 2019, 20, 1869–1882. [Google Scholar] [CrossRef]
- Zhao, S.; Zhang, J.; Zhu, M.; Zhang, Y.; Liu, Z.; Ma, Y.; Zhu, Y.; Zhang, C. Effects of functional groups on the structure, physicochemical and biological properties of mesoporous bioactive glass scaffolds. Journal of Materials Chemistry B 2015, 3, 1612–1623. [Google Scholar] [CrossRef]
- Lin, M.; Wang, H.; Ruan, C.; Xing, J.; Wang, J.; Li, Y.; Wang, Y.; Luo, Y. Adsorption Force of Fibronectin on Various Surface Chemistries and Its Vital Role in Osteoblast Adhesion. Biomacromolecules 2015, 16, 973–984. [Google Scholar] [CrossRef]
- Yang, X.; Wang, X.; Yu, F.; Ma, L.; Pan, X.; Luo, G.; Lin, S.; Mo, X.; He, C.; Wang, H. Hyaluronic acid/EDC/NHS-crosslinked green electrospun silk fibroin nanofibrous scaffolds for tissue engineering. RSC advances 2016, 6, 99720–99728. [Google Scholar] [CrossRef]
- Guler, Z.; Silva, J.C.; Sarac, A.S. Enhanced osteogenesis on biofunctionalized poly(ɛ-caprolactone)/poly(m-anthranilic acid) nanofibers. Journal of Biomaterials Applications 2016, 31, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Beiki, B.; Zeynali, B.; Seyedjafari, E. Fabrication of a three dimensional spongy scaffold using human Wharton’s jelly derived extra cellular matrix for wound healing. Materials Science and Engineering: C 2017, 78, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Koivusalo, L.; Kauppila, M.; Samanta, S.; Parihar, V.S.; Ilmarinen, T.; Miettinen, S.; Oommen, O.P.; Skottman, H. Tissue adhesive hyaluronic acid hydrogels for sutureless stem cell delivery and regeneration of corneal epithelium and stroma. Biomaterials 2019, 225, 119516. [Google Scholar] [CrossRef] [PubMed]
- Kołbuk, D.; Heljak, M.; Choińska, E.; Urbanek, O. Novel 3D Hybrid Nanofiber Scaffolds for Bone Regeneration. Polymers 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Park, E.J.; Gevrek, T.N.; Sanyal, R.; Sanyal, A. Indispensable platforms for bioimmobilization: Maleimide-based thiol reactive hydrogels. Bioconjugate Chemistry 2014, 25, 2004–2011. [Google Scholar] [CrossRef]
- Stynes, G.D.; Gengenbach, T.R.; Kiroff, G.K.; Morrison, W.A.; Kirkland, M.A. Thiol surface functionalization via continuous phase plasma polymerization of allyl mercaptan, with subsequent maleimide-linked conjugation of collagen. Journal of Biomedical Materials Research Part A 2017, 105, 1940–1948. [Google Scholar] [CrossRef]
- Yao, Y.; Wang, P.; Li, X.; Xu, Y.; Lu, G.; Jiang, Q.; Sun, Y.; Fan, Y.; Zhang, X. A di-self-crosslinking hyaluronan-based hydrogel combined with type I collagen to construct a biomimetic injectable cartilage-filling scaffold. Acta Biomaterialia 2020, 111, 197–207. [Google Scholar] [CrossRef]
- Cengiz, N.; Gevrek, T.N.; Sanyal, R.; Sanyal, A. Fabrication of Patterned Hydrogel Interfaces: Exploiting the Maleimide Group as a Dual Purpose Handle for Cross-Linking and Bioconjugation. Bioconjugate Chemistry 2020, 31, 1382–1391. [Google Scholar] [CrossRef]
- Friuli, M.; Nitti, P.; Madaghiele, M.; Demitri, C. A possible method to avoid skin effect in polymeric scaffold produced through thermally induced phase separation. Results in Engineering 2021, 12. [Google Scholar] [CrossRef]
- Yoo, K.M.; Murphy, S.V.; Skardal, A. A Rapid Crosslinkable Maleimide-Modified Hyaluronic Acid and Gelatin Hydrogel Delivery System for Regenerative Applications. Gels 2021, 7. [Google Scholar] [CrossRef]
- Yu, Y.; Xu, S.; Li, S.; Pan, H. Genipin-cross-linked hydrogels based on biomaterials for drug delivery: A review. Biomaterials science 2021, 9, 1583–1597. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Li, F.; Shao, W.; Gao, J.; Ling, D. Promoting Angiogenesis in Oxidative Diabetic Wound Microenvironment Using a Nanozyme-Reinforced Self-Protecting Hydrogel. ACS Central Science 2019, 5, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Biazar, E.; Kamalvand, M.; Avani, F. Recent advances in surface modification of biopolymeric nanofibrous scaffolds. International Journal of Polymeric Materials and Polymeric Biomaterials 2022, 71, 493–512. [Google Scholar] [CrossRef]
- Panchal, R.; Mateti, T.; Likhith, K.; Rodrigues, F.C.; Thakur, G. Genipin cross-linked chitosan–PVA composite films: An investigation on the impact of cross-linking on accelerating wound healing. Reactive and Functional Polymers 2022, 178, 105339. [Google Scholar] [CrossRef]
- Jing, D.; Bhushan, B. Quantification of Surface Charge Density and Its Effect on Boundary Slip. Langmuir 2013, 29, 6953–6963. [Google Scholar] [CrossRef]
- Kumar, S.; Raj, S.; Kolanthai, E.; Sood, A.K.; Sampath, S.; Chatterjee, K. Chemical functionalization of graphene to augment stem cell osteogenesis and inhibit biofilm formation on polymer composites for orthopedic applications. ACS applied materials & interfaces 2015, 7, 3237–3252. [Google Scholar]
- Zhang, Y.; Luan, J.; Jiang, S.; Zhou, X.; Li, M. The effect of amino-functionalized mesoporous bioactive glass on MC3T3-E1 cells in vitro stimulation. Composites Part B: Engineering 2019, 172, 397–405. [Google Scholar] [CrossRef]
- Cao, B.; Peng, Y.; Liu, X.; Ding, J. Effects of Functional Groups of Materials on Nonspecific Adhesion and Chondrogenic Induction of Mesenchymal Stem Cells on Free and Micropatterned Surfaces. ACS Applied Materials & Interfaces 2017, 9, 23574–23585. [Google Scholar] [CrossRef]
- Wang, F.; Qiao, W.; Guo, W.; Li, Z.; Cai, X. Fabrication and functionalization of biocompatible carboxymethyl chitosan/gelatin membranes via anodic electrophoretic deposition. RSC Advances 2022, 12, 5677–5685. [Google Scholar] [CrossRef]
- Wang, K.-Y.; Jin, X.-Y.; Ma, Y.-H.; Cai, W.-J.; Xiao, W.-Y.; Li, Z.-W.; Qi, X.; Ding, J. Injectable stress relaxation gelatin-based hydrogels with positive surface charge for adsorption of aggrecan and facile cartilage tissue regeneration. Journal of Nanobiotechnology 2021, 19, 214. [Google Scholar] [CrossRef]
- Bai, J.; Zuo, X.; Feng, X.; Sun, Y.; Ge, Q.; Wang, X.; Gao, C. Dynamic Titania Nanotube Surface Achieves UV-Triggered Charge Reversal and Enhances Cell Differentiation. ACS Applied Materials & Interfaces 2019, 11, 36939–36948. [Google Scholar] [CrossRef]
- Lin, Z.; Wu, M.; He, H.; Liang, Q.; Hu, C.; Zeng, Z.; Cheng, D.; Wang, G.; Chen, D.; Pan, H.; et al. 3D Printing of Mechanically Stable Calcium-Free Alginate-Based Scaffolds with Tunable Surface Charge to Enable Cell Adhesion and Facile Biofunctionalization. Advanced Functional Materials 2019, 29, 1808439. [Google Scholar] [CrossRef]
- González-Carrasco, J.L.; Cifuentes Cuellar, S.C.; Lieblich Rodríguez, M. 5 - Metals. In Bone Repair Biomaterials (Second Edition); Pawelec, K.M., Planell, J.A., Eds.; Woodhead Publishing, 2019; pp. 103–140. [Google Scholar]
- Hu, H.; Gao, L.; Liu, Y. Chapter 6 - Hydro-/ice-phobic coatings and materials for wind turbine icing mitigation. In Wind Turbine Icing Physics and Anti-/De-icing Technology; Hu, H., Gao, L., Liu, Y., Eds.; Academic Press, 2022; pp. 135–168. [Google Scholar]
- Lai, Y.; Pan, F.; Xu, C.; Fuchs, H.; Chi, L. Nanotube Arrays: In Situ Surface-Modification-Induced Superhydrophobic Patterns with Reversible Wettability and Adhesion (Adv. Mater. 12/2013). Advanced Materials 2013, 25, 1804–1804. [Google Scholar] [CrossRef]
- Arima, Y.; Iwata, H. Effect of wettability and surface functional groups on protein adsorption and cell adhesion using well-defined mixed self-assembled monolayers. Biomaterials 2007, 28, 3074–3082. [Google Scholar] [CrossRef] [PubMed]
- van Wachem, P.B.; Hogt, A.H.; Beugeling, T.; Feijen, J.; Bantjes, A.; Detmers, J.P.; van Aken, W.G. Adhesion of cultured human endothelial cells onto methacrylate polymers with varying surface wettability and charge. Biomaterials 1987, 8, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.-C.; Siedlecki, C.A. Effects of surface wettability and contact time on protein adhesion to biomaterial surfaces. Biomaterials 2007, 28, 3273–3283. [Google Scholar] [CrossRef]
- Lee, J.H.; Khang, G.; Lee, J.W.; Lee, H.B. Interaction of different types of cells on polymer surfaces with wettability gradient. Journal of colloid and interface science 1998, 205, 323–330. [Google Scholar] [CrossRef]
- Chen, F.; Xu, W.; Huang, S.; Liu, J.; Song, J.; Liu, X. Plasma Hydrophilization of Superhydrophobic Surface and Its Aging Behavior: The Effect of Micro/nanostructured Surface. Surface and Interface Analysis 2016, 48, 368–372. [Google Scholar] [CrossRef]
- Yang, H.; Fung, S.-Y.; Pritzker, M.; Chen, P. Modification of hydrophilic and hydrophobic surfaces using an ionic-complementary peptide. PLoS One 2007, 2, e1325. [Google Scholar] [CrossRef]
- Zhang, K.; Zheng, H.; Liang, S.; Gao, C. Aligned PLLA nanofibrous scaffolds coated with graphene oxide for promoting neural cell growth. Acta Biomaterialia 2016, 37, 131–142. [Google Scholar] [CrossRef]
- Kawai, T.; Shanjani, Y.; Fazeli, S.; Behn, A.W.; Okuzu, Y.; Goodman, S.B.; Yang, Y.P. Customized, degradable, functionally graded scaffold for potential treatment of early stage osteonecrosis of the femoral head. Journal of Orthopaedic Research 2018, 36, 1002–1011. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Bai, J.; Tao, H.; Hao, L.; Yin, W.; Ren, X.; Gao, A.; Li, N.; Wang, M.; Fang, S.; et al. Rational integration of defense and repair synergy on PEEK osteoimplants via biomimetic peptide clicking strategy. Bioactive Materials 2022, 8, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Khorramnezhad, M.; Akbari, B.; Akbari, M.; Kharaziha, M. Effect of surface modification on physical and cellular properties of PCL thin film. Colloids and Surfaces B: Biointerfaces 2021, 200, 111582. [Google Scholar] [CrossRef] [PubMed]
- Rabel, K.; Kohal, R.-J.; Steinberg, T.; Rolauffs, B.; Adolfsson, E.; Altmann, B. Human osteoblast and fibroblast response to oral implant biomaterials functionalized with non-thermal oxygen plasma. Scientific Reports 2021, 11, 17302. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.; Dinh, D.K.; Abbas, Q.; Imran, M.; Sattar, H.; Ul Ahmad, A. Controlled Surface Wettability by Plasma Polymer Surface Modification. Surfaces 2019, 2, 349–371. [Google Scholar] [CrossRef]
- Drobota, M.; Ursache, S.; Aflori, M. Surface Functionalities of Polymers for Biomaterial Applications. Polymers 2022, 14. [Google Scholar] [CrossRef]
- Porrelli, D.; Mardirossian, M.; Crapisi, N.; Urban, M.; Ulian, N.A.; Bevilacqua, L.; Turco, G.; Maglione, M. Polyetheretherketone and titanium surface treatments to modify roughness and wettability – Improvement of bioactivity and antibacterial properties. Journal of Materials Science & Technology 2021, 95, 213–224. [Google Scholar] [CrossRef]
- Kupka, V.; Dvořáková, E.; Manakhov, A.; Michlíček, M.; Petruš, J.; Vojtová, L.; Zajíčková, L. Well-Blended PCL/PEO Electrospun Nanofibers with Functional Properties Enhanced by Plasma Processing. Polymers 2020, 12. [Google Scholar] [CrossRef]
- Esfahani, H.; Ghiyasi, Y. Effect of HA Nanoparticles on Adsorption of Vitamin D3 on Super-Hydrophobic PA6 Nanofibrous Scaffold. Matéria (Rio de Janeiro) 2020, 25. [Google Scholar] [CrossRef]
- Padmanabhan, S.K.; Nitti, P.; Stanca, E.; Rochira, A.; Siculella, L.; Raucci, M.G.; Madaghiele, M.; Licciulli, A.; Demitri, C. Mechanical and biological properties of magnesium-and silicon-substituted hydroxyapatite scaffolds. Materials 2021, 14. [Google Scholar] [CrossRef]
- Zhang, J.; Li, L.; Peng, Y.; Chen, Y.; Lv, X.; Li, S.; Qin, X.; Yang, H.; Wu, C.; Liu, Y. Surface chemistry induces mitochondria-mediated apoptosis of breast cancer cells via PTEN/PI3K/AKT signaling pathway. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research 2018, 1865, 172–185. [Google Scholar] [CrossRef] [PubMed]
- Arbade, G.K.; Srivastava, J.; Tripathi, V.; Lenka, N.; Patro, T.U. Enhancement of hydrophilicity, biocompatibility and biodegradability of poly(ε-caprolactone) electrospun nanofiber scaffolds using poly(ethylene glycol) and poly(L-lactide-co-ε-caprolactone-co-glycolide) as additives for soft tissue engineering. Journal of Biomaterials Science, Polymer Edition 2020, 31, 1648–1670. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Salvi, G.E.; Huynh-Ba, G.; Ivanovski, S.; Donos, N.; Bosshardt, D.D. Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clinical oral implants research 2011, 22, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Visalakshan, R.M.; MacGregor, M.N.; Sasidharan, S.; Ghazaryan, A.; Mierczynska-Vasilev, A.M.; Morsbach, S.; Mailänder, V.; Landfester, K.; Hayball, J.D.; Vasilev, K. Biomaterial Surface Hydrophobicity-Mediated Serum Protein Adsorption and Immune Responses. ACS Applied Materials & Interfaces 2019, 11, 27615–27623. [Google Scholar] [CrossRef]
- Oliver-Cervelló, L.; Martin-Gómez, H.; Mas-Moruno, C. New trends in the development of multifunctional peptides to functionalize biomaterials. Journal of Peptide Science 2022, 28, e3335. [Google Scholar] [CrossRef]
- Mas-Moruno, C. 3 - Surface functionalization of biomaterials for bone tissue regeneration and repair. In Peptides and Proteins as Biomaterials for Tissue Regeneration and Repair; Barbosa, M.A., Martins, M.C.L., Eds.; Woodhead Publishing, 2018; pp. 73–100. [Google Scholar]
- von der Mark, K.; Park, J. Engineering biocompatible implant surfaces: Part II: Cellular recognition of biomaterial surfaces: Lessons from cell–matrix interactions. Progress in Materials Science 2013, 58, 327–381. [Google Scholar] [CrossRef]
- Dankovich, T.A.; Hsieh, Y.-L. Surface modification of cellulose with plant triglycerides for hydrophobicity. Cellulose 2007, 14, 469–480. [Google Scholar] [CrossRef]
- Oliver-Cervelló, L.; Martin-Gómez, H.; Reyes, L.; Noureddine, F.; Ada Cavalcanti-Adam, E.; Ginebra, M.-P.; Mas-Moruno, C. An Engineered Biomimetic Peptide Regulates Cell Behavior by Synergistic Integrin and Growth Factor Signaling. Advanced Healthcare Materials 2021, 10, 2001757. [Google Scholar] [CrossRef]
- Clauder, F.; Zitzmann, F.D.; Friebe, S.; Mayr, S.G.; Robitzki, A.A.; Beck-Sickinger, A.G. Multifunctional coatings combining bioactive peptides and affinity-based cytokine delivery for enhanced integration of degradable vascular grafts. Biomaterials Science 2020, 8, 1734–1747. [Google Scholar] [CrossRef]
- Liu, Q.; Zheng, S.; Ye, K.; He, J.; Shen, Y.; Cui, S.; Huang, J.; Gu, Y.; Ding, J. Cell migration regulated by RGD nanospacing and enhanced under moderate cell adhesion on biomaterials. Biomaterials 2020, 263, 120327. [Google Scholar] [CrossRef]
- Li, W.; Xu, H.; Han, X.; Sun, S.; Chai, Q.; Xu, X.; Man, Z. Simultaneously promoting adhesion and osteogenic differentiation of bone marrow-derived mesenchymal cells by a functional electrospun scaffold. Colloids and Surfaces B: Biointerfaces 2020, 192, 111040. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Cheng, Q.; Long, Y.; Xu, C.; Fang, H.; Chen, Y.; Dai, H. A chitosan based scaffold with enhanced mechanical and biocompatible performance for biomedical applications. Polymer Degradation and Stability 2020, 181, 109322. [Google Scholar] [CrossRef]
- Sharma, P.; Kaur, H.; Roy, S. Designing a Tenascin-C-Inspired Short Bioactive Peptide Scaffold to Direct and Control Cellular Behavior. ACS Biomaterials Science & Engineering 2019, 5, 6497–6510. [Google Scholar] [CrossRef]
- Camacho, P.; Busari, H.; Seims, K.B.; Schwarzenberg, P.; Dailey, H.L.; Chow, L.W. 3D printing with peptide–polymer conjugates for single-step fabrication of spatially functionalized scaffolds. Biomaterials science 2019, 7, 4237–4247. [Google Scholar] [CrossRef]
- Ghosh, M.; Halperin-Sternfeld, M.; Grinberg, I.; Adler-Abramovich, L. Injectable Alginate-Peptide Composite Hydrogel as a Scaffold for Bone Tissue Regeneration. Nanomaterials 2019, 9. [Google Scholar] [CrossRef]
- Eckhart, K.E.; Holt, B.D.; Laurencin, M.G.; Sydlik, S.A. Covalent conjugation of bioactive peptides to graphene oxide for biomedical applications. Biomaterials science 2019, 7, 3876–3885. [Google Scholar] [CrossRef]
- Hao, D.; Ma, B.; He, C.; Liu, R.; Farmer, D.L.; Lam, K.S.; Wang, A. Surface modification of polymeric electrospun scaffolds via a potent and high-affinity integrin α4β1 ligand improved the adhesion, spreading and survival of human chorionic villus-derived mesenchymal stem cells: A new insight for fetal tissue engineering. Journal of Materials Chemistry B 2020, 8, 1649–1659. [Google Scholar] [CrossRef]
- Nazeri, N.; Karimi, R.; Ghanbari, H. The effect of surface modification of poly-lactide-co-glycolide/carbon nanotube nanofibrous scaffolds by laminin protein on nerve tissue engineering. Journal of Biomedical Materials Research Part A 2021, 109, 159–169. [Google Scholar] [CrossRef]
- Nitti, P.; Palazzo, B.; Gallo, N.; Scalera, F.; Sannino, A.; Gervaso, F. Smooth-rough asymmetric PLGA structure made of dip coating membrane and electrospun nanofibrous scaffolds meant to be used for guided tissue regeneration of periodontium. Polymer Engineering and Science 2022, 62, 2061–2069. [Google Scholar] [CrossRef]
- Raut, H.K.; Das, R.; Liu, Z.; Liu, X.; Ramakrishna, S. Biocompatibility of Biomaterials for Tissue Regeneration or Replacement. Biotechnology Journal 2020, 15, 2000160. [Google Scholar] [CrossRef]
- Ghasemi-Mobarakeh, L.; Kolahreez, D.; Ramakrishna, S.; Williams, D. Key terminology in biomaterials and biocompatibility. Current Opinion in Biomedical Engineering 2019, 10, 45–50. [Google Scholar] [CrossRef]
- Yang, Y.; Qi, P.; Ding, Y.; Maitz, M.F.; Yang, Z.; Tu, Q.; Xiong, K.; Leng, Y.; Huang, N. A biocompatible and functional adhesive amine-rich coating based on dopamine polymerization. Journal of Materials Chemistry B 2015, 3, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Chen, H.; Zhang, H.; Guo, C.; Yang, K.; Chen, K.; Cheng, R.; Qian, N.; Sandler, N.; Zhang, Y.S.; et al. Vascularized 3D printed scaffolds for promoting bone regeneration. Biomaterials 2019, 190-191, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Nune, M.; Manchineella, S.; T, G.; K. S, N. Melanin incorporated electroactive and antioxidant silk fibroin nanofibrous scaffolds for nerve tissue engineering. Materials Science and Engineering: C 2019, 94, 17–25. [Google Scholar] [CrossRef]
- Jeong, Y.-W.; Jung, S.; Han, J.J.; Park, H.-J.; Kim, R.Y.; Kim, B.-H.; Kook, M.-S. Effectiveness of Surface Treatment with Amine Plasma for Improving the Biocompatibility of Maxillofacial Plates. Materials 2019, 12. [Google Scholar] [CrossRef]
- Li, C.; Zhou, Y.; Liu, S.; Guo, R.; Lu, C.; Yin, D.; Zhang, Y.; Xu, X.; Dong, N.; Shi, J. Surface Modification of Decellularized Heart Valve by the POSS–PEG Hybrid Hydrogel to Prepare a Composite Scaffold Material with Anticalcification Potential. ACS Applied Bio Materials 2022, 5, 3923–3935. [Google Scholar] [CrossRef]
- Friuli, M.; Nitti, P.; Aneke, C.I.; Demitri, C.; Cafarchia, C.; Otranto, D. Freeze-drying of Beauveria bassiana suspended in Hydroxyethyl cellulose based hydrogel as possible method for storage: Evaluation of survival, growth and stability of conidial concentration before and after processing. Results in Engineering 2021, 12, 100283. [Google Scholar] [CrossRef]
- Massardier-Nageotte, V.; Pestre, C.; Cruard-Pradet, T.; Bayard, R. Aerobic and anaerobic biodegradability of polymer films and physico-chemical characterization. Polymer Degradation and Stability 2006, 91, 620–627. [Google Scholar] [CrossRef]
- Da Silva, A.C.; Córdoba de Torresi, S.I. Advances in conducting, biodegradable and biocompatible copolymers for biomedical applications. Frontiers in Materials 2019, 6, 98. [Google Scholar] [CrossRef]
- Bhatia, S.K.; Wadhwa, P.; Hong, J.W.; Hong, Y.G.; Jeon, J.-M.; Lee, E.S.; Yang, Y.-H. Lipase mediated functionalization of poly(3-hydroxybutyrate-co-3-hydroxyvalerate) with ascorbic acid into an antioxidant active biomaterial. International Journal of Biological Macromolecules 2019, 123, 117–123. [Google Scholar] [CrossRef]
- Ladmiral, V.; Melia, E.; Haddleton, D.M. Synthetic glycopolymers: an overview. European Polymer Journal 2004, 40, 431–449. [Google Scholar] [CrossRef]
- Miura, Y. Synthesis and biological application of glycopolymers. Journal of Polymer Science Part A: Polymer Chemistry 2007, 45, 5031–5036. [Google Scholar] [CrossRef]
- Gumel, A.M.; Annuar, S.M.; Heidelberg, T. Single-step lipase-catalyzed functionalization of medium-chain-length polyhydroxyalkanoates. Journal of Chemical Technology & Biotechnology 2013, 88, 1328–1335. [Google Scholar] [CrossRef]
- Stieven Montagna, L.; Amaral Montanheiro, T.L.d.; Chiodi Borges, A.; Yumi Koga-Ito, C.; Paula Lemes, A.; Cerqueira Rezende, M. Biodegradation of PHBV/GNS nanocomposites by Penicillium funiculosum. Journal of Applied Polymer Science 2017, 134. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





